Abstract
Infectious diseases remain an essential global challenge in public health. For instance, novel coronavirus (COVID-19) has resulted in significant negative impacts on public health, infecting more than 214 million people and causing 4.47 million deaths worldwide as of August 2021. Geographic Information Systems have played an essential role in managing, storing, analyzing, and mapping disease and related risk information. This article provides an overview of a broad topic on applications of GIS into infectious disease research. Our review follows the framework of human–environment interactions, focusing on the environmental and social factors that cause the disease outbreak and the role of humans in disease control, including public health policies and interventions such as social distancing/face covering practice and mobility modeling. The work identifies key spatial decision-making issues where GIS becomes valued in the agenda for infectious disease research and highlights the importance of adopting science-based policies to protect the public during the current and future pandemics.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Infectious disease
- COVID-19
- Geographic information system (GIS)
- Social distancing
- Spatial decision-making
- Public health policy
8.1 Introduction
Environmental pollution, disasters, urbanization, global warming, and rapid population growth have become the significant factors that cause infectious disease outbreaks [1,2,3]. Infectious diseases remain an essential global challenge in public health, causing over 13 million deaths each year. According to statistics, viral hepatitis, influenza, and tuberculosis stand among the leading causes of illness and death in the United States [4]. Since 2019, novel coronavirus (COVID-19) started to be detected from humans, which rapidly developed into a global pandemic, infecting more than 214 million people, and causing 4.47 million deaths worldwide as of August 2021 [5]. COVID-19 has changed human production and life behavior not only affected the water system, but also had a strong impact on a wider range of energy systems and food systems under the global background of high coupling of food, energy, water, and environment, and then affects the process of sustainable development of economy, society, and environment in the whole region. For the energy system, the reduction of power demand and the decline of fossil fuel use caused by the economic recession during COVID-19 have significantly reduced the carbon dioxide emissions of the global power sectors [6,7,8].
The development of computer-based geographic information systems (GIS) for integrating and analyzing spatially referenced data has provided new tools for medical geographic research on infectious disease control. Infectious diseases have revealed strong spatial patterns, where Geographic Information Systems (GISs) played a central role in managing, storing, analyzing, and mapping disease information. The Coronavirus Resource Center established by the Johns Hopkins University is one of the noteworthy examples of this practice (see https://coronavirus.jhu.edu/map.html). Disease cartography began with Koch’s work, including the spatial mapping of pandemics such as the European plague and yellow fever [9]. Later, the GIS-based disease mapping tools also leveraged many other kinds of data such as demographic, social media, and environmental data to improve disease surveillance and decision-making [10,11,12].
Spatial decision-making and spatial decision support systems have been widely discussed in the GIS research for solving real-world problems such as disaster management, environmental and water resources management, agriculture risk management, and public health surveillance [13,14,15,16,17,18,19,20,21,22]. The existing literature describing GIS-based public health applications suggests that GIS diffusion into infectious diseases research and public health practice has moved beyond the early innovation phase [23]. Such publications can be identified in an extensive range of outlets, including multidisciplinary journals on public health, environmental science, social science studies, GIS conference proceedings, and government reports. For instance, numerous COVID-19 related research articles have been published since 2019 in the journals (or proceedings) of environmental science, geography, geosciences, infectious diseases, computer science, and multidisciplinary studies. Nevertheless, it is unclear to what extent and depth GIS has been utilized in infectious disease studies. For instance, which types of infectious diseases research have attracted most GIS applications? What kinds of GIS-based methodologies have been used in analyzing infectious diseases? Some infectious diseases such as COVID-19 are highly contagious, where public health policies (e.g., social distancing), human behavior, and mobility analysis have been extensively analyzed with the help of GIS-based data and methodologies in infectious disease studies.
This review article tends to systematically review and inductively summarize the influential literature on applications of GIS into infectious disease research. Figure 8.1 illustrates the workflow of the article. Our review follows the framework of human–environment interactions, where the term “environment” represents the environmental and social factors that contribute to disease outbreak and transmission. The term “human” represents the role of humans in disease control, including public health policies and interventions such as social distancing practice and mobility modeling. This reminder of this review paper is structured into the following sections. Section 8.2 systemically reviewed and summarized the typical applications of four types of GIS techniques in infectious disease-related research, including spatial clustering and statistics, spatial interpolation, WebGIS and spatial visualization, and spatial modeling. In Sect. 8.3, we conducted an in-depth review of COVID-19 related research works. We paid particular attention to an emerging geographic data source—fine-grained mobility data, reviewed, and summarized the existing efforts about how to use mobility data to assess different COVID-19 protective measures (e.g., social distancing) and how to use mobility data to facilitate decision-making during different stages of the pandemic.
8.2 Environmental Distribution of Infectious Disease and GIS-Related Research
This article first developed a search strategy with terms relating to “GIS/Geographic Information Systems” and “Infectious Disease.” This search was developed through an iterative process of incorporating new terms and refining those included based on results returned and identification of relevant citations. We conducted an electronic search on the Web of Science database with no restriction on the date or language of publication. We found 1944 peer-reviewed articles that focus on infectious disease and involved GIS or spatial analysis. Figure 8.2 illustrates the number of identified articles by different publishers, with Springer Nature publishing the most GIS-related infectious disease research, followed by Elsevier and Willey.
