Abstract
The muscarinic acetylcholine receptors (mAChRs) are receptors that produce the GPCR complex in the membrane of specific neurons and other cells. It performs a key role at the end of the receptor stimulated by the neurotransmitter. Ach liberates from postganglionic neurons in a parasympathetic region of ANS. The mAChRs constitute a family of five interrelated GPCRs that come under the category of α branch of GPCRs’ Class A. The five different subtypes of the mAChR family are designated as M1–M5. M1, M3 and M5 subtype receptors exhibit to pair through the Gq/11 family of G proteins, but the M2 and M4 subtype receptors particularly indicate through Gi/o family of G protein. The mAChRs play multifunctional peripheral and central roles in human physiology including regulation of muscle contraction, heartbeat, lung, secretion by gland and other functions of the CNS.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Muscarinic receptors
- Acetylcholine receptor
- Anticholinergic drugs
- Central nervous system
- Atropa belladonna
13.1 Introduction
Acetylcholine receptor (AChR) is an intrinsic membranous type of protein, which reacts to the binding of the neurotransmitter acetylcholine (ACh) molecule. It is classified into muscarinic and nicotinic receptors based on their pharmacology and relative target to molecules (Verma et al. 2018). Muscarinic and nicotinic receptors are the main type of the cholinergic system. The cholinergic system, portion of the visceral or autonomic nervous system (ANS), plays a significant role in many functions such as circadian rhythmicity, digestion, addiction, control of heartbeat, motivation, blood pressure, cognitive flexibility, pain and reward, spatial learning and perceptual memory (Prado et al. 2017). mAChRs are well-known metabotropic acetylcholine receptors that are mainly reactive to muscarine. mAChRs are termed after muscarine, a lethal alkaloid produced by the highly poisonous mushroom Amanita muscaria (Jo et al. 2014). Scopolamine and atropine are the best known naturally occurring muscarinic antagonist, which is reported in the fatal nightshade plant: Atropa belladonna (Albuquerque et al. 2009). Nicotinic acetylcholine receptors (nAChRs) are famous ionotropic acetylcholine receptors particularly responsive to nicotine, Na+, Ca2+ and K+ ion channel (Corradi and Bouzat 2016). nAChR is named after nicotine, an ideal agonist. d-tubocurarine compound, a toxic alkaloid isolated from the curare poison, is a very well-known nicotinic antagonist (Malca Garcia et al. 2015) (Fig. 13.1).
13.1.1 Structure and Function of Muscarinic Receptor and Their Subtypes
The mAChRs are acetylcholine receptors, which produce the GPCR complex in the membrane of specific neurons and other cells (Eglen 2006). It performs a key role at the end of the receptor stimulated by the neurotransmitter. Ach liberates from postganglionic neurons in a parasympathetic region of ANS. The mAChRs constitute a family of five interrelated GPCRs that comes under the category of α branch of GPCRs Class A (Fredriksson et al. 2003). The five different subtypes of the mAChR family are designated as M1–M5 (encoded by CHRM1–CHRM5 genes). M1, M3 and M5 subtype receptors exhibit to pair through the Gq/11 family of G proteins, but the M2 and M4 subtype receptors particularly indicate through Gi/o family of G protein (Haga 2013). The mAChRs play multifunctional peripheral and central roles in human physiology including regulation of muscle contraction, heartbeat, lung, secretion by gland and other functions of the CNS (Wess et al. 2007) (Fig. 13.2).
13.1.1.1 Muscarinic-1 Receptor (M1 Receptor)
Muscarinic-1 receptor (M1 receptor) is a cholinergic muscarinic type of receptor found in humans, rats and mice encoded by the CHRM1 gene (CHRM1 2020). The receptor belongs to the GPCR family and bound to Gq proteins (Qin et al. 2011). This is one of the five muscarinic receptors that act as the metabotropic roles of ACh in the CNS of humans. M1 receptors mostly found in nerve cells of the hippocampus and cerebral cortex. Initiation of the M1 receptor yields many reactions including the activation of ion channels such as Cl−, K+, inhibition of cAMP production and the upregulation of phospholipase C (Sanchez et al. 2009). M1 receptor agonists may also lead to secretion from the bronchoconstriction, stomach and salivary gland. M1 receptors generally participate in many processes including cardiac muscle contraction, control of seizure and cognitive activity (Hamilton et al. 2001; Bakker et al. 2018). The beginning of these receptors by selective agonists reduces harmful β-amyloid secretion and increases the secretion of the non-toxic α-amyloid peptide from amyloid precursor proteins (Jiang et al. 2014).
The M1 receptor is made up of 521 amino acid residues (Fig. 13.3). These are made up of five transmembrane domains: residues 1–239, 403–515, 240–255, 298–402, 256–298, respectively. The M1 muscarinic receptor interacts with the inhibitor tiotropium. Orthosteric and allosteric interaction sites play a significant role in drug specificity. It also reveals how allosteric modulation may be spread involving the two spatially discrete domains (Thal et al. 2016).
13.1.1.2 Muscarinic-2 Receptor (M2 Receptor)
The mAChR M2 is also known as the cholinergic receptor M2, which is encoded by the CHRM2 gene of mice, rats and humans (CHRM2 2020). M2 receptor is a member of the GPCRs family that binds to Gi protein, generally leading to inhibitory effects (Douglas et al. 2001). It regulates the metabotropic function of ACh in the CNS. The receptor is tightly engaged in brain regions, heart and smooth muscle. Initiation of the M2 receptor produces several responses such as initiation of Ca2+, K+ channels and the inhibition of adenylyl cyclase (Harvey and Belevych 2003). M2 receptor also participates in several processes such as regulation of atrial contraction, AV node conduction velocity, acquiring and retention of smooth muscle contraction (Andersson and Olshansky 2007). The receptor antagonist has been suggested useful in the remedy of Alzheimer’s disease (Clader and Wang 2005; Kumar et al. 2016; Wang et al. 2020) (Fig. 13.4).
