Abstract
In today’s world, mammalian cell cultures are used to understand various physiological and pathophysiological cell signaling events related to normal as well as various diseased cells such as cancer cells and others. Besides, mammalian cells such as Chinese hamster ovary (CHO) cells, baby hamster kidney (BHK) cells, human embryonic kidney (HEK) cells, African green monkey kidney (COS) cells, NSO cells, HT1080 cell, and PER-C6 cells (many others too) as well as their culture products (various recombinant proteins) have widespread use in biotechnology, pharmacology, and medicine. The major usefulness of cultured mammalian cells and their products described in this chapter include (i) use as a model system for physiological and pathophysiological studies; (ii) use in experimental drug/toxin research; (iii) use in vaccine production, particularly against pathogenic viruses; (iv) use for various recombinant protein production; (v) in cell therapy; and finally (vi) in gene therapy. The various mammalian cell culture recombinant DNA products described in this chapter are tissue plasminogen activator, urokinase, follicle-stimulating hormone, blood clotting factor VIII, and erythropoietin. All these recombinant proteins exhibit widespread significance in the medical field. In comparison, cell and gene therapy are new fields and their success against various human diseases is substantially in the initial stages.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Chinese Hamster Ovary (CHO) cells
- Baby Hamster Kidney (BHK) cells
- Human Embryonic Kidney (HEK) cells
- African Green Monkey Kidney (COS) cells
- NSO cells
- HT1080 cells
- PER-C6 cells
- Model for Physiological & Pathophysiological studies
- Cell Culture Products
- Recombinant Proteins
- Vaccines
- Cell Therapy
- Gene Therapy
1 Introduction
The culture of mammalian cells has manifold significance in every sphere of modern-day life. Various mammalian cell lines such as Chinese hamster ovary (CHO) cells, baby hamster kidney (BHK) cells, human embryonic kidney (HEK) cells, African green monkey kidney (COS) cells, NSO cells, HT1080 cells, PER-C6 cells, etc. are widely used, not only for understanding the mammalian cell physiology but also for clinical, pharmaceutical, and industrial purposes. The shape, size, morphology, structure, and functions of the mammalian cells are examined using in vitro cultured mammalian cells. In vitro cultured mammalian cells are used to understand the physiology and pathophysiology of cell proliferation (growth), survival, and apoptosis. Of note, cell proliferation and programmed death (apoptosis) are prominent physiological phenomena of mammalian cells. The efficacy of various newly synthesized/discovered drugs/chemicals/toxins is examined using in vitro cultured mammalian cells. The drug discovery laboratories throughout the world examine the effects of newly synthesized anticancer drugs or drugs produced against other diseases amidst the various cell cycle phases (G1-S-G2-M) using cultured cancer cells. The positive results from the in vitro cell culture experiments can serve as key cautions and guidelines for in vivo animal culture and other experiments. The pathogenic animal viruses use animal cells for their multiplication and propagation. One of the most imperative benefits of mammalian cells is for studying viral propagation and generating antivirus vaccines. Perhaps the most important application of cultured mammalian cells is the production of several recombinant proteins that are immensely useful in pharmaceutical or biotechnological industries and clinical or medical sciences. Various steps involved in recombinant protein production in cultured mammalian cells comprise isolation, characterization, and optimization of the gene of interest, choosing a suitable vector, selection of a suitable mammalian host cell, DNA delivery and integration into the mammalian host cell, transient versus stable transfection, selection and optimization of a positive clone and mammalian expression system for mass culture, selection and optimization of cell culture medium for mass culture, selection and optimization of cultivation mode – adherent versus non-adherent (perfusion and fed-batch) – purification of the expressed or secreted proteins (from lysed cells or the culture medium), and finally quality control and quality assurances. The most important recombinant proteins produced using mammalian cells are tissue plasminogen activator (tPA, used to dissolve blood clots), urokinase (used to dissolve blood clots), erythropoietin (EPO, stimulates RBC production), follicle-stimulating hormone (FSH, used for infertility treatment), blood coagulation factor VIII (used for hemophilia A treatment), and various monoclonal antibodies (used against various pathophysiological or diseased conditions including cancers, rheumatoid arthritis, osteoporosis, sepsis, Crohn’s disease, etc.). Additionally, mammalian cell culture is also used in replacement therapy (for replacement of old, damaged, or injured tissues and organs such as the skin), gene and cell therapy (for correcting genetic mutation), and cell fusion technology (such as hybridomas for the production of monoclonal antibodies). In a nutshell, the cultured mammalian cells have multiple significance, in experimental research, physiology, and pathophysiology, and the relevant applications in biotechnological, pharmaceutical, and medical sciences. The present chapter describes all these utility aspects of mammalian cell culture.
2 Use of Mammalian Cells as a Model System for Physiological and Pathophysiological Studies
More than 200 years have passed since the father of modern experimental physiology, Claude Bernard, was born. Extensive research works of numerous scientists led to the complete present-day knowledge of mammalian physiology. The use of mammalian cells and the in vitro culture of these cells is one of the most important tools and techniques, respectively, for key discoveries in mammalian physiology and pathophysiology.
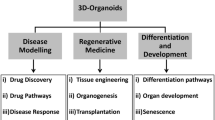
In vitro cell culture is frequently used to advance understanding of the mechanisms that underlie the in vivo cell behavior. These behaviors include cell growth (division/proliferation), differentiation, migration, and mechanics, all of which are sensitively influenced by their biochemical and biomechanical microenvironments. Deciphering the mechanisms behind these behaviors is vital to understanding the in vivo processes that eventually form the tissues and organs as well as allocating their functions. Ideally, laboratory experiments could be performed with a user-defined three-dimensional (3D) model that closely mimics the cellular microenvironment.
In vitro mammalian cell culture has the following significance:
-
To understand the specific phenotype including shape and size (morphology) of a particular cell type (e.g., endothelial cells have a cobblestone morphology) both in 2D and 3D culture.
-
To understand karyotyping and related genetic analysis of cells.
-
To understand the effects of specific environmental conditions (e.g., temperature, pH, moisture, O2/CO2 tension, medium composition, nutrition, etc.) on the growth and physiological behavior of cells.
-
To understand the processes through which cell division and proliferation take place along with studying the effects of varying nutrients, medium pH, temperature, moisture, etc. on the mammalian cells using cultured mammalian cells.
-
For deciphering the role of various cyclins (cyclins D, E, A, and B) and cyclin-dependent kinases (CDKs: CDK4, CDK6, CDK2, and CDK1) in the cell cycle regulation (various phases: (G1-S-G2-M)). Experimental studies on cultured mammalian cells help to dissect the altered cell cycle regulation in non-transformed along with its implicit comparative progress in transformed cells.
-
To understand the signaling processes involved in cell differentiation amidst 3D cell culture.
-
To understand the basic physiological functions of a cell. For example, the mechanism through which a neuron sends nerve impulse (through patch-clamp technique), a skeletal muscle contracts (sliding filament theory), or glucose transport by endothelial cells (via glucose transporter or GLUT), etc.
-
To understand the cellular metabolism in real-time and metabolic distinctions of non-transformed and transformed cells (the Warburg effect).
-
To understand the programmed (apoptosis) and non-programmed (necrosis) death of cells, from physiological and pathophysiological viewpoints.
-
To understand the cell-to-cell (cross-talk) and cell-to-extracellular matrix (ECM), interactions, and possible association for directional signaling using integrins, examined using mammalian cell culture.
-
Understanding the interaction between the cells and pathogens (host-pathogen interaction) can be demonstrated using cell culture.
-
To understand the physiological defense mechanism.
-
To understand the process through which various ions (Na+, K+, and Cl−) and nutrients (e.g., glucose, amino acids, etc.) are transported across biological membrane channels.
-
Observing the effects of various drugs, toxins, and other molecules on cultured mammalian cells are immensely useful.
-
To use the mammalian cells for the transfection of viruses and producing antiviral vaccines.
-
To use the mammalian cells for producing recombinant proteins, cytokines, chemokines, etc. Cultured mammalian cells are prime requirements for this.
-
To understand the alteration of various cellular processes amidst diverse pathophysiological conditions (e.g., cancers) (Mills and Estes 2016).
Overleaf paragraphs (step-by-step) describe the prominent utilities of mammalian cell culture:
3 Use of Mammalian Cells for Experimental Drug/Toxin Research
The research and development (R&D) section of biotech/pharmaceutical companies or basic scientific research laboratories is primarily focused on new drug discovery. To observe the efficacy of a newly synthesized drug, the first step is to examine the effects of a drug on the in vitro cultured mammalian cells. Various mammalian cultured cells are widely used either alone or in conjunction with animal cells, to study the effects of new drugs, cosmetics, and chemicals on their survival, growth, and biological activities. For the treatment of cells with various drugs/toxins and other molecules, it is pertinent that cells in the culture container reach a particular confluence status. In two-dimensional cultures, confluency implies the area of the cell culture container covered by growing cells. For example, 100% confluence indicates the cell culture vessel is full/occupied by growing cells and there is no place left to grow. Depending upon the type of experiments, cells are grown to varying confluence extents followed by their treatment with different experimental agents. For example, for transfection assay, cells can be grown at 40–50% confluence, while for apoptosis assay, cells can be grown at 90–100% confluence. Standardization of the drug/toxin dosage or concentration alongside the treatment stage is highly essential to monitor the effects of any drugs/toxins/other agents (Ekwall 1980; Paganuzzi-Stammati et al. 1981; Ekwall 1983).
The following paragraphs describe the dose and time response of an experimental drug:
3.1 Dose-Response of the Experimental Molecules
Dose-response comprises the monitoring of various concentrations of a drug/toxin/another agent on the cultured mammalian cell growth for a fixed time, following treatment to determine the optimum effective drug concentration manifesting desirous experimental effects. For example, if a drug administered is intended for breast cancer treatment (curtailing the corresponding cell proliferation), dose-response will check the suitable drug concentration for inhibiting breast cancer cell proliferation following a fixed duration treatment. In dose-response monitoring, time of the time-lapse of treatment efficacy monitoring and delivered drug concentration need to be the same in all simultaneous analyses.
Briefly, the technical steps may be as follows:
-
Take at least five (five) cell culture containers (plate/flasks) of the same type and size (like each as a 100 mm Petri plate).
-
To each container, add the same number of cells with the same medium volume. Suppose 1x106 endothelial cells are added to a 100 mm Petri plate with 10 ml M199 medium before being grown in a CO2 incubator for up to 80% confluency. Other culture plates should ideally be a replica of this culture plate.
NB: The volume of the medium, as well as cell number, varies with different container sizes.
-
Allow the cells to grow up to the desired confluence before drug treatment.
-
Dissolve the experimental drug in a suitable solvent (water/organic solvent like ethanol/DMSO, etc.) depending upon the solubility of the drug/chemical.
-
Serially dilute the chemical/drug with the solvent.
-
Keep one cell culture vessel as control. To this control cell culture container, add only the vehicle/solvent in which the experimental drug has been dissolved and serially diluted.
-
Add the drugs/chemical at logarithmic higher concentration (from lower to higher extent) using each cell culture container.
-
For example, the 05 cell culture containers mentioned above can be used with the following drug concentrations:
-
Plate 1: Solvent/vehicle alone (control)
-
Plate 2: Added with 10 pM drug concentration
-
Plate 3: Added with 30 pM drug concentration
-
Plate 4: Added with 100 pM drug concentration
-
Plate 5: Added with 1 nM drug concentration
-
NB: Depending upon the experiment, more plates with a logarithmic higher concentration of drugs may be needed. The concentrations acronyms signify the following: pM = picomolar, nM = nanomolar, μM = micromolar, mM = millimolar, M = molar.
-
Following administration of the drug(s), all cell culture containers are incubated at 37 °C in a CO2 incubator for the same time (say, for instance, 4 h).
-
The treated cells may be utilized for various assays (e.g., MTT assay for cell proliferation) or lysed to isolate DNA/RNA/proteins before being used in a defined experiment. It should also be screened whether the experimental desired gene/mRNA/protein is up- or downregulated.
-
Dose-response helps to determine the effective dose/concentration range of a drug corresponding to which the expected result/treatment responses are observed.
3.2 Time Response of the Experimental Molecules
Time response is the same as dose-response; the only exception is the fixed (experimental) drug concentration in all culture containers. However, the time of treatment varies from one to another cell culture container.
Briefly, the technical steps may be as follows:
-
Following the dose-response of a particular drug/chemical, the most effective drug concentration is examined by the researcher.
-
To determine the exact time at which the experimental drug is most effective, several similar-sized cell culture containers have to be grown as mentioned in the dose-response. The number of the cells and the volume of the same cell culture medium must be the same in all culture containers.
-
All the containers except control (the ones treated only with vehicle/solvent) are treated with the same drug(s) concentration (the most effective drug concentration can be chosen from the dose-response) for varying periods.
-
This means only one particular concentration (suppose 10 nM) of a drug could be added to every container for varying durations (e.g., control, 30 min, 1 h, 3 h, 10 h, etc.).
-
From the time response, one can choose the desired time till when the maximum up- or downregulation of desired DNA/RNA/proteins takes place.
-
The treated cells could be utilized for various purposes including multiple assays as mentioned in the dose-response.
NB: The early response genes may take minutes to hours to express the effects of a particular drug, whereas the late response genes may take hours to days for the same. Normal (non-transformed) mammalian cells grow in flat 2D cell culture containers, forming a monolayer and getting prompt drug access. Contrary to this, in a healthy body, physiological conditions are present within tissues and organs of complex architecture growing as multiple layers. Therefore, growing the cells in 3D cell culture containers and animal experiments is highly essential after the basic 2D cell culture experiments.
4 Mammalian Cell Culture in Cancer Research
Cancer is the uncontrolled proliferation (division by mitosis) of cells, culminating in an uncontrolled cell mass. This infers that cancer cells exhibit uninterrupted cell cycle progression and divide uncontrollably with a negligible or no G0 phase. In the G0 phase, cells do not perform any task about cell division, including preparation for cell division. Perhaps, that’s why this phase is sometimes also called as resting phase. The normal non-transformed cells can be transformed into a tumor/cancer cell because of their genetic and/or epigenetic alteration, leading to characteristic genotype and phenotype distinctions. Various immortal cancer cells are now available that can be in vitro cultured to understand distinctive identifying features of cancer cells. A separate chapter (chapter 10) herewith describes the culture of various cancer cells. Briefly, from the cultured cells, the following information may be collected (Masters 2000; Mirabelli et al. 2019).
4.1 Understanding the Phenotype and Genotype of Cancer Cells
The reason for the uncontrolled proliferation of cancer cells is either genetic or epigenetic alteration. Mutation in the gene sequence and alteration of chromosome number are the major reasons for genetic alteration. Besides spontaneous and induced reasons for mutation, transposons or retrotransposons may generate mutations. Changes in the acetylation and methylation of DNA are the major epigenetic alteration of a cancer cell. Karyotype changes lead to phenotype changes such as irregular in shape, varied in size, large nucleus (may be due to more number of chromosomes), etc. Cultured cells are the major resources to understand all the characteristic alterations of cancer cells both genotypically and phenotypically.
NB: Characteristic alterations or hallmarks of cancer are described in Chapter 11.
4.2 Understanding the Process Through Which a Normal Cell Can be Transformed into a Cancer Cell
In a research laboratory, under an experimental setting, a normal cell can be transformed into a cancer cell via stimulation either with various cancer-causing viruses called oncoviruses (e.g., DNA viruses) or oncogenic chemicals (e.g., methylcholanthrene, aflatoxins, asbestos, arsenic, etc.) or radiations (e.g., ultraviolet radiation). While animal models (particularly syngeneic or immunocompromised and knockout mice models) are the first choices for generating cancers, particularly xenograft mice models presently normal cell culture models are also utilized to generate cancer cells as well as understand the transformation mechanism.
4.3 Understanding the Role of Various Cell Cycle Phases in Regulating Cancer Cell Proliferation
The cell cycle is a normal physiological phenomenon in the life of a mammalian cell. It regulates and decides as and when a cell may undergo division (cell proliferation or growth) and how many times a cell has to divide. A typical cell cycle consists of a repeated cycle of G0-G1-S-G2-M phases. In the G0 phase, the newly divided cells undergo complete rest and prepare for the nutritional and physical requirements of cell division. While in the G1 phase, a cell synthesizes all the proteins (enzymes such as polymerases) necessary for DNA replication, in the S phase, DNA replicates (formation of two DNA from one DNA via a semiconservative model). In the G2 phase, cells check their preparation (vis-à-vis DNA, RNA, proteins, and cellular constituents) for cell division to an adequate extent, and finally, in the M phase, the actual cell division or mitosis happens, followed by cytokinesis, thereby completing the cell division.
According to Hayflick, all normal cells of a mammalian body (except neuronal cells or mature erythrocytes) undergo finite cell cycles and therefore a limited number of cell divisions. For example, endothelial cells have a capacity of around 50 divisions. Shortening of telomere after every division may be one of the reasons for a limited number of mammalian cell divisions. Following every cell division, each cell enters the G0 phase, the duration of which may vary from one to another cell type. An exception may be neuronal cells (always in the G0 phase) or mammalian mature erythrocytes (do not contain any nucleus), owing to which these cells never enter the cell cycle.
While in a G0 phase, cells receive a sufficient amount of positive signals from molecules such as growth factors, hormones, amino acids, etc., and the expression of cell cycle inhibitory or negative signaling molecules such as P53, P21, P27, PTEN, pRb, etc. declines to their basal level. The G0 phase cells transit to the G1 phase, which is followed by S and G2 phases, respectively, and finally cells enter the M phase. After the division, the two newly divided cells once again go through the same cycle of Go-G1-S-G2-M, and this cycle will go on and on, till a normal cell is capable of further dividing. However, a cancer cell has no G0 phase or very short G0 phase and exhibits a continuous cell cycle. This means one division ends and immediately prepared for the next cell division begins, i.e., starting cycle for cancer cells.
Cultured mammalian cells are widely utilized to understand the cell cycle, about which some prominent utilities are as ahead:
-
Checking the cell proliferation by MTT or other cell proliferation assays.
-
Understanding cell synchronization in a particular phase of the cell cycle. In synchronization, all cells in a particular population will be in the same cell cycle phase. This means all the cells will be in either G1 or S or G2 or M phase. Synchronization effectively helps to understand the role of various newly synthesized drugs, toxins, etc. on the cell cycle. This is indeed very helpful in new drug discovery.
-
Understanding the role of various cyclins and cyclin-dependent kinases (CDKs) on the cell cycle. While cyclins are regulatory subunits of a cell cycle regulatory enzyme, CDKs are catalytic subunits of the same enzyme. In a mammalian cell, there are several cyclins (cyclin D, cyclin E, cyclin A, and cyclin B) regulating the cell cycle phases. Similarly, various CDKs such as CDK4, CDK6, CDK2, and CDK1 catalyze the mammalian cell cycle. Cyclins (regulatory subunit) and CDKs (catalytic subunit) together comprise the complete cell cycle regulating enzymes.
-
Experimentally controlling cyclins or CDKs or both may help to regulate the cell cycle. For example, estrogen stimulates cyclin D1 synthesis and therefore activates the G1 phase of the cell cycle. So, attenuation of estrogen-dependent cyclin D1 synthesis may alter the cell cycle pace and arguably, the estrogen-dependent breast cancer as well.
4.4 Understanding the Process of Programmed Cell Death in Normal (Mortal) and Cancer (Immortal) Cells
Programmed cell death or apoptosis is a normal natural physiological phenomenon having paramount importance in various processes such as developmental biology and morphogenesis, renewal or replacement of old damaged/aged cells with new cells, etc. Every normal dividing cell loses the capacity for division after a certain number of divisions, and eventually these cells die by the process of programmed death or apoptosis. Apoptosis is regulated by the controlled regulatory activities of proapoptotic proteins such as Bad, Bax, Bid, etc., or antiapoptotic proteins such as BCl2, Bcl-xL, etc. While proapoptotic proteins activate apoptosis, antiapoptotic proteins forbid unnecessary apoptosis. The proapoptotic proteins may regulate several procaspases (inactive proteolytic enzymes which act as precursors of active enzymes) which upon activation are converted to caspases (active proteolytic enzymes). These enzymes execute a signaling cascade through apoptosis (e.g., inactive procaspase 3 will be converted to active caspase 3). However, cancer cells have a defunct apoptosis mechanism because of mutations in multiple apoptosis-activating proteins such as P53. Cultured mammalian cells are not only used to understand apoptosis but also to observe the effects of various pro- or antiapoptotic molecules. One of the mechanisms through which cancer biologists try to control the cancer cell population is via apoptotic induction in these cells.
