Abstract
Telemedicine has been used worldwide in several medical specialties including Ophthalmology. However, its use in infant eye screening especially for Retinopathy of Prematurity (ROP) has been more limited. Ironically, it is for this disease entity wherein telemedicine promises possibly the highest benefit. A short time window of screening, a standard classification of the disease, specially designed infant retinal cameras and lossless image transfer tools make this feasible. Furthermore, the lack of trained experts and the large number of infants that require screening in the outreach make “tele-ROP” an attractive prospect. Yet, its relatively poor adoption can be attributed to several real-world challenges like the cost of the technology, cost of implementation, cost benefit, and medicolegal concerns. Drawing from the experience of over 150,000 infant screening sessions in the “KIDROP- Tele-ROP” program in India, this chapter addresses these challenges and suggests possible solutions for a wider expansion.
Authors have no conflict of interest.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Retinopathy of prematurity
- Tele-medicine
- Tele-ROP
- KIDROP
- Wide-field imaging
- RetCam shuttle
- Neo
- WISE-ROP
- Impact
Telemedicine (TM) is a subset of telehealth aimed to address uneven distribution and shortage of human resources and infrastructure in delivering primary or secondary healthcare. It employs communication networks to provide healthcare services and/or medical education to another geographic location [1]. Telemedicine in radiology is in vogue for over five decades. Its uptake in other fields of medicine has become increasingly popular with the advent of image-based documentation and the ubiquitous internet.
Telemedicine in ophthalmology has been used especially in the screening and management of retinal disorders. A meta-analysis concluded that digital imaging techniques combining mydriasis with wide-field imaging can be effectively used for diabetic retinopathy (DR) screening [2]. It has also been used in the evaluation of the optic nerve, visual fields, and nerve fiber layer analysis. Increasingly, no ophthalmic subspecialty is untouched by telemedicine [3]. In middle-income countries like India, the telemedicine model has been successfully used for DR screening using non-mydriatic fundus photography captured on low-cost, portable, indigenous cameras that provide screening, especially in the rural areas [4, 5]. Telemedicine in pediatric retinal diseases, with a special focus on Retinopathy of prematurity (ROP) has evolved more recently and will be the focus of this chapter.
1 Telemedicine in Retinopathy of Prematurity
ROP appears to fulfill the criteria described by Wilson and Jungner [6] for screening a disease of public health importance. These include the fact that it is an important health problem in a defined population subset, with a natural history that is studied, an accepted diagnostic test, treatment, and an agreed policy on who to treat. Importantly, case finding should be a continuous process and not a “once and for all” project.
ROP is one of the leading causes of preventable infant blindness in the world especially plaguing middle-income countries. Indirect ophthalmoscopy was regarded as the gold standard for screening. However, with the increasing number of infants requiring screening and a scarcity of ROP specialists, other models of screening have been suggested and used around the world. (Table 8.1) [7] There has been an evolution from “proof of concept” regarding the use of telemedicine in ROP to real-world scenarios. A report by the American Association of Ophthalmologists AAO concluded that wide-angle digital fundus photography can complement standard ROP care. It provides objective documentation of clinical examination findings, improved recognition of disease progression by comparing previous photographs and opportunities for education and research [8, 9].The advantages of telemedicine in ROP are listed in (Table 8.2).
