Abstract
Respiratory viruses causing seasonal epidemics in the community are called community-acquired respiratory viruses (CARVs). CARVs include RNA viruses such as human rhinovirus, human respiratory syncytial virus, human parainfluenza virus, human coronavirus, human metapneumovirus, human enterovirus, human parechovirus, and DNA viruses such as human adenovirus and human bocavirus. Needless to say, influenza-like illness (ILI) is caused not only by influenza virus but also by other CARVs. Epidemiological studies targeting ILI patients revealed that CARVs other than influenza are universally detected, predominantly the rhinovirus. However, the viral etiology of ILI is affected by many factors such as the study population, season, setting (community or outpatient or inpatient), and regions. Previous studies investigated the utility of fever and cough as clinical diagnosis markers of influenza, nonetheless the sensitivity and specificity were modest. Since CARVs fairly cause respiratory and general symptoms including fever, cough, coryza, sore throat, headache, myalgia, and chills, predicting the causative virus by clinical symptoms is further difficult in most cases, except for diseases presenting with unique features such as laryngotracheobronchitis (croup), herpangina, and hand-foot-and-mouth disease. Consequently, clinical manifestations are not reliable enough for the differential diagnosis between influenza and other CARVs infection, therefore a rapid antigen test or molecular assay is critical to confirm the causative virus.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Respiratory viruses causing seasonal epidemics in the community are called community-acquired respiratory viruses (CARVs). Besides influenza virus, CARVs include human rhinovirus (HRV), human respiratory syncytial virus (RSV), human parainfluenza virus (HPIV), human adenovirus (HAdV), human coronavirus (HCoV), human metapneumovirus (HMPV), human bocavirus (HBoV), human enterovirus (HEV), and human parechovirus (HPeV). CARVs usually cause temporally upper respiratory tract infections in immunocompetent individuals; however, they can also cause severe lower respiratory tract infections (LRTIs) in susceptible individuals such as infants, elders, and immunocompromised patients. Although a vaccine and antiviral treatment have been established only against the influenza virus, knowledge about each CARV is also important from the perspective of clinical practice and infection control. This chapter focuses on CARVs other than influenza virus. Each CARV is briefly overviewed at the beginning, and then clinical aspects, emphasizing on the differential diagnosis between influenza and other respiratory viral infections, are discussed.
2 Brief Summary of CARVs
In this section, basic information for each CARV is briefly described. The taxonomy for CARVs is summarized in Table 8.1.
2.1 Human Rhinovirus (HRV)
HRV, first reported in 1956 [1], is a single-stranded, positive-sense RNA virus that belongs to the family Picornaviridae. The name originally derived from “rhinos” in Greek, meaning “of the nose.” HRV consists of more than 160 serotypes and is classified into three genotypes (A, B, and C) [2]. Although previous studies indicated that HRV-C was more virulent than other genotypes, being associated with asthma exacerbation and LRTIs, recent studies showed that specific genotypes are not linked to illness severity [3].
HRV is known as the most common virus causing mild self-limiting upper respiratory tract infections across all age groups; however, HRV can also cause severe LRTIs in immunocompromised patients [4]. Seo et al. reported that the mortality of transplant recipients with HRV present in the lower respiratory tract was as high as the rates of other viral pneumonias caused by RSV, HPIV, and influenza virus [5]. Respiratory viral infections often cause asthma exacerbation and chronic obstructive pulmonary disease (COPD), and HRV is known as the most detected virus in such vulnerable patients [6, 7]. Moreover, experimental inoculation studies revealed that HRV infection induced asthma exacerbations and COPD in human subjects [8,9,10].
