Abstract
Ophthalmology is a rapidly growing discipline of medicine with newer ocular implants and prostheses and improvements over the older ones being constantly introduced to reduce visual morbidity. These implants and devices are an easy target for biofilm formation and predispose to various ocular infections, which at times may lead to vision-threatening complications. One of the most feared complications in ophthalmology is postoperative endophthalmitis with majority of them occurring after cataract surgeries caused by the formation of biofilm over the intraocular lenses. Similar biofilms have been found over the contact lenses, lacrimal devices, ophthalmic implants, scleral plugs, and glaucoma drainage devices, leading to infections and their subsequent failures. Biofilms also disrupt the normal physiology of the eye and cause dry eye disease. Graft rejections after penetrating keratoplasty have commonly been attributed to the formation of biofilms leading to crystalline keratopathy. Current interventions aim at prevention of biofilm formation on the devices and implants by introducing antimicrobial-coated devices and by using biomaterials which have a lesser tendency of formation of biofilm. Prevention of biofilm formation in ophthalmology is an ongoing research with newer modalities being introduced consistently for the same.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Introduction
Ophthalmology is a rapidly growing discipline of medicine and has been at the forefront of medical innovation. Newer ocular devices and implants are constantly being introduced to reduce visual morbidity. The earliest known account of ocular prosthesis dates back to as long as 2900–2800 BCE, and the evidences also suggest that Sushruta was one of the first surgeons to have performed cataract surgery. The revolution in ophthalmic implants started around world war which also gave us the first PMMA intraocular lens, courtesy of Sir Harold Ridley. Ophthalmology, since then has come a long way with constant introduction of newer implants and prosthesis and improvements over the older ones like contact lenses, scleral buckles, glaucoma drainage devices, etc. However, these devices and implants are not exempted from the clutches of the biofilm formation. As a result, device-related ocular infections pose a risk to the success of such procedures. Also, biofilms disrupt the natural ocular physiology predisposing to various ocular infections. These infections may progress to devastating levels and cause permanent complications which may cause poor visual outcomes and occasionally blindness. Role of biofilms in the diseases of the eye had been underestimated in the past, but with better diagnostic and isolation modalities, more and more disease conditions of the eye are being attributed to the formation of biofilms.
The common biofilm-related infections of the eye include endophthalmitis, keratitis, scleral buckle infections, lacrimal system infections, and periorbital infections.
8.2 Endophthalmitis
Endophthalmitis is undoubtedly one of the most dreaded conditions in ophthalmology accounting for the most number of clinical eviscerations (45.5%) (Chaudhry et al. 2007). Organisms may enter intraocular tissues exogenously (after intraocular surgeries, intravitreal injections, penetrating open globe injury, and perforating corneal ulcers) or endogenously from a distant focus (Sadaka et al. 2012).
Postoperative endophthalmitis forms the majority of the cases, among which the most commonly encountered is the entry of bacteria post-cataract surgery. Cataract extraction along with intraocular lens implantation is the most commonly performed procedure by ophthalmologists worldwide, and postoperative endophthalmitis is the most common complication of cataract surgery causing blindness. The incidence of endophthalmitis after cataract surgery ranges from 0.028 to 0.2%, depending upon the technique used as well as according to the geographical distribution (Taban et al. 2005; West et al. 2005; Wykoff et al. 2010).
