Abstract
Chronic kidney disease (CKD) is a worldwide public health problem. In CKD patients, exercise endurance is lowered, and this phenomenon becomes more distinct as the renal dysfunction advances. This is due to the combined effects of uremic acidosis, protein-energy wasting, and inflammatory cachexia, which lead to and are further aggravated by a sedentary lifestyle. Together, these factors result in a progressive downward spiral of deconditioning. This review focuses on the benefits and risks of exercise training in CKD patients. In Japan, we have established the Japanese Society of Renal Rehabilitation in 2011 to evaluate and promote renal rehabilitation (RR). We use a comprehensive approach to RR including physical exercise and psychological, vocational, and dietary counseling. RR is a feasible, effective, and safe secondary prevention strategy following CKD and offers a promising model for new field of rehabilitation. Urgent efforts should be made to increase the implementation rate of the RR.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
4.1 Introduction
Chronic kidney disease (CKD) is a worldwide public health problem. The numbers of patients of hemodialysis (HD) in Japan are more than 340,000, which correspond to 1 in 370 of the total population. Furthermore, the numbers of patients of CKD in Japan are more than 11% of the total population.
In CKD patients, exercise endurance is lowered, and this phenomenon becomes more distinct as the renal dysfunction advances. This is due to the combined effects of uremic acidosis, protein-energy wasting (PEW), and inflammatory cachexia, which lead to and are further aggravated by a sedentary lifestyle. Together, these factors result in a progressive downward spiral of deconditioning.
CKD patients undergoing dialysis have very high mortality with cardiovascular diseases such as chronic heart failure, and yet higher mortality risk has been reported for sedentary CKD patients undergoing dialysis [1]. As well as being a strong cardiovascular risk factor, physical inactivity (PI) is associated with increased risk of rapid kidney function decline in CKD patients [2]. This review focuses on the benefits and risks of exercise training in CKD patients.
4.2 CKD and Physical Inactivity
PI is well recognized as a major health issue in today’s society. Regular exercise is important in maintaining health and preventing chronic disease. Moreover, the association between PI and poor outcomes is well established for CKD patients [3,4,5]. CKD patients typically engage in a lower level of PA than do the general population, which can induce a catabolic state including reduced neuromuscular functioning, reduced exercise tolerance, and reduced cardiorespiratory fitness.
Results from an international study of CKD patients undergoing dialysis indicate that regular exercise is associated with better outcomes, and that patients at facilities offering exercise programs have higher odds of exercising. In the Dialysis Outcomes and Practice Patterns Study (DOPPS), overall, 47.4% of participants were categorized as regular exercisers. The odds of regular exercise were 38% higher for patients from facilities offering exercise programs (P = 0.03) [4].
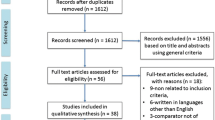
In addition to PI, cardiorespiratory fitness is an important consideration, as it is a strong predictor of mortality [6, 7]; low cardiorespiratory fitness presents a particularly high risk of death compared to other common risk factors, such as diabetes, high cholesterol, or hypertension [8]. Cardiorespiratory fitness is defined as the ability of the circulatory and respiratory systems to supply oxygen during sustained physical activity (PA) and is usually expressed as maximal oxygen uptake (VO2 max) or peak oxygen uptake (peak VO2) during exercise stress testing [9]. VO2 max is expressed either as an absolute rate in, for example, liters of oxygen per minute (L/min) or as a relative rate in, for example, milliliters of oxygen per kilogram of body mass per minute (e.g., mL/[kg min]). Figure 4.1 shows gas transport mechanisms for coupling cellular (internal) to pulmonary (external) respiration [10]. The gears represent the functional interdependence of the physiological components of the system. Cardiac output, pulmonary diffusion capacity, oxygen carrying capacity, renal function, and other peripheral limitations like muscle diffusion capacity, mitochondrial enzymes, and capillary density are all examples of VO2 max determinants.
