Abstract
Recurrent miscarriage (RM) is an important issue in the field of reproductive medicine. It has been estimated that it affects 2–5% of the women trying to conceive. From a clinical perspective, few cases of RM are caused by a single cause; most of them may in fact have a multifactorial background which involves the interaction of multiple genetic and environmental parameters. Indeed, if the fertility rate decreases as the woman ages, the miscarriage rate follows an opposite trend. RM is one of the suggested indications to preimplantation genetic testing for aneuploidies (PGT-A). PGT-A is a comprehensive chromosome testing approach aimed at identifying chromosomally normal embryos within a cohort of blastocysts produced by a couple during an IVF treatment. This embryo selection strategy prevents aneuploid blastocysts from being transferred, thus reducing both the risk for implantation failure per transfer and miscarriage due to chromosomal impairments. However, some limitations to PGT exist, data about its clinical efficacy per intention to treat and cost-effectiveness are yet missing, and a clear international consensus has not been reached yet.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Preimplantation genetic testing for aneuploidies
- PGS
- Recurrent miscarriage
- Euploid embryo
- Chromosome aneuploidies
- Maternal age
1 Introduction
Human reproduction is a very inefficient process. The possibility of conceiving per menstrual cycle is as low as 20% [1]. Furthermore, early pregnancy loss, also referred to as miscarriage or spontaneous abortion, is defined as the loss of a clinical pregnancy before 20 weeks of gestation or, if the gestational age is unknown, the loss of an embryo/fetus of <400 g [2].
Recurrent miscarriage (RM) is an important issue in the field of reproductive medicine. It has been estimated it affects 2–5% of the women attempting to conceive, and about 1% of women may go through three or more miscarriages in their reproductive lifespan [1]. The definition of RM has long been debated and is different among the international societies. According to the European Society for Human Reproduction and Embryology (ESHRE) [3, 4], RM is defined as three consecutive pregnancy losses, including the non-visualized ones. On the contrary, the American Society for Reproductive Medicine (ASRM) defined RM as two or more clinical pregnancy losses documented by ultrasonography or histopathologic evaluation, but not necessarily consecutive [5]. This difference in its definition affects also how its incidence and prevalence are calculated across different countries; indeed an international consensus is eagerly needed. The international societies are instead concordant that biochemical pregnancy losses, defined as a positive pregnancy test not associated with the establishment of a pregnancy [6], should not be considered proper miscarriages.
From a clinical perspective, few cases of RM derive from a single pathogenic cause; most of them may in fact have a multifactorial background which involves the interaction of multiple genetic and environmental parameters. Therefore, the outcome for the couples with RM is not determined by a single factor, and it should be carefully tailored upon each couple’s specific characteristics and clinical history.
The aim of this chapter is to summarize the current knowledge upon the causes of RM and discuss the role of preimplantation genetic testing for aneuploidies (PGT-A) and/or for structural rearrangements (PGT-SR) in patients with such indication.
2 Overview of the Main Factors Related to Recurrent Miscarriage
Each couple with RM has a different prognosis largely dependent upon their individual clinical history, a thorough diagnostic workup, and maternal age. Especially the latter is one of the most important elements to predict the reproductive potential of a woman [7]. Indeed, if the fertility rate decreases as the woman ages, the miscarriage rate follows an opposite trend. To this regard, Nybo Anderson and colleagues showed that the risk of miscarriage increases from 8.9% when a woman is aged 20–24 to 74.7% by the age of 44. They set 35 years as the age threshold beyond which this increase becomes more evident. Furthermore, this study also reported that the experience of a miscarriage is prognostic upon further pregnancy losses in following attempts to conceive. For instance, up to 35% and 45% of the parous and nulliparous women who have already experienced three spontaneous abortions may, respectively, undergo a further miscarriage [8].
A thorough investigation of the incidence of karyotypic imbalances in miscarriages highlights that some embryos affected by trisomies for few autosomes or sex chromosome aneuploidies may develop up to this stage of prenatal development, and collectively they account for 60–70% of the first trimester losses in humans [9, 10] (see the specific paragraph treating this topic hereafter). Nevertheless, additional factors can be associated with an increased risk for RM, such as uterine anomalies, antiphospholipid syndrome, and hormonal and metabolic disorders. Moreover, several other etiologies, as chronic endometritis, inherited thrombophilia, luteal phase deficiency, and high sperm DNA fragmentation, have been proposed as possible causes of RM, but are still to be considered controversial [1].
In the next paragraph, we will go through the proposed strategies for a diagnostic workup in patients that experienced RM.
3 Proposed Workup for Patients That Experienced Repeated Miscarriage
Preconception counseling is pivotal for patients with a history of RM, who may be more concerned and require more reassurance for the future attempts. Several investigations, ranging from genetic testing to lifestyle modifications and medication, could have a positive effect on the chances of obtaining a healthy baby. A universally valid workup has not been defined yet, even because any couple has its own medical history, and tailored investigations should be conducted by considering several clinical parameters.
