Abstract
In this paper we propose a fully automatic technique for Cobb angle computation from Scoliosis radiograph image where the objectives are to have no user intervention and to increase the reliability of spinal curvature magnitude quantification. The automatic technique mainly comprises of four steps, namely: Preprocessing, ROI identification, Object centerline extraction and Cobb angle computation from the extracted spine centerline. Bilateral image denoising is considered as the preprocessing step. Support Vector Machine classifier is used for object identification. We have assumed that the spine is a continuous contour rather than a series of discrete vertebral bodies with individual orientations. Morphological operation, Gaussian blurring, spine centerline approximation and polynomial fit are used to extract the centerline of spine. The tangent at every point of the extracted centerline is taken and Cobb angle is evaluated from these tangent values. To analyze the automated diagnosis technique, the proposed approach was evaluated on a set of 21 coronal radiograph images. Identification of ROI based on Support Vector Machine classifier is effective enough with a sensitivity and specificity of 100% and the center line extraction from this ROI gave correct results for 57.14% subjects with very less or negligible angular variability. As the vertebral endplates in radiograph images have poor contrast due to reduced radiation dose, the continuous contour based approach gives better reliability.
Access provided by CONRICYT-eBooks. Download conference paper PDF
Similar content being viewed by others
Keywords
- Spine radiograph (X-ray) image
- Scoliosis
- Cobb’s method
- Support Vector Machine
- Gabor feature
- Automated Computer Aided Detection and Diagnosis
1 Introduction
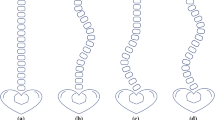
Scoliosis [7] a 3-dimensional deformity of spine is normally characterized by lateral curvature and often accompanied by rotation of individual vertebrae. The magnitude of scoliosis is determined by lateral curvature computation from medical image. This paper has selected the widely practiced Cobb’s method [7] for realizing the spine curve magnitude. Manual Cobb’s method from printed medical image includes identification of extreme vertebrae of the curve, which incline more severely towards the curve coactivity. One line is drawn following slope of upper extreme vertebrae and another line is drawn through slope of lower extreme vertebrae. Finally the interior angle formed by intersection of these two lines is the Cobb’s angle which gives the curve magnitude. An example is given in Fig. 1.
Radiograph imaging is common non-invasive form of diagnosis. This Cobb angle computation using radiograph image is standardized by the Scoliosis Research Society [12]. Cobb’s method is widely preferred because of its easier application and proper management of large spinal curvature angles. Many times there is not enough number of doctors or trained technicians to interpret the medical information from the image. So, a fully automatic Computer Aided Detection and Diagnosis (CADx) plays a significant role in medical treatment. Object recognition and segmentation are challenging tasks in radiograph image due to low radiation dose and anatomical overlap property. Such object recognition algorithm and segmentation techniques must accomplish its tasks in accurate and robust manner, because false results of CADx will break interpretation confidence and will reduce its clinical practice acceptability.
2 Related Works
In past years many digital techniques have been put forward for spine curve magnitude computation. The proposed work in this paper uses image processing techniques to develop an automated Cobb angle computation method for spinal curvature. The motivation of the proposed research is discussed in Sect. 3. “Our Approach” is followed by Sect. 4, “Automated Cobb Angle Computation” that explains the process for Cobb angle evaluation. In Sect. 5 “Results and Discussion” possess visual and experimental results with discussion. Conclusion and future work are discussed in Sect. 6.
