Abstract
Prevention and treatment of chronic kidney disease in diabetes (diabetic kidney disease [DKD]) with lifestyle intervention, including diet therapy, have been a focus of interest in research. Consideration of the amount of energy intake by carbohydrates and lipids and the amount of protein and salt intake is required for managing body weight, maintaining optimal blood glucose levels, and preventing diabetes-related vascular complications, including DKD. However, the clinical significance of protein restriction and the ideal recommended intake in view of its benefits and risks are controversial. Furthermore, the severity of DKD with which to implement dietary changes should also be considered. This section seeks to provide guidance regarding nutritional management of DKD and discusses the remaining clinical issues in this field.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Diabetic kidney disease
- Diabetic nephropathy
- Protein restriction
- Salt restriction
- Potassium restriction
- Microalbuminuria
- Macroalbuminuria
- Renal failure
1 Introduction
Comprehensive therapy focusing on managing blood glucose levels, blood pressure, and the lipid profile is the most recommended therapeutic approach for diabetic kidney disease (DKD). This therapy aims to manage progression toward end-stage kidney disease and cardiovascular disease. Comprehensive therapy involves various approaches, such as improving lifestyle habits (diet and exercise therapies) and pharmacotherapy. Therefore, sharing of information and collaboration within a medical team, including a physician, nursing staff, and nutritionist, in planning and performing treatment and education of patients, are important for promoting better clinical outcomes in DKD. Among these approaches, diet therapy is an essential part of comprehensive therapy, and it needs to be tailored to suit the stage of DKD. In diet therapy, there are no clear guidelines on protein restriction, which is important because it depends on factors, such as age, nutritional status, adherence, and risk of cardiovascular disease. In this section, we outline some salient points and issues of diet therapy according to the stages of DKD and discuss remaining issues in diet therapy in DKD.
2 Diet Therapy for DKD
An overview of diet therapy for DKD is shown in Table 7.1. This overview was modified from a clinical guideline published from the Japan Diabetes Society. A limitation is that standardizing dietary therapy worldwide is difficult because the cause of diabetes is slightly different among countries. In the United States, the main cause of diabetes is severe insulin resistance due to obesity and relatively insufficient insulin secretion. However, in some Asian countries including Japan, the cause of diabetes is commonly due to insufficient insulin secretion in addition to mild insulin resistance. Therefore, the dietary amount of each nutrient should be optimized and modified according to the health problem and situation in the individual country. Additionally, if available, diet therapy should be conducted according to a clinical guideline supplied in each country [1].
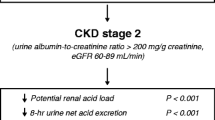
2.1 Diet Therapy in Chronic Kidney Disease Stages G1A1-2 and G2A1-2
2.1.1 Caloric Intake
The recommended caloric intake, taking into account the degree of obesity and degree of activity, is 25–30 kcal/ideal body weight (IBW) kg/day with a goal of a body mass index (BMI) <25 kg/m2. Several studies have reported that decreasing the caloric intake in patients with diabetes and obesity results in decreased albuminuria, as well as improved control of blood glucose levels [2, 3]. Therefore, in patients with severe obesity, the caloric intake can be decreased to 20–25 kcal/IBW kg/day.
2.1.2 Protein Intake
Protein intake depends on people’s habits in various countries. The diet of a person with diabetes should ideally comprise 50–60% carbohydrates, with 1–1.2 g of protein/kg of IBW per day, and lipids should comprise the rest of the diet. An excessive protein consumption of >1.3 g/IBW kg/day should be avoided for preventing initiation and progression of DKD.
However, when the proportion of energy from carbohydrates is 50–60% of the total energy, the quantity of proteins is generally 15–20%. Consequently, based on the total energy intake, protein intake is 1–1.5 g/IBW kg/day and can become greater than 1.3 g/IBW kg/day (Fig. 7.1). In particular, when the proportion of carbohydrates is 50–55%, provided that the proportion of lipids is less than 30%, the proportion of protein will increase, as well as intake of protein (Fig. 7.1). This situation raises the question of whether a high protein intake is harmful. A high protein intake might damage organs, including the kidneys. Halbesma et al. reported the possibility of an increased incidence of cardiovascular events in a group with high protein intake (1.38–3.27 g/kg/day) compared with a group with protein consumption of 1.10–1.26 g/kg/day [4]. The risk of kidney damage in healthy older subjects secondary to a high protein intake of 2.0 g/kg/day has been reported previously [5]. A long-term study over 11 years reported that in women with a slightly decreased renal function (estimated glomerular filtration rate [eGFR] of 55–88 ml/min/1.73 m2), protein intake of >1.3 g/kg/day was associated with a progressive decrease in renal function (10 g/day increase in protein intake was associated with a decrease in eGFR of 7.72 ml/min/1.73 m2) [5]. Therefore, even at this stage of DKD, when there is no clearly noticeable decrease in renal function, excessive protein intake of >1.3 g/IBW kg/day should be avoided because of the high risk of developing or worsening DKD and the risk of developing cardiovascular events.
