Abstract
Background
Type 2 diabetic kidney disease (DKD) is the most common cause of end-stage renal failure, and the prevention of its progression has been a topic of discussion.
Methods
Sixty type 2 DKD patients were retrospectively evaluated for 1 year. Factors independently affecting the annual Ccr decline were examined by multivariable linear regression analysis. Patients were further divided into 2 groups based on their degree of renal function, and between-group differences at study initiation were evaluated.
Results
Ccr values were 21.0 ± 11.8 mL/min/1.73 m2 at study initiation, and 15.7 ± 10.9 mL/min/1.73 m2 after 1 year of observation. The multivariable linear regression analysis indicated salt intake (standardized coefficient: −0.34, P = 0.010) and urinary protein excretion (standardized coefficient: −0.33, P = 0.011) to be factors independently affecting the annual Ccr decline. Although decliners (−9.8 ± 4.7 mL/min/1.73 m2/year) had a significantly higher salt intake than non-decliners (−1.1 ± 3.8 mL/min/1.73 m2/year) at study initiation, this difference disappeared at the end of the study as a result of intensive dietary education. In 21 decliners with an additional year of follow-up, the annual Ccr decline significantly improved from −10.1 ± 5.3 to −5.3 ± 7.4 mL/min/1.73 m2/year (P = 0.02).
Conclusion
Salt intake and urinary protein excretion were associated with annual Ccr decline in type 2 DKD patients. Furthermore, dietary education covering salt intake may have positively affected the change in Ccr.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic kidney disease (DKD), which develops in more than 40 % of type 2 diabetes patients, is one of the most important and common causes of end-stage renal disease [1–3]. This condition is characterized by persistent albuminuria, elevated blood pressure (BP), and a progressive decline in renal function [4, 5]. Thus far, several investigations of factors associated with kidney disease progression in type 2 diabetes have been reported. These studies have shown that age, HbA1c, insulin treatment, estimated glomerular filtration rate (eGFR) levels, systolic BP, hypertension, serum uric acid, serum albumin, hemoglobin, albuminuria, and proteinuria have significant relationships with the decline of renal function [6–9]. However, the nature of the relationship among the various factors and the decline of renal function varied from study to study, highlighting the need to better understand these associated risk factors. Furthermore, diabetes is known to be a salt-sensitive condition, and salt intake is a major risk factor for increased BP [10]. However, investigations of the impact of salt intake on the decline of renal function in type 2 DKD patients are scarce.
In this study, we evaluated the creatinine clearance rate (Ccr) calculated by 24-h urine collection as a marker of type 2 DKD progression. The aims of the present study were (1) to clarify factors affecting the annual Ccr decline in patients with type 2 DKD, and (2) to examine differences in clinical parameters according to the degree of annual Ccr decline in type 2 DKD patients (decliners vs. non-decliners).
Methods
Patients and study design
This retrospective observational study included 60 patients who met the following criteria: (1) type 2 DKD patients who were followed-up at the divisions of nephrology and endocrinology of our hospital for more than 1 year since January 2009, (2) A Ccr <60 mL/min/1.73 m2 as calculated by 24-h urine collection at the initiation of this study, (3) A Ccr measurement by 24-h urine collection performed at the end of this study, and (4) not receiving dialysis treatment at the time of study initiation.
At the time of study initiation, all patients had already received dietary education on the management of caloric intake and protein and salt restriction. Educational sessions were scheduled to take place when patients received medical examination at our divisions and reached 7.2 ± 2.7 times on average during the study period. This study was approved by the Institutional Review Board of our hospital (RIN 13–36) and conforms to the provisions of the Declaration of Helsinki (as revised in Tokyo, 2004).
