Abstract
Supraglottic Airway Devices belongs to a vast group of medical devices that can function as a conduit for ventilation, oxygenation, and the administering anaesthetic gases. Their adoption has steadily expanded over the past few decades, and they have become a vital instrument in contemporary anaesthesia. The introduction of Brain’s Laryngeal Mask Airway marked the beginning of a revolution as a new method for airway management, eventually replacing tracheal intubation as the most common. Initially intended for uncomplicated procedures, supraglottic airway devices (SADs) are acquiring additional uses as many advanced models with specific designs for improved ventilatory performance and increased patient safety. SADs also prove effective in emergency situations and during difficult intubation as rescue airways. When compared to the endotracheal tube (ET), their greater ease and speed of insertion, lower autonomic effect, and less post-operative discomfort for the patient are regarded as the greatest advantages. Its primary benefits include easier placement, more dependable ventilation, and hands-free operation. Several SADs have features better suited for certain conditions, which has resulted in a large number of devices being accessible concurrently, with the anesthesiologist being responsible for their selection.Here in this chapter, we discuss clinical application of supraglottic airway devices.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
-
1.
The use of supraglottic airway devices (SGADs) is associated with greater hemodynamic stability, avoidance of rise in intracranial pressure, and intraocular pressure compared to tracheal intubation and extubation.
-
2.
SGAD can be used as a conduit for intubation. The ability to continue ventilation till tracheal intubation is accomplished is a distinct advantage of SGASs in difficult airway scenarios.
-
3.
Most patients have a good view of the glottis when the fibreoptic bronchoscope is passed through the SGAD.
-
4.
Difficult airway management guidelines have incorporated SGAD both for backup and rescue indications.
-
5.
Removal of SGAD is associated with less coughing compared to extubation.
-
6.
Use of these devices in out-of-hospital cardiac arrest (OHCA) allows uninterrupted chest compression, improving the success rate.
-
7.
With the availability of appropriate size even for neonates and small infants, SGAD applications in paediatric patients have increased significantly.
1 Introduction
Supraglottic airway devices (SGADs) are used in various clinical settings, including anaesthesia, resuscitation, and intensive care (Table 19.1). The device can be considered as a milestone or a game changer in airway management. Large data has been developed over the last few decades. Reports of second-generation SADs have increased significantly in recent years. The various uses of supraglottic devices are discussed in this chapter.
2 Primary Airway Device During Routine Anaesthesia
SGADs are being used as the primary airway devices in place of endotracheal tube in an increasingly complex and wide variety of surgical and non-surgical procedures. This has resulted in a paradigm shift in airway management from a two-choice (face mask vs. ETT) framework to a three-choice (face mask vs. SGAD vs. ETT) framework. Advantages include the ability to insert without relaxant, even awake with local anaesthesia, greater hemodynamic stability, avoidance of rise in intracranial pressure, and intraocular pressure compared to tracheal intubation [1]. The use of SGAD is relatively quickly learned by medical and paramedical personnel, further broadening the indications [1].
SGADs play multiple roles in airway management incuding conduit for intubation, as a bridge to extubation, airway rescue in pre- and in-hospital environments, definitive device in elective and emergency anaesthesia, spontaneously breathing and ventilated patients [1]. Prerequisites for using SGAD as the primary device are adequate fasting status, supine position, non-laparoscopic surgery, duration of not more than 4 h, and surgeries away from the airway region. Contraindications for the use of SGAD are listed below (Table 19.2) most of which are relative. SGADs are also used in patients with difficult airway (DA) (Fig. 19.1), electively instead of endotracheal tubes. However, this statement is guarded because DA can be both an indication as well as a contraindication for SGADs, depending on the procedure and clinical judgement.
Insertion techniques of SGADs follows certain broad principles common to all and few specific instructions pertaining to individual designs.
-
1.