The receptor is made up of 467 amino acids with 68% helical (24 helices; 322 residues) and 2% beta sheet (4 strands; 13 residues). M2 receptor is devoid of the third intracellular loop and the natural glycosylation sites in the majority of cases. There are ample hydrophobic interactions that occur between receptor proteins within the transmembrane. The ligand QNB in the interior buried pocket specified by the side chains of TM3–TM7 (Haga et al. 2012). A hydrophobic layer formed by three amino acids, viz. Leu 65 in TM2, Leu 114 in TM4 and Ile 392 in TM6. The orthosteric binding pocket is produced by residues that are identical in M1–M5 receptors. All the muscarinic receptors (M1–M5) show common structural homology with other activity distinct acetylcholine interacting proteins from diverse species. M2 receptor structure imparts molecular insights into the contests of creating specific ligands for muscarinic receptors and their predisposition for allosteric control.
13.1.1.3 Muscarinic-3 Receptor (M3 Receptor)
The mAChR M3 is known as acetylcholine/cholinergic receptor M3, which is encoded by the CHRM3 gene of the mouse, rats and humans (CHRM3 2020). M3 receptor is a member of the GPCRs family that binds to Gq protein, which upregulates inositol triphosphate (IP3) and phospholipase C and increases the intracellular Ca2+ (Qin et al. 2011). It acts as the metabotropic role of ACh in the CNS. These receptors are generally found in the lungs, endocrine, exocrine glands, smooth muscle and CNS (Weston et al. 2012). The receptor agonist performs an important function in bronchoconstriction and smooth muscle constriction. Activation of the M3 receptor leads to various secretions from the pancreas, stomach and salivary gland (Gautam et al. 2006). Therefore, the M3 receptor actively participates in many metabolic activities such as regulation of the insulin release and the glucose homeostasis. Additionally, the receptor is a potentially beneficial target site in the case of the pulmonary block and in the progression of colon cancer (Moulton and Fryer 2011; Tolaymat et al. 2019). Moreover, initiation of the M3 receptor by selective agonists may also be useful in the case of type-2 diabetes (Gautam et al. 2006; Ito et al. 2019).
The M3 receptor is made up of 479 amino acid residues having four chains A, B, C, D and two domains (Fig. 13.5). The domain 1 lies from 1–202 to 368–479 range, whereas domain 2 ranges from 203 to 367 amino acid residues. No structure alignment results are available for all the four chains of PDB ID: 4DAJ (A to D) explicitly. Structural conservation comprises of intracellular loops 1 and 2. It also includes extracellular loops 1, 2 and 3, having extremely common resemblance in character; overall folds even though little sequence conservation. The M3 receptor shows distinctive characteristics, having a big extracellular vestibule as part of a lengthened hydrophilic route comprising the orthosteric binding pocket (Kruse et al. 2012). Molecular dynamics simulations study advocates that ligand tiotropium interacts momentarily to an allosteric site on the way to the cavity in the interior of the receptor that possesses suitable properties for binding a ligand. The binding pocket of the receptor may also provide an opportunity to design a novel ligand with enhanced therapeutics for the M3 receptors. The conserved residue (Thr234 of TM 5 and Tyr506 of TM 6) in all muscarinic receptors may perform a significant role in the designing of a novel stimulator for the activation of muscarinic receptors (Wess et al. 1992).
13.1.1.4 Muscarinic 4 Receptor (M4 Receptor)
The mAChR M4 receptor is also known as the cholinergic receptor M4. M4 receptor is present in rats, humans and mice, which is encoded by the CHRM4 gene (CHRM4 2020; Birdsall et al. 2019). This receptor is a participant of the GPCRs family, mostly bind to Gi proteins, leading to inhibitory effects (Douglas et al. 2001). It regulates the metabotropic functions of acetylcholine in the brain. This receptor is tightly involved in the lung and striatum. Activation of the M4 receptor response to several reactions includes the inhibition of adenylyl cyclase (Guo et al. 2010). The function of the M4 receptor is the indirect mediation of dopaminergic neurotransmission through cholinergic activity. M4 receptor is also reported to be involved in neuropathological diseases (Tzavara et al. 2004; Stepnicki et al. 2018).
The M4 receptor is made up of two domains and two chains (A & B). The first domain ranges from residues 1–204 to 326–422 and domain 2 ranges from residues 205 to 325 (Fig. 13.6). An alteration in the rotamer of D112 amino acid transmembrane 3 is conserved all over the biogenic amine G and acts as the counter ion for positively charged neurotransmitters (Van Rhee and Jacobson 1996). This rotameric alteration indicates that D112 of TM3 is beyond ligand tiotropium. The residues Y439 and Y443 play a significant affair to stabilize the various inoperative states of conformation to ligand interact with it. The orthosteric site of the M4 receptor is nearer to the M1 than the M2 subtypes. A deviation in amino acids covering allosteric site stresses the significance of this zone for designing specific drugs (Thal et al. 2016).
13.1.1.5 Muscarinic 5 Receptor (M5 Receptor)
The M5 receptor is encoded by the CHRM5 gene of rats, mouse and human, which is a member of the GPCRs subfamily of the integral membrane protein (CHRM5 2020). The receptor is coupled to Gq protein (Qin et al. 2011). It regulates the metabotropic function of ACh in the CNS. M5 receptor is the most closely occupied in the neurotransmitter containing neuronal cells in the cerebral cortex, striatum, hippocampus along substantia nigra of the brain (Foster et al. 2014). M5 receptor agonists regulate the level of the dopaminergic neuron and release dopamine into the striatum, which facilitates rude substances such as cocaine (Fink-Jensen et al. 2003). The clinical effect of this receptor is not very well-known; however, activation of the M5 receptor is identified which reduces the level of cyclic AMP and the activities of protein kinase C (Bender et al. 2018). M5 receptors may also probably beneficial in the treatment of memory deficits produced by diminished cerebrovascular function (Araya et al. 2006; Vuckovic et al. 2019).
The experimental structure of the M5 receptor is not available till date. M5 receptor participates in various cellular activities such as K+ channel modulation, phosphoinositide degradation and adenylate cyclase inhibition (UniprotID: P08912). All five subtypes (M1–M5) of mAChRs play a significant role in biological processes like renal, cardiac, intestinal function, motor control, cognitive and attention mechanisms. Different functions and diseases associated with these five subtypes along with their locations are given in Table 13.1.
