Abstract
Optic disc drusen (ODD) are acellular bodies of hyaline deposits located both intracellularly and extracellularly first described by Muller in 1858 (Muller 1858; Hamann et al. 2018). The main clinical significance of optic disc drusen is that they can simulate true optic disc edema. Misdiagnosing drusen as true disc edema may lead to an extensive, invasive, and unnecessary systemic work-up, including neuroimaging and lumbar puncture. An ODD prevalence of 2.4% has been found in autopsy studies, though it has been reported to be significantly lower using in vivo imaging modalities. The prevalence of ODD is higher in women and involvement is usually bilateral (Lorentzen 1966; Friedman et al. 1975).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
Optic disc drusen (ODD) are acellular bodies of hyaline deposits located both intracellularly and extracellularly first described by Muller in 1858 (Muller 1858; Hamann et al. 2018). The main clinical significance of optic disc drusen is that they can simulate true optic disc edema. Misdiagnosing drusen as true disc edema may lead to an extensive, invasive, and unnecessary systemic work-up, including neuroimaging and lumbar puncture. An ODD prevalence of 2.4% has been found in autopsy studies, though it has been reported to be significantly lower using in vivo imaging modalities. The prevalence of ODD is higher in women and involvement is usually bilateral (Lorentzen 1966; Friedman et al. 1975).
Etiopathogenesis
The pathogenesis of optic disc drusen formation has not been fully determined. The three classical theories on the formation of optic disc drusen postulate that they are caused by a disturbance in axonal metabolism with slowed axoplasmic flow (Tso 1981; Spencer 1978), vascular maldevelopment cause increased transudate release into the intercellular space which in turn acts as a nidus for the formation of ODD (Sacks et al. 1977), or a small scleral canal that physically compresses the optic nerve, causing ganglion cell death, with extrusion and calcification of mitochondria.
Clinical Features
Patients with optic disc drusen are frequently asymptomatic, and optic disc drusen are often discovered incidentally on ophthalmologic examination.
Visual Field Defects
Optic disc drusen are associated with two major types of visual field defects. Axonal loss induced by direct compression or displacement of the fibers by the drusen could lead to arcuate defect or pseudopapilledema and the large protrusion induced by the optic disc drusen leading to an enlargement of the blind spot (Mustonen 1983; Wilkins and Pomeranz 2004; Katz and Pomeranz 2006).
The visual field defects may progress over time; however, it is slow. The prevalence of visual field defect varies greatly between studies: from 75% of patients showing no or minimal visual field defect (Lee and Zimmerman 2005) to 86% of patients showing visual field defects (Mustonen 1983). Such inconsistency may be attributed to the difference in the proportion of various types of ODD, with the highest occurrence in eyes with superficial optic disc drusen (Mustonen 1983; Savino et al. 1979).
Examinations Findings
The appearance of the optic nerve head is usually elevated, when the drusen are superficial they can be easily identified as round deposits with a lumpy bumpy appearance (Fig. 11.1); buried drusen are difficult to appreciate on fundoscopy examination but may sometimes be seen adjacent to vessels or the disc margin with oblique slit lamp illumination. Optic disc drusen are typically buried in the optic disc early in life and become more superficial later (Frisen 2008); therefore, in children, drusen are more likely to be buried and may be more difficult to detect (Erkkila 1977).
Diagnostic Technique
Various ancillary tests, including B-scan ultrasonography, fundus autofluorescence, fluorescein angiography, orbital computed tomography (CT scan), and more recently optical coherence tomography (OCT), have been used to identify optic disc drusen (Mullie and Sanders 1985a, b; Sanders and Ffytche 1967; Pineles and Arnold 2012; Kurz-Levin and Landau 1999).
Fundus Autofluorescence
The autofluorescence characteristic of optic disc drusen (Fig. 11.2) can be helpful as a simple technique; however, it is only seen in superficial drusen and does not reliably detect buried drusen, possibly because of attenuation from overlying tissue. Kurz-Levin and Landau (1999) found that autofluorescence detected over 96% of superficial drusen but only 27% of buried drusen.
