Abstract
The components of the hepatic vascular system (hepatic arteries, portal and hepatic veins, sinusoids, and lymphatics) can be damaged by various injuries. Although vascular diseases in the liver are rare conditions, parts of these disorders lead to portal hypertension, hepatic failure, cirrhosis, and hepatocellular carcinoma. The progress of imaging modalities can make the diagnosis for hepatic vascular disorders easier. Imaging plays a crucial role in the early detection and assessment of the extent of hepatic vascular disorders. This article concisely reviews the classification, etiology, pathophysiology, and clinical presentation of hepatic vascular disorders and provides a detailed description of imaging and treatment options, particularly interventional management.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Budd-Chiari syndrome
- Hepatic vein thrombosis
- Idiopathic membranous obstruction of inferior vena cava
- Fontan-associated liver disease
- Sinusoidal obstruction syndrome
- Veno-occlusive disease
- Arterioportal fistulas
- Idiopathic non-cirrhotic portal hypertension
- Portal vein thrombosis
- Extrahepatic portal venous obstruction
- Pylephlebitis
- Portal vein aneurysm
- Hereditary hemorrhagic telangiectasia
- Osler-Weber-Rendu disease
- Peliosis hepatis
- Portal cavernoma
- Hepatocellular carcinoma
- Portal hypertension
11.1 Introduction
The liver has a dual blood supply: 60–70% from portal vein and 30–40% from hepatic artery. Arterioportal mixed blood in sinusoids streams to terminal hepatic veins from the periportal zone, and the venous blood collected in three hepatic veins is carried to inferior vena cava and right-sided atrium. Vascular disorders of the liver can be classified into three groups, the impairments of blood flow into (prehepatic), through (intrahepatic), or from (posthepatic) the liver (Table 11.1, Fig. 11.1). Then disturbance of blood flow in cardiovascular system (acute or chronic heart failure), hepatic veins or arteries, portal veins, and sinusoids must affect liver function, and these vascular lesions are closely associated with development of acute and chronic liver diseases. This chapter describes liver disorders caused by abnormal stream or obstruction of hepatic artery, portal or hepatic veins, and sinusoids.
Schematic representative of the anatomic classification of hepatic vascular disorders. Hepatic vascular disorders can be classified into prehepatic, intrahepatic (presinusoidal, sinusoidal, postsinusoidal), and posthepatic lesions. APF arterioportal fistula, BCS Budd-Chiari syndrome, CV central vein, EHPVO extrahepatic portal venous obstruction, FALD Fontan-associated liver disease, HA hepatic artery, HHT hereditary hemorrhagic telangiectasia, HV hepatic vein, INCPH idiopathic non-cirrhotic portal hypertension, IVC inferior vena cava, PV portal vein, PVT portal vein thrombosis, RA right atrium, SMV superior mesenteric vein, SV splenic vein
11.2 Hepatic Veins
The hepatic venous flow begins in terminal hepatic veins; drains into the intercalated veins, from there into the collecting veins and truncal veins; and reaches the inferior vena cava. Congestive cardiac failure (acute or chronic type), stenosis or obstruction of inferior vena cava, hepatic vein thrombosis, veno-occlusion, and endophlebitis obliterans cause acute or chronic liver disease and cirrhosis.
11.3 Budd-Chiari Syndrome (BCS)
Budd-Chiari Syndrome [1,2,3,4] is a rare disease with an estimated prevalence of 1/100,000 [5] and is a disorder caused by obstruction of hepatic veins and inferior vena cava (IVC). Primary BCS is due to endoluminal venous lesions such as thrombus or web. Secondary BCS is due to a lesion outside the venous system such as tumor, abscess, or cysts. Obstruction of a single hepatic vein out of three hepatic veins is clinically silent. The obstruction of 2–3 hepatic veins induces hepatic dysfunction and becomes symptomatic. According to the location of obstruction, BCS is classified into three types: pure obstruction of hepatic veins, pure obstruction of IVC, and combined obstruction of hepatic veins and IVC. Clinical manifestations are characterized by abdominal pain, edema, ascites, jaundice, hepatomegaly, hepatic encephalopathy, variceal bleeding, and/or formation of collateral circulation pathways in abdominal and chest walls. However, they vary according to whether the disorder is acute, subacute, or chronic [6].
On etiology, the primary BCS is associated with hypercoagulable states leading to vascular thrombosis and develops from hereditary conditions such as Factor V Leiden, protein C, S, or antithrombin deficiency [7]. Pregnancy and estrogen intake can promote or trigger BCS especially in the presence of an underlying risk factor of thrombosis. The secondary BCS is associated with invasion or extrinsic compression of the hepatic veins and/or IVC. Causes of vascular compression are a pyogenic infectious process, amoebas, hydatid disease or echinococcosis, and benign and/or malignant tumors. Idiopathic membranous obstruction of IVC (MOVC) is frequently seen in South Africa [8], India [9], Nepal [10], and Japan [11].
The clinical diagnosis of BCS can be accurately assessed with imaging modalities. Color Doppler ultrasonography (CDUS) [12] is a noninvasive technique and has high sensitivity and specificity. Typical findings are absence of flow or flat wave form without fluttering as against a triphasic pattern observed in patent hepatic vein. Small and tortuous intrahepatic or subcapsular collaterals are seen in about 80% patients. Abdominal computed tomography (CT) and magnetic resonance imaging (MRI) are also used as diagnostic tools. Triple-phase CT [13] shows the absence of hepatic vein opacity and a mottled appearance along with late enhancement of the hepatic periphery. MRI [13] is helpful for visualizing the entire length of IVC or intrahepatic collaterals and for differentiating acute from subacute or chronic BCS. In acute form, post-contrast MR show decreased T1 signal intensity and heterogeneously increased T2 signal intensity in the hepatic periphery. In the chronic form, T1 and T2 signal intensity are decreased on unenhanced MR imaging due to hepatic fibrosis. Noninvasive imaging modalities are sufficient for the diagnosis of BCS at most cases. However, if inadequate, venography and liver biopsy should be performed. Venograohy [13] is a useful modality for assessing extension and location of obstruction and measuring hepatic venous pressure.
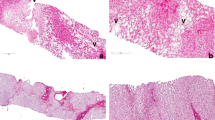
Liver biopsy is not required to confirm BCS and insufficient to assess the severity of BCS due to sampling errors but is useful for the differential diagnosis of veno-occlusive disease. As histologic findings in BCS have previously been described [14,15,16], zone 3 sinusoidal congestion and dilatation may be the only findings in the early stage. Centrilobular fibrosis and nodular regenerative hyperplasia may develop over time in chronic stage and may lead to cirrhosis.
Laparoscopy is a useful tool in the diagnosis of BCS, but only a few reports have described macroscopic findings in the liver [17]. We describe the laparoscopic appearance of the liver in BCS with MOVC to clarify the macroscopic features associated with liver histology.
Treatment depends on the causes, anatomic location, extent of thrombotic process, and functional capacity of the liver. The primary goal of the treatment is relieving hepatic venous outflow obstruction and improving liver perfusion, leading to preserve functioning hepatocytes. It is divided into medical treatment, including anticoagulation and thrombolysis, interventional procedures such as angioplasty and transjugular intrahepatic portosystemic shunt (TIPS), and surgical interventions including orthotopic or living donor liver transplantation. BCS should manage stepwisely [18, 19]. The first-line treatment is medical therapy which uses heparin or vitamin K antagonist. The second step is percutaneous transluminal angioplasty for patients with short-length stenosis of either the hepatic veins or IVC. TIPS is the third step in patients not responding to medical therapy and without response to or stenosis unsuitable for angioplasty/stenting. A transcaval approach has been found to be successful in most patients using covered stents [20]. The last step is liver transplantation. The remaining 10–20% of patients with BCS treated with a stepwise management strategy need rescue transplantation. A large series of transplanted patients have shown 5-year survival rates of up to 80% [21].
