Abstract
Acute respiratory distress syndrome (ARDS) is a collective term for the pathological conditions that develop acutely, following preexisting underlying diseases or injuries, resulting in extremely severe hypoxemia caused by non-hydrostatic pulmonary edema due to diffuse lung injury. Ever since its first description in 1967, the syndrome has been extensively investigated but continued as a contributor to the high mortality of patients in ICU settings. The American-European Consensus Conference (AECC) definition reported in 1994 was the first generally agreed-upon definition for ARDS. Although the AECC definition facilitated the many clinical trials, a number of limitations emerged. The Berlin definition established in 2012 was a revised version of the AECC definition maintaining a link to prior definition with refinement of diagnostic criteria of timing, chest imaging, origin of edema, and hypoxemia. The Berlin definition showed qualitative improvements over the AECC definition in several aspects. Three mutually exclusive categories of mild, moderate, and severe ARDS were validated as they were associated with higher mortality rates from mild to severe form of ARDS. The Berlin definition has been widely accepted, but it still has several limitations that require further investigations to establish a better definition of ARDS.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Acute respiratory distress syndrome (ARDS) is a collective term for the pathological conditions that develop acutely, following preexisting underlying diseases or injuries, resulting in extremely severe hypoxemia caused by diffuse lung injury. The pathophysiology of ARDS is a diffuse pulmonary edema that cannot be explained by cardiac failure, renal failure, or overhydration. Namely, the edema is not caused by an increase in capillary hydrostatic pressure but an increased alveolar permeability due to the disruption of the lung endothelium and the alveolar epithelium [1]. In general, patients have various kinds of risk factors that trigger the acute development of the lung injury within several days that require tracheal intubation with the mechanical ventilation, and sometimes extracorporeal membrane oxygenation (ECMO). Efforts to find an effective treatment to increase survivability and decrease mortality rates are still ongoing. Although no effective pharmaceutical measures have not been found, it is believed that the refined critical care setting offered a considerable decrease in mortality nowadays. Still, specific clinical definition is imperative for the clear diagnosis, prognosis, and severity of the illness to provide appropriate therapeutic measures for clinicians.
2 Before 1967
Laennec reported a queer condition that showed pulmonary edema without heart failure and described it as an idiopathic anazarca in 1821. This would be the first historically reported syndrome now recognized as acute respiratory distress syndrome (ARDS) [2].
Inhalation of phosgene and chlorine, chemical weapons used during the World War I era, posed devastating risks on many casualties. Once victims were exposed to these gases, the symptom of acute lung injury progressed gradually, usually overt on the following day [3]. Near the end of World War II, some refractory respiratory distress was identified among soldiers with non-thoracic injury and the syndrome was called as “wet lung” or “shock lung.” During Vietnam war, the more casualties were properly and promptly salvaged from battlefield, the more this strange lung syndrome became evident. Many soldiers succumbed unexpectedly due to respiratory distress during convalescence from well resuscitated traumatic or hemorrhagic shock [4]. The syndrome was called Da Nang lung as many cases were seen at a medical center at Da Nang in Vietnam, and some doctors suspected these cases as an endemic. Military doctors who then returned to private practice in a civilian environment encountered similar respiratory failure among citizen of all ages in the USA and suspected it as Da Nang lung. Then, they finally found the right answer in the publication by Ashbaugh and colleagues in 1967 [5, 6].
3 1967–1992
3.1 First Report of ARDS by Ashbaugh and Colleagues
Ashbaugh and colleagues described 12 patients with refractory respiratory distress followed by several clinically unrelated disorders such as viral pneumonia, severe multiple trauma with shock, acute pancreatitis, or gastric aspiration. The abnormalities have distinguished them from among 272 patients who had received respiratory support in the intensive care units at that time period. They observed acute onset of tachypnea, hypoxemia, and loss of lung compliance together with the effectiveness of positive end-expiratory pressure (PEEP) to combat these symptoms. They also postulated the lack of surfactant activity in the alveoli and suggested the use of corticosteroids, inotropes, and diuretics in some cases. At autopsy, they observed heavy and deep reddish lung resembling liver tissue. Microscopic appearance of the lungs showed diffuse interstitial inflammation with hyaline membranes and fibrosis was present in patients who died after a protracted course [5]. Although they described the syndrome as acute respiratory distress, 4 years later they coined the term “adult respiratory distress syndrome” as ARDS [7], because they address the notion of ARDS as an adult version of infant respiratory distress syndrome (IRDS), a syndrome of premature infants caused by the insufficiency of surfactant production and lung immaturity. Table 1.1 shows six characteristic findings proposed by Petty and Ashbaugh that became the source of concept and diagnostic criteria for ARDS definition. [7].