In the next step, we used the keyword “GIS” combined with different types of infectious disease keywords such as “HIV,” “Influenza,” and “COVID-19” to group the articles by different disease types. Table 8.1 illustrates the number of articles (with their corresponding citations) that applied GIS and spatial analysis for each type of infectious disease. According to Table 8.1, Malaria, COVID-19, and Human Immunodeficiency Virus (HIV) are the top three diseases that mostly utilized GIS and spatial analysis in their relevant research works.
8.2.1 Use of Spatial Clustering and Spatial Statistics in Identifying Disease Hotspots
Spatial clustering and spatial statistics are two of the mostly used spatial analysis techniques for evaluating infectious diseases’ geographic distribution (see Table 8.2). In this section, we searched for articles with keywords “infectious disease,” “GIS,” and “spatial clustering and statistics” in the Web of Science database. Results have returned with 49 articles. We removed duplicated and un-relevant articles and selected ten articles for analysis. Spatial clustering is used to partition spatial data (e.g., disease data) into a series of meaningful subclasses called spatial clusters, where spatial objects that are within the same cluster are similar to each other [36]. Spatial autocorrelation is often used in the GIS to identify how well objects correlate with other nearby objects across a spatial area [36]. As listed in Table 8.2, spatial autocorrelation was used in five articles for studying the spatial distribution of Hepatitis, Tuberculosis, HIV, Mumps, and SARS diseases. Spatial clustering methods such as Kulldorff’s spatial scan and self-organizing maps were used in seven articles. In these articles, the spatial scan statistic identified statistically significant hotspots based on the number of disease cases by systematically scanning circular windows using varying sizes across the study area [26,27,28]. A space-time scan was used to test the statistically significant clusters of the disease cases across space and time [35]. Other spatial statistical models such as Local Moran’s I are global clustering statistics that measure the tendency for points to occur closer together in space by chance across the entire study area [25, 31]. In contrast, the Kulldorff spatial scan statistic identifies local clusters in a particular region. Local clusters can exist in either the absence or presence of global clustering [26, 27].
8.2.2 Use of Spatial Interpolation in Estimating Disease Pattern
Another focused area of using GIS technology in infectious disease mapping is to create “heat maps’‘using data gathered in a limited number of locations to estimate values in unmeasured locations. Spatial interpolation is the process of using points with known values to estimate values at other points [36]. Traditional spatial interpolation methods include kriging interpolation, trend surface interpolation, and inverse distance weighted interpolation. As illustrated in Table 8.3, the kriging interpolation method has been used in six articles studying Burkholderia Pseudomallei, foot-and-mouth disease, norovirus, Tuberculosis, rotavirus, and influenza-like illness. Inverse distance weighted interpolation was used in four articles studying Malaria, Tuberculosis, Kala-azar disease, and Hepatitis. In these articles, spatial interpolation methods were often combined with spatial statistics to analyze spatial transmission patterns of infectious disease ([37, 40];). Spatial interpolation is often used to convert discrete data into continuous data for comparison with the spatial trend of infectious diseases [44, 45]. Others may consider spatial interpolation as a data processing method for spatial analysis [39, 40].
8.2.3 Spatial Visualization and Web-Based GIS Dashboard
With the advancement of web-based technologies (e.g., ArcGIS online), various web-based GIS platforms have been developed to visualize the infectious disease risks at different space-time scale. Some of the well-known dashboards include the WHO Coronavirus dashboard [46], John Hopkins University COVID-19 dashboard [47], the UK National Health Service (NHS) COVID-19 app [48], and CDC COVID-19 data tracker [5]. Spatial interpolation methods have often been combined with web-based geovisualization tools to predict the infectious disease spread patterns [37, 44, 45]. WebGIS and ESRI products such as ArcGIS dashboard are commonly used technology for geographical data sharing, visualizing [49]. WebGIS techniques were used in three articles for establishing visualization platforms [50, 51]. Google Maps were used in two articles for visualizing infectious disease information [50, 51]. As one of the most representative WebGIS platforms, ArcGIS Online provides various mapping and analysis functions, geographic data sources, and web-based applications, allowing users to effectively build up web applications without coding. Meanwhile, it also provides different GIS tools and APIs used by developers while it is not as functional as ArcGIS Desktop. The Google Maps API provides embedded Google Maps into web pages through JavaScript. The APIs provide many utilities to generate maps and customize the map content by adding additional information services. However, these APIs do not support complicated analysis functions. Table 8.4 illustrates selected articles that have used WebGIS techniques and geovisualization in infectious disease monitoring.
8.2.4 Exploring Environmental and Social Factors Using Spatial Regression Analysis
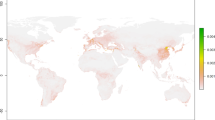
Several articles are focused on investigating the key factors that affect the occurrence and spread of infectious diseases. Geographically Weighted Regression (GWR) has a high utility in epidemiology, particularly for examining the relationship between the spread of infectious disease with different social, political, and environmental factors (e.g., built environment, health policies, and interventions). GWR is a local form of linear regression used to model spatially varying relationships [57]. Table 8.5 illustrates the key social and environmental factors that have been explored in infectious disease research. According to Table 8.5, environmental factors such as temperature, humidity, precipitation, wind speed, air pressure, altitude, and socioeconomic factors such as child population density and per capita Gross Domestic Product (GDP) are associated with Hand, Foot, and Mouth Disease (HFMD). Other environmental factors such as air pollution, brickfield density, land use, and public transportation facilities significantly impact on COVID-19 cases. Other sociodemographic factors such as gender, nationality, employment status, and occupation types are associated with malaria and tuberculosis.