Gas transport mechanisms for coupling cellular to pulmonary respiration: five major determinants for peak VO2. (Used with permission from Kohzuki [10])
The large increase in O2 utilization by the muscles (QO2) is achieved by increased extraction of O2 from the blood perfusing the muscles, the dilatation of selected peripheral vascular beds, an increase in cardiac output (stroke volume and heart rate), an increase in pulmonary blood flow by recruitment and vasodilatation of pulmonary blood vessels, and finally, an increase in ventilation. O2 is taken up (VO2) from the alveoli in proportion to the pulmonary blood flow and degree of O2 desaturation of hemoglobin in the pulmonary capillary blood. Metabolic acidosis in CKD patients promotes muscle protein wasting and PEW by increasing protein degradation [11] and reducing protein synthesis [12]. As a result, maintenance of muscle mass is impaired in CKD patients with altered protein turnover rates [13]. Adding to sarcopenia, metabolic acidosis, PEW, angiotensin II, myostatin overexpression in uremia contribute to the etiology in muscle wasting in CKD [14]. Moreover, the drug erythropoietin (EPO) can boost VO2 max by a significant amount in both humans and other mammals [15].
4.3 Effects of Exercise Training in CKD Patients
-
1.
The effect of exercise training in chronic kidney disease patients undergoing dialysis.
In DOPPS study, regular exercisers in CKD patients undergoing dialysis had higher health-related quality of life (HR-QL), physical functioning, and sleep quality scores; reported fewer limitations in physical activities; and were less bothered by bodily pain or lack of appetite [4]. Regular exercise was also correlated with more positive patient affect and fewer depressive symptoms [4]. In models extensively adjusted for demographics, comorbidities, and socioeconomic indicators, mortality risk was lower among regular exercisers (hazard ratio = 0.73 [0.69–0.78]; P < 0.0001) and at facilities with more regular exercisers (0.92 [0.89–0.94]; P < 0.0001 per 10% more regular exercisers) [4].
A systematic review and meta-analysis controlled trials were reported about regular exercise training for at least 3–10 months in CKD patients undergoing dialysis demonstrated that baseline, peak VO2 values were 70% of age-predicted values, exercise intervention patients improved post-training peak VO2 to 88% predicted [5]. In CKD patients undergoing dialysis, exercise training produced 26% improvements in eight studies that reported peak VO2. Equivocal results for change in short-form 36 health questionnaire scores were reported post-training [5]. Significant improvements in lean body mass, quadriceps muscle area, knee extension, hip abduction, and flexion strength were also reported [5]. They did not find any deaths directly associated with exercise in 28,400 patient-hours and no differences in withdrawal rates between exercise and control participants. Exercise training for 6 months or more conveyed larger improvements in peak VO2 than shorter programs. Therefore, exercise training is safe and imparts large improvements in peak VO2 and heart rate variability in CKD patients undergoing dialysis [5].
Moreover, a growing evidence suggests that exercise training in CKD patients undergoing dialysis improves VO2 max, left ventricular function, cardiac sympathetic and parasympathetic disharmony, PEW, anemia, sleep quality, anxiety, HR-QL, activities of daily living, shunt size, Kt/V, and mortality [3, 16].
-
2.
The effect of exercise training in pre-dialysis CKD animal models.
There is increasing evidence of the benefit of regular physical exercise in a number of long-term conditions including CKD. It is also necessary to consider the influence of exercise on renal functions because acute exercise causes proteinuria and subsequent reductions in both the renal blood flow and glomerular filtration rate (GFR). It has also been demonstrated clinically that sudden exercise decreases renal function. There are few reports on the influence of chronic exercise on renal function, and there is little information about the effect of exercise on pre-dialysis CKD patients. The optimal intensity and duration of exercise for pre-dialysis CKD patients have not yet been formulated.
We have published several papers in this field. We assessed the renal effects of moderate chronic treadmill exercise in several CKD rat models and reported that exercise does not worsen renal function and has renal-protective effects in some models of rats such as a remnant kidney model of spontaneously hypertensive rats with 5/6 nephrectomy, [17] 5/6-nephrectomized Wistar–Kyoto rats, [18] a rat model of diabetic nephropathy (Goto–Kakizaki rats), [19] and Zucker diabetic rats [20].
-
3.
The effect of regular exercise training in pre-dialysis chronic kidney disease patients.