After this publication, no widely accepted definition of ARDS was seen for a quarter of a century. During this period, the incidence or the mortality of ARDS varied as it could say that each facility has its own definition of ARDS. Garber et al. identified a total of 83 clinical ARDS studies from 1966 to 1994, and found only 49% of studies provided some definition of ARDS. At least seven substantially different definitions were found during this period that should cause significant variation in the incidence and mortality of ARDS [8].
3.2 Murray’s Definition with Lung Injury Score
In 1988, Murray and colleagues reported their definition of ARDS incorporating timing, risk factors, and severity (Table 1.2). The severity was measured by a Lung Injury Score (LIS) also shown in Table 1.2 [9]. Although LIS remains a commonly utilized measure of lung injury severity, there has been no report that the LIS is valid for the marker of mortality risk [10, 11].
4 1992–2012
4.1 AECC Definition
In 1992, a series of meetings were held during annual conferences of the American Thoracic Society and European Society of Intensive Care Medicine to discuss a clear and uniform definition of ARDS. The report was published in 1994 by the name of the American-European Consensus Conference (AECC). This so-called AECC definition was the first widely accepted and used ARDS definition. First of all, they decided to call ARDS as “acute” (rather than “adult”) respiratory distress syndrome. The consensus definition consists of four components, timing, oxygenation, chest XP, and pulmonary artery occlusion pressure (or no clinical sign of left arterial hypertension) (Table 1.3). It classified lung injury by PaO2/FiO2 ratio. Patients with PaO2/FiO2 ≤ 300 were defined as acute lung injury (ALI) and those who showed PaO2/FiO2 ≤ 200 (severer form of ALI) were defined as ARDS. Although ALI is an umbrella term for all patients with PaO2/FiO2 ≤ 300, it is frequently and misleadingly used for patients with PaO2/FiO2 between 201 and 300. Namely, all patients with ARDS have ALI, but not all patients with ALI have ARDS (see Fig. 1.1a). Thus, a milder form of ALI was sometimes called ALI without ARDS.
Schematic explanation of conceptual difference and resemblance of ARDS between the AECC definition and the Berlin definition based on the degree of oxygenation. Acute hypoxemic respiratory failure (AHRF) is a general term applied for patients with refractory severe hypoxemia usually defined as PaO2/FiO2 ≤ 300. Ketchams and colleagues reported that they identified 385 patients with AHRF and of whom 33% met criteria with Berlin definition [13]. Other causes of AHRF would be hydrostatic lung edema, volume overload, right-to-left intracardiac shunts, or pneumonia without fulfilling the criteria of ARDS definition, etc.
AECC members explained that although ARDS is caused by different types of risk factors, similar clinical features make clinicians understand ARDS as a single entity rather than characterize the individual risk factors as separate clinical entities. At the same time, AECC members noted that it would be useful to think of the pathogenesis as consisting of two pathways: direct effects of an insult on lung cells and the indirect result of an acute systemic inflammatory response (Table 1.4).
