Abstract
The importance of cardiovascular magnetic resonance image (CMRI) in the diagnosis of myocarditis is highlighted in the scientific statements on myocarditis from the European Society of Cardiology (ESC) and the American Heart Association (AHA). Nowadays, CMRI-based diagnosis, CMRI in combination with measurement of high sensitivity troponin levels, has become the non-invasive gold standard of myocarditis and is widely used in clinical practice. The unique ability of CMRI is that it can “image” and quantify tissue characteristics and thus provide pathophysiological information of myocardial injury in myocarditis as edema or necrosis. T2-based positive findings suggest myocardial edema, as enhanced regional myocardial signal on T2WI or increased T2 relaxation time, and T1-based positive findings suggest myocardial injury, as increased LGE, T1 relaxation time, and ECV. By the updated 2018 Lake Louise Criteria, a positive T1 marker and a positive T2 marker will provide strongest evidence of acute myocarditis. Other than diagnosis, CMRI also provides prognostic information for myocarditis. The utility of CMRI in FM is lacking. CMRI is usually not the initial diagnostic tool and is of limited value in disease monitoring in the case of FM. Future studies regarding the diagnostic and prognostic role of CMRI on FM are warranted.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
12.1 Introduction
The 1996 World Heart Federation/International Society and Federation of Cardiology (WHF/ISFC) task force defined myocarditis as an inflammatory disease of the myocardium that is diagnosed by established histological, immunological, and immunohistochemical criteria [1]. Given this definition, endomyocardial biopsy (EMB) is widely accepted as the gold standard for the diagnosis of myocarditis [1], and a definitive diagnosis of myocarditis can only be made by demonstration of inflammatory infiltrates in myocardial tissues via EMB. However, EMB has a relatively low diagnostic sensitivity [2, 3] and procedural risk, and is rarely performed in most medical centers. As a result, the diagnosis of myocarditis has been a clinical challenge for decades.
Over the past decades, the rapid advancement of cardiovascular magnetic resonance imaging (CMRI) has changed this paradigm. The hallmark is the introduction of the CMR Diagnostic Criteria (Lake Louise Criteria, LLC) for myocardial inflammation in 2009 [4]. Subsequently, scientific statements on myocarditis from the European Society of Cardiology and the American Heart Association clearly indicate the importance of CMRI in the diagnosis of myocarditis [5, 6]. In addition to evaluating the structural and functional abnormalities of the heart, the unique ability of multiparametric CMRI can also provide the pathophysiological characteristics of myocardial injury in myocarditis, including myocardial edema, hyperemia, capillary leak, and myocardial necrosis/fibrosis [7,8,9]. CMRI coupled with increased high-sensitivity troponin levels has provided a new noninvasive diagnostic work-up and has changed the management of suspected myocarditis. A CMRI-based diagnosis has been adopted more in the recently published series [10,11,12] than in the previous series, in which a biopsy-based diagnosis was usually used [13, 14].
Current studies and applications of CMRI are focused mainly on uncomplicated acute myocarditis (AM). Fulminant myocarditis (FM) can be considered AM, although with rapid onset, dramatic clinical course, and severe hemodynamic compromise, in which CMRI is usually not the initial diagnostic technique. Therefore, in this chapter, we will first describe the diagnostic and prognostic utility of CMR parameters in AM and then introduce the application of CMRI in FM, mainly based on our own studies and experiences.
12.2 Utility of CMRI in Acute Myocarditis
The CMRI manifestations of myocardial inflammation and the diagnostic utility of the CMR parameters in myocarditis are described in detail as follows.
T2-Weighted Imaging (T2WI)
T2WI has been proposed to detect myocardial edema, which appears as regional or global signal hyperintensity [15,16,17]. Edema is a typical marker of soft tissue inflammation, including myocardial inflammation. Damage to cardiomyocytes and the subsequent release of inflammatory factors lead to an increase in tissue-free water and protein content. The proton in free water has a long T2 effect in the magnetic field, and the increased free water content appears as an enhanced tissue signal on T2WI. Localized hyperintensity in T2WI represents focal myocardial edema and inflammatory lesions. An edema ratio, defined as the ratio of the signal intensity of the myocardial to adjacent skeletal muscle, is used to reflect the global T2 signal intensity and detect diffuse edema [4]. However, this ratio may yield false-negative results in the case of coexistence of myositis [18, 19]. The pooled weighted diagnostic sensitivity, specificity, and accuracy of T2WI for AM were 63%, 76%, and 68%, respectively [9]. Moreover, the T2WI scan performed within 2 weeks of symptom onset showed a higher incidence of abnormal signals [20, 21]. In addition to T2WI, novel CMRI techniques, such as quantitative T1 and T2 mapping, can also detect myocardial edema, which will be described below.
Early Gadolinium Enhancement (EGE)
In addition to increased tissue-free water content, inflammation also leads to hyperemia and capillary leakage, which increases the retention of the contrast agent. T1-weighted CMR images acquired before and after the administration of an extracellular gadolinium-based contrast agent (GBCA) can be used to analyze the retention of the contrast agent. Retention can be quantified using the EGE ratio, defined as the ratio of the early myocardial signal intensity after GBCA injection to the signal intensity in a skeletal muscle reference region. A ratio of ≥4.0 is believed to be EGE positive and is consistent with inflammation. Alternatively, the retention of GBCA can be analyzed semi-quantitatively by calculating the increase in myocardial signal intensity after early injection of GBCA [4, 8, 9]. A value of more than 45% relative to that before injection is pathological and indicates the presence of inflammation. The pooled weighted diagnostic sensitivity, specificity, and accuracy of EGE for AM are 66%, 70%, and 67%, respectively [9].