Organisms forming the ocular surface flora are the predominant causative agents of the endophthalmitis after cataract surgery. 76–90% of the culture-positive pseudophakic endophthalmitis is caused by gram-positive bacteria. In 38–59% cases of acute onset postoperative endophthalmitis, the cultures have been found to be positive for Staphylococcus epidermidis (a coagulase-negative staphylococci—CoNS (Driebe et al. 1986). While delayed-onset endophthalmitis is commonly caused by Propionibacterium acnes (Shirodkar et al. 2012), rarely, enterococcal endophthalmitis may also be seen after cataract surgery (Scott et al. 2003). Despite rigorous measures and intensive interventions, enterococcal endophthalmitis is associated with poor visual outcomes. Electrostatic forces cause bacterial adherence to the intraocular lenses which may get attached to the lens surface (26%) due to wiping of the lens around the wound at the time of intraocular lens implantation (Vafidis et al. 1984). Periocular skin and the eyelashes form the major pool of endophthalmitis causing bacterial source. Evidence suggests that bacteria are also capable of forming biofilms on the posterior capsular bag (Sawusch et al. 1989). After uneventful cataract surgery, the contamination of the anterior chamber has been reported to be found in 2–46% of the cases, the rate of which is higher than that of postoperative infection. This suggests that rapid turnover of the aqueous humor causes clearing of the bacterial inoculum from the anterior chamber which prevents its progression to endophthalmitis. Vitreous, on the other hand, is more stable and hence clearing of microbes attached to IOL surface is slow and inefficient. The intraocular lens provides an abiotic surface for the bacteria to form a biofilm; therefore, normal clearance mechanisms from anterior chamber are rendered futile.
The capability of bacteria of forming biofilm over IOL depends largely upon the material of the IOL as well as the species of organism. While S. epidermidis adheres firmly to polymethylmethacrylate (PMMA), Staphylococci have been found to have better adherence to polypropylene than PMMA (Sawusch et al. 1989). Epidemiological evidences suggest that polypropylene haptics increase the risk of endophthalmitis up to 4.5 times (Menikoff et al. 1991).
The ica locus plays an important role in staphylococcal biofilm formation. Studies from Japan, Mexico, and India have shown CoNS to be positive for icaA and icaD as well as icaAD gene locus (Suzuki et al. 2005; Makki et al. 2011; Juarez-Verdayes et al. 2013). In in vitro models, silicone is shown to have higher vulnerability toward biofilm formation, which is closely followed by hydrophobic acrylic and PMMA. Hydrophilic acrylic shows least propensity toward bacterial adherence (Baillif et al. 2018).
Various modifications in the surface of IOLs have been made to increase their water content by the use of different agents like methacryloyloxyethyl phosphorylcholine (MPC), heparin, and fluorine. In order to decrease the incidence of endophthalmitis, further developments are required in the form of medications which may cause disruption of the biofilms apart from making of IOLs of such material which can prevent the formation of biofilm altogether.
8.3 Contact Lens Associated Keratitis
Biofilms have been observed on contact lenses which are believed to cause microbial keratitis.
Of the predisposing risk factor for infectious keratitis, most common is the use of contact lenses. Both gram-negative (Pseudomonas aeruginosa and Serratia spp.) and gram-positive organisms (Staphylococcus aureus) have been found to cause bacterial keratitis (Cheng et al. 1999). Among protozoa, Acanthamoeba is the most common pathogen causing infectious keratitis, the incidence of which is rare but vision-threatening and often takes an aggressive course (Hammersmith 2006). The causative organisms gain access through contaminated lens care materials, lens cases and manual contaminations due to improper cleaning of the contact lenses, poor hygiene, and long-wearing time. Extended wear soft contact lenses, as well as daily disposable and silicone hydrogel contact lenses, pose a greater risk of keratitis in contrast to daily-wear rigid gas permeable lenses (Dart et al. 2008).
The incidence of infection being more among the contact lens users may be attributed to a combined effect of corneal epithelial damage and inoculation of contact lenses by colony-forming bacteria. Wearing contact lens leads to reduced corneal epithelial barrier function, either mechanically, due to accumulation of debris under the lens during night-time wear or due to friction and pressure from normal blinking during daytime wear. This causes the progress of infection originating from ocular surface, adnexa or biofilms over the contact lens, into the deeper corneal layers. These biofilms render the bacteria resistant to host mucosal defenses and antimicrobial treatment. The periodic release of organisms or their products such as endotoxins further damages the corneal epithelium, making it more vulnerable to infections. (Willcox et al. 2001; Zegans et al. 2005)
Contact lenses also induce corneal hypoxia and hypercapnia, thus affecting the epithelial response to the damage. Compromisation of the tear fluid exchange also limits the antimicrobial properties of the lens by alterations in the tear film composition.