Jeifries et al. [10] put a pair of points on every vertebra to approximate the center between each pair of points. Lines were taken parallel to vertebral body for calculating the Cobb angle. The method required much user intervention. Wever et al. [21] proposed a technique for Cobb method. The technique required six manual landmarks on every vertebra of the anterior-posterior input radiograph image. The coordinate values of landmarks helped in computing the midpoint of vertebral bodies. The lateral tilts of upper and lower endplates of every vertebra were computed by the computer algorithm. Huang et al. [9] proposed a fully automatic technique for Cobb method. The algorithm contains preprocessing, image segmentation and automatic Cobb angle measurement. The first step includes removing noise by Gaussian smoothing and histogram equalization to improve image quality. The second step possesses segmentation of vertebral column including ribs from the whole body bone scan. The Cobb angle is measured in the final step. The validation of the technique was performed on 11 random selected whole body bone scan image. The CADx results were compared with results obtained from experienced physician and a mean difference of 4.14 degree was obtained. We expect to have more experiments to validate the technique. Allen et al. [2] put forward a reliable Cobb angle computation technique using active shape model. Training set of radiograph images was taken that represented the scoliosis curve. The training set helped in recognition of vertebrae. The drawback of the technique was that active shape models could only produce shapes similar to the training set. At the time of training the boundary of the object is created by manual digitized landmark points on the perimeter of the region of interest. Zhang et al. [23] proposed a technique on Cobb angle measurement with prior vertebral shape. The extreme vertebrae of the curve which tilt more toward the curve coactivity were selected. Edge detection and Fuzzy Hough transform were performed to find the slope of the endplates of the two ROI. Cobb angle was computed from the obtained slopes. The technique is not user intervention free. Duong et al. [5] proposed a technique for detection of spinal curves from posterior-anterior radiograph image. Region of interest (ROI) was extracted. The region possesses 17 bounding boxes indicating T1 to L5 vertebral level. Texture descriptors for every block are computed and taken for training with support vector machines. Then vertebral regions are predicted and curve is fitted through the centers of predicted vertebral regions. A computer aided technique was proposed by Abuzaghleh and Barkana [1] where the ROI (spine) was cropped from the whole image. Sobel edge detection and image binarization helps in segmentation of the spine. The segmented spine was divided into blocks followed by contrast enhancement. Finally the Hough transform detected the slopes of the curvature. The number of experiments for establishing the reliability was very less. Besides this the technique need a prior selection of ROI. Anitha and Prabhu [3] put forward a technique for quantification of spinal curve in Scoliosis radiology image. The digital computation is done on a cropped ROI. Anisotropic diffusion denoising, Active Contour based vertebrae segmentation, morphological operations and Hough transform were used to compute the Cobb angle from the input radiograph. The proposed technique was validated on 250 radiograph image and shows reduced intra-observer and inter-observer error. These errors occurred due to selection of different end vertebrae. The major drawback of the technique is performing the CADx on a ROI. So, it can be said that the digital computation is not totally free from user interaction. There lies a scope of improvement to make the computation intervention free. Shaw et al. [17] put forward a technique for Cobb angle measurement in scoliosis using iPhone. Smartphone Cobb measurements were done using Apple iPhone, and a Tiltmeter software. The software was downloaded from Apple iTunes store. The Tiltmeter software required printed X-ray image and position the X-ray image on X-ray reader box. However the technique is not totally automated and requires printed X-ray images. Samuval et al. [14] proposed a mask-based segmentation algorithm for computation of Cobb angle from radiograph image. A manual landmark on center of each vertebra was taken. The mask was placed on the landmark and was resized to get the best match. So, one drawback is the technique needed user interaction. Sardjona et al. [15] proposed a technique for Cobb angle computation. A modified Charged Particle Model (CPM) has been developed and used to determine the spinal curvature. The radiograph image was charged negatively depending on the gradient-magnitude image, where the particles were attracted towards the object contour. The Cobb angle was computed from the spine contour. Yildiz [22] proposed a Computer-assisted Cobb angle measurement technique from posterior-anterior radiographs by curve fitting. Inaccurate selection of end vertebrae of a Scoliosis curve causes measurement errors in Cobb method. In this paper such subjectivity problem has been minimized by using a curve fitting method. Midpoints defined by user on digital posterior-anterior radiograph image denote the midpoints of the vertebrae. The midpoints were used to fit the polynomial equation. The end vertebrae locations were calculated using first order derivative of the polynomial equation and the Cobb angle was obtained. Small angle deviation proved that subjectivity was minimized. The drawback of the method is that it required user intervention.
3 Our Approach
The major contributions of our work are emphasized as follows:
-
1.
The proposed approach automatically identifies the region of interest (ROI), the spinal column. We have used Support Vector Machine classifier and Gabor feature to fit our purpose. The classification method was followed by morphological operation and outlier rejection of ROI. We have achieved a sensitivity and specificity of 100% for our identification method.