Therefore, when prescribing low-carbohydrate diet therapy to decrease intake or improve blood glucose levels at this stage of DKD, restricting carbohydrates to less than 50% of the energy requirement should be avoided because of the risks associated with excess protein intake. An increase in protein intake should also be considered when prescribing diet therapy with a carbohydrate intake of 50–55%, and patients should be closely monitored in the long term.
2.1.3 Salt Restriction
Hypertension is a major concomitant disorder in diabetic patients. Especially, masked hypertension is a common feature in type 2 diabetic patients being treated for hypertension, and high sodium intake is associated with this type of hypertension [6]. In case of hypertension, regardless of causes, salt intake should be less than 6 g/day. Salt restriction is recommended because it has an independent depressor effect. When salt restriction is combined with medications, along with the depressor effect, an effect on improving proteinuria and renal function decline can be observed [7, 8]. However, excessive restriction of salt intake lowers appetite (especially in older subjects) and can also cause a deterioration in renal function secondary to dehydration. Therefore, careful monitoring is necessary in this situation. Additionally, there are varying views regarding the association between salt restriction and long-term prognosis or cardiovascular events [9]. Future prospective, long-term, intervention studies can help establish guidelines for this issue. In the diagnosis and treatment guide of chronic kidney disease (CKD) of 2012, which was provided by the Japanese Society of Nephrology, a daily salt intake of at least 3 or <6 g is recommended in cases of CKD, including DKD.
2.1.4 Potassium Intake
A high potassium intake, especially potassium citrate, stimulates sodium excretion into urine, leading to better blood pressure control. A recent observational study showed that higher urinary potassium excretion, which might reflect the daily potassium intake, was associated with the slower decline of renal function and the lower incidence of cardiovascular complications in type 2 diabetic patients with normal renal function [10]. Therefore, as long as patients do not have hyperkalemia or take a renin–angiotensin system inhibitor that elevates serum potassium levels as an adverse effect, potassium intake from fresh vegetables or fruits is recommended. To conclude the effectiveness of high potassium intake on DKD, interventional trials are necessary.
2.2 Diet Therapy in CKD Stages G1-2A3 and G3-4
In addition to the issue regarding calorie intake, the requirement for and practice of protein restriction from the macroalbuminuria stage onward is discussed in this section.
2.2.1 Caloric Intake
In the macroalbuminuria stage with an eGFR ≧ 45 ml/min/1.73 m2 (CKD stage G1-2A3), the recommended caloric intake is 25–30 kcal/IBW kg/day (or 25–35 kcal/IBW kg/day depending on the degree of protein restriction) depending on the degree of obesity and degree of activity, with a goal of maintaining a BMI < 25 kg/m2. In the patients with an eGFR < 45 ml/min/1.73 m2, the recommended caloric intake is 25–35 kcal/IBW kg/day.
2.2.2 Restriction of Protein Intake
At present, protein restriction of 0.8–1.0 g/IBW kg/day should be performed from the stage of macroalbuminuria in DKD. Additionally, protein restriction to 0.6–0.8 g/IBW kg/day should be performed during the stage of renal dysfunction. Notably, protein restriction to 0.6–0.8 g/IBW kg/day should be considered even at the stage of macroalbuminuria from a GFR < 45 ml/min/1.73 m2.
Protein restriction has been recommended because it is expected to improve glomerular hypertension/hyperfiltration and control progression of DKD by reducing the phosphorus and acid loads and reduce uremic toxicity and the need for dialysis. However, meta-analyses, systematic reviews, and randomized, controlled trials regarding the renoprotective effects of protein restriction in patients with DKD have shown controversial results [11,12,13,14]. Currently, evidence on this issue is unclear.