We collected and retrospectively analyzed socio-demographic patient data, including age, gender, duration of diabetes and anti-hypertensive treatment with diuretics, angiotensin-converting enzyme inhibitors (ACEI), angiotensin receptor blockers (ARB), and calcium channel blockers (CCB), and biochemical variables. Energy intake was calculated by dietitians based on each patient’s daily meal record. Furthermore, 24-h urine collection was performed in each patient for the evaluation of urinary protein excretion (g/day), urinary urea nitrogen (UUN) excretion, and urinary Na+ excretion. The urine collection method was as follows: 24-h urine collection was started in the morning after the first morning urine was discarded in the patient’s toilet. Thereafter, the entire volume of urine was collected in a disposable container with a 3 L volume. To avoid the possibility of inadequate urine collection, we trained all patients to properly collect their urine samples and reinforced that 24-h urine collection must be initiated at a specific time and then completed at the same time the next day. Based on the values of UUN and urinary Na+ excretion obtained from the 24-h urine collection, we calculated the daily protein and salt intakes.
Protein intake was calculated using Maroni’s equation [11], described below:
where BW is the body weight (kg).
Salt intake was calculated using the following equation:
Evaluation of type 2 DKD progression
Progression of type 2 DKD was evaluated according to the annual decline of Ccr, which was measured by 24-h urine collection and calculated using the following equation:
where S-Cr is the serum creatinine concentration (mg/dL).
Furthermore, eGFR was calculated by using the following equation [12],
The annual Ccr or eGFR decline was calculated as the difference between these values at the initiation and the end (after 1 year of observation) of this study. We evaluated the annual Ccr or eGFR decline as a marker of disease progression for each patient throughout the follow-up period, and a multivariable linear regression analysis was performed to identify factors that independently affect the annual Ccr or eGFR decline at study initiation, respectively. Patients were further divided into the following 2 groups based on their degree of annual Ccr decline: a “decliners” group made up of patients (n = 30) with bottom-to-middle values of annual Ccr decline and a “non-decliners” group made up of patients (n = 30) with middle-to-upper (i.e., preserved) values of annual Ccr change. Between-group differences in clinical parameters at study initiation were evaluated. Ten patients showed a gradual deterioration of renal function and had to initiate hemodialysis therapy. In these cases, the patients were evaluated until just before HD initiation, and annual Ccr declines were calculated using Ccr values from study initiation up until HD initiation.
Statistical analysis
Data are expressed as mean ± SD. Student’s t test for non-paired values was used for comparisons. The Chi-square test was used to compare the utilization and distribution of anti-hypertensive medications and statins. Correlations between the 2 were evaluated by Pearson’s correlation coefficient and linear regression analysis. Variables that had a significant correlation with annual Ccr decline in a simple linear regression analysis were included in the multivariable linear regression analysis to clarify factors affecting Ccr decline in type 2 DKD patients.
Results
Demographic and clinical characteristics of all patients are shown in Table 1. The mean age was 67.6 ± 10.1 years, the duration of diabetes was 15.9 ± 8.7 years, and body mass index (BMI) was 24.8 ± 4.1 kg/m2. The value of Ccr was 21.0 ± 11.3 mL/min/1.73 m2 at study initiation, and 15.7 ± 10.9 mL/min/1.73 m2 after 1 year of observation, and the eGFR at initiation was 19.3 ± 10.7 mL/min/1.73 m2, while it was 14.3 ± 10.2 mL/min/1.73 m2 after 1 year. Thus, the annual Ccr and eGFR decline were −5.3 ± 6.5 mL/min/1.73 m2/year and −5.0 ± 4.7 mL/min/1.73 m2/year, respectively.