2.2 Human Respiratory Syncytial Virus (RSV)
RSV, reclassified into the family Pneumoviridae in 2016 (previously Paramyxoviridae), is a single-stranded, negative-sense RNA virus. This virus was firstly isolated from chimpanzees in 1955, and shortly thereafter detected in infants with respiratory symptoms [11]. There are two genotypes (RSV-A and RSV-B) and no difference in virulence was shown in previous studies between genotypes [12, 13]. Approximately 60% of infants under 1-year-old experience a RSV infection and almost all children become infected with this virus at least once by the age of 2 or 3 years old [14]. RSV is the most common virus causing bronchiolitis and pneumonia in infants. A multicenter study targeting 5067 children revealed that RSV was detected in 18% of all children with acute respiratory infections, and that 61% of these patients required hospitalization. Additionally, 2–3% of children younger than 12 months were hospitalized annually due to RSV infections in the United States [15]. RSV also causes LRTIs and exacerbations of underlying diseases in adults, especially in the elderly and in immunocompromised patients [16].
2.3 Human Parainfluenza Virus (HPIV)
HPIV, first isolated from infants with croup in 1956 [17], is a single-stranded, negative-sense RNA virus belonging to the family Paramyxoviridae. There are four serotypes (1, 2, 3, and 4); HPIV-1 and HPIV-3 are classified in the genus Respirovirus, while HPIV-2 and HPIV-4 belong to the genus Rubulavirus. Clinically, HPIV-1 and HPIV-2 are the leading cause of laryngotracheobronchitis (croup) in children, accounting for 60–75% of croup illnesses [18]. HPIV-3 is the most commonly detected serotype in all age groups and it often causes pneumonia and outbreaks in long-term care facilities [19]. The epidemiology of HPIV-4 infections is not well understood because the detection is relatively difficult and its symptoms often present as subclinical [18].
2.4 Human Adenovirus (HAdV)
HAdV was firstly isolated from surgically resected adenoid tissue of children and initially reported as a “cytopathogenic agent” in 1953 [20]. HAdV is a double-stranded DNA virus categorized into the Adenoviridae family. HAdV is further classified into seven species (HAdV-A through HAdV-G) containing 67 immunologically distinct serotypes [21]. HAdV infects the mucosal tissue and each serotype presents with tissue/organ tropism, therefore, HAdV causes a variety of illnesses including respiratory infections, keratoconjunctivitis, and gastroenteritis (Table 8.2). Among these serotypes, 1–5, 7, 21, and 41 are most commonly associated with human disease [22]. Serotypes 4, 7, 14, and 55 were reported to cause severe pneumonia in immunocompetent adults, and of note, the former two (HAdV-4, 7) are known as a common cause of respiratory illness among military recruits in the United States [22,23,24]. Although temporarily suspended, an oral live nonattenuated vaccine against both HAdV-4 and HAdV-7 is administered to military recruits in the United States [25]. It is also clinically important to consider that gastrointestinal symptoms are sometimes intercurrent in patients (especially in children) having a HAdV respiratory illness [22].
2.5 Human Coronavirus (HCoV)
HCoV is a single-stranded, positive-sense RNA virus and belongs to the family Coronaviridae. The term of “corona” derives from the crown-like appearance of virions, meaning crown in Latin, by electron microscopy. CoV is further classified into four genera: alpha-, beta-, gamma-, and delta-coronavirus. HCoV was first isolated from the nasal discharge of common cold patients in 1965 [26]. To date, there are seven HCoVs including two alpha-CoVs (HCoV-NL63, HCoV-229E) and five beta-CoVs (HCoV-OC43, HCoV-HKU1, severe acute respiratory syndrome-CoV (SARS-CoV)-1, SARS-CoV-2, and Middle East respiratory syndrome-CoV (MERS-CoV)) [27, 28]. HCoVs were initially considered as a mere pathogen causing common cold-like symptoms; however, emergence of SARS-CoV in 2002 [29], MERS-CoV in 2012 [30], and SARS-CoV-2 in 2019 [28] has reminded us of its significant impact on human public health.
2.6 Human Metapneumovirus (HMPV)
HMPV was first identified from nasopharyngeal samples in children with respiratory symptoms in 2001 [31]. HMPV is a single-stranded, negative-sense RNA virus, and currently reclassified into the family Pneumoviridae, which also includes RSV. A seroprevalence study revealed that most children experience HMPV infection at least once by 5 years of age and re-infection occurs throughout the life [32]. HMPV preferentially infects respiratory ciliated epithelial cells and causes a variety of respiratory symptoms. A study investigating the clinical features of HMPV pneumonia in long-term care facilities in Japan showed that HMPV pneumonia patients experienced wheezing more frequently compared to non-pneumonia HMPV infected patients (43% vs. 9%; p < 0.0001). Additionally, the authors suggested that proximal bronchial wall thickenings radiating outward from the hilum on chest X-ray is a common finding in HMPV induced pneumonia [33].
