Abstract
The biological mechanisms of cancer development involve both environmental and genetic factors. Among the environmental factors, tobacco and alcohol have been established as one of the most potent causative factors in promoting carcinogenesis while genetic variations in phase I and phase II xenobiotic metabolizing enzymes (XMEs) play an important role in determining the outcome of exposure to environmental carcinogens. The genes that contribute to cancer development fall into three broad categories, namely tumor suppressor genes, oncogenes, and DNA repair genes though several other genes are also involved. Cytochrome P450s (CYPs) are the most important super family of phase I XMEs while phase II Glutathione S-transferases (GSTs) conjugate a wide range of electrophilic substrates with the abundant cellular nucleophile-glutathione (GSH) promoting their metabolism, detoxification, and excretion. There has been a lot of interest in unravelling gene–environment interactions, i.e. whether the risk of cancer associated with a particular environmental exposure such as tobacco and alcohol differs with respect to functionally different polymorphisms of these genes. A large number of studies have been conducted involving several genes and many cancers and the results, though sometimes inconsistent, help in advancing the etiological understanding of cancer. Study of gene–environment interaction is important for improving accuracy and precision in the assessment of both genetic and environmental influences in promoting cancer. Gene–environment interaction also has important implications for public health as it helps in predicting cancer rates and provides a basis for appropriate recommendations for cancer prevention.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
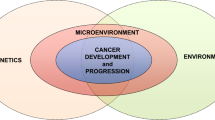
Cancer is caused by changes in genes that alter the way our cells perform their normal functions. Some of these genetic changes occur naturally when DNA is replicated during the process of cell division while others are the result of environmental exposures that damage DNA. Studies have shown that among the factors responsible for cancer, environmental factors play an important role particularly tobacco and alcohol (Brennan and Boffetta 2004). The relationship between cancer development and use of tobacco and alcohol was analyzed by two systematic reviews published by The World Cancer Research Fund in 2007 (World Cancer Research Fund 2007) and the International Agency for Research on Cancer in 2012 (International Agency for Research on Cancer 2012). The reviews concluded that long-term alcohol and tobacco consumption increases risk of cancer of the lips, oral cavity, pharynx, larynx, lung, stomach, colorectum, breast, pancreas, and liver. Similarly, studies have also been conducted that show that there is a relationship between cancer onset and alcohol consumption and tobacco smoking. The higher the amount of alcohol and tobacco consumed, the greater is the risk of cancer in the long term. However, inter-individual variations in susceptibility to cancer have also been observed. Individuals having the same amount and duration of usage of tobacco and alcohol may have differences in susceptibility to cancer which might be explained by gene–environment interactions. The genetic make-up of an individual decides the outcome of an exposure to a carcinogen (Fig. 10.1). Study of gene–environment interaction helps to improve accuracy and precision in the assessment of both genetic and environmental influences. Following sections discuss the risk factors for cancer, namely alcohol and tobacco, genetic variations in key enzymes and gene–environment interactions.
Environmental carcinogens get activated by CYPs and either get detoxified by GSTs followed by excretion from body or cause DNA damage resulting in cancer. However, more expression/activity of CYPs and/or less expression/activity of GSTs will promote carcinogenesis for the same environmental exposure as a result of gene–environment interaction
2 Environmental Risk Factors and Cancer Risk
2.1 Tobacco and Cancer Risk
The use of tobacco is a leading cause of cancer and also death from cancer. People who consume tobacco products or who are regularly around environmental tobacco smoke (also called second hand smoke) have an increased risk of cancer because tobacco products and second hand smoke have components that damage DNA. Processed tobacco leaves possess more than 3000 chemicals (Roberts 1988) which include leaf constituents as well as constituents derived from multiple sources. Unburned tobacco products contain carcinogenic nitrosamines, polycyclic aromatic hydrocarbons (PAHs), radioactive elements, and cadmium. Several forms of tobacco commonly used are cigarettes, smokeless tobacco, cigars, and pipes (Iribarren et al. 1999). The quality of smoked cigarette and quitting smoking also have a role in oral cancer risk as shown in studies that filtered cigarettes and smoking cessation substantially lower risk of oral cancer (Kabat et al. 1994). The smoke emanating from cigarettes has thousands of chemicals with around 60 of them carcinogens (Table 10.1 lists some of the major components in the cigarette smoke). Cigarette smokers have a lifetime increased risk for head and neck cancers (HNSCC) that are 5–25 fold increased over the general population (Andre et al. 1995). Those who quit smoking are at the same level of risk as of a non-smoker 20 years after smoking cessation. Risks of lung cancer and cancers of the upper respiratory tract increase with increased consumption and duration of smoking. Incidences of laryngeal cancer are strongly connected with exposure to tobacco smoke containing dozens of carcinogens. Genotoxic agents such as PAHs present in tobacco smoke are responsible for lesions of structure of DNA and formation of DNA adducts by metabolically activated intermediates.
Smokeless tobacco products like chewing tobacco and sucked tobacco are the other tobacco related risk factors involved in cancer development (Accort et al. 2005). Simultaneous consumption of betel nuts with smoking and drinking makes one susceptible for esophageal cancer several hundred times. A form of tobacco called “khaini” (mixture of tobacco, lime, and menthol or aromatic species) has very high level of nitrosamines (Stepanov et al. 2005) which can be attributed to the method of tobacco processing which converts nitrate to nitrite (Hoffmann et al. 1995). The consumption of khaini directly affects the oral mucosa via interactions with high amounts of nitrite as well as N-nitroso compounds formed endogenously. This has been seen in saliva of individuals consuming khaini (Stitch et al. 1992). Other forms of popular smokeless tobacco products are Zarda and Gutka. Zarda is produced by boiling tobacco leaves in water with lime and spices and has significantly high levels of nitrosamines, while Gutka contains less nitrosamine.
Around 75% of cancers of oral cavity and pharynx are caused by the use of tobacco. The association between tobacco and cancer becomes more pronounced with increased amount of tobacco consumption, either in the form of smoking or chewing, and also duration of consumption. In India, the per capita consumption of cigarettes has seen an increase by 2% over the last decade. Estimates for the annual number of persons developing disease attributable to their tobacco habit in mid-eighties included 1,08,000 annual incident cases of cancer (Brennan and Boffetta 2004). The first report of an association between tobacco smoking and lung cancer risk came in 1950 (Wynder and Graham 1950; Doll and Hill 1950) and over the subsequent years, several studies not only confirmed this finding but also found that tobacco smoking also increases the risk of several other neoplasms. In 2004, International Agency for Research on Cancer (IARC) classified tobacco smoking as carcinogenic to humans and gave evidence for the relationship between cigarette consumption and cancers of several regions of body such as lung, head and neck, stomach, pancreas, liver, kidney, ureter, urinary bladder, cervix, and leukemia. In Indian context, a National survey revealed that smoking tobacco is more prevalent in men while women chewed tobacco more and the regular consumption of tobacco is more prevalent in later stages of life (50 years and more) in both men and women (Neufeld et al. 2005). The recent National Cancer Registry Programme (NCRP) data on Tobacco related cancers (TRC) analyzed in a study conducted by Asthana et al. (2016) revealed that approximately one-fourth of all cancers among men and one-fifth among women were tobacco related. The maximum incidence among men was reported for esophagus, lungs, and hypopharynx cancers from the Northeast of India and mouth cancer for Western India. Among women, maximum rates were reported for esophagus and lung cancers in the Northeast region. The overall risk of developing TRC was highest in the Northeast region compared to all other regions. A study which compared the overall incidence of all cancer cases from Northeast region and other regions from India observed a higher cancer incidence in the Northeast. The study also compared Northeast cancer incidence data with global data and found its similarities with the Southeast Asian region. This might be due to the similarities between the genetic pool of people in Northeast region of India and Southeast Asian region (Sharma et al. 2014).
2.2 Alcohol and Cancer Risk
Alcohol has been known to be responsible for several health and social issues and is responsible for about three million deaths each year with about 5.1% of the global burden of disease and injury (World Health Organization 2018). Besides being a causal factor for several health issues such as liver cirrhosis, epilepsy, poisoning, etc., alcohol consumption was estimated to have caused around 500,000 cancer deaths worldwide in 2004, 4.4% of cancer deaths in China in 2005 and 3.5% in the USA in 2009. The first study demonstrating the carcinogenic effect of alcohol was published in 1903 (Newsholme 1903) followed by several such studies which paved the way for the International Agency for Research on Cancer (IARC) listing alcohol among the carcinogens for oral cavity and pharynx, esophagus, liver, and larynx. The list was updated to include two more sites colorectum and female breast in 2010 following the studies conducted by Hamajima et al. (2002) and Ferrari et al. (2007).
