Abstract
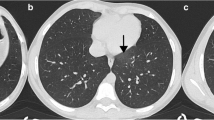
Background Although there were other reviews in 2019 and 2020, this is the first review of research that summarizes clinical features of the children with COVID-19 mentioned in literature in 2021. This paper analyses the findings on COVID-19 infection in children in three countries. Objective The purpose of this paper is to review publications using chest CT scans and chest X-ray findings for children with COVID-19 in 2021. Materials and methods Studies on COVID-19 for articles presenting scan findings in children with COVID-19 have been included in this review. This review focused on articles including 0 < age and age < 18 years using descriptive statistics to identify patterns including duration and several symptoms of the disease, and their relationship with outcomes. Results 12 research articles (n = 6212 children) based on chest CT scans and chest X-ray have been examined. The main results of this review article are as follows: (i) Approximately 1728 (27.81%) of pediatric patients with COVID-19 had normal chest CT scans and chest X-ray images. (ii) The most frequently detected parenchymal lesion was ground glass opacity (GGO) and also bilateral lesions were the common signs of lung lesions. (iii) The lung CT scan findings in children with COVID‐19 were less severe than in adult patients.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
An epidemic of coronavirus disease (COVID-19) emerged in China in December 2019, infecting people all around the world except Antarctica, and has changed the world dramatically. Then many regions and countries have been affected globally and this disease has been regarded as pandemic [1]. According to the World Health Organization (WHO), as of July 2021, there are 190 million cumulative cases globally of which 4.9 million were reported by the end of July, and there are more than 4 million cumulative deaths by the middle of July [2]. According to statistics, the fact is that if infected cases are not isolated/treated, COVID-19 can easily spread and infect many people. Medical imaging is extremely useful for the treatment of disease and has been highly preferred during clinical trials during the pandemic process. Chest CT/X-rays [3], can play a significant supplementary role in the assessment of COVID-19 complications. Because of high precision and accessibility, chest CT scan plays a magnificent role in the identification of COVID-19 and has been recognized as the most sensitive imaging modality to detect complications [4]. The majority of patients affected with COVID-19 disease have chest CT and chest X-rays abnormality and hence researchers prefer chest CT scans and chest X-rays to be used for early detection of COVID-19 and monitoring the progression of the disease progression. Although X-rays can view only one thing at limited viewing ranges, CT scans can take multiple images in a series. Therefore, it seems when research has been examined, CT scans of the patients are more important than X-ray results [5, 6]. At the early stage of its spread, COVID-19 mostly affected adults and old people; however, children were less influenced by the COVID-19 disease. The chest CT scan approach has some risks like need for sedation, radiation effect, etc. Considering these reasons, this approach cannot be easily preferred for children. In addition, infection complication factor for viral lower respiratory tract in children is lower than in adults therefore it is hugely challenging to determine COVID-19 at the early stage. Only a few studies have investigated COVID-19 in pediatric field. However, the number of children infected is increasing. It is accepted that the majority of pediatric cases are quiescent or asymptomatic but still children get infected by COVID-19 [7] and they have suffered from this virus. Also, it is still disputed that children become heavy spreaders during this process [8]. In March, 2020 which is the first COVID-19 case was reported from Turkey, and, the COVID-19 virus continued to spread in the world. COVID-19 diagnoses of pediatric patients is much like in adults. Despite the worldwide spread, clinical patterns of COVID-19 in pediatric patients still remain largely unclear [9].
This research review is mainly about CT/X-ray imaging finding in children while highlighting the value of radiology research of COVID-19 in pediatric patients. Inspired by this limitation of the research of ML-based [10] pediatric patients of COVID-19 diagnosis, various research has been conducted between January 2021 and November 2021. The contributions of this article are as follows: (1) A comprehensive review has been done examining research based on ML techniques in COVID-19 disease and they were categorized. (2) A comparison of articles has been provided in terms of their application, author, dataset size, laboratory parameters, and study results to provide valuable insights for pediatric cases. (3) This review provides a literature base for future research and fills the gap for understanding contribution from research in 2021 on COVID-19.