2.7 Human Bocavirus (HBoV)
HBoV was first isolated from the respiratory samples of infants as an unknown human parvovirus in 2005 [34]. HBoV is a single-stranded DNA virus belonging to the family Parvoviridae and further classified into four subtypes (HBoV-1, -2, -3, and -4). HBoV-1 causes respiratory illness especially in young children, while HBoV-2, -3, and -4 are associated with gastroenteritis [35].
2.8 Human Enterovirus (HEV) and Parechovirus (HPeV)
HEV and HPeV are positive-sense, single-stranded RNA virus and belong to the family Picornaviridae. HEV is classified into four species (HEV-A, -B, -C, and -D) and traditional viral names such as coxsackievirus, echovirus, and poliovirus are still retained for individual serotypes [36]. HEV causes a variety of diseases involving not only respiratory organs, but also the skin, eyes, heart, and central nervous system (Table 8.3). Acute flaccid paralysis/myelitis caused by wild-type poliovirus has been eradicated from most countries including Japan. Based on genetic analysis, echovirus 22 and 23 were reclassified into a new genus Parechovirus and renamed HPeV-1 and -2, respectively, in 1999. Currently, 16 different parechovirus genotypes are identified and HPeV 1-6 cause infectious diseases in human. Among these genotypes, HPeV-1, -3, and -6 are associated with respiratory infections, and HPeV-3 is known as a cause of sepsis-like illness in neonates [37].
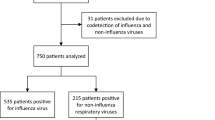
3 Viral Etiology in Patients with Influenza-Like Illness
World Health Organization defines influenza-like illness (ILI) as “an acute respiratory illness with a measured temperature of ≥38 °C and cough; with onset within the past 10 days” [38]. It is well known that CARVs other than influenza can cause ILI. A prospective, multinational, active community surveillance study involving 17 centers in eight countries was conducted from February 2010 to August 2011 [39]. In this study, upper respiratory specimens were collected from 2421 children aged 6 months to 10 years (3717 ILI episodes) and tested by multiplex PCR. As a result, CARVs were detected in 2958 of 3717 episodes (79.6%) and the most commonly detected virus was HRV/HEV (41.5%), followed by influenza (15.8%), HAdV (9.8%), HPIV and RSV (both 9.7%), HCoV (5.6%), HMPV (5.5%), and HBoV (2.0%). The assay used in the study was unable to distinguish between HRV and HEV. Another study enrolling 1023 children with ILI revealed HRV as the most detected virus (49.4%), followed by HPIV-3 (19.5%), HMPV (16.5%), and influenza (5.4%) [40]. Table 8.4 summarizes representative large-scale studies investigating viral etiology in adult patients with ILI [41,42,43,44,45,46,47]. Most studies revealed that HRV, as well as influenza virus, were the leading cause of ILI. Needless to say, the viral etiology of ILI varies by many factors such as the study sample (e.g., age, influenza vaccination history), season, setting (e.g., community or outpatient or inpatient), and regions. However, the important thing is that CARVs other than influenza virus are commonly detected even during influenza epidemics [39, 48].