-
2.
Some Scoliosis involves deformation of vertebrae where the end plate and edges of vertebrae are not properly visible in radiograph image. This deformation of vertebrae is also the source of error in the selection of extreme vertebrae in traditional Cobb method. This problem is overcome by our technique where the spine is considered as a continuous structure.
-
3.
As our technique has assumed the spine as a continuous structure, our technique works well for low radiation dose radiograph image where the vertebral endplates are not properly visible. Thus reducing the affect of ionization.
-
4.
No manual intervention is required for the total process. The paper proposes a totally automated CADx for Cobb angle determination.
-
5.
Cobb angle is the final result of the automated diagnosis. Our results were validated on 21 radiograph images and we have achieved reliable Cobb angle magnitude for 57.14% cases.
This paper proposes a first of its kind CADx approach for automated Cobb angle determination from digital radiograph image and shows reduced variability for estimating angle value. The method is based on supervised learning and no manual input was taken for the computation.
4 Automated Cobb Angle Computation
To perform Cobb method, the most tilted end vertebral bodies of the Scoliosis curve must be first selected. The vertebrae that have greatest tilt with respect to the horizontal baseline are the end vertebrae of the Scoliosis curvature. From literature review it can be revealed that segmentation of vertebral bodies and then decision about most tilted end vertebrae of curvature are another source of errors.
Most segmentation depends on edge information. Objects possessing prominent and continuous edges are comparatively easier for segmentation. Coronal radiograph image of spine have weak edges due to its accusation at low X-ray radiation. Low X-ray radiation is always preferred because X-ray is ionized in nature. It is always taken care to have an X-ray image that serve the diagnosis with use of minimum radiation dose. X-ray image also have anatomical overlap property where one structure overlap other. This increases the difficulty for segmentation. Besides this object shape variation is natural property in medical images. The spine is required to be isolated from undesired details like, the ribs, pelvic girdle, lungs and other organs. To overcome this we have considered the spine as a continuous structure which runs from top to bottom instead of number of isolated vertebral bodies. This assumption will help us to overcome the erroneous result that can occur due to segmentation. We have directly obtained the centerline of spine.
Slope at every point of the centerline are computed. Due to unavailability of enough number of double curvature (S-shaped) cases, we have showed our automated computation results for single curvature (C-shaped) Scoliosis. The longest adjacent positive and negative slope series were taken into account and the maximum positive slope and the minimum negative slope were added to get the Cobb angle. The pointing out of center points having maximum positive and minimum negative slopes of longest series is equivalent to the decision about most tilted end vertebrae of the scoliosis curve. So, this step further reduces the computation error.
Figure 2 presents the workflow of the proposed CADx. The process mainly comprise of four steps: Preprocessing, ROI identification, Object centerline extraction and Cobb angle computation from the centerline.
4.1 Preprocessing Using Bilateral Filter
Presence of noise in image will disturb image processing steps. In our proposed supervised technique the radiograph training-set and the input test radiograph image are preprocessed by Bilateral filter [19]. The filter preserves edges and features while removing noise from the image.
4.2 ROI Identification Using Support Vector Machine and Gabor Feature
Support Vector Machine (SVM) classifier using Gabor features is used for vertebral column recognition from coronal spine radiograph image.
In digital image processing, Gabor filter [Wikipedia] is a linear filter for edge detection. Frequency and orientation description of Gabor filters has high resemblance to that of human visual system, and they are found to be particularly proper for texture representation and distinction. Simple cells present in visual cortex of mammalian brains can be sculpted by Gabor functions. So, image analysis using Gabor filters is expected to be alike to perception in human visual system.
SVM [4, 13, 20] is associated with supervised classification which analysis data and recognizes pattern for regression and classification problem. SVM tries to maximize the decision boundary between two classes that helps in better classification. It is also efficient in classifying the object which is not linearly separable. The input data set is mapped to higher dimensional space where the data is separable by hyper-plane. It gives less over fitting. A set of feature vectors of radiograph vertebrae images were taken for designing the classifier. The training set possessed 506 numbers of positive images and 641 numbers of negative images. We took vertebra as positive image and other regions of spine radiograph as negative images. A generalized tool [16] using SVM classifier and Gabor feature was optimized for our classification implementation. We have prepared the positive and negative image database using spine radiograph images. The radiograph images were obtained from National Institute for the Orthopaedically Handicapped (NIOH).