Telemedicine for ROP uses remote digital fundus imaging (RDFI). The concept was first proposed in 1999 [10]. It used the store and forward, “hub and spoke” model. The images were obtained from the neonatal intensive care unit (NICU) and stored and then uploaded via the Internet. The images were then received and interpreted by the grader. Multiple NICU served as the spoke while the reader serves as the hub [11]. Ells et al. defined two important concepts for RDFI, i.e., “standardized fundus imaging” and “referral warranted ROP.” The standardized fundus images consisted of five images captured for each eye; these included posterior pole, temporal, nasal, superior, and inferior retinal fields. Referral-warranted ROP (RW-ROP) was defined as: any ROP in zone 1, the presence of plus disease, or the presence of any stage 3 ROP [12]. The PHOTO ROP trial gave another set of six standard images used widely [13, 14]. Six images consisted of five images from the study of Ells et al. and one external iris photograph. Lorenz et al. used the term “suspected treatment-requiring ROP” (STR- ROP) which included threshold ROP zone II, pre-threshold ROP zone I (type-1 ROP according to ETROP). Importantly, some ROP requiring treatment are not reliably gradable from the images [15]. Comparing both RW-ROP and STR-ROP eyes that finally received laser therapy, a different referral pattern emerged. In the study by Ells et al., only 43.5% of eyes with RW-ROP (10/23 eyes) received laser therapy compared to 88.2% of the eyes with STR-ROP in the study by Lorenz et al. (30/34). The wider definition of RW-ROP by Ells ensures a higher level of safety but considerably lowers the positive predictive value as to STR-ROP.
The KIDROP model is an example of a highly successful RDFI tele-ROP model in a middle-income country [16,17,18]. The model employs accredited nonphysicians to image, grade, and report ROP while in NICU. The reporting based on triage using a decision-based algorithm of “red,” “orange,” and “green” groups which represent patients requiring treatment, needing follow-up, or fit for discharge, respectively. These are based on the ETROP classification and creates a wider safety net. Images captured are uploaded on the cloud and are accessible on the smartphones of ROP specialists located remotely. Another layer in the safety net is that infants are discharged from screening only if “mature retina” appears, i.e., the vascularization noted up to the ora serrata is documented in two successive visits between 41 and 45 weeks postmenstrual age. The KIDROP model differed from other programs in: (1) non- physicians are allowed to report and analyze the images as the first point of contact, thereby providing the diagnosis and decision to the rural mother before she leaves the center; (2) indirect ophthalmoscopy is not mandated before an infant can be discharged from screening; and (3) the program aims at detecting any stage, not just treatment-requiring disease. This differs from other programs that used referral-warranted or treatment requiring ROP as their end-point [12, 15]. Table 8.3 compares various RDFI model. However, currently, telemedicine techniques amount to only 21% of ROP screening services [25].
2 Challenges in Tele-ROP
The challenges in the promotion of Tele-ROP screening in ROP have been summarized in Table 8.4 and have been addressed below:
-
1.
Cost of the implementation of an ROP program involves: (a) the cost of the camera and the viewing software and the maintenance of the equipment; (b) human resource training; (c) salaries of the imaging and grading teams; (d) recurrent transport costs of the device and team; and (e) cost of the consumables.
-
(a).
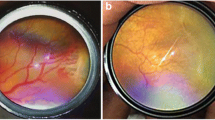
Cost of the camera: Cameras currently available for telemedicine screening in ROP are relatively expensive. Most tele-ROP programs have used the RetCam family of products, most commonly the RetCam Shuttle (Formerly Clarity Medical Systems, USA, now Natus, USA). More recently, the “3Nethra Neo” developed in India is a more affordable option [26]. The “Neo” is a wide-field camera providing a 120-degree field of view and has some advancements in the liquid lens system to dynamically focus the image, an LED light source, and an integrated lens hand piece. The image resolution is better at 2040 × 2040 pixels when compared to 1800 × 1600 of the RetCam Shuttle. The images are a “square” which provides an extra arc of the superior and inferior retina which are lost in images from the RetCam’s rectangular images. The “Neo” has been evaluated as an ROP screening tool by comparing it with images from the RetCam. Sensitivity of 97–99% and specificity of 75–81% were reported for diagnosis and decision from a cohort of preterm infants [27]. The systemic and ophthalmic safety of the camera have been established [26]. A novel smartphone-based fundus camera with the ability to image peripheral retina has been reported to be useful in imaging infants with ROP [28]. Comparison of the three camera systems is summarized in Table 8.5.