2 Infection in Children
According to Pediatric Healthcare Providers, on December 30, 2020, globally fewer reports of COVID-19 have been listed in children between the ages 0–17 as with adults. 22% of the US population consists of children [11, 12]. For the Pediatric Healthcare Providers, recent data show that COVID-19 is more prevalent among children in the United States than people think [13]. In August 2021, the estimated number of patients in children in the United States appears to have increased [14]. The incidence of COVID-19 disease in children is not truly understood because of the lack of generalized reports and the prioritization of testing for adults with COVID-19 disease. Latest data indicate that compared to adults, children most probably have a very much alike viral disease, [15] and can transmit the virus to other people [16, 17]. Preliminary statistics show that children have not been affected seriously by SARS-CoV-2 and less spread the virus because most of the countries were closed school early and parents struggle to protect their children therefore researchers still investigate to not affected children during the pandemic period. On the other hand, the rapid infectious of the disease by children have a significant role in the rapid contamination of the disease among human, so early detection of COVID-19 in children will help reduce the spread in both children and adults. Also, most countries in the world entered the new normalization process in the autumn of September 2021. In this process, when most of the schools and daycares reopened, understanding transmission potential in children will be important to guide public health measures. Children’s incubation period of COVID-19 is considered the same as in adults, at 2–14 days with a standard of 6 days [18]. Signs of COVID-19 in children are as follows: cough, fever, sore throat, myalgia, abdominal pain, loss of taste, loss of smell, headache, difficulty breathing, diarrhea nausea or vomiting, and poor appetite [19]. Most children may have all signs or some of these symptoms when they are infected with COVID-19. Although these symptoms in children similar to adults are considered, lack of statistics of symptoms or originality of signs for recognition or classification COVID-19 in children is especially challenging [20].
3 Methods and Included Studies
Twelve studies are analyzed from research articles published on COVID-19 from January 2021 to November 2021 using the keywords COVID-19, children, pediatrics, SARS-CoV-2, Epidemiology, Guidelines, Audio/Speech, CT Scan, X-ray images. This research focused on clinical journal articles and case reports/series. All journal articles and case reports written in English were analyzed and criticized. Also, the preprints have been examined due to the lack of COVID-19 statistics in children.
In this section, the scope of each review such as topics, types, interests, and architecture of the study are examined. The criteria of the present review are shown in Table 1 and pediatric COVID-19 cases included in the results and nation Table 2. Among 74 children has right-sided (4.3%) or bilateral (4.3%) GGO and also feeding vessel sign, halo sign, and pleural thickening [21]. In 1156 children did biochemical tests and complete blood count and chest CT/X-ray. Among these children, 263 have (22.7%) asymptomatic, 668 have (57.7%) mild disease, 209 have (18.1%) moderate disease, and 16 have (1.5%) severe disease [22]. Among 422 children, 23 have (29.5%) asymptomatic, 45 have (56.4%) mild disease, 10 have (12.9%) moderate, 1 have (1.2%) severe, and 0% critical cases [23]. Among 148 children CT finding was classified that 52 PCR positive patients and regarding CT finding 23 PCR positive and 12 negative patients, approximately (65%) unilateral, approximately (51%) multifocal, approximately (88%) peripheral, and approximately (61%) lower lobe involvement [24]. Among 177 children, 79 have (44.6%) bone lesions, 98 have (55.4%) normal [5]. Among 40 children result for chest CT; good sensitivity, GGO sub-pleural basal, nodular consolidation not frequent, peribronchial thickening frequent, pleural effusion possible, for chest X-ray result; low sensitivity, GGO sub-pleural basal, nodular consolidation not frequent, peribronchial thickening frequent, pleural effusion possible [25]. Among 3670 children, 1026 (36\%) was normal and 798 (28%) bilateral lesions, 1054 (37%) GG0 and consolidation or pneumonic infiltrates 22% [26]. Among 24 children, 7 (33%) was normal, 8 (38%) had patchy or streaky opacity, GGO geographic, 1 (5\%) had dense opacity, 3 (14%) had bronchial wall thickening, 1 (5%) had hyperinflation, 1 (5%) had wedge-like opacity, 2 (10%) had pleural effusion [27]. Among 47 children, 37/45 (82%) had pulmonary opacities (most often bilateral and diffuse), 8/45 (18%) were normal [28]. Among 16 children, 11 (69%) demanded ICU, 10 (63%) had hypotension or shock, 7 (44%) had hypoxia, 1 (6%) had intubation and mechanical ventilation [29]. Among 16 children, 4 (25%) had typical, 8 (50%) had indeterminate, 1 (6%) was atypical, 3 (19%) had negative [30]. Among 422 children, n = 95 patients between ages are 0–19 with PCR test positive for clinical presentation. They subdivided their study group according to age groups including n = 27 patients 0–2 years of infants, n = 27 patients 3–10 years of children, and n = 41 patients 11–19 years of adolescents. 45% of pediatric patients were hospitalized, of which 20% needed acceptance to ICU. The detected abnormalities identified were 35% GGO/consolidations. Also, they remarked GGO/consolidations were more common in older people than younger people [31].