There are several mechanisms by which alcohol consumption may exert its carcinogenic effect. Acetaldehyde production, polymorphisms in ethanol metabolizing genes, hormonal imbalances leading to breast cancer, dysregulation of immune system, dysregulation of folate metabolism, and damages to the epithelium resulting in increased absorption of carcinogens are some of the mechanisms that promote carcinogenesis (Boffetta and Hashibe 2006; Yu et al. 2010; Singletary and Gapstur 2001; Watson et al. 1994; Hamid et al. 2009; Doll et al. 1999). It has been found that methylation of p15-gene is accelerated by tobacco and alcohol promoting the development of head and neck cancer (Chang et al. 2004) as alcohol and tobacco are likely to be synergistic in causing head and neck cancer (Murata et al. 1996). In studies where alcohol is co-administered with other cancer-causing agents, it has been found to exert a synergistic effect in promoting carcinogenesis (Hsu et al. 1991). This is true for the association between alcohol, smoking and head and neck cancer risk though a study by Schlecht et al. (1999) found the joint effects of alcohol and moderate smoking to be more than multiplicative in pharyngeal cancers. The study pointed out that alcohol has both synergistic and independent effects in promoting carcinogenesis of head and neck region. The synergistic action could be by acting as a solvent for other carcinogens or promoting inflammation and generation of reactive oxygen species. Studies have reported an association between alcohol consumption and pancreatic and prostate cancer. With regard to pancreatic cancer, heavy consumption of alcohol was associated with an increased risk by 19% compared with non-drinkers or occasional drinkers while two studies reported a significant positive association between alcohol consumption and prostate cancer. Alcohol consumption is also associated with colorectal cancer, though gender specific differences do exist as a meta-analysis did not find any significant association between alcohol and colorectal cancer mortality in women (Cai et al. 2014).
The association of alcohol consumption has also been studied with an increased risk of melanoma. The possible mechanisms of alcohol-induced melanoma could be enhanced cellular damage in the presence of UV radiation and subsequently formation of skin cancers (Saladi et al. 2010) and increased immunodeficiency and immunosuppression (Watson et al. 1994), the conditions that facilitate melanoma formation (Mukherji 2013). A meta-analysis conducted by Bagnardi et al. (2015) found that heavy drinkers had a significant 15% increase of lung cancer risk as compared with non-drinkers or occasional drinkers. However, in another meta-analysis published by the same group, alcohol consumption was not associated with lung cancer risk in never smokers. Similarly, an association between alcohol consumption and stomach cancer was also observed. These positive associations must be interpreted with caution as the confounding effect of smoking cannot be ruled out given the fact that alcohol users are most commonly smokers too. Another important consideration is the influence of diet as heavy alcohol consumption leads to compromised nutrition and, thus, confounding by poor diet (Klatsky 2001) could not be ruled out. Inconsistent and inconclusive reports for the association between alcohol consumption and cancers of endometrium, ovary, cervix, thyroid, and brain have been reported though there are also studies which reported no association with cancer of bladder, adenocarcinoma of the esophagus, and stomach while significant association was observed with cancer of gall bladder (Bagnardi et al. 2015).
As opposed to the studies which show a positive association between alcohol consumption and cancer risk, there are also studies which reported an inverse relationship. Studies on Hodgkin’s and non-Hodgkin’s lymphomas reported an alcohol-induced decrease in the risk (Tramacere et al. 2012a, b) while protective effect of moderate alcohol consumption on the risk of renal cell cancer has also been reported. However, a European study did not report an inverse relationship between alcohol intake and lymphoid neoplasms (Heinen et al. 2013). The possible reasons for alcohol related decrease in the risk of lymphomas are not very evident though it may be attributed partly to the inappropriate classification of drinkers as non-drinkers as in the initial stages of the lymphomas, the cases either abstain from drinking or reduce the alcohol intake significantly. Similarly, alcohol could protect renal cells from cancer either due to its role in insulin sensitivity or diuresis though no concrete evidence exists between fluid intake and cancer risk (Altieri et al. 2003). Some studies have established an association between alcohol and risk of head and neck cancer. This was particularly evident in populations with a higher alcohol intake as revealed by cohort and case-control studies (Viswanathan and Wilson 2004). All forms of alcohol have been linked to the cancers of oral cavity and pharynx with the association more strong for oral cavity compared to the larynx and pharynx.
Alcohol poses less risk for laryngeal cancer compared to cigarette smoking; however, cancer of the oral cavity has an increased incidence among those who smoke and use alcohol (Choi and Kahyo 1991). The incidence of oral cancer may remain high several years after stopping alcohol use (Franceschi et al. 2000).
3 Genetic Variations in Enzymes Involved in Metabolism of Xenobiotics
3.1 Genetic Variations of Phase I Xenobiotic Metabolizing Enzymes (XMEs)
The metabolism of Polycyclic Aromatic Hydrocarbons (PAHs), N-nitrosamines, and aromatic amines is by a two-phase process. The first phase called as phase I involves the activation of the carcinogen by enzymes encoded by the CYP gene superfamily. Cytochrome P450s (CYPs) are the most important super family of phase I XMEs which are ubiquitously distributed and found from bacteria to humans (Nelson et al. 1996). The root symbol “CYP” for human (“cyp” for mouse) denotes “cytochrome P450.” The root symbol is followed by an Arabic numeral, designating the CYP family (Nebert and Russell 2002). The CYP1, CYP2, and CYP3 enzymes are primarily associated with the metabolism of exogenous compounds, whereas the other CYPs mainly have endogenous roles. It is estimated that CYPs in families 1–3 are responsible for about 75% of all phase I metabolism of clinically used drugs (Evans and Relling 1999). CYPs exhibiting important endogenous functions are well conserved, while almost all CYPs involved in xenobiotic metabolism are functionally polymorphic (Ingelman-Sundberg 2004). CYP1 family, which consists of CYP1A and CYP1B1, is involved in the metabolic activation of procarcinogens and promutagens to reactive carcinogenic and mutagenic species while CYP2 family which includes CYP2A, 2B, 2C, 2D, and 2E accounts for metabolism of majority of drugs. CYP2E1 is also primarily involved in the metabolism of alcohol and other low-molecular weight compounds and contributes to activation of many procarcinogens and several drugs to highly reactive metabolites (Nakajima and Aoyama 2000). Likewise, CYP2A6 has been specifically demonstrated to activate 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) and N′-nitrosonornicotine (NNN) tobacco smoke procarcinogens via α-hydroxylation (Patten et al. 1997). CYPs belonging to 2C and 2D family are the major drug metabolizing CYPs and lead to poor or extensive metabolizer phenotype.
CYP1 family members include three genes, CYP1A1, CYP1A2, and CYP1B1. CYP1A1 gene is located on the long arm of chromosome 15 (q22–24) and contains seven exons of which the first is noncoding (Hildebrand et al. 1985). The CYP1A1 m1 polymorphism (CYP1A1*2A) consists of a T-C substitution in the 3′ noncoding region of the gene, m2 polymorphism (CYP1A1*2C) is due to an A to G substitution at nucleotide 4889 in exon 7, m3 polymorphism (T5639C) is found only in African Americans, and m4 polymorphism (CYP1A1*4) leads to a C to A substitution (Cascorbi et al. 1996). While, both CYP1A1*2A and CYP1A1*2C have been reported in Asians, the frequency of CYP1A1*2C is rare in the Caucasians (Hung et al. 2003). CYP1A2 is also located on chromosome 15q22-q24 but shows different substrate specificity from CYP1A1 with a preference for heterocyclic amines, caffeine and a limited number of prescribed drugs including antipsychotics and theophylline (Schmidt 1996). Functionally important polymorphisms in the CYP1A2 are identified in upstream sequence and intron 1 and some of these may affect CYP1A2 protein expression. CYP1A2*1C results from a single nucleotide change from G to A at position −3858 in 5′ flanking region (Nakajima et al. 1999). The frequency of variant allele of CYP1A2*1C is estimated to be around 0.02–0.03 per cent in Caucasians and higher frequency is found in Japanese (0.10) and Chinese population (0.11). The second variant allele is a C to A transversion (CYP1A2*1F) in intron 1 at position 734 downstream of the first CYP1B1, located on chromosome 2, 2p21. Of the most common SNPs of CYP1B1 gene, four have been reported to result in amino acid substitutions including Arg by Gly at codon 48 (CYP1B1*2), Ala by Ser at codon 119 (CYP1B1*2), Leu by Val at codon 432 (CYP1B1*3), and Asn by Ser at codon 453 (CYP1B1*4). A higher catalytic activity for Val432 variants than the Leu432 variants of the enzyme have been reported suggesting that polymorphisms in the human CYP1B1 gene, especially those at codon 432, may contribute to differential susceptibility towards PAH and tobacco-induced cancers (Shimada et al. 1999).