We present four cases of acute (case 11.1), subacute (case 11.2), and chronic BCS (cases 11.3 and 11.4) including the clinical manifestations, image analyses, and liver histology results with or without macroscopic findings to derive an accurate diagnosis. The clinical signs and symptoms may be caused either by a large, sudden blockage of hepatic veins or by portal hypertension due to differentiate chronic BCS from liver cirrhosis. Therefore, cirrhotic patients with negative hepatitis B and C tests should be examined by US, CT, and MRI to detect obstruction of IVC or thrombus in hepatic veins. In subacute phase, sinusoids become collagenized, and hepatocytes become atrophic and are lost. In chronic BCS, small hepatic veins disappear as they are incorporated into septa that eventually link hepatic veins to form cirrhosis with relative sparing of portal triads, also known as reversed lobulation cirrhosis or venocentric cirrhosis.
Acute BCS is associated with various conditions, including malignancy, myeloproliferative disorders, infection, pregnancy, oral contraceptives, Bechet’s disease, and hypercoagulable state. The patient described in case 11.1 had leukocytosis, high transaminase levels, and prolonged prothrombin time; he rapidly developed hepatic failure. High serum aminotransferase levels are considered ominous in acute BCS. Hypercoagulable state after operation might cause the thrombosis of IVC or hepatic veins and pulmonary artery, leading to respiratory and hepatic failure. Autopsy of the liver in case 11.1 showed massive hemorrhagic necrosis in zones 2 and 3.
Case 11.1
A 44-year-old male had surgery for a herniated cervical disc and was on complete bed rest for 1 week. He experienced vertigo upon standing and was in shock. He had no history of autoimmune, myeloproliferative, or infectious disease and had not taken any hormonal drugs. His serum and blood examination showed TBIL 2.1 mg/dL, SGOT 1250 KU, SGPT 1130 KU, PT 13%, PLT 5.7 × 104/μL, total cholesterol 169 mg/dL, WBC 30,600/mm3, and serum creatinine 3.8 mg/dL. He developed hepatic failure, and abdominal US revealed thrombus in IVC (Fig. 11.2). He was transferred to the intensive care unit. CT revealed high-density material in IVC at the hepatic vein ostia (Fig. 11.3), and acute BCS was diagnosed. Anticoagulants were administered, and plasmapheresis and hemodialysis were initiated. However, he died from multiorgan failure due to a hypercoagulable state. Autopsy showed massive hemorrhagic necrosis in zones 2 and 3, while hepatocytes in zone 1 remained intact (Fig. 11.4). Thrombus was seen in the pulmonary artery, along with microthrombi in the adjacent small arteries and hemorrhage in surrounding tissues.
Case 11.2
A 37-year-old male had complained of leg edema for 6 months and developed epigastralgia and brown urine. On admission, his laboratory data were TBIL 2.1 mg/dL, SGOT 32 IU/L, SGPT 37 IU/L, ALP 13.9 KAU, total cholesterol 138 mg/dL, PLT 11.1 × 104/μL, and ICGR15 38.5%. Enhanced serial CT showed disappearance of IVC, presence of a thrombus in the IVC, dilated collateral veins, and enlarged caudate lobe (Fig. 11.5). Simultaneous inferior and superior venocavography showed a complete obstruction of the IVC and at the entry of the right and middle hepatic veins into the IVC (Fig. 11.6). Laparoscopy revealed enlarged liver with a dusky green color, and blue maculae and white markings were detected on the surface; numerous lymphatic cysts were seen, and small amount of ascites were present in the abdominal cavity; and laparoscopy-guided liver biopsy revealed a dilated portal vein and increasing fibrosis in the portal tract, and congestion was seen around the central vein (Fig. 11.7).
CT in subacute BCS with MOVC. Serial CT shows IVC (arrow) as a low-density or high-density area, and thrombus is seen in IVC. Collateral vein (arrow head) is next to thoracic or abdominal aortic artery. (Redrawn from Iwai M, et al. Clinical features, image analysis, and laparoscopic and histological liver findings in Budd-Chiari syndrome, Hepato-Gastroenterol 1998; 45: 2359–68)
Simultaneous superior and inferior venocavography. IVC is obstructed in right subatrium, and right and middle hepatic veins drain into IVC. (Redrawn from Iwai M, et al. Clinical features, image analysis, and laparoscopic and histological liver findings in Budd-Chiari syndrome, Hepato-Gastroenterol 1998; 45: 2359–68)
Macroscopic and histological findings of liver in subacute BCS with MOVC. (a) Greenish liver is enlarged, white markings are visible with blue maculae, and numerous lymphatic vesicles are visible on liver surface. (b) Hematoxylin eosin stain shows congestion around central vein, and portal tract is enlarged. C central vein, P portal tract
Case 11.3
The chest radiograph of an asymptomatic 42-year-old male showed the shadow of an enlarged azygos vein in the right paratracheal area (Fig. 11.8). His liver chemistries were TBIL 1.0 mg/dL, SGOT 19 IU/L, SGPT 19 IU/L, ALP 9.4 KAU, total cholesterol 123 mg/dL, PLT 11.0 × 104/μL, and ICGR15 23.5%. BCS was suspected. Superior and inferior venocavography showed complete obstruction of IVC and drainage of the right hepatic vein into IVC. Serial enhanced CT showed the presence of left, middle, and right hepatic veins. The right hepatic vein communicated with the IVC, but the connection of the middle and left hepatic veins with the IVC was not clear; the lumen of the IVC in the hepatic vein ostia was narrow, the post-occlusion portion of IVC was dilated, and dilated collateral veins were also seen (Fig. 11.9). Laparoscopy revealed enlarged, purplish liver with white markings and dilated peripheral portal veins, while liver biopsy revealed capsular thickening and subcapsular hemorrhage; the sinusoids were dilated and congested in the subcapsular area (Fig. 11.10). Routine chest radiograph showed the shadow of a dilated azygos vein, and this finding could be a valuable tool in the diagnosis of BCS [16].