-
(b).
Cost-effectiveness : Besides the cost of the camera, other recurrent costs include training and certification of the imagers, costs involved in data capture, storage and transfer while adhering to HIPAA and other regulatory requirements, financial compensation of the imagers and the cost of transport which would vary depending on the number of centers and the size of the geographic zones.
Telemedicine pricing has normalized costs across geographic areas. Pricing variation in the local market tends to normalize when the number of service providers increases and compete among themselves. The availability of more affordable ROP cameras in the last 5 years is an example in this regard.
NICUs often have contracts with local ophthalmologists to perform ROP screening using indirect ophthalmoscopy. The cost of hiring includes being paid for work and also for the perceived risk of medicolegal liability. With the increasing trend in the latter, there has been a decline in the number of specialized ophthalmologists willing to screen. A survey indicated that there was difficulty in retaining or maintaining screeners for ROP in NICU [25]. A survey by the AAO reported that only 76% of the specialists providing ROP screening services intended to continue forward [29]. This leads to failure of the NICU to hire screening specialists. In developing countries like India, there are less than 200 ROP specialists to screen an overwhelming number of preterm infants [30]. This leads to an inefficient screening model which is both time consuming for the screening physician and expensive to the service provider.
The cost-effectiveness of the tele-screening model over indirect ophthalmoscopy has been established previously [31]. A Hungarian tele-screening program concluded that bedside screening with remote interpretation was more cost-saving than transport-based screening with indirect ophthalmoscopy from the perspective of the service provider and also the return on initial (ROI) investment recovered within 5 years after the project initiation [32].
-
(c).
Image quality and resolution : Image quality plays a very important role in grading of ROP effectively and reliably. Ungradable images ranged from 8% to 21% among the published studies [13, 33].
Factors affecting the image quality are small palpebral fissure, suboptimal pupil dilatation, darkly pigmented fundi, poor contrast, corneal and vitreous haze due to extreme prematurity, cataract, vitreous hemorrhage, hyaloid reminant, retinal pigment epithelium thickness, choroidal blood vessels, and motion artifacts. Better image quality and a large number of images have been found to be associated with greater sensitivity for detecting RW-ROP. Repeated imaging or referral for standard ROP examination was suggested when less than four acceptable quality images were obtained [34]. Newer ROP cameras have better resolution of 2040 × 2040 compared to previously available RetCams [26].
Another method to improve image quality is by image enhancement. RetiView is a noninvasive and inexpensive method of customized image enhancement [35]. It helps to detect clinically difficult characteristics in APROP images and can influence treatment planning. Various image processing techniques like Gabor filter, Canny’s method, and geometrical methods, study changes in the characteristics of the major temporal arcade and provides good accuracy in computer-aided diagnosis of plus disease [36] especially useful in APROP [37].
-
(d).
Training and accreditation of imagers : Non-physician imagers form the backbone of any tele-ROP program. Reports suggest that non-physician graders after being trained and certified can detect ROP with good intra-grader and inter-grader consistency and minimal temporal drift. Various successful programs have used imaging personnel ranging from physician to non-physician imagers are summarized in Table 8.3. The KIDROP STAT (Score for Training and Accreditation of Technicians) was developed to train and certify imagers. This comprises of three levels (I, II, and III) and has a 20 point score, which tests the knowledge, skill, and practice patterns of the imager in their native setting. On average, training a new imager can take between 30 and 90 working days. The training period has been considerably shortened after the introduction of online training. The online platform “WISE-ROP” (Wide-field Imaging for Screening and Education for ROP) has several training modules based on the onsite training curriculum [38, 39]. Imagers read and undergo self-assessment quizzes at the end of each module. Video sessions and viva voce to correct the technique and practical difficulties are scheduled with an assigned mentor. Skill is graded as per the STAT-Score levels and tested before a completion certificate is awarded [16, 39].