4.2 Limitation of AECC Definition
Although only proven therapeutic measure so far was lung protective strategy with low tidal volume, the AECC definition was simple to apply in a clinical setting and has been adopted for many subsequent randomized control trials for the next two decades. Nonetheless, this definition had several flaws that challenged its reliability and validity to conduct epidemiological studies and clinical trials. First, at autopsy, only half of the patients diagnosed as ARDS by AECC definition revealed typical diffuse alveolar damage, the histopathological hallmark for the acute phase of ARDS [15]. Second, mechanical ventilatory support was not considered a requirement in defining ALI or ARDS, as they presumed ventilator therapy resources and physician’s practice patterns vary considerably. But in reality, it is evident that the level of PEEP or FiO2 can significantly influence oxygenation [16]. Third, although the chest radiograph is essential to diagnose ARDS, high inter-observer variability has been pointed out and sometimes makes it difficult to apply the result for proper diagnosis [17, 18]. Fourth, the onset of respiratory failure was simply defined as “acute,” not indicating a specific timeframe explicitly. Fifth, routine use of pulmonary artery catheters lost popularity as its use was associated with increased mortality [19], and pulmonary artery catheters guided therapy for ARDS showed no benefit compared to central venous catheter-guided therapy [20]. Also, hydrostatic edema in the form of cardiac failure or fluid overload may coexist with ARDS [20].
4.3 DELPHI Definition
The Delphi technique is a group interaction method of gaining consensus on a particular topic. Ferguson and colleagues implemented this technique to develop a new definition of ARDS. The definition was named after the technique as Delphi definition [21]. They also suggested that testing of sensibility, feasibility, reliability, and validity would be needed for the making reliable definition. This structured communication technique was applied afterward, such as to making of the Berlin definition or Surviving Sepsis Campaign guidelines [21, 22]. Subsequently, they compared the diagnostic accuracy among the AECC definition, the lung injury score (LIS), and the Delphi definition [23]. They showed that 42 out of 138 autopsied patients who were being mechanically ventilated had diffuse alveolar damage. Only 20 of these 42 patients had any mention of ARDS in the medical chart suggesting ARDS is often underrecognized in clinical practice. The sensitivities were not significantly different among three definitions. Whereas, specificity was significantly but moderately higher for the LIS and Delphi definition than for the AECC definition [21]. The Delphi definition did not gain popularity but created the atmosphere that the AECC definition should be reconsidered (Table 1.5).
5 After 2012
5.1 Berlin Definition; Draft Definition
In 2011, a panel of ARDS experts convened at the 24th annual meeting of the European Society of Intensive Care Medicine held in Berlin. They developed a conceptual model of ARDS mainly based on AECC definition, maintaining a link to prior AECC definitions with diagnostic criteria of timing, chest imaging, origin of edema, and hypoxemia, and proposed a draft definition [24]. Using teleconferencing, in-person discussions and retrospective data for checking validity, the panel published the final version of definition in 2012 [24]. In revising the definition of ARDS, the panel emphasized feasibility, reliability, face validity (i.e., how clinicians recognize ARDS), and predictive validity (i.e., ability to predict response to therapy, outcomes, or both).
In the draft definition, the term, acute lung injury (ALI) was eliminated. PEEP of at least 5 cm H2O was required to obtain the value of PaO2/FiO2 ratio. ARDS was then classified into three mutually exclusive subcategories (See Fig. 1.1 b), based on the degree of oxygenation, as mild (200 < PaO2/FiO2 ≤ 300 with PEEP or CPAP ≥5 cm H2O), moderate (100 < PaO2/FiO2 ≤ 200 with PEEP ≥ 5 cm H2O), and severe ARDS (PaO2/FiO2 ≤ 100 with PEEP ≥ 5 cm H2O). As nearly all patients with ARDS identified within 7 days, the timing for onset was proposed as within 1 week of a clinical insult or new/worsening respiratory symptoms. As for the chest imaging, bilateral opacities could be demonstrated either chest radiograph or CT scan. The utilization of pulmonary artery catheter to measure pulmonary wedge pressure was excluded. Patients can be diagnosed as having ARDS if they have respiratory failure with risk factors for ARDS. If no ARDS risk factor is found, objective assessment (e.g., echocardiography) will be required to exclude the hydrostatic edema or overhydration. In addition, the panel suggested to add four ancillary variables for severe ARDS; radiographic opacity on chest X-ray involving 3 or 4 quadrants, static compliance of respiratory system (≤40 mL/cm H2O), positive end-expiratory pressure (≥10 cm H2O), and corrected expired volume per minute (≥10 L/min).