Obtaining ROI
The resultant image from classification was converted to binary image. Morphological operation like hole filling [6] was performed to fill holes of binary image. A hole is a region of dark pixels (considered as background) surrounded by white pixels (foreground) in the binary image. Hole filling in digital image is accomplished based on dilation, complementation and intersection. In our CADx, the hole filling operation was performed on the identified regions.
Due to low contrast, structure overlapping property of radiograph image, variation of shape and size of vertebrae, some small isolated regions other than vertebral column were identified. Vertebral column lies in the center of the image. So, rejecting regions from extreme left and right portion would not create any disturbance in the next steps. To avoid the isolated regions the width of the coronal radiograph was divided into 5 segments. The regions that were in the first and last segment were not considered for the later computation.
Centroid of every region was computed. The centroid possessed two values, the X-coordinate and the Y-coordinate. The vertebral column has the central position in the radiograph image. So, the mean value of Y is taken which gives the estimated vertebral column central position along the width of the image. A 90 pixels length was considered as the width of ROI for a radiograph image having size 304 × 250. A width of length 45 pixels was subtracted from the central position and a width of length 45 pixels was added to the central position. This gave the width of the ROI. The height of ROI was considered along the minimum X-coordinate and maximum X-coordinate value. Figure 3 represents outputs from this section.
Object Centerline Extraction
Obtaining Continuous Structure
If we observe the vertebral column from up-down position, it appears as a continuous structure. The endplate in the radiograph image partitions the structure into segments. Down-sampling the radiograph will reduce the information of endplate which is not required in our next computational steps of the proposed CADx. Down-sampling will simultaneously reduce the vertical edge information of the spine. This edge makes the vertebral column appear like a canal. The vertebral column which is hard tissue has higher intensity value in comparison to the regions that lie on the left and right side of the vertebral column. So, even after down-sampling, the vertical lines of the vertebrae can be distinguished from its background. The radiograph image in the experiment is down-sampled to 213 × 175. Histogram equalization is performed on the down-sampled image to get better contrast. Matlab function “histeq” is used for this operation. As only centerline of spine is required for our automated Cobb computation, we are interested with only the spine. High Gaussian blurring was performed on the radiograph image that made the spine centerline and contour more prominent like a continuous structure, reducing other information of the spine. The next operation for centerline extraction was performed on this blurred image considering only the predetermined ROI. Figure 4 shows the results from this section.
(a) Original image (b) Down-sampled image (c) Contrast enhanced image (d) Output after high Gaussian blurring where the spine in radiograph image appears like a continuous structure. The bounding box shows the ROI superimposed on the blurred image where it encapsulates the continuous structured spinal column
Centerline Extraction
Center point is considered as a single point along a row of the ROI. The pixel having maximum intensity along a row is selected as the center point of the spine for that particular row. The center point determination starts from the first row and continues till the end row of the ROI. For every row we have an approximated center point. As the vertebral column is of hard tissue, it has higher intensity in comparison to its surrounding soft tissue region. It is observed that in most cases after high Gaussian blur ring the center of the spine for any particular row of the ROI has highest intensity value in that row. Figure 5 shows an intensity plot of rows in the ROI. Center points estimated from up down position of the spine gives the vertebral column centerline. We have selected three subjects for the illustration.
(a), (d), (g), shows the intensity plot of 40th, 70th and 100th row from the three respective radiograph subjects, where the highest intensity value of the row represent the center-point of the vertebral column. (b), (e), (h) are the superimposed center points on the respective Gaussian blurred image. (c), (f), (i) are the superimposed center points on original input image
Outlier Rejection
Some outliers if present after extraction of centerline were rejected based on the median value of the Y-coordinate of the centerline. The variation of the centerline was in Y-direction of the spine. Center points having Y-coordinates within the range median −15 pixels and median +15 pixels was observed to be a suitable range to consider the real center points and reject the outliers that lie far from the center of the spine.