CYP2 is the largest CYP family made up of 13 subfamilies which are involved in drug metabolism in mammals. The genes which code for proteins are CYP2A CYP2B, CYP2C, CYP2D, CYP2E, CYP2F, CYP2J, CYP2R, CYP2S, and CYP2W while CYP2A7 is the pseudogene which produces a hybrid gene with the CYP2A6 gene (Oscarson 2001). The CYP2A6 gene is 6 kb in size, has 9 exons, and is located within a 350-kilobase pair gene cluster made up of CYP2A7, CYP2A13, two CYP2A7 pseudogenes, and genes in CYP2B and CYP2F subfamilies (Hoffman et al. 1995). CYP2A6 exhibits several genetic polymorphisms such as wild type (CYP2A6*1A), gene conversion with CYP2A7 in the 3′-untranslated region (CYP2A6*1B), gene conversions with CYP2A7 in exons 3, 6, and 8 (CYP2A6*3), L160H (CYP2A6*2), G479V (CYP2A6*5), R128Q (CYP2A6*6), I471T (CYP2A6*7), R485L (CYP2A6*8), and S224P (CYP2A6*11) (Daigo et al. 2002). Other functionally important alleles include CYP2A6*9 which has a point mutation in the TATA box (T-48G), CYP2A6*10 (two simultaneous amino acid substitutions of CYP2A6*7 and CYP2A6*8), CYP2A6*4 (deletion of the whole CYP2A6 gene), and CYP2A6*1X2 (duplication of the CYP2A6 gene). Asian populations (Chinese, Japanese, and Korean) have higher prevalence of CYP2A6 variant alleles resulting in reduced enzyme activity as opposed to the Caucasian and African North American populations (Schoedel et al. 2004). Asian populations have prevalence of whole-gene deletion alleles (CYP2A6*4B and CYP2A6*4C), while European population have higher frequency of CYP2A6*2 and CYP2A6*3.
CYP2E1 metabolizes ethanol, low-molecular weight solvents, and tobacco specific nitrosamines. It is present on the tenth chromosome with 9 exons, 8 introns and has a characteristic TATA box (Guengerich et al. 1991). CYP2E1gene has several polymorphisms majority of which are present in the introns while others are present in 5′-regulatory, intron, and transcribed regions. The polymorphisms studied with restriction enzymes include PstI (G to C substitution at -1293 bp in the 5’noncoding region of the CYP2E1gene) and RsaI (C to T substitution at −1053 in 5’noncoding region of the CYP2E1) which are in linkage disequilibrium and together called as CYP2E1*5B, with c1 and c2 alleles (Watanabe et al. 1990). c2 allele results in about ten-fold higher gene transcription, protein level, and enzyme activity compared to the c1 allele. Another polymorphism studied using restriction enzyme XbaI is CYP2E1*1C having 43–60 bp six repeats and CYP2E1*1D with eight repeats. The intron region of CYP2E1also has several polymorphic sites such as DraI which constitutes a T to A substitution at 7668 bp in intron 6 that delete DraI restriction enzyme cleavage site and is represented as CYP2E1*6 allele. DraI polymorphism has two homozygous genotypes named as CC and DD and one heterozygous genotype, CD (Stephens et al. 1994). Conflicting reports are present regarding the effect of CYP2E1*6 on expression and activity with Persson et al. (1993) observing no effect while Uematsu et al. (1991) reported altered CYP2E1 catalytic activity with CYP2E1*6 allele but no effect on gene transcription. Another polymorphism present in intron 6 region of CYP2E1gene is the MspI polymorphism which leads to the A-G replacement at 6827 bp causing deletion of MspI restriction enzyme cleavage site. Little information is available about this polymorphism and it does not affect the expression or enzyme activity. There are several polymorphism of CYP2E1 which are present on coding region and lead to amino acid replacements (Danko and Chaschin 2005). The distribution of CYP2E1 genotypes exhibit ethnic variations with most of the polymorphisms of CYP2E1reported in Caucasians as well as in the Oriental population while only two polymorphisms (RsaI and DraI) are reported in Indian populations (Soya et al. 2005). Caucasians and Indians have similar prevalence of the minor allele c2 while the Orientals carry a higher frequency. For DraI polymorphism (CYP2E1*6), the minor allele frequency is higher in Indian or Oriental (20–30%) populations compared to the Caucasians (7–12%). Table 10.2 lists some of the functionally important polymorphisms in CYPs.
3.2 Genetic Variations of Phase II Xenobiotic Metabolizing Enzymes (XMEs)
One of the important classes of phase II xenobiotic metabolizing enzymes is Glutathione S-transferases (GSTs) which play an important role in the detoxification of tobacco carcinogens such as PAH diol epoxides, aromatic amines, hydrazines and products of oxidative stress. Of the five different families of GST, four are cytosolic and one is microsomal. Cytosolic GSTs conjugate glutathione (GSH) with electrophilic substrates increasing their solubility and excretion from the body. In humans, cytosolic GSTs exist in eight classes having one or more of the homodimeric or heterodimeric isoforms (Bolt and Their 2006). GSTs also regulate other physiologically important enzymes and proteins such as that of DNA repair (Huang et al. 2009) and are therefore important for both detoxification and maintaining cellular genomic integrity.
On the basis of their degree of sequence identity, GSTs have been assigned to eight families designated as Alpha (α), Mu (μ), Pi (π), Sigma (σ), Theta (θ), Zeta (ζ), Omega (ω), and Kappa (κ). The different isoforms such as GSTM1, GSTM3, GSTP1, and GSTT1have been shown to exhibit genetic polymorphisms. GSTM1, GSTM3, and GSTP1are involved in the detoxification of the PAH diol epoxides while GSTT1 detoxifies tobacco smoke components such as monohalomethanes and reactive epoxide metabolites of butadiene. GSTM1 is a member of GSTM family of enzymes and is involved in the detoxification of polycyclic aromatic hydrocarbons, ethylene oxide, epoxides, and styrene (Takahiko et al. 2008). Both the lack of this enzyme and overexpression can have consequences, as deficiency of this enzyme increases the cancer risk due to decreased elimination of carcinogenic compounds (Rebbeck 1997), while overexpression may result in chemotherapeutic resistance. Some factors, such as genetic variations, may alter gene expression or enzyme activity of GSTM1 and have an important bearing on cellular protection from environmental and oxidative stress and response to drugs. GSTM1 gene has 8 exons flanked by two almost identical 4.2-kb regions and GSTM1*0 deletion polymorphism is caused by a homologous recombination process involving both repeats (Xu et al. 1998). Studies focussing on genetic polymorphisms of GSTM1 have compared the homozygous deletion genotype with genotypes having one functional allele. Homozygous gene deletions exhibit variable frequencies in different ethnic groups. GSTM1 has two other alleles designated as GSTM1A and GSTM1B which differ by a C > G substitution at base position 534 resulting in the substitution of Asn > Lys at amino acid 172 (Seidegard et al. 1998) though this results in no functional difference between the two alleles. GSTM1A and GSTM1B are, therefore, categorized together as non-null conjugator phenotypes. Several studies have reported an association between GSTM1*0 (homozygous deletion) and increased risk of cancers and with better treatment outcomes.
The rates of prevalence of null genotypes of GSTM1 are high across several ethnic groups with a meta-analysis of 30 studies (Garte et al. 2001) involving over 10,000 individuals reporting a frequency of 53% for the Caucasians and a similar frequency was seen in Asians but lower in African Americans (16–36%). In the USA, different ethnic groups exhibit differences in frequencies of GSTM1 such as from 23% to 41% for persons of African descent, from 32% to 53% for persons of Asian descent, from 40% to 53% for those of Hispanic descent, and from 35% to 62% for those of European descent. For South American populations, studies have reported frequencies of 21% for Chileans (Quinones et al. 1999), 55% for Caucasian Brazilians, 33% for Black Brazilians, and 20% for Amazonian Brazilians. European populations also exhibit variations in deletion frequency with 46% for French, 53% for Italians, 44% for Hungarians and 50% for the Slovaks. Some groups such as Pacific Islanders and Malaysians have a very high GSTM1 deletion frequency of 62–100%. Similarly, other Asian populations, such as the Japanese and Chinese, have frequencies ranging from 48% to 50% and 35% to 63%, respectively (Rebbeck 1997).