Relatively few studies have included patients with stage 1–4 CKD, which limits the generalization of findings to pre-dialysis CKD patients. Sedentary pre-dialysis CKD men (eGFRcreat 27.5 ± 11.6 mL/min) were randomly assigned to a center-based exercise group, home-based exercise group, or control group. In exercise groups, the aerobic training was performed three times per week during 12 weeks. eGFRcreat increased 3.6 ± 4.6 mL/min (P = 0.03) in the center-based group. The parameter remained unchanged in the control group [21].
Greenwood et al. examined the effect of moderate-intensity exercise training on kidney function and indexes of cardiovascular risk in patients with progressive stages 3–4 CKD. Single-blind randomized controlled studies showed that a significant mean difference in rate of change in eGFRcreat was observed between the rehabilitation and usual care groups, with the rehabilitation group demonstrating a slower decline [22].
Chen et al. investigated the association of walking with overall mortality and renal replacement therapy (RRT) such as hemodialysis, peritoneal dialysis, or kidney transplantation in patients with stages 3–5 CKD. A total of 6363 patients (average age, 70 years) were analyzed. There were 1341 (21.1%) patients who reported walking as their most common form of exercise training. The incidence density rate of overall mortality was 2.7 per 100 person-years for walking patients and 5.4 for non-walking ones. The incidence density rate of RRT was 22 per 100 person-years for walking patients and 32.9 for non-walking ones. Walking, independent of patients’ age, renal function, and comorbidity, was linked to lower overall mortality and lower RRT risk in the multivariate competing-risks regression. The adjusted subdistribution hazard ratio (SHR) of walking was 0.67 (95% confidence interval [95% CI], 0.53–0.84; P < 0.001) for overall mortality and 0.79 (95% CI, 0.73–0.85; P < 0.001) for the risk of RRT. The SHRs of overall mortality were 0.83, 0.72, 0.42, and 0.41 for patients walking 1–2, 3–4, 5–6, and 7 times per week, and the SHRs of RRT were 0.81, 0.73, 0.57, and 0.56, respectively. Walking is the most popular form of exercise training in CKD patients and is associated with lower risks of overall mortality and RRT. The benefit of walking is independent of patients’ age, renal function, and comorbidity [23].
-
4.
The effect of regular exercise training in pre-dialysis chronic kidney disease patients with acute myocardial infarction.
Combined renal dysfunction worsens the subsequent prognosis in patients after acute myocardial infarction (AMI). We elucidated the association between PA level and changes in renal function in patients after AMI [24]. Renal function was evaluated based on cystatin C based-estimated glomerular filtration rate (eGFRcys) which is independent of skeletal muscle mass. Patients were stratified into low (2335 ± 1219 steps/day) and high groups (7102 ± 2365 steps/day). eGFRcys significantly increased from baseline to after 3 months in the high group (76.5 ± 13.8 to 83.2 ± 16.0 mL/min/1.73m2), whereas no significant change was observed in the low group (65.1 ± 15.9 to 62.2 ± 20.2 mL/min/1.73m2). Changes in eGFRcys was −2.9 mL/min/1.73m2 among low group versus +6.7 mL/min/1.73 m2 among high group [24]. PA level was positively associated with changes in renal function, demonstrating that high PA may suppress renal function decline in patients after AMI. Figure 4.2 shows the associations between the number of steps and ΔeGFRcys or ΔeGFRcreat in all patients [24]. The results of Pearson’s correlation analysis showed significant correlations between the number of steps and both parameters. Furthermore, the correlation coefficient between ΔeGFRcreat and the number of steps (r = 0.38, p = 0.015) was lower compared to the correlation coefficient between ΔeGFRcys (r = 0.55, p < 0.001) and the number of steps. As previously pointed out, changes in the serum creatinine level through movement of the skeletal muscles is one of the causes, and the significance of using eGFRcys as an indicator for renal function in this study was confirmed [25, 26].
In recent years, a prior prospective study verified the association between PA level and renal function in CKD patients [27]. The results of this study are similar to our present findings and indicate that maintaining a high level of PA in daily life leads to suppression of renal function deterioration. The present study is the first to show the association between PA level and changes in renal function after the onset of AMI using an accelerometer and eGFRcys. High PA was suggested to suppress renal function decline in patients with AMI. Our findings support the importance of interventions to maintain high PA as a strategy for renal protection in AMI patients. Future research should verify the long-term effect of PA level on renal function among AMI patients.