8.3 Human-Centered Efforts to Address COVID-19 Challenges
Novel coronavirus (COVID-19) has significant negative impacts on public health, infecting more than 214 million people and causing 4.47 million deaths worldwide as of August 2021. The COVID-19 pandemic is much more pronounced than many of the previous outbreaks of infectious diseases, including the 2002/2003 SARS. The enormous scope and magnitude of the COVID-19 outbreak reflects a highly contagious nature and exceedingly efficient transmission for SARS-CoV-2. There exists two primary pathways for respiratory viruses to be transmitted from person to person (Fig. 8.3a). Virus-bearing particles are produced from breathing, talking, coughing, or sneezing by an infected person. Interhuman transmission occurs by the direct (deposited on persons) or indirect (deposited on objects) contact route via respiratory droplets (>5 μm) or the airborne route via respiratory aerosols (<5 μm). While large respiratory droplets readily settle out of air to cause person/object contamination, small virial-bearing respiratory aerosols are efficiently dispersed in air and inhaled by human to lead direct deposition along the respiratory tract and to cause infection [13, 14, 19]. Well-established public health measures to prevent interhuman transmission include face covering, social distancing, and testing/quarantine (Fig. 8.3b). There exists now compelling scientific evidence for the importance of airborne transmission in spreading the COVID-19 disease and face covering in preventing interhuman [11, 13, 14, 19]. Also, increasing ventilation in an enclosed community setting has been shown to effectively reduce viral transmission [66]. Vaccination is commonly believed to mitigate viral transmission, albeit for the occurrence of break-through infections [67]. The effectiveness of vaccination has been clearly documented to significantly reduce hospitalization, severe syndromes, and mortality [68].
Transmission, science-based intervention, and application of GIS. (a) Illustration of viral transmission routes (adopted from Zhang et al. 2020). (b) Mitigation for preventing interhuman transmission and the application of GIS in decision-making. The boxes denote mitigation measures, and the circles depict the disease evolution
As the COVID-19 outbreak grew to an epidemic, and various GIS systems have been developed and implemented, leading the response to COVID-19 in many ways. For instance, Johns Hopkins University launched its COVID-19 dashboard using ESRI technology [47]. So far, social distancing plays an important role in controlling the spread of coronavirus. Governments issued different level of restrictions on traveling, institutions canceled gatherings, and citizens socially distanced themselves to limit the spread of the virus. Social distancing measures have significantly influenced the mobility patterns, which have been widely discussed in various COVID-19 related GIS applications. On the other hand, those literature are also tightly related to public health policy and social equity issues, which are worthy of future research. This article illustrates the key findings of using GIS in mobility and policy analysis during the COVID-19 pandemic. We structured our reviews by different stages of pandemic control, i.e., early stage, controlling stage, reopening stage, and post-pandemic recovering stage. We found 228 articles related to the topic. In the following four subsections, we discuss human-centered efforts that leverage mobility data in addressing COVID-19-related challenges.
8.3.1 Early in the Pandemic: Contact Tracing and Initial Control
At the early stage of the COVID-19 pandemic, location-based intelligence has been widely adopted to provide situational awareness for policy-makers and researchers. Human mobility records retrieved from cell phone users’ location data (by way of GPS, cell phone towers, and/or Wi-Fi), electronic wristbands, credit card transactions, and closed-circuit television (CCTV) systems can assist in tracking disease spread and enforcing social isolation measures [69]. In China, Alipay and WeChat, two big providers of mobile payment systems, released apps that combine users’ health, location, and financial data to generate a personal infection risk rating [70]. Other government-backed apps were also used in the early stage of the pandemic to collect users’ essential information, and necessary user scanning was required at checkpoints to better gauge people’s moving patterns. Besides efforts and guidelines by the officials, crowdsourcing efforts are also popular, as citizens themselves can contribute to contact tracing and surveillance by voluntarily sharing their whereabouts online. For instance, Private Kit (https://privatekit.mit.edu/), released by the Massachusetts Institute of Technology, is a crowdsourcing application that stores GPS location records from users every 5 min for up to 28 days. Users have the option to share their location data and notify health officials if they test positive for COVID-19. Numerous studies have proved that human mobility records with fine spatiotemporal granularity are essential for disease spread control, as reconstructed trajectories of individuals who have been tested positive can be used to alert those who may have been put at risk of infection [71, 72]. Zhang et al. [13, 14, 19] studied the relationship between human mobility and the cross-space infection in the early stage of the pandemic, based on which a variety of counterfactual analyses is developed to examine the necessity of lock-down and the other containment approaches.