-
(e).
Medicolegal liability and regulation : Medicolegal liability assumes importance in telemedicine in ROP where compensation awarded runs in millions of dollars [40]. In India, US$350,000 has been awarded as a compensation against a government tertiary hospital for not providing “timely ROP screening.” To date, no lawsuit related to tele-ROP screening has been reported. But with increasing telemedicine practice, the risks are bound to increase. The laws governing telemedicine are poorly defined and differs widely among countries. The regulations regarding the duties and responsibilities of ophthalmologists in telemedicine are also not defined. The joint technical report by the American Academy of Paediatrics, the American Academy of Ophthalmology, and the American Academy of Certified Orthoptists have outlined relevant practical and risk management considerations that should be followed when including imaging-based ROP care [9]. The obligation of the ophthalmologists interpreting images for a reading center but not providing ROP care at the hospital is also not defined. Tracking and follow-up of these infants must be a joint responsibility between the pediatrician and ophthalmologist until the acute screening and/or treatment is completed. The National Health and Medical Research Council (NHMRC, Australia) report based on the Center for Disease Control (CDC) guidelines [7] on the KIDROP program noted that “regressing back from the current model of tele-imaging to indirect ophthalmoscopy performed by inadequately trained ophthalmologists is fraught with the danger of sub-optimal management of ROP care.” [7] This underlines the importance of accreditation and validation of ROP caregivers.
-
(f).
Government and financial support : To maintain a successful tele-ROP model regulatory, logistic and financial support from the government are important. Unfortunately, not many tele-ROP programs are supported by the government. The KIDROP model in India is an example of public–private partnership. The national telemedicine network for retinopathy of prematurity screening in Chile has been funded by the government [22]. National Task Force of ROP in India is an apex body that regulates and promotes such activities. In India, the operational guidelines for ROP from the National Task force (2018) for the first time recommend image-based screening as a viable alternative for ROP screening to indirect ophthalmoscopy. More participation is needed from the state and federal government to promote ROP care in the public health delivery system.
The Future of Tele-ROP
Artificial intelligence (AI) appears as a relatively cost-effective alternate accessible screening modality that is being explored in ophthalmology. FDA has recently approved the first autonomous AI system to provide a diagnostic decision independent of human graders and also checks the image quality [41]. Remidio AI-based software can make the diagnosis of sight-threatening diabetic retinopathy with high sensitivity [42].
It is intuitive to expect that AI in ROP has a good potential. ROP compared to DR is relatively limited by retinal findings but the complexity lies in the urgency of intervention in type 1 ROP and in the management of systemic comorbidity in a neonate compared to adults with DR. Deep convoluted neural network (CNN) models to identify plus disease have already been investigated [43]. Recently CNN models accurately assessed retinal fundus image quality in ROP in a manner comparable with the experts [44]. The i-ROP deep learning (DL) system has been found to accurately identify diagnostic categories and overall disease severity in an automated fashion. This iROP DL system has only been trained on posterior pole vascular morphology [45]. The data provides a proof of concept that a deep learning system can be used in an automated fashion to diagnose ROP.
A significant advantage of ROP screening with imaging, rather than indirect ophthalmoscopy lies in the documentation of other non-ROP conditions. In a study of 1450 preterm infants screened by the KIDROP program, 7.7% had a diagnosis other than ROP, which included conditions as severe as retinoblastoma [46]. Furthermore, the program has expanded to provide “universal screening,” for full-term, healthy infants consistent with the government’s universal health coverage program. In a study of 1021 term infants imaged within 3 days of birth showed that 4.7% had an abnormality, 1.6% required medical or surgical intervention [47].