Consequently, various guidelines from countries, including the current American Diabetes Association guidelines, do not positively recommend protein restriction as diet therapy for DKD. Some of the reasons for unclear results regarding the renoprotective effect of protein restriction probably include problems with adherence to protein-restricted food, and the problem of which protein intake shows a renoprotective effect. A randomized, controlled trial with a duration of 5 years was carried out in Japan to determine the renoprotective effect of protein restriction in patients with type 2 diabetes with macroalbuminuria [12]. This trial did not show any obvious renoprotective effect of protein restriction [12]. This study also highlighted the difficulty of maintaining protein restriction over a long time. However, Nezu et al. reported the results of their meta-analysis, which indicated that GFR can be improved if protein restriction can be maintained [13]. Therefore, protein restriction can be expected to result in a consistent effect if it can be sustained. Consequently, renoprotective effects can be expected if there is clear adherence to the currently recommended protein restriction of 0.6–0.8 g/IBW kg/day. To achieve this goal, collaboration within a medical team is required.
Various researchers have investigated whether 0.6–0.8 g/IBW kg/day protein restriction is sufficient to demonstrate a renoprotective effect. Ideura et al. reported that in a clinical study on patients with glomerular nephritis (serum creatinine levels ≥6 mg/dL), a renoprotective effect was not observed with 0.6 g/IBW kg/day with protein restriction, but was observed with a higher degree of protein restriction (<0.5 g/IBW kg/day) [15]. Furthermore, Shimai et al. evaluated diabetic patients with severe renal dysfunction with serum creatinine levels ≥3.0 mg/dL and reported that a protein-restricted diet with 0.5 g/IBW kg/day resulted in a decrease in urine protein and delayed the need for dialysis treatment. However, these effects were not observed with a protein intake of ≥0.6 g/IBW kg/day. These results suggest that a more efficacious degree of protein restriction needs to be established to produce its renoprotective effects. Carrying out a high degree of protein restriction under current conditions in anticipation of renoprotective effects should be performed by using special low-protein food, with detailed physical evaluations by an experienced physician and nutritionist. This should be performed to avoid nutritional deficiencies such as those described below.
Protein restriction can be expected to have a consistent effect in protecting the kidneys, but more studies are required to establish the final guidelines. Furthermore, the quantity of protein required differs according to the age of an individual and individual nutritional status. Therefore, there is no single universal recommendation, and protein restriction should only be implemented after comprehensive evaluation of factors, such as age, pathology, risk, and compliance.
2.2.3 Issues of Performing Protein Restriction
After protein restriction is initiated, the nutritional status of the patient, including sarcopenia and frailty, as well as the course of proteinuria and renal function, should be evaluated. Although there are differences between reports on this issue depending on the method used to diagnose or evaluate nutritional disorders and the stage of CKD, protein–energy malnutrition (PEM) is found in approximately 20–50% of patients with CKD [16, 17]. Moreover, this state of malnutrition occurs during treatment prior to dialysis and the stage of dialysis and can contribute to an increased risk of cardiovascular disease and associated mortality rates via physical factors, such as chronic inflammation or increased oxidative stress. If adequate energy intake cannot be ensured when carrying out protein restriction, the protein consumed may not be efficiently used for protein synthesis, thus resulting in PEM. Therefore, when performing protein restriction from the stage of severe kidney dysfunction, an energy intake of at least 30–35 kcal per kg of ideal or actual body weight (when BMI is <18.5 kg/m2) is necessary. Additionally, 25 kcal per kg of ideal or actual body weight is possible in cases of obese subjects even before the stage of dialysis. Although increasing the intake of carbohydrate to ensure adequate energy intake during protein restriction is possible, this may lead to poorer control of blood glucose levels. Therefore, careful monitoring is necessary.
2.2.4 Restriction of Salt Intake
From this stage onward, salt restriction to 6 g/day is recommended, irrespective of the presence of concurrent hypertension. Salt restriction is especially recommended for patients with edema due to nephrotic-range proteinuria or cardiac dysfunction because uncontrollable fluid accumulation leads to early induction of dialysis therapy. However, as in the case of pre-DKD to microalbuminuria stages, careful monitoring is required to identify dehydration and a decrease in renal function due to excessive restriction of salt intake (especially when combined with renin–angiotensin system inhibitors and diuretics).
2.2.5 Potassium Restriction
Because many patients in this stage of DKD will be on renin–angiotensin system inhibitors for the expected renoprotective effect of these drugs, serum potassium levels should be monitored along with blood pressure. While potassium restriction is usually not necessary for all patients in the stage of macroalbuminuria, in the event of concurrent hyperkalemia, potassium should be restricted to <2 g/day, with restriction to <1.5 g/day in the stage of renal failure. Serum potassium levels should be managed within the range of 4.0–5.4 mEq/L.