8.3.2 During Control Measures: Compliance Monitoring
To contain the COVID-19 pandemic, one of the non-pharmacological epidemic control measures is to reduce the transmission rate of SARS-COV-2 in the population via social distancing or other similar quarantine measures [11, 73]. Besides the proof from epidemiologic simulations, many pieces of evidence have been found in numerous studies that the implementation of mobility-restricting measures is responsible for the declined transmission rates (e.g., [74, 75]). In certain cases, however, different countries, states/provinces, counties/towns, and other administrative units choose to handle COVID-19 in different ways, with great disparity in the implementation of policies and guidelines. Even in regions under the same level of restrictions, disparities in compliance tend to occur. Human mobility records, either at the individual level or aggregated to certain geographic units, can reflect how people adjust their travel patterns under the COVID-19 pandemic and whether policies are implemented in an effective manner. There are some notable efforts that Huang et al. [76] analyzed over 580 million tweets worldwide to investigate how people follow mobility-restricting measures at the global, country, and U.S. state levels. Their results revealed great discrepancies in responsiveness, evidenced by the contrasting mobility patterns in different epidemic phases at their investigated scales. Taking advantage of Google’s COVID-19 mobility reports, Bargain and Aminjonov [77] investigated how policy compliance is linked with political trust at the regional level in Europe. Their findings indicate that high-trust regions decrease their mobility significantly more than low-trust regions, and the efficiency of policy stringency in terms of mobility reduction significantly increases with trust. Other efforts coupled mobility-related indices with sociodemographic factors, aiming to reveal the determinants that potentially lead to the disparity in policy compliance (e.g., [78]; Chiou and Tucker). The general findings point to the luxury nature of mobility-restricting measures (e.g., working from home and other virtual working conditions) with which socioeconomically disadvantaged groups cannot afford to comply. Zhu et al. [79] utilized network optimization to identify how the geographical centers of the pandemic moved spatially over time across the USA in the context of various intervention policies. The pandemic has also witnessed much mis- and dis-information. Network reconstruction methods can be employed to measure the interaction between the information diffusion and the outbreak of COVID-19 across space, and identify both positive and negative impact of information on the pandemic [12, 15]. The above evidence reveals the essential role of mobility data in policy compliance monitoring during the COVID-19 pandemic, which benefits further policymaking in terms of adjusting controlling measures and mitigating compliance disparity.
8.3.3 Reopening: When, How, and Where
After the implementation of mobility-restricting measures, federal and local government officials have been investigating reopening strategies, such as when and where to reopen borders and business, and how much activities are allowed in certain places. These reopening strategies, however, should be determined in a scientific manner with the assistance of epidemiological models that consider human mobility dynamics. Many studies have been conducted to assist in reopening decision-making taking advantage of fine-grained human mobility data. One notable effort is by Chang et al. [80], who built enormous mobility networks containing 5.4 billion hourly edges from mobile phone data that cover hourly movements of 98 million people from 56,945 U.S. census block groups to 552,758 points of interest (POIs). The results suggested that, coupled with detailed mobility records, their simulation can estimate the effects of specific reopening strategies in the USA. Using the same dataset, Andersen et al. [81] examined U.S. college reopenings’ association with changes in human mobility within campuses and in COVID-19 incidence in the U.S. counties of the campuses over a 10-week period around college reopenings. They found that college reopenings were associated with increased campus mobility, responsible for the increased COVID-19 incidence by 2.7 cases per 100,000. Xiong et al. [82] investigated the partial reopening phases in the USA by leveraging anonymized mobile device location data from over 100 million monthly active users procured from multiple third-party data providers. The detailed mobility records coupled with their models revealed the high likelihood of a second spike in coronavirus in many early-opening regions. The above examples highlight the necessity of human mobility data in optimizing reopening decisions.
8.3.4 Post-Pandemic: Recovery and Transition Gauging
Human mobility data can be used to tell stories regarding how different regions recover after the lifting of strict mobility-restricting orders and the implementation of reopening policies by comparing the human moving patterns in post-pandemic situations to the ones in pre-pandemic situations. While some of the changes are temporary, such as the disruptive social, physical, and economic activities in urban and rural landscapes during the stay-at-home orders (most of which have largely recovered after the reopening), others seem to be permanent impacts that force multiperspective transitions in an irreversible manner. Human mobility data that cover multiple stages are expected to benefit the investigation of the dynamic, intertwining, long-term societal effects of the COVID-19 pandemic, filling the knowledge gaps in our understanding of how spatial and social interactions have shifted and transitioned in the post-pandemic world, and informing better adapting, responding, and recovering strategies that reduce inequalities and vulnerabilities. Despite the fact that it is difficult to decide when the post-pandemic era really starts, numerous efforts have been made to gauge recovery and transition when society functions resume. Kupfer et al. [83] investigated park visitation recovery by mapping and analyzing the spatiotemporal patterns of visitation for six national parks in the western USA, taking advantage of large mobility records sampled from mobile devices and released by SafeGraph as part of their Social Distancing Metric dataset. Huang et al. [78] leveraged multi-source mobility datasets from Google, Apple, Descartes Labs, and Twitter to investigate how people reduced their travels during the mobility-restricting period and how mobility recovered after the reopening at the county level in the USA. Their results revealed a great disparity in mobility dynamics in the recovery phase, as the poor countries tended to gain earlier and greater upward momentum than the wealthy counties. Such disparity in recovery has been noted by many studies that take advantage of mobility records (e.g., [76, 83]).
8.4 Conclusion and Discussion
Adopting science-based policies are paramount in protecting the public during the current and future pandemics. This article provides an overview and a summary on applying applications of GIS into infectious disease research, and application of GIS tools for analyzing and maintaining COVID-19. We paid special attention to COVID-19 related research in terms of human-environment interactions. The term “human” represents the role of humans in disease control, including public health policies such as social distancing practice and mobility modeling. A total of 1944 peer-reviewed GIS-based infectious disease research articles were identified, where Springer Nature published the most articles, followed by Elsevier and Willey. Spatial analysis methods such as spatial clustering, spatial statistics, and spatial interpolation (e.g., Kriging), and GWR analysis have been discussed in detail in those articles to demonstrate the important value of using GIS and spatial analysis in infectious disease monitoring. The article also provides the summary of web-based portals (e.g., GIS dashboards) in visualizing infectious disease risks.