Impact of Tele-ROP
An impact assessment of scaling up the image-based tele-ROP program in India showed that in the 10 high-risk ROP states, with a population of roughly 680 million, over 35,000 infants would be detected with ROP and over 1200 need treatment annually. The financial saving in “blind-person-year” (BPY) is estimated at USD 108 million [24]. The United Nations Development Program (UNDP) report on the tele-imaging program [48] and the National Health and Medical Research Council (NHMRC, Australia) report based on the Center for Disease Control (CDC) guidelines [7] on the KIDROP program, strongly suggest that wide-field imaging is likely to become the new gold standard in ROP screening for Indian and other nations with similar ROP demographics.
References
Sood S, Mbarika V, Jugoo S, Dookhy R, Doarn CR, Prakash N, Merrell RC. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E Health. 2007;13:573–90.
Shi L, Wu H, Dong J, Jiang K, Lu X, Shi J. Telemedicine for detecting diabetic retinopathy: a systematic review and meta-analysis. Br J Ophthalmol. 2015;99:823–31.
Newton MJ. The promise of telemedicine. Surv Ophthalmol. 2014;59:559–67.
Rani PK, Bhattarai Y, Sheeladevi S, ShivaVaishnavi K, Ali MH, Babu JG. Analysis of yield of retinal imaging in a rural diabetes eye care model. Indian J Ophthalmol. 2018;66:233–7.
Gadkari S. Innovative model for telemedicine-based screening for diabetic retinopathy in the developing world. Can J Ophthalmol. 2016;51:e109–11.
Wilson JMG, Jungner G. Principles and practice of screening for disease. WHO_PHP_34. (1968). Available at http://apps.who.int/iris/handle/10665/37650 Accessed 16 Oct 2017.
CDC. Developing an effective evaluation report. Available from: http://www.paediatrics.uwa.edu.au/__data/assets/pdf_file/0008/2816783/KIDROP-report-2015.pdf. (2013). Accessed 24 Apr 2020.
Chiang MF, Melia M, Buffenn AN, Lambert SR, Recchia FM, Simpson JL, Yang MB. Detection of clinically significant retinopathy of prematurity using wide-angle digital retinal photography: a report by the American Academy of Ophthalmology. Ophthalmology. 2012;119:1272–80.
Fierson WM, Capone JA. Telemedicine for evaluation of retinopathy of prematurity. Pediatrics. 2015;135:e238–54.
Lorenz B, Bock M, Muller HM, et al. Telemedicine based screening of infants at risk for retinopathy of prematurity. Stud Health Technol Inform. 1999;64:155–63.
Hartnett ME, editor. Pediatric retina. London: Lippincott Williams & Wilkins; 2005. p. 523–32.
Ells AL, Holmes JM, Astle WF, et al. Telemedicine approach to screening for severe retinopathy of prematurity: a pilot study. Ophthalmology. 2003;110:2113–7.
Photographic Screening for Retinopathy of Prematurity (Photo-ROP) Cooperative Group. The photographic screening for retinopathy of prematurity study (Photo-ROP): primary outcomes. Retina. 2008;28:S47–54.
Vinekar A, Trese MT, Capone A Jr, Photographic Screening for Retinopathy of Prematurity (PHOTO-ROP) Cooperative Group. Evolution of retinal detachment in posterior retinopathy of prematurity: impact on treatment approach. Am J Ophthalmol. 2008;145:548–55.
Lorenz B, Spasovska K, Elflein H, et al. Wide-field digital imaging based telemedicine for screening for acute retinopathy of prematurity (ROP). Six-year results of a multicentre field study. Graefes Arch Clin Exp Ophthalmol. 2009;247:1251–62.
Vinekar A, Gilbert C, Dogra M, Kurian M, Shainesh G, Shetty B, Bauer N. The KIDROP model of combining strategies for providing retinopathy of prematurity screening in underserved areas in India using wide-field imaging, tele-medicine, non-physician graders and smart phone reporting. Indian J Ophthalmol. 2014;62:41.
Vinekar A, Jayadev C, Mangalesh S, Shetty B, Vidyasagar D. Role of tele-medicine in retinopathy of prematurity screening in rural outreach centers in India–a report of 20,214 imaging sessions in the KIDROP program. Semin Fetal Neonatal Med. 2015;20:335–45.