4 Are Specific Symptoms Useful in Distinguishing Between Influenza and Other CARVs?
Before discussing symptoms, the most important factor in clinically diagnosing influenza is whether the patient presenting with ILI visits a clinic during an influenza epidemic. Some studies investigated the utility of fever and cough symptoms to predict the likelihood of influenza [49,50,51]. Michiels et al. reported that the likelihood of influenza was quite low in patients without fever and cough during influenza non-epidemic periods [49]. On the other hand, the presence of “previous flu-like contacts,” cough, “expectoration on the first day of illness,” and fever higher than 37.8 °C during an influenza epidemic increased the likelihood of influenza threefold. Ebell et al. reviewed five studies examining the diagnostic accuracy based on the “fever and cough rule” during the influenza season [51]. The sensitivity and specificity of the rule for influenza diagnosis was 30–78% and 55–94%, respectively, and the authors concluded that the rule had a modest accuracy. We should keep in mind that ILI symptoms sometimes lack in some population types such as the elderly, for example. Therefore, clinical diagnosis of influenza should be carefully made by taking a comprehensive decision based on several factors such as the epidemic situation around the region and patient background.
Predicting causative CARV by clinical symptoms is further difficult, except for diseases presenting unique features such as bronchiolitis in children (mostly caused by RSV [52]), laryngotracheobronchitis, known as croup (mostly caused by HPIV [53]), hand-foot-and-mouth disease and herpangina (both caused by HEV). Bellei et al. compared the clinical manifestations (fever, cough, coryza, sore throat, headache myalgia, and chills) of seven CARVs (influenza, HRV, HMPV, HAdV, RSV, HCoV, and HEV) in adult patients with acute respiratory symptoms [46]. Although the frequency of fever was relatively higher in patients with influenza (91%) compared to other viruses (51–60%), there was no virus-specific symptom overall. To identify the causative CARVs in patients with respiratory infections, rapid antigen tests using immunochromatography or molecular assays including nucleic acid amplification tests are useful [54].
5 Conclusions
In this chapter, basic information regarding viral and clinical aspects of CARVs other than influenza is briefly summarized. From an epidemiological point, CARVs other than influenza virus are commonly detected even during influenza epidemics, thus a differential diagnosis between influenza and other CARVs infections is important. Additionally, identification of CARVs is sometimes critical especially when managing severe pneumonia patients or in an outbreak setting. Since the usefulness of clinical manifestations for differential diagnosis between influenza and other CARVs infection is limited in most cases, rapid antigen tests or molecular assays are needed to confirm a causative virus.
References
Price WH. The isolation of a new virus associated with respiratory clinical disease in humans. Proc Natl Acad Sci U S A. 1956;42(12):892–6.
Bochkov YA, Grindle K, Vang F, Evans MD, Gern JE. Improved molecular typing assay for rhinovirus species A, B, and C. J Clin Microbiol. 2014;52:2461–71. https://doi.org/10.1128/JCM.00075-14.
Ljubin-Sternak S, Mestrovic T, Ivkovic-Jurekovic I, Kolaric B, Slovic A, Forcic D, et al. The emerging role of rhinoviruses in lower respiratory tract infections in children - clinical and molecular epidemiological study from Croatia, 2017-2019. Front Microbiol. 2019;10:2737. https://doi.org/10.3389/fmicb.2019.02737.
Gutman JA, Peck AJ, Kuypers J, Boeckh M. Rhinovirus as a cause of fatal lower respiratory tract infection in adult stem cell transplantation patients: a report of two cases. Bone Marrow Transplant. 2007;40(8):809–11. https://doi.org/10.1038/sj.bmt.1705827.
Seo S, Waghmare A, Scott EM, Xie H, Kuypers JM, Hackman RC, et al. Human rhinovirus detection in the lower respiratory tract of hematopoietic cell transplant recipients: association with mortality. Haematologica. 2017;102(6):1120–30. https://doi.org/10.3324/haematol.2016.153767.
Dougherty RH, Fahy JV. Acute exacerbations of asthma: epidemiology, biology and the exacerbation-prone phenotype. Clin Exp Allergy. 2009;39(2):193–202. https://doi.org/10.1111/j.1365-2222.2008.03157.x.
Hewitt R, Farne H, Ritchie A, Luke E, Johnston SL, Mallia P. The role of viral infections in exacerbations of chronic obstructive pulmonary disease and asthma. Ther Adv Respir Dis. 2016;10(2):158–74. https://doi.org/10.1177/1753465815618113.