The article also includes a review on human-centered methods for COVID-19 research, including the analysis of social distancing and mobility in COVID-19 disease control and policymaking. We structured this section by different pandemic stages, including early-pandemic, under strong control measures, reopening, and post-pandemic recovery. In the early stage, several articles discussed using human mobility records derived from emerging geo-data sources (e.g., cell phone location data, electronic wristbands, credit card transactions, and closed-circuit television (CCTV) to assist in tracking disease spread and enforcing social isolation measures. In the disease controlling stage, much evidence has been found that the implementation of mobility-restricting measures is responsible for the declined transmission rates. Later in the reopening and recovery stages, human mobility data has demonstrated effectiveness in determining how different regions recover after lifting social distancing orders by comparing the human moving patterns in post-pandemic situations to those in pre-pandemic situations.
According to the literature review performed in this study, GIS has been frequently used to prevent and control of infectious diseases to facilitate the appropriate spatial decision-making. By identifying spatial hot spots/patterns and potential risk factors of infectious diseases as well as vulnerable populations, the governmental and public health agencies, health care organizations, and other stakeholders, can put more efforts and resources into those regions and develop effective prevention strategies and mitigation actions. Furthermore, spatiotemporal disease modeling (e.g., Geographically and Temporally Weighted Regression) could also advance the understanding of spatiotemporal variation characteristics of the environmental and sociodemographic factors on the disease incidence and prevalence. Leveraging GIS techniques in COVID-19 research may produce broad impacts in spatial decision-making such as health care facility planning, public health policymaking, business intelligence, and health equity solutions.
References
Ge L, Zhao Y, Sheng Z, Wang N, Zhou K, Mu X, Guo L, Wang T, Yang Z, Huo X (2016) Construction of a seasonal difference-geographically and temporally weighted regression (SD-GTWR) model and comparative analysis with GWR-based models for hemorrhagic fever with renal syndrome (HFRS) in Hubei Province (China). Int J Environ Res Public Health 13(11):1062
Hassan MS, Bhuiyan MAH, Tareq F, Bodrud-Doza M, Tanu SM, Rabbani KA (2021) Relationship between COVID-19 infection rates and air pollution, geo-meteorological, and social parameters. Environ Monit Assess 193(1):1–20
Sun J, Wu S, Yan Z, Li Y, Yan C, Zhang F, Liu R, Du Z (2021) Using geographically weighted regression to study the seasonal influence of potential risk factors on the incidence of HFMD on the Chinese mainland. ISPRS Int J Geo Inf 10(7):448
ODPHP (Office of Disease Prevention and Health Promotion) (2021) Immunization and infectious diseases. https://www.healthypeople.gov/node/3527/data-
CDC (2021) COVID data tracker. https://covid.cdc.gov/covid-data-tracker/#datatracker-home. Accessed 31 Aug 2021
Forster PM, Forster HI, Evans MJ, Gidden MJ, Jones CD, Keller CA, Lamboll RD, Quéré CL, Rogelj J, Rosen D, Schleussner C, Richardson TB, Smith CJ, Turnock ST (2020) Current and future global climate impacts resulting from COVID-19. Nat Clim Chang 10(10):913–919
Le Quéré C, Peters GP, Friedlingstein P, Andrew RM, Canadell JG, Davis SJ, Jackson RB, Jones MW (2021) Fossil CO2 emissions in the post-COVID-19 era. Nat Clim Chang 11(3):197–199
Shan Y, Ou J, Wang D, Zeng Z, Zhang S, Guan D, Hubacek K (2021) Impacts of COVID-19 and fiscal stimuli on global emissions and the Paris agreement. Nat Clim Change 11(3):200–206. https://doi.org/10.1038/s41558-020-00977-5
Koch T, Koch T (2005) Cartographies of disease: maps, mapping, and medicine. Esri Press, Redlands, CA, p 840
Gao S, Mioc D, Anton F, Yi X, Coleman DJ (2008) Online GIS services for mapping and sharing disease information. Int J Health Geogr 7(1):1–12
Li Y, Zhang R, Zhao J, Molina MJ (2020) Understanding transmission and intervention for the COVID-19 pandemic in the United States. Sci Total Environ 748:141560. https://doi.org/10.1016/j.scitotenv.2020.141560
Ye X, Du J, Gong X, Na S, Li W, Kudva S (2021) Geospatial and semantic mapping platform for massive COVID-19 scientific publication search. J Geovisualiz Spatial Anal 5(1):1–12
Zhang R, Li Y, Zhang AL, Wang Y, Molina MJ (2020) Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc Natl Acad Sci U S A 117:14857–14863. https://doi.org/10.1073/pnas.2009637117