Late Gadolinium Enhancement (LGE)
If a myocardial injury caused by inflammation is severe enough, irreversible myocardial injury occurs, such as myocardial necrosis, fibrosis, and scarring, which can further increase GBCA accumulation and cause a hyperintense signal in the images acquired following a delay (usually 10 min) after contrast agent administration. Therefore, LGE has traditionally been considered to demonstrate irreversible injury and necrosis [4, 21,22,23]. However, studies have shown temporal changes in LGE content in AM and the histological correlation between LGE and active inflammation [24, 25]. LGE likely represents a reversible and irreversible injury in the acute phase of myocarditis but only an irreversible injury in the chronic phase. Overall, LGE is not specific for active or acute inflammation, and it alone cannot reliably differentiate acute from chronic myocardial injury [4, 8]. Of note, LGE had a higher signal-to-noise ratio, indicating myocardial necrosis and fibrosis. When the appropriate T1 time was selected, normal myocardial tissue showed a low signal, while the necrotic area had more contrast agent retention and showed a markedly enhanced signal. However, LGE imaging may not be sensitive to diffuse myocardial injury because it requires a normal myocardium as reference [26].
Additionally, the LGE distribution pattern is valuable in differentiating myocardial injury caused by inflammation from other etiologies, such as myocardial ischemia. In the case of myocarditis, the LGE pattern tends to be patchy and predominantly involves the sub-epicardium with a variable extension of the intramyocardial, in contrast to myocardial ischemic lesions that are mainly sub-endocardial and transmural, followed by coronary territories. The LGE “non-ischemic inflammatory injury” pattern shows high specificity and low sensitivity to diagnose myocarditis [4, 27]. The distribution and content of LGE may also predict the outcomes of patients with AM, and patients with LGE in the interventricular septum have a poor prognosis [28].
12.3 Lake Louise Criteria (LCC)
The three CMRI techniques discussed above were combined to form the consensus criteria for CMR in myocardial inflammation, first published in 2009 as “Lake Lousie Criteria” [4]. The original criteria proposed three major diagnostic targets using three corresponding tissue characterization techniques: (1) myocardial edema detected by T2-weighted imaging (T2WI); (2) cardiac hyperemia and capillary leak evaluated by EGE; and (3) myocardial necrosis and fibrosis assessed by LGE. A high probability of AM was suggested if two of the three above criteria were positive by CMRI.
Earlier studies reported a diagnostic accuracy, sensitivity, and specificity of 78%, 67%, and 91%, respectively [4, 15], for the 2009 LCC. Since then, these criteria have been widely used both clinically and in studies of myocardial inflammatory diseases. A recently published review and meta-analysis showed a diagnostic accuracy, sensitivity, and specificity of 83%, 80%, and 87%, respectively [9], based on pooled data for the 2009 LCC. Overall, the original LCC has good diagnostic performance, and in the clinical setting of suspected myocardial inflammation, the diagnosis of AM can be considered if two out of the three criteria are positive.
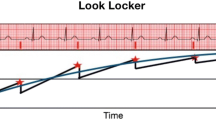
12.4 Novel CMR Mapping Techniques
In recent years, advances in CMRI technology, especially the development of cardiac mapping techniques (T1 mapping, T2 mapping, and extracellular volume [ECV]), have allowed the direct quantification of the characteristics of myocardial tissue. A quantitative myocardial map can be produced pixel by pixel, providing regional and global T1 or T2 values of the tissue. ECV was calculated by T1 mapping changes before and after GBCA injection and then adjusted by the hematocrit value. Each tissue has a normal range of T1/T2 and ECV values for the specific methods and protocols used, and changes in these values can identify pathological conditions [29, 30]. CMR mapping techniques have the advantage of not relying on relative signal intensity changes, less observer variability, and less artifacts. Moreover, native T1 and T2 mappings have the advantage of not requiring contrast agent administration. Recently, cardiac mapping techniques have been increasingly applied in myocarditis, and multiple studies have described their excellent diagnostic accuracy in myocarditis [9, 29,30,31].
Cardiac mapping is affected not only by the internal characteristics of tissues but also by different MRI systems, mapping approaches, and methods. Standardized mapping methods and protocols, as well as normal ranges and diagnostic thresholds for specific pathological conditions, including myocarditis, remain being established [32, 33].
T2 Mapping
T2 mapping allows direct measurement of water-induced myocardial relaxation time, and thus increased T2 relaxation time in the myocardium, reflecting increased tissue water content (edema) [34]. Recent data have shown that T2 mapping has higher diagnostic accuracy than traditional T2WI in detecting active inflammation. It may be particularly valuable for ruling out acute or active myocarditis and distinguishing active from healing inflammation [35, 36]. Therefore, in the absence of acute myocardial ischemia, an increase in T2 relaxation time is specific for and is an important marker of acute inflammation [36, 37].