13.2 Anticholinergic Drugs
Anticholinergic drugs are substances which inhibit the action of acetylcholine at the synapse of the PNS and CNS (Xu et al. 2017). It blocks the parasympathetic nerve impulse by non-selectively or selectively linking the neurotransmitter acetylcholine to its receptor site of neurons (Prommer 2013). These drugs are also called parasympatholytics or cholinergic antagonists. Anticholinergics drugs are divided into two main categories based on their specific target to PNS and CNS: antinicotinic drugs and antimuscarinic drugs.
13.2.1 Antinicotinic Drugs
The antinicotinic drugs attack on the nAChRs. The majority of antinicotinic drugs are non-depolarizing and depolarizing drivers. Non-depolarizing agents such as vecuronium, rocuronium, pancuronium, cisatracurium, atracurium and mivacurium are a type of neuromuscular blocker, which does not depolarize the motor end plate and causing action potential (Kim et al. 2017). Depolarizing agents such as succinylcholine, decamethonium, and others are a type of neuromuscular blocker which depolarize the motor end plate and produce an action potential (Ahmad et al. 2018). Both agents are used in muscle relaxants for clinical purposes (Clar and Liu 2020; Gulenay and Mathai 2020).
13.2.2 Antimuscarinic Drugs
Antimuscarinic drugs act on the mAChRs. Muscarinic antagonists (muscarinic anticholinergic drugs) disrupt the learning and memory processes (Table 13.2). These drugs are involved in causing cognitive and memory deficits in an experimental animal model for the pathological conditions identified in several human neuropathological diseases such as Alzheimer’s, Schizophrenia and other diseases (Robinson et al. 2011). Majority of anticholinergic drugs have been used in a wide range of clinical conditions like amnesia, mydriasis, bronchodilation and sedation (Prommer 2013).
13.3 Sources of Antimuscarinic Drugs
The most common sources of anticholinergic drugs are (1) Datura species (Datura 2016), (2) Atropabelladonna (Ulbricht et al. 2004; Belladonna 2020), (3) Hyoscyamusniger (Roberts and Wink 1999), (4) Brugmansia species (toxic plants 2020), (5) Garrya species (Nesom 2012) (6) and Mandragora officinarum (Duke 2002) plants.
13.4 Classification of Antimuscarinic Drugs
13.4.1 Based on Their Sources
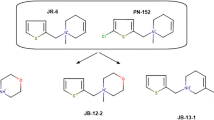
Antimuscarinic drugs are classified into three groups (Fig. 13.7): (1) natural alkaloids, (2) semi-synthetic drugs and (3) synthetic drugs.
13.4.1.1 Natural Alkaloids
Natural alkaloids are mostly natural organic compounds, which usually consist of a basic nitrogen atom. It also includes some correlated compounds with both neutral and weak acidic in nature (IUPAC 2012; Sheela 2013). Some alkaloids are synthetic or semisynthetic compounds of dissimilar or similar structures like natural alkaloids. Alkaloids have various important physiological roles in humans and animals (Lahlou 2014). Natural alkaloids such as scopolamine, atropine and tubocurarine are well known and may be toxic to the animal. They exhibit a broad range of pharmacological and biological properties (Yadav et al. 2014).
13.4.1.2 Semi-Synthetic Drugs
Semi-synthetic drugs are produced by the biochemical reaction between naturally occurring compounds to form a new product (Lahlou 2014). Semi-synthesis, a kind of biochemical synthesis, which uses chemical compound extracted from a natural source (plant material or microbial cell cultures) as the initial materials to yield other innovative compounds (Cragg and Newman 2013). These drugs are neither synthetic nor natural completely, which is a mixture of both. Semi-synthetic drugs are structurally related to atropine including tertiary ammonium compound (homatropine, biperiden, etc.), quaternary ammonium compound (homatropine methyl bromide, atropine methonitrate, etc.) and novel antibiotics (tetracycline, doxycycline, tigecycline and chemotherapy drug) which exhibit a wide variety of chemical and pharmacological properties (Lahlou 2014; Nelson and Levy 2011; Liu and Myers 2016).
13.4.1.3 Synthetic Drugs
The synthetic drug is a drug having similar properties and belongings to hallucinogen or narcotic drugs (Garcia-Romeu et al. 2016). These drugs are structurally dissimilar to atropine including tertiary amines (pirenzepine, dicyclomine, oxybutynin, etc.) and quaternary amine (propantheline, glycopyrrolate, trihexyphenidyl, etc.) which exhibits a wide variety of biological, physicochemical and pharmacological properties (Grynkiewicz and Gadzikowska 2008). Synthetic drugs are prepared from the beginning substance, which is not present in the environment; instead, they are formed from building blocks of a chemical substance (Lahlou 2014). The common process of synthetic drug discovery is analogous to the discovery of natural drugs (Mathur and Hoskins 2017). In the natural drugs discovery, the compounds are obtained from sources like the plant, animal and microorganism. In the case of synthetic drug discovery, the compound generally produces in vitro laboratory through combinatorial technique, which manufactured a hundred to million molecules from the building block of smaller chemical substances (Valecha et al. 2010).
13.4.2 Based on Their Mode of Action
Antimuscarinic drugs are classified into two groups (Fig. 13.8): (1) nonselective muscarinic receptor antagonist and (2) selective muscarinic receptor antagonist.
13.4.2.1 Nonselective Muscarinic Receptor Antagonist
The nonselective muscarinic antagonist is a drug, which is not selective for all subtypes of the muscarinic receptors on therapeutic doses (Svoboda et al. 2017). Most of the anticholinergic drugs such as scopolamine, atropine and homatropine are nonselective for the subtypes M1–M5 receptors. However, these drugs are specific to the muscarinic receptor (Svoboda et al. 2017). A nonselective muscarinic drug is used as a medication for clinical events like obstruction of muscle contraction, salivary secretion and cardio-protection; conversely, their beneficial function in the treatment of long standing is known (Chapple et al. 2002). Ipratropium and oxitropium are also nonselective antimuscarinic drugs that successfully retract airway hyperactivity and bronchoconstriction in humans (Coulson and Fryer 2003).