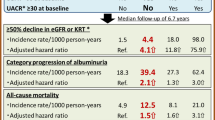
Table 2 shows correlations between annual Ccr or eGFR declines and clinical parameters at study initiation in a simple linear regression analysis. Systolic and diastolic BP, serum albumin concentration, total cholesterol, urinary protein excretion, and sodium intake significantly correlated with both annual Ccr and eGFR decline, respectively. However, only protein intake significantly correlated with annual Ccr decline. We further performed a multivariable linear regression analysis using variables that showed a significant correlation with annual Ccr or eGFR decline in the simple linear regression analysis. Multivariable regression analysis showed that the annual Ccr declines were independently associated with salt intake (standardized coefficient: −0.34, P = 0.010) and urinary protein excretion (standardized coefficient: −0.33, P = 0.011), whereas the annual eGFR declines were only associated with urinary protein excretion (standardized coefficient: −0.69, P < 0.01), and not associated with salt intake (standardized coefficient: −0.10, P = 0.37).
A comparison between decliners and non-decliners based on the annual Ccr declines showed no between-group differences in terms of the utilization and distribution of anti-hypertensive medications and statins. Furthermore, histamine receptor type 2 blockers including cimetidine, which are well known to inhibit tubular creatinine secretion, were taken by only 3 patients in the decliner group and 4 patients in the non-decliner group. Table 3 summarizes the differences between the 2 groups in clinical parameters at study initiation. The annual decline in Ccr was −9.8 ± 4.7 mL/min/1.73 m2/year (−25.0 to −5.4 mL/min/1.73 m2/year) in the decliners and −1.1 ± 3.8 mL/min/1.73 m2/year (−5.0 to 10.2 mL/min/1.73 m2/year) in the non-decliners although there were no differences in the distribution of chronic kidney disease (CKD) stage according to the CKD guidelines edited by the Japanese Society of Nephrology [12]. Decliners had significantly higher levels of systolic and diastolic BP, Ccr, serum Na, urinary protein excretion, protein intake, and salt intake compared to those in non-decliners. In particular, the number of patients with nephrotic range proteinuria (urinary protein excretion ≥3.5 g/day) was significantly higher in the decliner group than in the non-decliner group (decliners: 14 patients, non-decliners: 5 patients, P = 0.01). As shown in Table 4, there were no significant differences between decliners and non-decliners in the number of dietary education sessions provided during the study (decliners: 6.8 ± 2.9 times, non-decliners: 7.2 ± 2.7 times). Salt intake significantly decreased in decliners throughout the year of dietary education from 10.6 ± 4.3 to 7.5 ± 3.0 g/day (P < 0.05), and the between-group differences in clinical parameters including systolic and diastolic BP at the end of this study were not significant. In this study, 17 decliners and 15 non-decliners had an increase in the number of antihypertensive medicines. The number of antihypertensive medicines at study end significantly increased in comparison with that at study initiation in both decliners and non-decliners (decliners: 3.6 ± 1.4 at initiation, 4.2 ± 1.7 at study end; non-decliners: 3.5 ± 1.6 at initiation, 3.9 ± 1.5 at study end, P < 0.05, respectively), whereas there was no significant difference in the number of antihypertensive medicines used at both study initiation and end between decliners and non-decliners (Table 5). In 21 decliners with an additional year of follow-up data as shown in Fig. 1, salt intake at the end of an additional year was 7.8 ± 3.1 g/day, which was no significant difference compared with those at study end, and the annual Ccr decline significantly improved from −10.1 ± 5.3 to −5.3 ± 7.4 mL/min/1.73 m2/year (P = 0.02), whereas for 15 non-decliners with an additional year of follow-up data, salt intake at the end of an additional year was 7.7 ± 3.1 g/day, which was similar to the level at study end (7.4 ± 2.7 g/day), and there was no significant difference in annual Ccr decline between that at study end and after an additional year (end: −0.7 ± 3.1 mL/min/1.73 m2/year; additional year: −2.9 ± 3.1 mL/min/1.73 m2/year, P = 0.07). Furthermore, there were no significant differences in the annual Ccr declines (decliners, −5.3 ± 7.4 mL/min/1.73 m2/year; non-decliners, −2.9 ± 3.1 mL/min/1.73 m2/year; P = 0.26) and salt intake (decliners, 7.8 ± 3.1 g/day; non-decliners, 7.7 ± 3.1 g/day; P = 0.96) between decliners and non-decliners at the end of the additional year.