Polynomial Fit
A polynomial fit (curve fitting) was performed based on Y-coordinate. The operation involved interpolation that was performed on the pixel coordinated of the extracted spine centerline. A 3rd order polynomial was considered for the polynomial fit which means that the polynomial will fit through 4 points of the obtained centerline. In MATLAB for polynomial fit there is polynomial function. The “polyfit” function of order 3 was used to determine the polynomials. “polyval” function was followed to evaluate the new Y-coordinated of the polynomial curve. Figure 6 shows outputs from this section.
Cobb Angle Computation from the Centerline
Tangent
After polynomial fit on the extracted centerline, tangent was computed at every center point to get slope value. Slope value can be positive, negative or zero. For concave down graph, slopes of a tangent are decreasing as travelled from left to right and slope value increases when traveled right to left for concave up graph. Positive and negative slopes are explained in Fig. 7.
Cobb Angle Evaluation from Tangent
After calculating slope of every center point, the longest consecutive positive and negative slope series was selected as the curvature for computing the Cobb angle of the Scoliosis spine. The maximum positive slope and the minimum negative slope of the series represented the slope of the extreme vertebrae of the Scoliosis curve that tilt more severely w.r.t. the horizontal axis. The maximum positive slope and minimum negative slope values were summed together to generate the Cobb angle.
5 Results and Discussion
Radiograph images are taken from National Institute for the Orthopaedically Handicapped (Ministry of Social Justice and Empowerment) medical database. The experiments were validated on 21 digital radiograph images. For implementation of our CADx, MATLAB 2014a software was used. For every experiment of the paper, we have adjusted the input radiograph image size to 304 × 250 to get the best classification result from the used tool [16]. The supervised classification result is dependent on size of the positive and negative image database and size of the input test image. A machine specification of Intel (R) Core (TM) i3 CPU, 1.7 GHz, 4 GB RAM, 64 bit OS, Windows 7 was used. In practical a high specification RAM can speed up the CADx process. Aim of this paper was to develop a user intervention independent, reliable CADx technique.
5.1 ROI Identification Results
A series of results from our automated technique based on SVM classifier are shown in Fig. 8. The given results show the respective identified region of interest from posterior-anterior spine radiograph image. The ROI possess the vertebral column.
Classification
Sensitivity and Specificity
Performance verification metrics for classification are sensitivity and specificity. In classification ‘positive’ means ‘detected’ and ‘negative’ means ‘not detected’. Sensitivity verifies the positives that are in real detected and specificity verifies the real negatives. In our test, true positive, true negative, false positive and false negative are regarded as follows:
-
True Positive (TP) = correctly classified as spinal column
-
True Negative (TN) = correctly detected as background
-
False Positive (FP) = wrongly classified as spinal column
-
False Negative (FN) = wrongly detected as background
The equations of sensitivity and specificity are shown as follows:
The sensitivity and specificity was performed on 21 radiograph image. The image was classified into two groups the vertebral column (ROI) and the background possessing the other regions of the radiograph image. A sensitivity of 100% and specificity of 100% was obtained from our experiment.
Precision and Recall
Another metric for classification are precision and recall. Precision is the ratio of cases that are correctly classified as spinal column to the sum of cases correctly classified as spinal column and number of cases wrongly classified as spinal column. Equation of precision is expressed as follows:
Whereas recall is the ratio of cases correctly classified as spinal column to the total number of cases correctly classified as spinal column and cases wrongly classified as spinal column. The equation is illustrated as follows:
We have achieved a value of 100% for precision and have obtained a percentage of 100% for recall from 21 radiograph images.
5.2 Results from Object Centerline Extraction
The radiograph image is blurred to reduce unwanted information and obtain the spine as a continuous structure. Figure 9 shows a number of outputs after high Gaussian blur.
Output of centerline extractions are shown in Fig. 10. The Cobb angle is computed from the slopes of this extracted centerline.
A selection of polynomial fit for order 3 was taken instead of order 2 and order 4. It was observed that radiograph images gave better result for order 3 which is shown in Table 1. We have selected seven subjects for this experiment. The Cobb angle values from different polynomials are verified with the manual Cobb angle technique and it is observed that 3rd order polynomial gave most similar and consistent results considering manual as the standard Cobb angle value.