Pediatric COVID-19 cases distribution on gender and patient symptoms are given in Table 3. With 2996 (50.79%) males and 2889 (49.20%) females, the 12 eligible studies were from 3 different countries. 4 (33.33%) were from Turkey [21,22,23,24], including 2 (16.66%) from Italy [5, 25] and 6 (50%) from the US [26,27,28,29,30,31]. Among the 12 included studies, one (8.3%) was a case report [25], 10 (83.3%) were original research articles [5, 21, 22, 24, 26,27,28,29,30,31], and one (8.3%) was a brief report [5]. Except for these studies, there are 7 other studies in COVID-19 with different perspectives for pediatric cases [32,33,34,35,36,37,38,39].
4 Discussion
Many studies have focused on the fact that it is difficult to distinguish the diagnosis of COVID-19 from the diagnosis of non-COVID-19 diseases such as influenza or pneumonia. These studies have determined that various medical data (X-ray/CT images) are used for the diagnosis of COVID-19. However, since it is very difficult to understand the difference between the symptoms of COVID-19 disease and the symptoms of other diseases, it can cause misdiagnosis [39]. As a result of the misdiagnosis, many negative situations such as malpractice and wrong drug use can occur or it can cause permanent damage to patients. Hence, it is very important to have a mature, robust, and integrated system [40] that automatically detects the COVID-19 disease. It has been observed that the majority of studies in the pediatric field were conducted by researchers in the USA and Turkey. In addition, it is thought that there is an urgent need to conduct more studies on this subject.
5 Conclusion
COVID-19 is a contagious disease that has quickly endangered the health of humanity as a global pandemic. Due to this disease, this world is affected as communal, cultural, and economic. Even though COVID-19 mostly affects adults, children are affected by COVID-19 disease in many ways. This comprehensive review summarizes the clinical features of children with COVID-19 in 2021. Currently, most of the result of evidence results from studies and cases from China. However, the spread of COVID-19 disease accelerate worldwide, and because of the lack of European and US data on pediatric patients need further clinical cases to identify possible preventive scenarios. Also, it is fact that more research is still a requirement to understand how COVID-19 has affected children and to produce treatments and productive vaccines for children. In this research, the effects of COVID-19 on children in 2021 have examined, published and listed. Many children in pediatric patients have a mild course. Therefore, a balance between the risk of radiation and the vitalism for CT scan is very important.