4.5 Understanding the Effect of Various Experimental Anticancer Drugs on the Cultured Cancer Cells
Cell cycle proteins such as cyclins and CDKs regulate the proliferation (division) of cells. Various cells in a tissue or an organ are in distinct cell cycle phases and can be separated based on their specific phase using flow cytometer or cell sorter. Each of the cell cycle phases is regulated by specific cyclins and CDKs. For example, in mammals, the G1 to S phase transition (called G1-S transition) is mediated by cyclin D and CDK4/CDK6. By regulating these proteins, one can regulate the cell cycle as well as uncontrolled cellular proliferation. In vitro cell culture experiments showed that while the G1 to S transition regulates the cell cycle initiation, the G2-M transition checks whether every material necessary for cell division is present to an adequate extent. To check the effects of an experimental drug on the specific phase of the cultured cells, synchronization of cells at a particular cell cycle phase is highly essential (synchronization indicates that experimentally all the cells must be in the same phase of the cell cycle during experimental drug/chemical treatment). It is pertinent to note here that serum starvation and aphidicolin halt the cell cycle at the G1 phase; colchicine and nocodazole do so at the M phase, and 5-fluorodeoxyuridine halts the S phase of the cell cycle. Without the experimentally cultured cells, it is impossible to synchronize mammalian cells under in vivo conditions or inside the body.
5 Mammalian Cell Culture-Driven Vaccine Production
Vaccination is the twentieth century’s greatest public health triumph. It is the process of conferring protection to a mammalian body against a disease-causing pathogen or more specifically pathogen-generated molecules either by administering heat-killed or attenuated whole pathogen or a part of a pathogen. Vaccines are either prophylactic or therapeutic, with the former being used entirely against a physiologically normal host and the vaccine itself also cannot cause any diseased condition in the host’s body. Upon administering a prophylactic vaccine, the host organism (immunological cells) produces memory B cells and memory T cells. These memory B and T cells can be stored for years in the secondary lymphoid organs such as the spleen, lymph nodes, mucosa-associated lymphoid organs (MALT), gut-associated lymphoid organs (GALT), etc. In the event of any subsequent attack by the same pathogen/antigen on the host’s body, the memory cells against that particular pathogenic antigen readily recognize the pathogen/antigen and through a series of immunological reactions, effectively eliminate the pathogen/antigen. In therapeutic vaccination, the mammalian subject is already infected with a pathogen, and administering the vaccine to the subject either neutralizes or eliminates the pathogen/antigen. In therapeutic vaccination, since there is no formation of memory cells, the effect of the therapeutic vaccine is transient or for a short duration only. It infers that the therapeutic vaccine must be used every time the same pathogen enters the mammalian body and the vaccine is highly useful to neutralize or destroy the pathogen as long as there is no mutation in the epitope of the pathogen (antigenic drift/antigenic shift) against which the vaccine was produced (Plotkin et al. 1969; Montagnon et al. 1981).
Vaccination eradicated smallpox, lowered the global incidence of polio by 99% since 1988, and achieved dramatic reductions in measles, diphtheria, whooping cough (pertussis), tetanus, and hepatitis B. Approximately 20 vaccines are currently in use, contributing a small proportion ever since the first human vaccine was developed by Jenner in 1796 until today. This indicates the substantial major difficulties encountered to develop new vaccines with a large number of trials and clinical assays needed to ensure maximum safety and efficacy for patients. Vaccines for polio, measles, mumps, rubella, chickenpox, and more recently rotavirus and human papillomavirus (HPV) are currently being manufactured using cell cultures. Mammalian cells are used either as a host of the virus to be cultured or as a factory for producing recombinant proteins from the virus.
In general, vaccine generation against the influenza virus is accomplished using a chicken egg-based system and not using mammalian cell culture. Due to the H5N1 pandemic threat, research attempts involving cell culture for influenza vaccines are currently being funded by the US government, including the use of mammalian, avian, and insect cell-based processes as well as vegetable cell line and plants. Presently, a large number of scientists throughout the world had worked very hard to develop vaccines against COVID-19 in a relatively short duration and are continuing to develop the new COVID-19 vaccine, particularly for babies, toddlers, and young teenagers. Of note, the COVID-19 pandemic is caused by a single-stranded RNA virus, called SARS-CoV-2. As a consequence, currently, all paths are open, including novel insights from the recombinant DNA-based vaccines (made with new vectors) and the use of novel adjuvants. However, the removal or inactivation of adventitious viruses remains a unique challenge. Risk assessment related to cell culture techniques is more or less the same as identified in the 1950s.
Among the advantages of using cell culture-based manufacturing processes to produce vaccines include the following:
-
The capability for manufacturers to increase vaccine production with ease.
-
This enables vaccine production to be enhanced in proportion to easily meet any sudden increase in demand for vaccines such as in the event of a pandemic.
-
The ability to produce vaccines faster.
-
The production time of vaccines using a cell culture-based process reduces vaccine generation time by half about the embryonic egg process.
-
The reduced possibility of viral culture mutation during the manufacturing process.
-
Virus mutation can result in culturing vaccine failure and this may be possible while using embryonic eggs.
-
Cell-based vaccines are cultured in biosafety level 3 (BSL3) conditions.
-
This biosafety level provides an isolated environment to ensure safer generation and handling of pathogenic viruses without escaping into the environment.
-
People who are allergic to vaccines made from chicken eggs may not suffer similar allergies to vaccines made from cell cultures. Table 1 describes the susceptible cell lines of some widely used pathogenic viral stains, vis-à-vis manifested infection propagating tendencies.
However, the cell-based manufacturing process has the following disadvantages, which limit its application feasibility:
-
The relatively higher manufacturing costs. This may translate to more expensive vaccines. This process produces fewer viruses for vaccine manufacturing.
-
The volumetric yield of cell-based flu virus is about fourfold lower than the egg-based process. This means a requirement for a larger bioreactor volume along with a much higher capital investment for the production plant. This will further add to the vaccine cost.
-
This production method is relatively new in comparison to the process using embryonic eggs. Prominently, there is a lack of long-term safety or rare adverse event data.
5.1 Propagation of Virus in the Cultured Mammalian Cells and Vaccine Production
The propagation and vaccine production against a virus involves the following steps:
-
Step 1: Cell line selection and culture
-
Step 2: Propagation of virus in the cultured cells
-
Step 3: Harvesting and purification of viruses
-
Step 4: Inactivation and splitting of viruses
-
Step 5: Formulation of vaccines (adding adjuvants, preservatives, stabilizers)
-
Step 6: Quality control/quality assurances and batch release
Here is a brief description of the above steps:
5.1.1 Step 1: Cell Line Selection and Culture
-
Generally, continuous cell lines like Vero, HepG2, MDCK, CHO, etc. are the best options for viral cultures.
-
The cell line is produced in a seed lot system.
-
The chosen cell line must be able to propagate the virus in a large quantity and rapid and efficient manner.
-
In general virus, DNA should not integrate into the host cell genome (the virus should not activate the lysogenic cycle) (Browne and Al-Rubeai 2007).
5.1.2 Step 2: Propagation of Virus in the Cultured Cells
-
Before large-scale virus propagation begins, the virus must be checked for impurities, including other similar viruses and even mutated variations of the same virus. No antigenic drift or antigenic shift should be prevalent.
-
The seed must be kept under ideal conditions, usually frozen so that the virus is prevented from becoming either stronger or weaker than desired.
-
The virus must be stored in small glass or plastic containers.
-
A record of origin, passage history (including purification and characterization procedures), and storage conditions should be maintained for each seed batch.
-
Manufacturing begins with the use of small extents of a specific virus as a seed culture. Cell line propagation begins with the small-scale pre-culture propagation of seed cells after thawing.
-
The cells are then introduced to the bioreactor (bioreactors are used for large-scale cell cultures, inherently for industrial purposes, covered in Chap. 14 of this book) with the selected nutrient medium.
-
When the cell line reaches a predetermined cell density, the virus is introduced into the cell line following which it propagates in the cell line.
-
Two methods of mass (cell) cultivation are recognized in the industry, namely, microcarrier culture and free cell suspension cultures.
-
Both systems begin with cell line cultivation in a bioreactor, which can be further scaled up to thousands of liters.
5.1.3 Step 3: Harvesting and Purification of Viruses
-
Product isolation involves the removal of those components whose properties vary markedly from that of desired products.
-
Purification selectively separates and retains the desired products at the highest purity as per the pre-determined specification (removing unwanted compounds).
-
The most common method of vaccine production is based on an initial bioreactor cell culture followed by purification. Differential centrifugation, filtration, and different modes of chromatography, namely, ion-exchange chromatography, gel filtration chromatography, affinity chromatography, etc., are used to purify viruses.
5.1.4 Step 4: Inactivation and Splitting of Viruses
Viruses can be lipid-coated (enveloped) or non-enveloped. Virus inactivation involves dismantling a virus’s ability to infect cells without actually eliminating the virus.
Virus inactivation works by one of the following mechanisms:
-
By attacking the virus envelope or capsid and destroying its ability to infect or interact with host cells
-
By disrupting the viral DNA/RNA and preventing its replication
The following materials may be utilized for viral inactivation:
-
A.
Solvent detergent inactivation
-
B.
Pasteurization
-
C.
Acidic pH inactivation
-
D.
Ultraviolet inactivation
Here is a brief description of the materials needed for virus inactivation:
-
A.
Solvent detergent inactivation
-
Effective with lipid-coated viruses.
-
The detergent used in this method disrupts the interactions between molecules in the lipid coat, rendering the coat dysfunctional and impending replication.
-
Most enveloped viruses cannot live without their lipid coat, so they will die when exposed to these detergents.
-
Other viruses may still live but they are unable to reproduce, making them ineffective.
-
The detergent typically used is Triton X-100.
-
-
B.
Pasteurization
-
This process is effective for both non-lipid and lipid-coated viruses.
-
Because pasteurization involves increasing the temperature (63 °C for 30 min) of a solution to a limit that denatures the viral capsid proteins, it does not matter whether the virus is lipid-coated or not.
-
-
C.
Acidic pH inactivation
-
A most effective method for lipid-coated viruses.
-
Acidic condition inactivates the virus.
-
Incubation typically occurs at a pH of 4 and lasts anywhere between 6 h and 21 days.
-
-
D.
Ultraviolet ray inactivation
-
UV rays (wavelength 260 nm) can be used to inactivate viruses since virus particles are small and UV rays can access the genetic material, including the thymine dimerization (TMD) of the same DNA strand.
-
Once the DNA dimerizes, the virus particles cannot replicate their genetic materials.
-
In TMD, the thymine nucleotides of the same DNA strand join together and prevent the DNA to replicate.
-
5.1.5 Step 5: Formulation of Vaccines
The most important constituent of a vaccine is the particle/molecule/protein isolated from the microorganism/virus. This specific particle/molecule/protein needs to be purified from the lysed virus using various types of chromatography, electrophoretic separations, etc. The other components comprise suspending fluids. The final formulation must be thoroughly devoid of whole or live viruses.
5.1.5.1 Preservatives, Stabilizers, Antibiotics, and Antimycotics for Immunogenic Retainment of Vaccines
-
Monosodium glutamate (MSG ) and 2-phenoxy ethanol are used as stabilizers in a few vaccines to help the vaccine remain unaltered on being exposed to heat, light, acidity, or humidity.
-
Antibiotics are added to some vaccines to prevent the growth of microorganisms. The most frequently used antibiotics include neomycin, streptomycin, polymyxin B, chlortetracycline, and antimycotic amphotericin B.
-
Thimerosal may also be used in the containers of some vaccines as a preservative.
5.1.5.2 Adjuvants or Enhancers
-
Aluminum gels or salts (alum).
-
Alum is used in several licensed vaccines including H. influenzae, inactivated poliovirus, hepatitis A virus, etc.
5.1.5.3 Inactivating Agents
-
Formaldehyde is used in the formulation of some vaccines such as influenza, diphtheria, polio vaccines, etc.
NB: In general, formaldehyde is removed before packaging vaccines owing to its toxicity to human cells.
β-Propiolactone is used against the rabies virus.
5.1.6 Step 6: Quality control and Batch Release
Table 2 describes various quality control/quality assurance tests along with their screened parameters.
5.1.6.1 Interference Test
For products having two or more antigenic components, the test must confirm null interference between individual components, that is, one component suppressing the protective immunological response to another.
5.1.6.2 Consistency of Production
Before marketing approval of any product, each establishment should produce three consecutive production batches/serials of the completed product (in its facilities) to evaluate the production consistency.
5.1.6.3 Stability Tests
Stability studies (based on an acceptable potency test) are required to establish the validity of the expiry date that appears on the product package.
5.1.6.4 Batch/Serial Release for Distribution
Before release, the manufacturer must test each batch/serial for the following:
-
Batch/serial purity test
-
Batch/serial safety test
-
Batch/serial potency test
Ahead is a brief discussion about them:
5.1.6.4.1 Batch/Serial Purity Test
Purity is determined by testing for a variety of contaminants. Tests to detect contaminants are performed on master seeds, primary cells, master cell stock, ingredients of animal origin if not subjected to sterilization (e.g., fetal bovine serum (FBS), bovine albumin, etc.), and each batch of the final product before release.
5.1.6.4.2 Batch/Serial Safety Test
Batches are considered satisfactory if local and systematic reactions to vaccination with the batch to be released are in accord with those described in the registration dossier and product literature.
5.1.6.4.3 Batch/Serial Potency Test
A batch/serial potency test is required for each batch before release. These tests are designed to correlate with the host animal vaccination-challenge efficacy studies.
5.1.6.4.4 Other Tests
Depending on the form of vaccine being produced, certain tests may be indicated.
These tests may concern:
-
The level of moisture contained in desiccated products
-
The proportion of residual inactivated virus in killed products
-
Complete inactivation of killed products
-
pH
-
The extent of preservatives and permitted antibiotics
-
Physical stability of the adjuvant
-
Retention of vacuum in a desiccated product
-
A general physical examination of the final vaccine
5.1.6.5 Sampling
Sample should be selected from each batch/serial of product. The selector should pick arandom representative sample which could ensure uniformity of standard quality.
5.1.6.6 Labeling
Standards for labeling products vary from country to country basis (Walter et al. 1992; Werz et al. 1997). Figure 1 summarizes the chronological steps in vaccine production on an industrial scale.
6 Recombinant Protein Production Using Mammalian Cell Culture
Recombinant DNA technology (RDT) or genetic engineering is a process through which a specific gene of interest (called an insert) is inserted (technically called ligated) into a DNA vector for its multiplication (technically called cloning) and expression (synthesis of desired protein).
In RDT, vectors are specific DNA having a capacity to accept a foreign DNA (which is our gene of interest) for cloning (making multiple identical copies) and expression (synthesis of protein) in a suitable host cell. The protein produced by recombinant DNA technology is called recombinant or chimeric protein.
A DNA vector is incapable of cloning and expressing the gene of interest, without a host cell. While several different host cells including prokaryotic Escherichia coli and single-cell eukaryotic cells such as yeast (e.g., Saccharomyces cerevisiae) can be effectively and easily utilized for cloning and expression of various genes, multiple mammalian cells including the Chinese hamster ovary (CHO), human embryonic kidney (HEK), etc. are the best choice as the host for cloning and mammalian gene expression (Wurm 2004; Aricescu et al. 2006; Lai et al. 2013; Hunter et al. 2019).
This section is divided into two parts:
-
F.I. Process to Produce a Mammalian Protein Using Recombinant DNA Technology
-
F.2. Major Recombinant Proteins Produced by Mammalian Cell Culture
Here is a brief discussion about them:
6.1 Process to Produce a Mammalian Protein by Recombinant DNA Technology
In this section, the various steps involved in recombinant DNA technology are discussed.
6.1.1 Steps to Produce Recombinant Proteins
Initially, the gene of interest (GOI or gene of interest: the gene programmed for cloning and recombinant protein production) that produces the desired recombinant protein must be optimized. The isolation of a specific gene encoding a specific product (protein) can be made either from the mammalian genome (genomic library/cDNA library) or via specific sequence-driven synthesis. The gene must have the necessary transcription elements for the production of a stable and mature mRNA equivalent to the capacity of producing a complete desired protein (Fig. 2).
While the majority of (~90%) prokaryotes possess only one large DNA constituted of several genes, a eukaryotic cell contains many DNAs. For example, a human somatic cell contains 46 DNAs. In recombinant DNA technology, gene is defined as the small unit of DNA having the capacity to produce a single protein (in monocistronic eukaryotes) or more proteins (in polycistronic prokaryotes). Cloning implies making multiple copies of the gene of interest (GOI)/DNA of interest (technically also called an insert) by joining it with an auto-replicating (self-replicating) vector DNA to form a recombinant or chimeric vector. Thus, adequate standardization and characterization of a suitable vector are necessary for screening the ability to incorporate a foreign DNA, making it multiple copy clones and express the GOI in the in vitro cultured mammalian cells. In addition, a second gene present either in the same or different vector is transferred, conferring a selective advantage to recipient cells before transferring the recombinant vector into a suitable host cell (Schimke 1984; Omasa 2002).
The GOI expression is host-specific since a vector (a single carrier) or a recombinant vector (intentionally driven) needs a host cell for its multiplication and subsequent expression. Today, there is a wide range of expression systems available for large-scale recombinant protein production. These expression systems include Escherichia coli, baculovirus-mediated insect cell expression, yeast, and several mammalian-based systems. Each vector has its respective advantages concerning cost, usage simplicity, and implicit posttranslational modification profiles. In the presence of the selection agent, (generally administered after a few days of gene transfer), only those cells that express the selector gene survive.
Transfection involves the transfer of naked recombinant vectors/DNA to compatible mammalian host cells. In today’s RDT experiments, various transfection procedures are used such as transformation (involving Escherichia coli as a host cell), electroporation (use yeast and hard to transfect host cell), or just simple lipid-based transfection reagents (e.g., lipofectamine) or other transfection reagents (e.g., transfectamine) or nanoparticle-based transfection reagents (Sigma’s N-TER™) are used for mammalian cells.
After transfection of the host cell line with the expression vector containing the GOI and selection marker, the host cells grow and undergo drug selection enabling the screening of the desired host containing the recombinant vector. When gene amplification systems are used, concentrations of selection agents (e.g., MTX or MSX) can be increased stepwise to derive more productive cell clones. Cell clones with high recombinant protein titer are chosen for progressive expansions before cell banking and further clone evaluations such as production stability of the cell clones and quality of recombinant protein.
Following selection, surviving cells are transferred as single agents to a second cultivation vessel, and the cultures are expanded to produce clonal populations. Eventually, individual clones are evaluated for recombinant protein expression, with the highest producers being retained for further cultivation and analysis. From these candidates, one cell line with the appropriate growth and productivity is chosen for generating the recombinant protein. A cultivation process is then established as per the production requirements. So far, all mammalian recombinant therapeutics are naturally secreted proteins or have been developed from gene constructs involving protein secretion using rough surface endoplasmic reticulum (ER) and Golgi apparatus secretory pathway.
Here is the explanation of the steps involved in cloning and expression of various recombinant proteins using mammalian host cells:
-
1.
Optimization of gene of interest
-
2.
Selection of vector and optimization of mammalian expression system
-
3.
Selection of host cells
-
4.
DNA delivery and integration: transient and stable transfection
-
5.
Selection and optimization of positive clones
-
6.
Selection and optimization of cell culture medium
-
7.
Selection and optimization of cultivation mode: adherent vs nonadherent (perfusion and fed-batch)
-
8.
Purification of the expressed protein
-
9.
Quality control and quality assurances
Here is the step-by-step discussion of the above points:
6.1.1.1 Optimization of Gene of Interest
Gene is defined as a structural and functional unit of DNA. DNA consists of a linear sequence of many nonoverlapping genes. In humans, while the somatic cell contains 46 DNA, the reproductive or germ cell (sperm/ovum) contains only 23 DNAs. Every DNA has a specific number and a characteristic length and a proportionate varying number of distinct genes. Structurally, a mammalian gene includes the coding sequence (exons) for a protein the noncoding sequence (introns), having a regulatory role, the promoter (the region binding with the RNA polymerase to initiate transcription), and the terminator (the region which ends transcription). Functionally, a gene transfers genetic information from one generation to the other in the form of mRNA (synthesized via transcription), followed yet again by the synthesis of protein through translation.
To clone a small GOI, one can synthesize it artificially. However, to get a large GOI, one may use either a cDNA library or a genomic library. Due to the enormous size of the mammalian genome, the larger genomic library (a collection of genes in suitable vector and collective representation of the entire genome) is used to clone mammalian genes. Indeed, it is a mammoth task to identify any GOI from the genomic library. Therefore, isolation of the GOI from the cDNA library (collection of protein-coding exons only in a suitable vector, representing all mRNAs) is the best choice.
For preparing a cDNA library, mRNA is purified from cells using oligo-(dT) cellulose chromatography. The mRNA molecules bind to the oligo-(dT) linked to the cellulose column via polyA tails, while the remainder of RNA species flow through the column. The bound mRNAs are then eluted from the column. When the mRNA has been purified, double-stranded DNA must be synthesized from the cDNA.
One can choose any of the following sources to collect mRNA:
-
Gonadotrophic cells of the anterior pituitary produce follicle-stimulating hormone (FSH).
-
Human kidney cell line HT1080 secretes urokinase.
-
Endothelial cells from blood vessels synthesize tissue plasminogen activator (tPA).
-
Liver hepatocytes synthesize blood clotting factors like clotting factor VIII.
-
Pancreatic islets synthesize hormones like insulin, glucagon, and somatostatin.
-
Duodenal cells synthesize epidermal growth factor (EGF).