GSTT1 plays a role in detoxification of carcinogens found in tobacco smoke and pesticides, epoxybutanes and ethylene oxide. As opposed to the role of GSTM1, GSTT1 has both detoxification and activation roles as seen in case of activation of dihalomethanes to dichloromethane, which has been shown to cause liver and lung tumors in mice. GSTT1 is different from other members of GST family as it is expressed not only in the adult liver but also in human erythrocytes and thus has a wider role in detoxification of carcinogens in the body (Landi 2000). The GSTT subfamily is made up of two genes, GSTT1 and GSTT2.These are located at 22q11.2 and separated by about 50 kb having five exons each with identical intron/exon boundaries. However, these share only 55% amino acid identity. There is no role of GSTT2 in deletion of GSTT1 (Coggan et al. 1998). GSTT1 has two flanking 18 kb regions named as HA3 and HA5 with >90% homology and having identical 403-bp repeats, which function as deletion/junction regions of the GSTT1 null allele (Sprenger et al. 2000). GSTT1 deletion results from a homologous recombination event involving the left and right repeats causing a 54-kb deletion containing the entire GSTT1 gene. Ethnic variations have been reported regarding the distribution of null allele of GSTT1. Studies of GSTT1 null genotype demonstrate that 20% of Caucasians, 47–64% of Asians, 15–31% of Europeans and 22–29% of African Americans have deletion genotype of GSTT1. Asian populations have greater prevalence of GSTT1 compared to the Europeans as shown by studies which report 21% of Italians and 28% of Slovakians have deletion while 58% of Chinese, 38% of Malaysians (Lee et al. 1995), 42% and 46% Koreans have GSTT1 deletion genotype.
GSTP1 is involved in the metabolism and detoxification of many carcinogenic xenobiotics such as diol epoxides of polycyclic aromatic hydrocarbons (PAHs). GSTP1 has been the focus of several studies because of its over-expression in pre-neoplastic and tumor tissues which makes it useful as an early tumor marker, and is also responsible for drug resistance of many cancers. GSTP1 gene is located at 11q13 and is 2.8 kb long with seven exons (Morrow et al. 1989). The open reading frame starts at the 3′ end of the first exon and is 630 bp long, encoding a protein of 209 amino acids. GSTP1 has two common non-synonymous SNPs that result in Ile105Val and Ala114Val alterations in encoded amino acid sequence and are associated with variations in cancer risk and treatment response (McIlwain et al. 2006). The effect of Val105 substitution is due to steric restriction of the H-site due to shifts in the side chains of several amino acids which leads to less accommodation of less bulky substrates than the Ile105 allozyme (Johansson et al. 1998). Moreover, codon 105 variant allozyme has different thermal stability compared to the wild type (Johansson et al. 1998). These are the probable reasons for the use of GSTP1 as an early tumor marker and in pharmacogenetics. As seen with GSTM1 and GSTT1, ethnic variations have also been reported in the distribution of variant genotypes of GSTP1. In Africa, the frequency of GSTP1 Val105 variant has been reported to be 14% among South Africa, 16%, 12%, and 21% among Tanzanians, South African Venda, and Zimbabweans, respectively (Dandara et al. 2002) and 53% (The Gambia) (Wild et al. 2000). Caucasians have an allele frequency of 28–38%, while Asians have 16–26%. Another polymorphism of GSTP1, A114V, is less well studied and the variant allele is usually found in linkage disequilibrium with GSTP1 I105V. This polymorphism has not emerged as a prominent genetic variation of GSTP1 owing to its lower frequency and no effect on enzyme activity. It also exhibits a lower frequency of 5% in African Americans and 9% in European Americans (Watson et al. 1998). Table 10.3 lists some of the functionally important polymorphisms in GSTs.
4 Gene–Environment Interactions and Cancer Risk
4.1 Gene–Environment Interaction: Model and Issues
With rapid developments in the field of molecular biology, we now have a better understanding of the effect of genetic factors on human diseases though the genetic influences are exceedingly complex. Both genetic and environmental factors have role in determining the susceptibility to diseases and the study of gene–environment interaction is the key in genetic epidemiology. As for the interaction between any two risk factors for a disease, gene–environment interaction also faces the same complications such as the source of the interaction and its detection. Ottman (1996) provided possible models of relations between a genotype and an environmental exposure in terms of their effects on disease risk. In Model A, the effect of the genotype is to enhance the effect of a “risk factor” that can also be produced nongenetically, in Model B, the genotype worsens the effect of the risk factor, but there is no effect of the genotype in unexposed persons, in Model C, the exposure worsens the effect of the genotype, but there is no effect of the exposure in persons with the low-risk genotype, in Model D, both the exposure and the genotype are required to increase risk, and in Model E, the exposure and the genotype each have some effect on disease risk, and when they occur together risk is higher or lower than when they occur alone. For testing these models, individuals must be categorized based on the presence or absence of both the exposure and the high-risk genotype. Several strategies can be employed for testing these models such as testing for an identified susceptibility gene, measurement of candidate genes or ecogenetic markers (Perera and Whyatt 1994), using a genetic marker that is associated with the disease as a surrogate for the high-risk genotype (Saunders et al. 1993), linking of agenetic marker to a disease susceptibility gene, though the actual disease-causing mutation has not been identified and use of family history data as a surrogate for the genotype.
In the case of cancers, the model assumes that there is an association between cancer and the environmental factors such as tobacco smoking, and without the exposure, the genetic risk factors do not have a role in disease development. The genetic factors can modulate the association between exposure and cancer and in case of tobacco smoke, the relationship becomes more complex as the interaction is not linear but has a dose response (Taioli et al. 1998). There are also other important factors which need to be considered in taking smoking as an exposure. Some important factors are age when smoking started, smoking amount, type, duration, and number of quitting attempts (Vineis 2007). In case of breast cancer, age of starting smoking is crucial as young breast tissue is more prone to carcinogenesis compared to the more matured tissue. Moreover, age also plays a role in females as the sex hormone levels vary according to the age due to which the interaction between smoking and estrogen levels may play a significant role. The other important factor to consider is the interplay between causative factors of different cancer types and their interaction. For example, there is an effect of smoking on cancers which are caused by changes in hormone levels as tobacco smoking inhibits the aromatization of androgens into estrogens. Another area which also needs careful attention is epigenetic modifications. Environmental factors may trigger epigenetic changes which are independent of genetic variations as seen in case of hypermethylation of metabolic and DNA repair genes in several cancers (Russo et al. 2005). Studies have reported an association between methylation of genes and smoking, and, interestingly in one case, methylation of the p16 gene promoter was associated with early onset of smoking (Jarmalaite et al. 2003; Chang et al. 2004).
4.2 Interaction of Genetic Variations with Tobacco
Several studies have been conducted to decipher the association between genetic variations and cancer in relation to tobacco consumption. A number of meta- and pooled analysis have been done to study the association between several Phase I and Phase II metabolic gene polymorphisms and lung cancer (Schwartz et al. 2007). A study conducted by Singh et al. (2010) reported an increased risk of lung cancer in smokers who carried variant genotypes of CYP1A2. Similarly, an increased risk to lung cancer in cases who were regular tobacco chewers and carried variant genotypes of CYP1A2*1D or CYP1A2*1F was also observed in the study. Since CYP1A2 is induced by smoking and is involved in the metabolic activation of heterocyclic amines and procarcinogens (Landi et al. 1999; Bofetta et al. 2008), there is a strong interaction of smoking with polymorphic CYP1A2 genotypes in enhancing the risk to lung cancer. Other studies have also provided evidence for interaction of CYP1A1 and 1B1 genotypes with tobacco chewing in enhancing the susceptibility to lung cancer (Shah et al. 2008a, b). Apart from lung cancer, an elevated risk was also observed in smokers who carried variant alleles of CYP1A2*1D and CYP1A2*1F in pancreatic cancer (Li et al. 2006).
The Gallbladder cancer is a deadly malignancy which exhibits considerable differences in prevalence among certain ethnicities and geographic regions. The areas which are the most affected regions are the Indo-Gangetic plains of India, Mapuche Indians in Chile and South America (Sharma et al. 2017). A meta-analysis showed that GSTM1 deletion and NAT2 slow acetylator status were significantly associated with bladder cancer and an interaction with smoking was only observed for the NAT2 polymorphisms (García-Closas et al. 2005). Studies have also been carried out in the Indian population to study the role of genetic variations in the development of gall bladder cancer. A case-control genome-wide association study of gallbladder cancer cases and controls of Indian descent observed genome-wide significant associations for ABCB1 and ABCB4 genes which suggests the importance of hepatobiliary phospholipid transport in the pathogenesis of gallbladder cancer in Indian populations (Mhatre et al. 2017). Another study performed in a north Indian population showed significant associations of the SNPs in TERT (rs2736100C > A, CLPTM1L rs401681C > T and CASC8 rs6983267G > T) with gallbladder cancer risk (Yadav et al. 2018). Several other studies by Mittal and co-workers have also reported the association of polymorphisms in several genes with risk of gallbladder cancer in north Indian population. Genetic polymorphisms of IL-1 (Vishnoi et al. 2008), Complement receptor 1 (Srivastava and Mittal 2009), OGG1 and XRCC1 (Srivastava et al. 2009), ERCC2, MSH2, and OGG1 (Srivastava et al. 2010a), Caspase-8 (Srivastava et al. 2010b), CYP7A1 (Srivastava et al. 2010c), ADRβ3 T190C (Rai et al. 2014), and TERT-CLPTM1L and 8q24 (Yadav et al. 2018) were reported to be associated with gallbladder cancer risk. In an another gene–environment study in north Indian population, usage of tobacco (smoking or nonsmoking) by gallbladder cancer patients showed a significant increase in cancer risk with CYP1A1 Msp1 polymorphism (Pandey et al. 2008).