Vinekar A, Jayadev C, Bauer N. Need for telemedicine in retinopathy of prematurity in middle-income countries: e-ROP vs KIDROP. JAMA Ophthalmol. 2015;133:360–1.
Weaver DT, Murdock TJ. Telemedicine detection of type 1 ROP in a distant neonatal inten- sive care unit. J AAPOS. 2012;16:229–33.
Fijalkowski N, Zheng LL, Henderson MT, et al. Stanford University network for diagnosis of retinopathy of prematurity (SUNDROP): five years of screening with telemedicine. Ophthalmic Surg Lasers Imaging Retina. 2014;45:106–13.
Quinn GE, Ying G, Daniel E, et al. Validity of a telemedicine system for the evaluation of acute-phase retinopathy of prematurity. JAMA Ophthalmol. 2014;132:1178–84.
Ossandón D, Zanolli M, Stevenson R, Agurto R, Ortiz P, Dotan G. A national telemedicine network for retinopathy of prematurity screening. J AAPOS. 2018;22:124–7.
Shah SP, Wu Z, Iverson S, et al. Specialist nurse screening for retinopathy of prematurity: a pilot study. Asia Pac J Ophthalmol (Phila). 2013;2:300–4.
Vinekar A, Mangalesh S, Jayadev C, Gilbert C, Dogra M, Shetty B. Impact of expansion of telemedicine screening for retinopathy of prematurity in India. Indian J Ophthalmol. 2017;65:390.
Vartanian RJ, Besirli CG, Barks JD, Andrews CA, Musch DC. Trends in the screening and treatment of retinopathy of prematurity. Pediatrics. 2017;139(1):e20161978.
Vinekar A, Rao SV, Murthy S, Jayadev C, Dogra MR, Verma A, Shetty B. A novel, low-cost, wide-field, infant retinal camera, “neo”: technical and safety report for the use on premature infants. Transl Vis Sci Technol. 2019;8(2):2.
Vinekar A, Dogra MR, Jayadev C, Murthy S, Rao SV, Shetty B. Evaluation of a new, low-cost, portable, wide-field, digital, retinal camera,“Neo” for screening infants for retinopathy of prematurity–a prospective, multi-center, validation report in Asian Indian infants. Invest Ophthalmol Vis Sci. 2016;57:11–20.
Sharma A. Emerging simplified retinal imaging. In: Bandello F, editor. Management of Diabetic Retinopathy, vol. 60. Basel: S. Karger; 2017. p. 56–62.
Roach L. ROP crisis near, survey says. News in review. EyeNet 2006.
Vinekar A, Azad R, Dogra MR, Narendran V, Jalali S, Bende P. The Indian retinopathy of prematurity society: a baby step towards tackling the retinopathy of prematurity epidemic in India. Ann Eye Sci. 2017;2:6.
Jackson KM, Scott KE, Zivin JG, Bateman DA, Flynn JT, Keenan JD, Chiang MF. Cost-utility analysis of telemedicine and ophthalmoscopy for retinopathy of prematurity management. Arch Ophthalmol. 2008;126:493–9.
Kovacs G, Somogyvári Z, Maka E, Nagyjánosi L. Bedside ROP screening and telemedicine interpretation integrated to a neonatal transport system: Economic aspects and return on investment analysis. Early Hum Dev. 2017;106:1–5.
Wu C, Petersen RA, Vanderveen DK. Retcam imaging for retinopathy of prematurity screening. J AAPOS. 2006;10:107–11.
Bothun ED, Morrison D, Ying GS, Daniel E, Baumritter A, Quinn G. Impact of number and quality of retinal images in a telemedicine screening program for ROP: results from the e-ROP study. J AAPOS. 2016;20:e11–2.