Association between the number of steps and ΔeGFRcys or ΔeGFRcreat. (Used with permission from Sato et al. [24])
4.4 Indications and Contraindications of Exercise Stress Test and Exercise Training in CKD Patients
4.4.1 Medical Checkups
Prior to beginning exercise training programs, candidates should be assessed for clinical status and undergo examinations at rest and exercise stress tests to determine the appropriateness of exercise training for individual participants and to establish the appropriate exercise prescription. Clinical status should be assessed through medical interviews about subjective symptoms, medical history, family history, and lifestyle. Medical checkups should include measurement of blood pressure, pulse rate, and electrocardiographic activity. Levels of blood glucose, total cholesterol, triglycerides, hepatic enzymes, and body mass index should also be evaluated [28].
4.4.2 Exercise Stress Test
Those who have not participated in regular exercise training in the previous 3 months should be referred for medical clearance prior to beginning exercise training. Because cardiovascular disease (CVD) is the major cause of death in CKD patients, when symptoms are present or CVD is diagnosed, exercise stress test may be indicated as part of the medical clearance process prior to beginning an exercise program of moderate to vigorous intensity. In CKD patients undergoing dialysis, exercise stress test should be scheduled for non-dialysis days, and blood pressure should be monitored in the arm that does not contain the arteriovenous fistula. For comfort purposes, patients receiving continuous ambulatory peritoneal dialysis should be tested with little dialysate fluid in their abdomen [29].
However, some suggest that exercise test for CKD patients, as well as those who are frail, is not warranted because their performance may be affected by muscle fatigue, and such testing may act as an unnecessary barrier to their participation in an exercise program. If performed, exercise stress test of CKD patients should use standard test termination criteria and test termination methods [28].
Absolute contraindications for exercise stress test are acute myocardial infarction developed within 2 days, unstable angina not controlled with medical treatment, uncontrolled arrhythmia that causes symptoms or hemodynamic compromise, symptomatic severe aortic stenosis, uncontrolled symptomatic heart failure, acute pulmonary embolism or pulmonary infarction, acute myocarditis or pericarditis, acute aortic dissection, and mental disorders associated with communication difficulties [28].
Relative contraindications for exercise stress test are left main coronary artery stenosis, moderate stenotic valvular heart disease, electrolyte abnormality, severe hypertension (systolic blood pressure of >200 mmHg and/or a diastolic blood pressure of >110 mmHg,), tachyarrhythmia or bradyarrhythmia, hypertrophic cardiomyopathy or other outflow tract obstruction, mental or physical impairment leading to inability to exercise adequately, and advanced atrioventricular block [28].
Criteria for terminating exercise stress test are as follows: (1) Symptoms—anginal pain, dyspnea, syncope, dizziness, light-headed feeling, and leg pain (claudication); (2) signs—cyanosis, facial pallor, cold sweat, and ataxia; (3) blood pressure—insufficient increase or progressive decrease in systolic blood pressure during exercise, or abnormal increase in blood pressure (≥225 mmHg); (4) ECG—apparent ischemic ST-T changes, cardiac rhythm disorder (e.g., severe tachycardia or bradycardia, ventricular tachycardia, frequent arrhythmias, atrial fibrillation, R on T, and premature ventricular contractions), and second or third degree atrioventricular block [28].
4.4.3 Exercise Training
All CKD patients must be assessed carefully to determine whether exercise training is indicated.
Absolute contraindications for exercise training in CKD patients are as follows: (1) Exacerbation of heart failure symptoms (e.g., dyspnea, easy fatigability) during the last week, (2) unstable angina or low-threshold myocardial ischemia that is induced by slow walking on a flat surface (2 METs), (3) severe valvular heart disease indicated for surgery, especially aortic stenosis, (4) severe left ventricular outflow tract obstruction (hypertrophic obstructive cardiomyopathy), (5) untreated severe exercise-induced arrhythmia (ventricular fibrillation, sustained ventricular tachycardia), (6) active myocarditis, (7) acute systemic disease or fever, and (8) other diseases in which exercise is contraindicated (moderate or severe aortic aneurysm, severe hypertension, thrombophlebitis, embolism that developed in the last 2 weeks, and serious organ diseases) [28].