Zhang X, Ji Z, Zheng Y, Ye X, Li D (2020) Evaluating the effect of city lock-down on controlling COVID-19 propagation through deep learning and network science models. Cities 107:102869
Zhang X, Zhang ZK, Wang W, Hou D, Xu J, Ye X, Li S (2021) Multiplex network reconstruction for the coupled spatial diffusion of infodemic and pandemic of COVID-19. Int J Dig Earth 14(4):401–423
Zhang Z, Demšar U, Rantala J, Virrantaus K (2014) A fuzzy multiple-attribute decision-making modelling for vulnerability analysis on the basis of population information for disaster management. Int J Geogr Inf Sci 28(9):1922–1939
Zhang Z, Demšar U, Wang S, Virrantaus K (2018) A spatial fuzzy influence diagram for modelling spatial objects’ dependencies: a case study on tree-related electric outages. Int J Geogr Inf Sci 32(2):349–366
Zhang Z, Hu H, Yin D, Kashem S, Li R, Cai H et al (2018) A cyberGIS-enabled multi-criteria spatial decision support system: a case study on flood emergency management. Int J Dig Earth
Zhang Z, Laakso T, Wang Z, Pulkkinen S, Ahopelto S, Virrantaus K et al (2020) Comparative study of AI-based methods—application of analyzing inflow and infiltration in sanitary sewer subcatchments. Sustainability 12(15):6254
Zhang Z, Zou L, Li W, Usery L, Albrecht J, Armstrong M (2021) Cyberinfrastructure and intelligent spatial decision support systems. Trans GIS 25(4):1651–1653
Zhang Z, Yin D, Virrantaus K, Ye X, Wang S (2021) Modeling human activity dynamics: an object-class oriented space–time composite model based on social media and urban infrastructure data. Computat Urban Sci 1(1):1–13
Zhao J, Zhang Z, Sullivan CJ (2019) Identifying anomalous nuclear radioactive sources using Poisson kriging and mobile sensor networks. PLoS One 14(5):e0216131
Cromley EK, McLafferty SL (2011) GIS and public health. Guilford Press, New York
Stopka TJ, Goulart MA, Meyers DJ, Hutcheson M, Barton K, Onofrey S, Church D, Donahue A, Chui KK (2017) Identifying and characterizing hepatitis C virus hotspots in Massachusetts: a spatial epidemiological approach. BMC Infect Dis 17(1):1–11
Rao HX, Zhang X, Zhao L, Yu J, Ren W, Zhang XL, Ma YC, Shi Y, Ma BZ, Wang X, Wei Z (2016) Spatial transmission and meteorological determinants of tuberculosis incidence in Qinghai Province, China: a spatial clustering panel analysis. Infect Dis Poverty 5(1):1–13
Gwitira I, Mukonoweshuro M, Mapako G, Shekede MD, Chirenda J, Mberikunashe J (2020) Spatial and spatio-temporal analysis of malaria cases in Zimbabwe. Infect Dis Poverty 9(1):1–14
Gwitira I, Murwira A, Mberikunashe J, Masocha M (2018) Spatial overlaps in the distribution of HIV/AIDS and malaria in Zimbabwe. BMC Infect Dis 18(1):1–10
Aturinde A, Farnaghi M, Pilesjö P, Mansourian A (2019) Spatial analysis of HIV-TB co-clustering in Uganda. BMC Infect Dis 19(1):1–10
Yu G, Yang R, Wei Y, Yu D, Zhai W, Cai J, Long B, Chen S, Tang J, Zhong G, Qin J (2018) Spatial, temporal, and spatiotemporal analysis of mumps in Guangxi Province, China, 2005–2016. BMC Infect Dis 18(1):1–13
Lai PC, Wong CM, Hedley AJ, Lo SV, Leung PY, Kong J, Leung GM (2004) Understanding the spatial clustering of severe acute respiratory syndrome (SARS) in Hong Kong. Environ Health Perspect 112(15):1550–1556
Lee SS, Wong NS (2011) The clustering and transmission dynamics of pandemic influenza A (H1N1) 2009 cases in Hong Kong. J Infect 63(4):274–280
Lantos PM, Nigrovic LE, Auwaerter PG, Fowler VG Jr, Ruffin F, Brinkerhoff RJ, Reber J, Williams C, Broyhill J, Pan WK, Gaines DN (2015) Geographic expansion of Lyme disease in the southeastern United States, 2000–2014. Open Forum Infect Dis 2(4):ofv143. Oxford University Press
Yang AC, Wen TH, Shih CC, Fang CT (2011) Differentiating geographic patterns of human immunodeficiency virus (HIV) infection with different risk factors in northern Taiwan: 1997–2008. Appl Geogr 31(2):519–524
Basara HG, Yuan M (2008) Community health assessment using self-organizing maps and geographic information systems. Int J Health Geogr 7(1):1–8
Dong W, Yang K, Xu Q, Liu L, Chen J (2017) Spatio-temporal pattern analysis for evaluation of the spread of human infections with avian influenza a (H7N9) virus in China, 2013–2014. BMC Infect Dis 17(1):1–13
Longley PA, Goodchild MF, Maguire DJ, Rhind DW (2005) Geographic information systems and science. John Wiley & Sons, London
Saengnill W, Charoenjit K, Hrimpeng K, Jittimanee J (2020) Mapping the probability of detecting Burkholderia pseudomallei in rural rice paddy soil based on indicator kriging and spatial soil factor analysis. Trans R Soc Trop Med Hyg 114(7):521–530
Perez AM (2004) Probability co-kriging estimation of foot and mouth disease spatial distribution in Pakistan. GISVET’s 43
