Abstract
Effective pharmacological treatment of neurodegenerative disorders has remained elusive even as medical treatments in other fields have advanced. The complex pathways underlying neurodegeneration have made identifying potent targets difficult. Confounding this is the significant overlap in mechanisms responsible for the pathologies of various neurodegenerative disorders. In the following sections, recently elucidated mechanisms of representative neurodegenerative disorders are presented. These new insights provide an opportunity for the identification of new targets that may provide more effective treatment of neurodegenerative diseases.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Nicotinamide Mononucleotide Adenylyltransferase
- Excitatory Amino Acid Carrier
- Resveratrol
- MAPK Kinase Pathway
- Amyotrophic Lateral Sclerosis (ALS)
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
20.1 Introduction
Neurodegenerative diseases are conditions with complex etiologies resulting in progressive decline in functionality and, to date, have no cure. Significant progress has been made towards the mechanisms contributing to neurodegeneration in the past two decades, providing potential targets for the development of therapeutics. Not only are unique pathologies of specific neurodegenerative diseases becoming more clear, common features among different neurodegenerative diseases are also being elucidated. Perhaps the best illustration of this is our growing understanding of pathological steps that lead to amyotrophic lateral sclerosis (or motor neuron disease), little of which was understood until the identification of the first genetic link to the disease in 1990s. The goal of this review is to explore how novel mechanistic insights of neurodegenerative diseases may provide potential targets for the development of treatments. The primary focus will be on amyotrophic lateral sclerosis for the reasons stated above, but we will also address novel approaches for the treatment of Parkinson’s disease, and various forms of dementia.
20.2 Amyotrophic Lateral Sclerosis
ALS is a progressive neurodegenerative disease that affects motor neurons in the brain and spinal cord. As with many other neurodegenerative diseases, the pathophysiology and etiology that leads to amyotrophic lateral sclerosis (ALS) remains elusive. ALS exemplifies the multifactorial nature of neurodegenerative diseases. Several genetic, molecular, and cellular factors have been implicated in the initiation and progression of the disease. That said ALS is also an example of how continued elucidation of factors that contribute to the neurodegenerative disease process can provide avenues for the development of treatments. As the disease progresses, patients lose the ability to initiate and control muscle movement. Individuals with ALS exhibit high mortality rates within 3–5 years of diagnosis as the loss in movement control progresses to paralysis. There is considerable complexity and heterogeneity in the onset, sites initially affected, and in progression of the disease that is likely a result of the numerous factors that contribute to etiology and pathophysiology of ALS.
One of the first insights into the pathology of ALS was the observation that altered superoxide dismutase 1 (SOD-1) activity is associated with familial ALS [1]. SOD-1 is a Cu/Zn-binding cytosolic enzyme that catalyzes the dismutation of the toxic superoxide anion to oxygen and peroxide, serving as cellular antioxidant. SOD-1 mutations are detected in approximately 20% of familial ALS and 3% of sporadic ALS cases [2]. Although numerous mutations of SOD-1 have been linked to ALS, its role in the pathophysiology is not clear. A common feature of the many SOD-1 mutations is the disruption of protein folding. This has led some to conclude that the misfolding and aggregation of SOD-1, but not loss of dismutase activity, contribute to its pathological role in ALS [3, 4]. Despite the lack of a defined role of SOD-1 in ALS, transgenic animal models expressing SOD-1 mutations have been a cornerstone of our growing understanding of other mechanisms that contribute to ALS [5, 6].