While a GOI can be collected and isolated from the somatic cells present in any of the mammalian organs (because technically all the somatic cells contain the same gene or DNA), a specific cell type may be preferred because of the exact ORF (an ORF is a continuous stretch of codons beginning with a start codon (usually AUG) and ends at a stop codon (usually UAA, UAG, or UGA) of the GOI in specific somatic cells). In its native context, a GOI in other tissues may contain secondary structures, mRNA that might inhibit ribosome processing, alternative splicing sites, sequence elements signaling mRNA degradation, or codons that are rarely used in an expression host. Therefore, the variables that affect the ORF of the GOI and its ability to produce large extents of proteins in mammalian cells can be numerous. De novo DNA synthesis provides the researchers with the ability to create a full-length gene considering these parameters and controlling the presence or absence of specific restriction sites or motifs.
In addition to the optimization of the gene associated with the recombinant protein of interest, one must consider the subcellular location of the protein. The widespread use of mammalian cells has been dominated by the production of secreted proteins that require a signal sequence directing the synthesis of needed protein outside the cell.
The secretory proteins are produced by the rough surface endoplasmic reticulum (RER). While the protein synthesis is initiated on the ribosomal surface and continues, the amino terminus (leader sequence) of the de novo generated protein binds with the transporter of the signaling sequence (TRAP) and enters into the lumen of RER through sec 61 (a pore-forming protein on the RER surface). In the RER, complete folding (secondary to quaternary structure) and posttranslational modifications (including advanced N-linked glycosylation) of the protein take place before being secreted toward the cis-Golgi apparatus. Typically, RER secreted protein has a signaling sequence that binds with various vehicles (named as COP1, COP2, etc.) and enters the Golgi apparatus. In the Golgi apparatus, the protein is further modified (e.g., O-linked glycosylation), undergoes maturation, and is finally secreted from the trans-Golgi apparatus for the specific destination (may be any subcellular compartments including the membranes or extracellular space). For secretory proteins, the protein must be secreted into the extracellular space. Of note, the signaling sequence present in the protein determines its implicit final destination.
It has been reported that the expression of a recombinant protein does not always correlate with its mRNA levels, and a rate-limiting step can be the secretory pathway. Intuitively, the best choice of a signal sequence may be the protein’s native signal. However, testing a panel of commonly used signal sequences is desirable. Not surprisingly, the signal sequence can have a dramatic effect on protein productivity, with even fourfold enhanced expression levels.
Recombinant proteins of mammalian origin are commonly expressed in eukaryotic expression systems, particularly human cells as the host of choice to ensure the formation of disulfide bridges and proper glycosylation. Antibody and antibody-like molecules are examples of proteins that are relatively easily made in mammalian cells and are easily purified by protein A or protein G resin-dependent affinity chromatography. However, some recombinant proteins, sub-domains, and mutant protein versions can be plagued with issues regarding misfolding, aggregation, or entirely lacking expression. Fusion tags are frequently used to address such issues.
6.1.1.2 Selection of Vector and Optimization of Mammalian Expression System
A vector is a DNA molecule having the ability to accept any foreign DNA and spontaneously replicate it as and when it will replicate its DNA inside the host cells. As described in previous paragraphs, in molecular cloning, the foreign DNA has termed a gene of interest or GOI. So, a vector can make multiple copies of the GOI inside a suitable host cell. For expressing heterologous genes in mammalian cells, usually, vectors derived from mammalian viruses are used (Sambrook et al. 1989; Yarranton 1990; Kost and Condreay 2002).
A mammalian expression vector must have the following sequences:
-
Characteristics of normal cloning vectors such as the origin of replication, multiple cloning sites for insertion of GOI, unique restriction sites, selectable maker(s), and auto-replicating capacity.
-
Contains a eukaryotic origin of replication from an animal virus, e.g., Simian virus 40 (SV40).
-
May contain sequences for propagation in the prokaryotic host (Escherichia coli) and origin of replication from Escherichia coli (usually acts as a shuttle vector).
-
The GOI must contain a start codon.
-
A vector must contain an efficient promoter sequence for high-level transcriptional initiation. A strong promoter is essential to drive the expression of product gene(s). A strong promoter indicates a region of DNA has a better and stronger affinity with the RNA polymerase. Viral genetic elements are used to construct several eukaryotic expression vectors. Viruses are highly efficient replicators and viral gene expression is adapted to eukaryotic systems. Therefore, the strategy has been to use the regulatory elements of the viral genome, i.e., promoters, enhancers, polyadenylation signals, introns, replication origins, IRES elements . Moreover, the use of transcription control regions is also important. Very strong promoters, small introns (e.g., CMV intron), and regulatory elements are often constitutive and require only host transcription factor binding. Promoters such as those derived from Simian virus 40 (SV40) early promoters, the Rous sarcoma virus (RSV) long terminal repeat promoters, and cytomegalovirus (CMV) immediate early promoters constitutively drive the gene expression placed under their control. Inducible systems can also be used such as heat shock protein (HSP) inducible promoters, glucocorticoid hormone inducible promoters, and several others. However, the promoter sequences in general suffer leaky gene expression. Of note, nonviral promoter, such as the elongation factor (EF)-1, is also known.
-
The vector must contain a transcription start site.
-
The vector must contain a ribosome binding site (Kozak sequence, for eukaryotic/mammalian cells).
-
The use of transcription control regions in the vector is also vital (Fig. 3).
-
A vector must contain mRNA processing signals . Codon optimization for the target cell type, GC/AT ratio balancing, and signal sequence optimization have been demonstrated to accelerate mRNA processing and improve secretion.
-
Transcription termination sequences: Adenylation signals from animal viruses, e.g., SV40, are essential to add to the vector.
-
The vector must contain certain selectable markers and promoter sequences that drive the selectable marker gene(s). The common approach used in generating cell lines for producing therapeutic proteins relies on gene amplification induced by a selective marker such as dihydrofolate reductase (DHFR) or glutamine synthetase (GS). Bacterial gene neo (encoding neomycin phosphotransferase) confers resistance to G418 (geneticin, G418 sulfate). When DHFR is in use, the recipient cell must have a defective DHFR gene which makes them unable to grow in the presence of methotrexate (MTX), unlike transfected cells having a functional DHFR gene.
-
Besides gene-targeting technology, chromatin opening elements and attachment regions should also be incorporated into vector genetic machinery to augment the final product production.
-
Matrix-attachment regions.
-
Chromatin insulators and locus control regions.
-
Vectors must also possess the elements that create a genomic environment for high transcriptional activity (positional independence).
-
Targeting of expression vector to the transcriptionally active site in the genome is accomplished using homologous recombination.
-
Examples of mammalian expression vectors include the adenoviral vectors, the pSV (a plasmid vector designed for the expression of cloned sequences in mammalian cells driven by the SV40 early promoter and enhancer), and the pCMV (a plasmid vector containing cytomegalovirus immediate early promoter) series of plasmid vectors, vaccinia and retroviral vectors (permanently integrate the GOI into the host cell genome), and Baculovirus (DNA viruses that infect insect cells) vectors (Fig. 4).
6.1.1.3 Usefulness of Mammalian Expression Vector
Mammalian expression vectors offer considerable advantages (for the expression of mammalian proteins) over bacterial expression systems. The advantages of the mammalian expression system are as follows:
Mammalian expression vectors exhibit proper folding, posttranslational modifications, and relevant enzymatic activity. These may also be more desirable than other eukaryotic nonmammalian systems (e.g., yeast vectors such as YAC) whereby the expressed proteins may not contain the correct extent of glycosylation. These are of particular significance in producing membrane-associating proteins that require chaperones for proper folding and stability besides being comprised of numerous posttranslational modifications. The downside, however, is the low yield of product compared to prokaryotic vectors as well as the costly nature of the optimization and characterization techniques. The complicated technology and potential contamination with animal viruses of mammalian cell expression also manifested a constraint on their use in large-scale industrial production.
6.1.1.4 Drawbacks of Using Mammalian Expression Vector
The drawbacks of using mammalian expression vectors are as below:
-
Complicated technology involves complex requirements.
-
Possible contamination of animal viruses.
-
Generally, high cost is involved in mediating recombinant protein expression within the mammalian expression system.
6.1.2 Selection of Host Cells
For recombinant mammalian protein generation, mammalian cells are the first choice for recombinant vector transfection and subsequent recombinant protein expression. Mammalian host cells have several advantages for mammalian protein production when compared with single-cell eukaryotic yeast cells or even prokaryotic cells such as Escherichia coli (Browne and Al-Rubeai 2007).
The potential advantages of using mammalian cells as host cells are as follows:
-
Efficient intron removal using splicing (if used gene is from genomic library instead of cDNA library)
-
Mammalian/human-specific posttranslational modifications
-
Highest functionality due to posttranslational modification
-
High compatibility concerning humans
-
Low immunogenicity to humans
-
Safe to use
However, the use of mammalian cells includes some drawbacks also. The drawbacks of using mammalian cells as hosts are as follows:
-
Mammalian cells are fragile and sensitive to shear stress.
-
Slow growth.
-
Mandate fastidious growth requirement.
-
Selection take up time.
-
Expensive culture techniques.
-
Difficult to achieve transfection of gene of interest (low transfection efficiency).
-
Risk of animal viruses contamination.
-
Stringent control is required for screening contaminated viruses.
-
Sometimes specialized cell lines are needed for specific modifications.
Here is a brief description of frequently used mammalian cell lines for producing recombinant proteins.
6.1.2.1 Mammalian Cell Lines Used in Recombinant DNA Technology
Selected mammalian cell lines widely utilized for recombinant proteins production are as below:
-
Chinese hamster ovary (CHO) cells
-
NSO cell line
-
Human embryonic kidney (HEK) 293 cells
-
HT-1080 cell line
-
PER.C6 cells
Other mammalian cells used for recombinant protein production are the baby hamster ovary (BHO) cell line, COS cell line, HeLa, A549, MCF-7, HepG2, NIH3T3, U2OS, CAD, P19, L929, N2a, Y79, SO-Rb50, DUKX-X11, and J558L.
Ahead is a brief discussion of some of the widely used mammalian cell lines for recombinant DNA technology:
6.1.2.1.1 Chinese Hamster Ovary Cells
Regarding the various mammalian cells, Chinese hamster ovary (CHO) cells are the first line of choice for the stable expression of mammalian genes. The approval of CHO-derived tissue plasminogen activator (tPA, activase) in 1986 revolutionized medicine, raising the possibility of using mammalian cell culture for manufacturing therapeutic proteins. More than 30 years after tPA approval, CHO cells are the predominant hosts used to generate several therapeutic proteins. About 70% of all recombinant proteins produced today are made in CHO cells, including DUXB11, DG44, and CHOK1 lineages. While DUXB11 and DG44 cells do not have dihydrofolate reductase (DHFR) activity, the CHOK1 cells do exhibit endogenous DHFR activity. CHO cells remained the most preferred mammalian cell line for generating recombinant therapeutic proteins for several reasons which are discussed in the following points:
-
First, while CHO cells are naturally adherent in nature, they are capable of adapting and growing in suspension culture, ideal for large-scale (industrial) culture. In suspension culture, cells grow in larger densities than in the adherent culture.
-
Second, CHO cells pose less risk as few human viruses can propagate in them.
-
Third, CHO cells can grow in serum-free (less expensive) and chemically defined cell culture medium, ensuring reproducibility between different cell culture batches.
-
Fourth, CHO cells allow posttranslational modifications (PTMs) to recombinant proteins which are compatible and bioactive in humans. Specifically, glycosylation of glycoproteins produced by CHO cells is more humanlike, devoid of the immunogenic α-galactose epitope. However, CHO cells are unable to mediate human glycosylation (CHO cells lack α-sialyltransferase and α-fucosyltransferases) and produce glycans that are not expressed in humans, namely, α-gal and N-glycolylneuraminic acid (NGNA; a sialic acid which is not synthesized by humans). CHO cells can produce galactose-α-1,3 antigens on proteins. Circulating antibodies against both of these N-glycans are present in humans and are likely to manifest increased immunogenicity and altered pharmacokinetics upon being used in humans.
NB: It was later shown that CHO cells express low NGNA levels and that humans incorporate NGNA into proteins from dietary sources, which tempered immunogenicity concerns.
-
However, the attachment of nonhuman glycans may not be a concern for therapeutic proteins which do not require glycosylation, illustrating the importance of considering the specific product on choosing an appropriate cell line for protein production.
-
Fifth, several gene amplification systems are well established to make use of CHO cell’s genome instability and allow the consequent gene amplification, ultimately resulting in higher recombinant protein yield. Currently, recombinant protein titers from CHO cell culture have reached the gram per liter range, a nearly 100-fold improvement over a similar process in the 1980s. The significant titer improvement is substantially due to the progress in the establishment of stable and high-producing clones as well as significant culture process optimization. Due to these reasons, CHO cells are established host cell lines for regulatory approvals of therapeutic glycoprotein products.
6.1.2.1.2 NSO Cell Line
The NSO cell line originates from non-secreting mouse plasmacytoma (myeloma) cells that have undergone multiple cloning and selection rounds to yield immortalized non-IgG-secreting B cells. However, these cells possess the appropriate machinery for producing and secreting various monoclonal antibodies such as palivizumab and ofatumumab. Thus, NSO cells are non-immunoglobulin-secreting myeloma cells. These cells can be cultivated in serum and non-serum-containing cultivation medium and are reasonably amenable to scale up in large cultivation vessels (up to 20,000 L capacity).
However, NSO cells present some drawbacks that complicate their cultivation. Unlike most mammalian cell lines, NSO cells seldom grow in the absence of exogenous cholesterol (behave as cholesterol auxotrophs) and are therefore routinely cultivated in the presence of cholesterol, usually delivered from the serum. Since the presence of animal origin ingredients, as well as other proteins, is undesired in the cultivation medium, it complicates the use of NSO cells due to the difficulty of supplying cholesterol in a protein-free medium as it requires carriers such as cyclodextrins to enhance cholesterol “solubility.” The development of cholesterol-independent NSO cells has been demonstrated, although with a certain unpredictability that has limited their use.
Recent advances into the mechanism of cholesterol requirement have linked epigenetic gene silencing caused by methylation upstream of the 17-hydroxysteroid dehydrogenase type 7 coding region that catalyzes the lanosterol to lathosterol conversion, which has been listed as the cause of this deficiency. Although industrial groups have developed cholesterol-independent NSO lineage, no commercial production of mAbs using NSO cholesterol-independent cells is presently being pursued. It is quite possible (given their usage simplicity) that these biochemically and genetically understood cholesterol-independent cell lines could eventually be used for commercial production.
NSO cells lack endogenous glutamine synthetase (GS) activity, making them suitable for use with GS as a selectable marker for recombinant antibody expression. High antibody productivity has been reported from non-GS NSO cell lines as well. Mouse-derived cell lines, including NSO, produce N-glycolylneuraminic acid (NGNA; a sialic acid that cannot be synthesized by humans) at appreciable extents. This sialic acid form was initially believed as a potential immunogenicity concern in humans. Murine cells, including NSO, do produce alpha-Gal-alpha (1,3) Gal linkages, which antibodies have been shown to express in humans. Although NSO cells have been used in industry to produce therapeutic antibodies, their potential immunogenicity aspects have likely limited their use for therapeutic antibody production.
6.1.2.1.3 Human Embryonic Kidney 293 Cells
In 1973, Dr. Alex Van der EB’s laboratory from the University of Leiden, Holland, generated a cell line from human embryonic kidney (HEK) cells of an aborted normal human fetus via transformation with sheared adenovirus 5 DNA. In this transformation, a 4.5-kilobase (kb) DNA from the viral genome was incorporated into the human chromosome 19 of the HEK cells. Thus, the HEK name originated from human embryonic kidney cells, and the number 293 was probably the experiment number in Alex Van der EB’s laboratory.
HEK-293-T is a human cell line derived from the HEK-293 cell line that expresses a mutant version of the SV40 large T antigen. The HEK293 cell line stably expresses the Epstein-Barr virus nuclear antigen-1 (HEK293-EBNA1, or 293E). These cells are loosely adherent and can also grow as suspension cultures. This is the most commonly used cell line for large-scale culture owing to its capability of human-specific posttranslational modifications (PTMs). In the past few years, five therapeutic agents produced in HEK293 cells have been approved by the Federal Drug Administration (FDA, USA) or the European Medicines Agency (EMA) for therapeutic use. These agents are drotrecogin alfa (Xigris; Eli Lilly Corporation, Indianapolis, IN), recombinant factor IX Fc fusion protein (rFIXFc; Biogen, Cambridge, MA), recombinant factor VIII Fc fusion protein (rFVIIIFc; Biogen, Cambridge, MA), human cell line recombinant factor VIII (human-cl rhFVIII; NUWIQ; Octapharma, Lachen, Switzerland), and dulaglutide (Trulicity; Eli Lily, Indianapolis, IN).
6.1.2.1.4 HT-1080 Cell Line
HT-1080 is a human fibrosarcoma cell line. This cell line was created from tissues taken in a biopsy of a fibrosarcoma present in a 35-year-old human Caucasian male. The patient, who served as a sample source, had not undergone radio- or chemotherapy, making the introduction of unwanted mutations into the cell line a remote possibility. The cell line carries an isocitrate dehydrogenase 1 (IDH1) mutation and an activated N-RAS (RAS: rat sarcoma) oncogene . This cell line is capable of human-specific posttranslational modifications (PTMs) and is used for the production of agalsidase alpha (used in Fabry disease), idursulfase (Hunter syndrome), velaglucerase alfa (type 1 Gaucher disease), etc.
6.1.2.1.5 PER.C6 Cells
Among the emerging mammalian cell lines, the PER.C6 cell line appears to be the most advanced in its usage and acceptance. Cells of this cell line are derived from human embryonic retina cells immortalized by transfecting the E1 genes from adenovirus 5 DNA. Like NSO and CHO cells, PER.C6 cells can proliferate indefinitely in suspension under serum-free conditions. PER.C6 cells offer the potential for a humanlike glycosylation pattern with an added advantage of null undesired murine glycans. Several recent communications have disclosed that Per.C6 cells can be cultivated to very high densities at large-scale fed-batch culture, and their capability of supporting enhanced recombinant protein yields up to 8–10 g•L−1 of a tested monoclonal antibody (mAb). These promising data are vital aids for the Per.C6 cell line to gain appeal in the next few years as a potential platform for the production of recombinant mAbs or other proteins. Several Per.C6-based products are currently undergoing clinical trials. However, no mAb production platform based on Per.C6 cell cultivation has yet reached the regulatory registration stage. Regulatory concerns exist regarding the use of human-based cell lines for mAb production due to their lack of resistance against adventitious agents.
Additional cell lines such as baby hamster kidney (BHK-21) cells which are used for the production of factor VIII antigen are being highly researched. Of note, factor VIII antigen is involved in blood coagulation. African green monkey kidney (or COS) cells are also widely used for transient transfection of mammalian genes. COS is an acronym, derived from the cells being CV-1 in origin alongside carrying the SV40 genetic material. Another important cell line of use for recombinant protein production is SP2/O. All these cell lines have their advantages and disadvantages and so users must carefully choose them even before starting their research on recombinant protein production.
6.1.2.2 Process-Related Safety Concerns Using Mammalian Cell Line
For proteins produced in nonhuman as well as in human cell lines, potential safety concerns arise from the possibility of process-related contaminants and immunogenicity.
Process-related contaminants may include infectious agents (viral, bacterial, fungal, mycoplasma, etc.) with the potential to result in host infection, nucleic acid contaminants with the potential to integrate into the host genome (theoretical), and other contaminants from the manufacturing process such as exogenous nonhuman epitopes (e.g., from animal serum used during the manufacturing process) that can be incorporated into human cells and the resultant bio-therapeutic proteins.
However, current manufacturing technologies, typically including multiple viral inactivation or clearance steps (such as nanofiltration), have largely mitigated this concern and supposedly provide more effective viral clearance than observed in CHO cells. Additionally, the recombinant protein must not immunologically react with the host cell or must not interact with the host cells if used therapeutically.
6.1.3 DNA Delivery and Integration: Transient and Stable Transfection
6.1.3.1 The Methods of DNA Delivery into the Mammalian Cells
In 1973, Graham and van der EB showed that exposing cells to nanoparticles of DNA and calcium phosphate facilitates the DNA transfer into cultivated mammalian cells. Now, viral gene transfer remains the preferred approach to generating stable cell lines for manufacturing purposes. Calcium phosphate transfection, electroporation, lipofection, and biolistic and polymer-mediated gene transfer are routinely used and reasonably efficient and reliable transfection methods (Colosimo et al. 2000; Geisse and Henke 2005).
6.1.3.2 Calcium Phosphate Method
Very briefly the process is as follows: Culture cells in mammalian cell culture grade polystyrene container. Grow the cells within 50–60% confluence. Mix the cells thoroughly with DNA in a phosphate buffer. Thereafter, add the solution of calcium salt, which forms a precipitate. Incubate the calcium-treated mammalian cell culture plate treated with calcium at 37 °C. Cells take up the calcium phosphate crystals including finite proportions of DNA.
6.1.3.3 Liposome-Mediated DNA Delivery
A liposome could be described as a minute spherical sac of phospholipid molecules enclosing a water droplet, especially as one formed artificially, to carry drugs or other substances inside the tissues. Culture cells up to 50–60% confluence. Mix the DNA with lipid to form liposomes, small vesicles having some DNA inside. To gain entry into the cells, the DNA-carrying liposomes fuse with the cell membrane and carry DNA within the cell.