Serial enhanced CT in BCS. Narrowing of IVC is seen at hepatic vein ostia. Middle and left hepatic veins are visible, but there is no clear communication between both veins and IVC. Entry of right hepatic vein into IVC is visible, and IVC is dilated distant to occlusion. Azygos vein is dilated, and other collateral veins are seen. (Redrawn from Iwai M, et al. Clinical features, image analysis, and laparoscopic and histological liver findings in Budd-Chiari syndrome, Hepato-Gastroenterol 1998; 45: 2359–68)
Macroscopic and microscopic appearance of liver in an asymptomatic BCS patient. (a) Surface of enlarged liver is purplish red in color with white markings, and dilated peripheral portal veins are visible. (Redrawn from Iwai M, et al. Clinical features, image analysis, and laparoscopic and histological liver findings in Budd-Chiari syndrome, Hepato-Gastroenterol 1998; 45: 2359–68). (b) Histological appearance of the liver shows capsule of liver surface (arrow) to be thick, and subcapsular hemorrhage (H) is visible. Mallory-Azan stain shows peliosis (P) communicates with subcapsular hemorrhage
Case 11.4
A 66-year-old male with a 3-year history of liver cirrhosis underwent enhanced CT, which showed a thrombus in the hepatic portion of IVC. BCS was the suspected diagnosis. The sagittal view of his abdominal MRI showed obstruction of IVC, entry of right hepatic vein into IVC, and high-intensity thrombus in the hepatic vein ostia; MRI angiography revealed stenosis of IVC and dilated collateral veins communicating with the femoral vein (Fig. 11.11). Simultaneous inferior and superior venocavography showed obstruction at the hepatic vein ostia, nozzle-like tapering of IVC from the right atrium, and entry of right hepatic vein into IVC. Laparoscopy showed liver atrophy with formation of multiple nodules, capsular thickening, and numerous lymphatic cysts; the nodules were low in height, internodular space was wide, and scattered subcapsular hemorrhages were visible (see Fig. 4.9 in Chap. 4). Liver biopsy showed pseudolobular formation with wide septum of fibrosis, capsular thickening, and subcapsular hemorrhage; hemorrhaging was evident in the interspace between parenchymal cells and septal fibrosis in the portal area, and dilated portal veins were surrounded by increased fibrosis (Fig. 11.12).
MRI in chronic BCS with MOVC. (a) Sagittal MRI shows obstruction of IVC (arrow), entry of right hepatic vein into IVC, and highly intense thrombus (star) in hepatic vein ostia. (b) MRI angiography shows obstruction of IVC (arrow) in hepatic vein ostia, entry of right hepatic vein in IVC, and formation of collateral circulation. (Redrawn from Iwai M, et al. Clinical features, image analysis, and laparoscopic and histological liver findings in Budd-Chiari syndrome, Hepato-Gastroenterol 1998; 45: 2359–68)
Mallory-Azan stain of liver in chronic BCS. Thick capsule and subcapsular hemorrhage are visible. Hemorrhage is also visible around portal fibrosis. There is pseudolobular formation, and wide septum formation is seen between regenerating nodules. Portal veins are dilated, and lumen of central veins (arrow) is narrow. (Redrawn from Iwai M, et al. Clinical features, image analysis, and laparoscopic and histological liver findings in Budd-Chiari syndrome, Hepato-Gastroenterol 1998; 45: 2359–68)
11.4 Fontan-Associated Liver Disease (FALD)
In 1971, Fontan and Baudet reported an effective palliative operation for tricuspid atresia, and it is currently the most common surgical procedure performed in patients with single-ventricle physiology or when biventricular repair is not feasible. Advances in perioperative management have contributed to an improved outcome of the Fontan operation and an increase of long-term survivors. Venous congestion and decreased cardiac output are the hallmarks of Fontan circulation, and then it is rational that long-term survivors of Fontan surgery commonly progress to congestive hepatopathy [22]. FALD can be defined as abnormalities in liver structure and function that result from the Fontan circulation. FALD arises due to chronic congestion of the liver created by the elevated venous pressure and low cardiac output. Main pathologic features are massive or universal sinusoidal dilatation, centrilobular and /or sinusoidal fibrosis, and cardiac cirrhosis [23].
Elevated hepatic venous pressure due to Fontan circulation may diminish portal flow, and portal vein saturation can be decreased by the hepatic arterial buffering response. These changes may promote the development of focal nodular hyperplasia (FNH), since it arises secondary to arterial hyperperfusion. Recently, hepatocellular carcinoma (HCC) after Fontan operation has been reported [24]. There is a well-documented multistep process of progression to hepatocellular carcinoma. A subgroup of hyperplastic nodules may have malignant potential. The development of HCC gives a great impact for the prognosis of patients with FALD.
Noninvasive imaging modalities are useful for detecting FALD [25]. US can identify in liver parenchymal changes (parenchymal heterogeneity, liver surface irregularity), cirrhotic findings (hepatomegaly, splenomegaly, ascites), and liver tumors. CT and MRI can demonstrate IVC engorgement, hepatic vein dilatation, and hypervascular tumors. Hepatic elastography is a noninvasive tool for assessing hepatic fibrosis and hepatic congestion. Because it is not able to determine the true hepatic fibrosis excludes the effect of hepatic congestion, we should keep in mind that the elastography may overestimate hepatic fibrosis. Increased central venous pressure has been shown to be associated with increased morbidity and mortality in patients undergoing Fontan procedure. All Fontan patients should undergo the surveillance for FALD and HCC.
Case 11.5
This case was a 31-year-old man who was referred to our division for evaluation of liver nodules detected on US. He had undergone the Fontan procedure for a single ventricle at the age of 10 years, which was his second operation for congenital heart disease. He had also received insertion of a permanent pacemaker for sick sinus syndrome. When liver cirrhosis and esophageal varices were diagnosed at the age of 29 years, he was on treatment with diuretics, antiarrhythmic agents, and antithrombotic drugs, with his cardiac status being NYHA class III. On admission, he was cyanotic and showed poor growth with a reduced exercise capacity. He had moderate ascites and a pleural effusion. Laboratory tests revealed a hemoglobin 11.7 g/dL, platelet count 13.2 × 10,000/μL, AST 38 IU/L, ALT 21 IU/L, T-bil 1.8 mg/dL, and albumin 3.3 mg/dL. Serum AFP level was 4.0 ng/mL. US showed characteristic features of cirrhosis and several nodules ranging in size from 10 to 35 mm that were suspected to be regenerative nodules or FNH. CT demonstrated diffuse patchy enhancement of the hepatic parenchyma, as well as hypervascular nodules ranging from 10 to 35 mm in size (Fig. 11.13a). Most of the nodules displayed enhancement in the arterial phase and contrast retention in the portal venous phase, which are characteristics consistent with FNH. However, the 23 mm mosaic pattern nodule with a halo in S2 showing early arterial uptake followed by washout in the portal venous phase was suspected of hepatocellular carcinoma (Fig. 11.13b). Liver biopsy was contraindicated due to ascites and anticoagulant therapy. One year and a half later, follow-up imaging showed enlargement of the suspected hepatocellular carcinoma from 23 to 35 mm in diameter, while the other nodules were unchanged in size. The serum AFP level remained in the normal range. This patient died of combined hepatic and cardiac failure.