Device is chosen based on the procedural and patient requirement and familiarity. For example, for a short procedure in the lower limb, with no need for muscle relaxation, any SGAD is acceptable, including cLMA whereas if procedure is laparoscopic cholecystectomy, only second generation device like ProSeal LMA or iGel is desirable.
-
2.
The presence of any predictors of difficult SGAD insertion such as restricted mouth opening and altered anatomy of neck and face post-surgery, due to syndromes, infections, neoplasm, or irradiation, should be looked for [Table 19.3].
-
3.
Preparation of the device and insertion techniques, position confirmation for individual devices are described in Chap. 6.
-
4.
Laryngeal mask airways were initially designed for peak pressures below 20 cmH2O, and multiple studies have also shown that peak pressures between 15 and 20 cmH2O result in a limited leak and gastric insufflation. The LMA ProSeal was created for use with higher ventilation pressures (the cuff has a posterior extension to provide a “true seal”), and will generally allow peak airway pressures of up to 30 cmH2O. In a meta-analysis by Sang et al., 26 studies involving 2142 patients undergoing laparoscopic procedures with 8 different supraglottic devices were analysed and it was found that oropharyngeal leak pressure (OLP), peak inspiratory pressure (PIP), were highest in Ambu AuraGain before pneumoperitoneum and I-gel after pneumoperitoneum. Gastric tube insertion success rate was highest in LMA Supreme [2].
-
5.
Attempting to insert a SGAD several times increases the likelihood of airway damage. A total of three SGAD insertion attempts are recommended: two with the desired second-generation system and one with an alternative. After failed first attempt, size of the device can be changed, usually to one size higher. Bougie-assisted PLMA placement has been said to improve first-time placement [1, 3]. The introducer tool approach offers a better fibreoptic view of the cords via the PLMA, but bougie-assisted positioning provides better alignment of the drain port. A high success rate has been recorded for fibreoptically driven tracheal intubation using the i-gel. Second-generation SGADs have been identified that are specifically designed to make tracheal intubation easier, but data on their efficacy is poor.
3 Condiut for Intubation in Difficult Airway
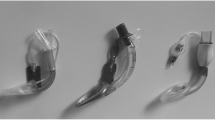
Supraglottic airway devices provide a conduit for intubation while maintaining ventilation so that oxygenation is not interrupted and depth of anaesthesia can be maintained [Fig. 19.2(1–9)]. However, not all devices are ideal for this purpose. Ambu Aura I, LMA supreme, Air-Q mask, LMA classic Excel are some of the examples of devices which are preferred for intubation, whereas LMA classic, iGel, Baska mask airway, etc. are not suitable [3]. Fibreoptic-guided intubation, with or without using Aintree Intubation Catheter, is the most preferred technique. Blind intubation is strongly discouraged unless there is no alternative available, as both risks of failure and trauma are higher [4].
SGAD as conduit for intubation. 1—preparation of fibreoptic device, 2 and 3—denotes fibreoptic placement inside oral cavity and ascertaining that the epiglottis is not folded, we don’t require step 1–3 in all cases, 4—denotes the insertion of supraglottic device (I gel no 4) over which air way exchange catheter is rail-roaded, 5—denotes removal of supraglottic device and air way exchange catheter is in situ (6), 7—denotes the placement of no 8—size endotracheal tube over air way exchange catheter, and 9—removal of airway exchange catheter and confirmation of accurate endotracheal tube placement
Although successful fibreoptic-guided intubation of a difficult airway has been reported using other supraglottic airway devices such as the LMA Classic, LMA ProSeal, and LMA Supreme, there is insufficient robust evidence to show that such devices are superior to the LMA Fastrach [5, 6]. A number of design features limit individual SGADs’ ability to function as effective conduits for ETT placement. To keep the epiglottis from falling back into the shaft, cLMA has bars on the pharyngeal bowl. This creates a mechanical barrier to the easy passage of the fibreoptic bronchoscope and ETT. A substantial amount of published data exists on using the “gold-standard LMA Fastrach” for blind intubation via a SGAD in patients with difficult-to-manage airways.