Jackson DJ, Makrinioti H, Rana BM, Shamji BW, Trujillo-Torralbo MB, Footitt J, et al. IL-33-dependent type 2 inflammation during rhinovirus-induced asthma exacerbations in vivo. Am J Respir Crit Care Med. 2014;190(12):1373–82. https://doi.org/10.1164/rccm.201406-1039OC.
Message SD, Laza-Stanca V, Mallia P, Parker HL, Zhu J, Kebadze T, et al. Rhinovirus-induced lower respiratory illness is increased in asthma and related to virus load and Th1/2 cytokine and IL-10 production. Proc Natl Acad Sci U S A. 2008;105(36):13562–7. https://doi.org/10.1073/pnas.0804181105.
Mallia P, Message SD, Gielen V, Contoli M, Gray K, Kebadze T, et al. Experimental rhinovirus infection as a human model of chronic obstructive pulmonary disease exacerbation. Am J Respir Crit Care Med. 2011;183(6):734–42. https://doi.org/10.1164/rccm.201006-0833OC.
Chanock R, Roizman B, Myers R. Recovery from infants with respiratory illness of a virus related to chimpanzee coryza agent (CCA). I. Isolation, properties and characterization. Am J Hyg. 1957;66(3):281–90. https://doi.org/10.1093/oxfordjournals.aje.a119901.
Martinello RA, Chen MD, Weibel C, Kahn JS. Correlation between respiratory syncytial virus genotype and severity of illness. J Infect Dis. 2002;186(6):839–42. https://doi.org/10.1086/342414.
Espinosa Y, San Martin C, Torres AA, Farfan MJ, Torres JP, Avadhanula V, et al. Genomic loads and genotypes of respiratory syncytial virus: viral factors during lower respiratory tract infection in Chilean hospitalized infants. Int J Mol Sci. 2017;18(3):654. https://doi.org/10.3390/ijms18030654.
Glezen WP, Taber LH, Frank A, Kasel J. Risk of primary infection and reinfection with respiratory syncytial virus. Am J Dis Child. 1986;40:543–6.
Hall CB, Weinberg GA, Iwane MK, Blumkin AK, Edwards KM, Staat MA, et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med. 2009;360(6):588–98. https://doi.org/10.1056/NEJMoa0804877.
Nam HH, Ison MG. Respiratory syncytial virus infection in adults. BMJ. 2019;366:–l5021.
Chanock RM. Association of a new type of cytopathogenic myxovirus with infantile croup. J Exp Med. 1956;104:555–76.
Branche AR, Falsey AR. Parainfluenza virus infection. Semin Respir Crit Care. 2016;37(4):538–54. https://doi.org/10.1055/s-0036-1584798.
Russell E, Ison MG. Parainfluenza virus in the hospitalized adult. Clin Infect Dis. 2017;65(9):1570–6. https://doi.org/10.1093/cid/cix528.
Rowe WP, Huebner RJ, Gilmore LK. Isolation of a cytopathogenic agent from human adenoids undergoing spontaneous degeneration in tissue culture. Proc Soc Exp Biol Med. 1953;84(3):570–3. https://doi.org/10.3181/00379727-84-20714.
Ison MG, Hayden RT. Adenovirus. Microbiol Spectr. 2016; https://doi.org/10.1128/microbiolspec.DMIH2-0020-2015.
Lynch JP III, Kajon AE. Adenovirus: epidemiology, global spread of novel serotypes, and advances in treatment and prevention. Semin Respir Crit Care Med. 2016;37(4):586–602. https://doi.org/10.1055/s-0036-1584923.
Low SY, Tan TT, Lee CH, Loo CM, Chew HC. Severe adenovirus pneumonia requiring extracorporeal membrane oxygenation support--serotype 7 revisited. Respir Med. 2013;107(11):1810–3. https://doi.org/10.1016/j.rmed.2013.09.008.
Sun B, He H, Wang Z, Qu J, Li X, Ban C, et al. Emergent severe acute respiratory distress syndrome caused by adenovirus type 55 in immunocompetent adults in 2013: a prospective observational study. Crit Care. 2014;18(4):456. https://doi.org/10.1186/s13054-014-0456-6.