13.4.2.2 Selective Muscarinic Receptor Antagonists
The muscarinic receptor is well-defined by selective agonists and antagonists. A selective muscarinic receptor grouping preceded the identification of acetylcholine (Schiechl et al. 2008). Telenzepine and pirenzepine antagonists have a comparatively strong binding affinity for the M1 receptor, which permitted for use in the therapy of peptic ulcer disease (Okabe et al. 2002). Conversely, M2 receptor antagonist includes Otenzepad peripherally acting in the remedy of bradycardia (Lanzafame et al. 2001). Darifenacin inhibitor is applied in the remedy of irritable bowel syndrome, urinary incontinence and is a specific M3 receptor (McFerren and Gomelsky 2015). Biperiden, a comparative specific M1 receptor antagonist, therapeutically applied to reduce the symptoms of Parkinson’s disease, memory and learning deficit in Alzheimer’s disease (Witkin et al. 2014).
A recent study was done in the chick model of myopia, which proved that the best selective M4 receptor antagonist himbacine is the most effective drug in the regulation of myopia (Carr et al. 2019; Cottriall et al. 2001). However, the M5 receptor has least worked out due to the absence of selective ligand subtypes of mAChRs. After the detection, characterization and synthesis of the first highly muscarinic and specific M5 orthosteric inhibitor, ML381 or VU0480131 have been reported (Gentry et al. 2014).
13.5 Mechanism of Antimuscarinic Drugs
The antimuscarinic drugs including atropine, scopolamine and others are more liposoluble because of their lipophilic nature, which act rapidly and are being absorbed from the gastrointestinal tract (GIT). However, it is less absorbed from injured or intact skin and easier to cross the blood–brain barrier (BBB), which upset the CNS and other organ systems (Rajput 2013; He et al. 2011). Most of the antimuscarinic drugs are usually observed to be safe taking at dose level 1.5 mg/day (Beyer et al. 2009; Ulbricht et al. 2004). Toxicity usually occurs after the ingestion of drugs at a dose level more than 1.5 mg/day in the brain, which caused unclear vision, delirium, incomprehensive speech, fatigue and unconsciousness (Milanlioglu 2011; Apfel et al. 2010; Bogan et al. 2009).
Antimuscarinic drugs competitively bind and inhibit acetylcholine from the binding site of the muscarinic receptors (Pergolizzi et al. 2012). However, their antagonistic actions may be decreased by elevating the concentration of the muscarinic agonists. The main action of antimuscarinic drugs like scopolamine, atropine and associated drugs competitively blocks the action of ACh agonists (Fig. 13.9). These drugs compete with such agonists for normal requisite on the muscarinic receptor. Many evidences support the idea that scopolamine- and atropine-related compounds compete with agonists for normal requisite on the muscarinic receptors (Snyder et al. 2005; Malik et al. 2015).
13.5.1 Epidemiology of Anticholinergic Drug
The epidemiological study suggests that about 20–50% of individuals of old age are regularly put in danger to anticholinergic drugs with possible activity (Fox et al. 2011). This shows that more than one half of the drug usually given for grown-up people is possible due to anticholinergic action (Chew et al. 2008). Anticholinergic agent’s actions in adult individuals differ with sex, age and comorbidities (Wawruch et al. 2012; Chatterjee et al. 2010; Agar et al. 2009).
13.5.2 Clinical Significance of Anticholinergic Drugs
Anticholinergic drugs with potential properties have been significantly used in medicine for many years to treat disease conditions including the following: (1) motion sickness, (2) Parkinson’s disease, (3) overactive bladder and urinary incontinence, (4) psychiatric disorders, (5) gastrointestinal disorders, (6) diarrhoea, (7) asthma, (8) chronic obstructive pulmonary disease (COPD), (9) surgery and anaesthesia for muscle relaxation, (10) anaesthesia during surgery, (11) insomnia, (12) Alzheimer’s disease and (13) toxicity of certain poisonings (Cahalan et al. 2009; Kees et al. 2015).
13.5.3 Side Effects of Anticholinergic Drugs
Different studies have indicated the side effects of anticholinergic drugs on different organ systems of the human body. The highly significant side effects of anticholinergic drugs are mentioned in Table 13.3.
13.6 Conclusions
The muscarinic receptor can be distinguished structurally, physiologically and pharmacologically. The muscarinic receptor is a family of GPCRs and commonly distributed in the human body. Each subtype performs a specific function and plays a significant biological activity in the PNS and CNS. Muscarinic receptor antagonists competitively inhibit postganglionic muscarinic receptor which regulates several essential functions and structures of the PNS and CNS. Thus, antagonistic activity of antimuscarinic drug acts as a target in correlation with muscarinic acetylcholine receptor subtypes in animal and is associated with human health risk.
Change history
29 July 2020
The book was inadvertently published with an incorrect affiliation of the authors Ram Naraian and Manish Kumar Gupta in Chapter 13 as Department of Biochemistry, Veer Bahadur Singh Purvanchal University, Jaunpur, Uttar Pradesh, India. The affiliation has been corrected as Department of Biotechnology, Veer Bahadur Singh Purvanchal University, Jaunpur, Uttar Pradesh, India.