Studies conducted on HNSCC reported an association between tobacco use and genetic variations of CYP1A1 (Singh et al. 2009). Amount of tobacco use also influences the outcome of such interaction as a study in a Japanese population reported that the risk associated with CYP1A1*2A genotype is inversely proportional to the amount of tobacco use (Sato et al. 1999; Tanimoto et al. 1999) and Sato et al. (2000) observed that the risk was highest in the group with the lowest cigarette dose level. Variant genotypes of CYP1B1*2 were found to interact with cigarette smoking while no such significant interaction was reported with CYP1B1*3 or CYP1B1*4 (Li et al. 2005; Singh et al. 2008b). However, contrasting reports are also available with Ko et al. (2001) reporting that variant genotypes of CYP1B1*3 significantly interact with smoking and smokers with the variant genotypes were 20 times more likely to show evidence of p53 mutations than those with a CYP1B1 wild type genotype. As observed with tobacco smoking, significant gene–environment interaction was observed with variant genotypes of CYP1B1*2 and CYP1B1*3 and tobacco chewing (Singh et al. 2008b). Studies also show a positive correlation of variant genotypes of CYP2C19 with tobacco use which could be possibly attributed to the lower ability of cases with genetic variations for detoxifying the carcinogens generated by tobacco chewing or smoking (Sugimoto et al. 2005). In contrast, CYP2D6 genotypes did not appear to interact significantly with tobacco (Caporaso et al. 2001).
A study by Ruwali et al. (2009a) suggested that polymorphic CYP2E1 genotypes interact with tobacco and increase the HNSCC risk with a greater increase in risk observed in tobacco chewers which may be due to enhanced formation of nitrosamines in tobacco chewing (Hecht and Hoffmann 1988). RsaI polymorphism leads to a greater increase in transcription or enzyme activity than the DraI genotypes due to which stronger association was observed with RsaI (Uematsu et al. 1994). Soya et al. (2008) also reported an interaction between CYP2E1*6 (DraI) genotypes and tobacco among South Indian tobacco users for upper aerodigestive tract cancers. In addition, Harth et al. (2008) found an interaction of CYP1B1 (Leu432Val) and CYP2E1 (−70G > T) genotypes among smokers indicating the relevance of combined genotypes with exposure to tobacco smoke in significantly enhancing the HNSCC risk. In contrast, another study by Ruwali et al. (2009b) reported a reduction for HNSCC risk in individuals who are exposed to risk factors such as tobacco consumption (in the form of smoking and chewing) when compared to individuals who are not exposed to such risk factors and carrying the variant genotypes of CYP2A6. This reduction in HNSCC risk may possibly be attributed to a higher number of cases with variant genotypes of CYP2A6 to be non-tobacco users than tobacco users as variant alleles of CYP2A6 have been reported to reduce the risk of tobacco consumption in the form of smoking and thus it is smoking that results in a decreased HNSCC risk.
Among the phase II xenobiotic metabolizing enzymes, several studies have been carried out to investigate the association between genetic variations in GSTs and tobacco use. Studies have reported an association between null genotypes of GSTM1 or GSTT1 and tobacco use in head and neck cancer patients (Sabitha et al. 2008; Singh et al. 2008a; Ruwali et al. 2011). Smoking intensity also plays an important role in deciding the outcome of the interaction. A significant association of GSTM1 null genotype with laryngeal cancer risk in light smokers was observed (Jourenkova et al. 1998), while in some studies GSTM1 or GSTT1 null genotype was found to be linked to upper aerodigestive tract (UADT), non-laryngeal UADT or oral cancer risk in heavy smokers. Among the reasons for such an interaction could be the higher sister chromatid exchange (SCE) and chromosomal aberration levels in smokers with GSTM1 null genotype than GSTM1 positive smokers (Nora 2004). In contrast to these studies, some of the earlier studies failed to find any significant interaction of GST genotypes with tobacco-induced oral and pharyngeal cancer (Jourenkova-Mironova et al. 1999). For GSTP1, inconsistent reports are available regarding the relationship between the GSTP1 polymorphisms and smoking status in HNSCC though the variant forms of GSTP1 are more efficient in detoxifying the carcinogenic epoxide of benzo(a)pyrene with high and selective activity (Saarikoski et al. 1998).
4.3 Interaction of Genetic Variations with Alcohol
Similar to tobacco use, significant interaction has been reported between alcohol and genetic variations in phase I and phase II xenobiotic metabolizing enzymes. Heterozygous or homozygous genotype of CYP1B1*2 either alone or in combination resulted in high (five to sixfold) or very high (about 20 fold) increase in the risk to HNSCC (Singh et al. 2008b) though alcohol was not found to interact with CYP1A1 genotypes (Singh et al. 2009). Studies have further shown that individuals with variant genotypes of CYP2C19*2, CYP2C19*3, CYP2D6*4 and who were regular alcohol users were at several fold increase in the risk to HNSCC when compared to the controls, who were regular alcohol drinkers (Yadav et al. 2008, 2010). Similarly, alcohol consumption was also found to interact with variant CYP2E1 genotypes as the risk associated with RsaI variant genotypes and DraI variant genotypes was significantly higher in the HNSCC cases who were regular alcohol users when compared with the controls (Ruwali et al. 2009a). However, a study by Singh et al. (2010) found no significant increase in risk to lung cancer in alcohol users among cases with variant genotypes of CYP1A2 when compared to non-alcohol users. A study by Shah et al. (2008a) reported about 5-6 fold increase in the risk for lung cancer in the alcohol users with the variant genotypes of CYP1A1*2A and CYP1A1*2C. In a pooled analysis of cohort studies, it was found that alcohol consumption was associated with increased risk to lung cancer in male never smokers (Freudenheim et al. 2005). Since people who smoke are also alcohol users, the major concern in the examination of an association between alcohol consumption and lung cancer has been the failure to control for confounding by smoking.
Among the phase II xenobiotic metabolizing enzymes, several studies have been carried out to investigate the association between genetic variations in GSTs and alcohol use. A higher increase in HNSCC risk was observed in cases who were regular alcohol users and carried null genotypes of GSTM1 or GSTT1 compared to non-alcohol users (Singh et al. 2008a). Similarly, strong association in regular alcohol users carrying GSTT1 null genotype and a higher risk for multiple primary neoplasmas in UADT cancers was also reported (Soya et al. 2007). The role of alcohol–tobacco interaction in HNSCC risk was investigated by Peters et al. (2006) in a study which showed that deletion of GSTM1 markedly increased the alcohol–tobacco interaction. Homozygous deletion of GSTM1, tobacco, and alcohol exhibit a tri-modal interaction with the risk being higher among those who were both heavy smokers and low alcohol consumers with the possibility that alcohol may be facilitating the entry of tobacco carcinogens into oral tissues (Howie et al. 2001). Interestingly, there is also report that variants in certain genes lower the risk of various types of cancers in individuals who consume alcohol. One such gene is alcohol dehydrogenase (ADH) which is involved in the metabolism of alcohol. A study by Hashibe et al. (2008) analyzed six ADH variants in more than 3800 individuals with aerodigestive cancer and over 5200 controls. One variant each in ADH1B and ADH7 was significantly protective against aerodigestive cancer specifically in individuals who were alcohol drinkers, and most strongly in those who had higher alcohol intake. Individuals with the protective variant in ADH1B are known to metabolize alcohol up to 100 times faster than those without it, suggesting that lower exposure to alcohol is protective against the disease.
5 Conclusions
Environmental risk factors such as tobacco (in the form of smoking or chewing) or alcohol use increase the cancer risk in cases carrying the variant genotypes of phase I and phase II XMEs compared to those not exposed to these risk factors. Cancer is caused by certain changes in genes that control the functions of the cell related to growth and division. Cancer-causing gene mutations either occur over the course of a lifetime or are inherited from parents. Studies suggest that genetic variations in genes metabolizing tobacco and alcohol interact with these environmental risk factors and increase the cancer risk clearly stating the significance of gene–environment interactions. The studies indicate that gene–environment studies have a higher power than only environmental studies. The applications of gene–environment studies range from searching for new causes of disease (when the effects of the tested genes, environmental exposures or both are unknown), or exploring the mechanisms of cellular action of established environmental factors, such as smoking. Such studies need to assemble large data sets and large well-characterized populations in order to test complex gene–environment interaction pathways. This will help in improving accuracy and precision in the assessment of both genetic and environmental influences leading to well-informed recommendations for cancer prevention.