Kuschner RA, Russell KL, Abuja M, Bauer KM, Faix DJ, Hait H, et al. A phase 3, randomized, double-blind, placebo-controlled study of the safety and efficacy of the live, oral adenovirus type 4 and type 7 vaccine, in U.S. military recruits. Vaccine. 2013;31(28):2963–71. https://doi.org/10.1016/j.vaccine.2013.04.035.
Tyrrell DA, Bynoe ML. Cultivation of a novel type of common-cold virus in organ cultures. Br Med J. 1965;1(5448):1467–70. https://doi.org/10.1136/bmj.1.5448.1467.
Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17(3):181–92. https://doi.org/10.1038/s41579-018-0118-9.
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33. https://doi.org/10.1056/NEJMoa2001017.
Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, Emery S, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med. 2003;348(20):1953–66. https://doi.org/10.1056/NEJMoa030781.
Zaki AM, van Boheemen S, Besterbroer TN, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367(19):1814–20. https://doi.org/10.1056/NEJMoa1211721.
van den Hoogen BG, de Jong JC, Groen J, Kuiken T, de Groot R, Fouchier RAM, et al. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat Med. 2001;7(6):719–24. https://doi.org/10.1038/89098.
Williams JV, Harris PA, Tollefson SJ, Halburnt-Rush LL, Pingsterhaus JM, Edwards KM, et al. Human metapneumovirus and lower respiratory tract disease in otherwise healthy infants and children. N Engl J Med. 2004;350(5):443–50. https://doi.org/10.1056/NEJMoa025472.
Karimata Y, Kinjo T, Parrott G, Uehara A, Nabeya D, Haranaga S, et al. Clinical features of human metapneumovirus pneumonia in non-immunocompromised patients: an investigation of three long-term care facility outbreaks. J Infect Dis. 2018;218(6):868–75. https://doi.org/10.1093/infdis/jiy261.
Allander T, Tammi MT, Eriksson M, Bjerkner A, Tiveljung-Lindell A, Andersson B. Cloning of a human parvovirus by molecular screening of respiratory tract samples. Proc Natl Acad Sci U S A. 2005;102(36):12891–6. https://doi.org/10.1073/pnas.0504666102.
Broccolo F, Falcone V, Esposito S, Toniolo A. Human bocaviruses: possible etiologic role in respiratory infection. J Clin Virol. 2015;72:75–81. https://doi.org/10.1016/j.jcv.2015.09.008.
Dunn JJ. Enteroviruses and parechoviruses. Microbiol Spectr. 2016; https://doi.org/10.1128/microbiolspec.DMIH2-0006-2015.
Olijve L, Jennings L, Walls T. Human parechovirus: an increasingly recognized cause of sepsis-like illness in young infants. Clin Microbiol Rev. 2017;31(1):e00047–17. https://doi.org/10.1128/CMR.00047-17.
Fitzner J, Qasmieh S, Mounts AW, Alexander B, Besselaar T, Briand S, et al. Revision of clinical case definitions: influenza-like illness and severe acute respiratory infection. Bull World Health Organ. 2018;96(2):122–8. https://doi.org/10.2471/BLT.17.194514.
Taylor S, Lopez P, Weckx L, Borja-Tabora C, Ulloa-Gutierrez R, Lazcano-Ponce E, et al. Respiratory viruses and influenza-like illness: epidemiology and outcomes in children aged 6 months to 10 years in a multi-country population sample. J Infect. 2017;74(1):29–41. https://doi.org/10.1016/j.jinf.2016.09.003.
Chang ML, Jordan-Villegas A, Evans A, Bhore R, Brock E, Mejias A, et al. Respiratory viruses identified in an urban children’s hospital emergency department during the 2009 influenza a(H1N1) pandemic. Pediatr Emerg Care. 2012;28(10):990–7. https://doi.org/10.1097/PEC.0b013e31826ca980.
Al-Romaihi HE, Smatti MK, Ganesan N, Nadeem S, Farag E, Coyle PV, et al. Epidemiology of respiratory infections among adults in Qatar (2012-2017). PLoS One. 2019;14(6):e0218097. https://doi.org/10.1371/journal.pone.0218097.