6.1.3.4 Electroporation
Electroporation is a physical transfection method requiring an electrical pulse to create temporary pores in cell membranes through which substances like nucleic acids can pass into cells. Cells grow till 50–60% confluence and then using the electroporator (the machine involved in electroporation) are subjected to electrical shock according to the protocol. It is a highly efficient strategy for the introduction of foreign nucleic acids into many cells, particularly hard to transfect cells because of the thick outer walls such as mycobacteria (M. tuberculosis).
6.1.3.5 Biolistic and Polymer-Mediated Gene Transfer
Gene gun design was invented by John C Sanford, Ed Wolf, and Nelson Allen at Cornell University and by Ted Klein of DuPont, between 1983 and 1986. The original target was onions (chosen for their large cell size), being used to deliver marker gene-coated particles. The method is also called holistic gene transfer, although its first use was for plant cell transformation. However, the technology was later successfully applied in mammalian cells in vitro as well as in vivo. The incumbent gene transfer is accomplished by bombarding target cells with DNA-coated gold particles driven by a pressurized inert gas such as helium or via high-voltage electronic discharge. Efficient gene transfer necessitates fine optimization of the procedure to maintain penetration capacity, alongside minimizing the tissue/cell damage. Among the parameters that impact the gene transfer efficiency include the microsphere’s size and density, bombardment force, gene gun instrumentation, and microspheres to DNA stoichiometry. Typically, these parameters vary with different cells and tissues in animals.
Biolistic gene transfer is advantageous in being fast, simple, and highly efficient. Moreover, the technique is highly suited to deliver a wide range of macromolecules, such as nucleic acids and proteins. It is impossible to assess whether any of the above methods is superior to the others because of the cell-specific suitability and inadequate comprehensive studies.
6.1.3.6 Mode of Transfection: Transient Versus Stable Transfection
The process of transferring naked GOI or recombinant vector into the eukaryotic host cells is called transfection.
Transfection may be of two types:
-
Transient transfection
-
Stable transfection
Ahead is a brief description of each regime:
6.1.3.6.1 Transient Transfection
-
Transfer of naked DNA (DNA without any cell)/plasmid DNA into the cytoplasm not integrated into the mammalian host cell genome using any of the above transfection procedures.
-
With time the DNA/plasmids may be lost from the progeny because the host cell may not able to replicate the transfected DNA.
-
So, the production of recombinant protein may be for small durations (temporary) only.
-
Applicability to a wide range of host cell lines, including various mammalian cells.
-
Intrinsic genetic stability and consistency due to the extremely short time frame between vector generation and product recovery.
-
Suitability to multiple processing, allowing the study of multiple genes or mutants at the same time.
-
Simplicity, in particular for the construction of expression vectors (Liu et al. 2008).
6.1.3.6.2 Stable Transfection
A selectable marker is included in the plasmid vector so that after the cells have been transformed, the rare cell incorporating plasmid DNA into its genome (through DNA repair and recombination enzymes) can be isolated and cloned (because the progeny of the transformed cell will inherit the plasmid DNA including the selectable marker gene, e.g., antibiotic resistance gene).
Thus, the major criteria of stable transfection necessitate a stable integration of GOI into the host genome, becoming part and parcel of the host genome, and thereafter transferring the coded genetic information from generation to generation (as and when the host genome will transfer its genetic information to the next generation). In this case, the site-specific recombination is such that it will not interrupt or jeopardize the GOI expression as well as the drug resistance/other selectable markers.
6.1.3.7 Position Effects of Integrated Gene of Interest into the Host Genome
The site of integration of the GOI has a major effect on the transcription rate of the recombinant gene (a phenomenon known as the position effect). Integration into inactive heterochromatin results in little or no transgene expression, whereas integration into active euchromatin readily allows transgene expression.
However, integration into euchromatin may not be adequate to ensure the long-term expression of the recombinant gene. Transgene expression in mammalian cells is rapidly inactivated (silenced) in many cases, substantially due to the influence of neighboring condensed chromatin. Gene silencing correlates with histone hypoacetylation, lysine of histone H3 methylation, and an increase in CpG methylation within the transgene promoter region.
Several strategies have been demonstrated to overcome the negative position effects of random integration. Protective cis-regulatory elements include insulators, boundary elements, scaffold/matrix attachment regions, ubiquitous chromatin opening elements, and conserved antirepressor elements. Flanking transgenes with these elements reduces the effects of heterochromatin, allowing stable transgene expression. Another option to inhibit silencing is to block the histone deacetylation using butyrate. However, homologous recombination between transfected plasmid DNA and the vector genome rarely occurs.
One way to enhance the probability of targeted integration is via enzymes such as bacteriophage P1 Cre recombinase, lambda phage integrase, or yeast Flp recombinase to mediate the DNA exchange between the genome and transfected plasmid. These enzymes catalyze the exchange at a high frequency if the donor and recipient DNAs are bordered by specific attachment regions. The identification of a highly active transcription site in gene targeting is crucial. If an active site is not found, the receptor site for recombination is inserted randomly, and hundreds of clones are screened for those which have been integrated into so-called good sites (Sambrook et al. 1989).
6.1.4 Selection and Optimization of Positive Clone
Since transfection efficacy is never 100%, it is highly essential to select the positive clones not only having vector but recombinant vector as well, i.e., the vector with GOI. However, in general, for efficient recombinant protein expression, it is not important whether GOI and selector genes are on the same plasmid or not. The recombinant gene and the selector gene can be present on the same vector or distinct vectors. When present on the same vector, they can be expressed using a polycistronic mRNA. To increase the chance of obtaining high-level producer cell lines, the selective gene can be driven by a weak promoter. Although this approach usually reduces the stable transfection efficiency, the cells that survive selection yield greater recombinant products.
The most popular genes for selection are dihydrofolate reductase (DHFR) and glutamine synthetase (GS). In both cases, selection occurs in the absence of appropriate metabolites (hypoxanthine and thymidine with DHFR, glutamine, and with GS, it prevents the growth of non-transformed cells). The transformants are selected using methotrexate strengthening the selection via quenched DHFR activity. This compels the cells to express more DHFR (exogenous) and consequently more recombinant protein for survival. Readers are suggested to refer to Table 3 for different marker proteins in the mammalian cells.
Similarly, most mammalian cells require glutamine. So, using a vector that contains the product gene and the GS gene allowing glutamine synthesis is always better. In such a case, the exclusive cells with the GS gene will survive. It is however necessary to include a weak promoter on the GS gene and a strong promoter on the product gene. Regarding usefulness, GS is widely used for antibody expression in NSO cells (lacking endogenous GS). GS can also be used in CHO cells using methionine sulfoximine to inhibit endogenous GS.
G418 is another important selection gene in eukaryotes, expressing the neo gene. G418 is an aminoglycoside antibiotic produced by Micromonospora rhodorangea. It blocks polypeptide synthesis in eukaryotic cells via irreversible binding to 80S ribosomes and subsequently disrupted proofreading capability. Resistance to G418 is conferred by the neo gene from transposon Tn5, encoding an aminoglycoside 3′-phosphotransferase (APH 3′ II3). This protein inactivates G418 by covalently modifying its amino or hydroxyl functions and concurrent inhibition of antibiotic-ribosome interactions (Sambrook et al. 1989; Zeyda et al. 1999; Wurm 2004).
6.1.5 Selection and Optimization of Cell Culture Medium
Each mammalian cell has its preference for nutrients and growth supplements which are supplemented by the cell culture medium. For small-scale laboratory culture, serum originating from the bovine animals such as fetal bovine serum (FBS) or fetal calf serum (FCS) is an important constituent. The serum not only supplies various nutrients and maintains pH but also optimizes the osmolarity of the medium and thereby the cultured cells. However, since the serum is costly, to reduce the recombinant protein production cost, serum supplements instead of serum are used. The use of serum or serum proteins also increases the chances of viral contamination and other infectious agents such as mycoplasma. Therefore, it is generally recommended to completely avoid serum use, particularly concerning large-scale culture for product commercialization. Thus, it is highly essential to standardize all serum supplementing constituents so that optimum cell growth and culture medium osmolarity could be maintained. Moreover, most mammalian cells (except some leukocytes) are adherent in nature, the culture of which is not only difficult but poses another constraint as the recombinant proteins generated by adherent culture are much lower in quantity. Nevertheless, adherent cells such as CHO cells can be adapted to suspension culture. Here also, standardization of the culture medium and conditions is necessary so that mammalian cells grow without hassles in suspension mode (Almo and Love 2014).
6.1.6 Selection and Optimization of Cultivation Mode in Bioreactor
For producing large quantities of recombinant proteins, various large culture vessels such as bioreactors are used. Once adapted to small-scale culture, a selected high-product (protein) producing clone needs to be adapted well toward suspension-mediated growth in a serum-free medium inside a bioreactor for large-scale production of recombinant proteins. The most common cultivation modes used in bio-manufacturing are fed-batch and perfusion culture. The use of one or the other technology depends on the biochemical requirements of cultured cells concerning the maximum production of the desired protein. Cells are cultivated either attached to carriers or in suspension. HEK-293 and CHO cells are maintained as either suspension or adherent cultures, with the former being particularly favored for their ease of handling and scale-up. HEK-293 and CHO cells in suspension mode typically exhibit a doubling time of fewer than 24 h, growing to higher than five million per ml densities, depending on culture conditions. Therefore, these cells are of immense importance for mammalian recombinant protein production (Huang and McDonald 2009).
6.1.7 Purification of the Expressed Protein
Most of the recombinant proteins isolated from cultured mammalian cells are either secreted proteins or the secretion sequences added to their gene so that they can be secreted into the cell culture medium. So, the first step of purification is the collection of cell culture medium using centrifugation . Since the harvested/collected cell culture medium contains the secreted recombinant protein in a diluted concentration, the generated protein is thereafter concentrated using tangential flow filtration. This decreases the volume and thereby makes it easier to handle followed by purification using multiple methods such as differential centrifugation , filtration , chromatography , etc. Various fusion proteins tagged with the recombinant protein help to identify and purify the latter. These proteins include the constant IgG domain (the Fc region), maltose-binding protein (MBP) , small ubiquitin-like modifier (SUMO) , and human serum albumin (HSA) . All these tagged fusion proteins have been shown to improve either yield or solubility or both for the protein with which these are tagged. The Fc tag does cause artificial dimerization of fused proteins, likely to induce aggregation with certain partners. As many of these tags are large, it is often necessary to remove them after the purification of the fusion protein. The most common solution is to engineer a protease cleavage site between the solubility tag and the partner recombinant protein (Gray 1997; Dalton and Barton 2014).
6.1.8 Quality Control and Quality Assurances
Quality control and quality assurance is the last important step before labeling and packaging recombinant mammalian proteins.
Very briefly here are the steps:
-
The purified recombinant protein can be estimated via UV-visible spectroscopy using various protein concentration determination techniques such as Bradford, Lowry, bicinchoninic acid (BCA), etc.
-
Then, the proteins are biochemically analyzed using SDS-PAGE, Western blot, or ELISA.
-
Thereafter, the protein activity is determined using various assays involving a specific substrate (of the protein).
-
The product must also be checked for possible contamination with a residual live virus (if any at all).
-
After full-scale checking, a generally high concentration of purified recombinant protein is stored at −20 °C in the presence of stabilizing agents such as glycerol or polyethylene glycol (PEG) (Sissolak et al. 2017).
6.2 Major Recombinant Proteins Produced by Mammalian Cell Culture
In this section, we talk about various proteins produced by applying recombinant DNA technology to mammalian cells, including human cells. The tissue plasminogen activator (tPA) is the first protein produced via applying recombinant DNA technology to mammalian cell culture. Other widely used recombinant proteins produced using mammalian cell culture are urokinase, follicle-stimulating hormone (FSH), Epogen (erythropoietin), blood clotting factor VIII, Remicade (infliximab), and several monoclonal antibodies (Khan 2013).
Therefore, several recombinant proteins are produced by mammalian cell culture. Each of these proteins has tremendous importance in today’s human society including in medical science.
Here is a list of some widely used recombinant proteins:
-
1.
Tissue plasminogen activator
-
2.
Urokinase
-
3.
Erythropoietin
-
4.
Follicle-stimulating hormone
-
5.
Blood factor VIII or factor VIII antigen
-
6.
Monoclonal antibodies
The following paragraphs briefly discuss the abovementioned proteins:
6.2.1 Tissue Plasminogen Activator
The first approved biologic from a mammalian bioprocess platform was tissue plasminogen activator (tPA), produced in 1986–1987 by Genentech Inc.
Here is a brief description of tPA.
6.2.1.1 Origin of Tissue Plasminogen Activator
The tissue plasminogen activator (tPA) of human origin exists in a very small quantity in human normal tissues such as blood vessels (e.g., endothelial cells), kidneys, uteri, etc. Recombinant tPA can be produced by transferring a recombinant vector containing the human tPA gene into Escherichia coli, yeast, or mammalian cells as host cells. Of the various mammalian cells, the culture medium of Chinese hamster ovary (CHO) cells is used for the large-scale isolation and purification of medium secreted tPA.
6.2.1.2 Structural Biochemistry of Tissue Plasminogen Activator
It is known that the tPA isolated from the culture medium can be divided into two classes, based on its molecular structure. The original tPA secreted by human melanoma cells has a single chain form, composed of 527 amino acids and some sugar chains. In the culture medium, it is converted into tPA comprising two chains, by the action of a protease within the culture medium. This protease cleaves the peptide bond between the 275th arginine and the 276th isoleucine, counted from the amino terminus of the peptide chain, finally manifesting as a two-chain form tPA, with the two strands being joined together by one disulfide linkage. Therefore, the tPA isolated in the usual method from the culture medium is a mixture of single- and double-chain tPA forms. It is recognized that these two kinds of tPA have a molecular weight of about 69,000 kDa when measured by SDS-polyacrylamide gel electrophoresis under the nonreducing condition. However, under the reducing conditions, it is recognized that single-chain form tPA has a molecular weight of about 69,000, and double-chain tPA has two values, namely, 36,000 and 33,000. The molecule is divided into five structural domains, lasting from the N to C terminus.
These domains are as follows:
-
Looped finger domain
-
A growth factor domain
-
Kringle 1 domain
-
Kringle 2 domain
-
Serine protease domain
The correct folding of tPA requires the right pairing of 17 disulfide bridges in the molecule.
6.2.1.3 Function of Tissue Plasminogen Activator
Tissue plasminogen activator (tPA) is a serine protease involved in blood clot breakdown (fibrinolysis). As an enzyme, it catalyzes the conversion of plasminogen to plasmin. Both looped finger and kringle 2 domains bind specifically to the fibrin clots, thereby accelerating tPA protein activation of bound plasminogen. Next to the kringle 2 domains are the serine protease domain that is responsible for converting plasminogen to plasmin. Plasmin is important for the homeostasis of fibrin formation and clot dissolution.
The fate of tPA within a human body can take the following three roots:
-
Uptake by the liver and cleared through receptors therein.
-
Inhibited by a plasminogen activator inhibitor (PAI) and subsequently cleared from the liver.
-
The activation and plasminogen to plasmin conversion (for degradation) result in fibrin degradation product (FDP) (Fig. 5).
6.2.1.4 Production of Recombinant Tissue Plasminogen Activator Using Chinese Hamster Ovary Cells
The following are the steps for tPA production from the cultured CHO cells:
-
Use antibody-based immunoprecipitation to isolate tPA mRNA from human melanoma cells.
-
The mRNA is converted to cDNA by reverse transcriptase enzyme after which a cDNA library can be constructed.
-
The resulting cDNA library is subsequently screened via sequence analysis and compared to a whole-genome library for confirming specific protein isolation and accuracy.
-
Next, the cDNA is cloned into a synthetic plasmid and initially expressed in prokaryotic bacteria including Gram-negative Escherichia coli cells, followed by yeast cells (e.g., Saccharomyces cerevisiae, a single-cell eukaryote) with successful results confirmed via sequencing before attempting in mammalian CHO cells.
-
The transformants are selected using methotrexate, which strengthens their selection by inhibiting DHFR activity which then compels the cells to express more DHFR (exogenous) and consequently more recombinant protein for survival.
-
The highly active transformants are now placed in a bioreactor for large-scale culture.
-
The tPA which is then secreted into the culture medium is collected.
-
After this, the medium containing tPA is concentrated and purified (for therapeutic use) by various techniques including chromatography.
-
The purified protein is then characterized.
-
Recombinant tPA is commonly referred to as r-tPA and is sold under multiple brand names.
-
For pharmaceutical purposes, tPA is the first pharmaceutical drug produced using mammalian cell culture, specifically CHO cell culture (Bernik and Kwaan 1969; Rijken and Collen 1981; Jones and Garnick 1990; Griffiths and Electricwala 2005).
6.2.1.5 Usefulness of Tissue Plasminogen Activator in Medical Sciences
The thrombolytic agent tPA was the first recombinant protein/drug produced by Genentech in 1988–1987 using the recombinant tPA gene in mammalian cells. Its market name is activase (alteplase). The recombinant thrombolytic tPA is safe and effective for dissolving blood clots in patients with heart diseases and thrombotic disorders. It is used to treat heart attacks, strokes, clots in the lungs, and cancer treatment.
6.2.2 Urokinase
Urokinase, also known as urokinase-type plasminogen activator (uPA), is a serine protease present in humans and other animals. It physiologically acts as a plasminogen-activating proteolytic enzyme and facilitates the dissolution of blood clots.
The following paragraphs describe the urokinase production and characterization:
6.2.2.1 Origin of Urokinase
The human urokinase enzyme was discovered, but not named, by McFarlane and Pilling in 1947. It is a cell-secreted protein and is therefore present in blood and urine. In the human body, urokinase is produced by many tissues and is therefore present in the extracellular matrix (ECM) of those cells and tissues. The human kidneys produce the largest amount of urokinase. It has been reported that the urokinase secreted by kidney cells is antigenically similar to the one isolated from the urine. Since the amount of urokinase in the human urine is very low, the recombinant urokinase is produced on a large scale using the cultured CHO cells or HEK-293 cells.
6.2.2.2 Structural Biochemistry of Urokinase
Urokinase is encoded in humans by the PLAU gene , which stands for “plasminogen activator, urokinase.” Urokinase is synthesized as a zymogen (urokinase or single-chain urokinase) and is activated by proteolytic cleavage between Lys158 and Ile159. The two resulting chains are held together by a disulfide bond. There are two configurations of this enzyme, the one with low molecular weight (LMW, 32,400) and the other being high molecular weight (HMW, 54000) urokinase. The LMW is an autocatalytic fragmentation product of the HMW and both forms are glycoproteins. The LMW form of human urokinase consists of an A chain of 2000 Daltons linked by a sulfhydryl bond to a B chain of 32,400 Daltons. The HMW urokinase is a two-chain glycoprotein containing 411 amino acids with 12 disulfide bonds. Its molecular weight is 54,000 Daltons.
This enzyme consists of the following three domains :
-
Serine protease domain
-
Kringle domain
-
Growth factor domain
6.2.2.3 Functions of Urokinase
Urokinase is a serine protease that activates plasminogen into plasmin by cleaving the Arg-Val linkage in the Pro-Gly-Arg-Val sequence of the former, which in turn degrades the fibrin clots. Thus, the primary physiological substrate of this enzyme is plasminogen, an inactive form (zymogen) of the serine protease plasmin. Activation of plasmin triggers a proteolytic cascade which, depending on the physiological environment, participates in thrombolysis or extracellular matrix degradation. This cascade is involved in vascular diseases and cancer progression.
Hence, urokinase finds its significance as an important anti-thromboembolic drug. The need for urokinase production has increased significantly in recent years, and current production levels have not kept the proportionate pace. Mammalian cells exhibit posttranslational modifications, owing to which mammalian cell lines are nowadays preferred for the production of recombinant urokinase. HEK-293 cells of human origin are a suitable host for recombinant urokinase production because they grow exceptionally well inside the bioreactor.
6.2.2.4 Production of Urokinase Using Human Embryonic Kidney Cell Line
The major source of commercially available urokinase is human urine. However, extremely low urokinase concentrations (10–15 μg/ml) in human urine create a major problem in its isolation and purification. HEK-293 cells, cultured in vitro, are a recognized source of urokinase. These cells are known to secrete biologically active and heavily glycosylated urokinase in the culture medium. Thus, since the amount of secreted urokinase in the human urine is too low, it is produced by culturing mammalian kidney cells such as HEK-293 cells. CHO cells can also be used for preferential greater urokinase production (Barlow 1976; White et al. 1966).
Production of urokinase by mammalian cell culture comprises synthesis, regulation, and secretion. Production and accumulation of this product in a hollow fiber bioreactor is a real challenge for biochemical engineers. All characterized commercial urokinase preparations contain one or both constitutive enzymatically active forms (LMW and HMW) of urokinase. The yields of this enzyme are relatively low. To enhance the urokinase production by these cells, it is required to optimize operational strategies and perform medium standardizations for cell growth and enzyme production. Moreover, urokinase production per unit confluent area and per unit time must be increased. This potential for increased urokinase secretion by the cells is an important consideration for using cell culture-mediated urokinase production. Figure 6 outlines the salient aspects of urokinase production from a human embryonic kidney cell line.