2.2.6 Phosphorus Restriction
An elevation in serum phosphorus levels is thought to be strongly associated with CKD–mineral and bone disorder and secondary hyperparathyroidism in chronic renal failure and with ectopic calcification, including calcification of blood vessels. Additionally, a meta-analysis showed that elevation of serum phosphorus levels in patients with CKD is an independent risk factor for progression toward renal failure and an increased mortality rate [18]. Therefore, management of serum phosphorus levels is critically important to extend a healthy life span in patients with DKD.
Consequently, serum phosphorus should be maintained within the normal range (approximately 2.5–4.5 mg/dL) until initiation of renal replacement therapy. Additionally, phosphorus restriction should be included in diet therapy to avoid elevated serum phosphorus levels in the stage of renal failure when there is concurrent hyperphosphatemia. However, because there is an association of elevated serum phosphorus levels with protein intake, phosphorus restriction should be introduced in association with protein restriction. Phosphorus is present in cellular components, and therefore, nearly all foods contain phosphorus. Approximately all of the phosphorus is bound to proteins. Consequently, excess protein intake leads to an increased intake of phosphorus. However, in particular, foods with a high phosphorus/protein ratio, such as some dairy products, liver, small fish such as dried whitebait and shishamo smelt (Spirinchus lanceolatus), and other dried whole fish, should be avoided. Although phosphorus in food is organic phosphorus, many food additives include inorganic phosphorus. While only approximately half of the organic phosphorus ingested is absorbed, approximately 90% of inorganic phosphorus consumed is absorbed. Therefore, excessive consumption of fast foods, instant foods, soft drinks, snacks, and confectioneries, which contain a large amount of food additives, should be avoided to prevent excess ingestion of inorganic phosphorus and the resulting accumulation of phosphorus.
2.3 Other Issues in Diet Therapy of Clinical DKD
Quality control of each nutrient should be performed. Over the decades, many clinical studies have been conducted to identify the optimal amount of nutrients to prevent DKD. However, carbohydrates, proteins, and lipids include several types of nutrients in each of them. In foods, glucose and fructose are mainly contained. Fructose has been focused on as a poor food for DKD [19]. High level of serum uric acid is associated with progression of DKD and cardiovascular events in diabetic patients [20, 21]. High fructose intake stimulates uric acid production, resulting in progression of DKD [19, 22]. In a study, consumption of fructose-containing beverages representing 25% of energy requirements for 10 weeks significantly raised serum uric acid level, compared with the glucose-containing beverages [23]. In the National Health and Nutrition Examination Survey (NHANES), the consumption of sugar-sweetened soft drinks was positively associated with serum uric acid levels, suggesting that the fructose in soft drinks could increase uric acid levels [24]. Because soft drinks contain fructose as well as much inorganic phosphorus, for diabetic patients these sugar-sweetened soft drinks should not be recommended.
Dietary fatty acids consist of saturated and unsaturated fatty acids. Many clinical guidelines suggest that saturated fatty acids should be avoided, but unsaturated fatty acids, particularly omega-3 polyunsaturated fatty acid, are recommended for preventing vascular complications in diabetes [25].
Furthermore, some recent reports, including the Dietary Approaches to Stop Hypertension (DASH) Trial, have shown that a high intake of plant-based proteins has a benefit for controlling blood pressure and preventing CKD progression [26]. However, animal-based proteins are associated with progression of CKD [27, 28]. Collectively, we need to identify an optimal dietary therapy in DKD that is based on quality control of each nutrient, as well as quantity controls.
Hypoglycemia must be avoided, especially in patients who are treated with an insulin analog or oral agents that stimulate insulin secretion independently to blood glucose levels. Symptomatic hypoglycemia is associated with a higher mortality risk [29]. In diabetic patients with renal dysfunction, a hypoglycemic event frequently occurs, which must be prevented. Excess fluid intake also must be avoided for patients who have cardiac failure, renal failure, or nephrotic syndrome. Therefore, fasting carbohydrates that are suitable for patients with renal impairment include dextrose tablets, hard candy, honey, and non-cola regular pop instead of the generally recommended strategy with juice or cola beverages.