Hence, contact lenses contribute to corneal infections by providing an adequate surface for bacteria to form biofilms, inducing corneal hypoxia and damage to the corneal epithelial cells.
8.4 Crystalline Keratopathy
Infectious crystalline keratopathy (ICK), a rare form of microbial keratitis, may occur in both normal as well as compromised corneas, following penetrating keratoplasty in corneal grafts or around sutures (Gorovoy et al. 1983; Reiss et al 1986). The main feature of ICK is branching crystalline opacities in the corneal epithelium and stroma and minimum inflammatory response. The most common pathogen associated with ICK is viridans streptococci. Other bacterial and fungal species like staphylococci, Candida, and Enterobacter and Acanthamoeba are also known to cause ICK.
The periodic acid–Schiff (PAS) stain of the corneal samples obtained from the patients of ICK indicates high concentrations of polysaccharides. The levels of polysaccharides are associated with the ability of bacteria to form biofilms which are well-organized multicellular structures. Topical corticosteroid therapy for extended period of time and prior penetrating keratoplasty has been found to be important risk factors of ICK (Fulcher et al. 2001). The features of ICK can be explained by the formation of a biofilm on the corneal lamellae, though the underlying mechanism is yet to be explained. It is proposed that anatomical changes resulting from keratoplasty cause inflammation and immunological activity, which encourage biofilm growth by the causative organism.
ICK is highly resistant and hence is unresponsive to rigorous antimicrobial treatment. More recently, disruption of biofilms using Nd:YAG laser along with further antimicrobial therapy has been proposed (Masselos et al. 2009).
8.5 Dry Eye
Dry eye disease is a complex of multiple etiologies; hence, the disease presentation is usually overlapping. A new theory of dry eye has recently emerged which combines blepharitis and dry eye into one simple condition, dry eye blepharitis syndrome (DEBS) (Rynerson and Perry 2016).
It is proposed that biofilms have a significant role in causation of DEBS. Biofilms are formed on the surfaces that provide moisture and nutrients. The eyelid margin provides an ideal habitat for the bacterial biofilm to thrive due to the presence of moisture, nutrients, and warmth. It is proposed that biofilm formation commences right after birth with colonization of the lids by bacteria. Many factors such as medications, hormonal state, and reduced blinking, exacerbate dry eye, but the underline etiology originates from a biofilm, which is present from infancy. This biofilm eventually achieves quorum-sensing gene activation and releases virulence factors.
DEBS is caused by Staphylococcus aureus in all age groups but how early in life is the presentation of symptoms of DEBS is dependent on the strain of S. aureus.
Four stages of DEBS are suggested being affected by biofilm in a sequential manner:
-
Stage I—folliculitis: inflammation and edema of lash follicles.
-
Stage II—meibomian gland dysfunction: impaction and inflammation of the meibomian gland.
-
Stage III—lacrimitis: impaction and inflammation of the glands of Krause and Wolfring.
-
Stage IV—breakdown of structural integrity of eyelids leading to chronic inflammatory lid disease presenting as lid laxity, entropion, ectropion, and floppy eyelid syndrome.
Hence, it is required that patients should be educated about eyelid hygiene and prevention of blepharitis so that the chronic problem of DEBS can be drastically reduced. With growing knowledge regarding the role of biofilms in dry eye syndrome, microblepharoexfoliation using a device called BlephEx has shown promising results in treatment of DEBS. In this procedure, a rotary device with a sponge tip is used along with an eyelid cleanser to remove biofilms from the eyelid margins and eye lashes. This has proven more effective than any other measure.
8.6 Ocular Implants and Biofilms
8.6.1 Conjunctival Plug
Conjunctival plugs employed to treat dry eye are made of silicon, hydrophobic acrylic, collagen, and hydrogels. Secondary infections can occur following implantation of these plugs. These conditions usually have delayed onset and are unresponsive to treatment, hence, they are presumed to be caused due to biofilm formation on the implant (Yokoi et al. 2000). These infections can range from canaliculitis, dacryocystitis to conjunctivitis. When punctal plugs from patients without any symptomtic infection were removed and examined, 53% of the samples showed the presence of bacterial biofilms (Sugita et al 2001). Yokoi et al. demonstrated S. haemolyticus and Candida tropicalis in the conjunctival plug removed from a case reported to have developed conjunctivitis in the eye following the implant.