Discussion
Diabetes itself raises salt-sensitivity, and salt intake leads to salt-sensitive hypertension. It was previously reported that salt consumption is a major risk factor for increased BP and that salt restriction (at least less than 5–6 g/day) reduced BP in type 2 diabetes [10]. Experimental studies have also reported that chronic salt overload leads to a BP increase in diabetes mellitus, but not in non- diabetes mellitus, and that BP levels were positively correlated with urinary sodium excretion in diabetes mellitus patients [13]. In the present study, salt intake at study initiation was the strongest factor affecting the annual declines in Ccr among type 2 DKD patients and was significantly higher in decliners than in non-decliners. Furthermore, decliners showed significantly higher systemic BP levels and serum Na concentrations at study initiation. Therefore, a disorder of sodium metabolism, including the increase of salt intake and the decrease of sodium excretion, would affect the progression of renal dysfunction in type 2 DKD patients. We provided intensive dietary education to all patients during this study, and the number of education sessions reached 7.2 ± 2.7 times on average. As a result of these education sessions, salt intake significantly decreased at the end of this study, and the significant differences in systemic BP, urinary protein excretion, and salt intake between decliners and non-decliners at study initiation completely disappeared at the end of this study. Furthermore, in decliners who were available for follow-up 1 year later, annual Ccr declines were compared with those of the prior year to confirm the effect of salt restriction, and showed significant improvement. Thus, salt restriction through dietary education would be effective for maintaining renal function in type 2 DKD patients. Urinary protein excretion at study initiation was also independently associated with annual Ccr declines. Proteinuria/albuminuria has been previously reported to accelerate the progression of type 2 DKD [6–9] and our result is thought to be consistent with previous reports. With regard to urinary protein excretion, proteinuria and albuminuria have been reported as major risk factors for the progression of type 2 DKD patients [14, 15]. Furthermore, experimental data suggest that proteinuria per se may contribute to glomerular and tubulointerstitial damage [16]. To reduce proteinuria in type 2 DKD patients, the use of ACEIs/ARBs and CCBs (L/T type and L/N type) has been recommended [17, 18]. The renoprotective mechanism of these medicines is mainly a reduction in intraglomerular pressure via vasodilation of the glomerular efferent artery [18, 19]. In fact, about 80 % of patients in this study had been taking ACEIs/ARBs and CCBs prior to the examination. Therefore, based on our results, persistent proteinuria would affect the deterioration of renal function even while taking these medications. Regarding the non-significant improvement in BP and decrease of proteinuria observed among decliners at the end of this study, the effect of dietary education, especially in terms of the significant decrease of salt intake, might be pointed out. Salt restriction has the potential to decrease sodium retention, improve body-fluid status, lead to BP improvement, and reduce proteinuria. The significant improvement of the annual Ccr decline over the following year in decliners would be associated with the favorable effects of BP improvement and proteinuria reduction in addition to the significant decrease of salt intake.
As a marker of renal function, many types of eGFR calculation methods based on data including serum creatinine concentration, age, sex, and so on have been proposed and widely accepted in clinical settings in many countries. However, in patients with chronic kidney disease, some eGFR equations have a large bias at eGFRs less than 60 mL/min/1.73 m2, and the evaluation of renal dysfunction using an eGFR calculation would misguide the classification of chronic kidney disease [20]. In addition, a significant difference between eGFR and Ccr measured through 24-hour urine collection at eGFR values less than 60 mL/min/1.73 m2 was previously reported [21]. This difference between the eGFR and Ccr values was believed to be due to the fact that the concept of eGFR was originally developed for epidemiologic research and not for clinical evaluation of renal function in patients with altered renal function [22]. Furthermore, in a renal drug dose algorithm approved by the Food and Drug Administration, Ccr measured from 24-h urine collection is recommended for evaluating renal function rather than eGFR [23] although it is desirable to measure both markers to evaluate renal dysfunction in patients with CKD. In this study, urinary protein excretion was associated with annual declines in Ccr and eGFR; however, salt intake was only associated with annual declines in Ccr, not in eGFR. Therefore, the progression of renal function was evaluated using annual declines in Ccr rather than eGFR, and we further examined the effect of salt restriction on the annual Ccr declines in type 2 DKD patients.