Increased proteinuria is a critical prognostic factor for developing CKD, regardless of kidney disease. Most diabetic patients with a CKD stage below G3 showed macroalbuminuria in the 1900s [30]. In contrast, recently, but the number of diabetic patients who have albuminuria has been decreasing, but the number of diabetic patients with a lower eGFR (<60 ml/min/1.73 m2), even without albuminuria, has been increasing [30]. Currently, there is no clinical evidence of diet therapy for diabetic patients who have an early decline in the eGFR. In the future, an optimal dietary strategy for these patients should be provided.
2.4 Mechanisms Behind Dietary Therapy-Related Renoprotection in Experimental Diabetic Kidney Disease and Vascular Damage
Glomerular hypertension related to hyperactivation of the renin–angiotensin system (RAS) and intra- and extracellular metabolic alterations due to hyperglycemia and dyslipidemia are considered typical and classical aspects of the pathogenesis of DKD. Both of these factors lead to increased albuminuria and cell damage in a variety of cells including vascular endothelial cells, mesangial cells, podocytes, and tubular cells. These events synergistically injure the kidney, leading to progression of the stage of DKD.
Among dietary regimens, the mechanism behind protein restriction-mediated renoprotection has been the most extensively examined. Protein levels are linked to the activity of the RAS. Protein overload activates the RAS, whereas protein restriction suppresses the intrarenal RAS activation [31,32,33]. Peters et al. reported that RAS blockade and a low protein diet have additive effects on disease reduction in nephritic rats [34], suggesting that protein restriction exerts an additional mechanism to halt progression of kidney disease beyond RAS inhibitors. Furthermore, dietary protein overload increases the excretion of amino acids from the glomerulus, which leads to the increased reabsorption of amino acids, sodium, and chloride in the proximal tubules, resulting in a deficiency in the chloride levels achieved in the juxtaglomerular apparatus [35]. Subsequently, the tubular glomerular feedback system is activated. Then, the glomerular filtration rate is increased by protein overload [36]. Therefore, the modulation of intraglomerular pressure achieved with a protein restriction theoretically protects against the progression of DKD.
In addition to protein restriction, salt restriction also reduces hyperfiltration [37]. Thus, improvement of hemodynamic changes, particularly glomerular hyperfiltration, should be involved in the renoprotective mechanism of protein and salt restriction, possibly via reducing protein permeability of glomeruli.
Alterations of intra- and extracellular metabolism, such as oxidative stress, activation of PKC signaling, the polyol and hexosamine pathways, and excess accumulation of advanced glycated end products are classical ideas in DKD pathogenesis [38]. All these changes are due to hyperglycemia and dyslipidemia. Thus, amelioration of these pathogenic signals should be involved in the renoprotective mechanism of reducing calorie intake and resultant better body weight, glycemic, and lipid controls.
In addition to the traditional models of the pathogenesis of DKD, novel models of pathogenesis have been proposed experimentally. Vascular calcification is often observed in DKD patients and is associated with higher cardiovascular events and CKD progression [39]. Phosphorus metabolism is also strongly associated with these events. Experimentally, phosphorus toxicity caused vascular calcification-related endothelial dysfunction and CKD progression [40]. Thus, the restriction of dietary phosphorus should receive more attention to prevent vascular injury-related CVD events and DKD progression.
Intracellular nutrient sensing systems are currently being focused on as another promising model for the pathogenesis of DKD [41]. Nutrient-sensing signals and their related intracellular machinery have evolved to combat prolonged periods of starvation in mammals; and these systems are conserved in the kidney. Recent studies have suggested that the activity of three nutrient-sensing signals, mechanistic target of rapamycin complex 1 (mTORC1), AMP-activated protein kinase (AMPK) and mammalian homolog of sirtuin 1 (Sirt1), is altered in the diabetic kidney. In animal models of experimental DKD, hyperactivation of mTORC1 caused severe podocyte injury and obesity-related proximal tubular cell damage [42, 43]. A diabetes-related decrease in AMPK activity is also associated with DKD [44]. Furthermore, Sirt1 activity in proximal tubular cells and podocytes decreased in streptozotocin-induced diabetic mice, which was associated with increased proteinuria [45]. Interestingly, protein restriction suppressed mTORC1 signaling in diabetic kidneys of rats [46] and calorie restriction preserved both Sirt1 and AMPK activation [47]. Thus, normalization of all these signals may be involved in protein restriction- and calorie restriction-mediated renoprotection in DKD.