5.2 Berlin Definition; Empirical Evaluation of the Draft Definition
The draft definition was then evaluated empirically using database from four multicenter clinical studies (4188 patients with ARDS) [25,26,27,28] and three single-center physiological studies (269 patients with ARDS) [29,30,31]. Using these databases, characteristics of patients in each category of ARDS were determined and predictive validity for mortality was examined. The panel convened 4 months later by multiple teleconferences to produce a final version of the definition. The final version of the Berlin definition for ARDS is shown in Table 1.6. While the AECC definition classified ARDS into direct and indirect lung injury categories, the Berlin definition abandoned this idea and emphasized that knowing underlying disease regardless of its direct or indirect nature leading to ARDS would serve to guide therapy (Table 1.7). And risk factor was partly incorporated into the definition [32].
The four ancillary variables were revealed to have no better predictive validity of severe ARDS for mortality and were removed from the final definition [24]. The panel also considered to include potential diagnostic criteria, such as minimal FiO2 requirement, SpO2/FiO2 ratio, higher PEEP requirement, thoracic computed tomography, electrical impedance tomography, extravascular lung water, inflammatory biomarkers, genetic markers, plateau pressure, dead space, respiratory system compliance, minute ventilation, and pathological finding of diffuse alveolar damage by lung biopsy. However, they were rejected during definition development because of a lack of association data, impact on feasibility, or both [32]. In addition, to enhance inter-observer reliability, a reference set of chest radiographs were provided, and illustrative vignettes were created to guide judgments whether the illustrating cases qualify as ARDS based on ruling out hydrostatic edema [32].
As for the predictive validity of the Berlin definition, the three mutually exclusive categories of mild, moderate, and severe ARDS were validated, as they were associated with the significant progressive higher mortality rate from mild to moderate to the severe form of ARDS, 27% [95%CI, 24–30%], 32% [95%CI, 29–34%], and 45% [95%CI, 42–48%], respectively, based on the data from four clinical trials. The definition performed similarly in the physiological database as in the clinical database. Likewise, ventilator-free days declined, and the median duration of mechanical ventilation in survivors increased with stages of ARDS from mild to moderate to severe. Although, each stage is associated with increased mortality, prediction ability of mortality using this definition is still poor, with an area under the curve of only 0.577, and has not been much improved compared to 0.536 for the AECC definition [24].
5.3 Berlin Definition; Limitation of the Berlin Definition
The Berlin definition of ARDS offers several major advances over previous definitions and numerous clinical trials proposed and are now in progress [33]. However, there remains considerable controversy about the Berlin Definition whether it is valid and meets clinicians’ need.
First, as it does not eliminate the underlying heterogeneity, some investigators are afraid that the Berlin definition may merely contribute to generating additional negative trials [34]. Second, as for the interobserver reliability of ARDS diagnosis, Sjoding and colleagues reported that clinicians had only moderate interobserver agreement when diagnosing ARDS, and major cause of the variability was the interpretation of chest images [35]. Third, the correlation of pathological findings of diffuse alveolar damage by open lung biopsy and ARDS diagnosed by Berlin definition is modest [36]. Still, fewer than half of patients with Berlin definition ARDS have diffuse alveolar damage [37]. Fourth, Villar and colleagues showed that under standardized ventilator settings (VT = 7 mL/kg of predicted body weight, PEEP = 10 cm H2O, and FiO2 0.5), measurement of PaO2/FiO2 24 h from the initial assessment improved the stratification and resulted in better predictive validity for the mortality [38, 39]. As they pointed out, under non-standardized assessment of oxygenation, PaO2/FiO2 can vary considerably with PEEP and FiO2 titration, further researches would be needed to determine whether incorporating more specific guidelines based on a standard method of evaluating oxygenation status (i.e., a specific level of PEEP and FiO2) add value to the definition. Fifth, most recent epidemiological data were provided by LUNG-SAFE (Large Observational Study to Understand the Global Impact of Severe Acute Respiratory Failure). Of 29,144 patients who were admitted to the ICUs, 12,906 (44.3%) received mechanical ventilation upon ICU admissions, and 3022 (10.4%) fulfilled the Berlin definition of ARDS. The clinical recognition of ARDS was 51.3% in mild, and 78.5% in severe ARDS. These findings suggest that ARDS was underrecognized in the ICU settings [40]. However, some investigators criticized that their observation was an overestimation of incidence caused by incapability of Berlin definition to identify true ARDS patients [41]. Caser and colleagues prospectively evaluated 130 ARDS (fulfilled with AECC or Berlin definition) patients in the Brazilian ICU setting, and did not observe significant differences in mortality among the mild, moderate, and severe ARDS based on the Berlin definition, and could not show any improvement of predictive mortality compared to AECC definition (area under the ROC curve was 0.5625 for the AECC and 0.5664 for the Berlin definition, P = 0.9510) [42]. Finally, although noninvasive ventilation or high-flow nasal cannula without positive pressure ventilation became popular nowadays, definition applicable in these settings was lacking.