Jayadev C, Vinekar A, Mohanachandra P, Desai S, Suveer A, Mangalesh S, Bauer N, Shetty B. Enhancing image characteristics of retinal images of aggressive posterior retinopathy of prematurity using a novel software,(RetiView). Biomed Res Int. 2015;2015:898197.
Oloumi F, Rangayyan RM, Casti P, Ells AL. Computer-aided diagnosis of plus disease via measurement of vessel thickness in retinal fundus images of preterm infants. Comput Biol Med. 2015;66:316–29.
Rajashekar D, Srinivasa G, Vinekar A. Comprehensive retinal image analysis for aggressive posterior retinopathy of prematurity. PLoS One. 2016;11:e0163923.
Vinekar A. A Novel Online Retinopathy Of Prematurity (ROP) Training Model For Rural India–“WISEROP. COM”. Best Free Papers
Vinekar A, Bhende P. Innovations in technology and service delivery to improve Retinopathy of Prematurity care. Community Eye Health. 2018;31:S20.
Reynolds JD. Malpractice and the quality of care in retinopathy of prematurity (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2007;105:461.
Abràmoff MD, Lavin PT, Birch M, Shah N, Folk JC. Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices. Npj Digit Med. 2018;1:39.
Rajalakshmi R, Subashini R, Anjana RM, Mohan V. Automated diabetic retinopathy detection in smartphone-based fundus photography using artificial intelligence. Eye. 2018;32:1138–44.
Brown JM, Campbell JP, Beers A, Chang K, Ostmo S, Chan RP, Dy J, Erdogmus D, Ioannidis S, Kalpathy-Cramer J, Chiang MF. Automated diagnosis of plus disease in retinopathy of prematurity using deep convolutional neural networks. JAMA Ophthalmol. 2018;136:803–10.
Brown JM, Campbell JP, Beers A, Chang K, Donohue K, Ostmo S, Chan RP, Dy J, Erdogmus D, Ioannidis S, Chiang MF. Fully automated disease severity assessment and treatment monitoring in retinopathy of prematurity using deep learning. In Medical Imaging 2018: Imaging Informatics for Healthcare, Research, and Applications. 2018;10579:105790Q. International Society for Optics and Photonics.
Redd TK, Campbell JP, Brown JM, Kim SJ, Ostmo S, Chan RV, Dy J, Erdogmus D, Ioannidis S, Kalpathy-Cramer J, Chiang MF. Evaluation of a deep learning image assessment system for detecting severe retinopathy of prematurity. Br J Ophthalmol. 2018; https://doi.org/10.1136/bjophthalmol-2018-313156.
Jayadev C, Vinekar A, Bauer N, Mangalesh S, Mahendradas P, Kemmanu V, Mallipatna A, Shetty B. Look what else we found-clinically significant abnormalities detected during routine ROP screening. Indian J Ophthalmol. 2015;63:373.
Vinekar A, Govindaraj I, Jayadev C, Kumar AK, Sharma P, Mangalesh S, Simaldi L, Avadhani K, Shetty B, Bauer N. Universal ocular screening of 1021 term infants using wide‐field digital imaging in a single public hospital in India–a pilot study. Acta Ophthalmol. 2015;93:e372–6.
Good Practices Resource Book: Niti Ayog & UNDP. 2015. Last accessed 9 Apr 2019. http://www.niti.gov.in/writereaddata/files/human-development/Resource_Book_on_Good_Practices.pdf
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Vinekar, A., Sinha, S. (2021). Telemedicine in Retinopathy of Prematurity. In: Wu, WC., Lam, WC. (eds) A Quick Guide to Pediatric Retina. Springer, Singapore. https://doi.org/10.1007/978-981-15-6552-6_8
Download citation
DOI: https://doi.org/10.1007/978-981-15-6552-6_8
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-6551-9
Online ISBN: 978-981-15-6552-6
eBook Packages: MedicineMedicine (R0)