At first, an accurate anamnesis should be conducted for both partners aiming at defining their modifiable lifestyle habits (smoking, abuse of alcohol, diet, etc.) and their family history of infertility and miscarriage [11].
Secondly, a specific blood workup is required to examine possible factors that can affect the prognosis of the couples and the possibility for the woman to carry a pregnancy to term [1]. They may include:
-
(a)
Prolactin (PRL) [12].
-
(b)
Thyroid-stimulating hormone (TSH) serum levels and, in case of abnormal levels, also thyroid autoantibodies testing [13].
-
(c)
Antiphospholipid antibody syndrome could also be investigated by testing anticardiolipin antibodies, anti-β II glycoprotein I antibodies, and lupus anticoagulant [14].
-
(d)
Factor V Leiden, prothrombin gene mutation, protein C and protein S deficiency, antithrombin III deficiency, and hyper-homocysteine, since thrombophilia is one of the causes associated with RM [15].
Nonetheless, for what concerns, for instance, the association of the latter with RM, a meta-analysis of 9 studies including overall 1228 women with an experience of at least two previous miscarriages failed to show any positive impact of anticoagulation treatment (aspirin and low-molecular-weight heparin, or the combination of both) upon a further attempt to conceive [16]. Indeed, this is an example that more consistent data from multicenter studies are yet required to solve the current controversies upon this topic.
Thirdly, a transvaginal three-dimensional ultrasound, sonohysterography, and hysteroscopy should be performed to evaluate the uterine cavity, and pelvic magnetic resonance imaging can also be useful in complex cases of anatomic defects. In fact, uterine anomalies have been reported in up to 20% of women that experienced RM [1, 17].
Besides all the anatomic, endocrine, and immunologic evaluations we may conduct, for about half of the women affected from RM, its causes go undetected, and the main answers up to date could be generally found in the genetics [5, 11].
4 The Genetic Cause of Miscarriage
There is a clear association between maternal age and the incidence of aneuploidies in the embryos produced [7, 18, 19]. However, more than 90% of the chromosomally abnormal embryos, even if they may develop as fully expanded good-quality blastocysts or follow a standard morphodynamic development in vitro [20, 21], either do not implant or are spontaneously aborted. Whole chromosome copy number variations, such as trisomy, polyploidy, or sex chromosome aneuploidies (e.g., 45, X karyotype), are mostly observed in spontaneous abortions. Specifically, almost half of the products of conception after a miscarriage may carry chromosomal abnormalities, a rate that varies depending on woman age and may rise up to 70% [7, 22, 23]. This is mainly due to the meiotic impairment of oogenesis, which is a clear consequence of aging, and may follow different paths, such as meiosis I or meiosis II non-disjunction, premature separation of sister chromatids, or the recently described reverse segregation [24,25,26]. Oogenesis is indeed a long path: the ovarian reserve is established at birth and depleted from menarche to menopause, the oocytes arrest in the late prophase of meiosis I for decades, and, once recruited, they undergo an asymmetrical division and a fast meiosis II post-fertilization. Conversely, spermatogenesis begins with puberty, proceeds uninterrupted, and leads to symmetrical divisions. It has been in fact estimated that only a minority (1–2%) of the spermatozoa carry chromosomal impairments [9, 18], probably also caused by gender-specific differences in the meiotic silencing checkpoint. Essentially, this mechanism seems to be more stringent during sperm than during oocyte maturation processes, thus leading to the arrest of sperms that do not show a perfect matching of the chromosomes [27].
Another important genetic cause of miscarriage is structural chromosomal abnormalities. The most frequent are balanced reciprocal translocations that have an incidence in prenatal diagnosis of 1/560 fetuses and balanced Robertsonian translocations and inversions with an incidence of 1/1100–1200 fetuses. The incidence of unbalanced structural abnormalities is instead even lower [28, 29]. These chromosomal imbalances are independent from maternal age and may equally affect both the partners. In this regard, a history of RM in young women advocates an increased risk of structural chromosome abnormality in one of the components of the couple [29]. Indeed, the incidence of balanced structural chromosome abnormalities is 0.7% in the general population, but it increases to 2.2% after one miscarriage, 4.8% after two miscarriages, and up to 5.2% after three miscarriages [30]. Yet, RM is more frequent when the abnormality is present in the maternal karyotype rather than in paternal one, and again this is probably caused by the differences in the stringency of the meiotic silencing checkpoint [27]. Possibly, as suggested in cytogenetic studies of gametes from patients with balanced structural chromosome abnormalities, such impairments in males more commonly result in a lower fertility, rather than in the production of chromosomally imbalanced sperms [31].