Furthermore, autophagy activity, which is regulated by the abovementioned nutrient-sensing signals, is also altered in both podocytes and proximal tubular cells under diabetic conditions [43, 48]. Under diabetic conditions, an altered nutritional state owing to nutrient excess may disturb cellular homeostasis regulated by nutrient-sensitive systems, leading to exacerbation of organelle dysfunction and DKD. Interestingly, in diabetic rats, decreased autophagy activity in diabetes was reversed upon protein restriction, which resulted in maintenance of normal mitochondrial morphology and function [46]. Interestingly, excess phosphorus is also likely to weaken autophagy activity. Thus, reactivation of autophagy may play a central role in renoprotection due to protein restriction, calorie restriction, and phosphorus restriction in DKD.
3 Conclusion
This section outlined diet therapy in DKD according to the stages of this disease from the pre-DKD stage to the stage of renal failure. Important questions to consider regarding diet therapy in DKD in the pre-dialysis stages are whether protein restriction should be implemented, and if it should, at what stage and to what degree? However, there are numerous issues that remain to be studied, such as the degree of protein restriction, quality of protein required (animal or plant), and the balance between amino acids to achieve a renoprotective effect.
In routine diagnosis and treatment, a diabetic diet based on energy restriction should be switched to a diet for DKD based on protein restriction with an adequate energy intake to prevent PEM. However, depending on the individual patient’s characteristics, the results can be ambiguous. To avoid this situation, microalbuminuria needs to be correctly diagnosed, and the patient should be educated from this stage of the disease to avoid future development toward renal failure. At any stage of DKD, the type of diet therapy should be tailored to each individual after considering age, compliance, and overall physical condition. Additionally, after introducing diet therapy, the efficacy of the diet needs to be evaluated by monitoring body weight, performing a nutritional evaluation, conducting a physical examination, and compliance over time.
References
Whitham D. Nutrition for the prevention and treatment of chronic kidney disease in diabetes. Can J Diabetes. 2014;38(5):344–8.
Look ARG, Pi-Sunyer X, Blackburn G, Brancati FL, Bray GA, Bright R, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care. 2007;30(6):1374–83.
Morales E, Valero MA, Leon M, Hernandez E, Praga M. Beneficial effects of weight loss in overweight patients with chronic proteinuric nephropathies. Am J Kidney Dis. 2003;41(2):319–27.
Halbesma N, Bakker SJ, Jansen DF, Stolk RP, De Zeeuw D, De Jong PE, et al. High protein intake associates with cardiovascular events but not with loss of renal function. J Am Soc Nephrol. 2009;20(8):1797–804.
Walrand S, Short KR, Bigelow ML, Sweatt AJ, Hutson SM, Nair KS. Functional impact of high protein intake on healthy elderly people. Am J Physiol Endocrinol Metab. 2008;295(4):E921–8.
Uzu T, Nakao K, Kume S, Araki H, Isshiki K, Araki S, et al. High sodium intake is associated with masked hypertension in Japanese patients with type 2 diabetes and treated hypertension. Am J Hypertens. 2012;25(11):1170–4.
Kanauchi N, Ookawara S, Ito K, Mogi S, Yoshida I, Kakei M, et al. Factors affecting the progression of renal dysfunction and the importance of salt restriction in patients with type 2 diabetic kidney disease. Clin Exp Nephrol. 2015;19(6):1120–6.
Parvanova A, Trillini M, Podesta MA, Iliev IP, Ruggiero B, Abbate M, et al. Moderate salt restriction with or without paricalcitol in type 2 diabetes and losartan-resistant macroalbuminuria (PROCEED): a randomised, double-blind, placebo-controlled, crossover trial. Lancet Diabetes Endocrinol. 2018;6(1):27–40.
Taylor RS, Ashton KE, Moxham T, Hooper L, Ebrahim S. Reduced dietary salt for the prevention of cardiovascular disease: a meta-analysis of randomized controlled trials (Cochrane review). Am J Hypertens. 2011;24(8):843–53.
Araki S, Haneda M, Koya D, Kondo K, Tanaka S, Arima H, et al. Urinary potassium excretion and renal and cardiovascular complications in patients with type 2 diabetes and normal renal function. Clin J Am Soc Nephrol. 2015;10(12):2152–8.
Hansen HP, Tauber-Lassen E, Jensen BR, Parving HH. Effect of dietary protein restriction on prognosis in patients with diabetic nephropathy. Kidney Int. 2002;62(1):220–8.
Koya D, Haneda M, Inomata S, Suzuki Y, Suzuki D, Makino H, et al. Long-term effect of modification of dietary protein intake on the progression of diabetic nephropathy: a randomised controlled trial. Diabetologia. 2009;52(10):2037–45.