References
Agar M, Currow D, Plummer J, Seidel R, Carnahan R, Abernethy AP (2009) Changes in anticholinergic load from regular prescribed medications in palliative care as death approaches. Palliat Med 36(3):257–265
Agrawal RV, Murthy S, Sangwan V, Biswas J (2010) Current approach in diagnosis and management of anterior uveitis. Indian J Ophthalmol 58(1):11–19
Ahmad M, Khan NA, Furqan A (2018) Comparing the functional outcome of different dose regimes of succinylcholine. When used for rapid induction and intubation. J Ayub Med Coll Abbottabad 30(3):401–404
Albuquerque EX, Pereira EFR, Alkondon M, Rogers SW (2009) Mammalian nicotinic acetylcholine receptors: from structure to function. Physiol Rev 89:73–120
Andersson KE, Olshansky B (2007) Treating patients with overactive bladder syndrome with antimuscarinics: heart rate considerations. BJU Int 100(5):1007–1014
Apfel CC, Zhang K, George E, Shi S, Jalota L, Hornuss C, Fero KE, Heidrich F, Pergolizzi JV, Cakmakkaya OS, Kranke P (2010) Transdermal scopolamine for the prevention of postoperative nausea and vomiting: asystematic review and meta-analysis. Clin Ther 32:1987–2002
Araya R, Noguchi T, Yuhki M, Kitamura N, Higuchi M, Saido TC, Seki K, Itohara S, Kawano M, Tanemura K, Takashima A, Yamada K, Kondoh Y, Kanno I, Wess J, Yamada M (2006) Loss of M5 muscarinic acetylcholine receptors leads to cerebrovascular and neuronal abnormalities and cognitive deficits in mice. Neurobiol Dis 24(2):334–344
Bakker G, Vingerhoets C, Boucherie D, Caan M, Bloemen O, Eersels J, Booij J, van Amelsvoort T (2018) Relationship between muscarinic M1 receptor binding and cognition in medication-free subjects with psychosis. Neuroimage Clin 18:713–719
Belladonna (2020) MedlinePlus, US national library of medicine. https://medlineplus.gov/druginfo/natural/531.html. Accessed Mar 2020
Bender AM, Cho HP, Nance KD, Lingenfelter KS, Luscombe VB, Gentry PR, Voigtritter K, Berizzi AE, Sexton PM, Langmead CJ, Christopoulos A, Locuson CW, Bridges TM, Chang S, O’Neill JC, Zhan X, Niswender CM, Jones CK, Conn PJ, Lindsley CW (2018) Discovery and optimization of potent and CNS penetrant M5-preferring positive allosteric modulators derived from a novel, chiral N-(Indanyl) piperidine amide scaffold. ACS Chem Neurosci 9(7):1572–1581
Berdai MA, Labib S, Chetouani K, Harandou M (2012) Atropa belladonna intoxication: a case report. Pan Afr Med J 11:72
Beyer J, Drummer OH, Maurer HH (2009) Analysis of toxic alkaloids in body samples. Forensic Sci Int 185:1–9
Birdsall NJM, Bradley S, Brown DA, Buckley NJ, Challiss RJ, Christopoulos A, Eglen RM, Ehlert F, Felder CC, Hammer R, Kilbinger HJ, Lambrecht G, Langmead C, Mitchelson F, Mutschler E, Nathanson NM, Schwarz RD, Tobin AB, Valant C, Wess J. (2019) Acetylcholine receptors (muscarinic) (version 2019.4) in the IUPHAR/BPS Guide to pharmacology database. IUPHAR/BPS Guide to pharmacology CITE, 2019(4). http://journals.ed.ac.uk/gtopdb-cite/article/view/3156
Bogan R, Zimmermann T, Zilker T, Eyer F, Thiermann H (2009) Plasma level of atropine after accidental ingestion of Atropa belladonna. Clin Toxicol 47:602–604
Cahalan MD, Barash PG, Cullen BF, Stoelting RK (2009) Clinical anesthesia. Lippincott Williams & Wilkins, Hagerstwon MD
Carr BJ, Nguyen CT, Stell WK (2019) Alpha2-adrenoceptor agonists inhibit form-deprivation myopia in the chick. Clin Exp Optom 102(4):418–425
Cetinel B, Onal B (2013) Rationale for the use of anticholinergic agents in overactive bladder with regard to central nervous system and cardiovascular system side effects. Korean J Urol 54(12):806–815
Chapple CR, Yamanishi T, Chess-Williams R (2002) Muscarinic receptor subtypes and management of the overactive bladder. Urology 60(5):82–88
Chatterjee S, Mehta S, Sherer JT, Aparasu RR (2010) Prevalence and predictors of anticholinergic medication use in elderly nursing home residents with dementia: analysis of data from the 2004 national nursing home survey. Drugs Aging 27(12):987–997
Chew ML, Mulsant BH, Pollock BG, Lehman ME, Greenspan A, Mahmoud RA, Kirshner MA, Sorisio DA, Bies RR, Gharabawi G (2008) Anticholinergic activity of 107 medications commonly used by older adults. J Am Geriatr Soc 56(7):1333–1341
Cheyne L, Irvin-Sellers MJ, White J (2013) Tiotropium versus ipratropium bromide for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 9(9):CD009552
CHRM1 (2020) Cholinergic receptor muscarinic 1 (Gene ID: 1128). https://www.ncbi.nlm.nih.gov/gene/1128. Accessed Mar 2020
CHRM2 (2020) Cholinergic receptor muscarinic 2 (Gene ID: 1129). https://www.ncbi.nlm.nih.gov/gene/1129. Accessed Mar 2020
CHRM3 (2020) Cholinergic receptor muscarinic 3 (Gene ID: 1131). https://www.ncbi.nlm.nih.gov/gene/1131. Accessed Mar 2020
CHRM4 (2020) Cholinergic receptor muscarinic 4 (Gene ID: 1132). https://www.ncbi.nlm.nih.gov/gene/1132. Accessed Mar 2019
CHRM5 (2020) Cholinergic receptor muscarinic 5 (Gene ID: 1133). https://www.ncbi.nlm.nih.gov/gene/1133. Accessed Mar 2020
Clader JW, Wang Y (2005) Muscarinic receptor agonists and antagonists in the treatment of Alzheimer’s disease. Curr Pharm Des 11(26):3353–3361
Clar DT, Liu M (2020) Non-depolarizing neuromuscular blockers. Stat Pearls Publishing, Treasure Island
Corradi J, Bouzat C (2016) Understanding the bases of function and modulation of a7 nicotinic receptors: implications for drug discovery. Mol Pharmacol 90:288–299
Cottriall CL, Truong HT, McBrien NA (2001) Inhibition of myopia development in chicks using himbacine: a role for M4 receptors. Neuroreport 12:2453–2456
