Abstract
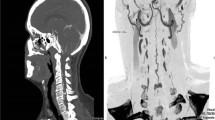
A 50-year-old man presented with a history of numbness in both lower limbs and associated urine and fecal incontinence for 6 months. There was no history of trauma. MRI scan showed multiple flow voids in the lower cervical and dorsal spine along with cord edema in the lower thoracic cord suggestive of a vascular malformation (Fig. 80.1). Spinal angiography demonstrated spinal dural AV fistula at L4–L5 levels with arterial feeders from the lateral sacral branches (Fig. 80.2).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Case
A 50-year-old man presented with a history of numbness in both lower limbs and associated urine and fecal incontinence for 6 months. There was no history of trauma. MRI scan showed multiple flow voids in the lower cervical and dorsal spine along with cord edema in the lower thoracic cord suggestive of a vascular malformation (Fig. 80.1). Spinal angiography demonstrated spinal dural AV fistula at L4–L5 levels with arterial feeders from the lateral sacral branches (Fig. 80.2).
Issues
-
1.
Multiple small tortuous feeders
Management
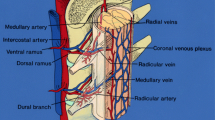
A small 11-cm-long 5F sheath (Cordis) was used to access the right femoral artery. Following this a 5F diagnostic catheter (Cook) was positioned in the left internal iliac artery. The diagnostic catheter acts as a guiding catheter. Following this, a Marathon 1.5F microcatheter (ev3 Neurovascular, Irvine, CA) over a Mirage 0.008 micro-guidewire (ev3 Neurovascular, Irvine, CA) was placed as distal as possible. Due to the ultra-narrow caliber of the feeders and tortuosity, it was not possible to navigate the microcatheter till the fistula site (Fig. 80.3).
Once the microcatheter was positioned as distal as possible in the feeding artery, the fistula was embolized using 15% glue (mixed with lipiodol). The glue penetrated into the venous side obliterating the fistula (Fig. 80.4).
(a) The fistula was embolized using much diluted glue (15%). The blue arrow marks the microcatheter position, while the red arrow marks the entry of glue into the proximal draining vein. (b) Post-embolization angiogram demonstrates complete obliteration of the fistula. (c) Post-procedure DynaCT (angiographic CT) demonstrated the complete glue cast and more importantly, the obliteration of the vein (green arrow)
Patient made good clinical recovery with significant improvement over a period of 6 months.
Tips and Tricks
-
1.
The aim of treatment in spinal dural fistula is to obliterate the draining vein.
-
2.
A proximal arterial occlusion will lead to a transient improvement of symptoms; however, the fistula is prone to recur from collaterals.
-
3.
A slow continuous injection of much dilute glue (15% glue and 85% lipiodol) has a higher chance of reaching the draining vein and obliterating the fistula.
-
4.
In cases of suspected spinal fistula, complete spinal and cranial angiogram is essential as the feeding arteries can be superior or inferior to the fistulous segment.
-
5.
Use of flow guided microcatheter is highly recommended.
Suggested Reading
Andres RH, Barth A, Guzman R, Remonda L, El-Koussy M, Seiler RW, Widmer HR, Schroth G. Endovascular and surgical treatment of spinal dural arteriovenous fistulas. Neuroradiology. 2008;50:869–76.
Willinsky R, terBrugge K, Montanera W, et al. Spinal epidural arteriovenous fistulas: arterial and venous approaches to embolization. AJNR Am J Neuroradiol. 1993;14:812–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 The Author(s)
About this chapter
Cite this chapter
Gupta, V. (2019). Spinal Dural Arteriovenous Fistula (AVF). In: Gupta, V., Puri, A., Parthasarathy, R. (eds) 100 Interesting Case Studies in Neurointervention: Tips and Tricks. Springer, Singapore. https://doi.org/10.1007/978-981-13-1346-2_80
Download citation
DOI: https://doi.org/10.1007/978-981-13-1346-2_80
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-1345-5
Online ISBN: 978-981-13-1346-2
eBook Packages: MedicineMedicine (R0)