CT in a patient with FALD and HCC. (a) CT demonstrated diffuse patchy enhancement of the hepatic parenchyma, as well as hypervascular nodules ranging from 10 to 35 mm in size. (b) The 23 mm mosaic pattern nodule with a halo in S2 showing early arterial uptake followed by washout in the portal venous phase was suspected of hepatocellular carcinoma (arrowheads)
11.5 Sinusoidal Obstruction Syndrome (SOS)/Veno-Occlusive Disease (VOD)
Sinusoidal obstructive syndrome (SOS) known as veno-occlusive disease (VOD) is a condition characterized by toxic destruction of hepatic sinusoidal endothelial cells with sloughing and downstream occlusion of terminal hepatic venules. Initially, VOD was well-established as a hepatic complication by either chemical or radiation. In the 1970s, hepatic VOD in patients undergoing bone marrow transplantation was reported. A large number of drugs and toxins have been associated with SOS/VOD. Causal factors include hematopoietic stem cell transplantation, adjuvant or neoadjuvant chemotherapy with hepatectomy for metastatic liver diseases, radiation (total body or hepatic) chemotherapy for acute leukemia, liver transplantation, use of herbal remedies, and VOD with immunodeficiency. The presentation mimics BCS. In its acute form, presentation may include hepatomegaly, ascites, and liver failure. The chronic form leads to cirrhosis and portal hypertension with esophageal varices. Liver biopsy typically shows striking centrilobular congestion around the hepatic venule with centrilobular hepatocellular necrosis in acute phase (Fig. 11.14). The terminal hepatic venules exhibit subintimal edema without obvious fibrin deposition or thrombosis. This is accompanied by dissection of erythrocytes into the space of Disse and downstream accumulation of cellular debris in the terminal vein. In the subacute phase, collagen deposition occurs in and around the terminal venules, resulting in progressive obliteration of the venule. In the chronic phase, dense perivenular fibrosis radiating out into the parenchyma develops [26]. Currently, no effective therapy is available other than to remove the etiologic agent, typically a drug. As a medical treatment, defibrotide has shown the most promising results in clinical trials, which showed 32% of patients who underwent hematopoietic stem cell transplantation (HSCT) achieved complete response [27]. High-dose methylprednisolone has also been used. Liver transplantation should be considered only in patients who are expected to have a good outcome [28]. The prevention is needed for patients at high risk for developing SOS. Ursodeoxycholic acid or low-dose heparin prophylaxis and aggressive fluid management during HSCT are available.
Sinusoidal obstruction syndrome. (a) Periodic acid Schiff’s stain in SOS shows zone 3 hepatocytes have been replaced by blood cells. A small vein contains macrophages and fibrous tissue. (b) Hematoxylin eosin stain shows loss of hepatocytes around the hepatic vein in SOS. (Courtesy of Professor Michael A Kern)
11.6 Hepatic Artery
Forty to 50% of the oxygen requirement and 35% of the blood volume of the liver are supplied by hepatic artery. The common hepatic artery continues as the proper hepatic artery and branches into the right and left hepatic artery. Clinical disorders of the hepatic artery are aneurysm [25], occlusion or infarction [26], and arteriovenous fistula [27, 28]. Some of these diseases should be diagnosed immediately to prevent circulatory insufficiency and liver failure by using image analysis of US, CT with contrast medium, and angiography.
11.7 Arterioportal Fistulas (APFs)
APFs are fistulas between any of the splanchnic arteries and the portal veins and represent an infrequent cause of presinusoidal portal hypertension. They can be acquired or congenital. Acquired APFs can be by liver trauma, interventional procedures (liver biopsy, percutaneous transhepatic catheterization of bile duct, radiofrequency ablation, etc.), artery aneurysm, and hepatic tumors (hepatocellular carcinoma). Many patients with APF are asymptomatic. Symptoms depend on the location of APF and the amount of shunted blood. They are usually secondary to portal hypertension. Common manifestations include gastrointestinal bleeding, ascites, congestive heart failure, and diarrhea. The pathologic features of APFs are the dilatation of the sinusoids and portal branches in the early stage and venous intimal hyperplasia and arterialization of the portal branches, called hepatoportal sclerosis after persistent portal hypertension. Doppler US is the first-choice tool for the diagnosis or a screening of APFs. Doppler US demonstrates pulsatile flow in the portal system with or without hepatofugal flow. On triple-phase enhanced CT, the early filling of the portal vein and the presence of wedge-shaped, transient peripheral enhanced area are observed in the arterial phase. Hepatic arteriography reveals early visualization of the portal system after celiac or hepatic artery injection. Superior mesenteric arteriovenous fistulas (SMAVF) are usually caused by iatrogenic or traumatic damage, though a few congenital cases have also been reported [29, 30]. Fistula formation originates from a transfixion suture through the artery and vein simultaneously or via mass ligation in the mesentery [31, 32]. Some patients with SMAVF have suffered cardiac failure or liver failure [33, 34]. Treatment indication is to prevent the development of portal hypertension. Extrahepatic APFs should be treated because of no spontaneous closure of APFs. Arterial embolization is effective in treating single or a few APFs. Next options are hepatic artery ligation or fistula resection. Liver transplantation may be the last possible therapy in patients with extensive involvement, especially congenital multiple APFs.
We present a case of SMAVF occurring after small bowel resection to treat an ileus.
Case 11.6
A 38-year-old woman was admitted for watery and bloody diarrhea and abdominal distension for several weeks. She had undergone a wide resection of the small bowel to relieve intestinal obstruction 6 years earlier. Physical examination revealed massive ascites, and a bruit was audible in the periumbilical area. On admission, her heart rate was 98/min, and blood pressure was 110/70 mmHg. Her hemoglobin level was 10.6 g/dL and hematocrit 33.2%. Liver chemistries revealed TBIL 0.6 mg/dL, GOT 34 IU/L, GPT 34 IU/L, TP 6.7 g/dL, and gamma globulin 11.5%. US examination revealed massive ascites, dilated intrahepatic and extrahepatic portal veins, and “rabbit tail” appearance of the superior mesenteric vein communicating with some vessels (Fig. 11.15). Conventional enhanced CT showed a dilated portal vein in parallel with the superior mesenteric artery, and the bowel wall was enhanced by contrast medium (Fig. 11.16); a connection between the portal vein and superior mesenteric artery was suspected. Superior mesenteric arteriography revealed a fistula of the dilated mesenteric vein, with its artery at the level of the fourth lumbar vertebra (Fig. 11.17). Hematochezia was frequent, and hematemesis occurred due to rupture of esophageal varices. Cardiac output was measured via isotope dilution, and the cardiac index was 7.78 L/mm/m2. Cardiac failure occurred, and blood urea nitrogen and creatinine were elevated to 85 and 4.7 mg/dL, respectively. The fistula between the superior mesenteric artery and vein was ligated as an emergency procedure. The pressure in the superior mesenteric vein before and after ligation was 56 and 47 mmHg, respectively. No regenerating nodules were seen on the liver surface, and a wedge biopsy of the liver showed arteriolized portal veins surrounded by increasing fibrosis (Fig. 11.18). Neither septum nor pseudolobular formation was seen.
US in SMAV fistula. (a) The extrahepatic and intrahepatic portal vein (P) is dilated. (b) The superior mesenteric vein (V) is dilated and is connected to a stenotic vessel. (Reuse of Iwai M, et al. Iatrogenic superior mesenteric arteriovenous fistula: Ultrasonographic, CT and angiographic features and histological findings of the liver biopsy. J Gastroenterol Hepatol 1990; 5: 586–9, with permission of Wiley)
Enhanced CT in SMAV fistula. The dilated superior mesenteric vein is contiguous to the superior mesenteric artery (a), and the vein makes a fistula with the artery (b). The small intestine is enhanced by contrast medium. (Reuse of Iwai M, et al. Iatrogenic superior mesenteric arteriovenous fistula: Ultrasonographic, CT and angiographic features and histological findings of the liver biopsy. J Gastroenterol Hepatol 1990; 5: 586–9, with permission of Wiley)
SMAV fistula. Superior mesenteric arteriography shows a fistula of the dilated mesenteric vein. (Reuse of Iwai M, et al. Iatrogenic superior mesenteric arteriovenous fistula: Ultrasonographic, CT and angiographic features and histological findings of the liver biopsy. J Gastroenterol Hepatol 1990; 5: 586–9, with permission of Wiley)
SMV fistula. Liver histology shows deposition of collagen fibers (CF) surrounding the portal vein (PV). A artery, B bile duct. (Reuse of Iwai M, et al. Iatrogenic superior mesenteric arteriovenous fistula: Ultrasonographic, CT and angiographic features and histological findings of the liver biopsy. J Gastroenterol Hepatol 1990; 5: 586–9, with permission of Wiley)
11.8 Portal Vein
Portal vein is formed by gastric or pyloric and superior or inferior mesenteric and splenic veins. The portal vein divides into left and right branch, and the branch reaches interlobular veins and interlobular venules and continues into afferent venules and into sinusoids.