For the separation of urokinase from the human urine, a series of concentration steps followed by conventional chromatographic separations are utilized. In one such reported work, Hou and Zaniewski purified urinary urokinase by an SP cation exchanger followed by a zinc-chelated affinity chromatographic cartridge reporting an 18-fold increase in urokinase-specific activity with nearly 70% yield. For separation and purification of urokinase from different mammalian cells using conditioned cell culture media, multistep chromatographic methods have been reported.
Urokinase production is a product-inhibited (feedback regulated) process. Therefore, in situ urokinase separation is required to operate a bioreactor corresponding to its maximum urokinase formation rate. Structural similarities in the known synthetic substrates and inhibitors of urokinase have enabled the formulation of suitable competitive inhibitors for affinity chromatography ligands such as BAPA (α-benzylsulfonyl-p-amino phenylalanine) , amino benzamidine, homoarginine benzyl ester, or agmatine coupled to a gel matrix. However, these adsorbents do not exhibit specificity to yield highly purified urokinase. Immunoaffinity chromatography offers a powerful approach for the separation of highly pure urokinase from the cell culture broth. However, because of the high costs and low operational stability of the antibody columns, this approach suffers from some limitations. Most of the isolation methods for urokinase use a multistep approach providing lower yields coupled with high capital and increased operating costs, thus resulting in cost and purity issues as the possible limitations in urokinase purification from crude sources.
Thus, the new developments for efficient and cost-effective urokinase separation strategies are highly desired.
6.2.2.5 Usefulness of Urokinase in Medical Sciences
Urokinase is responsible for the dissolution of clots in blood vessels. The urokinase-produced plasmin dissolves the fibrin clots in blood vessels. Perhaps due to this very reason, urokinase is intravenously administered for the treatment of thromboembolic diseases such as pulmonary embolism.
6.2.3 Erythropoietin
Erythropoietin (EPO) is a glycoprotein exclusively produced by the cells of the liver and kidney and some other mammalian body organs. It activates the hematopoietic stem cells (erythroid progenitor cells) within the bone marrow for its proliferation, differentiation, and maturation to erythrocytes or red blood cells (RBCs). One of the most important contributions of erythropoietin is the hemoglobin synthesis (the oxygen/carbon dioxide-carrying metalloprotein) in the RBC.
6.2.3.1 Origin of Erythropoietin
In infants, erythropoietin (EPO) is produced mostly in the liver, but the kidneys become the primary site of EPO synthesis shortly after birth. The adult kidney produces EPO under hypoxic or normoxic conditions in the arterial blood, caused by anemia. Circulating EPO binds to the receptors on the surface of erythroid progenitor cells that in turn mature into RBCs. In the 1970s, human EPO was first isolated and later purified from urine. The gene encoding EPO was cloned and several groups devised recombinant DNA methods for EPO production by the mid-1980s. Amgen Inc. holds a US patent for erythropoietin preparation using recombinant DNA technology in the CHO cell line. The recombinant protein is commercially known as Epogen (Davis and Arakawa 1987; Takeuchi et al. 1989; Egrie 1990).
6.2.3.2 Structural Biochemistry of Erythropoietin
Human EPO is a 30,400 Dalton molecule (30.4 kDa) containing 165 amino acids and four carbohydrate chains that incorporate sialic acid residues. There are several EPO forms, designated by Greek letters that differ only in the carbohydrate content.
6.2.3.3 Functions of Erythropoietin
EPO is a glycoprotein that serves as the primary regulator for the RBCs population in mammals. It stimulates hematopoietic stem cells or more specifically erythroid progenitor cells which differentiate into RBCs, controlling hemoglobin synthesis and red blood cell population.
6.2.3.4 Production of Recombinant Erythropoietin Using Chinese Hamster Ovary Cells
The commercially purified EPO is called Epogen. For EPO production, Chinese hamster ovary (CHO) cells are seeded into roller bottles that are filled to 10–30% extent with medium, and on being slowly rotated, the cells begin to adhere. The rotation assures a regular wetting of the cells and oxygen is supplied by the ample “head space in the bottle.”
After a period of growth and maintenance of the culture at confluence for a few days, the product is harvested from the decanted supernatant culture medium as EPO is a secretory protein. The process can be easily scaled-up and the number of roller bottles handled in parallel determines the scale. The product is concentrated by filtration and purified by chromatographic techniques.
Product recovery is possible within the 50–200 mg/L range, providing protein in the kilogram range, on an annual basis. It is unlikely that such a process would deliver gram/liter product concentrations because the cell-to-volume ratio is much lower than in an optimized stirred-tank reactor process.
Today’s Epogen process is essentially a robot-based manufacturing procedure whereby all the critical handling steps, including cell seeding, filling the bottles with cell culture medium, and harvesting of cell culture fluids/medium, are executed within air-filtered environments without human intervention. This reduces the contamination possibilities.
6.2.3.5 Usefulness of Erythropoietin in Medical Sciences
Recombinant human EPO has been effectively used to treat anemia (in general) or anemia associated with AIDS, renal failure, etc.
6.2.4 Follicle-Stimulating Hormone
Follicle-stimulating hormone (FSH) is a glycoprotein produced by the anterior pituitary gland that stimulates both female and male gonads for their growth and maturation. Gonadal maturation leads to the complete development of reproductive processes which completes the pubertal maturation.
6.2.4.1 Origin of Follicle-Stimulating Hormone
Follicle-stimulating hormone (FSH) is produced by the gonadotropic cells of the anterior pituitary gland of mammals (both male and female). The hypothalamus, the center of the autonomic nervous system, releases a hormone called follicle-stimulating hormone-releasing hormone (FSHRH). In general, FSHRH is also called a gonadotropic hormone-releasing hormone (GnRH) since it stimulates another hormone, luteinizing hormone (LH), to get released from the anterior pituitary. After being released by the hypothalamus, FSHRH reaches the anterior pituitary through the hypothalamic-hypophyseal portal system and stimulates the anterior pituitary to release FSH. Of note, another name for the pituitary is hypophysis. Through the blood, FSH reaches the gonads (ovary/testes) and helps in ovulation (in females) and spermatogenesis (in males). The level of gonadal hormones like estrogens, progesterone, and testosterone is regulated by FSH and LH/ LTH.
6.2.4.2 Structural Biochemistry of Follicle-Stimulating Hormone
FSH is a 35.5 kDa heterodimeric glycoprotein, consisting of an alpha (α) and beta (β) peptides. The α and β chains are encoded by separate genes. FSH structure is similar to those of luteinizing hormone (LH), thyroid-stimulating hormone (TSH), and human chorionic gonadotropin (HCG).
The α-subunits of the glycoproteins LH, TSH, HCG, and FSH are identical and consist of 96 amino acids having five disulfide bonds, while the β-subunits vary from each other. FSH has a β-subunit of 111 amino acids (FSH-β) with six disulfide bonds, which confers its specific biologic action and is responsible for interaction with the FSH receptors. The sugar moiety of the hormone is covalently bonded to asparagine and is composed of N-acetyl galactosamine, mannose, N-acetyl glucosamine, galactose, and sialic acid. Of the four Ans-linked glycosylation sites in FSH, two are located on the α-subunit (Asn 52 and 78), while the other two are on the β-subunit (Asn 07 and 24). Both subunits are required for biological activity.
FSH exists in multiple charged isoforms, and the biological activity, half-life, and immunogenicity of FSH are strongly influenced by the glycosylation pattern throughout the cultivation process. Differences in constitutional carbohydrate moieties can consequently result in significant distinctions for the aforementioned characteristics.
6.2.4.3 Functions of Follicle-Stimulating Hormone
FSH is involved in the following actions:
-
Stimulating the maturation of primordial germ cells and thereby regulating the development, growth, pubertal maturation, and reproductive processes of the human body (Fig. 7).
-
In males, FSH induces Sertoli cells to secrete androgen-binding proteins (ABPs), regulated via inhibiting negative feedback mechanism on the anterior pituitary gland. Specifically, activation of Sertoli cells by FSH sustains spermatogenesis and stimulates inhibin B secretion.
-
In females FSH initiates follicular growth, specifically affecting granulosa cells within the ovary. With the concomitant rise in inhibin B, FSH levels subsequently decline in the late follicular phase. This seems to be critical in selecting only the most advanced Graafian follicle to proceed to ovulation. Of note, ovulation is the process in which mature ovum is released from the ruptured Graafian follicle, and subsequently, the empty, ruptured Graafian follicle is converted to corpus luteum. At the end of the luteal phase, there is a slight rise in FSH, which is significant to start the next ovulatory cycle.
-
Experimentally in rats, low-frequency gonadotropin-releasing hormone (GnRH) pulses increase FSH mRNA but are not directly correlated with the increment in circulating FSH. GnRH has been shown to play an important role in FSH secretion, with hypothalamic-pituitary disconnection leading to its cessation. GnRH administration leads to a return of FSH secretion.
-
FSH is subject to estrogenic feedback from the gonads via the hypothalamic-pituitary-gonadal axis.
6.2.4.4 Production of Recombinant Follicle-Stimulating Hormone Using Chinese Hamster Ovary Cells
The FSH present in the human urine (uFSH) is much diluted and therefore very difficult to purify. Many groups have prepared and described the actions of human recombinant FSH (rFSH) produced by transfected CHO cells. Recombinant rat FSH production by CHO cells with subsequent purification and functional characterization was also reported. Cloning and expression of cynomolgus monkey (Macaca fascicularis), gonadotropins, luteinizing hormone, and FSH were also described.
The specific activity of rFSH is estimated at 10,000 IU/mg extent, nearly a hundred folds greater than uFSH. The most obvious advantages of rFSH include greater purity and specificity. It has been inferred that smaller doses and a more predictable response will result in much reduced (potentially serious) ovarian hyper-stimulation syndrome. The most dramatic disadvantage to the health provider and patient, however, is a marked increase in the product price.
Similar to most recombinant proteins, the production of recombinant human FSH (r-hFSH) generally follows a well-established development process involving (i) transfection of cultivated mammalian cells (e.g., CHO cells) with the human FSH gene (α-FSH and β-FSH), (ii) clonal selection and isolation of produced cell line, (iii) cell banking to supply cell substrates from the selected clone for unobstructed product manufacture, and (iv) large-scale production, involving bioreactor and purification. The development of the manufacturing process starts with pilot batches for process optimization before validation and industrial-scale production in full-scale batches with reproducible quality.
Due to their easy growth and survival adaptability in suspension culture, CHO cells are considered capable of reaching high cell densities. CHO-based processes can easily be up-scaled to more than 10,000 L bioreactors, followed by downstream processing (Howles 1996; Hakola et al. 1997).
6.2.4.5 Usefulness of Follicle-Stimulating Hormone in Medical Sciences
The utility prospects of FSH in medical sciences are as detailed ahead:
-
Infertility Therapy
-
FSH is used commonly in infertility therapy , mainly for ovarian hyper-stimulation as part of IVF.
-
-
Anovulation Therapy
-
It can be used squarely well for ovulation induction and anovulation reversal. FSH is available as mixed with LH activity in various menotropins including more purified forms of urinary gonadotropins such as Menopur as well as without LH activity, as recombinant FSH (Gonapure, Gonal-F, Follistim, Follitropin alpha).
-
-
Studying the Structure and Functions of Glycoprotein Hormones
-
FSH is used for studying the structure and functions of glycoprotein hormones, via the creation of a genomic library in the CHO cells through cloning DHFR gene expression (Fig. 8). Since these are free from contaminating hormones, their structure and function can be studied extensively because of their substantial availability. FSH also helps to understand estrogen feedback mechanisms.
-
6.2.5 Blood Coagulation Factor VIII
Blood coagulation factor VIII (FVIII) is a glycoprotein in the mammalian blood coagulation cascade, the deficiency of which may lead to hemophilia A, a pathophysiological or disease condition. Hemophilia A is characterized by profuse bleeding with slow or no blood coagulation following an injury to the blood vessels. Defects in the FVIII gene result in hemophilia A, a recessive X-linked coagulation disorder having a prevalence of 1 in 5,000 males.
6.2.5.1 Origin of Blood Coagulation Factor VIII
Factor VIII is produced by the endothelial cells in the blood vessels throughout the body and by the liver sinusoidal cells. The protein is secreted in the blood and binds with von Willebrand factor, another protein released by vascular endothelial cells. This binding form of factor VIII remains inactive until an injury to the blood vessels separates the von Willebrand factor from it. The active coagulation factor VIII interacts with another coagulation factor, called factor IX. This interaction sets off a chain of additional chemical reactions to collectively form a blood clot. Thus, factor VIII acts as a nonenzymatic cofactor for blood coagulation.
6.2.5.2 Structural Biochemistry of Blood Coagulation Factor VIII
The secretary protein factor VIII is synthesized as a 2351-amino acid residue single-chain precursor. This chain is thereafter translocated to the endoplasmic reticulum (ER) where a 19-residue signal peptide is cleaved. The precursor protein is proteolytically processed to generate a 90 to 200 kDa sized amino-terminal-derived heavy chain and an 80 kDa, carboxyl-terminal-derived light chain. It is unknown whether this cleavage occurs intracellularly or in the plasma. In plasma, factor VIII exists as a metal ion complex of a 200 kDa heavy chain and an 80 kDa light chain doublet. This complex is non-covalently bound to the von Willebrand factor in 1:100 ratios.
The final mature factor VIII is composed of three domains, occurring in the order of A1-A2-B-A3-C1-C2: The A domain occurs twice in the heavy chain and once in the light chain and has homology to ceruloplasmin, a copper-binding plasma protein, a single B domain, and two C domains in the light chain having homology to phospholipid-binding proteins. The protein contains 25 potential N-linked glycosylation sites, 19 of which are in the B domain. The B domain is proteolytically released upon activation by thrombin or factor Xa and is not required for in vitro or in vivo pro-coagulation (Gitschier et al. 1984). Figure 9 summarizes the characteristic structural traits of blood coagulation factor VIII for an easier experimental follow-up.
6.2.5.3 Functions of Blood Coagulation Factor VIII
Blood coagulation factor VIII is produced in liver sinusoidal cells and endothelial cells in the blood vessels throughout the body. This protein circulates in the bloodstream in an inactive form, bound to another molecule called von Willebrand factor, until an injury damaging blood vessels occurs. Factor VIII activates FIXa, FX, and Ca++ on the membrane surface and causes blood coagulation.
Blood coagulation factor VIII is proteolytically activated by thrombin, resulting from cleavage of the heavy chain in Arg372 (A1-A2 domain linkage) and Arg740 (A2-B domain linkage) amino acid sites and of the light chain in Arg1689 (B-A3 domain linkage) site. The active form of coagulation factor VIII, FVIIIa, is a trimer consisting of A1 (amino acids 1–372), A2 (amino acids 373–740), and linked A3-C1-C2 (amino acids 1690–2332) domains. The B domain does not comprise the active form of coagulation factor VIII. The function of FVIIIa in the coagulation cascade is to accelerate FX activation in the presence of FIXa, phospholipids, and calcium ions.
6.2.5.4 Production of Recombinant Blood Coagulation Factor VIII by Using Chinese Hamster Ovary Cells or Baby Hamster Kidney Cells
Owing to its large size and complexity, the expression level of recombinant FVIII is two to three orders of magnitude lower than other recombinant proteins produced in mammalian cell lines. Thus, despite the knowledge acquired over more than 25–30 years of industrial production, efficient production of recombinant coagulation factors remains a challenge for the industry, which is striving hard to improve the manufacturing operations for a timid and cost-effective treatment of patients. Currently, at least 12 recombinant FVIII and five recombinant FIX products are available in the market.
The traditional source of FVIII has donated blood plasma, which is in short supply and poses a significant risk of virus and prion transmission, even after rigorous (batch-wise) screening and multiple viral inactivation treatments. Recombinant human FVIII (rhFVIII) for hemophilia A treatment may be obtained from cultured mammalian cells purified to clinical grade using affinity chromatography, three or four rounds of conventional chromatography, solvent-detergent-mediated viral inactivation, and nanofiltration or heating. Marketed variants of r-hFVIII are expressed in CHO or BHK cells and are fully equivalent to the plasma-derived FVIII in replacement therapy.
The major drawback of r-hFVIII production techniques is the FVIII low expression extent, caused by the unusual size and structural complexity of the target protein (Andersson et al. 1986; Campos-da-Paz et al. 2008; Fantacini and Picanço-Castro 2018).
6.2.5.5 Recombinant Blood Coagulation Factor VIII Products
Several generations of blood coagulation factor VIII products are presently available on the market.
Here is the discussion on some of them:
-
The First-Generation Products
-
The first recombinant coagulation factor VIII was launched in 1992 by Genetics Institute and Baxter Healthcare Corporation, Hyland Division. Kogenate, made by Bayer Healthcare Pharmaceuticals, was launched a few months later, in 1993. Both entities were developed using animal-derived proteins in the cell culture medium, having human serum albumin in the final formulation, being considered first-generation products.
-
-
The Second-Generation Products
-
The risk of exposure to transmissible agents (non-enveloped viruses, hepatitis A and parvovirus B19, Creutzfeldt-Jakob agent and its variant or yet unknown agents) has led to the development of the second-generation products, having the culture medium supplemented with human-derived proteins instead of animal-derived proteins (fetal bovine serum), wherein no albumin was added to the final formulation. In this case, new technologies were used to stabilize the FVIII, with sucrose and trehalose, for example.
-
-
The Third-Generation Products
-
The third-generation products involve those in which no animal or human proteins for cell cultivation and purification are used. Some studies have shown that patients treated with second-generation rFVIII products harbor a higher risk of inhibitor development compared to those administered third-generation products. FVIII inhibitor is an immunoglobulin G (IgG) produced by the patient having a high polyclonal affinity directed against the FVIII protein. Inhibitory antibodies are directed usually against the A2, A3, and C2 FVIII domains. The binding of an inhibitor in these domains results in a steric blockade of the FVIII functional epitopes.
-
6.2.5.6 Usefulness of Blood Coagulation Factor VIII in Medical Sciences
Hemophilia A is a blood disorder, prevailing as a sex-linked genetic disease in humans. The patients suffering from hemophilia A lack factor VIII which plays an important role in blood clotting. Current therapy for this disease involves the transfusion of blood factor VIII into patients.
6.2.6 Recombinant Monoclonal Antibodies
Immunoglobulins (Ig) or antibodies (Ab) are specific glycoproteins produced by the B lymphocytes and are involved in humoral immunity. An antibody carries out a dual role and is intrinsic in its structure. One Ab has two active sites, called fragment antigen-binding (Fab), that have the ability of independent binding with the two active sites of an antigen (Ag) called an epitope. An antibody also can induce an immune response. Based on the affinity of binding with the active site of an antigen (called epitopes), antibodies are classified either as polyclonal or monoclonal (mAbs). While a polyclonal antibody recognizes and binds more than one epitope on the Ag, the monoclonal Abs recognize and bind only one or single epitope (Trill et al. 1995; Andersen and Reilly 2004; Li et al. 2010; Chartrain, 2008; Rita Costa, 2010).
6.2.6.1 Production of Recombinant Monoclonal Antibodies in Mammalian Host Cells
The following are the steps involved in the production of recombinant antibodies in mammalian cells:
6.2.6.1.1 Construction of Antibody-Coding Vectors
An antibody is a complex protein comprising two identical heavy chains (HCs) and two identical light polypeptide chains (LCs). The sequences of both heavy and light chains can be commercially synthesized (e.g., by GenScript, Piscataway, NJ, USA). Each of the antibody chains should be cloned into separate expression vectors under the control of the same human cytomegalovirus (CMV) immediate-early enhancer and promoter. The cloned sequences are subsequently confirmed by DNA sequencing.
6.2.6.1.2 Co-Expression of Light and Heavy Chain Genes
Based on the heavy chain, antibodies are divided into five different classes. They are IgG (two identical γ heavy chains), IgA (two identical α heavy chains), IgM (two identical μ heavy chains), IgE (two identical lε heavy chains), and IgD (two identical δ heavy chains).
Complex interactions occur between light and heavy chains during the folding and assembly of an IgG mAb [most abundant (~80% of Ab) and smallest Ab in the human plasma]. The light chain/heavy chain peptide ratio plays an important role in the kinetics of mAb formation. The excess light chain is reported to be beneficial for higher mAb expression levels. There are also reports that light to heavy chain ratios above 1.5 result in minimal product aggregation extents. As light chain/heavy chain ratio could affect mAb assembly, it is suggested that mAb glycosylation could also vary with changing light to heavy chain proportions. It is of prime interest to mediate these mAb subunit expressions at the optimal stoichiometric ratio for a higher mAb production.
A light chain and heavy chain genes are traditionally introduced by co-transfecting on two separate vectors or via transfecting a single larger vector carrying all the required genes. Light and heavy chain peptide ratios can be varied under transient conditions while co-transfecting the genes on separate vectors by changing the relative extents of each plasmid. Controlling the ratio by this method, the transfection is usually not stable owing to a random integration process with randomly assorted gene copies and an uncontrolled site of integration. Single vectors provide better control of the ratio as these enable the integration of all genes at the same site. One possible issue that could arise with having multiple promoters nearby is the resulting transcriptional interference. This interference suppresses gene expression to varying extents depending on the site of integration. Choosing single-promoter and single-vector systems for expressing light and heavy chains have a stricter control on their mutual stoichiometries. One such system uses internal ribosome entry site (IRES) elements to express light and heavy chains.