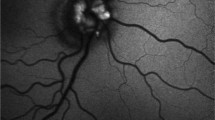
Fluorescein Angiography
Fluorescein angiography may be used to distinguish between optic disc drusen and true optic disc edema (Fig. 11.3a–c). Pineles was able to demonstrate that true disc edema is characterized by early or late disc leakage, while optic disc drusen displayed staining without leakage (Pineles and Arnold 2012).
(a). Early phase fluorescein angiography demonstrating nodular staining of the optic disc drusen. (b) Late phase fluorescein angiography demonstrating nodular staining of the optic discs with no leakage, same patient (a). (c) Late phase fluorescein angiography demonstrating nodular staining of the optic discs with no leakage, same patient (b)
B-scan Ultrasonography
B-scan ultrasonography is considered the gold standard imaging modality to detect optic disc drusen (Kurz-Levin and Landau 1999; Pineles and Arnold 2012; Atta 1988) (Fig. 11.4). Drusen characteristically appear hyperechoic with posterior shadowing on ultrasonography, due to the inherent high reflectivity of calcium. This technique is helpful in detecting buried drusen, but the echogenicity of drusen is dependent on the calcium content which also hampers the ability of CT scans to detect optic disc drusen.
Optical Coherence Tomography
A relatively new modality for imaging optic disc drusen is spectral-domain optical coherence tomography (SD-OCT) and, more recently, enhanced depth OCT. It became possible to image the acellular deposits in the optic nerve head with or without a border of high reflectance of calcification, and evaluate the interplay with other structures (Fig. 11.5a, b) (Heidary and Rizzo 2010; Kulkarni et al. 2014; Silverman et al. 2014).
Complications
Although optic disc drusen are typically considered benign, they may be associated with ocular complications.
Vascular anomalies appear to predispose patients with ODD to central and branch retinal artery occlusion and central retinal vein occlusion. Patients with ODD who suffer with these retinal vascular occlusions tend to be younger than individuals who do not have optic disc drusen. In most cases, these patients also had another systemic risk factor including hypertension, contraceptive use, atrioseptal defect, or migraine (Auw-Haedrich et al. 2002; Gifford 1895).
Choroidal neovascular membrane is also associated with ODD, the neovascular membrane is typically located in the peripapillary region, and is frequently associated with good visual acuity without treatment (Auw-Haedrich et al. 2002; Savino et al. 1979).
Management
If true optic disc edema has been ruled out, patients with asymptomatic optic disc drusen may be observed with serial visual field testing and regular examinations to ensure that treatable complications of ODD are appropriately managed. As the presence of ODD can predispose the patient to glaucomatous optic nerve damage at lower intraocular pressures and glaucoma may coexist with ODD, in the presence of visual field damage, lowering the intraocular pressure should be considered (Samples et al. 1985).
Manage of vascular complications associated with ODD is similar to the management of these disorders in the absence of drusen. Treatment of neovascularization in ODD is not always required as the prognosis is usually good (Samples et al. 1985; Auw-Haedrich et al. 2002).
References
Atta HR. Imaging of the optic nerve with standardised echography. Eye. 1988;2(4):358–66.
Auw-Haedrich C, Staubach F, Witschel H. Optic disk drusen. Surv Ophthalmol. 2002;47(6):515–32.
Erkkila H. Optic disc drusen in children. Acta Ophthalmol. 1977;55(Suppl 129):7–44.
Friedman AH, Gartner S, Modi SS. Drusen of the optic disc. A retrospective study in cadaver eyes. Br J Ophthalmol. 1975;59:413–21.
Frisen L. Evolution of drusen of the optic nerve head over 23 years. Acta Ophthalmol. 2008;86(1):111–2.
Gifford H. An unusual case of hyaline bodies in the optic nerve. Arch Ophthalmol. 1895;24:395–401.
Hamann S, Malmqvist L, Costello F. Optic disc drusen: understanding an old problem from a new perspective. Acta Ophthalmol. 2018;96(7):673–84.