Siya A, Kalule BJ, Ssentongo B, Lukwa AT, Egeru A (2020) Malaria patterns across altitudinal zones of mount Elgon following intensified control and prevention programs in Uganda. BMC Infect Dis 20(1):1–16
Bhunia GS, Kesari S, Chatterjee N, Kumar V, Das P (2013) Spatial and temporal variation and hotspot detection of kala-azar disease in Vaishali district (Bihar), India. BMC Infect Dis 13(1):1–12
Liu K, Cai J, Wang S, Wu Z, Li L, Jiang T, Chen B, Cai G, Jiang Z, Chen Y, Wang Z (2016) Identification of distribution characteristics and epidemic trends of hepatitis E in Zhejiang Province, China from 2007 to 2012. Sci Rep 6(1):1–11
Inaida S, Shobugawa Y, Matsuno S, Saito R, Suzuki H (2013) The south to north variation of norovirus epidemics from 2006–07 to 2008–09 in Japan. PLoS One 8(8):e71696
Ding P, Li X, Jia Z, Lu Z (2017) Multidrug-resistant tuberculosis (MDR-TB) disease burden in China: a systematic review and spatio-temporal analysis. BMC Infect Dis 17(1):1–29
Török TJ, Kilgore PE, Clarke MJ, Holman RC, Bresee JS, Glass RI (1997) Visualizing geographic and temporal trends in rotavirus activity in the United States, 1991 to 1996. Pediatr Infect Dis J 16(10):941–946
Sakai T, Suzuki H, Sasaki A, Saito R, Tanabe N, Taniguchi K (2004) Geographic and temporal trends in influenzalike illness, Japan, 1992–1999. Emerg Infect Dis 10(10):1822
World Health Organization (2021) WHO coronavirus dashboard. https://covid19.who.int. Accessed 31 Aug 2021
Johns Hopkins University Center for Systems Science and Engineering (2021) Covid-19 dashboard. https://coronavirus.jhu.edu/map.html. Accessed 31 Aug 2021
NHS (2021) NHS COVID-19 app. https://covid19.nhs.uk. Accessed 1 Sept 2021
Alesheikh AA, Helali H, Behroz HA (2002) Web GIS: technologies and its applications. In Symposium on geospatial theory, processing and applications (Vol. 15)
Li YP, Fang LQ, Gao SQ, Wang Z, Gao HW, Liu P, Wang ZR, Li YL, Zhu XG, Li XL, Xu B (2013) Decision support system for the response to infectious disease emergencies based on WebGIS and mobile services in China. PLoS One 8(1):e54842
Yang K, Sun LP, Huang YX, Yang GJ, Wu F, Hang DR, Li W, Zhang JF, Liang YS, Zhou XN (2012) A real-time platform for monitoring schistosomiasis transmission supported by Google earth and a web-based geographical information system. Geospat Health 6(2):195–203
Lu X (2009) Web GIS based information visualization for infectious disease prevention. In 2009 Third International Symposium on Intelligent Information Technology Application (Vol. 1, pp. 148–151). IEEE
Al Manir MS, Brenas JH, Baker CJ, Shaban-Nejad A (2018) A surveillance infrastructure for malaria analytics: provisioning data access and preservation of interoperability. JMIR Public Health Surveill 4(2):e10218
Patrick R, Greenberg A, Magnus M, Opoku J, Kharfen M, Kuo I (2017) Development of an HIV testing dashboard to complement the HIV care continuum among MSM, PWID, and heterosexuals in Washington, DC, 2007–2015. J Acquir Immune Defic Syndr 75(Suppl 3):S397
Cheng CK, Ip DK, Cowling BJ, Ho LM, Leung GM, Lau EH (2011) Digital dashboard design using multiple data streams for disease surveillance with influenza surveillance as an example. J Med Internet Res 13(4):e85
Ravinder R, Singh S, Bishnoi S, Jan A, Sharma A, Kodamana H, Krishnan NA (2020) An adaptive, interacting, cluster-based model for predicting the transmission dynamics of COVID-19. Heliyon 6(12):e05722
Jiang H, Hu H, Li B, Zhang Z, Wang S, Lin T (2021) Understanding the non-stationary relationships between corn yields and meteorology via a spatiotemporally varying coefficient model. Agric For Meteorol 301:108340
Wu X, Zhang J (2021) Exploration of spatial-temporal varying impacts on COVID-19 cumulative case in Texas using geographically weighted regression (GWR). Environ Sci Pollut Res:1–15
Hong Z, Mei C, Wang H, Du W (2021) Spatiotemporal effects of climate factors on childhood hand, foot, and mouth disease: a case study using mixed geographically and temporally weighted regression models. Int J Geogr Inf Sci:1–23
Hu B, Qiu W, Xu C, Wang J (2020) Integration of a Kalman filter in the geographically weighted regression for modeling the transmission of hand, foot and mouth disease. BMC Public Health 20(1):1–15
Dong W, Yang P, Liao H, Wang X, Wang Q (2016) The effects of weather factors on hand, foot and mouth disease in Beijing. Sci Rep 6(1):1–9
Hu M, Li Z, Wang J, Jia L, Liao Y, Lai S, Guo Y, Zhao D, Yang W (2012) Determinants of the incidence of hand, foot and mouth disease in China using geographically weighted regression models. PLoS One 7(6):e38978