Relative contraindications for exercise training in CKD patients are as follows: (1) NYHA classification of Class IV heart failure or heart failure requiring intravenous cardiotonics, (2) heart failure with an increase in body weight by ≥2 kg during the last week, (3) exercise-induced decrease in systolic blood pressure, (4) moderate left ventricular outflow tract obstruction, (5) exercise-induced moderate arrhythmia (e.g., non-sustained ventricular tachycardia, tachycardiac atrial fibrillation), (6) advanced atrioventricular block, (7) exacerbation of exercise-induced symptoms (e.g., fatigue, dizziness, excessive sweating, dyspnea) [28].
Moreover, CKD patients are likely to be on multiple medications including those that are commonly used in the treatment of hypertension, dyslipidemia, and diabetes mellitus. If they have such diseases, they should follow indications and contraindications for exercise training in lifestyle-related diseases too. Indications are shown as follows: Hypertension—BP of 140–159/90–94 mmHg; diabetes—fasting blood glucose level of 110–139 mg/dL; dyslipidemia—TC of 220–249 mg/dL or TG of 150–299 mg/dL; and obesity—BMI of 24.0–29.9 [28].
Conditional indications are shown as follows: Hypertension—BP of 160–179/95–99 mmHg, ongoing antihypertensive treatment with BP less than the contraindicated level, men over 40 years and women over 50 years should undergo exercise stress tests whenever possible. If exercise stress tests are not feasible, prescribe walking or other light exercise. Diabetes—fasting blood glucose level of 140–249 mg/dL; ongoing antidiabetic treatment with glucose levels less than the contraindicated level; men over 40 years and women over 50 years should undergo exercise stress tests whenever possible. If exercise stress tests are not feasible, prescribe walking or other light exercise. Dyslipidemia—TC of ≥250 mg/dL or TG of ≥300 mg/dL, ongoing lipid management; men over 40 years and women over 50 years should undergo exercise stress tests whenever possible. If exercise stress tests are not feasible, prescribe walking or other light exercise. Obesity—BMI of 24.0–29.9, detailed assessment for leg joint disorder; limitation of exercise [28].
Contraindications are shown as follows: Hypertension—BP of ≥180/100 mmHg; chest X-ray findings with a CTR of ≥55%; ECG indicating severe arrhythmia or ischemic changes (excluding those with favorable results of exercise stress tests); hypertensive changes (IIb or higher) on funduscopy; urinary protein of ≥100 mg/dL. Diabetes—Fasting blood glucose level of ≥250 mg/dL; positive urinary ketones; diabetic retinopathy; and obesity—BMI ≥30.0 [28].
4.5 Barriers to Exercise Participation Among CKD Patients
Unfortunately, the role of PA in CKD has been largely overlooked. The supply of exercise advice and rehabilitation programs for CKD patients are lagging behind that of cardiology and pulmonary services.
The Kidney Disease Outcomes Quality Initiative (K/DOQI) clinical practice guidelines on management of cardiovascular disease state that, “all dialysis patients should be counseled and regularly encouraged by nephrology and dialysis staff to increase their level of PA” [30].
In multivariate analysis, a greater number of reported barriers were associated with lower levels of PA. Lack of motivation was associated with less PA. Endorsement of too many medical problems and not having enough time on dialysis days were also associated with less activity in adjusted analysis [31].
Delgado et al. administered a 30-item survey regarding exercise counseling to nephrologists attending the American Society of Nephrology meeting in 2007 [32]. In multivariate analysis, older nephrologists (odds ratio; 95% CI) (3.3; 1.2–9.0) and those more physically active (5.5; 2.0–14) were more likely to ask and counsel patients about PA [32]. Opinions associated with less counseling behavior included lack of confidence in ability to discuss PA. They also reported that CKD patients undergoing dialysis were interested in PA [31]. They reported that 92% of participants reported at least one barrier to PA. The most commonly reported barriers were fatigue on dialysis days and non-dialysis days and shortness of breath. In multivariate analysis, a greater number of reported barriers were associated with lower levels of PA. Lack of motivation was associated with less PA. Endorsement of too many medical problems and not having enough time on dialysis days were also associated with less activity in adjusted analysis [31].