A meta-analysis included 16 randomized controlled trials with a total of 2014 patients to evaluate the efficacy of SGAD devices as a method for unassisted tracheal intubation. LMA-CTrach, LMA-Fastrach, Air-Q, i-gel, CobraPLA, Ambu-Aura, and single-use LMA were among the SGAD devices evaluated. According to the Supraglottic airway devices as a strategy for unassisted tracheal intubation (SUCRA), the LMA-CTrach (which provides video-assisted tracheal tube guidance), single-use LMA-Fastrach, and LMA-Fastrach are the three best SGADs for unassisted tracheal intubation [4, 7].
3.1 Supraglottic Airway Devices for Blind Tracheal Intubation
Blind insertion of the ETT through a SGAD may be indicated in certain clinical scenarios and has been reported to have success rates of 50–97% with several SGADs [8]. There is insufficient evidence to support generalising individual SGAD success rates with intubation in emergency. When inserted through most first-generation devices, the pharyngeal anatomical dimensions favour passage of the ETT into the oesophagus rather than the trachea whereas the air-Q and intubating LMA, Fastrach have design advantages that may improve blind tracheal intubation success rates. In a study comparing the LMA Fastrach and the air-Q, successful blind intubation after 2 attempts was achieved in 75 out of 76 (99%) of LMA Fastrach patients versus 60 out of 78 (77%) of air-Q patients [8]. Another study comparing blind tracheal intubation with the i-gel versus the LMA Fastrach found that 69% of patients with the i-gel and 74% of patients with the LMA Fastrach succeeded on the first attempt [9].
3.2 Supraglottic Tracheal Intubation Using Fibreoptic-Guided Airway Devices
The majority of patients have a good view of the glottis when the fibreoptic bronchoscope is placed into the SGAD. Intubating SGADs have features that aid or increase endotracheal intubation success rates. Design aspects of the ILMA include latex-free materials, V-shaped-guiding ramp for facilitating tracheal intubation towards glottic opening, and epiglottis elevating bar to displace epiglottis as tracheal tube emerges from mask aperture. Intubation through the SGAD with a flexible intubating scope (FIS) [9] has higher success rates than blind attempts. When the ideal ETT’s diameter is too large to pass through the LMA, a two-stage technique involving the use of an Aintree intubation catheter (AIC) is recommended. Once AIC is passed into the trachea, SGAD is removed and endotracheal tube rail-roaded. AIC being hollow allows oxygen administration and can be used for jet ventilation in emergency.
ILMA, specifically designed for difficult airway, provides effective ventilation in 97–100% of patients in both anticipated and unanticipated DA [5, 6]. Many other SGADs including ProSeal LMA, Supreme LMA, the i-gel, Ambu-i, the Air-Q, CobraPLA, and CobraPLUS, have also found to provide effective ventilation in DA, in case reports or series (level 4). The Laryngeal Tube, which was intended for emergency ventilation, also has been successfully used in the operating room for difficult airway control in elective adult and paediatric cases [10]. Langenstein and Moeller compared the chances of success for ventilation through the cLMA and the ILMA in patients with difficult-to-intubate tracheas: efficacy was similar, with 92%and 93% success, respectively [11]. Similarly, there was no substantial difference in terms of effective ventilation between both the single-use ILMA and the i-gel in two RCTs. Though several newer SGADs have evidence of effective ventilation in patients with difficult airways, superiority of any one device over others has not been proved. Often, SGAD blind intubations fail due to device orifice misalignment with the glottis or, more commonly, because a tube or introducer passed down the SGAD exits the ventilation orifice posteriorly and enters the oesophagus. With the exception of those specifically designed for intubation, most SGADs require fibreoptic guidance to increase the rate of effective intubation above 15%, including in patients with normal airways [12,13,14,15].