There are congenital or acquired diseases of portal veins, and their diseases cause portal hypertension. Portal hypertension arises due to obstruction of hepatic blood flow, and patients with portal hypertension are classified as having either presinusoidal or postsinusoidal obstruction. Congenital anomalies of the portal vein, portosystemic shunts, or arterioportal fistula cause portal hypertension, and acquired diseases of large or small portal veins (idiopathic portal hypertension) lead to liver disturbance with or without cirrhotic change.
11.9 Idiopathic Non-cirrhotic Portal Hypertension (INCPH)
Idiopathic non-cirrhotic portal hypertension has been recently proposed to replace terms, for example, hepatoportal sclerosis, idiopathic portal hypertension, and so on [35]. INCPH is defined as a presinusoidal non-cirrhotic portal hypertension of unknown etiology with a patent extrahepatic portal vein and hepatic veins. Anemia, thrombocytopenia, and esophageal or gastric varices are clinically manifested, and splenomegaly is always detected. Liver biopsy should be performed for the diagnosis of INCPH. Pathological features are (1) obliterative portal venopathy, (2) portal fibrosis without inflammation, (3) paraportal shunting vessels, (4) enlarged portal branches, and (5) increased number of portal vascular channels [36, 37].
The diagnosis of INCPH is based on the portal hypertension with patent portal and hepatic veins in the absence of known causes of liver damage. In patients with INCPH, hepatic synthetic capacity is usually preserved. Imaging modalities have poor sensitivity and specificity. These modalities demonstrated portal hypertension findings such as splenomegaly, collateral shunts, and enlarged caudate lobe. US shows thickened PV with echogenic walls, normal liver size, and normal echotexture.
Variceal bleeding is a life-threatening complication [38], and combined pharmacological and endoscopic therapy is effective to control acute bleeding [39]. Endoscopic variceal ligation [40] and transjugular intrahepatic portosystemic shunt [41] are applied for prophylaxis of bleeding, and balloon-occluded retrograde transvenous obliteration is indicated to prevent gastric variceal bleeding [42]. The natural course of INCPH is good except for uncontrolled gastrointestinal bleeding. Long-term survival after eradication of esophagogastric varices is nearly 100% [43]. Hepatic reserve usually remains well preserved, but 20% of patients develop parenchymal atrophy with subsequent decompensation.
Case 11.7
A 58-year-old female complained of melena and was found to have anemia. Her liver test showed AST 23 IU/L, ALT 18 IU/L, ALP 495 IU/L, GGT 73 IU/L, and PLT 11.7 × 104/μL. Upper abdominal CT with contrast medium showed esophageal varices in the venous phase, and another slice of CT revealed splenomegaly and development of a collateral portal vein around the stomach (Fig. 11.19). Upper gastrointestinal fiberscope showed esophageal varices with RC sign. Three-dimensional CT showed presence of esophageal varices, collateral portal branch around the stomach, and splenomegaly (Fig. 11.20). Liver biopsy showed non-cirrhotic liver, bile ducts and artery in a portal tract, and herniated portal vein (Fig. 11.21). Thrombocytopenia and anemia are found in idiopathic portal hypertension, and hematemesis or melena develops. Histological findings show non-cirrhotic liver, narrow lumen or destruction of the portal vein, and herniation of the portal vein.
Case 11.8
A 53-year-old female was diagnosed with esophageal varices. Her liver function tests showed ALT 14 IU/L, AST 21 IU/L, LDH 303 IU/L, gamma globulin 23.3%, and ICGR15 9.8%. Neither HBsAg nor HCV Ab were present. Her thrombocyte level was 6.1 × 104/μL. US revealed splenomegaly with collateral vein formation, and splenectomy was performed to reduce portal hypertension. MRI revealed dilatation of the portal trunk and tapering of the intrahepatic portal veins. Regenerating hyperplastic nodules were laparoscopically seen on the liver surface, but no cirrhotic nodules were detected, and liver biopsy showed portal fibrosis and dilated peripheral portal veins with herniated abnormal vessels (Fig. 11.22).
11.10 Portal Vein Thrombosis (PVT)
Portal vein thrombosis refers to thrombosis that develops in the portal trunk including its right and left branches and extends to the splenic or superior mesenteric veins [44]. The pathogenesis of PVT is reduced portal flow, a hypercoagulable state and vascular endothelial injury. Etiology of PVT is cirrhosis, primary hepatobiliary malignancy, secondary hepatobiliary malignancy, abdominal infection including pancreatitis and cholangitis, and a myeloproliferative disorder. Cirrhosis is associated with increased intrahepatic vascular resistance and reduced portal flow, leading to venous stasis. Levels of both pro- and anticoagulant factors are reduced in cirrhosis. Its balance may often tilt toward hypercoagulability in cirrhotic patients. Bacterial translocation and endotoxemia lead to portal endothelial injury and the activation of coagulation cascade. Cirrhotic patients are higher risky due to these three pathogeneses.
On the diagnosis of PVT [45], US is the first-choice diagnostic modality. It shows hypo (recent thrombus)-, iso-, or hyperechoic (elderly) material within portal vein either filling the lumen partially or completely. Color Doppler US and contrast-enhanced US allow the diagnosis of an occlusion of the veins by an elimination of the flow signal. They can reveal collateral flows such as in a portal cavernoma, which is multiple tortuous small vessels with hepatopetal flow or varices. Enhanced CT shows a bland thrombus as a low density, non-enhancing defect within portal veins. CT and MRI can provide additional information such as extension of thrombus, collaterals, differentiation from tumor thrombus, and status of adjacent organs. The variations of T1- and T2-weighted signals allow defining the age of thrombus formations. The increase of both signal intensity is due to fresh thrombus. The aim of the treatment is to reverse or prevent advancement of PVT. Anticoagulation therapy should be initiated with heparin or low molecular weight heparin and maintained 2–3 weeks [46]. Later, oral vitamin K antagonists should be given to maintain an INR of 2–3. Thrombolytic therapy with recombinant tissue plasminogen activator, urokinase, for very fresh PVT can be done via indirect intra-arterial infusion into the superior mesenteric artery or directly into portal vein and might improve regional clot lysis. However, there is a high rate of bleeding.
Extrahepatic portal venous obstruction (EHPVO) refers to chronic portal obstruction in the absence of associated liver disease [47]. EHPVO should be considered as a separate entity. Etiology of EHPVO in children is infection, congenital anomaly, or a primary thrombotic disorder. Infections include omphalitis, neonatal umbilical sepsis, repeated abdominal infection, or umbilical vein catheterization. However, 50% of patients still remain idiopathic. EHPVO in adult is due to prothrombotic disorders, intra-abdominal infection, pregnancy, or oral contraceptives.
