Abstract
IgG4-related disease (RD) was originally recognized in 2001 in a patient with autoimmune pancreatitis with elevated serum IgG4. Subsequently, a fibro-inflammatory condition, characterized by tumefactive lesions at multiple sites, with dense lymphoplasmacytic infiltrate, rich in IgG4-positive plasma cells, storiform fibrosis, and obliterative phlebitis was found to be associated with autoimmune pancreatitis. The sites include the biliary tree, salivary glands, periorbital tissue, kidneys, lungs, lymph nodes, meninges, aorta, breast, prostate, thyroid, pericardium, and skin. Mikulicz syndrome with lacrimal and salivary gland enlargements is now considered as IgG4-RD. Clinically, the lacrimal gland is the most affected among the ophthalmic tissues, but the others include extraocular muscles, trigeminal nerve, orbital fat, eyelids, and nasolacrimal system. For ophthalmic disease, the term IgG4-related ophthalmic disease (IgG4-ROD) is used.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
IgG4-related disease (RD) was originally recognized in 2001 in a patient with autoimmune pancreatitis with elevated serum IgG4. Subsequently, a fibro-inflammatory condition, characterized by tumefactive lesions at multiple sites, with dense lymphoplasmacytic infiltrate , rich in IgG4-positive plasma cells , storiform fibrosis , and obliterative phlebitis was found to be associated with autoimmune pancreatitis . The sites include the biliary tree, salivary glands, periorbital tissue, kidneys, lungs, lymph nodes, meninges, aorta, breast, prostate, thyroid, pericardium, and skin. Mikulicz syndrome with lacrimal and salivary gland enlargements is now considered as IgG4-RD. Clinically, the lacrimal gland is the most affected among the ophthalmic tissues, but the others include extraocular muscles, trigeminal nerve, orbital fat, eyelids, and nasolacrimal system. For ophthalmic disease, the term IgG4-related ophthalmic disease (IgG4-ROD) is used.
Clinically, the lacrimal gland is the most affected among the ophthalmic tissues, but the others include extraocular muscles (EOM) , trigeminal nerve, orbital fat , eyelids , and nasolacrimal system. For ophthalmic disease, the term IgG4-related ophthalmic disease (IgG4-ROD) is used.
Clinical Scenarios
Case 1: Eyelid
A 55-year-old Eurasian male presented with progressive painless right lower eyelid swelling for 2 months. On examination, there was a well-defined mass occupying the whole width of the right lower eyelid . The mass was non-tender and firm on palpation, and the skin over the mass was slightly erythematous and mobile (Fig. 11.1). The rest of the eye examination was normal.
CLOSE summary is shown in Table 11.1.
Differential Diagnosis
-
Lymphoproliferative disease including lymphoma
-
Skin carcinomas, especially sebaceous gland carcinoma
-
Necrobiotic xanthogranuloma
-
Rosai-Dorfman disease
-
Schwannoma
-
Sarcoidal lesion
-
Infective granulomas such as TB/syphilis
-
Kaposi’s sarcoma
-
IgG4-related disease
-
Kimura’s disease
Radiology
The CT scan showed an enhancing soft tissue lesion inferior to right globe in the lower eyelid (Fig. 11.2). The lesion was seen extending posteriorly and medially into the orbit, abutting the tendinous portion of the inferior rectus (IR) muscle. Equivocal mild enlargement of IR muscle was noted. It was in close proximity to the right lacrimal sac. There was no involvement of the optic nerve. Incidentally, extensive bilateral sinusitis was noted.
Investigations included the following:
-
FBC: normal except for eosinophilia
-
ESR: raised at 91 mm/h
-
CRP: <5 mg/l
-
ANA: positive
-
SLE, ENA panels, and ANCA: negative
-
Myeloma screen: generalized increase in immunoglobulin
-
Hepatitis B/C screen: negative
-
TB spot: borderline
-
IgG subclass: total IgG, subclasses 1, 2, and 3 elevated, IgG4 not elevated
Intervention
An incisional biopsy of the eyelid lesion was carried out and the specimens sent fresh for histopathology and flow cytometry. The patient also underwent a biopsy of the nasal mucosa.
Case 2: Lacrimal Gland
A 53-year-old Malay female with co-morbidities such as diabetes mellitus, hypertension, and hyperlipidaemia presented with painless right upper lid swelling of 1-month duration. About 6 months earlier, she had undergone biopsy for bilateral breast lumps. The biopsy revealed atypical lymphoid proliferation and negative for malignancy.
The eye examination revealed normal visual acuities and mild ptosis of the right upper eyelid with full ocular motility. There was fullness in the lateral aspect of the right upper eyelid (Fig. 11.3) with the lacrimal gland slipping under the fingers on palpation, it was non-tender, and the conjunctiva was white. There was no proptosis as measured by exophthalmometer.
CLOSE summary is given in Table 11.2.
Differential Diagnosis
-
Sarcoidosis
-
Ideopathic orbital inflammation
-
Autoimmune disease such as Sjogren’s syndrome
-
IgG4 inflammation
-
Lymphoproliferative disorder
-
Malignant epithelial tumour/metastasis
Radiology
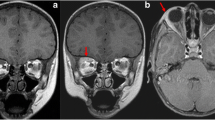
CT scan of the orbits showed enlargement of the right lacrimal gland (Fig. 11.4). Soft tissue swelling was noted in the upper eyelid . The left lacrimal gland was also mildly enlarged which was not noted clinically. The rest of the orbits was unremarkable. Possibility of a lymphoma was considered.