5.4 Future Perspective
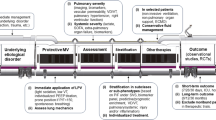
In general, a precise and appropriate definition is absolutely necessary to facilitate clinicians in making timely decisions for diagnosis, specific therapies or prognosis of the disease, and investigators in proceeding reproducible clinical trials. The fundamental challenge to making a better definition of ARDS is the lack of a gold standard diagnostic test for ARDS. Like other critical illness syndromes such as sepsis, ARDS is a heterogeneous syndrome with complex pathology and mechanisms. Proposed definitions so far are based on clinical criteria and did not offer enough reliability and validity, unable to identify patients with specific disease processes such as diffuse alveolar damage. This situation makes clinicians and researchers difficult to identify ARDS properly and leads to paucity of successful therapeutic interventions in ARDS [43]. Some investigators insist that for patients who meet the clinical definitions for ARDS, there are subgroups/subphenotypes of patients who are more or less likely to benefit from a particular therapy. There are several factors for identifying phenotypes based on physiological (such as PaO2/FiO2 ratio, dead space fraction, or driving pressure), clinical (age, sex, ethnicity, routine laboratory tests, and imaging techniques), and biologic (genetic polymorphisms, genomic, transcriptomic, proteomic, or metabolomic) data [44, 45].
As for the clinical data, if anyone would find some clinical phenotypes in ARDS identifiable at hospital that correlate with the host response patterns and clinical outcomes, that would facilitate clinicians for a better and tailored management of this heterogeneous syndrome. Calfee and colleagues identified two phenotypes of ARDS differently responding to treatment and named them as hyperinflammatory or hypoinflammatory subphenotypes. These phenotypes were identified based on the baseline demographics (age and sex), baseline clinical data (direct and indirect ARDS risk factors, bilirubin, creatinine, platelet count, PaO2 to FiO2 ratio, plateau pressure, tidal volume, and use of vasopressors), and baseline interleukin 6 and sTNFr1 values [44, 46]. Further study will be needed to validate this strategy to incorporate the idea into future definitions. As for the biologic phenotyping, the researchers have just started the studies and now expanding the evidence steadily in basic science. Comprehensive definition would be accomplished when the exact phenotyping is established that would minimize heterogeneity of the syndrome and enable stratification of subject selection for enrollment in clinical trial and proper treatment.
As far as we do not have a gold standard for the recognition of ARDS or its subtypes, any new feasible diagnostic and prognostic tools more objective and accurate than our current bedside assessment to identify the disease process will be incorporated into new draft definition and will be evaluated in terms of its feasibility, reliability, and predictive/face validity. Possibly, a new definition would maintain a link to prior definitions to facilitate the comparison of the studies.
Another aspect of the future definition is that to develop several noninvasive techniques detecting ARDS promptly at the bedside or limited resource environment, possibly identify the candidate of mechanical ventilation beforehand. SpO2 (pulse oximetric saturation)/FiO2 ratio has been proposed as a promising noninvasive alternative to PaO2/FiO2 ratio [47]. Lung ultrasound is also a noninvasive and easy to perform tool to diagnose ARDS at the bedside. Bass reported that combination of pulse SpO2/FiO2 ratio and lung ultrasound analysis enabled clinicians to diagnose ARDS at the bedside noninvasively in a limited resource environment where arterial blood gas measurement and chest radiography are not routinely available [48]. Riviello and colleagues suggested the validity of this combination in Rwanda [49]. These studies should shed light on another aspect to develop a new definition that can be used in all settings.