6.2.6.1.3 Using Mammalian Cells for Recombinant Monoclonal Antibody Production
Mammalian cells are currently the main hosts for the commercial production of therapeutic proteins, including mAbs. African green monkey kidney (COS) cells may be appropriate if the aim is to produce mAbs in small-scale quantities, for preliminary investigation. Indeed, they have been used for transient expression of active antibodies since 1987. However, they are not the most suitable cells for large-scale production, since they lose the production ability over time. If the aim is large-scale production, the most suited cells are the CHO cells, which have gathered increasing laboratory-scale importance. Other mammalian cells in use for mAbs production are murine lymphoid cells (NS0, SP2/0), human cells such as human embryonic kidney (HEK) cells, and PER.C6 cells.
6.2.6.1.4 Transfection and Generation of Stable Cell Lines
Transfection is carried out in duplicate in 6-well tissue culture plates. For each well, 2 × 106 cells are seeded and transfected with 3 μg linearized plasmid DNA, using X-tremeGENE/HD reagent (Roche, Basel, Switzerland) according to the manufacturer’s instructions.
To generate stable cell lines, CHO cells can be first transfected with LC-expressing vectors (PL or PUL) and selected with G418 (400 μg/ml) (Sigma-Aldrich). Then the resulting LC-expressing stable cells can be transfected with HC-expressing vectors (PH or PUH) before being selected with zeocin (500 μg/ml), 72 h post-transfection over 14 days. Stable cell lines could be generated using different antibody vector combinations: (1) CHO-HL transfected with PH and PL vectors and (2) CHO-UHUL transfected with PUH and PUL vectors.
6.2.6.1.5 Culture of Mammalian Cells
The selection of an expression system (cells along with suitable genetic materials) is determined by the host’s capability to deliver high productivity with suitable product quality attributes. Guidelines on cell engineering for mAbs production are also reported previously. Using heterologous promoters, enhancers, and amplifiable genetic markers, the yields of antibody and antibody fragments could be enhanced.
In the development of all pharmaceutical production processes, including those of human Abs by CHO cells, decisions regarding the optimum process parameters and methods are made based on cost, time, and titer comparisons. Often, multiple scalable platforms are examined before a final process is transferred to pilot- or scale-up laboratories. Significant research and development time and capital are invested to increase yields, reduce costs, and improve the current bioreactor and bioprocess technologies.
In the batch method, all nutrients are supplied in an initial base medium. The fed-batch method adds nutrients once they are depleted. The perfusion method circulates the medium through a growing culture, allowing simultaneous removal of waste, the addition of nutrients, and product harvesting.
The application of single-use equipment is on the rise in bioprocess development owing to the reduced turn-around times and cross-contamination risks. Adding an ATF filtration device and using a solid growth-support matrix in a packed-bed vessel allow for simple cell retention with higher cell and product yields. Much greater productivity can be achieved through prolonged perfusion culture with up to 2 or 3 months of continuous antibody harvesting after the initial inoculation.
6.2.6.2 Downstream Processing of Antibodies
The cultured cells secrete Ab into the cell culture medium after which the culture medium is purified. Cell culture sample constitutes primarily the medium components such as growth factors, hormones, transferrin, secreted cytokines, etc. There may also be bacterial contamination contributing to bacterial endotoxins.
The mAb from the cell culture medium could be purified using the following steps:
6.2.6.2.1 Centrifugation and Filtration
The cell debris, lipids, and clotted materials are removed firstly by centrifugation and thereafter by filtration, using a 0.45 μm filter.
6.2.6.2.2 Ultrafiltration and Dialysis
After the removal of cell debris and clotted residual cell materials, the sample is concentrated using ultrafiltration or dialysis.
6.2.6.2.3 Purification of the Sample
Most of the charged impurities are usually anions such as nucleic acids and endotoxins. These can be separated using ion-exchange chromatography. The cation-exchange chromatography is used at a low enough pH over which the desired antibody binds to the column while anions flow through. Contrary to this, the anion-exchange chromatography is used at a high enough pH over which the desired antibody flows through the column while anions bind to it. Various proteins can also be separated along with the anions based on their isoelectric point (pI, pH(I), IEP). In proteins, the pI is defined as the pH, corresponding to which no charge prevails.
Large-scale mAbs purification is based on various chromatographic techniques. Protein affinity purification is used in the majority of cases in combination with at least one ion-exchange step. It is common to include at least one and sometimes more polishing steps using ion exchange, hydrophobic interaction, and/or size exclusion chromatography for Abs purification. The steps are designed to remove contaminant proteins from cells or medium (to ppm levels) and DNA (to ppb extents). Depending on the process, there may be additional specific contaminants (e.g., leached protein A) that need to be removed. In addition to contaminants, it may also be necessary to remove several undesirable derivatives of the product itself such as degradation products and aggregates.
For mammalian cell processes, one also has to take account of potential viral risks while establishing the ability of the purification pattern(s) capable of removing a range of viruses. In addition, at least two viral removal/inactivation steps are included, typically based on filtration and low pH treatment and sometimes, involving the use of solvent/detergent.
Typical yields from an antibody purification process are within the 60–80% range, depending on the number of steps. With increasing upstream concentrations, increasing attention is being paid to downstream recovery as this account for a significant proportion of the total cost and can also limit the overall plant throughput.
6.2.6.2.4 Antibody Quantification
Recombinant mAb concentration was measured using sandwich ELISA where the antibody could be characterized using Western blotting.
6.2.6.3 Usefulness of Recombinant Monoclonal Antibodies
The mAbs were first described nearly 50 years ago, by the Nobel Laureates, Kohler and Milstein. Over the years, mAbs have become invaluable assets in all spheres of our life. The mAbs are now the second-largest category of biopharmaceutical products in development and are predominantly manufactured by being cultured mammalian cells.
The following are the major area of mAbs usefulness:
-
Use of monoclonal antibodies in basic laboratory research
-
Use of monoclonal antibodies in diagnostic technologies
-
Use of monoclonal antibodies as therapeutic tools
Overleaf is the brief presentation of each of the above.
6.2.6.3.1 Use of Monoclonal Antibodies in Basic Laboratory Research
Monoclonal antibodies (mAbs) are widely used in basic laboratory techniques such as serotyping, characterization of antigens/antibodies by immunoprecipitation/immunodiffusion, immunohistochemistry, immunocytochemistry, flow cytometry, Western blotting, ELISA, and related techniques.
Radioimmunoassay; gel shift assay and gel and super-shift assay; confocal/ fluorescent microscopy for detection, localization, and quantification of specific proteins/antigens; and a large number of other assays are also based on the specific binding proximity of mAbs. In these techniques, the specific mAbs bind with the specific epitope present on the Ag (the sample) and subsequently help in localization detection, quantification, and characterization of Ags/mAbs interaction.
Thus, in today’s world of immunology/cell biology/biochemistry/molecular biology/protein engineering, mAbs are one of the basic functional probes.
6.2.6.3.2 Use of Monoclonal Antibodies in Diagnostic Technologies
Monoclonal antibodies have several utilities in diagnostic technology, for example, detection of the insulin level in the blood of healthy or diabetic subjects via radioimmunoassay, detection of disease-causing agents such as HIV in the blood (using ELISA), pregnancy test (through the urine of pregnant women: ascertaining HCG presence) using anti-HCG antibody, and so on.
The immunodiagnosis of protozoal and parasitic diseases has been significantly improved by mAb technology because the tests involving mAb as diagnostic reagents overcome the limitations of polyclonal antibodies. MAbs were found extremely useful in containing the rapid outbreak of East Coast fever (ECF). MAbs of diagnostic value have also been developed against Trichomonas vaginalis, Leishmania donovani, Trypanosoma congolense, Babesia bovis, and many other diseases that are diagnosed today using specific mAbs.
6.2.6.3.3 Use of Monoclonal Antibodies as Therapeutic Tools
The use of mAbs in the treatment of various diseases (enclosed as under) is as described.
In the last 30–40 years, mAbs are predicted as useful against various cancers, chronic inflammatory diseases, and chronic infections (such as mAbs anti-HIV have shown promising results in human HIV therapy). These agents are also effective against transplantation rejection, ankylosing spondylitis, allergy, Crohn’s disease, psoriasis, ulcerative colitis, and rheumatoid arthritis. The interest in this class of mAbs has increased over the years including manifold enhancement in the specific research.
Some FDA-approved antibodies used for the treatment of various cancers are alemtuzumab, bevacizumab, cetuximab, gemtuzumab ozogamicin, ipilimumab, ofatumumab, panitumumab, pembrolizumab, ranibizumab, rituximab, and trastuzumab. mAbs used against autoimmune diseases include infliximab and adalimumab and are also screened effectively in rheumatoid arthritis, Crohn’s disease, ulcerative colitis, and ankylosing spondylitis through their ability to bind and inhibit TNFα, a pro-inflammatory cytokine. Basiliximab and daclizumab inhibit pro-inflammatory cytokine IL-2 on activated T cells and thereby help in preventing acute rejection of kidney transplants. Similarly, omalizumab inhibits human immunoglobulin E (IgE) and is useful in treating moderate-to-severe allergic asthma.
The commercial development of therapeutic mAbs commenced in the early 1980s, and by 1986 the first therapeutic mAb was produced. This mAb was named ortho-clone (OKT3) and was approved for use in preventing kidney transplant rejection. Since the OKT3 approval, therapeutic mAbs and antibody-related products such as Fc-fusion proteins, antibody fragments, and antibody-drug conjugates (collectively referred to as monoclonal antibody products) have emerged as the dominant product class within the biopharmaceutical market. Recombinant mAbs fulfill a large spectrum of functions spanning from research to diagnosis and treatment therapies for various diseases. Their specificity and low immunogenicity make them a significant alternative to traditional treatment regimes, increasing the accuracy of targeting specific molecules and minimizing the adverse side effects.
Recombinant antibodies have been explored as treatment agents against cancer, HIV, herpes simplex virus (HSV), and several other critical disorders. ScFv has been a part of the highly promising therapeutic approach of universal chimeric antigen receptor (uniCAR) technology, enabling authentic corrective results. The ScFv is part of the technology in the form of target modules, directing the immune response to specific cancer cells expressing the target antigen. In the case of research into HIV treatment, recombinant antibodies are rather used for their neutralizing attributes. The same holds for HSV infection wherein specific recombinant antibodies are being designed to bind with the surface heparin sulfate proteoglycan (HSP), complicating or even disabling the HSV entry into the host cell. This is a method that significantly decreases the severity of HSV infection.
6.2.6.4 Major Limiting Factors toward the Clinical Applications of Monoclonal Antibodies
Potential limiting factors toward the advancing clinical applications of mAbs include the followings:
-
Immunogenicity
-
Difficulty and cost of production on an adequate scale
-
Unwanted biological activity due, for example, to direct effects on the cells of the immune system
-
Limited binding affinity, which necessitates the injection of large antibody quantities to achieve a therapeutic effect
-
Lack of direct functional action, requiring conjugation of drugs or other biologically active materials
-
Limited penetration into the target tissue, especially dense, poorly vascularized tumor tissue
6.2.6.5 Overcoming the Limitations of Monoclonal Antibody
-
Antibody engineering is the best option for overcoming the limitation of mAbs usefulness. Here are some way-outs through which we can overcome the shortcomings of mAbs applicability:
-
Preparation from existing hybridoma genes or genes encoding for small proteins, which include the antigen-binding site but omit most of the remaining molecules including sequences responsible for the biological effects of antibodies.
-
Modification to increase antigen-binding affinity (affinity maturation).
-
Preparation of fusion proteins consisting of the antigen-binding site linked directly to, for example, a toxin, an enzyme, or a sequence suitable for radioisotope labeling another antibody sequence, to achieve increased or novel biological activities.
-
Modification to make the sequence more humanlike and less immunogenic.
-
Generation of gene libraries through derivation from human antibody genes. This avoids the immunogenicity associated with foreign protein.
-
Genetic modification of mice so that they produce human antibodies followed by immunizing and hybridoma preparation in a classical way.
-
Preparation of antibody fragments in bacterial culture for increased yield.
7 Mammalian Cell Culture in Cell Therapy
Cell therapy involves the delivery of living cells to a patient for the treatment of various diseases. This technique relies on the use of technologies that minimize the risk of contamination and achieve the strictly controlled, secure environment necessary for growing healthy, viable cells.
The most common cell therapy is blood transfusion involving the transfusion of red blood cells, white blood cells, and platelets from a donor. Another common cell therapy is the transplantation of hematopoietic stem cells to create the bone marrow which has been performed for over 40 years.
While there is no formal classification of cell therapy based on the origin, the process may be called autologous or allogenic (cell therapy). The cells used in cell therapy can be classified by their potential to transform into different cell types. For instance, pluripotent cells can transform into any cell in the body and multipotent cells can transform into other cells, but their repertoire is more limited than pluripotent cells. Differentiated or primary cells are of a fixed type (Fischbach et al. 2013).
The following paragraphs chronologically describe autologous and allogeneic cell therapy and then various stem cells used for cell therapy:
7.1 Autologous Cell Therapy
In this process, the cells are derived from the patient and modified in the laboratory (usually genetically) before being re-administered back to the patient. Since the cells originated from the recipient’s own body, there will be no chances of rejection. The patient-specific nature of autologous cell therapies can make large-scale production extremely challenging because a separate batch needs to be produced for each patient. Companies often struggle to scale up manufacturing as a necessary practice, in clinically and commercially viable ways.
In 1997, the US Food and Drug Administration (FDA) approved a product consisting of autologous cultured chondrocytes (Carticel, Genzyme Biosurgery). Derived from the in vitro culture of a patient’s normal femoral articular cartilage, this product showed clinical benefits in developing hyaline cartilage that is lost in the event of acute or recurring trauma. However, adverse reactions, most commonly hypertrophic tissue development, have been reported in both intra- and postoperative circumstances.
7.2 Allogeneic Cell Therapy
In this process, the cells are derived from another individual and reveal a certain resemblance with the potential new host, similar to blood transfusion. Some companies are exploring the use of allogeneic cell therapies, deriving treatments or doses for multiple patients from the cells of a single donor. Since single donor cells are administered to several patients, manufacturing may be efficient and cost-saving.
However, the use of cell therapies (cells derived from one donor and administered to a different recipient) involves a greater risk of immune rejection. As a consequence, cells for allogeneic therapies must be extensively cultured and cryopreserved for long-term storage. This prolonged culture increases the risk of cell transformation (e.g., tumorigenicity), and often the frozen product requires further manipulation before administration.
7.2.1 Basic Reasons for Cell Therapy
Cell therapy involves the transfer of cells having a relevant function into a patient.
Cell therapy is adopted in the following conditions:
-
1.
Diseases that are caused by a gene mutation
-
2.
Diseases that are resistant to conventional therapy for which there is no effective treatment
-
3.
Cases where current therapy involves long-term administration of an expensive therapeutic agent or an invasive procedure
Many non-communicable human diseases such as cancers, rheumatoid arthritis, diabetes, Parkinson’s disease, Alzheimer’s disease, etc. can be treated by cell therapy or gene therapy. Present-day cancer cell therapy focuses on eliminating the cancer cells, blocking tumor vascularization, and boosting the immune response to tumor antigens.
The following paragraphs describe the cell therapy procedure and various cells being used for cell therapy:
7.2.2 Cells Utilized in Cell Therapy
In general, various stem cells are used for cell therapy. Since a separate chapter (Chap. 12) is dedicated to stem cell culture, here we briefly discuss various stem cells.
Embryonic stem cells
Induced pluripotent stem cells
Nuclear transfer of embryonic cells
Parthenogenetic embryonic stem cells
Hematopoietic stem cells
Mesenchymal stem cells
Neural stem cells
Epithelial stem cells
Immune cell therapy
Here is a very brief discussion of various stem cells utilized in cell therapy:
7.2.2.1 Embryonic Stem Cells
Embryonic stem cells (ESCs) are derived from embryos. Generally, the embryos used to isolate stem cells are unused embryos generated from in vitro fertilization (IVF) for assisted reproduction. As ESCs are pluripotent, they retain the ability to self-renew and form any cell in the body. ESCs have the advantage of versatility due to their pluripotency, but the use of embryos in the development of therapeutic strategies raises some ethical concerns. In addition, stem cell lines generated from embryos are not genetically matched to the patient, owing to which there is an increased likelihood of transplanted cell rejection by the patient’s immune system.
7.2.2.2 Induced Pluripotent Stem Cells
Induced pluripotent stem cell (IPSC) is a differentiated adult (somatic) cell, such as a skin cell, and is reprogrammed to return to a pluripotent state. These cells offer the advantage of pluripotency. IPSCs may be derived from a patient and thus avoid the problem of immune rejection. IPSCs are produced by transforming the adult cell with a cocktail of genes usually delivered via a viral vector. While the efficiency of the process has been greatly improved since its inception, the relatively low rate of reprogramming remains a concern. Another concern is that IPSCs are derived from adult cells and are, therefore, “older” than ESCs as evidenced by enhanced programmed cell death, lower rate of DNA damage repair, and increased incidence of point mutations.
7.2.2.3 Nuclear Transfer of Embryonic Cells
Nuclear transferred embryonic stem cells (ntESCs) are pluripotent cells produced by transferring the nucleus from an adult cell obtained from a patient to an oocyte obtained from a donor. The process of transferring the nucleus reprograms the egg cell to pluripotency. As with iPSCs, the derived cells match the nuclear genome of the patient and are unlikely to be rejected by the body. However, the major advantage of this technique is that the resulting ntESCs carry the nuclear DNA of the patient alongside mitochondria from the donor, making this technique particularly appropriate for diseases where the mitochondria are damaged or dysfunctional. A drawback of ntESCs is the cumbersome generation process, requiring a donor oocyte. This technique has only been successful in lower mammals and for higher animals, including wherever human research is going on.
7.2.2.4 Pathogenetic Embryonic Stem Cells
For the production of parthenogenetic embryonic stem cells (pES) , the oocyte is treated with chemicals that induce embryo generation without the addition of sperm (parthenogenesis), and ESCs are harvested from the developing embryo. This technique generates ESCs that are genetically identical to the female patient. However, this method is in the early stages of development, and it is not yet known if cells and tissues derived from parthenogenesis are capable of normal development.
7.2.2.5 Hematopoietic Stem Cells
Hematopoietic stem cells (HSCs) are multipotent blood stem cells that give rise to all types of blood cells. HSCs can be found in adult bone marrow, peripheral blood, and umbilical cord.
7.2.2.6 Mesenchymal Stem Cells
Mesenchymal stem cells (MSCs) are multipotent cells present in multiple tissues including the umbilical cord, bone marrow, and fat tissue. MSCs give rise to bone, cartilage, muscle, and adipocytes (fat cells) which promote the marrow adipose tissue.
7.2.2.7 Neural Stem Cells
Adult neural stem cells (NSCs) are present in small numbers within defined regions of the mammalian brain. These multipotent cells replenish neurons and supporting cells of the brain. However, adult neural stem cells cannot be obtained from patients due to their residing in the brain. Therefore, neural stem cells used for cell therapies are obtained from iPSCs or ESCs.
7.2.2.8 Epithelial Stem Cells
Epithelial stem cells (EpSCs) are those which form the surfaces and linings of the body including the epidermis and the gastrointestinal tract lining. Multipotent epithelial stem cells are found in these areas along with unipolar stem cells that only differentiate into one kind of cells. Epithelial stem cells have been successfully used to regenerate the corneal epithelium.
7.2.2.9 Immune Cell Therapy
Cells that rapidly reproduce in the body such as immune cells, other blood cells, or skin cells can usually do so ex vivo given the right conditions. This allows differentiated, adult immune cells to be used for cell therapy. These cells can be removed from the body, isolated from a mixed cell population, modified, and then expanded before being reintroduced into the body. A recently developed cell therapy involves the transfer of adult self-renewing T lymphocytes that are genetically modified to augment their immune potency. Various other immunological cells such as dendritic cells, cytotoxic T cells, etc. can also be isolated from the cancer patients before being cultured in the laboratory and thereafter, injected (adoptive transfer) into the same cancer patient to increase the potential immunity and destruct the cancer cells.
7.2.3 Phases of Cell Therapy
Cell therapy can be described as the following four phases:
-
Discovery
-
Process optimization
-
Production
-
Therapeutic delivery
Here is a brief presentation of the above phases:
7.2.3.1 Discovery
In this phase, the major working domain involves new product characterization. Functional assays and cellular and molecular profiling are useful tools for this phase.
7.2.3.2 Process Optimization
The process optimization stage involves quantifying the relationship between culture parameters and cell output. The rational design of experiments and high-throughput screening using micro-culture platforms can be used to generate empirical cell-based models, which can be thereafter integrated with molecular profiling technologies to develop more mechanistic, molecular-based models.
7.2.3.3 Production
Considerations in the production phase include the scale-up strategy and quality control.