Investigations
Serum IgG subclasses
Total IgG | 1740 mg/dl (raised) | Normal range: 767–1590 |
|---|---|---|
IgG1 | 993 mg/dl (raised) | Normal range: 341–894 |
IgG2 | 1030 mg/dl (raised) | Normal range: 171–632 |
IgG3 | 130 mg/dl (raised) | Normal range: 18.4–106 |
IgG4 | 590 mg/dl (raised) | Normal range: 2.4–121 |
Intervention
An incisional biopsy of the right lacrimal gland and orbital fat was performed through an anterior orbitotomy and lid crease incision. Tissues were sent fresh for histopathology.
Histopathology
The histopathological features from three biopsies (eyelid , nasal mucosa from case 1, and lacrimal gland in case 2) showed similar features. There was dense fibrosis and prominent aggregates of lymphoid cells admixed with numerous plasma cells (Fig. 11.5). The lymphocytes were composed of a mixture of B cells (CD20 and PAX5 positive), as well as T cells (CD3 positive). There were more than 100 IgG4-positive plasma cells per high-power field. The IgG4/IgG ratio was more than 40% (Fig. 11.6). The histologic features were consistent with a diagnosis of IgG4-related disease in the appropriate clinical context.
Comment from pathologist: Other features that would be supportive of a diagnosis of IgG4-related disease include storiform fibrosis and obliterative phlebitis . These features were not prominent in these biopsies and are seldom seen in orbital tissues. It should be noted that the quantitative criteria might vary according to the site of the biopsy.
IgVH mutation from paraffin block from case 1 showed polyclonality, thus ruling out MALT lymphoma as a possibility.
The breast biopsy from case 2 was reviewed, and in retrospect, similar IgG and IgG4 staining characteristics were noted in the tissues.
Management
Case 1 had sinus involvement and case 2 breast involvement. Patients underwent systemic screening for more organ involvements but were negative. They were treated with oral steroids. The response was good, and eventually steroid-sparing agent azathioprine was started. The eyelid lesion reduced in size in case 1. In case 2, repeat serum IgG subclasses revealed normal levels of total IgG1, IgG2, and IgG3, while IgG4 remained slightly elevated although it was less than the previous reading.
Discussion
IgG4-RD was first described in autoimmune pancreatitis with tumefactive lesions showing classic features of dense lymphoplasmacytic infiltrate rich in IgG4+ plasma cells, storiform fibrosis, and obliterative phlebitis . An elevated serum IgG4 ≥ 135 mg/dl concentrations may or may not be present, and only 40% of patients show raised subclass IgG4 concentrations. Some studies have shown that in the lacrimal glands , there may not be any obliterative phlebitis or storiform fibrosis , but instead a collagenous fibrosis is present.
Imaging in the form of CT or MRI is useful in cases where the soft tissues of the orbit or EOM are affected. The MRI shows isodensity in T1-weighted images and hypodensity on T2-weighted images with homogeneous enhancement with gadolinium. FDG-PET scans can be used for systemic evaluation.
IgG4-ROD is diagnosed with the criteria (Goto et al.) listed in Table 11.3.
Histologic diagnosis of IgG4-ROD is made only if two of the three criteria mentioned in Table 11.3 are present; in which case, it should show a number of IgG4-staining plasma cells on immunostaining to be >50 per high-power field and the ratio of IgG4 plasma cells to IgG plasma cells be at least 40%. Bilateral involvement is likely to have higher IgG4 serum levels.
A subset of patients with IgG4-RD are known to have associated allergic symptoms with raised eosinophilia (as in our first patient) and elevated IgE.
Until discoveries pertaining to the aetiology and pathophysiology of the disease surface, the term IgG4-RD or ROD will be used in the light of the presence of IgG4 (as per the guidelines) within involved organs with elevated serum IgG4 concentrations.
The mainstay of treatment is systemic corticosteroids. In cases where serum IgG concentrations are elevated, it may be used as a marker for monitoring treatment response and for relapse of the disease.
Learning Points
IgG4-related ophthalmic disease (ROD) is still evolving. There are some variations in the presentation of ophthalmic disease compared to systemic IgG4-RD.
IgG4 inflammation is rare in the eyelids , but more common in lacrimal glands and extraocular muscles , and should be suspected in all painless lumps in ocular adnexa.
Further Reading
Deshpande V, Zen Y, Chan JK, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25(9):1181–92.
Gervasio KA, Chelnis J, Burkat CN. IgG4-related orbital inflammation.eyewiki.aao.org. 2017.
Goto H, Takahira M, Azumi A, et al. Diagnostic criteria for IgG4 related ophthalmic disease. Jpn J Ophthalmol. 2015;59:1–7.
Sogabe Y, Miyatani K, Goto R, et al. Pathological findings of infraorbital nerve enlargement in IgG4-related ophthalmic disease. Jpn J Ophthalmol. 2012;56:511–4.
Toyoda K, Oba H, Kutomi K, et al. MR imaging of IgG4-related disease in the head and neck and brain. Am J Neuroradiol. 2012;33(11):2136–9.
Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG-RD), 2011. Mod Rheumatol. 2012;22:21–30.
Wallace ZS, Deshpande V, Stone JH. Ophthalmic manifestations of IgG4-related disease: single centre experience and literature review. Semin Arthritis Rheum. 2014;43(6):806–17.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Amrith, S., Young, S.M., Ting, E., Wu, B., Nga, M.E., Sundar, G. (2019). IgG4-Related Ophthalmic Disease. In: Amrith, S., Sundar, G., Young, S. (eds) Ocular Adnexal Lesions. Springer, Singapore. https://doi.org/10.1007/978-981-13-3798-7_11
Download citation
DOI: https://doi.org/10.1007/978-981-13-3798-7_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-3797-0
Online ISBN: 978-981-13-3798-7
eBook Packages: MedicineMedicine (R0)