Case 11.9
A 21-year-old female using low-dose pill for premenstrual syndrome complained acute severe stomachache. Her liver function test showed ALT 16 IU/L, AST 17 IU/L, ALP 161 IU/L, GGT 15 IU/L, and PLT 18.0 × 104/μL. Abdominal enhanced CT showed persistent well-defined filling defect within superior mesenteric vein to extrahepatic portal vein (Fig. 11.23a). She was diagnosed portal vein thrombosis and underwent anticoagulant therapy. Enhanced CT after anticoagulant therapy revealed hepatopetal collaterals (portal cavernoma) around pancreas (Fig. 11.23b). Portal vein thrombi disappeared after anticoagulant therapy, but superior mesenteric vein remained narrowed.
Portal vein thrombosis. (a) Portal vein thrombosis on coronal section. Contrast-enhanced CT showed filling defect from superior mesenteric vein to intrahepatic portal vein in the portal phase. (b) Portal cavernoma (arrow) around the pancreas on coronal section. Contrast-enhanced CT showed collaterals with hepatopetal flow around pancreas in the portal phase
11.11 Pylephlebitis
Pylephlebitis is characterized by suppurative thrombosis of the portal vein and is a deadly complication of intra-abdominal infections such as appendicitis, diverticulitis, pancreatitis, peritonitis, or cholangitis [48]. An uncontrolled infection in the regions neighboring or drained by the portal system induces thrombophlebitis of small mesenteric veins and can spread to the portal system and to the liver. It is not easy in clinical settings to get the culture-positive fluid from the portal system for its diagnosis. As an alternative method, it is defined as the presence of portal mesenteric venous thrombosis with or without bacteremia within 30 days of intra-abdominal infection. It is advocated to use broad-spectrum antibiotics for pylephlebitis, even without bacteremia.
11.12 Portal Vein Aneurysm (PVA)
PVA is an unusual vascular dilatation of the portal vein with an incidence of 0.06% and defined as a diameter exceeding 15 mm in normal liver and 19 mm in cirrhosis [49]. Etiology of PVA is still unclear but considered to be congenital or acquired. The congenital cause is the incomplete regression of the right primitive distal vitelline vein. Moreover, the presence of vein wall defects can facilitate the development of the aneurysm. The acquired cause is mainly portal hypertension in cirrhosis. The high splanchnic flow and hyperdynamic circulation cause the portal dilatation with weakening venous wall. Other causes are pancreatitis, trauma, and invasion of portal wall by malignancies.
One third of patients are asymptomatic. Main symptom is abdominal pain. Symptoms by the compression of adjacent organs, gastrointestinal hemorrhage, and spontaneous rupture are rare. Most of the cases are diagnosed with US or CT. US, especially color Doppler US, can show hemodynamics of the portal vein and PVA. CT is useful to evaluate the positional relationship with adjacent organs. Surgical indications are patients with complicated PVA such as rupture, high risk of the rupture, and thrombosis.
11.13 Hereditary Hemorrhagic Telangiectasia (HHT)
Hereditary hemorrhagic telangiectasia (HHT) was initially reported as Osler-Weber-Rendu disease named Rendu in 1896, Osler in 1901, and Weber in 1907. HHT is a genetic vascular disorder characterized by the primarily dominant autosomal hereditary transmission of dermal, mucosal, and visceral telangiectasia and arteriovenous malformations (AVMs). The genetic mutations lead to the impairment of blood vessel development, resulting in telangiectasia and AVMs. Liver involvement is more common with an incidence of about 75% [50,51,52]. Hepatic histological features are a honeycombed meshwork of dilated sinusoids or tortuous veins, adjacent arteries, and increased portal vascular channels. Portal fibrosis may be seen. Triple-phase enhanced CT demonstrates arteriovenous, arterioportal, or portovenous shunts in the liver. Arteriovenous shunt is the most common and may induce congestive heart failure, hepatomegaly, and pulmonary hypertension. Arterioportal shunt may induce portal hypertension including splenomegaly or esophagogastric varices.
The diagnosis of HHT is widely used Curaçao criteria [53] which is based on the most characteristic features of disease: (a) recurrent spontaneous epistaxis, (b) a family medical history, (c) mucocutaneous telangiectasia, and (d) the presence of visceral lesions. A definitive diagnosis of HHT is made if a patient exhibits at least three of the four criteria. If the diagnosis of HHT is proven or assumed, all patients should be screened for cerebral vascular malformations, pulmonary AVMs, and hepatic vascular malformations and annual hemoglobin examined.
The therapeutic options for hepatic involvement were limited. Complications of portal hypertension such as bleeding of varices or ascites should be treated with medical and endoscopic treatments. High-output cardiac failure can be treated with medical treatment. Liver transplantation may be the only curative option for hepatic vascular malformations and apply to uncontrolled high-output cardiac failure, cholangitis, and portal hypertension.
Case 11.10
A 60-year-old man was admitted because of iron deficient anemia. Telangiectasia in the tongue was observed. Upper gastrointestinal endoscopy showed many gastrointestinal angioectasia and esophageal varices. His blood test was hemoglobin 7.1 g/dL, platelet count 197,000/μL, albumin 4.0 g/dL, total bilirubin 0.5 mg/dL, AST 15 U/L, ALT 15 U/L, γ-GTP 73 mg/dL, Fe 28 μg/dL, TIBC 373 μg/dL, ferritin 10.3 ng/mL, HBs antigen-negative, and HCV antibody-negative, antinuclear antibody-negative, and anti-mitochondrial antibody-negative. From these data, he was diagnosed iron deficient anemia. Color Doppler US showed an arterioportal shunt and a portovenous shunt in the liver (Fig. 11.24a, b). MDCT also showed an arterioportal shunt and a portovenous shunt between a left portal vein and a middle hepatic vein (Fig. 11.24c, d). Angiography revealed the multiple arterioportal shunts in both lobes (Fig. 11.24e, f).
Hereditary hemorrhagic telangiectasia. (a) An arteriovenous shunt (arrow) is presented in the liver with color Doppler ultrasonography. (b) A portovenous shunt (arrow) is presented in the liver with color Doppler ultrasonography. (c) An arterioportal shunt (arrow) is shown between a left gastric artery and portal vein with contrast-enhanced computed tomography. (d) A portovenous shunt (arrow) is presented between a portal vein and a middle hepatic vein with contrast-enhanced computed tomography. (e, f) Multiple arterioportal shunts are presented with angiography
11.14 Sinusoids
Sinusoids are lined by endothelial cells containing fenestrations, and Kupffer cells reside in the lumen, and hepatic stellate cells, natural killer cells, and mast cells are found within the space of Disse. Pericellular fibrosis, sinusoidal dilatation, peliosis hepatis, and microvascular injury may be related to drugs, toxins, and ischemia.
11.15 Peliosis Hepatis
Peliosis hepatis is defined as blood-filled cystic spaces, either nonlined or lined with sinusoidal endothelial cells in the liver [54, 55]. At gross inspection, it looks like “Swiss cheese appearance.” Microscopically, it is classified into two types; the first type is designated “parenchymal peliosis” and consists of irregular cavities that are neither lined by sinusoidal cells nor by fibrous tissue. The second type is “phlebectatic peliosis” and characterized by regular spherical cavities lined by endothelium and /or fibrosis [56]. Macroscopic peliosis hepatis is induced by anabolic, estrogenic, or adrenocortical steroids. It can also be caused by malnutrition, leukemia, tuberculosis, leprosy, vasculitis, and AIDS. Microscopic lesions are caused by the intake of drugs for organ transplantation and various malignancies.