Nezu U, Kamiyama H, Kondo Y, Sakuma M, Morimoto T, Ueda S. Effect of low-protein diet on kidney function in diabetic nephropathy: meta-analysis of randomised controlled trials. BMJ Open. 2013;3(5):e002934.
Pan Y, Guo LL, Jin HM. Low-protein diet for diabetic nephropathy: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2008;88(3):660–6.
Ideura T, Shimazui M, Morita H, Yoshimura A. Protein intake of more than 0.5 g/kg BW/day is not effective in suppressing the progression of chronic renal failure. Contrib Nephrol. 2007;155:40–9.
Pupim LB, Cuppari L, Ikizler TA. Nutrition and metabolism in kidney disease. Semin Nephrol. 2006;26(2):134–57.
Stenvinkel P, Heimburger O, Paultre F, Diczfalusy U, Wang T, Berglund L, et al. Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int. 1999;55(5):1899–911.
Da J, Xie X, Wolf M, Disthabanchong S, Wang J, Zha Y, et al. Serum phosphorus and progression of CKD and mortality: a meta-analysis of cohort studies. Am J Kidney Dis. 2015;66(2):258–65.
Bjornstad P, Lanaspa MA, Ishimoto T, Kosugi T, Kume S, Jalal D, et al. Fructose and uric acid in diabetic nephropathy. Diabetologia. 2015;58(9):1993–2002.
Ficociello LH, Rosolowsky ET, Niewczas MA, Maselli NJ, Weinberg JM, Aschengrau A, et al. High-normal serum uric acid increases risk of early progressive renal function loss in type 1 diabetes: results of a 6-year follow-up. Diabetes Care. 2010;33(6):1337–43.
Jalal DI, Rivard CJ, Johnson RJ, Maahs DM, McFann K, Rewers M, et al. Serum uric acid levels predict the development of albuminuria over 6 years in patients with type 1 diabetes: findings from the Coronary Artery Calcification in Type 1 Diabetes study. Nephrol Dial Transplant. 2010;25(6):1865–9.
Stirpe F, Della Corte E, Bonetti E, Abbondanza A, Abbati A, De Stefano F. Fructose-induced hyperuricaemia. Lancet. 1970;2(7686):1310–1.
Cox CL, Stanhope KL, Schwarz JM, Graham JL, Hatcher B, Griffen SC, et al. Consumption of fructose- but not glucose-sweetened beverages for 10 weeks increases circulating concentrations of uric acid, retinol binding protein-4, and gamma-glutamyl transferase activity in overweight/obese humans. Nutr Metab (Lond). 2012;9(1):68.
Choi JW, Ford ES, Gao X, Choi HK. Sugar-sweetened soft drinks, diet soft drinks, and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2008;59(1):109–16.
Shapiro H, Theilla M, Attal-Singer J, Singer P. Effects of polyunsaturated fatty acid consumption in diabetic nephropathy. Nat Rev Nephrol. 2011;7(2):110–21.
Rebholz CM, Crews DC, Grams ME, Steffen LM, Levey AS, Miller ER 3rd, et al. DASH (dietary approaches to stop hypertension) diet and risk of subsequent kidney disease. Am J Kidney Dis. 2016;68(6):853–61.
Haring B, Selvin E, Liang M, Coresh J, Grams ME, Petruski-Ivleva N, et al. dietary protein sources and risk for incident chronic kidney disease: results from the Atherosclerosis Risk in Communities (ARIC) study. J Ren Nutr. 2017;27(4):233–42.
Lew QJ, Jafar TH, Koh HW, Jin A, Chow KY, Yuan JM, et al. Red meat intake and risk of ESRD. J Am Soc Nephrol. 2017;28(1):304–12.
Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376(9739):419–30.
Afkarian M, Zelnick LR, Hall YN, Heagerty PJ, Tuttle K, Weiss NS, et al. Clinical manifestations of kidney disease among US adults with diabetes, 1988–2014. JAMA. 2016;316(6):602–10.
Martinez-Maldonado M, Benabe JE, Wilcox JN, Wang S, Luo C. Renal renin, angiotensinogen, and ANG I-converting-enzyme gene expression: influence of dietary protein. Am J Phys. 1993;264(6 Pt 2):F981–8.