Finally, supraglottic airway device ventilation can be converted to endotracheal tube ventilation using a retrograde technique in which a guidewire is passed through cricothyroid membrane (CTM), directed cranially through the supraglottic airway device, and used to guide an obturator anterograde via the proximal end of the device and then out through the distal end, that can then be used to direct the placement of an endotracheal tube [16].
Regarding removal of supraglottic device postintubation is specific for Fastrach LMA and include following simple steps; (1) deflate the cuff completely while keeping the ETT cuff inflated, (2) tap or swing device handle around the chin caudally, (3) slide the device of the pharynx and into the oral cavity, using the curvature of the airway tube as a guide, (4) apply counter pressure to the ETT with the finger, (5) remove the ETT connector and insert the Stabilizer Rod to hold the ETT in position until the proximal end of the ETT is in level with the proximal end of the airway channel, (6) when the LMA Fastrach cuff is clear of the mouth, remove the LMA Stabilizer Rod while keeping the ETT in place to avoid accidental dislodgment, and (7) replace the ETT connector and ventilate [17].
4 Rescue Device in Difficult Airway
An SGAD can be used as a rescue device to manage a difficult/failed mask ventilation, failed intubation, and failed oxygenation. These are in addition to the indications as elective primary airway device and conduit for intubation. Furthermore, SGAD is used for oxygenation and as a conduit for FOB during elective or emergency front of neck procedures. Once inserted and patient condition improves, surgery can be progressed with SGAD as the primary airway device or the patient can be woken up.
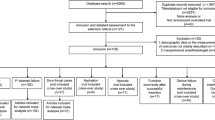
By establishing ventilation and/or allowing intubation through the device following failed intubation attempt(s), the SGAD can serve as an airway rescue device. If SGAD is used as a rescue device for ventilation after induction of anaesthesia, the decision must be made whether to continue the procedure using the SGAD, attempt endotracheal intubation using the SGAD as a conduit, or awaken the patient, depending on the clinical situation. Supraglottic airway devices play a role in the management of patients with difficult airway [Fig. 19.3] and are included in almost all airway guidelines (Fig. 19.4).
SGAD insertion in a case of difficult airway secondary to reconstructive surgeries there was hardly 2 cm mouth opening. An i-gel size 2.5 was secured via the lateral side of the mouth [18]
4.1 Rescue Airway: Difficult Intubation, Failed Intubation, Cannot Intubate, and Cannot Ventilate
In the initial stages, recognition of the LMA’s role in difficult airway management influenced clinical acceptance of SGAD technology. They could be lifesaving when both mask ventilation and intubation have failed. NAP4 findings have led to recommendations for second-generation SGADs to be available always for emergency as well as elective airway management and emphasised on education and practice to develop and retain competence. SGAD insertion and the positioning both of first- and second-generation devices are hindered by cricoid pressure, which reduces hypopharyngeal space. If laryngoscopy was difficult, During Plan A, cricoid pressure should be reduced or released during SGAD insertion if there is no regurgitation. Second-generation SGADs should always be preferred due to the superior protection they provide against aspiration.
5 Ventilatory Assist Devices for Elective/Emergency Front of Neck Access
Supraglottic airway device can be used for ventilation if face mask is ineffective during emergency front of the neck procedures (eFONA). It can also be used to facilitate ventilation during elective procedures, especially when relaxant has been used and provides as a conduit for fiberscope during FONA. The main objective of airway management is to ensure alveolar oxygenation. eFONA is the last lifesaving step in airway management, used to reverse hypoxia and prevent brain injury, cardiac arrest, and death [14]. A second-generation supraglottic airway device with large-bore gastric access might very well enable egress or suctioning, but it may not offer additional efficient aspiration protection. Intubation via a supraglottic airway device in a bleeding airway has been defined as “blind” (i.e., without the assistance of a flexible, optical endoscope) and might even be considered as a last desperate measure prior to emergency FONA.