Segmental (or partial) aneuploidies, either copy number variations (CNVs) or microdeletions and microduplications (MMs), are another class of chromosomal imbalances apparently not related to maternal age or gender in general that may be responsible for RM [32, 33]. However, only in <1% they are inherited [34]; it is most probable for them to occur because of a de novo mutation, equally probable during either oogenesis and spermatogenesis or post-fertilization mitotic events. Their estimated prevalence in the newborn population ranges between 0.5 and 2/10000 [35, 36]. Even if their incidence is largely lower than whole chromosome aneuploidies, they may have an equally dramatic impact on reproduction if the copy number state of putative dosage-sensitive genes is altered. Notably though, many segmental aneuploidies do not have a clear pathogenic definition and should be considered variants of unknown significance, whose incidence in miscarriages is 2–3%, different from the pathogenic ones which may reach up to 5% and 0.5% in spontaneous abortions and newborns, respectively [37].
Other chromosomal causes of miscarriage may be embryonic mosaicism (as we will discuss later in this chapter), ploidy impairments, or uniparental disomy. For all of them, the incidence in miscarriage is never higher than 2% [33, 38, 39]. However, they cannot be predicted or accurately diagnosed because of either biological or technical issues (or both), and there is no risk factor related to parental characteristics to predict them.
Future molecular studies on the patients who experienced RM and/or on the products of conception themselves may provide a more thorough view of the mechanisms underlying the occurrence of miscarriage and possibly novel strategies for prevention and/or treatment.
5 What Can We Do for Woman with RM?
Historically, chromosome analysis has been suggested for couples with RM. However, some controversy still exists upon its prognostic value. Those in favor of a routine karyotyping suggest that it should be included as part of the counseling provided to couples with RM, while the opponents claim that even in the presence of RM, only a selected population of patients may benefit from it [29]. Specifically, parental karyotyping is suggested especially in case of young women that underwent more than two pregnancy losses.
In general, though, no strategies are available to counteract the age-related increase of aneuploidies or the establishment of a pregnancy characterized by a partial or structural chromosomal abnormality. In this regard, diagnostic programs either in the preimplantation period on the embryos produced during IVF treatments or in the prenatal period (prenatal diagnosis, PND) were introduced to limit the occurrence of aneuploid pregnancies, especially for older women or with specific indications [40]. Currently, the only available options to minimize this risk are (i) fertility preservation in young women by oocyte vitrification; (ii) egg or sperm donation, where allowed by the local regulation; or (iii) PGT-A and/or PGT-SR at the blastocyst stage during IVF cycles.
PGT is a diagnostic approach aimed at identifying chromosomally normal blastocysts within a cohort of embryo produced during ART. This embryo selection strategy prevents aneuploid blastocysts from being transferred, thus reducing both the risk for implantation failure per transfer and miscarriage due to chromosomal impairments [41,42,43].
At first, PGT (which was previously wrongly referred to as preimplantation genetic screening, PGS) did not show any clinical value in its first version [44], which was designed as a largely ineffective, if not detrimental [45, 46], strategy based on the 9 chromosome-FISH analysis of a single blastomere retrieved from cleavage stage embryos. Conversely, now it is conducted through 24-chromosome testing techniques, namely, array comparative genome hybridization (aCGH), single nucleotide polymorphisms array (SNP-array), quantitative polymerase chain reaction (qPCR), or next-generation sequencing (NGS), on trophectoderm biopsies at the blastocyst stage, a strategy that (i) ensures reliable information; (ii) does not impact embryo reproductive potential [45, 46]; (iii) is cost-effective since the analysis is conducted only on developmentally competent embryos that developed as blastocysts; (iv) guarantees high positive and negative clinical predictive values, which are ≥50% independently from maternal age and ≥ 96%, respectively [47]; and (v) provides a more efficient IVF treatment in terms of higher implantation and lower miscarriage rates according to all the randomized controlled trials (RCTs) conducted up to now and reviewed in two recent meta-analyses [41, 42].
Nevertheless, first class data from RCTs about its efficacy on a per intention-to-treat basis, as well as an analysis of its cost-effectiveness, are still required [43]. Only one study to date showed a comparable efficacy, but lower multiple pregnancy and miscarriage rates when a euploid single blastocyst transfer policy was introduced in a single large IVF center with respect to the previous untested double embryo transfer policy, but it is limited from its retrospective and observational design [48].
At present, PGT could be considered a valid option for couples with RM to select euploid blastocysts with the highest possible developmental potential and the lowest possible risk of miscarriage. Furthermore, it allows to confidently adopt a single embryo transfer policy, thus inherently reducing the risk for multiple pregnancies and relatively negative obstetrical and perinatal outcomes [49, 50].