Coulson FR, Fryer AD (2003) Muscarinic acetylcholine receptors and airway diseases. Pharmacol Ther 98(1):59–69
Cragg GM, Newman DJ (2013) Natural products: a continuing source of novel drug leads. Biochim Biophys Acta 1830:3670–3695
Datura (2016) Datura metel. plants.ces.ncsu.edu
De Caen AR, Berg MD, Chameides L et al (2015) Part 12: pediatric advanced life support: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 132(18):S526–S542
De Maagd GA, Davenport TC (2012) Management of urinary incontinence. P T 37(6):345–361
Douglas CL, Baghdoyan HA, Lydic R (2001) M2 muscarinic autoreceptors modulate acetylcholine release in prefrontal cortex of C57BL/6J mouse. J Pharmacol Exp Ther 299(3):960–966
Duke JA (2002) Handbook of medicinal herbs, 2nd edn. CRC Press, Boca Raton
Eglen RM (2006) Muscarinic receptor subtypes in neuronal and non-neuronal cholinergic function. Auton Autacoid Pharmacol 26(3):219–233
Fink-Jensen A, Fedorova I, Wortwein G, Woldbye DP, Rasmussen T, Thomsen M, Bolwig TG, Knitowski KM, McKinzie DL, Yamada M, Wess J, Basile A (2003) Role for M5 muscarinic acetylcholine receptors in cocaine addiction. J Neurosci Res 74(1):91–96
Foster DJ, Gentry PR, Lizardi-Ortiz JE, Bridges TM, Wood MR, Niswender CM, Sulzer D, Lindsley CW, Xiang Z, Conn PJ (2014) M5 receptor activation produces opposing physiological outcomes in dopamine neurons depending on the receptor's location. J Neurosci 34(9):3253–3262
Fox C, Richardson K, Maidment ID, Savva GM, Matthews FE, Smithard D, Coulton S, Katona C, Boustani MA, Brayne C (2011) Anticholinergic medication use and cognitive impairment in the older population: the medical research council cognitive function and ageing study. J Am Geriatr Soc 59(8):1477–1483
Fredriksson R, Lagerstrom MC, Lundin LG, Schioth HB (2003) The G-protein-coupled receptors in the human genome form five main families. Phylogenetic analysis, paralogon groups, and fingerprints. Mol Pharmacol 63:1256–1272
Garcia-Romeu A, Kersgaard B, Addy PH (2016) Clinical applications of hallucinogens: a review. Exp Clin Psychopharmacol 24(4):229–268
Gautam D, Han SJ, Hamdan FF, Jeon J, Li B, Li JH, Cui Y, Mears D, Lu H, Deng C, Heard T, Wess J (2006) A critical role for (beta cell) M3 muscarinic acetylcholine receptors in regulating insulin release and blood glucose homeostasis in vivo. Cell Metab 3(6):449–461
Gentry PR, Kokubo M, Bridges TM, Cho HP, Smith E, Chase P, Hodder PS, Utley TJ, Rajapakse A, Byers F, Niswender CM, Morrison RD, Daniels JS, Wood MR, Conn PJ, Lindsley CW (2014) Discovery, synthesis and characterization of a highly mAChR selective M5 orthosteric antagonist, VU0488130 (ML381): a novel molecular probe. ChemMedChem 9(8):1677–1682
Grynkiewicz G, Gadzikowska M (2008) Tropane alkaloids as medicinally useful natural products and their synthetic derivatives as new drugs. Pharmacol Rep 60(4):439–463
Gulenay M, Mathai JK (2020) Depolarizing neuromuscular blocking drugs. Stat Pearls Publishing, Treasure Island
Guo ML, Mao LM, Wang JQ (2010) Modulation of M4 muscarinic acetylcholine receptors by interacting proteins. Neurosci Bull 26(6):469–473
Haga T (2013) Molecular properties of muscarinic acetylcholine receptors. Proc Jpn Acad Ser B Phys Biol Sci 89(6):226–256
Haga K, Kruse AC, Asada H, Yurugi-Kobayashi T, Shiroishi M, Zhang C, Weis WI, Okada T, Kobilka BK, Haga T, Kobayashi T (2012) Structure of the human M2 muscarinic acetylcholine receptor bound to an antagonist. Nature 482(7386):547–551
Hamilton SE, Hardouin SN, Anagnostaras SG, Murphy GG, Richmond KN, Silva AJ, Feigl EO, Nathanson NM (2001) Alteration of cardiovascular and neuronal function in M1 knockout mice. Life Sci 68(22–23):2489–2493
Harvey RD, Belevych AE (2003) Muscarinic regulation of cardiac ion channels. Br J Pharmacol 139:1074–1084
Harvey AR, Baker LB, Reddihough DS, Scheinberg A, Williams K (2018) Trihexyphenidyl for dystonia in cerebral palsy. Cochrane Database Syst Rev 5:CD012430
He Y, Luo J, Kong L (2011) Preparative separation of atropine and scopolamine from Daturae metelis Flos using pH-zone-refining counter-current chromatography with counter-rotation and dual-mode elution procedure. J Sep Sci 34(7):806–811
Ito Y, Kaji M, Sakamoto E, Terauchi Y (2019) The beneficial effects of a muscarinic agonist on pancreatic β-cells. Sci Rep 9(1):16180
IUPAC (2012) Compendium of chemical terminology. Gold book. https://goldbook.iupac.org/. Accessed Mar 2020
Ivanovic SR, Dimitrijevic B, Cupic V, Jezdimirovic M, Borozan S, Savic M, Savic D (2016) Downregulation of nicotinic and muscarinic receptor function in rats after subchronic exposure to diazinon. Toxicol Rep 3:523–530
Jiang S, Li Y, Zhang C, Zhao Y, Bu G, Xu H, Zhang YW (2014) M1 muscarinic acetylcholine receptor in Alzheimer's disease. Neurosci Bull 30(2):295–307
Jo WS, Hossain MA, Park SC (2014) Toxicological profiles of poisonous, edible, and medicinal mushrooms. Mycobiology 42(3):215–220
Katzung B, Trevor A (2014) Basic and clinical pharmacology. McGraw-Hill Education, New York
Kees M, Beckel N, Sharp C (2015) Successful treatment of Solanum dulcamara intoxication in a Labrador retriever puppy. Can Vet J 56(12):1283–1286
Kim YB, Sung TY, Yang HS (2017) Factors that affect the onset of action of non-depolarizing neuromuscular blocking agents. Korean J Anesthesiol 70(5):500–510
Kobayashi F, Yageta Y, Segawa M, Matsuzawa S (2007) Effects of imidafenacin (KRP-197/ONO-8025), a new anti-cholinergic agent, on muscarinic acetylcholine receptors. High affinities for M3 and M1 receptor subtypes and selectivity for urinary bladder over salivary gland. Arzneimittelforschung 57(2):92–100