Benabe JE, Fernandez-Repollet E, Tapia E, Luo C, Martinez-Maldonado M. Angiotensin II and catecholamines interaction in short-term low protein feeding. Kidney Int. 1993;44(2):285–93.
Benabe JE, Wang S, Wilcox JN, Martinez-Maldonado M. Modulation of ANG II receptor and its mRNA in normal rat by low-protein feeding. Am J Phys. 1993;265(5 Pt 2):F660–9.
Peters H, Border WA, Noble NA. Angiotensin II blockade and low-protein diet produce additive therapeutic effects in experimental glomerulonephritis. Kidney Int. 2000;57(4):1493–501.
Gonska T, Hirsch JR, Schlatter E. Amino acid transport in the renal proximal tubule. Amino Acids. 2000;19(2):395–407.
Sallstrom J, Carlstrom M, Olerud J, Fredholm BB, Kouzmine M, Sandler S, et al. High-protein-induced glomerular hyperfiltration is independent of the tubuloglomerular feedback mechanism and nitric oxide synthases. Am J Physiol Regul Integr Comp Physiol. 2010;299(5):R1263–8.
Lau C, Sudbury I, Thomson M, Howard PL, Magil AB, Cupples WA. Salt-resistant blood pressure and salt-sensitive renal autoregulation in chronic streptozotocin diabetes. Am J Physiol Regul Integr Comp Physiol. 2009;296(6):R1761–70.
Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54(6):1615–25.
Sigrist MK, Taal MW, Bungay P, McIntyre CW. Progressive vascular calcification over 2 years is associated with arterial stiffening and increased mortality in patients with stages 4 and 5 chronic kidney disease. Clin J Am Soc Nephrol. 2007;2(6):1241–8.
Scialla JJ, Lau WL, Reilly MP, Isakova T, Yang HY, Crouthamel MH, et al. Fibroblast growth factor 23 is not associated with and does not induce arterial calcification. Kidney Int. 2013;83(6):1159–68.
Kume S, Thomas MC, Koya D. Nutrient sensing, autophagy, and diabetic nephropathy. Diabetes. 2012;61(1):23–9.
Inoki K, Mori H, Wang J, Suzuki T, Hong S, Yoshida S, et al. mTORC1 activation in podocytes is a critical step in the development of diabetic nephropathy in mice. J Clin Invest. 2011;121(6):2181–96.
Yamahara K, Kume S, Koya D, Tanaka Y, Morita Y, Chin-Kanasaki M, et al. Obesity-mediated autophagy insufficiency exacerbates proteinuria-induced tubulointerstitial lesions. J Am Soc Nephrol. 2013;24(11):1769–81.
Zhao J, Miyamoto S, You YH, Sharma K. AMP-activated protein kinase (AMPK) activation inhibits nuclear translocation of Smad4 in mesangial cells and diabetic kidneys. Am J Physiol Renal Physiol. 2015;308(10):F1167–77.
Hasegawa K, Wakino S, Simic P, Sakamaki Y, Minakuchi H, Fujimura K, et al. Renal tubular Sirt1 attenuates diabetic albuminuria by epigenetically suppressing Claudin-1 overexpression in podocytes. Nat Med. 2013;19(11):1496–504.
Kitada M, Ogura Y, Suzuki T, Sen S, Lee SM, Kanasaki K, et al. A very-low-protein diet ameliorates advanced diabetic nephropathy through autophagy induction by suppression of the mTORC1 pathway in Wistar fatty rats, an animal model of type 2 diabetes and obesity. Diabetologia. 2016;59(6):1307–17.
Kume S, Uzu T, Horiike K, Chin-Kanasaki M, Isshiki K, Araki S, et al. Calorie restriction enhances cell adaptation to hypoxia through Sirt1-dependent mitochondrial autophagy in mouse aged kidney. J Clin Invest. 2010;120(4):1043–55.
Tagawa A, Yasuda M, Kume S, Yamahara K, Nakazawa J, Chin-Kanasaki M, et al. Impaired podocyte autophagy exacerbates proteinuria in diabetic nephropathy. Diabetes. 2016;65(3):755–67.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kume, S. (2021). Nutrition and Diet Therapy for DKD. In: Wada, T., Furuichi, K., Kashihara, N. (eds) Diabetic Kidney Disease. Springer, Singapore. https://doi.org/10.1007/978-981-15-9301-7_7
Download citation
DOI: https://doi.org/10.1007/978-981-15-9301-7_7
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-9300-0
Online ISBN: 978-981-15-9301-7
eBook Packages: MedicineMedicine (R0)