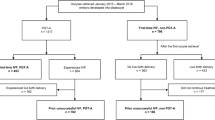
6 The Criticisms Underneath Preimplantation Genetic Testing Technology
In a recent paper, Murugappan and colleagues compared the pregnancy outcomes after IVF-PGT versus the expected management in patients with RM [51]. They claimed that the former provides similar outcomes in terms of pregnancy, live birth, and clinical miscarriage rates per intent to treat as the latter. This paper had a great impact in the scientific community, especially since it was highlighted by the editor in chief of the journal as an evidence that PGT should not be considered a valid clinical option for the treatment of RM. However, Rienzi et al. [52], besides appreciating the effort invested in performing this study due to the absence of clear evidences and an international consensus upon this issue, pointed out some methodological criticisms in its design that unequivocally undermine its reliability. Firstly, no randomization was performed, and there was a significant difference of 2 years in the maternal age between the IVF-PGT (37.1 ± 4.1) and the expected management (35.7 ± 3.9) groups; and secondly, in 20% (n = 40/198) of the IVF cycles, no aneuploidy testing was actually conducted because of poor blastocyst yield and/or embryo morphological quality. As expected, these standard IVF cycles resulted in 50% miscarriage rate versus 14% in the PGT group (p = 0.003). In other terms, the paper by Murugappan and colleagues does not represent high-quality data not using PGT in RM patients. On the contrary, it implicitly stresses the evidence that morphological criteria are very poor predictors of embryo chromosomal architecture and viability. Indeed, if few or only poor-quality blastocysts are produced during an IVF cycle, this should not be a reason to cancel aneuploidy testing, thereby exposing the patients to the consequences of an aneuploid embryo transfer. PGT is not a tool to assess embryo quality; it rather is a diagnostic test to exclude reproductively incompetent embryos from the cohort, namely, the embryos that may generate implantation failures or miscarriages.
There is also a concern about clinically recognizable false-negative errors in PGT, in other terms the risk that an aneuploid blastocyst is diagnosed as euploid and results in a miscarriage or chromosomally abnormal pregnancy. To date, two papers have been published that showed these data with two different molecular techniques: Werner et al. reported it to be as low as 0.32% per clinical pregnancy and 0.13% per ongoing pregnancy by qPCR-based trophectoderm analysis [53], while Tiegs et al. reported it to be 1.5% per clinical pregnancy and a 0.7% per ongoing pregnancy by array-CGH [54].
False-positive results are instead an issue that may result in a different consequence, namely, euploid blastocysts diagnosed as aneuploid and thereby prevented from being transferred. Only Scott and colleagues to date could provide some tremendously valuable data about the negative predictive value of PGT. In a non-selection prospective study conducted by SNP-array, where a trophectoderm biopsy was retrieved and analyzed only after embryo transfer and in a blinded fashion with respect to the clinical outcome, they reported that 4% of the embryos that would have been identified as aneuploid were instead implanted [47]. Later, the same group presented a study to the ASRM annual meeting in 2015 (Werner et al., 2015, ASRM national meeting), where the same design was applied, but a targeted-NGS molecular analysis was conducted. None of the 41 blastocysts that would have been diagnosed aneuploid were then implanted in this interim analysis.
Another important current hot topic in the international scientific and clinical community, which is closely related to the risk for both false-positive and false-negative results, is the issue of chromosomal mosaicism. It is defined as the presence of cell lines with different karyotypes within the same embryo, which may arise because of a mitotic missegregation that occurred post-fertilization. The earlier the error occurs along preimplantation development, the higher the extent of mosaicism. Importantly, aneuploid mosaicism (the presence of cells with different aneuploid chromosomal constitution) does not represent a problem for the diagnosis; only a euploid/aneuploid constitution does. From a biological perspective, an unavoidable sampling bias limits the possibility to identify and properly diagnose mosaic embryos; from a technical perspective, the current comprehensive chromosome testing molecular techniques may suggest the presence of mosaicism through an intermediate log2 ratio for a given chromosome, yet it is not possible to resolve a genuine biological variability from a possible amplification bias [55, 56]. The most probable prevalence of mosaicism in human blastocysts, collectively reported by basic research studies that analyzed disaggregated blastocysts (inner cell mass and 2–3 fragments of trophectoderm) donated for research, is 5% [56]. Its impact in clinical pregnancies achieved from infertile women, reported on thousands of specimens in PND by Huang and colleagues, never exceeds 1.4% after either spontaneous or IVF-derived conceptions, where real mosaicism (not only confined to the placenta) accounts for about 0.5% [38]. Recently, Greco and colleagues in a paper published in the New England Journal of Medicine reported the clinical outcomes after the transfer of 18 allegedly mosaic euploid/aneuploid embryos according to an aCGH-based diagnosis in couples with no other transferable embryo produced during a PGT cycle [57]. They resulted in six full-term pregnancies of chromosomally normal children. This paper, especially with the implementation of novel more sensible NGS-based techniques, introduced the yet controversial transfer of allegedly mosaic embryos in the clinical practice. Clearly, a thorough counseling, which must acknowledge the biological and technical limitations of this controversial practice, should be provided to the couple.