References
Accort NA, Waterbor JW, Beall C et al (2005) Cancer incidence among a cohort of smokeless tobacco users (United States). Cancer Causes Control 16:1107–1115
Altieri A, La Vecchia C, Negri E (2003) Fluid intake and risk of bladder and other cancers. Eur J Clin Nutr 57:S59–S68
Andre K, Schraub S, Mercier M et al (1995) Role of alcohol and tobacco in the aetiology of head and neck cancer: a case-control study in the Doubs region of France. Eur J Cancer B Oral Oncol 5:301–309
Asthana S, Patil RS, Labani S (2016) Tobacco-related cancers in India: a review of incidence reported from population-based cancer registries. Indian J Med Paediatr Oncol 37:152–157
Bagnardi V, Rota M, Botteri E et al (2015) Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer 112:580–593
Bofetta P, Hecht S, Grey N et al (2008) Smokeless tobacco and cancer. Lancet Oncol 9:667–675
Boffetta P, Hashibe M (2006) Alcohol and cancer. Lancet Oncol 7:149–156
Bolt HM, Their R (2006) Relevance of the deletion polymorphisms of the glutathione S-Transferases GSTT1 and GSTM1 in pharmacology and toxicology. Curr Drug Metab 7:613–628
Brennan P, Boffetta P (2004) Mechanistic considerations in the molecular epidemiology of head and neck cancer. IARC Sci Publ 157:393–414
Cai S, Li Y, Ding Y et al (2014) Alcohol drinking and the risk of colorectal cancer death: a meta-analysis. Eur J Cancer Prev 23:532–539
Caporaso NE, Lerman C, Audrain J et al (2001) Nicotine metabolism and CYP2D6 phenotype in smokers. Cancer Epidemiol Biomark Prev 10:261–263
Cascorbi I, Brockmoeller J, Roots I (1996) A C4887A polymorphism in exon 7 of human CYP1A1: population frequency, mutation linkages, and impact on lung cancer susceptibility. Cancer Res 56:4965–4969
Chang HW, Ling GS, Wei WI et al (2004) Smoking and drinking can induce p15 methylation in the upper aerodigestive tract of healthy individuals and patients with head and neck squamous cell carcinoma. Cancer 101:125–132
Choi SY, Kahyo H (1991) Effect of cigarette smoking and alcohol consumption in the aetiology of cancer of the oral cavity, pharynx and larynx. Int J Epidemiol 20:878–885
Coggan M, Whitbread L, Whittington A et al (1998) Structure and organization of the human theta-class glutathione S-transferase and D-dopachrome tautomerase gene complex. Biochem J 334:617–623
Daigo S, Takahashi Y, Fujieda M et al (2002) A novel mutant allele of the CYP2A6 gene (CYP2A6*11) found in a cancer patient who showed poor metabolic phenotype towards tegafur. Pharmacogenetics 12:299–306
Dandara C, Sayi J, Masimirembwa CM et al (2002) Genetic polymorphism of cytochrome P450 1A1 (CYP1A1) and glutathione transferases (M1, T1 and P1) among Africans. Clin Chem Lab Med 40:952–957
Danko IM, Chaschin NA (2005) Association of CYP2E1 gene polymorphism with predisposition to cancer development. Exp Oncol 27:248–256
Doll R, Hill AB (1950) Smoking and carcinoma of the lung; preliminary report. Br Med J 2:739–748
Doll R, Forman D, La Vecchia C et al (1999) Alcoholic beverages and cancers of the digestive tract and larynx. In: Health issues related to alcohol consumption, 2nd edn. Blackwell, Oxford, pp 351–393
Evans WE, Relling MV (1999) Pharmacogenomics: translating functional genomics into rational therapeutics. Science 286:487–491
Ferrari P, Jenab M, Norat T et al (2007) Lifetime and baseline alcohol intake and risk of colon and rectal cancers in the European prospective investigation into cancer and nutrition (EPIC). Int J Cancer 121:2065–2072
Franceschi S, Levi F, Dal Maso L et al (2000) Cessation of alcohol drinking and risk of cancer of the oral cavity and pharynx. Int J Cancer 85:787–790
Freudenheim JL, Ritz J, Smith-Warner SA et al (2005) Alcohol consumption and risk of lung cancer: a pooled analysis of cohort studies. Am J Clin Nutr 82:657–667
García-Closas M, Malats N, Silverman D et al (2005) NAT2 slow acetylation, GSTM1 null genotype, and risk of bladder cancer: results from the Spanish bladder Cancer study and meta-analyses. Lancet 366:649–659
Garte S, Gaspari L, Alexandrie AK et al (2001) Metabolic gene polymorphism frequencies in control populations. Cancer Epidemiol Biomark Prev 10:1239–1248
Guengerich FP, Kim DH, Iwasaki M et al (1991) Role of human cytochrome P-450 IIE1 in the oxidation of many low molecular weight cancer suspects. Chem Res Toxicol 4:168–179
Hamajima N, Hirose K, Tajima K et al (2002) Alcohol, tobacco and breast cancer--collaborative reanalysis of individual data from 53 epidemiological studies, including 58,515 women with breast cancer and 95,067 women without the disease. Br J Cancer 87:1234–1245
Hamid A, Wani NA, Kaur J (2009) New perspectives on folate transport in relation to alcoholism-induced folate malabsorption–association with epigenome stability and cancer development. FEBS J 276:2175–2191
Harth V, Schafer M, Abel J et al (2008) Head and neck squamous-cell cancer and its association with polymorphic enzymes of xenobiotic metabolism and repair. J Toxicol Environ Health 71:887–897
Hashibe M, McKay J, Curado M et al (2008) Multiple ADH genes are associated with upper aerodigestive cancers. Nat Genet 40:707–709
Hecht SS, Hoffmann D (1988) Tobacco-specific nitrosamines, an important group of carcinogens in tobacco and tobacco smoke. Carcinogenesis 9:875–884
Heinen MM, Verhage BA, Schouten LJ et al (2013) Alcohol consumption and risk of lymphoid and myeloid neoplasms: results of the Netherlands cohort study. Int J Cancer 133:1701–1712
Hildebrand CE, Gonzalez FJ, Kozak CA et al (1985) Regional linkage analysis of the dioxin-inducible P-450 gene family on mouse chromosome 9. Biochem Biophys Res Commun 130:396–406
Hoffman SM, Fernandez-Salguero P, Gonzalez FJ et al (1995) Organization and evolution of the cytochrome P450 CYP2A–2B-2F subfamily gene cluster on human chromosome 19. J Mol E 41:894–900
Hoffmann D, Djordjevic MV, Fan J et al (1995) Five leading US commercial brands of moist stuff in 1994: assessment of carcinogenic N-nitrosamines. J Natl Cancer Inst 87:1862–1869
Howie NM, Trigkas TK, Cruchley AT et al (2001) Short-term exposure to alcohol increases the permeability of human oral mucosa. Oral Dis 7:349–354
Hsu T, Furlong C, Spitz MR (1991) Ethyl alcohol as a cocarcinogen with special reference to the aerodigestive tract: a cytogenetic study. Anticancer Res 11:1097–1101
Huang RS, Chen P, Wisel S et al (2009) Population-specific GSTM1 copy number variation. Hum Mol Genet 15:366–372
Hung RJ, Boffetta P, Brockmoller J et al (2003) CYP1A1 and GSTM1 genetic polymorphisms and lung cancer risk in Caucasian non-smokers: a pooled analysis. Carcinogenesis 24:875–882
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans (2012) Personal habits and indoor combustions. Volume 100 E. a review of human carcinogens. IARC Monogr Eval Carcinog Risks Hum 100:1–538
Ingelman-Sundberg M (2004) Human drug metabolising cytochrome P450 enzymes: properties and polymorphisms. Naunyn Schmiedeberg’s Arch Pharmacol 369:89–104
Iribarren C, Tekawa IS, Sidney S et al (1999) Effect of cigar smoking on the risk of cardiovascular disease, chronic obstructive pulmonary disease, and cancer in men. N Engl J Med 340:1773–1780
Jarmalaite S, Kannio A, Anttila S et al (2003) Aberrant p16 promoter methylation in smokers and former smokers with nonsmall cell lung cancer. Int J Cancer 106:913–918
Johansson AS, Stenberg G, Widersten M et al (1998) Structure-activity relationships and thermal stability of human glutathione transferase P1-1 governed by the H-site residue 105. J Mol Biol 278:687–698
Jourenkova N, Reinikainen M, Bouchardy C et al (1998) Larynx Cancer risk in relation to glutathione S-Transferase M1 and T1 genotypes and tobacco smoking. Cancer Epidemiol Biomarkers Prev 7:19–23
Jourenkova-Mironova N, Voho A, Bouchardy C et al (1999) Glutathione S-transferase GSTM1, GSTM3, GSTP1 and GSTT1 genotypes and the risk of smoking-related oral and pharyngeal cancers. Int J Cancer 81:44–48