Kruse AC, Hu J, Pan AC, Arlow DH, Rosenbaum DM, Rosemond E, Green HF, Liu T, Chae PS, Dror RO, Shaw DE, Weis WI, Wess J, Kobilka BK (2012) Structure and dynamics of the M3 muscarinic acetylcholine receptor. Nature 482(7386):552–556
Kumar A, Nisha CM, Silakari C, Sharma I, Anusha K, Gupta N, Nair P, Tripathi T, Kumar A (2016) Current and novel therapeutic molecules and targets in Alzheimer’s disease. J Formos Med Assoc 115(1):3–10
Lahlou M (2014) The success of natural products in drug discovery. PP 4(3):17–31
Langmead CJ, Watson J, Reavill C (2008) Muscarinic acetylcholine receptors as CNS drug targets. Pharmacol Ther 117:232–243
Lanzafame A, Christopoulos A, Mitchelson F (2001) The allosteric interaction of otenzepad (AF-DX 116) at muscarinic M2 receptors in guinea pig atria. Eur J Pharmacol 416(3):235–244
Le T, Bhushan V (2014) First aid for the USMLE step 1. McGraw-Hill Education, New York
Lebois EP, Thorn C, Edgerton JR, Popiolek M, Xi S (2018) Muscarinic receptor subtype distribution in the central nervous system and relevance to aging and Alzheimer’s disease. Neuropharmacology 136:362–373
Lee JH, Francis PT, Ballard CG, Aarsland D, Kalaria RN, Wong PT, Chen CP, Lai MK (2016) Muscarinic M1 receptor coupling to g-protein is intact in Parkinson's disease dementia. J Parkinsons Dis 6(4):733–739
Lieberman JA (2004) Managing anticholinergic side effects. Prim Care Companion J Clin Psychiatry 6(2):20–10
Liu F, Myers AG (2016) Development of a platform for the discovery and practical synthesis of new tetracycline antibiotics. Curr Opin Chem Biol 32:48–57
Macdiarmid SA (2008) Concomitant medications and possible side effects of antimuscarinic agents. Rev Urol 10(2):92–98
Malca Garcia GR, Hennig L, Shelukhina IV, Kudryavtsev DS, Bussmann RW, Tsetlin VI, Giannis A (2015) Curare alkaloids: constituents of a Matis dart poison. J Nat Prod 78:2537–2544
Malik M, Rangel-Barajas C, Sumien N, Su C, Singh M, Chen Z, Huang RQ, Meunier J, Maurice T, Mach RH, Luedtke RR (2015) The effects of sigma (σ1) receptor-selective ligands on muscarinic receptor antagonist-induced cognitive deficits in mice. Br J Pharmacol 172(10):2519–2531
Mathur S, Hoskins C (2017) Drug development: Lessons from nature. Biomed Rep 6(6):612–614
McEvoy GK (2003) Benztropine mesylate: AHFS drug information. American Society of Health-System Pharmacists, Bethesda MD, pp 1185–1186
McEvoy GK (2005) Scopolamine: AHFS drug information. American Society of Health-System Pharmacists, Bethesda MD, pp 1254–1257
McEvoy GK (2018) Atropine: AHFS drug information. American Society of Health-System Pharmacists, Bethesda MD
McFerren SC, Gomelsky A (2015) Treatment of overactive bladder in the elderly female: the case for trospium, oxybutynin, fesoterodine and darifenacin. Drugs Aging 32(10):809–819
Milanlioglu A (2011) Toxic encephalopathy after Atropa belladonna poisoning/Milanlioglu/Pakistan. Pak J Med Sci 27:26–928
Mintzer J, Burns A (2000) Anticholinergic side-effects of drugs in elderly people. J R Soc Med 93(9):457–462
Moulton BC, Fryer AD (2011) Muscarinic receptor antagonists, from folklore to pharmacology; finding drugs that actually work in asthma and COPD. Br J Pharmacol 163(1):44–52
Muise ED, Gandotra N, Tackett JJ, Bamdad MC, Cowles RA (2017) Distribution of muscarinic acetylcholine receptor subtypes in the murine small intestine. Life Sci 169:6–10
Nelson ML, Levy SB (2011) The history of the tetracyclines. Ann N Y Acad Sci 1241:17–32
Nesom GL (2012) Notes on the Garrya ovata (Garryaceae) complex. Phyton 97:1–6
Okabe S, Shimosako K, Amagase K (2002) Pharmacological control of gastric acid secretion for the treatment of acid-related peptic disease: past, present, and future. J Physiol Pharmacol 52(4):639–656
Pergolizzi JV, Philip BK, Leslie JB, Taylor R, Raffa RB (2012) Perspectives on transdermal scopolamine for the treatment of postoperative nausea and vomiting. J Clin Anesth 24:334–345
Prado VF, Janickova H, Al-Onaizi MA, Prado MAM (2017) Cholinergic circuits in cognitive flexibility. Neuroscience 345:130–141
Prommer E (2013) Anticholinergics in palliative medicine: an update. Am J Hosp Palliat Care 30(5):490–498
Qin K, Dong C, Wu G, Lambert NA (2011) Inactive-state preassembly of Gq- coupled receptors and Gq heterotrimers. Nat Chem Biol 7(10):740–747
Rajput H (2013) Effects of atropa belladonna as an anti-cholinergic. Nat Prod Chem Res 1:104. https://doi.org/10.4172/2329-6836.1000104
Ramnarine M (2020) Anticholinergic toxicity. https://emedicine.medscape.com/article/812644-overview. Accessed Mar 2020
Rang HP (2003) Pharmacology, 5th edn. Churchill Livingstone, Edinburgh
Roberts MF, Wink M (1999) Alkaloids: biochemistry, ecology and medicinal applications. J Nat Prod 62(4):662–664
Robinson L, Platt B, Riedel G (2011) Involvement of the cholinergic system in conditioning and perceptual memory. Behav Brain Res 221:443–465
Sanchez G, Colettis N, Vazquez P, Cervenansky C, Aguirre A, Quillfeldt JA, Jerusalinsky D, Kornisiuk E (2009) Muscarinic inhibition of hippocampal and striatal adenylyl cyclase is mainly due to the M(4) receptor. Neurochem Res 34(8):1363–1371
Saternos HC, Almarghalani DA, Gibson HM, Meqdad MA, Antypas RB, Lingireddy A, AbouAlaiwi WA (2018) Distribution and function of the muscarinic receptor subtypes in the cardiovascular system. Physiol Genomics 50(1):1–9