SOD-1 mutations remained the only known molecular link to ALS until causative mutations in TAR DNA-binding protein 43 (TDP-43) were found [7]. A pathological hallmark of ALS is the presence of ubiquitinated inclusions in surviving spinal motor neurons that results from proteasomal dysfunction [8, 9]. Some misfolded proteins are targets for ubiquitination, and the ubiquitinated forms of these proteins aggregate in various regions of the cell [10]. Both SOD-1 and TDP-43 mutations associated with ALS are known to be ubiquitinated and form aggregates in neurons, suggesting that as with other protein misfoldeding diseases (e.g., Alzheimer’s disease) cellular aggregation of altered proteins may be the causal factor in ALS [3]. Consistent with this hypothesis, ubiquitinated TDP-43 is also observed in frontotemporal dementia [7], and more recently, TDP-43 has been shown to interact with the main characteristic pathologies of Alzheimer’s disease, amyloid plaques and Tau tangles. The presence of TDP-43 in combination with the plaques and tangles was more likely to result in diagnosed Alzheimer’s dementia than plaques and tangles alone [11]. Despite these similarities with other misfolding diseases, however, where SOD-1 is concerned protein misfolding and ubiquitinated cytoplasmic inclusions do not appear to be the primary casual factor in ALS. In three distinct transgenic SOD-1 animal models of ALS, enhancing the capacity of mitochondria to buffer calcium levels resulted in reduced aggregation of SOD-1 and suppression of motor neuron death; however, muscle denervation, motor axon degeneration, and disease progression and survival remained unaltered [12]. In addition, contribution of SOD-1 mutations to the ALS is about 10–20% of familial and 1–2% sporadic cases [13]. In contrast, TDP-43 proteinopathy is present in approximately 97% of all ALS cases [14,15,16].
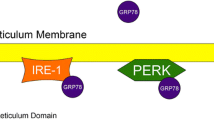
TDP-43 is a widely expressed DNA/RNA-binding protein that has a nuclear localization signal and primarily localizes to the nucleus, but can also move between the nucleus and the cytoplasm [17, 18]. The identified biological roles of TDP-43 include: inhibition of retroviral replication, RNA splicing, and nucleocytoplasmic shuttling of messenger RNA [18,19,20]. TDP-43 localization to the cytoplasm is enhanced by mutations associated with ALS and appears to contribute to neurotoxicity [9, 21]. Expression of exogenous wild-type TDP-43 in rat cortical neurons results in higher levels of protein in the nucleus without producing neurotoxicity, whereas expression of mutant TDP-43 results in significantly higher accumulation in the cytoplasm with an associated increase in neurotoxicity [22]. Overexpression of wild-type TDP-43 in transgenic mice produces the same proteinopathy and disease observed with mutant forms of TDP-43, likely related to enhanced TDP-43 accumulation in the cytoplasm [23]. A feature of many neurodegenerative diseases is the prion-like spreading of underlying pathology into specific regions of the central nervous system as the disease progresses [24,25,26,27]. In ALS, the spread of TDP-43 proteinopathy has been used to stage the course of the disease into four distinct steps based on the brain regions affected [28]. The brain regions affected correlate with the neurological deficits that manifest in ALS suggesting a link between TDP-43 proteinopathy and disease progression. Elevated levels of cytoplasmic TDP-43, as a result of overexpression or mutant forms of the protein, clearly contribute to pathogeneses of ALS, but TDP-43 is also essential for viability and motor neuron function. Complete knockout of TDP-43 in transgenic animals is lethal, and selective knockout in motor neurons, muscle, or glia alone precipitates ALS promoting some researches to refer to TDP-43 as the “Goldilocks” protein [29,30,31,32]. The role of TDP-43 in ALS appears to result from either gain or loss of function suggesting that potential therapeutics for ALS are ones that can prevent TDP-43 aggregation (Fig. 20.1) [15]. What are the factors that contribute to aggregation? In addition to mutations of TDP-43, aggregation can result from cellular stress and altered protein degradation, perhaps serving as a link between genetic and environmental factors [33, 34].