6 Conclusion
In this chapter, the definition of ARDS was historically summarized. It is important to note that ARDS, as the name implies, is a syndrome, not a disease, and there is no laboratory, imaging, or biological gold standard at this time to diagnose ARDS. Therefore, it has to be defined by a constellation of clinical and physiological criteria like the AECC definition and the Berlin definition. Both definitions had enabled clinicians to prospectively identify patients with ARDS and apply suitable therapy such as a lung protective procedure promptly or to enroll patients in many clinical trials. However, clinical heterogeneity observed among patients diagnosed as ARDS based on the current definitions had likely contributed to the epidemiologic variations among studies and the paucity of appropriate therapies for ARDS despite a large number of promising preclinical studies and clinical trials. Specifying distinct ARDS subgroups by the discovery of new phenotyping may substantially change the definition of ARDS, and hopefully leading to precision/tailored treatment of ARDS.
References
Matthay MA, McAuley DF, Ware LB. Clinical trials in acute respiratory distress syndrome: challenges and opportunities. Lancet Respir Med. 2017;5(6):524–34. https://doi.org/10.1016/S2213-2600(17)30188-1.
Bernard GR. Acute respiratory distress syndrome: a historical perspective. Am J Respir Crit Care Med. 2005;172(7):798–806. https://doi.org/10.1164/rccm.200504-663OE.
Li W, Pauluhn J. Phosgene-induced acute lung injury (ALI): differences from chlorine-induced ALI and attempts to translate toxicology to clinical medicine. Clin Transl Med. 2017;6(1):19. https://doi.org/10.1186/s40169-017-0149-2.
Fishman AP. Shock lung: a distinctive nonentity. Circulation. 1973;47(5):921–3. https://doi.org/10.1161/01.cir.47.5.921.
Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet. 1967;2(7511):319–23.
Petty TL. In the cards was ARDS: how we discovered the acute respiratory distress syndrome. Am J Respir Crit Care Med. 2001;163(3 Pt 1):602–3.
Petty TL, Ashbaugh DG. The adult respiratory distress syndrome. Clinical features, factors influencing prognosis and principles of management. Chest. 1971;60(3):233–9.
Garber BG, Hebert PC, Yelle JD, Hodder RV, McGowan J. Adult respiratory distress syndrome: a systemic overview of incidence and risk factors. Crit Care Med. 1996;24(4):687–95.
Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis. 1988;138(3):720–3.
Monchi M, Bellenfant F, Cariou A, Joly LM, Thebert D, Laurent I, et al. Early predictive factors of survival in the acute respiratory distress syndrome. A multivariate analysis. Am J Respir Crit Care Med. 1998;158(4):1076–81.
Kangelaris KN, Calfee CS, May AK, Zhuo H, Matthay MA, Ware LB. Is there still a role for the lung injury score in the era of the Berlin definition ARDS? Ann Intensive Care. 2014;4(1):4. https://doi.org/10.1186/2110-5820-4-4.
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. The American-European consensus conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–24.
Ketcham SW, Sedhai YR, Miller HC, Bolig TC, Ludwig A, Co I, et al. Causes and characteristics of death in patients with acute hypoxemic respiratory failure and acute respiratory distress syndrome: a retrospective cohort study. Crit Care. 2020;24(1):391. https://doi.org/10.1186/s13054-020-03108-w.
Ware LB, Matthay MA. Medical progress: the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1334–49.
De Hemptinne Q, Remmelink M, Brimioulle S, Salmon I, Vincent JL. ARDS: a clinicopathological confrontation. Chest. 2009;135(4):944–9.
Villar J, Kacmarek RM. The American-European consensus conference definition of the acute respiratory distress syndrome is dead, long live positive end-expiratory pressure! Med Intensiva. 2012;36(8):571–5. https://doi.org/10.1016/j.medine.2012.10.011.
Rubenfeld GD, Caldwell E, Granton J, Hudson LD, Matthay MA. Interobserver variability in applying a radiographic definition for ARDS. Chest. 1999;116(5):1347–53.