Imaging modalities do not allow a clear diagnosis of peliosis hepatis. It should be differentially diagnosed from hemangioma, hepatocellular adenoma, hepatocellular carcinoma, focal nodular hyperplasia, abscess, and metastatic adenocarcinoma. US shows heterogenous with both hypo- and hyperechoic areas. On enhanced CT, they appear hypervascular in the arterial phase and then become isodense. On unenhanced T2-weighted MR images, they demonstrate high intensity with high-intensity multiple spots, which are attribute to hemorrhagic necrosis.
We present a case of macroscopic peliosis hepatis of unknown etiology.
Case 11.11
A 29-year-old female complained of mild fever accompanied by right-sided hypochondralgia and a backache. Contrast-enhanced abdominal CT showed a low-density area 6 cm by 4 cm in diameter in the early phase, and the area was still low in density in the late phase (Fig. 11.25). No abnormal values on liver function tests were seen, and no coagulopathy was detected. Echo-guided tumor biopsy showed dilatation of sinusoids with preservation of the portal tracts; the sinusoids were congested with red blood cells and destroyed (Fig. 11.26). Peliosis hepatis is usually of no significance, but macroscopic peliosis may rupture spontaneously [57].
Change history
12 December 2019
Chapter 11: E-mail address of Masahiko Koda was not included in the original version. This has been corrected now.
Abbreviations
- APF:
-
Arterioportal fistula
- AVM:
-
Arteriovenous malformations
- BCS:
-
Budd-Chiari syndrome
- CDUS:
-
Color Doppler ultrasonography
- CV:
-
Central vein
- EHPVO:
-
Extrahepatic portal venous obstruction
- FALD:
-
Fontan-associated liver disease
- FNH:
-
Focal nodular hyperplasia
- HA:
-
Hepatic artery
- HCC:
-
Hepatocellular carcinoma
- HHT:
-
Hereditary hemorrhagic telangiectasia
- HSCT:
-
Hematopoietic stem cell transplantation
- HV:
-
Hepatic vein
- INCPH:
-
Idiopathic non-cirrhotic portal hypertension
- IVC:
-
Inferior vena cava
- MOVC:
-
Idiopathic membranous obstruction of IVC
- PV:
-
Portal vein
- PVT:
-
Portal vein thrombosis
- RA:
-
Right atrium
- SMAV fistula:
-
Superior mesenteric arteriovenous fistula
- SMV:
-
Superior mesenteric vein
- SV:
-
Splenic vein
- TIPS:
-
Transjugular intrahepatic portosystemic shunt
References
Budd G. On diseases of the liver. London: John Churchill; 1845. p. 135.
Chiari H. Experiences about infarction in human liver. Zeitschrift fur Hailkunde. 1898;19:475–512.
Rajani R, Melin T, Bjornsson E, Broome U, Sangfelt P, Danielsson A, et al. Budd-Chiari syndrome in Sweeden; epidemiology, clinical characteristics and survival – an 18-year experience. Liver Int. 2008;29:253–9.
Orloff MJ, Daily PO, Orloff SL, Girard B, Orloff MS. A 27-year experience with surgical treatment of Budd-Chiari syndrome. Am Surg. 2000;232:340–52.
Aydinli M, Bayraktar Y. Budd-Chiari syndrome: etiology, pathogenesis and diagnosis. World J Gastroenterol. 2007;13:2693–6.
Dilawari JB, Bambery P, Chawla Y, Kaur U, Bhusnurmath SR, Malhotra HS, et al. Hepatic outflow obstruction (Budd-Chiari syndrome). Experience with 177 patients and a review of the literature. Medicine. 1994;73:21–36.
Denninger MH, Chait Y, Casadevall N, Hillaire S, Guillin MC, Bezeaud A, et al. Cause of portal or hepatic venous thrombosis in adults: the role of multiple concurrent factors. Hepatology. 2003;31:587–91.
Simon IW. Membranous obstruction of the inferior vena cava and hepatocellular carcinoma in South Africa. Gastroenterology. 1982;68:171–8.
Datta DV, Saha S, Singh SA, Gupta BB, Aikat BK, Chuttani PN. Clinical spectrum of Budd-Chiari syndrome in Chandigarh with particular reference to obstruction of intrahepatic portion of inferior vena cava. Indian J Med Res. 1972;60:385–402.
Shrestha SM, Shrestha S. Hepatic vena cava disease: etiologic relation to bacterial infection. Hepatol Res. 2007;37:196–204.
Okuda H, Yamagata H, Obata H, Iwata H, Sasaki R, Imai F, et al. Epidemiological and clinical features of Budd-Chiari syndrome in Japan. J Hepatol. 1995;22:1–9.
Das CJ, Soneja M, Tayal S, Chahal A, Srivastava S, Kumar A, et al. Role of radiological imaging and interventions in management of Budd-Chiari syndrome. Clin Radiol. 2018. pii: S0009–9260(18)30084–9. https://doi.org/10.1016/j.crad.2018.02.003. [Epub ahead of print].
Copelan A, Remer EM, Sands M, Nghiem H, Kapoor B. Diagnosis and management of Budd Chiari syndrome: an update. Cardiovasc Intervent Radiol. 2015;38:1–12.
Henderson JM, Warren WD, Millikan WJ, Galloway JR, Kawasaki S, Stahl RL, et al. Surgical options, hematologic evaluation, and pathologic changes in Budd-Chiari syndrome. Am J Surg. 1990;159:41–50.
Mitchell MC, Boitnott JK, Kaufman S, Cameron JL, Maddrey WC. Budd-Chiari syndrome: etiology, diagnosis and management. Medicine. 1982;61:199–218.
Bourlière M, Le Treut YP, Arnoux D, Castellani P, Bordigoni L, Maillot A, et al. Acute Budd-Chiari syndrome with hepatic failure and obstruction of the inferior vena cava as presenting manifestations of hereditary protein C deficiency. Gut. 1990;31:949–52.
Bhargawa DK, Arova A, Dasarathy AS. Laparoscopic features of the Budd-Chiari syndrome. Endoscopy. 1991;23:259–61.
Mancuso A. An update on management of Budd-Chiari syndrome. Ann Hepatol. 2014;13:323–6.
European Association for the Study of the Liver. EASL clinical practice guidelines: vascular diseases of the liver. J Hepatol. 2016;64:179–202.
Tripathi D, Macnicholas R, Kothari C, Sunderraj L, Al-Hilou H, Rangarajan B, Chen F, Mangat K, Elias E, Olliff S. Good clinical outcomes following transjugular intrahepatic portosystemic stent-shunts in Budd-Chiari syndrome. Aliment Pharmacol Ther. 2014;39:864–72.
Mentha G, Giostra E, Majno PE, Bechstein WO, Neuhaus P, O’Grady J, Praseedom RK, Burroughs AK, Le Treut YP, Kirkegaard P, Rogiers X, Ericzon BG, Hockerstedt K, Adam R, Klempnauer J. Liver transplantation for Budd-Chiari syndrome: a European study on 248 patients from 51 centres. J Hepatol. 2006;44:520–8.
Deal BJ, Jacobs ML. Management of the failing Fontan circulation. Heart. 2012;98:1098–104.
Rychik J, Veldtman G, Rand E, Russo P, Rome JJ, Krok K, et al. The precarious state of the liver after a Fontan operation: summary of a multidisciplinary symposium. Pediatr Cardiol. 2012;33:1001–12.
Ghaferi AA, Hutchins GM. Progression of liver pathology in patients undergoing the Fontan procedure: chronic passive congestion, cardiac cirrhosis, hepatic adenoma, and hepatocellular carcinoma. J Thorac Cardiovasc Surg. 2005;129:1348–52.