Factors that contribute to axonal damage and death of motor neurons in ALS. One of the major factors linked to ALS is TDP-43. TDP-43 is primarily a nuclear protein involved in RNA processing. In ALS TDP-43 cytosol accumulation, ubiquitination, and incorporation into protein inclusions is thought to result in motor neuron loss. Mechanisms that decrease cytosolic TDP-43 such as hUPF1-dependent nonsense-mediated decay (NMD) and Drb1 produced products (see text) that sequester and prevent its aggregation provide potential therapeutic approaches. In C. elegans model of ALS, TDP-43-induced neuronal damage and paralysis is blocked by an ortholog of human SARM1. SARM1 plays a critical role in axonal degeneration (Wallerian degeneration) that follows axonal injury. SARM1 is directly inhibited by nicotinamide nucleotide adenylyl transferase 1(NMNAT1). It remains to be seen if TDP-43-induced neuronal damage is tied to SARM1. Another protein that can promote axonal damage and astrocyte-induced necroptosis is RIPK1, providing a link between inflammation and neuronal damage
A protein that regulates TDP-43 levels is human up-frameshift protein 1 (hUPF1), an RNA helicase and regulator of nonsense-mediated mRNA decay (NMD) (Fig. 20.1) [32]. NMD is a surveillance mechanism that serves to mitigate errors in translation by recognizing anomalous mRNA transcripts and is thought to have evolved to eliminate abnormal transcripts due to routine errors in gene expression. Messenger RNAs that prematurely terminate translation because of a frameshift or nonsense mutation are selectively degraded by NMD [35]. In mammalian cells, NMD works on newly synthesized mRNA and is dependent on pre-mRNA splicing. NMD has been shown to modulate the severity of a number of diseases pointing to a possible mechanism for the development of therapeutics [36]. TDP-43 has been shown to autoregulate its synthesis by triggering nonsense-mediated RNA degradation that results from direct binding of TDP-43 to the 3′ untranslated region of its own mRNA and enhancing splicing of an intron region [37]. Barmada et al. tested the hypothesis that nonsense-mediated RNA degradation of TDP-43 was mediated by NMD [38]. In rat cortical neurons expressing wild-type or mutant forms of TDP-43, they were able to demonstrate that co-expression of hUPF1 reduced neuronal death by 40–50% through a mechanism that incorporates NMD. Similar results were observed with primary neurons expressing fused in sarcoma (FUS) protein, mutants of which are associated with familial, but not sporadic ALS [39]. FUS and TDP-43 are associated with multiple steps of RNA processing, especially in processing of long pre-mRNAs, but have largely non-overlapping RNA targets [40]. Although the results with hUPF1 are limited to a cellular model of ALS, they provide insight into a novel mechanism that can be exploited to modulate TDP-43 levels by enhancing hUPF1 activity or by targeting another component of NMD.
An alternative mechanism to preventing TDP-43 aggregation involves the protein Dbr1 (Fig. 20.1). Dbr1 is an intron lariat debranching enzyme, essential for normal processing of mRNA [41]. Reducing Dbr1 activity can block the toxic effects of TDP-43 in human neuronal cell line or in primary rat cortical neuron models of ALS [42]. An increase in the cellular pools of lariat RNA is thought to sequester TDP-43, thereby preventing its aggregation. Inhibitors of Dbr1 could be useful in the treatment of TDP-43-mediated ALS and the related neurodegenerative disease frontotemporal dementia. To that end, Montemayor et al. have solved the crystal structure of Dbr1, which should greatly aid in the development of selective small molecules with the capacity to inhibit the enzyme [43]. The feasibility of this approach is yet to be determined, however, because deletion of the DBR1 gene results in growth and morphological defects in yeast [43].
Whether protein aggregation is the pathological process that contributes to ALS is debated [44,45,46]. A long held view on the pathogenesis of Alzheimer’s disease was that amyloid plaque formation was the casual factor in the disease; however, there is evidence to suggest that amyloid plaque formation may serve a protective function [46]. Similar process may occur in ALS. A study by Yonashiro et al. has uncovered a mechanism by which transcripts that stall ribosomal activity result in the tagging of the nascent polypeptide chain for aggregation, and a protein (Listerin/Ltn1) implicated in ALS-like symptoms is integral to this process [47]. What isn’t known is whether the aggregates produced by ribosome-associated quality control are the same aggregates as those that result from mutants of TDP-43, FUS, or SOD-1.