Meade MO, Cook RJ, Guyatt GH, Groll R, Kachura JR, Bedard M, et al. Interobserver variation in interpreting chest radiographs for the diagnosis of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2000;161(1):85–90.
Connors AF Jr, Speroff T, Dawson NV, Thomas C, Harrell FE Jr, Wagner D, et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT investigators. JAMA. 1996;276(11):889–97.
Wheeler AP, Bernard GR, Thompson BT, Schoenfeld D, Wiedemann HP, deBoisblanc B, et al. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med. 2006;354(21):2213–24.
Ferguson ND, Davis AM, Slutsky AS, Stewart TE. Development of a clinical definition for acute respiratory distress syndrome using the Delphi technique. J Crit Care. 2005;20(2):147–54. https://doi.org/10.1016/j.jcrc.2005.03.001.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637. https://doi.org/10.1097/CCM.0b013e31827e83af.
Ferguson ND, Frutos-Vivar F, Esteban A, Fernandez-Segoviano P, Aramburu JA, Najera L, et al. Acute respiratory distress syndrome: underrecognition by clinicians and diagnostic accuracy of three clinical definitions. Crit Care Med. 2005;33(10):2228–34.
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–33. https://doi.org/10.1001/jama.2012.5669.
Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, et al. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353(16):1685–93.
Bersten AD, Edibam C, Hunt T, Moran J. Incidence and mortality of acute lung injury and the acute respiratory distress syndrome in three Australian states. Am J Respir Crit Care Med. 2002;165(4):443–8.
Needham DM, Dennison CR, Dowdy DW, Mendez-Tellez PA, Ciesla N, Desai SV, et al. Study protocol: the improving care of acute lung injury patients (ICAP) study. Crit Care. 2006;10(1):R9. https://doi.org/10.1186/cc3948.
Britos M, Smoot E, Liu KD, Thompson BT, Checkley W, Brower RG, et al. The value of positive end-expiratory pressure and Fio2 criteria in the definition of the acute respiratory distress syndrome. Crit Care Med. 2011;39(9):2025–30. https://doi.org/10.1097/CCM.0b013e31821cb774.
Bellani G, Guerra L, Musch G, Zanella A, Patroniti N, Mauri T, et al. Lung regional metabolic activity and gas volume changes induced by tidal ventilation in patients with acute lung injury. Am J Respir Crit Care Med. 2011;183(9):1193–9. https://doi.org/10.1164/rccm.201008-1318OC.
Terragni PP, Rosboch G, Tealdi A, Corno E, Menaldo E, Davini O, et al. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2007;175(2):160–6.
Terragni PP, Del Sorbo L, Mascia L, Urbino R, Martin EL, Birocco A, et al. Tidal volume lower than 6 ml/kg enhances lung protection: role of extracorporeal carbon dioxide removal. Anesthesiology. 2009;111(4):826–35.
Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, et al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med. 2012;38(10):1573–82. https://doi.org/10.1007/s00134-012-2682-1.
Del Sorbo L, Ranieri VM, Ferguson ND. The Berlin definition met our needs: yes. Intensive Care Med. 2016;42(5):643–7. https://doi.org/10.1007/s00134-016-4286-7.
Vincent JL. The Berlin definition met our needs: not sure. Intensive Care Med. 2016;42(5):651–2. https://doi.org/10.1007/s00134-016-4319-2.
Sjoding MW, Hofer TP, Co I, Courey A, Cooke CR, Iwashyna TJ. Interobserver reliability of the Berlin ARDS definition and strategies to improve the reliability of ARDS diagnosis. Chest. 2018;153(2):361–7. https://doi.org/10.1016/j.chest.2017.11.037.
Kao KC, Hu HC, Chang CH, Hung CY, Chiu LC, Li SH, et al. Diffuse alveolar damage associated mortality in selected acute respiratory distress syndrome patients with open lung biopsy. Crit Care. 2015;19(1):228. https://doi.org/10.1186/s13054-015-0949-y.
Thille AW, Esteban A, Fernandez-Segoviano P, Rodriguez JM, Aramburu JA, Penuelas O, et al. Comparison of the Berlin definition for acute respiratory distress syndrome with autopsy. Am J Respir Crit Care Med. 2013;187(7):761–7. https://doi.org/10.1164/rccm.201211-1981OC.