Tan XQ, Zhao X, Lee VJ, Loh JP, Tan BH, Koh WHV, et al. Respiratory viral pathogens among Singapore military servicemen 2009-2012: epidemiology and clinical characteristics. BMC Infect Dis. 2014;14:204. https://doi.org/10.1186/1471-2334-14-204.
Noh JY, Song JY, Cheong HJ, Choi WS, Lee J, Lee JS, et al. Laboratory surveillance of influenza-like illness in seven teaching hospitals, South Korea: 2011-2012 season. PLoS One. 2013;8(5):e64295. https://doi.org/10.1371/journal.pone.0064295.
Todd S, Huong NTC, Thanh NTL, Vy NHT, Hung NT, Thao TTN, et al. Primary care influenza-like illness surveillance in Ho Chi Minh City, Vietnam 2013-2015. Influenza Other Respir Viruses. 2018;12(5):623–31. https://doi.org/10.1111/irv.12574.
Falsey AR, McElhaney JE, Beran J, van Essen GA, Duval X, Esen M, et al. Respiratory syncytial virus and other respiratory viral infections in older adults with moderate to severe influenza-like illness. J Infect Dis. 2014;209(12):1873–81. https://doi.org/10.1093/infdis/jit839.
Bellei N, Carraro E, Perosa A, Watanabe A, Arruda E, Granato C. Acute respiratory infection and influenza-like illness viral etiologies in Brazilian adults. J Med Virol. 2008;80(10):1824–7. https://doi.org/10.1002/jmv.21295.
Louie JK, Hacker JK, Gonzales R, Mark J, Maselli JH, Yagi S, Drew WL. Characterization of viral agents causing acute respiratory infection in a San Francisco university medical center clinic during the influenza season. Clin Infect Dis. 2005;41(6):822–8. https://doi.org/10.1086/432800.
Jain A, Prakash S, Jain B. Contribution of non- influenza respiratory viruses in causation of influenza like illness (ILI) during influenza epidemic: a laboratory based study. Clin Epidemiol Glob Health. 2017; https://doi.org/10.1016/j.cegh.2017.06.001.
Michiels B, Thomas I, Van Royen P, Coenen S. Clinical prediction rules combining signs, symptoms and epidemiological context to distinguish influenza from influenza-like illnesses in primary care: a cross sectional study. BMC Fam Pract. 2011;12:4. https://doi.org/10.1186/1471-2296-12-4.
Eskin B, Levy R. Evidence-based emergency medicine/rational clinical examination abstract. Does this patient have influenza? Ann Emerg Med. 2007;49(1):103–5. https://doi.org/10.1016/j.annemergmed.2006.08.016.
Ebell MH, Afonso A. A systematic review of clinical decision rules for the diagnosis of influenza. Ann Fam Med. 2011;9(1):69–77. https://doi.org/10.1370/afm.1192.
Meissner HC. Viral bronchiolitis in children. N Engl J Med. 2016;374(1):62–72. https://doi.org/10.1056/NEJMra1413456.
Smith DK, McDermott AJ, Sullivan JF. Croup: diagnosis and management. Am Fam Physician. 2018;97:575–80.
Zhang N, Wang L, Deng X, Liang R, Su M, He C, et al. Recent advances in the detection of respiratory virus infection in humans. J Med Virol. 2020;92(4):408–17. https://doi.org/10.1002/jmv.25674.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kinjo, T., Fujita, J. (2021). Differential Diagnosis Between Influenza and Other Respiratory Viral Infections: What Are the Differential Diagnoses?. In: Fujita, J. (eds) Influenza. Respiratory Disease Series: Diagnostic Tools and Disease Managements. Springer, Singapore. https://doi.org/10.1007/978-981-15-9109-9_8
Download citation
DOI: https://doi.org/10.1007/978-981-15-9109-9_8
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-9108-2
Online ISBN: 978-981-15-9109-9
eBook Packages: MedicineMedicine (R0)