Yang D, Xu C, Wang J, Zhao Y (2017) Spatiotemporal epidemic characteristics and risk factor analysis of malaria in Yunnan Province, China. BMC Public Health 17(1):1–10
Lak A, Sharifi A, Badr S, Zali A, Maher A, Mostafavi E, Khalili D (2021) Spatio-temporal patterns of the COVID-19 pandemic, and place-based influential factors at the neighborhood scale in Tehran. Sustain Cities Soc:103034
Mohidem NA, Osman M, Hashim Z, Muharam FM, Mohd Elias S, Shaharudin R (2021) Association of sociodemographic and environmental factors with spatial distribution of tuberculosis cases in Gombak, Selangor, Malaysia. PLoS One 16(6):e0252146
Bazant MZ, Bush WM (2021) A guideline to limit indoor airborne transmission of COVID-19. Proc Natl Acad Sci U S A 118(17):e2018995118. https://doi.org/10.1073/pnas.2018995118
Fowlkes A, Gaglani M, Groover K, Thiese MS, Tyner H, Ellingson K (2021) Effectiveness of COVID-19 vaccines in preventing SARS-CoV-2 infection among frontline workers before and during B.1.617.2 (Delta) variant predominance — eight U.S. Locations, December 2020–August 2021. MMWR Morb Mortal Wkly Rep 70:1167–1169. https://doi.org/10.15585/mmwr.mm7034e4
Tregoning JS, Flight KE, Higham SL, Wang Z, Pierce BF (2021) Progress of the COVID-19 vaccine effort: viruses, vaccines and variants versus efficacy, effectiveness and escape. Nat Rev Immunol. https://doi.org/10.1038/s41577-021-00592-1
Rosenkrantz L, Schuurman N, Bell N, Amram O (2021) The need for GIScience in mapping COVID-19. Health Place 67:102389
Calvo RA, Deterding S, Ryan RM (2020) Health surveillance during covid-19 pandemic. BMJ:369
Colizza V, Grill E, Mikolajczyk R, Cattuto C, Kucharski A, Riley S, Kendall M, Lythgoe K, Bonsall D, Wymant C, Abeler-Dörner L (2021) Time to evaluate COVID-19 contact-tracing apps. Nat Med 27(3):361–362
Li J, Guo X (2020) COVID-19 contact-tracing apps: a survey on the global deployment and challenges. arXiv preprint arXiv:2005.03599
Huang X, Li Z, Lu J, Wang S, Wei H, Chen B (2020) Time-series clustering for home dwell time during COVID-19: what can we learn from it? ISPRS Int J Geo Inf 9(11):675
Hadjidemetriou GM, Sasidharan M, Kouyialis G, Parlikad AK (2020) The impact of government measures and human mobility trend on COVID-19 related deaths in the UK. Transport Res Interdisc Perspect 6:100167
Kraemer MU, Yang CH, Gutierrez B, Wu CH, Klein B, Pigott DM, Du Plessis L, Faria NR, Li R, Hanage WP, Brownstein JS (2020) The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 368(6490):493–497
Huang X, Li Z, Jiang Y, Li X, Porter D (2020) Twitter reveals human mobility dynamics during the COVID-19 pandemic. PLoS One 15(11):e0241957
Bargain O, Aminjonov U (2020) Trust and compliance to public health policies in times of COVID-19. J Public Econ 192:104316
Huang X, Li Z, Jiang Y, Ye X, Deng C, Zhang J, Li X (2021) The characteristics of multi-source mobility datasets and how they reveal the luxury nature of social distancing in the US during the COVID-19 pandemic. Int J Dig Earth 14(4):424–442
Zhu D, Ye X, Manson S (2021) Revealing the spatial shifting pattern of COVID-19 pandemic in the United States. Sci Rep 11(1):1–9
Chang S, Pierson E, Koh PW, Gerardin J, Redbird B, Grusky D, Leskovec J (2021) Mobility network models of COVID-19 explain inequities and inform reopening. Nature 589(7840):82–87
Andersen MS, Bento AI, Basu A, Marsicano C, Simon K (2021) College openings, mobility, and the incidence of COVID-19 cases. medRxiv:2020–2009
Xiong C, Hu S, Yang M, Luo W, Zhang L (2020) Mobile device data reveal the dynamics in a positive relationship between human mobility and COVID-19 infections. Proc Natl Acad Sci U S A 117(44):27087–27089
Kupfer JA, Li Z, Ning H, Huang X (2021) Using Mobile device data to track the effects of the COVID-19 pandemic on spatiotemporal patterns of National Park Visitation. Sustainability 13(16):9366
Acknowledgments
This work was supported by the COVID-19 Research Projects of West China Hospital Sichuan University (Grant no. HX-2019-nCoV-057), the Regional Innovation Cooperation between Sichuan and Guangxi Provinces (2020YFQ0019), and the National Natural Science Foundation of China (32070671).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Huang, X. et al. (2022). Health-Based Geographic Information Systems for Mapping and Risk Modeling of Infectious Diseases and COVID-19 to Support Spatial Decision-Making. In: Shen, B. (eds) Translational Informatics. Advances in Experimental Medicine and Biology, vol 1368. Springer, Singapore. https://doi.org/10.1007/978-981-16-8969-7_8
Download citation
DOI: https://doi.org/10.1007/978-981-16-8969-7_8
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-8968-0
Online ISBN: 978-981-16-8969-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)