The starting amount of DNA which is retrieved from a biopsy is not sufficient itself to conduct the downstream molecular analyses; therefore, preamplification protocols are required for PGT. Mainly whole genome amplification (WGA) or targeted amplifications strategies may be applied. The former elicits a random amplification of 40–60% of the genome, while the latter allows the sole amplification of predetermined sequences on each chromosome. In a paper published in the European Journal of Human Genetics, Capalbo and colleagues blindly compared WGA-based aCGH and targeted qPCR on two different trophectoderm biopsies obtained from aneuploid blastocysts and, in case of discordant results, analyzed a third biopsy by WGA-based SNP-array [58]. They reported 99.9% of concordance between the methods on a per chromosome analysis. However, if a discordant diagnosis was returned, aCGH was reported as significantly more prone to false-positive errors with respect to qPCR (7% versus 0.5%; p < 0.01). This is ascribable to WGA itself and to the amplification bias that may derive from it, thereby impacting the reliability of the diagnosis. Similarly, the doubt that part of the blastocysts diagnosed as “mosaic” with WGA-based methods could actually be the result of technical errors persists. There is therefore the need for a more thorough validation of the techniques used to this end, by studying multiple biopsies of the same allegedly mosaic blastocyst with different molecular approaches (preferably one of the two should be a targeted approach), before this practice could be adopted in PGT cycles.
Nevertheless, targeted approaches are limited to the diagnosis of only full chromosome aneuploidies and admit a 0.5% risk for clinically significant segmental aneuploidies to term. However, this limitation, for what concerns de novo CNVs and MMs, is shared with WGA-based technologies, which cover just a portion of the genome (40–60%) [59] and may be biased [58] by the preamplification protocol itself. On top of that, a repository database of CNVs/MMs and their consequences on preimplantation embryo development is still missing. It is therefore complex to provide a clinical interpretation of the reproductive impact of any given segmental aneuploidy detected in the preimplantation period.
7 Future Perspectives
Even if PGT-A is an efficient diagnostic tool, it cannot change the embryo intrinsic implantation potential or improve its reproductive competence. The scientific community is therefore investing big efforts to this end.
Firstly, by unveiling any other factor, besides female aging, which may cause aneuploidies [60], some guidelines may be provided to the community to reduce the prevalence of miscarriages and try to broaden woman reproductive lifespan. Moreover, cellular processes involved in chromosome missegregation may be targeted to prevent (or find a solution to) their occurrence. For instance, Wu et al. are investigating the effects of salubrinal in obese mice, as a tool to counteract the diet-derived metabolic stress in the endoplasmic reticulum and reestablish the oocyte maturation potential both in vivo and in vitro [61].
Secondly, by comprehensively characterizing the meiotic machinery and all its different components, we may identify putative key gene/protein targets, whose functionality must be preserved to prevent defective chromosome segregation (e.g., DNA damage response genes (for instance, [62, 63])).
Thirdly, chromosome therapy is a fascinating future perspective to perform functional correction on living cells. Up to now, two protocols have been set up in human/animal cell models: the XIST (X-inactive specific transcript)-driven heterochromatization of chromosome 21 [64] and the ZSCAN4 (zinc finger and SCAN domain containing 4) mRNA-mediated correction of trisomy 18 and 21 [65].
Lastly, several functional and molecular studies in both the academic and clinical fields are ongoing to characterize also the endometrial cells and their receptive potential [66,67,68,69,70]. These studies may bring about novel evidences to increase our knowledge of this topic and possibly introduce novel tools to treat this condition.
8 Conclusion
RM is an important reproductive topic. Various etiologies have been identified over the years, and successful treatment strategies have been implemented. A comprehensive workup can be started following two consecutive losses, especially in women aged >35 years, to identify treatable causes that include uterine abnormalities and immunological, endocrine, and genetic conditions. The modification of some lifestyle habits should also be proposed to increase the reproductive prognosis of a couple. Nevertheless, almost half of the RM cases are still unexplained and yet require future specific investigations. Whatever the cause of RM is, thorough investigations and follow-up supported by a psychological care may help many couples to obtain a successful live birth.
RM is one of the main indications for PGT. However, even if Chen and colleagues reported that the miscarriage rate is significantly lowered after euploid embryo transfer in their meta-analysis [42], some limitations exist. Specifically, data about PGT clinical efficacy per intention to treat and cost-effectiveness are yet missing, and a clear international consensus has not been reached yet. Many clinical studies are in the pipeline, and several research projects are investigating the issue of RM, especially for what concerns the non-chromosomic pregnancy losses, which will hopefully provide novel evidences in the next years.
References
El Hachem H, Crepaux V, May-Panloup P, Descamps P, Legendre G, Bouet PE. Recurrent pregnancy loss: current perspectives. Int J Women's Health. 2017;9:331–45.
Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520–4.
Kolte AM, Bernardi LA, Christiansen OB, Quenby S, Farquharson RG, Goddijn M, et al. Terminology for pregnancy loss prior to viability: a consensus statement from the ESHRE early pregnancy special interest group. Hum Reprod. 2015;30:495–8.
Jauniaux E, Farquharson RG, Christiansen OB, Exalto N. Evidence-based guidelines for the investigation and medical treatment of recurrent miscarriage. Hum Reprod. 2006;21:2216–22.
Practice Committee of the American Society for Reproductive M. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98:1103–11.