The location of the exercise training is also an important factor influencing adherence. In CKD patients undergoing dialysis, intra-dialysis programs have been found to achieve higher adherence rates compared to home exercise programs or supervised programs on non-dialysis days [33].
4.6 Renal Rehabilitation
Several international initiatives and working groups have been established to tackle the specific contribution of physical inactivity to the burden of disease in CKD patients [34,35,36,37]. In line with recommendations for the general population, Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend that patients with CKD undertake moderate PA for at least 30 min five times per week [38].
In Japan, we established the Japanese Society of Renal Rehabilitation (JSRR) in 2011 to evaluate and promote renal rehabilitation (RR). We define RR as, “RR is coordinated, multifaceted interventions designed to optimize a renal patient’s physical, psychological, and social functioning, in addition to stabilizing, slowing, or even reversing the progression of renal deterioration, thereby reducing morbidity and mortality. RR includes five major components: such as exercise training, diet and fluid management, medication and medical surveillance, education, psychological and vocational counseling” [3, 16]. We use a comprehensive approach to RR including physical exercise and psychological, vocational, and dietary counseling. We first published the book titled Renal Rehabilitation [3, 16]. In recent years, the concept of RR has become widely known among nephrology specialists, dialysis specialists, kidney transplantation specialists, rehabilitation specialists, nutrition specialists, guideline specialists, nurses, physiotherapists, and representatives of patients. In order to make clear the methods and effectiveness of renal rehabilitation in Japan, we launched Renal Rehabilitation Guideline Preparation Committee in 2016 as a part of works in the JSRR and created a guideline in accordance with the “Minds Handbook for Clinical Practice Guideline Development 2014” [39, 40]. Six recommendations for the condition of each kidney disorder, groups addressing nephritis/nephrosis, chronic kidney diseases, dialysis therapy, and kidney transplantation were created. All the recommendation grades were determined by a consensus conference participated in by representatives of patients and various professionals.
Moreover, to our knowledge, health-care systems in most countries offer no or limited reimbursement for exercise training for CKD patients. In contrast, such infrastructure and reimbursement systems do exist in many countries for rehabilitation after cardiac diseases. Therefore, CKD patients are largely unsupported in overcoming barriers to exercise and in finding suitable exercise facilities [41]. To our knowledge, Japan is the only country to offer exercise training for patients with diabetes and pre-dialysis CKD stage 3B–5 that is covered by the national health insurance system [42, 43].
4.7 Adding Life to Years and Years to Life
As super-aged society has come, the number of persons with multimorbidity and multiple disabilities and their needs of rehabilitation have increased rapidly more than we had expected [44]. Medical science basically aims to “Adding Years to Life” by increasing life expectancy. Rehabilitation generally aims to “Adding Life to Years” by helping patients with impairment achieve, and use, their full physical, mental, and social potential. However, recent growing evidence suggests that rehabilitation for patients with visceral impairment such as renal, cardiac, and pulmonary impairment can not only improve exercise performance and HR-QL but also increases survival (Fig. 4.3) [45]. Therefore, modern comprehensive rehabilitation for CKD patients does not simply aim to “Adding Life to Years” but “Adding Life to Years and Years to Life,” which is a new rehabilitation concept [45].
Renal rehabilitation is a new paradigm of rehabilitation. (Used with permission from Kohzuki et al. [45])
4.8 Conclusion
In RR, we should improve not only HR-QL but also biological lifespan in CKD patients. RR is a feasible, effective, and safe secondary prevention strategy following CKD and offers a promising model for new field of rehabilitation. Future larger randomized controlled trials should focus more on the effects of exercise training and rehabilitation programs as these subjects and exercise types have not been studied as much as cardiovascular exercise. Moreover, urgent efforts should be made to increase the implementation rate of the RR.
References
O’Hare AM, Tawney K, Bacchetti P, et al. Decreased survival among sedentary patients undergoing dialysis: results from the dialysis morbidity and mortality study wave 2. Am J Kidney Dis. 2003;41:447–54.
Johansen KL. Exercise in the end-stage renal disease population. J Am Soc Nephrol. 2007;18:1845–54.
Kohzuki M. Renal rehabilitation: present and future perspectives. In: Suzuki H, editor. Hemodialysis. London: Intech; 2013. p. 743–51.