Native T1 Mapping
T1 relaxation time is highly sensitive to the increase in free water content in the myocardium caused by acute and chronic inflammation. Meanwhile, vascular dilation, congestion, and tissue space volume expansion caused by acute inflammation can also increase T1 relaxation time [38]. Compared with T2 mapping, T1 relaxation time is less specific for acute myocardial inflammation and edema and may not be useful to distinguish acute inflammation from chronic inflammation [18, 37, 38]. Overall, T1 is a sensitive index for diagnosing myocardial inflammation, and its negative predictive value for myocardial inflammation was 92% [9, 36]. It alone is not specific for the activity of the disease and may be best paired with T2-based imaging to detect AM.
Extracellular Volume (ECV) Mapping
The quantification of ECV requires the administration of a contrast agent, and the percentage of ECV is then estimated using T1 maps acquired before and after GBCA administration. ECV expansion reflects increased extracellular tissue space in myocarditis compared with LGE; ECV can detect mild and diffuse edema and fibrosis, which may not be detected by LGE [29, 30]. Therefore, it can be used as an additional indicator to detect inflammatory lesions in myocarditis [30]. More data are needed to verify its diagnostic performance alone and in combination with other CMR mapping parameters.
12.5 Functional Abnormalities
Cardiac dysfunction results from myocardial inflammation and can occur as regional or global left ventricular dysfunction. In mild cases, the ejection fraction may be normal, even in the presence of elevated T2 or LGE. Wall motion abnormalities and ventricular systolic dysfunction may be caused by other conditions, such as ischemic heart disease. Therefore, functional abnormalities are neither sensitive nor specific to the diagnosis of myocarditis and can only be used as supporting evidence of myocarditis. However, in patients with suspected myocarditis, severe ventricular systolic dysfunction usually indicates more extensive myocardial involvement.
12.6 Pericardial Abnormalities
Myocarditis can involve the pericardium and vice versa. Of note, the presence of pericardial effusion alone cannot be used as a marker of active pericarditis, as it may only be a manifestation of heart failure coexisting with myocarditis. Active pericardial inflammation is likely in the presence of pericardial thickening in high-resolution fast spin-echo T1 images, pericardial high signal in T2WI and T1/T2 mapping, and abnormal pericardial LGE. Pericardial active inflammation can be used as supporting evidence of myocarditis [39].
12.7 Update to the LCC
With more data that prove the diagnostic performance of CMR mapping techniques, the original 2009 LLC was updated in 2018 by incorporating the novel cardiac mapping parameters discussed above (Central Illustration in Fig. 12.1) [8]. The updated 2018 criteria proposed the following two categories of CMRI parameters to support myocardial inflammation: (1) T2-based markers of myocardial edema: T2 weighted imaging or T2 mapping; (2) T1-based markers of myocardial injury: delayed enhancement (LGE), T1 mapping, or ECV. In the revised criteria, EGE was removed and superseded by T1 quantification. The Consensus Group recommends that in patients with a high pretest clinical probability of AM, having both positive T1 and T2 markers will provide the strongest evidence of acute myocardial inflammation with high specificity; having only one of the two markers may still support a diagnosis of acute myocardial inflammation, albeit with less specificity [8]. The updated criteria also include functional and pericardial abnormalities as supporting evidence for the diagnosis of myocarditis.
The updated 2018 criteria represent a “two out of two” approach, and different combinations may have different diagnostic performances. The combination of T2 mapping and LGE produces very good diagnostic accuracy, according to two published studies [36, 37]. Combining T2-based CMR with native T1-mapping is attractive because it does not require contrast agent administration. Combining T2 mapping and ECV may increase sensitivity in cases of diffuse edema where LGE may be negative. A recent study compared the original LCC with the updated 2018 criteria in a cohort and demonstrated better diagnostic performance for the updated criteria, with a sensitivity of 87.5% and a specificity of 96.1% [40].
12.8 Utility of CMRI in FM
In contrast to acute non-FM, the utility of CMRI in FM has not been systematically studied, but individual reports and personal experiences of experts. A small study at our center has described the appearance of CMRI and the application of multiparametric CMR in detecting and monitoring myocardial inflammatory injury in FM [41]. Here, we describe the appearance of FM based on our experience and unpublished data. It is worth noting that CMRI is usually not the initial diagnostic modality for FM. In our center, the CMRI examination time in most patients was in the convalescence stage, usually a few days before discharge, and a very small percentage of patients were in the very early stage before deterioration of the disease. The median interval between patient admission and CMRI scan was 7 days, and the average hospitalization time at our center for FM was 12 days. Therefore, the characteristics of CMRI in FM summarized here may not represent the true characteristics of FM in the peak or mostly active stage of inflammatory myocardial injury, which may have the best diagnostic performance for FM.