5.3 Angle Evaluation
Analysis tests were carried out for our automated Cobb angle (Lateral curvature angle from posterior-anterior) computation from 2D digital radiograph image. For every subject the analysis was performed by 3 observers on 2 different occasions. The tests were performed by Doctor, Radiologist and Researcher. It was noticed that the Cobb angle value generated from our automated CADx gave same value on a particular image for every experiment. For experimental verification, manual and digital comparison was done where manual is considered as the standard value for our verification. But in practical Manual Cobb angle measurement may itself be subject to error many times. We have taken care so that an accurate Manual Cobb angle is measured. For this we have tried to cross the line for angle computation exactly through correct corners of the endplate. Every observer for every subject performed the angle computation twice, one for manual Cobb computation and other for automated Cobb computation. The automated Cobb angles that were quite similar to the manual angle values were considered as true angles from our automated technique. ±5º changes of Cobb angle value in radiographs w.r.t. manual value are regarded to be clinically significant [12]. From our test results out of 21, 12 subjects gave significant Cobb angle values.
Relative Difference
Cobb angle assessment based on relative difference is shown in Table 2 where the Cobb angle assessment was done between automated Cobb value and manual Cobb value. The minimum and maximum relative difference values for every observer on 12 radiograph subjects (whose angle deviation is between ±5º) are given for observation (Observation 1, Observation 2).
Mean Absolute Deviation
Mean Absolute Deviation (MAD) was used as another metric for realizing the angle variation. The experiment was performed only on the subjects that gave significant results (±5º difference). An Intra-observer and inter-observer angle variation analysis based on MAD is shown in Tables 3 and 4 respectively. The tabulated results show the mean value on 12 subjects that have acceptable variance (±5º) [12] for angle computation with respect to manual computation.
Thus the results of the proposed method reflect good influence with less Cobb angle measurement variability.
6 Conclusions and Future Work
This paper presented Cobb angle evaluation from radiograph image which was based on supervised classification and centerline extraction. From the point of view some previous computerized Cobb angle computations yield good results, but still the research prefers a method that will require no user intervention at all and will give significant results for every spine radiograph image. The advantage of this approach is to have no user intervention for the total process. It was a challenging task to extract the centerline from radiograph images having low contrast, anatomical overlap and object shape variation of radiograph images. The ROI identification based on traditional SVM classifier was efficient to establish the automated CADx. And the center line extraction from this ROI gave correct results for 57.14% subjects with very less or negligible angular variability. The results and findings of this automated research is an effective step in CADx for clinical application. Future study will focus on to perform Cobb angle computation with more adaptive supervised technique and get more information from Scoliosis spine radiograph image.
References
Abuzaghleh, T., Barkana, B.: Computer-aided technique for the measurement of the Cobb angle. In: Proceedings of the WorldCom 2012 (2012)
Allen, S., Parent, E., Khorasani, M., Hill, D.L., Lou, E., Raso, J.V.: Validity and reliability of active shape models for the estimation of Cobb angle in patients with adolescent idiopathic scoliosis. J. Digit. Imaging 21(2), 208–218 (2008)
Anitha, H., Prabhu, G.K.: Automatic quantification of spinal curvature in scoliotic radiograph using image processing. J. Med. Syst. 36, 1943–1951 (2012)