6 Extubation Assist Device
To minimize the hemodynamic response, coughing and or manage airway hyperreactivity, SGADs can be used for deep extubation. It can be either placed after removal of endotracheal tube or placed behind the tube (Bailey manoeuvre) as it is being removed. SGAD can be removed when patient is fully awake either in the operating room or in the recovery. This is one of the recommendations of DA guidelines for extubation.
Raveendra et al. also identified a novel technique for establishing a bridging SGAD in a patient with a difficult airway using an airway exchange catheter [19]. The exchange catheter was inserted into the airway tube lumen of a size-3 LMA-ProSeal and the LMA was introduced into the pharynx without the use of a metal introducer. The LMA-ProSeal was attached to an elbow connector with a bronchoscopy port, with the proximal end of the exchange catheter protruding through the port. The exchange catheter was removed after a standard capnography waveform confirmed proper positioning of the LMA-ProSeal and no cuff leak. The patient was then allowed to awaken from anaesthesia, after resumption of spontaneous efforts and ProSeal LMA was removed without any bouts of coughing. The ETT would have been reintroduced over the exchange catheter, accompanied by a traditional extubation procedure, if either positive pressure or spontaneous ventilation through the LMA-ProSeal had been insufficient.
During the Bailey manoeuvre, various SGADs such as the classic laryngeal mask airway (LMA) and the Ambu laryngeal mask have been mentioned in the literature. ProSeal LMA was compared to the I-gel supraglottic airway for ease of insertion, proper positioning, and haemodynamic responses during the Bailey manoeuvre in a study by et al. The I-gel (41/50 patients requiring a single attempt with no resistance at insertion) had a higher ease of insertion than the ProSeal LMA (39/50 patients required a single attempt with no resistance at insertion), which was statistically comparable. The I-gel revealed the glottis more clearly than the ProSeal LMA (92% in group II and 66% in group I had Brimacombe scores of III or IV), which was statistically relevant (p <0.05) [20].
7 Supraglottic Airway Devices in the Pre-hospital Airway Management
Potentially every airway in the pre-hospital setting is difficult. In such situations, SGADs can complement or replace either face mask or endotracheal tube or both. Emergency team members including nonanaesthesia medical professionals may be more comfortable with using an SAD rather than intubating a patient in an out of hospital setting with multiple limiting factors. Although several supraglottic devices, including the LMA Classic, LMA Supreme, LMA Fastrach, and i-gel, have been considered for pre-hospital airway management, there is no strong evidence to support the routine use of any one device over the others. The benefits of SGADs over face mask and tracheal intubation are summarised in Table 19.4.
Once the supraglottic airway is in place, it can be used as a conduit for endotracheal intubation using one of several techniques. Some SGADs (for example, i-gel, LMA Fastrach, air-Q, and LMA Protector) allow for the direct passage of an endotracheal tube (ETT). However, intubation through SGAD is an advanced airway technique requiring specific knowledge and expertise and can involve transient apnoea. Furthermore, flexible video endoscope is never used in pre-hospital settings and blind technique is even more potentially harmful. Teamwork and assistance for such a procedure is unlikely in those settings. Second-generation SADs are preferred and are more effective with respect to insertion, stability, ventilation, and protection.
The use of a SGAD in an OHCA allows for constant cardiac compressions without the need for pausing ventilation. This could be a contributory factor in improving the outcome. A meta-analysis by Barr et al. showed the second-generation devices to be safe and feasible as alternate airway devices, even for first responders and particularly in developing EMS systems [21].
8 SGAD and Special Patient Groups
8.1 Patients with Gastroesophageal Reflux Disease (GERD)
In patients with severe SGAD is not an ideal choice for general anaesthesia and is reserved only as a rescue device in failed intubation. However, they can be used in patients with moderate GERD, on proton pump inhibitors (PPIs). Always, second-generation devices with gastric drainage should be used to provide maximum protection against aspiration. Currently, the most sensitive technique for detecting reflux events is multichannel intraluminal impedance-pH (MII-pH) monitoring, which incorporates several impedance channels with traditional pH catheters [22]. Using MII-pH monitoring along with SGAD-based general anaesthesia can aid in detecting ongoing reflux/regurgitation in patients’ oesophagus during the perioperative period [22].