Myocardial Edema
Compared with acute non-FM, myocardial edema in FM is usually diffuse and presents as a diffusive or global enhanced signal on T2WI (Fig. 12.2a). Some patients with FM may also present with patchy areas of edema, which are typically in a non-coronary distribution as non-complicated AM. Due to the lack of normal myocardium as a reference for diffusive edema, T2WI is likely negative and quantitative T1 and T2 mapping and ECV are superior to T2WI in the case of FM. Patients with FM had significantly higher T1 and T2 relaxation times than normal controls (Fig. 12.3a, b), indicating a wider involvement of the myocardium and more severe inflammatory injuries. In the healing stage of FM, T1 and T2 relaxation times decreased significantly but were still higher than normal controls (Fig. 12.3c, d). Therefore, T1 and T2 mappings are excellent tools to discriminate FM from healed myocarditis and are useful in monitoring changes in inflammatory myocardial injury [41].
CMRI in a 19-year-old male with a clinical diagnosis of FM. On T2WI, there was global enhanced signal in the left ventricular myocardium (a, yellow arrowheads), significant EGE (b, orange arrowheads) and LGE (c, blue arrowheads) signals in the corresponding segments, predominant involving the mid-wall and sub-epicardium myocardium, and involving the left ventricular septum
T1 and T2 mapping in the same patient as in the Fig. 12.1. (a) and (b) showed significantly increased T1 (1460 ms) and T2 relaxation time (48 ms); (c) and (d) showed decreased T1 (1290 ms) and T2 relaxation time (38 ms) to the level of about normal range in the repeated CMRI at 3-month follow-up visit. Normal references of T1 and T2 relaxation time are about 1240 and 40 ms in our center
Hyperemia and Capillary Leakage
EGE, assessed in T1-weighted CMR images before and shortly after GBCA administration, also appear as diffusive or global hyperintensities (Fig. 12.2b).
Myocardial Necrosis and Fibrosis
LGE are also diffusive in most patients with FM. The spatial extent of LGE is more extensive in patients with a regional LGE appearance. The sub-epicardium and mid-myocardium are predominantly involved, but some patients with FM had transmural involvement (Fig. 12.2c). It remains unclear whether patients with transmural LGE have a poor prognosis. Our unpublished data showed that LGE in most patients with FM predominantly involved the sub-epicardium and mid-myocardium, while 34% of them had transmural LGE. Meanwhile, LGE in the interventricular septum was observed in 93% of cases, followed by the inferior wall of the left ventricle; 38% of cases presented with diffuse LGE, while others presented with linear or patchy LGE. The LGE appearance in FM demonstrated that patients with FM had more extensive and severe myocardial injury than those with non-fulminant AM, which is consistent with the more severe clinical manifestations of patients with FM. However, further studies are warranted to prove whether the extent and location of LGE can predict the outcomes of FM.
Cardiac Structural and Functional Abnormalities
Compared with non-fulminant AM, all patients with FM had a variable reduction in left ventricular systolic function (Fig. 12.4a). Our unpublished data showed that the average left ventricular ejection fraction was 47.8% in patients with FM, and it is worth noting that the CMRI scans in most patients were performed in the convalescence stage at our center. In addition, patients with FM usually had a thicker interventricular septum than normal controls, with an average thickness of 10.6 mm (Fig. 12.4a, b). However, the thickened septum returned to the normal range during follow-up (Fig. 12.4c, d). A previous study using echocardiography also showed a thicker interventricular septum in AM than in non-FM [42]. Overall, compared with acute non-FM, patients with FM have a greater reduction in left ventricular systolic function and greater thickness in the interventricular septum. Furthermore, patients with FM are more likely to have pericardial effusion and pericardial inflammation. In our unpublished data, 85% of patients with FM had pericardial effusion (Fig. 12.3a, b), which usually disappeared during the healing stage (Fig. 12.4c, d).
Structural and functional abnormalities showed by CMRI in a 55-year-old woman with clinical diagnosis of FM. The four-chamber and short-axis views were shown. (a and b) were initial CMRI during hospitalization, and (c and d) were repeated CMRI at 3 months follow-up. The patients had reduced LVEF (47%) that recovered to 56% at 3 months follow-up. The interventricular septum was thickened at a wall thickness of 1.2 cm initially (a and b) and decreased to normal (0.9 cm) at following-up (c and d). In addition, pericardial and bilateral pleural effusion were present initially (a and b) and disappeared at the follow-up (c and d)
12.9 Prognostic Value of CMRI in Myocarditis
CMRI is not only used as an excellent diagnostic tool, but it can also provide prognostic information for patients with myocarditis. However, studies on CMRI measurements as prognostic indicators of myocarditis are also mainly in non-fulminant AM, and the prognostic role of CMRI in FM is less investigated. In uncomplicated AM, the presence and extent of LGE may be a powerful predictor of cardiac events, and LGE located in the septum is considered to have the worst prognosis [11, 25, 43]. Another study involving 670 patients with suspected myocarditis with a median follow-up period of 4.7 years showed that septal and midwall LGE had the strongest associations with major adverse cardiovascular events (MACE) and LGE extent (per 10% increase) corresponding to a 79% increase in the risk of MACE [44]. In contrast, a normal CMR corresponded to a low annual MACE and death rate [44]. In addition to LEG, T1 and T2 mappings provide excellent performance to differentiate acute from healed myocarditis, and abnormal T2 mapping correlated with adverse outcomes [45, 46]. ECV may also have incremental value in the risk stratification of patients with suspected myocarditis [47]. A CMRI is suggested to be repeated in the follow-up in athletes with myocarditis before restarting active training [48], and the absence of edema on CMRI may be an indicator of physical activity reintroduction, as suggested by Ammirati et al. [7].