Heidary G, Rizzo JF 3rd. Use of optical coherence tomography to evaluate papilledema and pseudopapilledema. Semin Ophthalmol. 2010;25(5–6):198–205.
Katz BJ, Pomeranz HD. Visual field defects and retinal nerve fiber layer defects in eyes with buried optic nerve drusen. Am J Ophthalmol. 2006;141(2):248–53. https://doi.org/10.1016/j.ajo.2005.09.029.
Kulkarni KM, Pasol J, Rosa PR, Lam BL. Differentiating mild papilledema and buried optic nerve head drusen using spectral domain optical coherence tomography. Ophthalmology. 2014;121(4):959–63.
Kurz-Levin MM, Landau K. A comparison of imaging techniques for diagnosing drusen of the optic nerve head. Arch Ophthalmol. 1999;117(8):1045–9.
Lee AG, Zimmerman MB. The rate of visual field loss in optic nerve head drusen. Am J Ophthalmol. 2005;139(6):1062–6. https://doi.org/10.1016/j.ajo.2005.01.020.
Lorentzen SE. Drusen of the optic disk. A clinical and genetic study. Acta Ophthalmol. 1966;44(Suppl 90):1–180.
Muller H. Anatomische Beitrage zur Ophthalmologie ueber niveau-Veranderungen an der eintrittstelle des Sehnerven. Albrecht von Graefes Arch Klin Exp Ophthalmol. 1858;4:1–40.
Mullie MA, Sanders MD. Scleral canal size and optic nerve head drusen. Am J Ophthalmol. 1985a;99(3):356–9.
Mullie MA, Sanders MD. Computed tomographic diagnosis of buried drusen of the optic nerve head. Can J Ophthalmol. 1985b;20(3):114–7.
Mustonen E. Pseudopapilloedema with and without verified optic disc drusen. A clinical analysis II: visual fields. Acta Ophthalmol. 1983;61(6):1057–66.
Pineles SL, Arnold AC. Fluorescein angiographic identification of optic disc drusen with and without optic disc edema. J Neuroophthalmol. 2012;32(1):17–22.
Sacks JG, O’Grady RB, Choromokos E, Leestma J. The pathogenesis of optic nerve drusen. A hypothesis. Arch Ophthalmol. 1977;95(3):425–8.
Samples JR, van Buskirk M, Shults WT, Van Dyk HJ. Optic nerve head drusen and glaucoma. Arch Ophthalmol. 1985;103(11):1678–80.
Sanders MD, Ffytche TJ. Fluorescein angiography in the diagnosis of drusen of the disc. Trans Ophthalmol Soc U K. 1967;87:457–68.
Savino PJ, Glaser JS, Rosenberg MA. A clinical analysis of pseudopapilledema. II. Visual field defects. Arch Ophthalmol. 1979;97:71–5.
Silverman AL, Tatham AJ, Medeiros FA, Weinreb RN. Assessment of optic nerve head drusen using enhanced depth imaging and swept source optical coherence tomography. J Neuroophthalmol. 2014;34(2):198–205.
Spencer WH. Drusen of the optic disk and aberrant axoplasmic transport. The XXXIV Edward Jackson memorial lecture. Am J Ophthalmol. 1978;85(1):1–12.
Tso MO. Pathology and pathogenesis of drusen of the optic nerve head. Ophthalmology. 1981;88:1066–80.
Wilkins JM, Pomeranz HD. Visual manifestations of visible and buried optic disc drusen. J Neuroophthalmol. 2004;24(2):125–9.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Peres, N.J.P. (2020). Optic Disc Drusen. In: Rodrigues, E., Meyer, C., Tomazoni, E. (eds) Trauma and Miscellaneous Disorders in Retina. Retina Atlas. Springer, Singapore. https://doi.org/10.1007/978-981-13-8550-6_11
Download citation
DOI: https://doi.org/10.1007/978-981-13-8550-6_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-8549-0
Online ISBN: 978-981-13-8550-6
eBook Packages: MedicineMedicine (R0)