With the exception of salt intake and urinary protein excretion, there were no associations between annual Ccr decline and other clinical parameters in our study. Notably, restriction of protein intake is known to be a treatment strategy for the preservation of renal function via improvement of renal hemodynamics including intraglomerular hypertension. Restriction of protein intake in type 1 diabetes had been reported to reduce the risk for decline in GFR or Ccr or the risk for an increase in urinary albumin excretion [24]. On the other hand, convincing data indicating whether the restriction of protein intake in type 2 DKD patients can preserve their renal function are still lacking [25, 26]. In this study, although protein intake had a significant association with annual Ccr decline in a simple linear regression analysis, this association was absent in a multivariable regression analysis. Thus, we also cannot demonstrate an association between protein intakes and type 2 DKD progression on the basis of this study.
Regarding the limitations of this study, the sample size was relatively small, and the observation period lasted 1–2 years, which was also relatively short. Therefore, longer studies with adequate dietary therapy will be required to confirm the associations of annual Ccr declines with salt intake and urinary protein excretion we found in type 2 DKD patients.
Conclusion
The findings of this study suggest that salt intake and urinary protein excretion are associated with annual Ccr decline in type 2 DKD patients. Moreover, dietary education covering salt intake may have positively affected the change in Ccr in this study.
References
Rotz E, Rychlik I, Locatelli F, Halimi S. End stage renal failure in type 2 diabetes: a medical catastrophe of world wide dimensions. Am J Kidney Dis. 1999;34:795–808.
Byme C, Steenkamp R, Castledine C, Ansell D, Feehally J. UK renal registry 12th annual report: chapter 4: UK ESRD prevalent rates in 2008: national and centre-specific analysis. Nephron Clin Pract. 2010;115(Suppl 1):c41–67.
Nakai S, Iseki K, Itami N, Ogata S, Kazama JJ, Kimata N, et al. An overview of regular dialysis treatment in Japan. Ther Apher Dial. 2012;16:483–521.
Gall MA, Nielsen FS, Smidt UM, Parving HH. The course of kidney function in type 2 (non-insulin-dependent) diabetic patients with diabetic nephropathy. Diabetologia. 1993;36:1071–8.
American Diabetes Association. Standards of medical care in diabetes-2011. Diabetes Care. 2011;34(Suppl 1):S11–61.
Rossing K, Christensen PK, Hovind P, Tarnow L, Rossing P, Parving HH. Progression of nephropathy in type 2 diabetic patients. Kidney Int. 2004;66:1596–605.
Unsal A, Koc Y, Basturk T, Akgun AO, Sakaci T, Ahbap E. Risk factors for progression of renal disease in patient with diabetic nephropathy. Eur Rev Med Pharmacol Sci. 2012;16:878–83.
Zoppini G, Targher G, Chonchol M, Ortalda V, Negri C, Stoico V, Bonora E. Predicted of estimated GFR decline in patients with type 2 diabetes and preserved kidney function. Clin J Am Soc Nephrol. 2012;7:401–8.
Altemtam N, Russell J, Nahas ME. A study of the natural history of diabetic kidney disease (DKD). Nephrol Dial Transplant. 2012;27:1847–54.
Suckling RJ, He FJ, Macgregor GA. Alterd dietary salt intake for preventing and treating diabetic kidney disease. Cochrane Database Syst Rev. 2010;8:CD006763. doi:10. 1002/14651858. CD006763.pub2.