Greenway SC, Crossland DS, Hudson M, Martin SR, Myers RP, Prieur T, et al. Fontan-associated liver disease: implications for heart transplantation. J Heart Lung Transplant. 2016;35:26–33.
Fan CQ, Crawford JM. Sinusoidal obstruction syndrome (hepatic veno-occlusive disease). J Clin Exp Hepatol. 2014;4:332–46.
Richardson PG, Smith AR, Triplett BM, Kernan NA, Grupp SA, Antin JH, et al. Defibrotide study group. Defibrotide for patients with hepatic Veno-occlusive disease/sinusoidal obstruction syndrome: interim results from a treatment IND study. Biol Blood Marrow Transplant. 2017;23:997–1004.
Norris S, Crosbie O, McEntee G, Traynor O, Molan N, McCann S, et al. Orthotopic liver transplantation for veno-occlusive disease complicating autologous bone marrow transplantation. Transplantation. 1997;63:1521–4.
Takehara H, Komi N, Hino M. Congenital arteriovenous fistula of the superior mesenteric vessels. J Pediatr Surg. 1988;23:1029–31.
Wood M, Nykamp PW. Traumatic arteriovenous fistula of the superior mesenteric vessels. J Trauma. 1980;20:378–82.
Benedetto JC, Liszewski RF. Superior mesenteric arteriovenous fistula: case report and literature review. J Am Osteopath Assoc. 1988;88:517–20.
Lee KR, Kishore P, Hardin CA. Postsurgical arteriovenous fistula. Acquired AV fistula of the mesentery. J Kans Med Soc. 1974;75:87–90.
Rabhan NB, Guillebeau JG, Brachney EG. Arteriovenous fistula of the superior mesenteric vessels after a gunshot wound. N Engl J Med. 1962;266:603–5.
Brunner JH, Stanley RJ. Superior mesenteric arteriovenous fistula. JAMA. 1973;223:316–8.
Riggio O, Gioia S, Pentassuglio I, Nicoletti V, Valente M, d’Amati G. Idiopathic noncirrhotic portal hypertension: current perspectives. Hepat Med. 2016;8:81–8.
Tsuneyama K, Ohta K, Zen Y, Sato Y, Niwa H, Minato H, et al. A comparative histological and morphometric study of vascular changes in idiopathic portal hypertension and alcoholic fibrosis/cirrhosis. Histopathology. 2003;43:55–61.
Ohbu M, Okudaira M, Watanabe K, Kaneko S, Takai T. Histopathological study of intrahepatic aberrant vessels in cases of noncirrhotic portal hypertension. Hepatology. 1994;20:302–8.
Dhiman RK, Chawla Y, Vasishta RK, Kakkar N, Dilawari JB, Trehan MS, et al. Non-cirrhotic portal fibrosis (idiopathic portal hypertension): experience with 151 patients and a review of the literature. J Gastroenterol Hepatol. 2002;17:6–16.
de Franchis R, Dell’Era A, Iannuzzi F. Diagnosis and treatment of portal hypertension. Dig Liver Dis. 2004;36:787–98.
Lay CS, Tsai YT, Lee FY, Lai YL, Yu CJ, Chen CB, et al. Endoscopic variceal ligation versus propranolol in prophylaxis of first variceal bleeding in patients with cirrhosis. J Gastroenterol Hepatol. 2006;21:413–9.
Patidar KR, Sydnor M, Sanyal AJ. Transjugular intrahepatic portosystemic shunt. Clin Liver Dis. 2014;18:853–76.
Shimoda R, Horiuchi K, Hagiwara S, Suzuki H, Yamazaki Y, Kosone T, et al. Short-term complications of retrograde transvenous obliteration of gastric varices in patients with portal hypertension: effects of obliteration of major portosystemic shunts. Abdom Imaging. 2005;30:306–13.
Sarin SK, Kumar A, Chawla YK, Baijal SS, Dhiman RK, Jafri W, et al. Members of the APASL working party on portal hypertension. Noncirrhotic portal fibrosis/idiopathic portal hypertension:APASL recommendations for diagnosis and treatment. Hepatol Int. 2007;1:398–413.
Chawla YK, Bodh V. Portal vein thrombosis. J Clin Exp Hepatol. 2015;5:22–40.
Hauenstein K, Li Y. Radiological diagnosis of portal/mesenteric vein occlusion. Viszeralmedizin. 2014;30:382–7.
Manzano-Robleda Mdel C, Barranco-Fragoso B, Uribe M, Méndez-Sánchez N. Portal vein thrombosis: what is new? Ann Hepatol. 2015;14:20–7.
Khanna R, Sarin SK. Idiopathic portal hypertension and extrahepatic portal venous obstruction. Hepatol Int. 2018;12(Suppl 1):148–67.
Choudhry AJ, Baghdadi YM, Amr MA, Alzghari MJ, Jenkins DH, Zielinski MD. Pylephlebitis: a review of 95 cases. J Gastrointest Surg. 2016;20:656–61.
Laurenzi A, Ettorre GM, Lionetti R, Meniconi RL, Colasanti M, Vennarecci G. Portal vein aneurysm: what to know. Dig Liver Dis. 2015;47:918–23.
Ianora AA, Mememo M, Sabba C, Cirulli A, Rotondo A, Angelelli G. Hereditary hemorrhagic telangiectasia: multi-detector row helical CT assessment of hepatic involvement. Radiology. 2004;230:250–9.
Bernard G, Mion F, Henry L, Plauchu H, Paliard P. Hepatic involvement in hereditary hemorrhagic telangiectasia: clinical, radiological, and hemodynamic studies of 11 cases. Gastroenterology. 1993;105:482–7.
Piskorz MM, Waldbaum C, Volpacchio M, Sorda J. Liver involvement in hereditary hemorrhagic telangiectasia. Acta Gastroenterol Latinoam. 2011;41:225–9.
Shovlin CL, Guttmacher AE, Buscarini E, Faughnan ME, Hyland RH, Westermann CJ, Kjeldsen AD, Plauchu H. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-weber syndrome). Am J Med Genet. 2000;91:66–7.
Wold LE, Ludwig J. Peliosis hepatis: two morphologic variants? Hum Pathol. 1981;12:388–9.
Tsokos M, Erbersdobler A. Pathology of peliosis. Forensic Sci Int. 2005;149:25–33.
Crocetti D, Palmieri A, Pedullà G, Pasta V, D’Orazi V, Grazi GL. Peliosis hepatis: personal experience and literature review. World J Gastroenterol. 2015;21:13188–94.
Choi SK, Jin JS, Cho SG, Choi SJ, Kim CS, Choe YM, et al. Spontaneous liver rupture in a patient with peliosis hepatis: a case report. World J Gastroenterol. 2009;15:5493–7.
Acknowledgment
We are grateful to Professor Michael A. Kern for constructive advice and helpful suggestions in first edition of this chapter.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Koda, M., Matono, T., Taniai, M., Iwai, M. (2019). Vascular Disorders in the Liver. In: Hashimoto, E., Kwo, P., Suriawinata, A., Tsui, W., Iwai, M. (eds) Diagnosis of Liver Disease. Springer, Singapore. https://doi.org/10.1007/978-981-13-6806-6_11
Download citation
DOI: https://doi.org/10.1007/978-981-13-6806-6_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-6805-9
Online ISBN: 978-981-13-6806-6
eBook Packages: MedicineMedicine (R0)