12.10 Limitations of CMRI in FM
CMRI scans take a long time to complete and cannot be performed at the bedside. Patients with FM are often hemodynamically unstable or with severe heart failure on admission. They are often treated with mechanical assistance devices in the acute stage, making it unlikely to perform CMRI scans in FM. Therefore, CMRI is not usually the initial diagnostic tool for FM. In our study, most CMRI examinations were performed in the convalescent period before discharge and therefore cannot represent true myocardial injury in the acute phase of FM. Therefore, the early clinical diagnostic value of CMRI examinations for patients with FM may be limited. For the same reason, CMRI cannot be repeated frequently and is unsuitable for dynamic monitoring of disease changes in the acute stage of bedside echocardiography. Furthermore, CMRI cannot identify the histological type of myocarditis, which has prognostic and therapeutic implications in FM [49]. In the case of FM, EMB is still recommended to characterize the histological type of FM, thus guiding optimal medical treatment [5].
12.11 Conclusion
In conclusion, CMRI can be used to “image” myocardial histological characteristics, including edema, hyperemia/capillary leakage, myocardial necrosis, and subsequent fibrosis, which means that CMRI can provide pathophysiological information on myocardial injury in myocarditis and thereafter has been a noninvasive diagnostic tool in myocarditis. New CMRI techniques, such as T1 and T2 mapping, have the advantage of quantitatively evaluating features of myocardial tissue and can provide incremental evidence of inflammatory activity. Currently, CMRI has been widely used in clinical practice as a substitute “gold standard” for EMB in the diagnosis of myocarditis. CMRI can also be used in the differential diagnosis of myocarditis and has a certain value in predicting the prognosis of the disease. Combined with elevated myocardial injury markers, such as troponin and other suspicious clinical manifestations, CMRI presentation in accordance with the diagnostic criteria of myocardial inflammation, a clinical diagnosis of myocarditis can be made.
Key Points
-
1.
Evidence of active myocardial inflammation by CMRI: First, T2 imaging suggests myocardial edema, including enhanced regional myocardial signal in T2WI, ratio of myocardial signal to adjacent skeletal muscle signal ≥2.0, or increased T2 relaxation time suggested by quantitative T2 mapping; Second, T1 imaging suggests myocardial injury, including increased LGE, T1 relaxation time, and ECV, indicating myocardial necrosis and fibrosis, myocardial hyperemia or capillary leakage, and intracellular and extracellular edema.
-
2.
Meeting two of the above criteria has the highest specific diagnostic value for AM; meeting one of the two criteria supports the diagnosis of AM in certain clinical settings.
-
3.
Other CMRI findings, including abnormal left ventricular function, pericardial effusion, pericardial thickening, as well as pericardial hyperintensity in T2WI, increased pericardial T1/T2 relaxation time, and abnormal pericardial LGE, may be supporting evidence of the presence of myocarditis.
-
4.
The characteristic manifestations of AM on CMRI can provide diagnostic evidence of myocardial inflammation and allow the diagnosis of myocarditis in patients with clinically suspected FM, and help distinguish FM from myocardial infarction.
-
5.
Although CMRI is the imaging gold standard and has a higher specificity for the diagnosis of AM, it is of limited value in early diagnosis and monitoring the dynamic changes of myocardial injury in the case of FM due to the intrinsic requirements to perform CMRI scans and the unstable status of patients with FM.
References
Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O’Connell J, Olsen E, Thiene G, Goodwin J, Gyarfas I, et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the definition and classification of cardiomyopathies. Circulation. 1996;93:841–2. https://doi.org/10.1161/01.cir.93.5.841.
Krieghoff C, Barten MJ, Hildebrand L, Grothoff M, Lehmkuhl L, Lucke C, Andres C, Nitzsche S, Riese F, Struber M, et al. Assessment of sub-clinical acute cellular rejection after heart transplantation: comparison of cardiac magnetic resonance imaging and endomyocardial biopsy. Eur Radiol. 2014;24:2360–71. https://doi.org/10.1007/s00330-014-3246-2.
Leone O, Veinot JP, Angelini A, Baandrup UT, Basso C, Berry G, Bruneval P, Burke M, Butany J, Calabrese F, et al. 2011 consensus statement on endomyocardial biopsy from the Association for European Cardiovascular Pathology and the Society for Cardiovascular Pathology. Cardiovasc Pathol. 2012;21:245–74. https://doi.org/10.1016/j.carpath.2011.10.001.
Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT, White JA, Abdel-Aty H, Gutberlet M, Prasad S, et al. Cardiovascular magnetic resonance in myocarditis: a JACC White Paper. J Am Coll Cardiol. 2009;53:1475–87. https://doi.org/10.1016/j.jacc.2009.02.007.
Bozkurt B, Colvin M, Cook J, Cooper LT, Deswal A, Fonarow GC, Francis GS, Lenihan D, Lewis EF, McNamara DM, et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation. 2016;134:e579–646. https://doi.org/10.1161/CIR.0000000000000455.
Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, Fu M, Helio T, Heymans S, Jahns R, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34:2636–2648, 2648a–2648d. https://doi.org/10.1093/eurheartj/eht210.