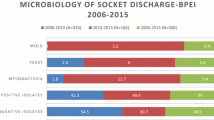
8.6.2 Scleral Buckles
Scleral buckles made of silicon are largely employed in the treatment of rhegmatogenous retinal detachment. Gram-positive cocci, in particular coagulase-negative staphylococci, nontuberculous mycobacterium (M. chelonae) and Proteus mirabilis are commonly found to cause infections of the scleral buckles. Presence of biofilms has been found on 65% of scleral buckles removed for infection and extrusion, as demonstrated by electron microscopy (Holland et al. 1991; Pathengay et al. 2004).
It is possible that bacteria attach to the buckle at the time of surgery and form biofilms which lead to indolent infections. Biofilm formation on these prosthetic devices may cause chronic inflammation and tissue damage due to cytotoxic damage by the bacteria as well as the host response to the planktonic cells shed by the biofilm (Costerton et al. 1999).
8.6.3 Lacrimal Intubation Devices
Lacrimal stents and Jones tube often employed in the treatment of chronic dacryocystitis provide a surface for biofilm formation by microorganisms. Failure of polyurethane stents, as well as infections following placement of silicone or Jones tube, has been attributed to formation of biofilms on these devices as demonstrated by scanning electron microscopy. Staphylococcus aureus, Streptococcus epidermidis, and Pseudomonas aeruginosa have been found to cause the majority of these implant-related biofilms (Kim et al. 2018).
Ali et al. (2017), in a study, found that the Monoka stents removed showed evidence of biofilm formation and physical deposits. The external surfaces, cut ends as well as intraluminal surfaces were all involved with the ampullary portion of the stent head being the most common site of deposition. Longer duration of the stent retention was associated with more extensive biofilm formation with more widespread deposits in stents retained for three months than those retained for six weeks.
8.6.4 Orbital Implants
Samimi et al., in a study, demonstrated biofilm formation in periorbital biomaterials. The orbital implants such as orbital plates and anophthalmic socket implants, all demonstrated biofilm deposits. The organisms demonstrated, varied from S. aureus, gram-negative bacilli such as Achromobacter and Pseudomonas, M. chelonae, Pantoea agglomerans, to yeasts such as Candida and Trichosporon. A greater undertaking of the role of biology of biofilms may help prevent complications related to these prosthetic devices.
8.6.5 Other Biomaterials Used in Ophthalmology
Recently, biofilm formation has been implicated in the pathogenesis of infections associated with keratoprosthesis and glaucoma drainage devices as they may provide a suitable surface for bacterial inoculation and environment for biofilms to thrive. A few cases have recently been reported in which role of biofilm formation in glaucoma drainage device has been suspected (Masood et al. 2016; Esporcatte et al. 2016). Jassim et al. (2015) found that 85% of the eyes with Boston type 1 K-Pro Keratoprosthesis had positive cultures of which 57.7% had biofilm-forming capacity. The coagulase-negative staphylococcus isolated from these K-Pro eyes had reduced susceptibility to vancomycin. Further investigation is required to look for the contribution of biofilms in the causation of these infections.
8.7 Prevention and Treatment of Biofilms
Given the dreaded outcomes of ocular biofilms, it becomes important to incorporate practices to remove the biofilm or reduce its formation. Current interventions aim at prevention of biofilm formation on the devices and implants. Biocidal molecules can be covalently attached to slowly release antibiotics or modify the surface to prevent colonization of surfaces (Bispo et al. 2015).