7.2.3.4 Therapeutic Delivery
The final phase is the therapeutic delivery of the cell product. It should be noted that the development phase’s feedback on one another during process optimization affects the biological discoveries which could be made. The design space gradually becomes better defined during the production phase. Specific issues associated with cell transplantation include biological or donor-to-donor variability, microbiological contamination, immunological responses to alloantigen, and tumorigenicity of the transplanted cells. The delivery of a cell therapy product will depend on its effectiveness in a clinical setting and the ability for its viable manufacture from a translational viewpoint.
7.2.4 The Modern Challenges of Cell Therapy
While cell therapies exhibit significant promise in bringing innovative and much-needed treatments to patients, several key issues currently limit their broader adoption.
Ahead are some challenges of cell therapy:
-
Safety concerns over the administration of the live cells to the patients, uncertainties over the regulatory aspects of these therapies, unknown downstream effects, and the need for sufficient investment to fully commercialize the research are frontline challenges that must be overcome to accelerate the furtherance of cell therapies.
-
Owing to the huge variability potential within treatments, an additional challenge in cell therapy is the requirement of robust manufacturing processes that consistently deliver safe and effective products. Cell therapy manufacturing processes can range from the simple expansion of autologous cells that would be administered back to patients to the complex genetic manipulation of allogeneic cells that could be stored and banked for the treatment of multiple patients. The regulations surrounding cell therapies must therefore be sufficiently broad to cover a wide range of therapeutic processes while still safeguarding product safety and quality.
-
From a manufacturing point of view, autologous cell therapies can be more challenging to carry out than allogeneic cell therapies as each dose is a single batch and is derived from a different source. This presents problems for cell culture, as cells from different patients are more likely to respond in distinct ways, and thereby, the source material will contain a variety of cells with widely dissimilar growth and differentiation capabilities.
-
Additionally, if the cells are stored together, there is an increased contamination risk across batches. Contrary to autologous cell cultures, allogeneic cell therapy manufacturing processes are less prone to cross-contamination as they are usually derived from a single large batch. However, other manufacturing challenges do pose a constraint.
-
Maintaining product consistency throughout the different stages of development is often a difficult task as many variables can affect cell growth. As such, developers of cell therapy products must consistently monitor their processes and adopt the best cell culture methods to ensure that products are manufactured with the desired critical quality attributes.
8 Mammalian Cell Culture in Gene Therapy
Gene therapy involves the transfer of genetic material (e.g., a gene), usually in a carrier or vector, and the uptake of the gene within the appropriate cells of the body. In the broadest sense, gene therapy involves the introduction, removal, or change in the content of a person’s genetic code to treat or cure a disease that cannot be treated by traditional therapy. The transferred genetic material significantly alters the production of a single or a group of proteins, produced by the specific somatic cells. Gene therapy can be used to reduce the expression levels of a disease-causing version of a protein, resulting in increased production of disease-fighting or generating new/modified proteins (Wu et al. 2002).
Gene therapy can be divided into the following few types:
-
Gene addition
-
Gene correction
-
Gene silencing
-
Reprogramming
-
Cell elimination
Ahead is a brief discussion of these gene therapy variations:
8.1 Gene Addition
This process involves the insertion of a new gene copy into the target cells to augment a higher protein expression. Most often, a modified virus such as an adeno-associated virus (AAV) is used to carry the gene into the cells. Therapies based on gene addition are being developed to treat many diseases, including adenosine deaminase severe combined immunodeficiency (ADA-SCID), congenital blindness, hemophilia A, Leber Congenital Amaurosis, lysosomal storage diseases, X-linked chronic granulomatous disease, and many others.
8.2 Gene Correction
This process can be achieved by modifying a part of a gene using recently developed gene-editing technology (e.g., CRISPR/cas9, TALEN, or ZFN) to remove repeated or faulty gene elements or to replace a damaged or dysfunctional DNA region. The goal of gene correction is to produce a protein that functions in a normal manner rather than contributing to a disease’s development. It may be possible to use gene correction in the treatment of a wide range of diseases; recent experimental work has used gene editing to extract HIV from the genome of affected laboratory mice and to excise the expanded region responsible for Huntington’s disease, from the human genes.
8.3 Gene Silencing
This process prevents the production of a specific protein by targeting messenger RNA (mRNA) for degradation so that no protein is produced. The mRNA exists in a single-stranded form in human and animal cells, whereas some RNA viruses have double-stranded RNA (dsRNA). Human and animal cells recognize dsRNA as being viral in origin and destroy it to prevent its spread. Gene silencing uses small RNA sequences to bind unique sequences in the target mRNA, making it double-stranded. This triggers mRNA destruction using the cellular machinery that destroys viral RNA. Gene silencing is an appropriate gene therapy-mediated disease treatment wherever too much of a protein is produced. For example, too much tumor necrosis factor-alpha (TNFα) is often observed in the afflicted joints of rheumatoid arthritis patients. As TNFα is needed in small amounts by the rest of the body, gene silencing is used to reduce TNFα expression extents in the affected tissues.
8.4 Reprogramming
This process involves adding one or more genes to the specific cells with the intent to change their characteristics. This technique is particularly powerful in tissues where multiple cell types exist and the disease is caused by the impaired functioning of one kind of cell. For example, type I diabetes occurs because many of the insulin-producing islet cells (β cells) of the pancreas are damaged. At the same time, the cells of the pancreas that produce digestive enzymes are not damaged. Reprogramming these cells so that they start producing insulin offers a novice treatment for type I diabetic patients.
8.5 Cell Elimination
This strategy is typically used to destroy malignant (cancerous) tumor cells but can also be used to target the overgrowth of benign (noncancerous) tumor cells. Tumor cells can be eliminated via the introduction of “suicide genes,” which enter the tumor cells and release a prodrug that induces cell death in those cells. Viruses can be engineered to develop an affinity for tumor cells. These oncotropic viruses can carry therapeutic genes to increase toxicity within the tumor cells, stimulating the immune system to attack the tumor or inhibit the growth of blood vessels supplying nutrients to the tumor.
8.6 Potential Level of Gene Therapy
Three potential levels of gene therapy are known concerning their application to treat genetic diseases (Fig. 10).
Level 1: Substitutional gene therapy is a transient, non-heritable replacement or augmentation of a working product for a null gene product, one that is typically knocked out by a mutation. The repeated use of recombinant human insulin by insulin-dependent diabetics as a replacement for genetically defective insulin and glucocerebrosidase in the case of Gaucher disease is an example of successful substitutional gene therapy.
Level 2: Somatic cell gene therapy is a long-term, non-heritable modification of somatic cell genomes to cure or prevent deleterious conditions, without modifying the gametes or germ-line cells. Typically, body cells are removed from an (genetically modified or engineered) individual before being placed back into the same individual. The first successful application of somatic gene therapy in humans occurred in the well-known case of Ashanti de Silva, a 4-year-old girl affected with a genetic form of SCID called adenosine deaminase deficiency, who, on September 14, 1990, at 12:52 pm, successfully received a transfusion of her cells carrying her genetically modified, defective ADA gene. Similarly, an aerosol system delivering a genetically engineered CFTR product to cystic fibrosis patients has also been developed. These first two levels of gene therapy substitute or repair genes in a patient’s body cells only wherein the sex cells quite uncharacteristically remain unaffected. If the patient then chooses to reproduce, the children may be affected with the same condition as that of the parent.
Level 3: Gametic gene therapy (also called germ-line or germ-cell gene therapy) is the practice of permanent genetic engineering of either a patient’s gametes or a fertilized pre-morula zygote after which certain alterations are perpetuated in all the cell lines of a resulting embryo and the normal gene may be transmitted to future generations if the patient later chooses to reproduce. To date, gametic gene therapy has never been attempted in humans. Gametic gene therapy is the only form of gene therapy that can potentially eliminate a genetic disease from an individual family line by engineering both body (somatic) and sex/gonadal cells so that subsequent reproduction results in unaffected offspring. Ethical issues seriously limit the conduct of gametic gene therapy in humans.
8.7 Process of Gene Delivery to the Target Cells
Scientists and clinicians mainly use both viral and nonviral vector methods to carry genetic material into the targeted cells.
Here is a brief discussion about them:
8.8 Viral Vector Methods
Viruses have an innate ability to invade normal cells in a potential host. Viral vectors for gene therapy are modified to utilize the cell entering ability of viruses after disabling the viral capability to further divide. Different viruses have been engineered to function as gene therapy vectors. In the case of adeno-associated virus (AAV) and retrovirus/lentivirus vectors, the gene(s) of interest and control signals replace all or most of the essential viral genes in the vector to prevent replication of the viral vector.
For oncolytic viruses, such as adenovirus and herpes simplex virus, fewer viral genes are replaced, and the virus is still able to replicate in a restricted number of varying cell types. The different viral vectors preferentially enter a subset of different tissues, express genes at different levels, and interact with the immune system distinctively.
8.9 Nonviral Vector Methods
Nonviral vector methods such as electroporation, passive delivery, and ballistic delivery are also used for gene therapy. Simple strands of naked DNA or RNA can be pushed into cells using high-voltage electroporation. This is a common technique used in the lab. Naked DNA or RNA may also be taken up by target cells using a normal cellular process called endocytosis after it is added to the medium surrounding the cells. Finally, (sheer) mechanical force facilitates the introduction of genetic material with an instrument called a “gene gun.”
All these techniques are already briefly discussed earlier. Genetic material can be packaged into artificially created liposomes (sacs of fluid surrounded by a fatty membrane) that are more easily taken up by the cells than naked DNA/RNA. Different types of liposomes are being developed to preferentially bind the specific tissues. Recent work has utilized a membrane vesicle subtype that is endogenously produced and released by cells (extracellular vesicles or “exosomes”) to carry small RNA sequences into specific tissues.
8.10 Combination of Cell and Gene Therapy
Importantly, gene therapy can be combined with cell therapy protocols as discussed previously. In such attempts, cells are collected from the patient or matched donor before being purified and expanded in vitro. Scientists and clinicians then deliver the gene to the cells using one of the earlier described methods. The cells that express the therapeutic gene are thereafter, readministered to the patient.
8.11 Risks Associated with Cell and Gene Therapy
Risks of any medical treatment depend on the exact composition of the therapeutic agent and its selective route of administration (intravenous, intradermal, or surgical). Risks include the outcomes limiting the successful conduct of gene or cell therapy in line with the expectations, possibly prolonging or worsening symptoms, or complicating the conditions with manifold adverse effects.
-
The administration of genetic material may induce a strong immune response to the protein in the case the replaced proteins are associated with genetic diseases. Ultimately, an aggravated immune response is noted, leading to normal proteins or cells being attacked, as in autoimmune diseases.
-
On the other hand, in cancer or viral/fungal/bacterial infections, the immune response may be below par (or lower than normal); otherwise, the targeted cell or microorganisms may develop resistance to the therapy.
-
With the current generation of vectors in clinical trials, there is no optimized mechanism to “turn off” gene expressions, and the chances of developing unwanted effects are quite high.
-
With retroviral or lentiviral vectors, integration of the genetic material into the patient’s DNA may occur next to a gene involved in cell growth regulation, and the insertion may induce a tumor over time via “insertional mutagenesis.”
-
High doses of some viruses can be toxic to some individuals or specific tissues, especially if the individuals are immunologically compromised.
-
Gene therapy evaluation is generally done after birth. There is little data on what effects this therapeutic approach might have on embryos owing to which pregnant women are usually excluded from clinical trials.
8.12 Usefulness of Gene and Cell Therapy in Medical Sciences
Amniocentesis, a diagnostic technique that enables doctors to remove and culture fetal cells from pregnant women, has emerged as an asset for doctors for the timely diagnosis of fetal disorders. The damaged cells can then be examined for abnormalities in their chromosomes and genes using karyotyping, chromosome painting, and other molecular techniques.
The usefulness of gene therapy can be divided into the overleaf sections based on the specific genetic disorders they cause:
-
Gene therapy against various cancers
-
Gene therapy against muscular disorders
-
Gene therapy against eye/vision disorders
-
Gene therapy against cardiovascular disorders
-
Gene therapy against neurological disorders
-
Gene therapy against bone disorders
Here are some examples of FDA-approved gene therapy against various diseases:
8.12.1 Gene Therapy against Various Cancers
-
In August 2017, the US FDA approved the use of Kymriah (Novartis) for the treatment of specific instances of B-cell acute lymphoblastic leukemia. This chimeric antigen receptor (CAR) T-cell therapy modifies the patient’s immune cells (T cells) to engineer their aggressive countering of leukemia cells. Clinical trials are currently underway for additional uses of Kymriah in adult patients and other forms of cancers. More information is expected to be made available in the near future.
-
In October 2017, Yescarta (axicabtagene ciloleucel, Axi-Cel, Kite Pharma, Inc), another CAR-based T-cell therapy, was approved by the US FDA for the treatment of non-Hodgkin lymphoma, adult sufferers with a history of at least two failed systemic therapies.
-
Yescarta (Kite Pharma Inc./Gilead) became the first US FDA-approved CAR T-cell therapy for use in adult patients, in October 2017. The drug was approved to treat adults with relapsed or refractory large B-cell lymphoma and was the second-ever approved mediator for CAR T-cell therapy.
-
Gendicine gene therapy drug, harboring the Tp53 gene, has been developed to treat head and neck squamous cell carcinoma (HNSCC). This recombinant adenovirus was developed by Shenzhen Sibiono GeneTech and was approved by China Food and Drug Administration (CFDA) on October 16, 2003. The drug found its way to the commercial market in 2004. In gendicine (drug), the E1 region of human serotype 5 adenovirus (Ad5) is replaced by human wild-type Tp53. The Tp53 expression in cancer cells stimulates antitumor attributes by initiating apoptotic pathways, suppressing DNA repair and antiapoptotic events, and seizing the survival pathways. The vector is produced in HEK293 cells by co-transfection of the Tp53 expression cassette shuttle vector with an Ad5 genome recombinant plasmid. The cassette contains the Rous sarcoma virus (RSV) promoter, the wild-type human Tp53 gene, and a bovine poly-A signal. Upon intra-tumor injection at a concentration of 1 × 1012 viral vector particles per vial, gendicine binds to the coxsackie virus-adenovirus receptor, entering the tumor cells via receptor-mediated endocytosis, expressing ectopic Tp53 gene. The most common side effect of gendicine is self-limiting fever (of 37.5 °C to 39.5 °C), normally occurring 2–4 h after administration, and lasting for approximately 2–6 h.
-
As the first oncolytic virus approved by CFDA, recombinant human adenovirus type 5 (rAd5-H101) was commercially marketed under the brand name Oncorine, in November 2005. The drug was manufactured by Shanghai Sunway Biotech and was initially licensed for the treatment of patients with terminal stage refractory nasopharyngeal cancer in combination with chemotherapy, following phase III of the clinical trial.
-
Rexin-G is a retroviral vehicle harboring a cytocidal cyclin G1 construct, considered the world’s first tumor-targeting injectable gene therapy vector, approved by FDA for metastatic pancreatic cancer. The drug was officially approved by the Philippine FDA in December 2007 resulting in the progression of clinical studies to phase III trials, in the USA.
-
Pegaptanib was developed by EyeTech Pharmaceuticals and Pfizer Inc. with the brand name Macugen. It is a polynucleotide aptamer targeting vascular endothelial growth factor (VEGF165 isoform) for neovascular age-related macular degeneration (AMD) treatment. Pegaptanib was the first anti-angiogenic drug approved by the US FDA in December 2004 and was the only therapy for AMD treatment. It is also the first therapeutic aptamer with RNA structure, achieving FDA market approval. AMD is the most common cause of severe vision loss and blindness among aged individuals in the developed world. It is characterized by deterioration of the central region of the retina. Abnormal blood vessel growth accounts for 90% of severe vision losses. It has been suggested that VEGF plays a prominent role in the growth and permeability of new vessels in AMD. Anti-VEGF agents are used as molecular therapies which attempt to block angiogenesis as well as vessel permeability. Pegaptanib is a 28-mer RNA oligonucleotide covalently linked to two-branched 20-kD polyethylene glycol chains. It specifically binds to the VEGF165 isoform at the heparin-binding site, thus preventing the heparin binding to VEGF receptors located on the vascular endothelial cells’ surface. VEGF165 has been implicated in pathological ocular neovascularization via enhanced vascular permeability and inflammation. The recommended dose is 0.3 mg/90 μl pegaptanib, administered once every 6 weeks via intravitreal injection into the eye. Based on preclinical data, Pegaptanib is metabolized by endo- and exonucleases and is not influenced by the cytochrome P450 system. In two clinical trials involving 1186 participants, the efficacy of pegaptanib was determined by the ability of patients to lose less than 15 letters of visual acuity from baseline without dose-response monitoring. The result demonstrated pegaptanib as an effective AMD therapy. Moreover, a clinical trial assessed the side effects and the efficacy of pegaptanib in the treatment of 23 participants suffering from neovascular AMD with a previous history of arterial thromboembolic events (ATEs). Pegaptanib administration did not reveal any systemic or ocular side effects nor did it leads to any recurrent ATEs.
-
Imlygic or talimogene laherparepvec is a genetically manipulated oncolytic herpes simplex virus (HSV) type 1, developed against multiple solid tumors such as unresectable cutaneous, subcutaneous, and nodal lesions of melanoma. Imlygic was created by BioVex Inc. under the brand name, OncoVEXGM-CSF. The drug was approved by the US FDA in October 2015 for targeting melanoma. It was subsequently approved in Europe and Australia in 2016.
8.12.2 Gene Therapy against Muscular Disorders
-
In May 2019, the FDA approved Zolgensma for spinal muscular atrophy treatment in less than 2-year-old children.
-
Eteplirsen was developed by Sarepta Therapeutics under the trade name, Exondys 51. This drug is a 30-mer phosphorodiamidate morpholino oligomer (PMO) designed to cause exon 51 (of dystrophin gene) depletion. Expression of functional dystrophin (a protein) in patients with Duchenne muscular dystrophy (DMD) having mutated DMD gene is amenable by skipping exon 51. The studied group of patients involved nearly 13% of all DMD cases, making exon 51 a suitable gene therapy target. In September 2016, the FDA approved Exondys 5 in a hurried procedure based on the dystrophin production in skeletal muscle as noticed in some cases, upon being treated with the drug.
-
Nusinersen, commercialized under the name Spinraza by Biogen, was the first-ever medication approved for spinal muscular atrophy (SMA) treatment. Nusinersen was approved by the DA in December 2016 and by European Medicines Agency (EMA) in May 2017.
8.12.3 Gene Therapy against Eye/Vision Disorders
-
The first virally delivered gene therapy to be approved for clinical usage in the USA, Luxturna (Spark Therapeutics), was approved in December 2017 by the FDA. Luxturna is a one-time gene therapy treatment used to improve vision in patients with established genetic vision loss due to Leber congenital amaurosis or retinitis pigmentosa, both being inherited retinal diseases.
-
Vitravene, also called fomivirsen, is an antisense oligonucleotide (ASO) designed as a therapeutic strategy for cytomegalovirus (CMV) retinitis in HIV-positive patients, having no viable option for CMV retinitis treatment. Fomivirsen is the first-ever gene-silencing antisense therapy approved for marketing by the FDA. This drug was developed through a collaboration between Isis Pharmaceuticals and Novartis Ophthalmics and was approved by FDA in August 1998 and a year later by EMA/EMEA to treat cytomegalovirus retinitis.
8.12.4 Gene Therapy against Cardiovascular Disorders
-
In 2010, the Human Stem Cells Institute of Russia developed Neovasculgen (PI-VEGF165), a plasmid DNA encoding VEGF 165 under the control of a CMV promoter for atherosclerotic, peripheral arterial disease (PAD) treatment. The drug was listed in Vital and Essential Drugs (EUVED) of the Russian Ministry of Health in 2012 and was then distributed in the Russian market.
-
Mipomersen , with a market name of Kynamro, emerged useful as an adjunct therapy for homozygous familial hypercholesterolemia (HoFH). Mipomersen was developed by Ionis Pharmaceuticals as a novel ASO inhibitor for the HoFH cure. It was rejected by EMA in 2012 due to cardiovascular and liver adverse effects. However, in January 2013, the FDA approved its marketing as an orphan drug for HoFH management.
-
Alipogene tiparvovec , marketed as Glybera, is the gene therapy drug for lipoprotein lipase deficiency (LPLD) treatment. It was developed by Amsterdam Molecular Therapeutics (AMT) in April 2012. In October 2012, the European Commission (EC) approved UniQure as the marketing authorization of Glybera for treating LPLD. Glybera is the first licensed gene therapy product for an inherited disorder in Europe.
8.12.5 Gene Therapy against Neurological Disorders
With the brand name Onpattro, patisiran is the only FDA-approved RNA interference (RNAi) drug targeting polyneuropathy caused by hereditary transthyretin-mediated amyloidosis (hATTR). The FDA approved this targeted RNA-based drug on August 10, 2018. Alnylam Pharmaceuticals, Inc. (NASDAQ), the leading RNAi therapeutics company, developed this lipid complex drug to treat familial amyloid polyneuropathy (FAP) in adults.
8.12.6 Gene Therapy against Bone Disorders
Invossa (TissueGene-C) has completed phase III trials in the USA and attained marketing approval in Korea by Kolon TissueGene as a first-in-class cell-mediated gene therapy strategy for symptomatic and persistent knee osteoarthritis (OA) treatment. It contains a 3:1 mixture of non-transformed and retrovirally transduced allogeneic chondrocytes that upregulate transforming growth factor β1 (TGFβ1) expression.