Ammirati E, Veronese G, Bottiroli M, Wang DW, Cipriani M, Garascia A, Pedrotti P, Adler ED, Frigerio M. Update on acute myocarditis. Trends Cardiovasc Med. 2021;31:370–9. https://doi.org/10.1016/j.tcm.2020.05.008.
Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U, Kindermann I, Gutberlet M, Cooper LT, Liu P, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018;72:3158–76. https://doi.org/10.1016/j.jacc.2018.09.072.
Lagan J, Schmitt M, Miller CA. Clinical applications of multi-parametric CMR in myocarditis and systemic inflammatory diseases. Int J Cardiovasc Imaging. 2018;34:35–54. https://doi.org/10.1007/s10554-017-1063-9.
Ammirati E, Cipriani M, Moro C, Raineri C, Pini D, Sormani P, Mantovani R, Varrenti M, Pedrotti P, Conca C, et al. Clinical presentation and outcome in a contemporary cohort of patients with acute myocarditis: multicenter lombardy registry. Circulation. 2018;138:1088–99. https://doi.org/10.1161/CIRCULATIONAHA.118.035319.
Aquaro GD, Perfetti M, Camastra G, Monti L, Dellegrottaglie S, Moro C, Pepe A, Todiere G, Lanzillo C, Scatteia A, et al. Cardiac MR with late gadolinium enhancement in acute myocarditis with preserved systolic function: ITAMY study. J Am Coll Cardiol. 2017;70:1977–87. https://doi.org/10.1016/j.jacc.2017.08.044.
White JA, Hansen R, Abdelhaleem A, Mikami Y, Peng M, Rivest S, Satriano A, Dykstra S, Flewitt J, Heydari B, et al. Natural history of myocardial injury and chamber remodeling in acute myocarditis. Circ Cardiovasc Imaging. 2019;12:e008614. https://doi.org/10.1161/CIRCIMAGING.118.008614.
Anzini M, Merlo M, Sabbadini G, Barbati G, Finocchiaro G, Pinamonti B, Salvi A, Perkan A, Di Lenarda A, Bussani R, et al. Long-term evolution and prognostic stratification of biopsy-proven active myocarditis. Circulation. 2013;128:2384–94. https://doi.org/10.1161/CIRCULATIONAHA.113.003092.
Kindermann I, Kindermann M, Kandolf R, Klingel K, Bultmann B, Muller T, Lindinger A, Bohm M. Predictors of outcome in patients with suspected myocarditis. Circulation. 2008;118:639–48. https://doi.org/10.1161/CIRCULATIONAHA.108.769489.
Abdel-Aty H, Boye P, Zagrosek A, Wassmuth R, Kumar A, Messroghli D, Bock P, Dietz R, Friedrich MG, Schulz-Menger J. Diagnostic performance of cardiovascular magnetic resonance in patients with suspected acute myocarditis: comparison of different approaches. J Am Coll Cardiol 2005;45:1815–22. https://doi.org/10.1016/j.jacc.2004.11.069.
Higgins CB, Herfkens R, Lipton MJ, Sievers R, Sheldon P, Kaufman L, Crooks LE. Nuclear magnetic resonance imaging of acute myocardial infarction in dogs: alterations in magnetic relaxation times. Am J Cardiol. 1983;52:184–8. https://doi.org/10.1016/0002-9149(83)90093-0.
Simonetti OP, Finn JP, White RD, Laub G, Henry DA. “Black blood” T2-weighted inversion-recovery MR imaging of the heart. Radiology. 1996;199:49–57. https://doi.org/10.1148/radiology.199.1.8633172.
Ferreira VM, Piechnik SK, Dall’Armellina E, Karamitsos TD, Francis JM, Ntusi N, Holloway C, Choudhury RP, Kardos A, Robson MD, et al. T(1) mapping for the diagnosis of acute myocarditis using CMR: comparison to T2-weighted and late gadolinium enhanced imaging. JACC Cardiovasc Imaging. 2013;6:1048–58. https://doi.org/10.1016/j.jcmg.2013.03.008.
Laissy JP, Messin B, Varenne O, Iung B, Karila-Cohen D, Schouman-Claeys E, Steg PG. MRI of acute myocarditis: a comprehensive approach based on various imaging sequences. Chest. 2002;122:1638–48. https://doi.org/10.1378/chest.122.5.1638.
Hinojar R, Foote L, Arroyo Ucar E, Jackson T, Jabbour A, Yu CY, McCrohon J, Higgins DM, Carr-White G, Mayr M, et al. Native T1 in discrimination of acute and convalescent stages in patients with clinical diagnosis of myocarditis: a proposed diagnostic algorithm using CMR. JACC Cardiovasc Imaging. 2015;8:37–46. https://doi.org/10.1016/j.jcmg.2014.07.016.
Monney PA, Sekhri N, Burchell T, Knight C, Davies C, Deaner A, Sheaf M, Baithun S, Petersen S, Wragg A, et al. Acute myocarditis presenting as acute coronary syndrome: role of early cardiac magnetic resonance in its diagnosis. Heart. 2011;97:1312–8. https://doi.org/10.1136/hrt.2010.204818.