References
WHO Director-General’s Statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV). https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov). Accessed 2021/05/01
Weekly epidemiological update on COVID-19—20 Jul 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---20-july-2021. Accessed 2021/08/01
Borakati A, Perera A, Johnson J, Sood T (2020) Diagnostic accuracy of X-ray versus CT in COVID-19: a propensity-matched database study. BMJ Open 10(11)
Sun Z, Zhang N, Li Y, Xu X (2020) A systematic review of chest imaging findings in COVID-19. Quant Imaging Med Surg 10(5):1058
Bottari G, Stellacci G, Ferorelli D, Dell’Erba A, Aricò M, Benevento M, Palladino G, Solarino B (2021) Imaging appropriateness in pediatric radiology during COVID-19 pandemic: a retrospective comparison with no COVID-19 Period. Children 8(6):463
Bai HX, Hsieh B, Xiong Z, Halsey K, Choi JW, Tran TML, Pan I, Shi LB, Wang DC, Mei J, Jiang XL, Liao WH (2020) Performance of radiologists in differentiating COVID-19 from non-COVID-19 viral pneumonia at chest CT. Radiol 296(2):E46–E54
Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P (2020) Hyperinflammatory shock in children during COVID-19 pandemic. The Lancet 395(10237):1607–1608
Cao Q, Chen YC, Chen CL, Chiu CH (2020) SARS-CoV-2 infection in children: transmission dynamics and clinical characteristics. J Formos Med Assoc 119(3):670
Jin XM, Xu X (2013) The society of pediatrics, Chinese Medical Association-an intensive training programme for developmental and behavioral pediatrics. Zhonghua er ke za zhi= Chin J Pediatr 51(11):879–880
Shi F, Wang J, Shi J, Wu Z, Wang Q, Tang Z, He K, Shi Y, Shen D (2020) Review of artificial intelligence techniques in imaging data acquisition, segmentation, and diagnosis for COVID-19. IEEE Rev Biomed Eng 14:4–15
Stokes EK, Zambrano LD, Anderson KN, Marder EP, Raz KM, Felix SEB, Tie Y, Fullerton KE (2020) Coronavirus disease 2019 case surveillance—United States, 22 Jan–30 May, 2020. Morb Mortal Wkly Rep 69(24):759
Williams N, Radia T, Harman K, Agrawal P, Cook J, Gupta A (2021) COVID-19 severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review of critically unwell children and the association with underlying comorbidities. Eur J Pediatr 180(3):689–697
U.S. Census Bureau. Quick Facts United States. https://www.census.gov/quickfacts/fact/table/US/AGE295219#AGE295219externalicon. Accessed 2021/07/01
Centers for Disease Control and Prevention. Demographic trends of COVID-19 cases and deaths in the US reported to CDC. https://www.cdc.gov/covid-data-tracker/index.html#demographics. Accessed 2021/08/01
Heald-Sargent T, Muller WJ, Zheng X, Rippe J, Patel AB, Kociolek LK (2020) Age-related differences in nasopharyngeal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) levels in patients with mild to moderate coronavirus disease 2019 (COVID-19). JAMA Pediatr 174(9):902–903
Yonker LM, Neilan AM, Bartsch Y, Patel AB, Regan J, Arya P, Gootkind E, Park G, Hardcastle M, John AS, Appleman L, Fasano A (2020) Pediatric severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): clinical presentation, infectivity, and immune responses. J Pediatr 227:45–52
Laws RL, Chancey RJ, Rabold EM, Chu VT, Lewis NM, Fajans M, Reses HE, Duca LM, Dawson P, Conners EE, Gharpure R, Kirking HL (2021) Symptoms and transmission of SARS-CoV-2 among children—Utah and Wisconsin, March–May 2020. Pediatr 147(1)
Centers for Disease Control and Prevention. COVID-19 pandemic planning scenarios. https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html#table-2. Accessed 2021/08/05
Information for Pediatric Healthcare Providers. https://www.cdc.gov/coronavirus/2019-ncov/hcp/pediatric-hcp.html. Accessed 2021/08/05
Poline J, Gaschignard J, Leblanc C, Madhi F, Foucaud E, Nattes E, Faye A, Bonacorsi S, Mariani P, Varon E, Smati-Lafarge M, Ouldali N (2021) Systematic severe acute respiratory syndrome coronavirus 2 screening at hospital admission in children: a French prospective multicenter study. Clin Infect Dis 72(12):2215–2217
Bayramoglu Z, Canıpek E, Comert RG, Gasimli N, Kaba O, Yanartaş MS, Torun SH, Somer A, Erturk SM (2021) Imaging features of pediatric COVID-19 on chest radiography and chest CT: a retrospective, single-center study. Acad Radiol 28(1):18–27