Maroni BJ, Steinman TI, Mitch WE. A method for estimating nitrogen intake of patients with chronic renal failure. Kidney Int. 1985;27:58–65.
Japan Nephrology Society. Special issue. Clinical practice guidebook for diagnosis and treatment of chronic kidney disease 2012. Nihon Jinzo Gakkai Shi. 2012;54:1034–191.
Maeda CY, Schaan BD, Oliveira E, Oliveira V, De Angelis KD, Irigoyen MC. Chronic salt loading and cardiovascular-associated changes in experimental diabetes in rats. Clin Exp Pharmacol Physiol. 2007;34:574–80.
Keane WF, Brenner BM, de Zeeuw D, Grunfeld JP, Mcgrill J, Mitch WE, Ribeiro AB, Shahinfar S, Simpson RL, Snapinn SM, Toto R. The risk of developing end-stage renal disease in patients with type 2 diabetes and nephropathy: The RENAAL Study. Kidney Int. 2003;63:1499–507.
Rossing K, Christensen PK, Hovind P, Tarnow L, Rossing P, Parving HH. Progression of nephropathy in type 2 diabetic patients. Kidney Int. 2004;66:1596–605.
Remuzzi G, Bertani T. Is glomerulosclerosis a consequence of altered glomerular permeability to macromolecules? Kidney Int. 1990;38:384–94.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Struijker Boudier HA, Zanchetti A. Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;2007(25):1105–87.
Hayashi K, Wakino S, Sugano N, Ozawa Y, Homma K, Saruta T. Ca2+ channel subtypes and pharmacology in the kidney. Circ Res. 2007;100:342–53.
Kobori H, Mori H, Masaki T, Nishiyama A. Angiotensin II blockade and renal protection. Curr Pharm Des. 2013;19:3033–42.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Diamandopoulos A, Goudas P, Arvanitis A. Comparison of estimated creatinine clearance among five formulae (Cockroft–Gault, Jelliffe, Sanaka, simplified 4-variable MDRD and DAF) and the 24 h-urine-collection creatinine clearance. Hippokratia. 2010;14:98–104.
Dowling TC, Wang ES, Ferrucci L, Sorkin JD. Glomerular filtration rate equations overestimate creatinine clearance in older individuals enrolled in the Baltimore Longitudinal Study on aging: impact on renal drug dosing. Pharmacotherapy. 2013;33:912–21.
Dowling TC, Matzke GR, Murphy JE, Burckart GL. Evaluation of renal drug dosing: prescribing information and clinical pharmacist approaches. Pharmacology. 2010;30:776–86.
Pedrini MT, Levey AS, Lau J, Chalmers TC, Wang PH. The effect of dietary protein restriction on the progression of diabetic and nondiabetic renal disease: a meta-analysis. Ann Intern Med. 1996;124:627–32.
Koya D, Haneda M, Inomata S, Suzuki Y, Suzuki D, Makino H, Shikata K, Murakami Y, Tomino Y, Yamada K, Araki SI, Kashiwagi A, Kikkawa R. Low-protein diet study group. Long-term effect of modification of dietary protein intake on the progression of diabetic nephropathy: a randomized controlled trial. Diabetologia. 2009;52:2037–45.
Williams ME, Stanton R. Chapter 31-nutritional and metabolic management of the diabetic patients with chronic kidney disease and chronic renal failure. In: Kopple JD, Massry SG, Kalantar-Zadeh K, editors. Nutritional management of renal disease. 1st ed. Amsterdam: Elsevier; 2013. p. 485–502.
Conflict of interest
The authors have declared that no conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kanauchi, N., Ookawara, S., Ito, K. et al. Factors affecting the progression of renal dysfunction and the importance of salt restriction in patients with type 2 diabetic kidney disease. Clin Exp Nephrol 19, 1120–1126 (2015). https://doi.org/10.1007/s10157-015-1118-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-015-1118-y