Lenton EA, Hooper M, King H, Kumar A, Monks N, Verma S, et al. Normal and abnormal implantation in spontaneous in-vivo and in-vitro human pregnancies. J Reprod Fertil. 1991;92:555–65.
Heffner LJ. Advanced maternal age - how old is too old? N Engl J Med. 2004;351:1927–9.
Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M. Maternal age and fetal loss: population based register linkage study. BMJ. 2000;320:1708–12.
Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2:280–91.
Nagaoka SI, Hassold TJ, Hunt PA. Human aneuploidy: mechanisms and new insights into an age-old problem. Nat Rev Genet. 2012;13:493–504.
Kutteh WH. Novel strategies for the management of recurrent pregnancy loss. Semin Reprod Med. 2015;33:161–8.
Chen H, Fu J, Huang W. Dopamine agonists for preventing future miscarriage in women with idiopathic hyperprolactinemia and recurrent miscarriage history. Cochrane Database Syst Rev. 2016;7:CD008883.
De Carolis C, Greco E, Guarino MD, Perricone C, Dal Lago A, Giacomelli R, et al. Anti-thyroid antibodies and antiphospholipid syndrome: evidence of reduced fecundity and of poor pregnancy outcome in recurrent spontaneous aborters. Am J Reprod Immunol. 2004;52:263–6.
Opatrny L, David M, Kahn SR, Shrier I, Rey E. Association between antiphospholipid antibodies and recurrent fetal loss in women without autoimmune disease: a metaanalysis. J Rheumatol. 2006;33:2214–21.
Rey E, Kahn SR, David M, Shrier I. Thrombophilic disorders and fetal loss: a meta-analysis. Lancet. 2003;361:901–8.
de Jong PG, Kaandorp S, Di Nisio M, Goddijn M, Middeldorp S. Aspirin and/or heparin for women with unexplained recurrent miscarriage with or without inherited thrombophilia. Cochrane Database Syst Rev. 2014:CD004734.
Sugiura-Ogasawara M, Ozaki Y, Katano K, Suzumori N, Mizutani E. Uterine anomaly and recurrent pregnancy loss. Semin Reprod Med. 2011;29:514–21.
Hassold T, Hall H, Hunt P. The origin of human aneuploidy: where we have been, where we are going. Hum Mol Genet. 2007;16(2):R203–8.
Franasiak JM, Forman EJ, Hong KH, Werner MD, Upham KM, Treff NR, et al. The nature of aneuploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril. 2014;101:656–63.
Capalbo A, Rienzi L, Cimadomo D, Maggiulli R, Elliott T, Wright G, et al. Correlation between standard blastocyst morphology, euploidy and implantation: an observational study in two centers involving 956 screened blastocysts. Hum Reprod. 2014;29:1173–81.
Rienzi L, Capalbo A, Stoppa M, Romano S, Maggiulli R, Albricci L, et al. No evidence of association between blastocyst aneuploidy and morphokinetic assessment in a selected population of poor-prognosis patients: a longitudinal cohort study. Reprod Biomed Online. 2015;30:57–66.
Sugiura-Ogasawara M, Ozaki Y, Katano K, Suzumori N, Kitaori T, Mizutani E. Abnormal embryonic karyotype is the most frequent cause of recurrent miscarriage. Hum Reprod. 2012;27:2297–303.
Werner M, Reh A, Grifo J, Perle MA. Characteristics of chromosomal abnormalities diagnosed after spontaneous abortions in an infertile population. J Assist Reprod Genet. 2012;29:817–20.
Ottolini CS, Newnham LJ, Capalbo A, Natesan SA, Joshi HA, Cimadomo D, et al. Genome-wide maps of recombination and chromosome segregation in human oocytes and embryos show selection for maternal recombination rates. Nat Genet. 2015;47:727–35.
Capalbo A, Bono S, Spizzichino L, Biricik A, Baldi M, Colamaria S, et al. Sequential comprehensive chromosome analysis on polar bodies, blastomeres and trophoblast: insights into female meiotic errors and chromosomal segregation in the preimplantation window of embryo development. Hum Reprod. 2013;28:509–18.
Handyside AH, Montag M, Magli MC, Repping S, Harper J, Schmutzler A, et al. Multiple meiotic errors caused by predivision of chromatids in women of advanced maternal age undergoing in vitro fertilisation. Eur J Hum Genet. 2012;20:742–7.
Turner JM. Meiotic silencing in mammals. Annu Rev Genet. 2015;49:395–412.
Forabosco A, Percesepe A, Santucci S. Incidence of non-age-dependent chromosomal abnormalities: a population-based study on 88965 amniocenteses. Eur J Hum Genet. 2009;17:897–903.
Franssen MT, Korevaar JC, Leschot NJ, Bossuyt PM, Knegt AC, Gerssen-Schoorl KB, et al. Selective chromosome analysis in couples with two or more miscarriages: case-control study. BMJ. 2005;331:137–41.
De Braekeleer M, Dao TN. Cytogenetic studies in couples experiencing repeated pregnancy losses. Hum Reprod. 1990;5:519–28.