Villar J, Perez-Mendez L, Blanco J, Anon JM, Blanch L, Belda J, et al. A universal definition of ARDS: the PaO2/FiO2 ratio under a standard ventilatory setting – a prospective, multicenter validation study. Intensive Care Med. 2013;39(4):583–92. https://doi.org/10.1007/s00134-012-2803-x.
Villar J, Blanco J, del Campo R, Andaluz-Ojeda D, Diaz-Dominguez FJ, Muriel A, et al. Assessment of PaO2/FiO2 for stratification of patients with moderate and severe acute respiratory distress syndrome. BMJ Open. 2015;5(3):e006812. https://doi.org/10.1136/bmjopen-2014-006812.
Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788–800. https://doi.org/10.1001/jama.2016.0291.
Villar J, Schultz MJ, Kacmarek RM. The LUNG SAFE: a biased presentation of the prevalence of ARDS! Crit Care. 2016;20(1):108. https://doi.org/10.1186/s13054-016-1273-x.
Caser EB, Zandonade E, Pereira E, Gama AM, Barbas CS. Impact of distinct definitions of acute lung injury on its incidence and outcomes in Brazilian ICUs: prospective evaluation of 7,133 patients*. Crit Care Med. 2014;42(3):574–82. https://doi.org/10.1097/01.ccm.0000435676.68435.56.
Pham T, Rubenfeld GD. Fifty years of research in ARDS. The epidemiology of acute respiratory distress syndrome. A 50th birthday review. Am J Respir Crit Care Med. 2017;195(7):860–70. https://doi.org/10.1164/rccm.201609-1773CP.
Wilson JG, Calfee CS. ARDS subphenotypes: understanding a heterogeneous syndrome. Crit Care. 2020;24(1):102. https://doi.org/10.1186/s13054-020-2778-x.
Metwaly S, Cote A, Donnelly SJ, Banoei MM, Mourad AI, Winston BW. Evolution of ARDS biomarkers: will metabolomics be the answer? Am J Physiol Lung Cell Mol Physiol. 2018;315(4):L526–34. https://doi.org/10.1152/ajplung.00074.2018.
Calfee CS, Delucchi KL, Sinha P, Matthay MA, Hackett J, Shankar-Hari M, et al. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: secondary analysis of a randomised controlled trial. Lancet Respir Med. 2018;6(9):691–8. https://doi.org/10.1016/S2213-2600(18)30177-2.
Rice TW, Wheeler AP, Bernard GR, Hayden DL, Schoenfeld DA, Ware LB. Comparison of the SpO2/FIO2 ratio and the PaO2/FIO2 ratio in patients with acute lung injury or ARDS. Chest. 2007;132(2):410–7. https://doi.org/10.1378/chest.07-0617.
Bass CM, Sajed DR, Adedipe AA, West TE. Pulmonary ultrasound and pulse oximetry versus chest radiography and arterial blood gas analysis for the diagnosis of acute respiratory distress syndrome: a pilot study. Crit Care. 2015;19:282. https://doi.org/10.1186/s13054-015-0995-5.
Riviello ED, Kiviri W, Twagirumugabe T, Mueller A, Banner-Goodspeed VM, Officer L, et al. Hospital incidence and outcomes of the acute respiratory distress syndrome using the Kigali modification of the Berlin definition. Am J Respir Crit Care Med. 2016;193(1):52–9. https://doi.org/10.1164/rccm.201503-0584OC.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Hashimoto, S. (2022). Definition of ARDS: Does the Berlin Definition Fit the Clinical Entity and Predict the Outcome?. In: Tasaka, S. (eds) Acute Respiratory Distress Syndrome. Respiratory Disease Series: Diagnostic Tools and Disease Managements. Springer, Singapore. https://doi.org/10.1007/978-981-16-8371-8_1
Download citation
DOI: https://doi.org/10.1007/978-981-16-8371-8_1
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-8370-1
Online ISBN: 978-981-16-8371-8
eBook Packages: MedicineMedicine (R0)