Observations that link immune function to development of the disease provide another avenue for the development of potential therapeutics for ALS. Although ALS lacks the hallmark signs of autoimmune disease, the infiltration of circulating lymphocytes, factors that stimulate inflammation are present in central nervous system of people with ALS [48]. The role of immune response in ALS, however, appears to be mixed: protective or potentially destructive [49,50,51]. Recent studies in a C. elegans model of ALS, in which the animals were induced to undergo motor degeneration by the expression of TDP-43 or FUS, degeneration of motor neurons was induced by an innate immune response mediated by TIR-1 [52]. TIR-1 plays an integral role in response to microbial infection as part of the innate immune system in C. elegans [43]. Deleting the tir-1 gene in C. elegans results in significantly reduced neurodegeneration and paralysis induced by expression of TDP-43 or FUS, which demonstrates the link between immune function and ALS disease progression [53]. The human ortholog of the tir-1 gene, SARM1 (sterile alpha and TIR motif containing 1), plays a role in maintaining the integrity of neurons [54, 55]. Mitochondrial dysfunction, a feature of multiple neurodegenerative diseases, in sensory neurons causes neuron death through a SARM1-dependent mechanism [56]. SARM1 has also been implicated in Wallerian degeneration, a localized form of programmed axon destruction that occurs in response to axon trauma or disease (Fig. 20.1) [57]. Axon degeneration is an early pathological event in many neurological disorders, including ALS [58]. In response to injury, SARM1 promotes axonal degeneration by depleting cellular levels of NAD+ (nicotinamide adenine dinucleotide) limiting energy generation in axons [59]. In SARM1 knockout mice mechanical severed axons remained intact 24 h post injury, whereas axonal degeneration was evident in mice carrying functional SARM1. Yang et al. have provided insight into the mechanisms by which axonal damage results in energy deficit near the sight of injury [60]. They show that SARM1 must activate the MAPK kinase pathway to initiate the process, and that SARM1 activation of the MAPK kinase pathway can be blocked by cytosolic version of nicotinamide mononucleotide adenylyl transferase 1 (NMNAT1) (Fig. 20.1). NMNAT1 is one of three homologous enzymes involved in the synthesis of NAD+ that is known to have neuroprotective effects [61,62,63]. SARM1 and NMNATs appear to have apposing effects in neurodegenerative process [64]. NMNAT2 deletion causes neurodegeneration that is reversed by eliminating the expression of SARM1 [64, 65]. Surprisingly, NMNAT1 counters SARM1 effects on NAD+ depletion not by increasing NAD+ synthesis but by blocking injury-induced SARM1-dependent NAD+ depletion through a mechanism that is still to be determined [66]. Inhibitors of SARM1 and activiators of NMNATs make for intriguing therapeutic approaches for ALS and other axonal degeneration diseases. SARM1 contains a SAM (sterile α motif) or TIR (Toll-interleukin-1 receptor) domains that must interact for SARM1-induced neurodegeneration [54]. In addition, unique motifs in the SARM1 domain have been identified that are essential for its prodegeneration effects pointing to possible mechanisms that could be targeted by small molecules [67].
If SARM1 contributes to axonal degeneration, what contributes to motor neuron death? Are there other inflammatory processes that contribute to ALS? The answer to these questions comes from studies that measured the effect of astrocytes derived from patients with either familial or sporadic cases of ALS on co-cultured motor neurons [68]. When cells were co-cultured, the derived astrocytes produced toxic effects on the motor neurons in culture. This effect is specific to astrocytes isolated from ALS patients and occurs through necroptosis, a form of programmed necrosis [69, 70]. Necroptosis can be reduced by inhibition of RIPK1 (receptor-interacting kinase 1) (Fig. 20.1) [71]. RIPK1 is a critical regulator of cell death and inflammation [72]. Recent work by Ito et al. has linked RIPK1 to ALS; in transgenic mice with an optineurin (OPTN, mutations of which have been linked to familial and sporadic forms of ALS) knockout, the loss of OPTN resulted in demyelination and axonal degeneration through processes that required RIPK1 [73, 74]. Selective inhibitors of RIPK1 have already been identified and characterized, and have shown the ability to block necroptosis, providing the necessary tools to further explore the potential of RIPK1 as a therapeutic target [75, 76].
20.3 Parkinson’s Disease
Parkinson’s disease (PD) is a chronic neurodegenerative disorder characterized by a wide range of motor symptoms and pathological features, some or all of which may be present in any individual patient [77]. While the ultimate cause of PD is unknown, both genetic and environmental factors appear to be involved, and PD etiology suggests multiple potential mechanisms involving dopaminergic neurons and disruptions in neurotransmitter metabolism [78]. Currently, there is no cure for PD, and symptoms are managed primarily through routes that attenuate the effects of disruptions in dopamine metabolism [79]. As more underlying mechanisms are elucidated, additional targets for potential pharmacotherapy are coming into focus. One such target is protein deglycase (DJ-1, alternatively called Parkinson disease protein 7 or PARK7) [80].