Kurahashi H, Tsutsumi M, Nishiyama S, Kogo H, Inagaki H, Ohye T. Molecular basis of maternal age-related increase in oocyte aneuploidy. Congenit Anom (Kyoto). 2012;52:8–15.
Ottolini CS, Capalbo A, Newnham L, Cimadomo D, Natesan SA, Hoffmann ER, et al. Generation of meiomaps of genome-wide recombination and chromosome segregation in human oocytes. Nat Protoc. 2016;11:1229–43.
Wang Y, Cheng Q, Meng L, Luo C, Hu H, Zhang J, et al. Clinical application of SNP array analysis in first-trimester pregnancy loss: a prospective study. Clin Genet. 2016;91(6):849–58.
Levy B, Sigurjonsson S, Pettersen B, Maisenbacher MK, Hall MP, Demko Z, et al. Genomic imbalance in products of conception: single-nucleotide polymorphism chromosomal microarray analysis. Obstet Gynecol. 2014;124:202–9.
Kort DH, Chia G, Treff NR, Tanaka AJ, Xing T, Vensand LB, et al. Human embryos commonly form abnormal nuclei during development: a mechanism of DNA damage, embryonic aneuploidy, and developmental arrest. Hum Reprod. 2016;31:312–23.
Vega M, Breborowicz A, Moshier EL, McGovern PG, Keltz MD. Blastulation rates decline in a linear fashion from euploid to aneuploid embryos with single versus multiple chromosomal errors. Fertil Steril. 2014;102:394–8.
Wapner RJ, Martin CL, Levy B, Ballif BC, Eng CM, Zachary JM, et al. Chromosomal microarray versus karyotyping for prenatal diagnosis. N Engl J Med. 2012;367:2175–84.
Huang A, Adusumalli J, Patel S, Liem J, Williams J 3rd, Pisarska MD. Prevalence of chromosomal mosaicism in pregnancies from couples with infertility. Fertil Steril. 2009;91:2355–60.
Gueye NA, Devkota B, Taylor D, Pfundt R, Scott RT Jr, Treff NR. Uniparental disomy in the human blastocyst is exceedingly rare. Fertil Steril. 2014;101:232–6.
Vermeesch JR, Voet T, Devriendt K. Prenatal and pre-implantation genetic diagnosis. Nat Rev Genet. 2016;17:643–56.
Dahdouh EM, Balayla J, Garcia-Velasco JA. Comprehensive chromosome screening improves embryo selection: a meta-analysis. Fertil Steril. 2015;104:1503–12.
Chen M, Wei S, Hu J, Quan S. Can comprehensive chromosome screening technology improve IVF/ICSI outcomes? A meta-analysis. PLoS One. 2015;10:e0140779.
Vaiarelli A, Cimadomo D, Capalbo A, Orlando G, Sapienza F, Colamaria S, et al. Pre-implantation genetic testing in ART: who will benefit and what is the evidence? J Assist Reprod Genet. 2016;33:1273–8.
Mastenbroek S, Twisk M, van der Veen F, Repping S. Preimplantation genetic screening: a systematic review and meta-analysis of RCTs. Hum Reprod Update. 2011;17:454–66.
Scott RT Jr, Upham KM, Forman EJ, Zhao T, Treff NR. Cleavage-stage biopsy significantly impairs human embryonic implantation potential while blastocyst biopsy does not: a randomized and paired clinical trial. Fertil Steril. 2013;100:624–30.
Cimadomo D, Capalbo A, Ubaldi FM, Scarica C, Palagiano A, Canipari R, et al. The impact of biopsy on human embryo developmental potential during preimplantation genetic diagnosis. Biomed Res Int. 2016;2016:7193075.
Scott RT Jr, Ferry K, Su J, Tao X, Scott K, Treff NR. Comprehensive chromosome screening is highly predictive of the reproductive potential of human embryos: a prospective, blinded, nonselection study. Fertil Steril. 2012;97:870–5.
Ubaldi FM, Capalbo A, Colamaria S, Ferrero S, Maggiulli R, Vajta G, et al. Reduction of multiple pregnancies in the advanced maternal age population after implementation of an elective single embryo transfer policy coupled with enhanced embryo selection: pre- and post-intervention study. Hum Reprod. 2015;30:2097–106.
Forman EJ, Hong KH, Ferry KM, Tao X, Taylor D, Levy B, et al. In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertil Steril. 2013;100:100–7.
Forman EJ, Hong KH, Franasiak JM, Scott RT Jr. Obstetrical and neonatal outcomes from the BEST Trial: single embryo transfer with aneuploidy screening improves outcomes after in vitro fertilization without compromising delivery rates. Am J Obstet Gynecol. 2014;210:157.e1–6.
Murugappan G, Shahine LK, Perfetto CO, Hickok LR, Lathi RB. Intent to treat analysis of in vitro fertilization and preimplantation genetic screening versus expectant management in patients with recurrent pregnancy loss. Hum Reprod. 2016;31:1668–74.