Tentori F, Slder SJ, Thumma J. Physical exercise among participants in the Dialysis Outcomes and Practice Patterns Study (DOPPS): correlates and associated outcomes. Nephrol Dial Transplant. 2010;25:3050–62.
Smart N, Steele M. Exercise training in haemodialysis patients: a systematic review and meta-analysis. Nephrology. 2011;16:626–32.
Sieverdes JC, Sui X, Lee DC, et al. Physical activity, cardiorespiratory fitness and the incidence of type 2 diabetes in a prospective study of men. Br J Sports Med. 2010;44:238–44.
Blair SN, Kohl HW, Paffenbarger RS, et al. Physical fitness and all-cause mortality: a prospective study of healthy men and women. JAMA. 1989;262:2395–401.
Blair SN, Sallis RE, Hutber A, et al. Exercise therapy — the public health message. Scand J Med Sci Sports. 2012;22:24–8.
Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–31.
Kohzuki M. New ideas on limitations to VO2max: five major determinants for VO2max. Pulm Res Respir Med Open J. 2018;5(1):e1–2. https://doi.org/10.17140/PRRMOJ-5-e010.
Caso G, Garlick PJ. Control of muscle protein kinetics by acid-base balance. Curr Opin Clin Nutr Metab Care. 2005;8:73–6.
Bailey JL, Wang X, England BK. The acidosis of chronic renal failure activates muscle proteolysis in rats by augmenting transcription of genes encoding proteins of the ATP-dependent ubiquitin-proteasome pathway. J Clin Invest. 1996;97:1447–53.
Mitch WE. Influence of metabolic acidosis on nutrition. Am J Kidney Dis. 1997;29:16–8.
Fahal IH. Uraemic sarcopenia: aetiology and implications. Nephrol Dial Transplant. 2014;29:1655–65.
Kolb EM. Erythropoietin elevates VO2, max but not voluntary wheel running in mice. J Exp Biol. 2010;213:510–9. https://doi.org/10.1242/jeb.029074.
Kohzuki M. Renal rehabilitation: Difinition and evidence. In: Kohzuki M, editor. Renal Rehabilitation. Tokyo: Ishiyaku Publishers; 2012. p. 10–7.
Kohzuki M, Kamimoto M, Wu XM, et al. Renal protective effects of chronic exercise and antihypertensive therapy in hypertensive rats with chronic renal failure. J Hypertens. 2001;19:1877–82.
Kanazawa M, Kawamura T, Li L, et al. Combination of exercise and enalapril enhances renoprotective and peripheral effects in rats with renal ablation. Am J Hypertens. 2006;19:80–6.
Tufescu A, Kanazawa M, Ishida A, et al. Combination of exercise and losartan enhances renoprotective and peripheral effects in spontaneously type 2 diabetes mellitus rats with nephropathy. J Hypertens. 2008;26:312–21.
Ito D, Cao P, Kakihana T, et al. Chronic running exercise alleviates early progression of nephropathy with upregulation of nitric oxide synthases and suppression of glycation in Zucker diabetic rats. PLoS One. 2015;10(9):e0138037. https://doi.org/10.1371/journal.
Baria F, Kamimura MA, Aoike DT, et al. Randomized controlled trial to evaluate the impact of aerobic exercise on visceral fat in overweight chronic kidney disease patients. Nephrol Dial Transplant. 2014;29:857–64.
Greenwood SA, Koufaki P, Mercer TH, et al. Effect of exercise training on estimated GFR, vascular health, and cardiorespiratory fitness in patients with CKD: a pilot randomized controlled trial. Am J Kidney Dis. 2015;65:425–34.
Chen IR, Wang SM, Liang CC, et al. Association of walking with survival and RRT among patients with CKD stages 3-5. Clin J Am Soc Nephrol. 2014;9:1183–9.
Sato T, Kohzuki M, Ono M, et al. Association between physical activity and change in renal function in patients after acute myocardial infarction. PLoS One. 2019;14(2):e0212100. https://doi.org/10.1371/journal.pone.0212100.
Séronie-Vivien S, Delanaye P, Piéroni L, et al. Cystatin C: current position and future prospects. Clin Chem Lab Med. 2008;46:1664–86.