Cortes, C., Vapnik, V.: Support-vector networks. Mach. Learn. 20(3), 273–297 (1995). https://doi.org/10.1007/BF00994018
Duong, L., Cheriet, F., Labelle, H.: Automatic detection of scoliotic curves in posteroanterior radiographs. IEEE Trans. Biomed. Eng. 57(7), 1143–1151 (2010)
Gonzalez, R.C.: Digital Image Processing. Prentice Hall, Upper Saddle River (2008). ISBN 9780131687288
Greiner, K.A.: Adolescent idiopathic scoliosis: radiologic decision-making. Am. Fam. Phys. 65(9), 1817–1822 (2002)
Grigorescu, S.E., Petkov, N., Kruizinga, P.: Comparison of texture features based on gabor filters. IEEE Trans. Image Process. 11(10), 1160–1167 (2002)
Huang, J.Y., Kao, P.F., Chen, Y.S.: Automatic Cobb angle measurement system by using nuclear medicine whole body bone scan. In: MVA2007 IAPR Conference on Machine Vision Applications, Tokyo, pp. 16–18 (2007)
Jeifries, B.F., Tarlton, M., De Smet, A.A., Dwyer, S.J., Brower, A.C.: Computerized measurement and analysis of scoliosis: a more accurate representation of the shape of the curve. Radiology 134, 381–385 (1980)
Li, Y., Savvides, M.: An automatic iris occlusion estimation method based on high-dimensional density estimation. IEEE Trans. Pattern Anal. Mach. Intell. 35(4), 784–796 (2013)
Morrissy, M., Goldsmith, G., Hall, E., Kehl, D., Cowie, G.: Measurement of the Cobb angle on radiographs of patients who have scoliosis. Evaluation of intrinsic error. J. Bone Joint Surg. 72, 320–327 (1999)
Murty, M.N., Raghava, R.: Support Vector Machines and Perceptrons. Springer, Berlin (2016). https://doi.org/10.1007/978-3-319-41063-0
Samuvel, B., Thomas, V., Mini, M.G.: A mask based segmentation algorithm for automatic measurement of Cobb angle from scoliosis x-ray image. Paper presented at: Proceedings of the International Conference on Advances in Computing, Communications and Informatics, Chennai, pp. 110–113 (2012)
Sardjono, T.A., Wilkinson, M.H.F., Veldhuizen, A.G., Van Ooijen, P.M.A., Purnama, K.E., Verkerke, G.J.: Automatic Cobb angle determination from radiographic images. SPINE 38(20), E1256–E1262 (2013)
Sakhi, O.: Face Detection using Support Vector Machine (SVM) (2010). http://in.mathworks.com/matlabcentral/fileexchange/29834-face-detection-using-support-vector-machine-svm/content/fdsvm11/main.m
Shaw, M., Adam, C.J., Izatt, M.T., Licina, P., Askin, G.N.: Use of the iPhone for Cobb angle measurement in scoliosis. Eur. Spine J. 21, 1062–1068 (2012)
Tanure, M.C., Pinheiro, A.P., Oliveria, A.S.: Reliability assessment of Cobb angle measurements using manual and digital methods. Spine J. 10, 769–774 (2010)
Tomasi, C., Manduchi, R.: Bilateral filtering for gray and color images. In: Proceedings of the IEEE International Conference on Computer Vision, Bombay (1998)
Tzotsos, A., Argialas, D.: Support vector machine classification for object-based image analysis. In: Blaschke, T., Lang, S., Hay, G.J. (eds.) Object-Based Image Analysis. Springer, Berlin (2008). https://doi.org/10.1007/978-3-540-77058-9_36
Wever, D.J., Tonseth, K.A., Veldhuizen, A.G., Cool, J.C., Van, H.J.R.: Curve progression and spinal growth in brace treated idiopathic scoliosis. Clinic Orthop. Relat. Res. 377, 169–179 (2000)
Yildiz, I.: Computer-assisted Cobb angle measurement from posteroanterior radiographs by a curve fitting method. Turk. J. Electr. Eng. Comput. Sci. 24, 4604–4610 (2015)
Zhang, J., Lou, E., Le, L.H., Hill, D.L., Raso, J.V., Wang, Y.: Automatic Cobb measurement of scoliosis based on fuzzy Hough transform with vertebral shape prior. J. Digit. Imaging 22(5), 463–472 (2009)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper
Kundu, R., Chakrabarti, A., Lenka, P. (2018). Automated Cobb Angle Computation from Scoliosis Radiograph. In: Mandal, J., Sinha, D. (eds) Social Transformation – Digital Way. CSI 2018. Communications in Computer and Information Science, vol 836. Springer, Singapore. https://doi.org/10.1007/978-981-13-1343-1_16
Download citation
DOI: https://doi.org/10.1007/978-981-13-1343-1_16
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-1342-4
Online ISBN: 978-981-13-1343-1
eBook Packages: Computer ScienceComputer Science (R0)