8.2 Paediatric Patients
Age is no contraindication per se for using supraglottic airway device as appropriate size devices are available even for neonates. Insertion in children can be blind, bougie-guided, suction catheter-guided, or laryngoscopy-guided. Guidelines also recommend the use of second-generation SGADs in children with unexpectedly difficult airways. SGAD fitting and seal are confirmed to be as important in paediatric patients as they are in adult patients. In a study of children aged 1 month to 12 years, it was discovered that the I-gelTM had a significantly higher OPLP in the supine and lateral positions than the ProSealTM LMA. OPLP decreased significantly when the position was changed from supine to lateral in both I-gelTM and ProSealTM LMA groups, resulting in tidal volume loss. In both I-gelTM and ProSealTM LMA, the percentage reduction in OPLP from supine to lateral was comparable [23, 24].
The LMA has also been used in neonates affected by malformations of the upper airway in emergency situations and during laryngoscopy and bronchial endoscopy. In particular, the LMA has proved useful in neonates affected by multiple congenital arthrogryposis and micrognathia, and patients with bronchopulmonary dysplasia undergoing cryotherapy for retinopathy of the prematurity for ventilation [25].
8.3 Obese Patients
Obese patients are more likely to have difficult airway, including difficulty with SAD use. They frequently require higher peak airway pressures, putting them at a higher risk of inadequate ventilation with an SGAD, leak around the device, and gastric insufflation. A systematic review comparing the use of the LMA ProSeal versus placement of an endotracheal tube (ETT) for patients with obesity (BMI >30 kg/m2) found that the leaks were more common around the laryngeal mask airway (LMA), and approximately 4% of patients had their LMA replaced with an ETT due to poor placement. There were no serious complications or cases of aspiration, and postoperative hypoxemia (O2 saturation 92%) was less common with LMA use.
As a rule, SGADs are avoided for obese patients (a) with BMIs greater than 35 kg/m2, (b) surgery lasting more than 90 min, (c) lithotomy position, and (d) limited access to airway during the procedure. These are not, however, absolute guidelines, and the selection of an airway device in a specific patient is a matter of clinical experience and judgement [26]. Role in rescue airway management remains the same as nonobese patients. Exceptions are made based on clinical experience and judgement (Fig. 19.5).
8.4 Prone Positioning
SGADs have been used in the prone position for patients undergoing surgery, both for planned airway management and as rescue devices [27]. In some cases, patients are positioned prone prior to anaesthesia induction and SGA placement. The time from induction to incision is reduced, less manpower is required for positioning, and the time to extubation at the end of surgery is usually shorter than when an ETT is used. The patient can confirm that the neck and head positions are comfortable by self-positioning. There may be a lower risk of injury to the patient or operating room personnel, as well as a lower risk of dislodging intravenous (IV) lines or the airway device, compared to prone positioning after induction. Self-positioning may result in fewer hemodynamic changes than the prone position.
Limitations and disadvantages include the need for higher airway pressures may be required for positive pressure ventilation (PPV), increasing the risk of inadequate ventilation, leak, and/or gastric insufflation. In the prone position, the LMA provides a less secure airway than an ETT, and manipulation or replacement may be more difficult, if not impossible. Hence, ideally, the use of SGAD in prone position should be selected with lot of discretion based on experience and with preparation for managing potential perioperative complications. A retrospective review of 245 cases in which the LMA ProSeal was placed prone revealed that the LMA was used successfully in all patients with no complications. Cuff inflation should be limited to 40 cmH2O or the minimum volume required for an adequate seal [27].