8.13 Gene Therapy against Other Diseases
-
Defibrotide , commercially known as Defitelio, is manufactured by Jazz Pharmaceuticals plc. Defitelio is a DNA derivative anticoagulant used for patients with hepatic sinusoidal obstruction syndrome/veno-occlusive disease (SOS/VOD) with renal or pulmonary dysfunction following the cytoreductive treatment before hematopoietic stem cell transplantation (HSCT). The efficacy data from 528 investigated hepatic VOD participants exhibiting renal or pulmonary dysfunction following HSCT supported approval of defibrotide by the FDA in March 2016. It was also evaluated and approved by EMA in May 2017.
-
Recently, AveX, a drugmaker owned by pharmaceutical giant Novartis, developed onasemnogene abeparvovec with the brand name Zolgensma. It is the most recent authorized gene therapy drug by the FDA (May 2019). It was previously well-known with the compound name AVXS-101. Zolgensma is a proprietary gene therapy strategy for curing pediatric patients below 2 years, who have mutations in both alleles of the SMN1 gene. Zolgensma has been designed to render a healthy copy of the SMN gene to arrest the disease progression by maintaining normal SMN gene expression with a single, one-time intravenous infusion.
9 Mammalian Cell Culture in Cell Fusion Technology
In cell fusion technology, two cells of either the same or different lineages use together to form a single cell.
Based on the nucleus, the fused cells can be divided into two groups:
-
Synkaryon
-
Heterokaryon
Here is a brief description of synkaryon and heterokaryo.
9.1 Synkaryon
When the fusion of two cells gives rise to only one cell having a single nucleus with 4 N, it is called a synkaryon. In the case of synkaryon, chromosomes are ultimately lost or resorted.
9.2 Heterokaryon
When the fusion of two cells gives rise to only one cell having two nuclei with 2 N + 2 N chromosomal distribution, it is called heterokaryon.
Cell fusion technology has widespread applications in molecular cell biology, such as the following:
-
Production of hybridoma for antibody generation
-
Study of the malignancy tissues
-
Gene mapping
-
Study of the controlling gene expression, differentiation, and viral application
9.3 Methods of Cell Fusion
In the 1960s, hybrid cells were successfully produced from mixed cultures of two different mouse cell lines, in France for the first time. The procedure involved induction of cells growing in the culture using some viruses such as the Sendai virus to fuse and form hybrids. This virus induces two different cells to form heterokaryons, at first. During mitosis, the heterokaryon chromosomes move toward the two poles and later on the fuse to form hybrids. It is important to remove the surface carbohydrates to facilitate cell fusion. Besides Sendai virus-dependent cell fusion, some other fusion methods include electrical cell fusion , polyethylene glycol cell fusion, and thermoplasmonics-induced cell fusion.
The four methods of cell fusion are as below:
-
1.
Electrically facilitated cell fusion
-
2.
Polyethylene glycol aided cell fusion
-
3.
Sendai virus-induced cell fusion
-
4.
Thermoplasmonics-induced cell fusion
Ahead is a brief discussion of the above four methods of cell fusion:
9.3.1 Electrically Facilitated Cell Fusion
The process was discovered in 1978 by Zimmermann, who has initiated ongoing development ever since.
9.3.1.1 The Principle of Electrically Facilitated Cell Fusion
First, the cells are brought into very close contact via dielectrophoresis. Unlike electrophoresis, in which direct current is applied to move molecules, dielectrophoresis uses high-frequency alternating current. In particles such as living cells, dipoles are induced, driving cell alignment in a manner resembling a string of pearls that are in very close contact with each other.
A very short high-voltage pulse is then applied, which causes permeation of the cell membrane and the subsequent combining, thereafter resulting in cell fusion. To stabilize the process, an alternating voltage is then applied for a brief duration. The resulting formation is described as a heterokaryon because, despite the fusion of the outer cell membrane, two or more cell nuclei still prevail. The cell nuclei also fuse at a later stage within the cell. In most cases, this results in a drastic reduction in the chromosomal number in the nucleus.
By definition, electrically assisted fusion is a double-conditioned process:
-
1.
Close physical contact between cells has to be established.
-
2.
Cell membranes have to be brought into a fusogenic state.
Physical contact between cells can be achieved in several ways, though the most widely used is dielectrophoresis, where cells are aligned in pearl chains using alternating electric fields. Dielectrophoresis is most frequently used especially in hybridoma technology and the production of cell vaccines since it enables establishing contacts between suspended cells.
The second condition for electrically assisted cell fusion involves the achieving of membrane fusogenic state via electric pulse application resulting in structural rearrangement of the lipid bilayer.
It is generally accepted that the transmembrane voltage induced on the cell membrane during exposure to high electric fields reduces the energy barrier for the formation of hydrophilic pores in the lipid bilayer, although other explanations are also plausible. The phenomenon is termed electroporation and is related to the experimental witness of the dramatic increase in membrane permeability. At the same time, membrane fusogenicity correlates with electroporation. Both the extent of electroporation and fusion yield can be controlled by the amplitude, duration, and a number of the applied pulses. Increasing any of the mentioned pulse parameters leads to enhanced membrane electroporation and consequently a greater number of fused cells. However, parameters of the electric pulses must be carefully chosen to ensure that electroporation is reversible, i.e., cells survive. A deviation from this leads to irreversible cell electroporation, thereby reducing cell survival as well as consequent viable fused cell yield.
At a given electric field, strength of the extent of membrane electroporation further depends on the cell size. One of the major advantages of electrofusion is the possibility of optimizing electroporation conditions for each cell line on an individual basis. Unfortunately, there is a substantial challenge in fusing cell lines that differ considerably in their size. Electric pulses that are usually used for electrofusion range from 10 to 100 μs, ensuring that cell membranes become fully charged amidst exposure to electric pulse. Under such conditions, the induced transmembrane potential difference is proportional to the cell radius, implying that small cells are electroporated (i.e., brought into a fusogenic state) at higher electric field strengths. Applying pulses that effectively electroporated small cells thus inevitably leads to excessive electroporation and consequently the death of large fusion partner cells. An example where a difference in cell size hinders the optimization of pulse parameters is the hybridoma technology since B lymphocytes (approximate radius of human B lymphocytes corresponds to 3.85 ± 0.35 μm) are considerably smaller than myeloma cells (approximate radii of human and mouse NS1 cells correspond to 5.25 ± 0.25 μm and 7.75 ± 0.25 μm, respectively).
The efficiency of electrofusion depends on the following parameters:
-
Size of the cells to be fused
-
Pulse parameters
-
Composition of the fusion medium
-
Osmolarity of the fusion medium
-
Temperature
-
Post pulse cell incubation
-
Other factors
However, despite many efforts for improving electrofusion of cells having dissimilar sizes, higher susceptibility of larger cells to electric pulses remained one of the obstacles, and the number of viable hybridomas obtained concerning the number of input B lymphocytes remained only ~1% or less.
It is an essential step in some of the most innovative modern biology methods. This method begins when two cells are brought into contact by dielectrophoresis. Dielectrophoresis uses a high-frequency alternating current, unlike electrophoresis in which a direct current is applied. Once the cells are brought together, a pulsed voltage is applied. The pulse voltage causes the cell membrane to permeate and subsequent combining of the membranes results in cell fusion. After this, an alternative voltage is applied for a brief duration to stabilize the process. The result of this is that the cytoplasm of two cells gets mixed and the cell membrane has completely fused. All that remains separate is the nuclei, which fuse at a later stage within the cell, producing a heterokaryon cell, as a result.
Exposure of cells or liposomes to a brief pulse of a strong electrical field can result in a reversible breakdown of the outer membrane. Such breakdown causes an enhanced plasmalemma permeability which however reseals after a short incubation (i.e., till when the original impermeability is restored). Two or more cells in contact can be made to fuse by this process, provided that the contact is close enough and that the electric field pulse is short enough not to damage the cells. Methods of achieving this contact by electrical and magnetic fields are well-demonstrated. The magnetic method does not require a manifested low conductivity of media (used earlier). Other possible modifications of this flexible technique are also described and are used to understand the modification of the technique and its subsequent application to membrane research, medicine, and plant breeding.
9.3.2 Polyethylene Glycol Aided Cell Fusion
Polyethylene glycol (PEG)-mediated cell fusion is a simple and efficient technique used widely for the production of somatic cell hybrids and nuclear transfer in mammalian cloning. Fusion can be performed between adherent and suspension cells. Either whole cells or microcells can be used as donors to fuse with recipient cells. Microcell fusion is particularly useful in the transfer of a single or a limited number of chromosomes between various cells.
PEG is capable of fusing a wide variety of cells, including interspecific and interkingdom cell types. PEG exhibits a very low degree of cytotoxicity; it is only toxic at high concentrations (greater than 50%) and on a prolonged incubation (typically minutes for most cell lines). PEG is a water-soluble fusogen unlike nonpolar or amphipathic chemical fusogens , such as fatty acids, retinol, and lysolecithin which act by entering the bilayer. Thus, it is relatively easy to remove PEG from the cell medium by washing. The use of PEG has several additional advantages over other fusogens: reproducibility in fusion capabilities, high fusion efficiency, inexpensiveness, easier availability, and ease of handling. The attainment of cell fusion by PEG involves its action as a dehydrating agent, attaining the fusion of not only plasma membranes but also intracellular membranes. This leads to cell fusion since PEG induces cell agglutination and cell-to-cell contact. Though this regime of cell fusion is the most widely used, it still has downfalls. Oftentimes, PEG can cause uncontrollable fusion of multiple cells, leading to the appearance of giant polykaryons. Also, standard PEG cell fusion is poorly reproducible and different cells have various fusion susceptibilities. This kind of cell fusion is widely used for producing somatic cell hybrids and nuclear transfer in mammalian cloning. Thus, PEG-mediated cell fusion is a simple and efficient technique used widely for the production of somatic cell hybrids and nuclear transfer in mammalian cloning. Using this method, one can successfully introduce mammalian mini-chromosomes into a variety of vertebrate cells.
9.3.3 Sendai Virus-Induced Cell Fusion
-
Cell fusion by the Sendai virus occurs in four distinct temperature-regulated steps. During the first stage (lasting no longer than 10 min), viral adsorption takes place and the adsorbed virus is thereafter inhibited by viral antibodies.
-
The second stage is typical 20 min and comprises a pH-dependent process, wherein the addition of viral antiserum can inhibit ultimate fusion.
-
In the third step, the antibody-refractory stage and viral envelope constituents remain detectable on the cell surface.
-
During the fourth stage, cell fusion becomes evident with a concurrent disappearance of HA neuraminidase and fusion factor. The first and second stages are the only two pH-dependent steps.
9.3.4 Thermoplasmonics-Induced Cell Fusion
Thermoplasmonics is based on a near-infrared (NIR) laser and a plasmonic nanoparticle treatment. The laser which typically acts as an optical trap is used to heat the nanoscopic plasmonic particle to very high and extremely local elevated temperatures. Optical trapping of such a nano-heater at the interface between two membrane vesicles or two cells leads to immediate fusion, inferred via simultaneous content and lipid mixing. Advantages include full flexibility of which cells to fuse and the conduct of fusion in any buffer condition, unlike the salt-affected electro-formation.
10 Conclusions
The primary focus of this chapter was to discuss the usefulness of mammalian cells such as CHO, BHK, HEK, COS, NSO, HT1080, and PER-C6 and their products concerning a thorough understanding of various physiological and pathophysiological events. The topics primarily discussed include (i) use of mammalian cells as a model system for physiological and pathophysiological studies; (ii) use of mammalian cells for experimental drug/toxin research; (iii) usefulness of mammalian cell culture in vaccine production, particularly against pathogenic viruses; (iv) usefulness of mammalian cell culture for various recombinant protein production such as tissue plasminogen activator, urokinase, follicle-stimulating hormone, blood clotting factor VIII, and erythropoietin; (v) mammalian cell culture in cell therapy; and finally (vi) mammalian cell culture in gene therapy. This chapter will enhance readers’ understanding of the usefulness of cells, their culture, and the corresponding products in cell biology, physiology/pathophysiology (e.g., cancers), biotechnology, pharmacology, and medical sciences.
References
Almo SC, Love JD. Better and faster: improvements and optimization for mammalian recombinant protein production. Curr Opin Struct Biol. 2014;26:39–43.
Andersen DC, Reilly DE. Production technologies for monoclonal antibodies and their fragments. Curr Opin Biotechnol. 2004;15:456–62.
Andersson LO, Forsman N, Huang K, et al. Isolation and characterization of human factor VIII: molecular forms in commercial factor VIII concentrate, cryopricitate, and plasma. PNAS USA. 1986;83:2979–83.
Aricescu AR, Lu W, Jones EY. A time and cost-efficient system for high-level protein production in mammalian cells. Acta Crystallogr D Biol Crystallogr. 2006;62:1243–50.
Barlow GH. Urinary and kidney cell plasminogen activator (urokinase). Methods in Enzymol. 1976;45:239–44.
Bernik MB, Kwaan HC. Plasminogen activator activity in cultures from human tissues. An immunological and histochemical study. J Clin Invest. 1969;48:1740–53.
Browne SM, Al-Rubeai M. Selection methods for high-producing mammalian cell lines. Trends Biotechnol. 2007;25:425–32.
Campos-da-Paz M, Costa CS, Quilici LS, Simoes IDC, Kyaw CM, Maranhao AQ, et al. Production of recombinant human factor VIII in different cell lines and the effect of human XBP1 co-expression. Mol Biotechnol. 2008;39:155–8.
Colosimo A, Goncz KK, Holmes AR, Kunzelmann K, Novelli G, Malone RW, et al. Transfer and expression of foreign genes in mammalian cells. Bio Techniques. 2000;20:314–31.
Dalton AC, Barton WA. Over-expression of secreted proteins from mammalian cell lines. Protein Sci. 2014;23:517–25.
Davis JM, Arakawa T. Characterization of recombinant human erythropoietin produced in Chinese hamster ovary cells. Biochemistry. 1987;26:2633–8.
Egrie J. The cloning and production of recombinant human erythropoietin. Pharmacotherapy. 1990;10:3S–8S.
Ekwall B. Screening of toxic compounds in tissue culture. Toxicology. 1980;17:127–42.
Ekwall B. Screening of toxic compounds in mammalian cell cultures. Ann N Y Acad Sci. 1983;407:64–77.
Fantacini DMC, Picanço-Castro V. Production of recombinant factor VIII in human cell lines. Methods Mol Biol. 2018;1674:63–74.
Fischbach MA, Bluestone JA, Lim WA. Cell-based therapeutics: the next pillar of medicine. Sci Transl Med. 2013;5:179ps7.
Geisse S, Henke M. Large-scale transient transfection of mammalian cells: a newly emerging attractive option for recombinant protein production. J Struct Funct Genom. 2005;6:165–70.
Gitschier J, Wood WI, Goralka TM, Wion KL, Chen EY, Eaton DH, et al. Characterization of the human factor VIII gene. Nature. 1984;312:326–30.
Gray D. Overview of protein expression by mammalian cells. Curr Protoc Protein Sci. 1997;10:5.9.1–5.9.18.
Griffiths JB, Electricwala A. Production of tissue plasminogen activators from animal cells. Vertebrate Cell Culture. 2005;I:147–66.
Hakola K, Van der Boogaart P, Mulders J, de Leeuw R, Schoonen W, Heyst JV, et al. Recombinant rat follicle-stimulating hormone; production by Chinese hamster ovary cells, purification and functional characterization. Mol Cell Endocrinol. 1997;127:59–69.
Howles CM. Genetic engineering of human FSH (gonal-F). Hum Reprod Update. 1996;2:172–91.
Huang TK, McDonald KA. Bioreactor engineering for recombinant protein production in plant cell suspension cultures. Biochem Eng J. 2009;45:168–84.
Hunter M, Yuan P, Vavilala D, Fox M. Optimization of protein expression in mammalian cells. Current Prot in Protein Sci. 2019;95:e77.
Jones AJ, Garnick RL. Quality control of rDNA-derived human tissue-type plasminogen activator. Bioprocess Technol. 1990;10:543–66.
Khan KH. Gene expression in mammalian cells and its applications. Adv Pharm Bull. 2013;3:257–63.
Kost TA, Condreay JP. Recombinant baculoviruses as mammalian cell gene-delivery vectors. Trends Biotechnol. 2002;20:173–80.
Lai T, Yang Y, Ng SK. Advances in mammalian cell line development technologies for recombinant protein production. Pharmaceuticals (Basel). 2013;6:579–603.
Li F, Vijayasankaran N, Shen A, Kiss R, Amanullah A. Cell culture processes for monoclonal antibody production. MAbs. 2010;2:466–77.
Liu C, Dalby B, Chen W, Kilzer JM, Chiou HC. Transient transfection factors for high-level recombinant protein production in suspension cultured mammalian cells. Mol Biotechnol. 2008;39:141–53.
Masters JRW. Human cancer cell lines: fact and fantasy. Nat Rev Mol Cell Biol. 2000;1:233–6.
Mills M, Estes MK. Physiologically relevant human tissue models for infectious diseases. Drug Discov Today. 2016;21:1540–52.
Mirabelli P, Coppola L, Salvatore M. Cancer cell lines are useful model systems for medical research. Cancers (Basel). 2019;11:1098.
Montagnon BJ, Fanget B, Nicolas AJ. The large-scale cultivation of Vero cells in microcarrier-culture for virus-vaccine production: preliminary results for killed poliovirus-vaccine. Dev Biol Stand. 1981;47:55–64.
Omasa T. Gene amplification and its application in cell and tissue engineering. J Biosci Bioeng. 2002;94:600–5.
Paganuzzi-Stammati A, Silano V, Zucco F. Toxicology investigations with cell culture systems. Toxicology. 1981;20:91–153.
Plotkin SA, Eagle H, Hayflick L, Ikic D, Koprowski H, Perkins F. Serially cultured animal cells for preparation of viral vaccines. Science. 1969;165:1278–82.
Rijken DC, Collen D. Purification and characterization of the plasminogen activator secreted by human melanoma cells in culture. J Biol Chem. 1981;256:7035–41.
Sambrook, Fritsch, Maniatis. Molecular cloning: a laboratory manual. 2nd ed. New York: Cold Spring Harbor Laboratory Press, Cold Spring Harbor; 1989;3:Apendix B.12
Schimke RT. Gene amplification in cultured animal cells. Cell. 1984;37:705–13.
Sissolak B, Kandra K, Stosch MV, Mayer M, Striedner G. Quality by control: towards model predictive control of mammalian cell culture bioprocesses. Biotechnol. 2017;12. Special Issue: Biochemical Engineering Science
Takeuchi M, Inoue N, Strickland TW, Kubota M, Wada M, Shimizu R, et al. Relationship between sugar chain structure and biological activity of recombinant human erythropoietin produced in Chinese hamster ovary cells. Proc Nati Acad Sci USA. 1989;86:7819–22.
Trill JJ, Shatzman AR, Ganguly S. Production of monoclonal antibodies in COS and CHO cells. Curr Opin Biotechnol. 1995;6:553–60.
Walter JK, Werz W, Berthold W. Virus removal and inactivation. Concept and data for process validation of downstream processing. Biotech Forum Europe. 1992;9:560–4.
Werz W, Hoffmann H, Haberer K, Walter JK. Strategies to avoid virus transmissions by biopharmaceutic products. Arch Virol Suppl. 1997;13:245–56.
White WF, Barlow GH, Mozen MM. The isolation and characterization of plasminogen activators (urokinase) from human urine. Biochemist. 1966;5:2160–9.
Wu SC, Huang GYL, Liu JH. Production of retrovirus and adenovirus vectors for gene therapy: a comparative study using microcarrier and stationary cell culture. Biotechnol Prog. 2002;18:617–22.
Wurm FM. Production of recombinant protein therapeutics in cultivated mammalian cells. Nat Biotechnol. 2004;22:1393–8.
Yarranton GT. Mammalian recombinant proteins: vectors and expression systems. Curr Opin Biotechnol. 1990;1:133–40.
Zeyda M, Borth N, Kunert R, Katinger H. Optimization of sorting conditions for the selection of stable, high-producing mammalian cell lines. Biotechnol Prog. 1999;15:953–7.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Singapore Pte Ltd.
About this entry
Cite this entry
Mukherjee, S., Malik, P., Mukherjee, T.K. (2023). Mammalian Cells, Tissues and Organ Culture: Applications. In: Mukherjee, T.K., Malik, P., Mukherjee, S. (eds) Practical Approach to Mammalian Cell and Organ Culture. Springer, Singapore. https://doi.org/10.1007/978-981-19-1731-8_17-2
Download citation
DOI: https://doi.org/10.1007/978-981-19-1731-8_17-2
Received:
Accepted:
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-1730-1
Online ISBN: 978-981-19-1731-8
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences
Publish with us
Chapter history
-
Latest
Mammalian Cells, Tissues and Organ Culture: Applications- Published:
- 20 January 2023
DOI: https://doi.org/10.1007/978-981-19-1731-8_17-2
-
Original
Mammalian Cells, Tissues and Organ Culture: Applications- Published:
- 10 December 2022
DOI: https://doi.org/10.1007/978-981-19-1731-8_17-1