Kabat GC, Chang CJ, Wynder EL (1994) The role of tobacco, alcohol use, and body mass index in oral and pharyngeal cancer. Int J Epidemiol 23:1137–1144
Klatsky AL (2001) Diet, alcohol, and health: a story of connections, confounders, and cofactors. Am J Clin Nutr 74:279–280
Ko Y, Abel J, Harth V et al (2001) Association of CYP1B1 codon 432 mutant allele in head and neck squamous cell cancer is reflected by somatic mutations of p53 in tumor tissue. Cancer Res 61:4398–4404
Landi S (2000) Mammalian class theta GST and differential susceptibility to carcinogens: a review. Mutat Res 463:247–283
Landi MT, Sinha R, Lang NP et al (1999) Human cytochrome P4501A2. IARC Sci Publ 148:179–195
Lee EJ, Wong JY, Yeoh PN et al (1995) Glutathione S-transferase theta (GSTT1) genetic polymorphism among Chinese, Malays and Indians in Singapore. Pharmacogenetics 5:332–334
Li G, Liu Z, Sturgis EM et al (2005) CYP2E1 G1532C, NQO1 Pro187Ser, and CYP1B1 Val432Leu polymorphisms are not associated with risk of squamous cell carcinoma of the head and neck. Cancer Epidemiol Biomark Prev 14:1034–1036
Li D, Jiao L, Li Y et al (2006) Polymorphisms of cytochrome P4501A2 and N-acetyltransferase genes, smoking, and risk of pancreatic cancer. Carcinogenesis 27:103–111
McIlwain C, Townsend D, Tew K (2006) Glutathione S-transferase polymorphisms: cancer incidence and therapy. Oncogene 25:1639–1648
Mhatre S, Wang Z, Nagrani R et al (2017) Common genetic variation and risk of gallbladder cancer in India: a case-control genome-wide association study. Lancet Oncol 18:535–544
Morrow CS, Cowan KH, Goldsmith ME (1989) Structure of the human genomic glutathione S-transferase-pi gene. Gene 75:3–11
Mukherji B (2013) Immunology of melanoma. Clin Dermatol 31:156–165
Murata M, Takayama K, Choi B et al (1996) A nested case-control study on alcohol drinking, tobacco smoking, and cancer. Cancer Detect Prev 20:557–565
Nakajima T, Aoyama T (2000) Polymorphism of drug-metabolizing enzymes in relation to individual susceptibility to industrial chemicals. Ind Health 38:143–152
Nakajima M, Yokoi T, Mizutani M et al (1999) Genetic polymorphism in the 5′-flanking region of human CYP1A2 gene: effect on the CYP1A2 inducibility in humans. J Biochem (Tokyo) 125:803–808
Nebert DW, Russell DW (2002) Clinical importance of the cytochromes P450. Lancet 360:1155–1162
Nelson DR, Koymans L, Kamataki T et al (1996) P450 superfamily: update on new sequences, gene mapping, accession numbers and nomenclature. Pharmacogenetics 6:1–42
Neufeld KJ, Peters DH, Rani M et al (2005) Regular use of alcohol, and tobacco in India and its association with age, gender and poverty. Drug Alcohol Depend 77:283–291
Newsholme A (1903) The possible association of the consumption of alcohol with excessive mortality from cancer. Br Med J 2:1529–1531
Nora H (2004) Cytogenetic biomarkers and genetic polymorphisms. Toxicol Lett 149:309–334
Oscarson M (2001) Genetic polymorphisms in the cytochrome P450 2A6 (CYP2A6) gene: implications for interindividual differences in nicotine metabolism. Drug Metab Dispos 29:91–95
Ottman R (1996) Gene-environment interaction: definitions and study designs. Prev Med 25:764–770
Pandey SN, Choudhuri G, Mittal B (2008) Association of CYP1A1 Msp1 polymorphism with tobacco-related risk of gallbladder cancer in a north Indian population. Eur J Cancer Prev 17:77–81
Patten CJ, Smith TJ, Friesen MJ et al (1997) Evidence for cytochrome P450 2A6 and 3A4 as major catalysts for N′-nitrosonornicotine alpha-hydroxylation by human liver microsomes. Carcinogenesis 18:1623–1630
Perera FP, Whyatt R (1994) Biomarkers and molecular epidemiology in mutation/cancer research. Mutat Res 313:117–129
Persson I, Johansson I, Bergling H et al (1993) Genetic polymorphism of cytochrome P4502E1 in a Swedish population relationship to incidence of lung cancer. FEBS Lett 319:207–211
Peters ES, McClean MD, Marsit CJ et al (2006) Glutathione S-transferase polymorphisms and the synergy of alcohol and tobacco in oral, pharyngeal, and laryngeal carcinoma. Cancer Epidemiol Biomark Prev 15:2196–2202
Quinones L, Berthou F, Varela N et al (1999) Ethnic susceptibility to lung cancer: differences in CYP2E1, CYP1A1, and GSTM1 genetic polymorphisms between French Caucasian and Chilean populations. Cancer Lett 141:167–171
Rai R, Sharma KL, Misra S (2014) Association of adrenergic receptor gene polymorphisms in gallbladder cancer susceptibility in a north Indian population. J Cancer Res Clin Oncol 140:725–735
Rebbeck T (1997) Molecular epidemiology of the human glutathione S-transferase genotypes GSTM1 and GSTT1 in cancer susceptibility. Cancer Epidemiol Biomark Prev 6:733–743
Roberts DL (1988) Natural tobacco flavour. Recent Adv Tobacco Sci 14:45–81
Russo AL, Thiagalingam A, Pan H et al (2005) Differential DNA hypermethylation of critical genes mediates the stage-specific tobacco smoke-induced neoplastic progression of lung cancer. Clin Cancer Res 11:2466–2470
Ruwali M, Khan AJ, Shah PP et al (2009a) Cytochrome P450 2E1 and head and neck cancer: interaction with genetic and environmental risk factors. Env Mol Mut 50:473–482
Ruwali M, Pant MC, Shah PP et al (2009b) Polymorphism in cytochrome P450 2A6 and glutathione S-transferase P1 modifies head and neck cancer risk and treatment outcome. Mutat Res 669:36–41
Ruwali M, Singh M, Pant MC et al (2011) Polymorphism in glutathione S-transferases: susceptibility and treatment outcome for head and neck cancer. Xenobiotica 41:1122–1130
Saarikoski ST, Voho A, Reinikainen M et al (1998) Combined effect of polymorphic GST genes on individual susceptibility to lung cancer. Int J Cancer 77:516–521
Sabitha K, Reddy MVV, Jamil K (2008) GST genotypes in head and neck cancer patients and its clinical implications. Afr J Biotechnol 7:3853–3859
Saladi RN, Nektalova T, Fox JL (2010) Induction of skin carcinogenicity by alcohol and ultraviolet light. Clin Exp Dermatol 35:7–11
Sato M, Sato T, Izumo T et al (1999) Genetic polymorphism of drug-metabolizing enzymes and susceptibility to oral cancer. Carcinogenesis 20:1927–1931
Sato M, Sato T, Izumo T et al (2000) Genetically high susceptibility to oral squamous cell carcinoma in terms of combined genotyping of CYP1A1 and GSTM1 genes. Oral Oncol 36:267–271
Saunders AM, Strittmatter WJ, Schmechel D et al (1993) Association of apolipoprotein E allele ε4 with late-onset familial and sporadic Alzheimer’s disease. Neurology 43:1467–1472
Schlecht NF, Franco EL, Pintos J et al (1999) Interaction between tobacco and alcohol consumption and the risk of cancers of the upper aero-digestive tract in Brazil. Am J Epidemiol 150:1129–1137
Schmidt JV, Bradfield CA (1996) Ah receptor signaling pathways. Ann Rev Cell Dev Biol 12:55–89
Schoedel KA, Hoffmann EB, Rao Y et al (2004) Ethnic variation in CYP2A6 and association of genetically slow nicotine metabolism and smoking in adult Caucasians. Pharmacogenetics 14:615–626
Schwartz AG, Prysak GM, Bock CH et al (2007) The molecular epidemiology of lung cancer. Carcinogenesis 28:507–518
Seidegard J, Vorachek W, Pero R et al (1998) Hereditary differences in the expression of the human glutathione transferase active on trans-stilben oxide are due to a gene deletion. Proc Natl Acad Sci U S A 85:7203–7207
Shah PP, Singh AP, Singh M et al (2008a) Association of functionally important polymorphisms in cytochrome P4501B1 with lung cancer. Mutat Res 633:31–37
Shah PP, Singh AP, Singh M et al (2008b) Interaction of cytochrome P4501A1 genotypes with other risk factors and susceptibility to lung cancer. Mutat Res 639:1–10
Sharma JD, Kalit M, Nirmolia T et al (2014) Cancer: scenario and relationship of different geographical areas of the globe with special reference to north East-India. Asian Pac J Cancer Prev 15:3721–3729