Rienzi L, Capalbo A, Vajta G, Ubaldi FM. PGS for recurrent pregnancy loss: still an open question. Hum Reprod. 2017;32:476–7.
Werner MD, Leondires MP, Schoolcraft WB, Miller BT, Copperman AB, Robins ED, et al. Clinically recognizable error rate after the transfer of comprehensive chromosomal screened euploid embryos is low. Fertil Steril. 2014;102:1613–8.
Tiegs AW, Hodes-Wertz B, McCulloh DH, Munne S, Grifo JA. Discrepant diagnosis rate of array comparative genomic hybridization in thawed euploid blastocysts. J Assist Reprod Genet. 2016;33:893–7.
Capalbo A, Rienzi L. Mosaicism between trophectoderm and inner cell mass. Fertil Steril. 2017;107:1098–106.
Capalbo A, Ubaldi FM, Rienzi L, Scott R, Treff N. Detecting mosaicism in trophectoderm biopsies: current challenges and future possibilities. Hum Reprod. 2016;32(3):492–8.
Greco E, Minasi MG, Fiorentino F. Healthy babies after intrauterine transfer of mosaic aneuploid blastocysts. N Engl J Med. 2015;373:2089–90.
Capalbo A, Treff NR, Cimadomo D, Tao X, Upham K, Ubaldi FM, et al. Comparison of array comparative genomic hybridization and quantitative real-time PCR-based aneuploidy screening of blastocyst biopsies. Eur J Hum Genet. 2015;23:901–6.
Gawad C, Koh W, Quake SR. Single-cell genome sequencing: current state of the science. Nat Rev Genet. 2016;17:175–88.
Hunter JE, Allen EG, Shin M, Bean LJ, Correa A, Druschel C, et al. The association of low socioeconomic status and the risk of having a child with Down syndrome: a report from the national Down syndrome project. Genet Med. 2013;15:698–705.
Wu LL, Russell DL, Wong SL, Chen M, Tsai TS, St John JC, et al. Mitochondrial dysfunction in oocytes of obese mothers: transmission to offspring and reversal by pharmacological endoplasmic reticulum stress inhibitors. Development. 2015;142:681–91.
Caburet S, Arboleda VA, Llano E, Overbeek PA, Barbero JL, Oka K, et al. Mutant cohesin in premature ovarian failure. N Engl J Med. 2014;370:943–9.
Hopkins J, Hwang G, Jacob J, Sapp N, Bedigian R, Oka K, et al. Meiosis-specific cohesin component, Stag3 is essential for maintaining centromere chromatid cohesion, and required for DNA repair and synapsis between homologous chromosomes. PLoS Genet. 2014;10:e1004413.
Jiang J, Jing Y, Cost GJ, Chiang JC, Kolpa HJ, Cotton AM, et al. Translating dosage compensation to trisomy 21. Nature. 2013;500:296–300.
Amano T, Jeffries E, Amano M, Ko AC, Yu H, Ko MS. Correction of Down syndrome and Edwards syndrome aneuploidies in human cell cultures. DNA Res. 2015;22:331–42.
Larsen EC, Christiansen OB, Kolte AM, Macklon N. New insights into mechanisms behind miscarriage. BMC Med. 2013;11:154.
Weimar CH, Macklon NS, Post Uiterweer ED, Brosens JJ, Gellersen B. The motile and invasive capacity of human endometrial stromal cells: implications for normal and impaired reproductive function. Hum Reprod Update. 2013;19:542–57.
Weimar CH, Post Uiterweer ED, Teklenburg G, Heijnen CJ, Macklon NS. In-vitro model systems for the study of human embryo-endometrium interactions. Reprod Biomed Online. 2013;27:461–76.
Diaz-Gimeno P, Ruiz-Alonso M, Blesa D, Bosch N, Martinez-Conejero JA, Alama P, et al. The accuracy and reproducibility of the endometrial receptivity array is superior to histology as a diagnostic method for endometrial receptivity. Fertil Steril. 2013;99:508–17.
Ruiz-Alonso M, Blesa D, Diaz-Gimeno P, Gomez E, Fernandez-Sanchez M, Carranza F, et al. The endometrial receptivity array for diagnosis and personalized embryo transfer as a treatment for patients with repeated implantation failure. Fertil Steril. 2013;100:818–24.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Vaiarelli, A., Cimadomo, D., Rienzi, L., Ubaldi, F.M. (2020). Preimplantation Genetic Testing for Aneuploidies (PGT-A) in Recurrent Miscarriage. In: Allahbadia, G.N., Ata, B., Lindheim, S.R., Woodward, B.J., Bhagavath, B. (eds) Textbook of Assisted Reproduction. Springer, Singapore. https://doi.org/10.1007/978-981-15-2377-9_73
Download citation
DOI: https://doi.org/10.1007/978-981-15-2377-9_73
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-2376-2
Online ISBN: 978-981-15-2377-9
eBook Packages: MedicineMedicine (R0)