Biocide-coated and antimicrobial-releasing ophthalmic devices are in research. IOL coated with antimicrobials like rifampicin, doxycycline, and norfloxacin are being tested on animal models. Other substances that have shown promising results in preventing biofilm formation are gallium nitrate and silver. However, the long-term exposure of ocular tissue to these antimicrobial treatments and development of resistant strains may pose a threat to the advancement of these implants.
Biofilm-related infections can also be reduced by using materials with a lower predisposition for biofilm formation such as one-piece PMMA intraocular lenses (Elder et al. 1995). Polymers, such polyacrylamide, dextran, or polyethylene glycol, and also nanopores, nanotubes, and nanopillars made of anodized aluminum, titanium dioxide, or polymethylmethacrylate prevent adherence of biofilm-forming organisms (Samimi et al. 2013). However, changes in the material surface may cause opacities, hence limiting its use.
New therapeutic strategies are being suggested and experimented everyday to prevent the formation of biofilm and elimination of organisms in a formed biofilm. Strategies are required to reduce enzymatic degradation of antibiotics within the biofilm, to change nutrition to the biofilm-forming bacteria, and possibly, to alter gene expression which can offer resistance to biofilm formation.
References
Ali MJ, Baig F, Lakhsman M, Naik MN (2017) Scanning electron microscopic features of extubated monoka stents. Ophthalmic Plast Reconstr Surg 33:90–92. https://doi.org/10.1097/IOP.0000000000000610
Baillif S, Ecochard R, Casoli E, Freney J, Burillon C, Kodjikian L (2018) Adherence and kinetics of biofilm formation of Staphylococcus epidermidis to different types of intraocular lenses under dynamic flow conditions. J Cataract Refract Surg 34:153–158. https://doi.org/10.1016/j.jcrs.2007.07.058
Bispo PJ, Haas W, Gilmore MS (2015) Biofilms in infections of the eye. Pathogens 4:111–136. https://doi.org/10.3390/pathogens4010111
Chaudhry IA, AlKuraya HS, Shamsi FA, Elzaridi E, Riley FC (2007) Current indications and resultant complications of evisceration. Ophthalmic Epidemiol 14:93–97. https://doi.org/10.1080/09286580600943598
Cheng KH, Leung SL, Hoekman HW, Beekhuis WH, Mulder PG, Geerards AJ, Kijlstra A (1999) Incidence of contact-lens-associated microbial keratitis and its related morbidity. Lancet 354:181–185. https://doi.org/10.1016/S0140-6736(98)09385-4
Costerton JW, Stewart PS, Greenberg EP (1999) Bacterial biofilms: a common cause of persistent infections. Science 284:1318–1322. https://doi.org/10.1126/science.284.5418.1318
Dart JK, Radford CF, Minassian D, Verma S, Stapleton F (2008) Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology 115:1647–1654. https://doi.org/10.1016/j.ophtha.2008.05.003 Epub 2008 Jul 2
Driebe WT Jr, Mandelbaum S, Forster RK, Schwartz LK, Culbertson WW (1986) Pseudophakic endophthalmitis. Diagnosis and management. Ophthalmology 93:442–448. https://doi.org/10.1016/s0161-6420(86)33722-9
Elder MJ, Stapleton F, Evans E, Dart JK (1995) Biofilm-related infections in ophthalmology. Eye (Lond) 9:102–109. https://doi.org/10.1038/eye.1995.16
Esporcatte BLB, Teixeira LF, Rolim-de-Moura C (2016) Panophthalmitis with orbital cellulitis following glaucoma drainage implant surgery in a pediatric patient. Arq Bras Oftalmol 79:123–125. https://doi.org/10.5935/0004-2749.20160037