Mavrogeni S, Spargias C, Bratis C, Kolovou G, Markussis V, Papadopoulou E, Constadoulakis P, Papadimitropoulos M, Douskou M, Pavlides G, et al. Myocarditis as a precipitating factor for heart failure: evaluation and 1-year follow-up using cardiovascular magnetic resonance and endomyocardial biopsy. Eur J Heart Fail. 2011;13:830–7. https://doi.org/10.1093/eurjhf/hfr052.
Zagrosek A, Abdel-Aty H, Boye P, Wassmuth R, Messroghli D, Utz W, Rudolph A, Bohl S, Dietz R, Schulz-Menger J. Cardiac magnetic resonance monitors reversible and irreversible myocardial injury in myocarditis. JACC Cardiovasc Imaging. 2009;2:131–8. https://doi.org/10.1016/j.jcmg.2008.09.014.
Lurz P, Eitel I, Adam J, Steiner J, Grothoff M, Desch S, Fuernau G, de Waha S, Sareban M, Luecke C, et al. Diagnostic performance of CMR imaging compared with EMB in patients with suspected myocarditis. JACC Cardiovasc Imaging. 2012;5:513–24. https://doi.org/10.1016/j.jcmg.2011.11.022.
Mahrholdt H, Wagner A, Deluigi CC, Kispert E, Hager S, Meinhardt G, Vogelsberg H, Fritz P, Dippon J, Bock CT, et al. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation. 2006;114:1581–90. https://doi.org/10.1161/CIRCULATIONAHA.105.606509.
Kim RJ, Shah DJ, Judd RM. How we perform delayed enhancement imaging. J Cardiovasc Magn Reson. 2003;5:505–14. https://doi.org/10.1081/jcmr-120022267.
Yilmaz A, Ferreira V, Klingel K, Kandolf R, Neubauer S, Sechtem U. Role of cardiovascular magnetic resonance imaging (CMR) in the diagnosis of acute and chronic myocarditis. Heart Fail Rev. 2013;18:747–60. https://doi.org/10.1007/s10741-012-9356-5.
Natale L, De Vita A, Baldari C, Meduri A, Pieroni M, Lombardo A, Crea F, Bonomo L. Correlation between clinical presentation and delayed-enhancement MRI pattern in myocarditis. Radiol Med. 2012;117:1309–19. https://doi.org/10.1007/s11547-012-0790-x.
Radunski UK, Lund GK, Saring D, Bohnen S, Stehning C, Schnackenburg B, Avanesov M, Tahir E, Adam G, Blankenberg S, et al. T1 and T2 mapping cardiovascular magnetic resonance imaging techniques reveal unapparent myocardial injury in patients with myocarditis. Clin Res Cardiol. 2017;106:10–7. https://doi.org/10.1007/s00392-016-1018-5.
Radunski UK, Lund GK, Stehning C, Schnackenburg B, Bohnen S, Adam G, Blankenberg S, Muellerleile K. CMR in patients with severe myocarditis: diagnostic value of quantitative tissue markers including extracellular volume imaging. JACC Cardiovasc Imaging 2014;7:667–75. https://doi.org/10.1016/j.jcmg.2014.02.005.
Kotanidis CP, Bazmpani MA, Haidich AB, Karvounis C, Antoniades C, Karamitsos TD. Diagnostic accuracy of cardiovascular magnetic resonance in acute myocarditis: a systematic review and meta-analysis. JACC Cardiovasc Imaging. 2018;11:1583–90. https://doi.org/10.1016/j.jcmg.2017.12.008.
Messroghli DR, Moon JC, Ferreira VM, Grosse-Wortmann L, He T, Kellman P, Mascherbauer J, Nezafat R, Salerno M, Schelbert EB, et al. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovasc Magn Reson. 2017;19:75. https://doi.org/10.1186/s12968-017-0389-8.
Moon JC, Messroghli DR, Kellman P, Piechnik SK, Robson MD, Ugander M, Gatehouse PD, Arai AE, Friedrich MG, Neubauer S, et al. Myocardial T1 mapping and extracellular volume quantification: a Society for Cardiovascular Magnetic Resonance (SCMR) and CMR Working Group of the European Society of Cardiology consensus statement. J Cardiovasc Magn Reson. 2013;15:92. https://doi.org/10.1186/1532-429X-15-92.
Fernandez-Jimenez R, Sanchez-Gonzalez J, Aguero J, Del Trigo M, Galan-Arriola C, Fuster V, Ibanez B. Fast T2 gradient-spin-echo (T2-GraSE) mapping for myocardial edema quantification: first in vivo validation in a porcine model of ischemia/reperfusion. J Cardiovasc Magn Reson. 2015;17:92. https://doi.org/10.1186/s12968-015-0199-9.
Lurz P, Luecke C, Eitel I, Fohrenbach F, Frank C, Grothoff M, de Waha S, Rommel KP, Lurz JA, Klingel K, et al. Comprehensive cardiac magnetic resonance imaging in patients with suspected myocarditis: the MyoRacer-trial. J Am Coll Cardiol. 2016;67:1800–11. https://doi.org/10.1016/j.jacc.2016.02.013.
von Knobelsdorff-Brenkenhoff F, Schuler J, Doganguzel S, Dieringer MA, Rudolph A, Greiser A, Kellman P, Schulz-Menger J. Detection and monitoring of acute myocarditis applying quantitative cardiovascular magnetic resonance. Circ Cardiovasc Imaging. 2017;10:e005242. https://doi.org/10.1161/CIRCIMAGING.116.005242.