9 Contraindications for Use of SGADs
Given that the most serious complications associated with SGADs are ventilatory failure, aspiration, displacement, and interference in surgical procedures. Consequently, contraindications include patient factors that increase these risks. Obesity and obstructive airways disease increase the risk of device failure due to inadequate ventilation, whereas active gastroesophageal reflux, intestinal obstruction, hiatal hernia, trauma, and intoxication increase the risk of aspiration. Patients who have sustained traumatic airway injuries are more likely to experience complications from SGAD placement. Many contraindications are relative where use of SGAD depends on the clinical judgement [28, 29].
10 Conclusions
SGADs have enhanced the safety and quality of airway management in both normal and difficult airways across the patient population. It has been successful in reducing the dependence on endotracheal tube in more than 50% of surgeries worldwide. With excellent safety profile, ease of insertion, better tolerance, and simplicity of the device, supraglottic airway management has become a standard routine when there exist no contraindications. It is essential, from the patient safety perspective, that anaesthesiologists, other clinicians, and paramedical professionals must have appropriate training in the use of these devices.
References
Pennant JH, White PF. The laryngeal mask airway. Its uses in anesthesiology. Anesthesiology. 1993;79:144–63.
Sang WY, Hyun K, Geun JC, Choongun R, Yong HP, Chong WB, et al. Comparison of supraglottic airway devices in laparoscopic surgeries: a network meta-analysis. J Clin Anesth. 2019;55:52–66.
Joly N, Poulin LP, Tanoubi I, et al. Randomized prospective trial comparing two supraglottic airway devices: i-gel™ and LMA-Supreme™ in paralyzed patients. Can J Anaesth. 2014;61:794.
Ahn E, Choi G, Kang H, Baek C, Jung Y, Woo Y, Bang S. Supraglottic airway devices as a strategy for unassisted tracheal intubation: a network meta-analysis. PLoS One. 2018;13(11):e0206804. https://doi.org/10.1371/journal.pone.0206804. PMID: 30395614; PMCID: PMC6218066.
Timmermann A. Supraglottic airways in difficult airway management: successes, failures, use and misuse. Anaesthesia. 2011;66(Suppl 2):45–56. https://doi.org/10.1111/j.1365-2044.2011.06934.x. PMID: 22074079.
Cook TM, Brooks TS, Van der Westhuizen J, Clarke M. The Proseal LMA is a useful rescue device during failed rapid sequence intubation: two additional cases. Can J Anaesth. 2005;52:630.
Jagannathan N, Sequera-Ramos L, Sohn L, Wallis B, Shertzer A, Schaldenbrand K. Elective use of supraglottic airway devices for primary airway management in children with difficult airways. Br J Anaesth. 2014;112(4):742–8.
Abdel-Halim TM, Abo MA, Enin E, Elgoushi MM, Afifi MG, Atwa HS. Comparative study between Air-Q and intubating laryngeal mask airway when used as conduit for fiber-optic. Egypt J Anaesth. 2014;30(2):107–13.
Karim YM, Swanson DE. Comparison of blind tracheal intubation through the intubating laryngeal mask airway (LMA Fastrach™) and the Air-Q™. Anaesthesia. 2011;66(3):185–90. https://doi.org/10.1111/j.1365-2044.2011.06625.x. PMID: 21320087.
Scheller B, Schalk R, Byhahn C, et al. Laryngeal tube suction II for difficult airway management in neonates and small infants. Resuscitation. 2009;80:805–10.
Langenstein H, Moller F. The importance of the laryngeal mask in the difficult intubation and early experience with the intubating laryngeal mask airway--ILMA--Fastrach. Anaesthesiolgie Intensivmedizin Notfallmedizin Schmerztherapie. 1998;33:771–80.
Michálek P, Donaldson W, McAleavey F, et al. The i-gel supraglottic airway as a conduit for fibreoptic tracheal intubation—a randomized comparison with the single-use intubating laryngeal mask airway and CTrach laryngeal mask in patients with predicted difficult laryngoscopy. Prague Med Rep. 2016;117:164.