Fulcher TP, Dart JK, McLaughlin-Borlace L, Howes R, Matheson M, Cree I (2001) Demonstration of biofilm in infectious crystalline keratopathy using ruthenium red and electron microscopy. Ophthalmology 108:1088–1092. https://doi.org/10.1016/s0161-6420(01)00561-9
Gorovoy MS, Stern GA, Hood CI, Allen C (1983) Intrastromal noninflammatory bacterial colonisation of a corneal graft. Arch Ophthalmol 101:1749–1752. https://doi.org/10.1001/archopht.1983.01040020751018
Hammersmith KM (2006) Diagnosis and management of Acanthamoeba keratitis. Curr Opin Ophthalmol 17:327–331. https://doi.org/10.1097/01.icu.0000233949.56229.7d
Holland SP, Pulido JS, Miller D, Ellis B, Alfonso E, Scott M, Costerton JW (1991) Biofilm and scleral buckle-associated infections. A mechanism for persistence. Ophthalmology 98:933–938. https://doi.org/10.1016/S0161-6420(91)32199-7
Jassim SH, Sivaraman KR, Jimenez JC, Jaboori AH, Federle MJ, de la Cruz J, Cortina MS (2015) Bacteria colonizing the ocular surface in eyes with Boston type 1 keratoprosthesis: analysis of biofilm-forming capability and vancomycin tolerance. Invest Ophthalmol Vis Sci 56:4689–4696. https://doi.org/10.1167/iovs.15-17101
Juarez-Verdayes MA, Ramon-Perez ML, Flores-Paez LA, Camarillo-Márquez O, Zenteno JC et al (2013) Staphylococcus epidermidis with the icaa(−)/icad(−)/is256(−) genotype and protein or protein/extracellular-DNA biofilm is frequent in ocular infections. J Med Microbiol 62:1579–1587. https://doi.org/10.1099/jmm.0.055210-0 Epub 2013 Jul 16
Kim DJ, Park J-H, Chang M (2018) Species-specific characteristics of the biofilm generated in silicone tube: an in vitro study. BMC Ophthalmol 18:85. https://doi.org/10.1186/s12886-018-0750-1
Makki AR, Sharma S, Duggirala A, Prashanth K, Garg P, Das T (2011) Phenotypic and genotypic characterization of coagulase negative staphylococci (CoNS) other than Staphylococcus epidermidis isolated from ocular infections. Invest Ophthalmol Vis Sci 52:9018–9022. https://doi.org/10.1167/iovs.11-7777
Masood I, Shah P, Benjamin M, Salloukh AE, Sii F (2016) Recurrent glaucoma drainage device erosion associated with occult infection with biofilm-producing organisms. Br Microbiol Res J 17:1–5. https://doi.org/10.9734/BMRJ/2016/28289
Masselos K, Tsang HH, Ooi JL, Sharma NS, Coroneo MT (2009) Laser corneal biofilm disruption for infectious crystalline keratopathy. Clin Exp Ophthalmol 37:177–180. https://doi.org/10.1111/j.1442-9071.2008.01912.x Epub 2008 Dec 29
Menikoff JA, Speaker MG, Marmor M, Raskin EM (1991) A case-control study of risk factors for post-operative endophthalmitis. Ophthalmology 98:1761–1768. https://doi.org/10.1016/s0161-6420(91)32053-0
Pathengay A, Karosekar S, Raju B, Sharma S, Das T (2004) Hyderabad Endophthalmitis Research Group. Microbiologic spectrum and susceptibility of isolates in scleral buckle infection in india. Am J Ophthalmol 138:663–664. https://doi.org/10.1016/j.ajo.2004.04.056
Reiss GR, Campbell RJ, Bourne WM (1986) Infectious crystalline keratopathy. Surv Ophthalmol 31:69–72. https://doi.org/10.1016/0039-6257(86)90053-6
Rynerson JM, Perry HD (2016) DEBS - a unification theory for dry eye and blepharitis. Clin Ophthalmol 10:2455–2467. https://doi.org/10.2147/OPTH.S114674
Sadaka A, Durand ML, Gilmore MS (2012) Bacterial endophthalmitis in the age of outpatient intravitreal therapies and cataract surgeries: Host-microbe interactions in intraocular infection. Prog Retin Eye Res 31:316–331. https://doi.org/10.1016/j.preteyeres.2012.03.004