Luetkens JA, Homsi R, Sprinkart AM, Doerner J, Dabir D, Kuetting DL, Block W, Andrie R, Stehning C, Fimmers R, et al. Incremental value of quantitative CMR including parametric mapping for the diagnosis of acute myocarditis. Eur Heart J Cardiovasc Imaging. 2016;17:154–61. https://doi.org/10.1093/ehjci/jev246.
Ferreira VM, Piechnik SK, Dall’Armellina E, Karamitsos TD, Francis JM, Ntusi N, Holloway C, Choudhury RP, Kardos A, Robson MD, et al. Native T1-mapping detects the location, extent and patterns of acute myocarditis without the need for gadolinium contrast agents. J Cardiovasc Magn Reson. 2014;16:36. https://doi.org/10.1186/1532-429X-16-36.
Bogaert J, Francone M. Cardiovascular magnetic resonance in pericardial diseases. J Cardiovasc Magn Reson. 2009;11:14. https://doi.org/10.1186/1532-429X-11-14.
Luetkens JA, Faron A, Isaak A, Dabir D, Kuetting D, Feisst A, Schmeel FC, Sprinkart AM, Thomas D. Comparison of original and 2018 lake louise criteria for diagnosis of acute myocarditis: results of a validation cohort. Radiol Cardiothorac Imaging. 2019;1:e190010. https://doi.org/10.1148/ryct.2019190010.
Li H, Zhu H, Yang Z, Tang D, Huang L, Xia L. Application of multiparametric quantitative cardiac magnetic resonance for detection and monitoring of myocardial injury in patients with fulminant myocarditis. Acad Radiol. 2021;28:e35–43. https://doi.org/10.1016/j.acra.2020.01.034.
Felker GM, Boehmer JP, Hruban RH, Hutchins GM, Kasper EK, Baughman KL, Hare JM. Echocardiographic findings in fulminant and acute myocarditis. J Am Coll Cardiol. 2000;36:227–32.
Grigoratos C, Di Bella G, Aquaro GD. Diagnostic and prognostic role of cardiac magnetic resonance in acute myocarditis. Heart Fail Rev. 2019;24:81–90. https://doi.org/10.1007/s10741-018-9724-x.
Grani C, Eichhorn C, Biere L, Murthy VL, Agarwal V, Kaneko K, Cuddy S, Aghayev A, Steigner M, Blankstein R, et al. Prognostic value of cardiac magnetic resonance tissue characterization in risk stratifying patients with suspected myocarditis. J Am Coll Cardiol. 2017;70:1964–76. https://doi.org/10.1016/j.jacc.2017.08.050.
Bohnen S, Radunski UK, Lund GK, Ojeda F, Looft Y, Senel M, Radziwolek L, Avanesov M, Tahir E, Stehning C, et al. Tissue characterization by T1 and T2 mapping cardiovascular magnetic resonance imaging to monitor myocardial inflammation in healing myocarditis. Eur Heart J Cardiovasc Imaging. 2017;18:744–51. https://doi.org/10.1093/ehjci/jex007.
Spieker M, Haberkorn S, Gastl M, Behm P, Katsianos S, Horn P, Jacoby C, Schnackenburg B, Reinecke P, Kelm M, et al. Abnormal T2 mapping cardiovascular magnetic resonance correlates with adverse clinical outcome in patients with suspected acute myocarditis. J Cardiovasc Magn Reson. 2017;19:38. https://doi.org/10.1186/s12968-017-0350-x.
Grani C, Biere L, Eichhorn C, Kaneko K, Agarwal V, Aghayev A, Steigner M, Blankstein R, Jerosch-Herold M, Kwong RY. Incremental value of extracellular volume assessment by cardiovascular magnetic resonance imaging in risk stratifying patients with suspected myocarditis. Int J Cardiovasc Imaging. 2019;35:1067–78. https://doi.org/10.1007/s10554-019-01552-6.
Eichhorn C, Biere L, Schnell F, Schmied C, Wilhelm M, Kwong RY, Grani C. Myocarditis in athletes is a challenge: diagnosis, risk stratification, and uncertainties. JACC Cardiovasc Imaging. 2020;13:494–507. https://doi.org/10.1016/j.jcmg.2019.01.039.
Ammirati E, Veronese G, Brambatti M, Merlo M, Cipriani M, Potena L, Sormani P, Aoki T, Sugimura K, Sawamura A, et al. Fulminant versus acute nonfulminant myocarditis in patients with left ventricular systolic dysfunction. J Am Coll Cardiol. 2019;74:299–311. https://doi.org/10.1016/j.jacc.2019.04.063.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Wang, H. (2022). Cardiac Magnetic Resonance in Fulminant Myocarditis. In: Wang, D.W. (eds) Fulminant Myocarditis. Springer, Singapore. https://doi.org/10.1007/978-981-19-5759-8_12
Download citation
DOI: https://doi.org/10.1007/978-981-19-5759-8_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-5758-1
Online ISBN: 978-981-19-5759-8
eBook Packages: MedicineMedicine (R0)