Sharma A, Sharma KL, Gupta A et al (2017) Gallbladder cancer epidemiology, pathogenesis and molecular genetics: recent update. World J Gastroenterol 23:3978–3998
Shimada T, Watanabe J, Kawajiri K et al (1999) Catalytic properties of polymorphic human cytochrome P4501B1 variants. Carcinogenesis 20:1607–1613
Singh M, Shah PP, Singh AP et al (2008a) Association of genetic polymorphisms in glutathione S-transferases and susceptibility to head and neck cancer. Mutat Res 638:184–194
Singh AP, Shah PP, Mathur N et al (2008b) Genetic polymorphisms in cytochrome P4501B1 and susceptibility to head and neck cancer. Mutat Res 639:11–19
Singh AP, Shah PP, Ruwali M et al (2009) Polymorphism in cytochrome P4501A1 is significantly associated with head and neck cancer risk. Cancer Investig 27:869–876
Singh AP, Pant MC, Ruwali M et al (2010) Polymorphism in cytochrome P450 1A2 and their interaction with risk factors in determining risk of squamous cell lung carcinoma in men. Cancer Biomark 8:351–359
Singletary KW, Gapstur SM (2001) Alcohol and breast cancer: review of epidemiologic and experimental evidence and potential mechanisms. JAMA 286:2143–2151
Soya SS, Padmaja N, Adithan C (2005) Genetic polymorphism of CYP2E1 and GSTP1 in a south Indian population-comparisons with North India, Caucasians and Chinese. Asian Pac J Cancer Prev 6:315–319
Soya SS, Vinod T, Reddy KS et al (2007) Genetic polymorphisms of glutathione-S-transferase genes (GSTM1, GSTT1 and GSTP1) and upper aerodigestive tract cancer risk among smokers, tobacco chewers and alcoholics in an Indian population. Eur J Cancer 43:2698–2706
Soya SS, Vinod T, Reddy KS et al (2008) CYP2E1 polymorphisms and gene-environment interactions in the risk of upper aerodigestive tract cancers among Indians. Pharmacogenomics 9:551–560
Sprenger R, Schlagenhaufer R, Kerb R et al (2000) Characterization of the glutathione S-transferase GSTT1 deletion: discrimination of all genotypes by polymerase chain reaction indicates a trimodular genotype–phenotype correlation. Pharmacogenetics 10:557–565
Srivastava A, Mittal B (2009) Complement receptor 1 (A3650G RsaI and intron 27 HindIII) polymorphisms and risk of gallbladder cancer in north Indian population. Scand J Immunol 70:614–620
Srivastava A, Srivastava K, Pandey SN (2009) Single-nucleotide polymorphisms of DNA repair genes OGG1 and XRCC1: association with gallbladder cancer in north Indian population. Ann Surg Oncol 16:1695–1703
Srivastava K, Srivastava A, Mittal B (2010a) Polymorphisms in ERCC2, MSH2, and OGG1 DNA repair genes and gallbladder cancer risk in a population of northern India. Cancer 116:3160–3169
Srivastava K, Srivastava A, Mittal B (2010b) Caspase-8 polymorphisms and risk of gallbladder cancer in a northern Indian population. Mol Carcinog 49:684–692
Srivastava A, Choudhuri G, Mittal B (2010c) CYP7A1 (−204 a>C; rs3808607 and −469 T>C; rs3824260) promoter polymorphisms and risk of gallbladder cancer in north Indian population. Metabolism 59:767–773
Stepanov I, Hecht SS, Ramakrishnan S et al (2005) Tobacco specific nitrosamines in smokeless tobacco products marketed in India. Int J Cancer 116:16–19
Stephens EA, Taylor JA, Kaplan N et al (1994) Ethnic variation in the CYP2E1 gene: polymorphism analysis of 695 African-Americans, European-Americans and Taiwanese. Pharmacogenetics 4:185–192
Stitch HF, Parida BB, Brunnemann KD (1992) Localized formation of micronuclei in the oral mucosa and tobacco specific nitrosamines in the saliva of reverse smokers. Int J Cancer 50:172–176
Sugimoto M, Furuta T, Shirai N et al (2005) Poor metabolizer genotype status of CYP2C19 is a risk factor for developing gastric cancer in Japanese patients with helicobacter pylori infection. Aliment Pharmacol Ther 22:1033–1040
Taioli E, Zocchetti C, Garte S (1998) Models of interaction between metabolic genes and environmental exposure in cancer susceptibility. Environ Health Perspect 106:67–70
Takahiko K, Yuko Y, Mayumi T et al (2008) Genetic polymorphisms of human cytosol glutathione S-transferases and prostate cancer. Pharmacogenomics 9:93–104
Tanimoto K, Hayashi S, Yoshiga K et al (1999) Polymorphisms of the CYP1A1 and GSTM1 gene involved in oral squamous cell carcinoma in association with a cigarette dose. Oral Oncol 35:191–196
Tramacere I, Pelucchi C, Bonifazi M (2012a) A meta-analysis on alcohol drinking and the risk of Hodgkin lymphoma. Eur J Cancer Prev 21:268–273
Tramacere I, Pelucchi C, Bonifazi M (2012b) Alcohol drinking and non-Hodgkin lymphoma risk: a systematic review and a meta-analysis. Ann Oncol 23:2791–2798
Uematsu F, Kikuchi H, Motomiya M et al (1991) Association between restriction fragment length polymorphism of the human cytochrome P45011E1 gene and susceptibility to lung cancer. Jpn J Cancer Res 82:254–256
Uematsu F, Ikawa S, Kikuchi S et al (1994) Restriction fragment length polymorphism of the human CYP2E1 (cytochrome P450IIE1) gene and susceptibility to lung cancer: possible relevance to low smoking exposure. Pharmacogenetics 4:58–63
Vineis P (2007) The challenge of low levels of exposure. Prev Med 44:107–108
Vishnoi M, Pandey SN, Choudhuri G et al (2008) IL-1 gene polymorphisms and genetic susceptibility of gallbladder cancer in a north Indian population. Cancer Genet Cytogenet 186:63–68
Viswanathan H, Wilson JA (2004) Alcohol--the neglected risk factor in head and neck cancer. Clin Otolaryngol Allied Sci 29:295–300
Watanabe J, Hayashi S, Nakachi K et al (1990) PstI and RsaI RFLPs in complete linkage disequilibrium at the CYP2E gene. Nucleic Acids Res 18:7194
Watson RR, Nixon P, Seitz HK et al (1994) Alcohol and cancer. Alcohol Alcohol Sul 2:453–455
Watson MA, Stewart RK, Smith GB et al (1998) Human glutathione S-transferase P1 polymorphisms: relationship to lung tissue enzyme activity and population frequency distribution. Carcinogenesis 19:275–280
Wild CP, Yin F, Turner PC et al (2000) Environmental and genetic determinants of aflatoxin-albumin adducts in the Gambia. Int J Cancer 86:1–7
World Cancer Research Fund (2007) Food, nutrition, physical activity, and the prevention of Cancer: a global perspective. American Institute for Cancer Research, Washington DC
World Health Organization (2018) Global status report on alcohol and health. World Health Organization, Geneva
Wynder EL, Graham EA (1950) Tobacco smoking as a possible etiologic factor in bronchiogenic carcinoma; a study of 684 proved cases. J Am Med Assoc 143:329–336
Xu SJ, Wang YP, Roe B et al (1998) Characterization of the human class mu glutathione S-transferase gene cluster and the GSTM1 deletion. J Biol Chem 273:3517–3527
Yadav SS, Ruwali M, Shah PP et al (2008) Association of poor metabolizers of cytochrome P450 2C19 with head and neck cancer and poor treatment response. Mutat Res 644:31–37
Yadav SS, Ruwali M, Pant MC et al (2010) Interaction of drug metabolizing cytochrome P450 2D6 poor metabolizers with cytochrome P450 2C9 and 2C19 genotypes modify the susceptibility to head and neck cancer and treatment response. Mutat Res 684:49–55
Yadav S, Chandra A, Kumar A et al (2018) Association of TERT-CLPTM1L and 8q24 common genetic variants with gallbladder Cancer susceptibility and prognosis in north Indian population. Biochem Genet 56:267–282
Yu HS, Oyama T, Isse T et al (2010) Formation of acetaldehyde-derived DNA adducts due to alcohol exposure. Chem Biol Interact 188:367–375
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Ruwali, M., Shukla, R. (2021). Interactions of Environmental Risk Factors and Genetic Variations: Association with Susceptibility to Cancer. In: Singh, A., Srivastava, S., Rathore, D., Pant, D. (eds) Environmental Microbiology and Biotechnology. Springer, Singapore. https://doi.org/10.1007/978-981-15-7493-1_10
Download citation
DOI: https://doi.org/10.1007/978-981-15-7493-1_10
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-7492-4
Online ISBN: 978-981-15-7493-1
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)