Poortmans JR, Gulbis B, De Bruyn E, et al. Limitations of serum values to estimate glomerular filtration rate during exercise. Br J Sports Med. 2012;47:1166–70. https://doi.org/10.1136/bjsports-2012-090976.
Robinson-Cohen C, Littman AJ, et al. Physical activity and change in estimated GFR among persons with CKD. J Am Soc Nephrol. 2014;25:399–406.
JCS Joint Working Group. Guidelines for Rehabilitation in Patients With Cardiovascular Disease (JCS 2012). Circ J. 2014;78:2022–93.
American College of Sports Medicine. In: Riebe D, Ehrman JK, Liguori G, editors. ACSM’s guidelines for exercise testing and prescription. 10th ed. South Holland: Wolters Kluwer; 2018. p. 334–8.
K/DOQI Workshop. K/DOQI clinical practice guidelines dor cardiovascular disease in dialysis patients. Am J Kidney Dis. 2005;45(Suppl 3):S1–S153.
Delgado C, Johansen KL. Barriers to exercise participation among dialysis patients. Nephrol Dial Transplant. 2012;27:1152–7.
Delgado C, Johansen KL. Deficient counseling on physical activity among nephrologists. Nephron Clin Pract. 2010;116:cc336, 330.
Konstantinidou E, Koukouvou G, Kouidi E, et al. Exercise training in patients with end-stage renal disease on hemodialysis: comparison of three rehabilitation programs. J Rehabil Med. 2002;34:40–5.
Wilund KR, Painter P. Formation of an exercise in CKD working group. Am J Kidney Dis. 2016;67(5):812. https://doi.org/10.1053/j.ajkd.2015.12.026.
Krause R, WGRR-European Working Group on Renal Rehabilitation and Exercise Physiology (Affiliated to the ERA-EDTA). Nephrologists’ view on exercise training in chronic kidney disease (results of the questionnaire at the WCN 2003). Clin Nephrol. 2004;61(Suppl 1):S2–4.
Schrag WF, Campbell M, Ewert J, et al. Multidisciplinary team renal rehabilitation: interventions and outcomes. Adv Ren Replace Ther. 1999;6:282–8.
Kohzuki M, Yamagata K, Shibagaki Y et al. (2019) Japanese Society of Renal Rehabilitation. JSRR. http://jsrr.jimdo.com/ (in Japanese).
National Kidney Foundation. KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl. 2012;2:337–414.
Japanese Society of Renal Rehabilitation. Guideline for renal rehabilitation. Renal replacement therapy (in Japanese). Tokyo: Nankodo; 2018. p. 1–87.
Yamagata K, Hoshino J, Sugiyama H, et al. Clinical practice guideline for renal rehabilitation: systematic reviews and recommendations of exercise therapies in patients with kidney diseases. Renal Replace Ther. 2019;5:28.
Williams AD, Fassett RG, Coombes JS. Exercise in CKD: why is it important and how should it be delivered? Am J Kidney Dis. 2014;64:329–31.
Didsbury M, McGee RG, Tong A, et al. Exercise training in solid organ transplant recipients. Transplantation. 2013;95:679–87.
Zelle DM, Klaassen G, van Adrichem E, et al. Physical inactivity: a risk factor and target for intervention in renal care. Nat Rev Nephrol. 2017;13:152–68.
Kohzuki M. Paradigm shift in rehabilitation medicine in the era of multimorbidity and multiple disabilities (MMD). Phys Med Rehabil Int. 2014;1(2):id1006.
Kohzuki M, Sakata Y, Kawamura T, et al. A paradigm shift in rehabilitation medicine: from “adding life to years” to “adding life to years and years to life”. Asian J Human Serv. 2012;2:1–8.
Conflict of Interest
The author declares no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kohzuki, M., Sato, T., Cho, C., Yoshida, N. (2020). Benefit and Risk of Exercise Training in Chronic Kidney Disease Patients. In: Kato, A., Kanda, E., Kanno, Y. (eds) Recent Advances of Sarcopenia and Frailty in CKD. Springer, Singapore. https://doi.org/10.1007/978-981-15-2365-6_4
Download citation
DOI: https://doi.org/10.1007/978-981-15-2365-6_4
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-2364-9
Online ISBN: 978-981-15-2365-6
eBook Packages: MedicineMedicine (R0)