Samimi DB, Bielory BP, Miller D, Johnson TE (2013) Microbiologic trends and biofilm growth on explanted periorbital biomaterials: a 30-year review. Ophthalmic Plast Reconstr Surg 29:376–381. https://doi.org/10.1097/IOP.0b013e31829a7313
Sawusch MR, Michels G, Stark WJ, Bruner WE, Annable WL, Green WR (1989) Endophthalmtis due to Propionibacterium acnes sequestered between iol optic and posterior capsule. Ophthalmic Surg 20:90–92. https://doi.org/10.3928/1542-8877-19890201-04
Scott IU, Loo RH, Flynn HW Jr, Miller D (2003) Endophthalmitis caused by Enterococcus faecalis: antibiotic selection and treatment outcomes. Ophthalmology 110:1573–1577. https://doi.org/10.1016/S0161-6420(03)00502-5
Shirodkar AR, Pathengay A, Flynn HW Jr, Albini TA, Berrocal AM, Davis JL, Lalwani GA, Murray TG, Smiddy WE, Miller D (2012) Delayed-versus acute-onset endophthalmitis after cataract surgery. Am J Ophthalmol 153:391–398.e2. https://doi.org/10.1016/j.ajo.2011.08.029 Epub 2011 Oct 25
Sugita J, Yokoi N, Fullwood NJ, Quantock AJ, Takada Y, Nakamura Y, Kinoshita S (2001) The detection of bacteria and bacterial biofilms in punctal plug holes. Cornea 20:362–365. https://doi.org/10.1097/00003226-200105000-00005
Suzuki T, Kawamura Y, Uno T, Ohashi Y, Ezaki T (2005) Prevalence of Staphylococcus epidermidis strains with biofilm-forming ability in isolates from conjunctiva and facial skin. Am J Ophthalmol 140:844–850. https://doi.org/10.1016/j.ajo.2005.05.050
Taban M, Behrens A, Newcomb RL, Nobe MY, Saedi G, Sweet PM, McDonnell PJ (2005) Acute endophthalmitis following cataract surgery: a systematic review of the literature. Arch Ophthalmol 123:613–620. https://doi.org/10.1001/archopht.123.5.613
Vafidis GC, Marsh RJ, Stacey AR (1984) Bacterial contamination of intraocular lens surgery. Br J Ophthalmol 68:520–523. https://doi.org/10.1136/bjo.68.8.520
West ES, Behrens A, McDonnell PJ, Tielsch JM, Schein OD (2005) The incidence of endophthalmitis after cataract surgery among the U.S. Medicare population increased between 1994 and 2001. Ophthalmology 112:1388–1394. https://doi.org/10.1016/j.ophtha.2005.02.028
Willcox MD, Harmis N, Cowell, Williams T, Holden (2001) Bacterial interactions with contact lenses; effects of lens material, lens wear and microbial physiology. Biomaterials 22:3235–3247. https://doi.org/10.1016/s0142-9612(01)00161-2
Wykoff CC, Parrott MB, Flynn HW Jr, Shi W, Miller D, Alfonso EC (2010) Nosocomial acute-onset postoperative endophthalmitis at a university teaching hospital (2002–2009). Am J Ophthalmol 150:392–398.e2. https://doi.org/10.1016/j.ajo.2010.04.010 Epub 2010 Jul 8
Yokoi N, Okada K, Sugita J, Kinoshita S (2000) Acute conjunctivitis associated with biofilm formation on a punctal plug. Jpn J Ophthalmol 44:559–560. https://doi.org/10.1016/S0021-5155(00)00214-8
Zegans ME, Shanks RM, O’Toole GA (2005) Bacterial biofilms and ocular infections. Ocul Surf 3:73–80. https://doi.org/10.1016/j.ophtha.2005.02.028
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Garg, P., Garg, R., Raj, P. (2019). Biofilm-Mediated Diseases of the Eye. In: Kumar, S., Chandra, N., Singh, L., Hashmi, M., Varma, A. (eds) Biofilms in Human Diseases: Treatment and Control. Springer, Cham. https://doi.org/10.1007/978-3-030-30757-8_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-30757-8_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-30756-1
Online ISBN: 978-3-030-30757-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)