Karbuz A, Akkoc G, Demirdag TB, Ciftdogan DY, Ozer A, Cakir D, Torun SH, Kepenekli E, Erat T, Dalgic N, Ilbay S, Kara A (2021) Epidemiological, clinical, and laboratory features of children with COVID-19 in Turkey. Front Pediatr 9
Berksoy E, Kanik A, Çiçek A, Bardak Ş, Elibol P, Demir G, Yilmaz N, Nalbant T, Gökalp G, Yilmaz Çiftdoğan D (2021) Clinical and laboratory characteristics of children with SARS‐CoV‐2 infection. Pediatr Pulmonol
Kalin S, Ciraci S, Cakir D, Oysu AS, Sozeri B, Demir F, Bukte Y (2021) Evaluation of radiological findings in pediatric patients with COVID-19 in Turkey. Northern Clin Istanbul 8(4):332
Ferrero P, Piazza I (2021) Cardio-thoracic imaging and COVID-19 in the pediatric population: a narrative review. World J Radiol 13(4):94
Deville JG, Song E, Ouellette CP (2021) COVID-19: clinical manifestations and diagnosis in children
Romberg EK, Menashe SJ, Kronman MP, Tang ER, Stanescu AL, Otto RK, Otjen JP (2021) Pediatric radiologic manifestations of COVID-19. Clin Imaging 75:165–170
Fenlon Iii EP, Chen S, Ruzal-Shapiro CB, Jaramillo D, Maddocks AB (2021) Extracardiac imaging findings in COVID-19-associated multisystem inflammatory syndrome in children. Pediatr Radiol 51(5):831–839
Blumfield E, Levin TL, Kurian J, Lee EY, Liszewski MC (2021) Imaging findings in multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease (COVID-19). Am J Roentgenol 216(2):507–517
Rostad BS, Shah JH, Rostad CA, Jaggi P, Richer EJ, Linam LE, Alazraki AL, Riedesel EL, Milla SS (2021) Chest radiograph features of multisystem inflammatory syndrome in children (MIS-C) compared to pediatric COVID-19. Pediatr Radiol 51(2):231–238
Nino G, Molto J, Aguilar H, Zember J, Sanchez‐Jacob R, Diez CT, Tabrizi PR, Mohammed B, Weinstock J, Xuchen X, Kahanowitch R, Linguraru MG (2021) Chest X‐ray lung imaging features in pediatric COVID‐19 and comparison with viral lower respiratory infections in young children. Pediatr Pulmonol
Irfan O, Muttalib F, Tang K, Jiang L, Lassi ZS, Bhutta Z (2021) Clinical characteristics, treatment and outcomes of paediatric COVID-19: a systematic review and meta-analysis. Arch Dis Child 106(5):440–448
Adeyinka A, Bailey K, Pierre L, Kondamudi N (2021) COVID 19 infection: pediatric perspectives. J Am Coll Emerg Phys Open 2(1):e12375
Shuja J, Alanazi E, Alasmary W, Alashaikh A (2021) COVID-19 open source data sets: a comprehensive survey. Appl Intell 51(3):1296–1325
Mamikutty R, Aly AS, Marhazlinda J (2021) Databases selection in a systematic review of the association between anthropometric measurements and dental caries among children in Asia. Child 8(7):565
Zang ST, Han X, Cui Q, Chang Q, Wu QJ, Zhao YH (2021) Imaging characteristics of coronavirus disease 2019 (COVID-19) in pediatric cases: a systematic review and meta-analysis. Transl Pediatr 10(1):1
Trout AT, Westra SJ (2021) Imaging in support of the clinical diagnoses of COVID-19 and multisystem inflammatory syndrome in children. Pediatr Radiol 51(5):693–694
Tulchin-Francis K, Stevens Jr W, Gu X, Zhang T, Roberts H, Keller J, Dempsey D, Borchard J, Jeans K, VanPelt J (2021) The impact of the coronavirus disease 2019 pandemic on physical activity in US children. J Sport Health Sci 10(3):323–332
Bayesheva D, Boranbayeva R, Turdalina B, Fakhradiyev I, Saliev T, Tanabayeva S, Zhussupov B, Nurgozhin T (2021) COVID-19 in the paediatric population of Kazakhstan. Paediatr Int Child Health 41(1):76–82
Savaş BK, Becerikli Y (2020) Real time driver fatigue detection system based on multi-task ConNN. IEEE Access 8(1):12491–12498
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper
Savaş, B.K. (2023). A Review of a Research in 2021 on Coronavirus Disease (COVID-19) in Pediatric Patients. In: Yang, XS., Sherratt, S., Dey, N., Joshi, A. (eds) Proceedings of Seventh International Congress on Information and Communication Technology. Lecture Notes in Networks and Systems, vol 448. Springer, Singapore. https://doi.org/10.1007/978-981-19-1610-6_70
Download citation
DOI: https://doi.org/10.1007/978-981-19-1610-6_70
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-1609-0
Online ISBN: 978-981-19-1610-6
eBook Packages: EngineeringEngineering (R0)