Schiechl G, Himmelsbach M, Buchberger W, Kerschbaum HH, Lutz-Meindl U (2008) Identification of acetylcholine and impact of cholinomimetic drugs on cell differentiation and growth in the unicellular green alga Micrasterias denticulate. Plant Sci 175(3):262–266
Sheela JRH (2013) Qualitative analysis of secondary metabolites of the plant clematis gouriana. Int J Innov Res Sci Eng Technol 2(6):2356–2358
Snyder PJ, Bednar MM, Cromer JR, Maruff P (2005) Reversal of scopolamine-induced deficits with a single dose of donepezil, an acetylcholinesterase inhibitor. Alzheimers Dement 1(2):126–135
Stepnicki P, Kondej M, Kaczor AA (2018) Current concepts and treatments of schizophrenia. Molecules 23(8):2087
Svoboda J, Popelikova A, Stuchlik A (2017) Drugs interfering with muscarinic acetylcholine receptors and their effects on place navigation. Front Psych 8:215
Thal DM, Sun B, Feng D, Nawaratne V, Leach K, Felder CC, Bures MG, Evans DA, Weis WI, Bachhawat P, Kobilka TS, Sexton PM, Kobilka BK, Christopoulos A (2016) Crystal structures of the M1 and M4 muscarinic acetylcholine receptors. Nature 531(7594):335–340
Tolaymat M, Larabee SM, Hu S, Xie G, Raufman JP (2019) The role of M3 muscarinic receptor ligand-induced kinase signaling in colon cancer progression. Cancers 11:308
Toxic plants (2020) Safe and poisonous garden plants. University of California. https://ucanr.edu/sites/poisonous_safe_plants/Toxic_Plants_by_common_Name_659/. Accessed Mar 2020
Tytgat GN (2007) Hyoscine butylbromide: a review of its use in the treatment of abdominal cramping and pain. Drugs 67(9):1343–1357
Tzavara ET, Bymaster FP, Davis RJ, Wade MR, Perry KW, Wess J, McKinzie DL, Felder C, Nomikos GG (2004) M4 muscarinic receptors regulate the dynamics of cholinergic and dopaminergic neurotransmission: relevance to the pathophysiology and treatment of related CNS pathologies. FASEB J 18(12):1410–1412
Ulbricht C, Basch E, Hammerness P, Vora M, Wylie J Jr, Woods J (2004) An evidence-based systematic review of belladonna by the natural standard research collaboration. J Herb Pharmacother 4(4):61–90
Valecha N, Looareesuwan S, Martensson A, Abdulla SM, Krudsood S, Tangpukdee N, Mohanty S, Mishra SK, Tyagi PK, Sharma SK, Moehrle J, Gautam A, Roy A, Paliwal JK, Kothari M, Saha N, Dash AP, Bjorkman A (2010) Arterolane, a new synthetic trioxolane for treatment of uncomplicated Plasmodium falciparum malaria: a phase II, multicentre, randomized, dose-finding clinical trial. Clin Infect Dis 51(6):684–691
Van Rhee AM, Jacobson KA (1996) Molecular architecture of G protein-coupled receptors. Drug Dev Res 37:1–38
Verma S, Kumar A, Tripathi T, Kumar A (2018) Muscarinic and nicotinic acetylcholine receptor agonists: current scenario in Alzheimer's disease therapy. J Pharm Pharmacol 70(8):985–993
Vuckovic Z, Gentry PR, Berizzi AE, Hirata K, Varghese S, Thompson G, van der Westhuizen ET, Burger WAC, Rahmani R, Valant C, Langmead CJ, Lindsley CW, Baell JB, Tobin AB, Sexton PM, Christopoulos A, Thal DM (2019) Crystal structure of the M5 muscarinic acetylcholine receptor. Proc Natl Acad Sci U S A 116(51):26001–26007
Wang H, Peng G, Wang B, Yin H, Fang X, He F, Zhao D, Liu Q, Shi L (2020) IL-1R−/− alleviates cognitive deficits through microglial M2 polarization in AD mice. Brain Res Bull 157:10–17
Wawruch M, Macugova A, Kostkova L, Luha J, Dukat A, Murin J, Drobna V, Wilton L, Kuzelova M (2012) The use of medications with anticholinergic properties and risk factors for their use in hospitalised elderly patients. Pharmacoepidemiol Drug Saf 21(2):170–176
Wess J, Maggio R, Palmer JR, Vogel Z (1992) Role of conserved threonine and tyrosine residues in acetylcholine binding and muscarinic receptor activation. A study with m3 muscarinic receptor point mutants. J Biol Chem 267(27):19313–19319
Wess J, Eglen RM, Gautam D (2007) Muscarinic acetylcholine receptors: mutant mice provide new insights for drug development. Nat Rev Drug Discov 6:721–733
Weston GK, Huang XF, Lian J, Deng C (2012) Effects of olanzapine on muscarinic M3 receptor binding density in the brain relates to weight gain, plasma insulin and metabolic hormone levels. Eur Neuropsychopharmacol 22(5):364–373
Witkin JM, Overshiner C, Li X, Catlow JT, Wishart GN, Schober DA et al (2014) M1 and M2 muscarinic receptor subtypes regulate antidepressant-like effects of the rapidly acting antidepressant scopolamine. J Pharmacol Exp Ther 351:448–456
Xu D, Anderson HD, Tao A, Hannah KL, Linnebur SA, Valuck RJ, Culbertson VL (2017) Assessing and predicting drug-induced anticholinergic risks: an integrated computational approach. Ther Adv Drug Saf 8(11):361–370
Yadav KN, Kadam PV, Patel JA, Patil MJ (2014) Strychnos Potatorum: phytochemical and pharmacological review. Pharmacogn Rev 8(15):61–66
Yazdani N, Sadeghi R, Momeni-Moghaddam H, Zarifmahmoudi L, Ehsaei A (2018) Comparison of cyclopentolate versus tropicamidecycloplegia: a systematic review and meta-analysis. J Optom 11(3):135–143
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Singh, P.K., Nath, R., Naraian, R., Gupta, M.K. (2020). Structural and Functional Aspects of Muscarinic Receptors in Correlation with Anticholinergic Drugs. In: Singh, D., Tripathi, T. (eds) Frontiers in Protein Structure, Function, and Dynamics. Springer, Singapore. https://doi.org/10.1007/978-981-15-5530-5_13
Download citation
DOI: https://doi.org/10.1007/978-981-15-5530-5_13
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-5529-9
Online ISBN: 978-981-15-5530-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)