Ahn E, Choi G, Kang H, et al. Supraglottic airway devices as a strategy for unassisted tracheal intubation: a network meta-analysis. PLoS One. 2018;13:e0206804.
Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, O’Sullivan EP, Woodall NM, Ahmad I, Difficult Airway Society intubation guidelines working group. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115(6):827–48.
Henderson JJ, Popat MT, Latto IP, Pearce AC, Difficult Airway Society. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004;59(7):675–94. https://doi.org/10.1111/j.1365-2044.2004.03831.x. PMID: 15200543.
Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on management of the difficult airway. Anesthesiology. 2013;118:251–70.
Nair I, Bailey PM. Use of the laryngeal mask for airway maintenance following tracheal extubation. Anaesthesia. 1995;50(2):174–5.
Gupta B, Gupta N, Jaishankaraswamy HM, Chattopadhyay D, Kakkar K. I-gel as an airway device in an anticipated difficult airway in a patient with bear bite and flap overgrowth post-surgery. Korean J Anesthesiol. 2020;73(4):354–6.
Raveendran R, Sastry SG, Wong DT. Tracheal extubation with a laryngeal mask airway and exchange catheter in a patient with a difficult airway. Can J Anaesth. 2013;60(12):1278–9.
Kalra N, Gupta A, Sood R, Kaur M. Comparison of proseal laryngeal mask airway with the I-gel supraglottic airway during the bailey manoeuvre in adult patients undergoing elective surgery. Turk J Anaesthesiol Reanim. 2020;49(2):107–13. https://doi.org/10.5152/TJAR.2020.29569.
Barr S, Smith G, Darroch S. Use of supraglottic airway devices by paramedics in the management of adult prehospital cardiac arrest patients. Austral J Paramed [Internet]. 2017 [cited 2021 May 6];14(1).
Roux M, Drolet P, Girard M, et al. Effect of the laryngeal mask airway on oesophageal pH: influence of the volume and pressure inside the cuff. Br J Anaesth. 1999;82:566.
Brimacombe JR, Berry A. The incidence of aspiration associated with the laryngeal mask airway: a meta-analysis of published literature. J Clin Anesth. 1995;7:297.
Warner MA, Warner ME, Weber JG. Clinical significance of pulmonary aspiration during the perioperative period. Anesthesiology. 1993;78:56.
Trevisanuto D, Micaglio M, Ferrarese P, Zanardo V. The laryngeal mask airway: potential applications in neonates. Arch Dis Child Fetal Neonatal Ed. 2004;89:F485–9.
Moser B, Keller C, Audigé L, et al. Fiberoptic intubation of severely obese patients through supraglottic airway: a prospective, randomized trial of the Ambu® AuraGain™ laryngeal mask vs the i-gel™ airway. Acta Anaesthesiol Scand. 2019;63:187.
Brimacombe JR, Wenzel V, Keller C. The proseal laryngeal mask airway in prone patients: a retrospective audit of 245 patients. Anaesth Intensive Care. 2007;35:222–5.
Rabey PG, Murphy PJ, Langton JA, et al. Effect of the laryngeal mask airway on lower oesophageal sphincter pressure in patients during general anaesthesia. Br J Anaesth. 1992;69:346.
Yu SH, Beirne OR. Laryngeal mask airways have a lower risk of airway complications compared with endotracheal intubation: a systematic review. J Oral Maxillofac Surg. 2010;68:2359.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Tripathy, D.K., Gupta, B. (2023). Supraglottic Airway Devices: Clinical Applications. In: Ubaradka, R.S., Gupta, N., Bidkar, P.U., Tripathy, D.K., Gupta, A. (eds) The Airway Manual. Springer, Singapore. https://doi.org/10.1007/978-981-19-4747-6_19
Download citation
DOI: https://doi.org/10.1007/978-981-19-4747-6_19
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-4746-9
Online ISBN: 978-981-19-4747-6
eBook Packages: MedicineMedicine (R0)