Mutations of the PARK7/DJ-1 gene are responsible for one form of recessive early-onset Parkinson’s disease, making PARK7 an attractive target for pharmacotherapy [81]. There is growing evidence that the protein product of this gene, PARK7, along with homologs, functions as glyoxal- and methylglyoxalases, thus attenuating the maturation of early glycation products into advanced glycation end products (AGEs) [82, 83]. Over time, AGEs promote the cross-linking of several classes of biomolecules, including proteins, lipids, and nucleic acids. These cross-linked biomolecules result in vascular and tissue damage and contribute to the underlying pathology of not only Parkinson’s disease, but other disorders including other neurodegenerative disorders, diabetes, atherosclerosis, cardiovascular disease, and chronic renal failure [84,85,86].
One significant protein that exhibits extensive cross-linking by AGEs is α-synuclein [87], which is the primary protein component of Lewy bodies [88]. While found in other tissues, most notably at the neuromuscular junctions of cardiac and skeletal muscles, the primary location of expression is in the presynaptic neuron [89]. The native function of the α-synuclein appears to be the regulation of neurotransmitter transport, acting at the early stages of vesicular trafficking and possibly dopamine re-uptake [90, 91]. There is a high degree of homology among the synuclein protein family and they appear to have at least some functional redundancy [90, 92]. The aggregation of α-synuclein into a Lewy body structure is kinetically mediated by the equilibrium which exists between the membrane-bound, helix-rich monomer and a pathologic α-sheet-containing conformer which can aggregate into insoluble fibrils, making up the fibrous protein component of the Lewy body [93,94,95]. Even prior to Lewy body formation, the synuclein aggregates exhibit neurotoxicity [95,96,97]. AGE-cross-linking presumably increases toxicity by stabilizing the aggregation of the ß-sheet conformer, driving the equilibrium towards oligomer formation [98, 99].
Targeting PARK7 would presumably be a viable route towards clearing certain early glycation products, thus attenuating the formation of AGE-cross-linked synuclein aggregates. Methylglyoxal forms as a spontaneous by-product of triose degradation during glycolysis and covalently links to various amino acid side chains, including cysteine, arginine, and lysine [100]. The covalent modification of proteins by methylglyoxal can be reversed at all three of these amino acids by the actions of PARK7 and its prokaryotic homolog, YajL, releasing the methylglyoxal as lactate [82, 101, 102].
PARK7 deficiency has been shown to result in increased oxidative stress through the loss of ROS quenching capacity [103, 104]. This effect on neuron oxidative state may occur through the regulation of amino acid uptake specifically that of glutamate/glutamine and serine [105, 106]. Serine can potentially act as a precursor to glycine and cysteine synthesis. Glycine and cysteine, along with glutamate, which can be taken up directly or synthesized from glutamine, are in turn the precursors to glutathione (GSH). Decreased uptake and synthesis capacity of these amino acids could result in a GSH deficiency [107]. Indeed, model systems of PARK7 deficiency have been shown to exhibit decreased biosynthesis of serine and GSH as well as a downregulation in the expression of key enzymes involved in cysteine, glutamate, and GSH metabolism [106, 108, 109].
PARK7 may exert influence through its actions as a sensor for oxidative stress. Under oxidative conditions, alterations to PARK7 cysteine residues lead to nuclear and mitochondrial translocation, where it may act as a transcription factor [110, 111]. In addition to the aforementioned effect on glutathione pathways, PARK7 deficiency results in decreased expression of the lipid raft proteins flotillin-1 and caveolin-1, which have been shown to be involved in functioning of dopamine transporter (DAT) and excitatory amino acid carrier (EAAT) [105, 112,113,114]. The transcription activity of PARK7 also influences dopamine synthesis directly, as tyrosine hydroxylase is also upregulated [110].
The involvement of PARK7 by these mechanisms in the pathogenesis of PD is supported by the observation that amphetamine use increases the risk of developing PD [115, 116]. Amphetamines exert their effect through disruption of dopamine transporter and endocytosis of cell membrane EAATs, which would disrupt glutamate metabolism in much the same way as PARK7 dysfunction [117, 118].
PARK7 may also influence protein function directly. Oxidation-triggered translocation to the mitochondria results in PARK7 interactions with Complex I and Complex II activity, which is diminished with PARK7 deficiency [111, 119]. PARK7 potentially acts as a protein chaperone for cysteine-rich proteins by forming mixed disulfides with the thiol proteome [102]. The prokaryote PARK7 homolog YajL has been shown to chaperone and other thiol containing biomolecules as well, and this activity may allow PARK7 to participate in the reduction of oxidized thiols and may be a mechanistic route towards the observed attenuation of α-synuclein aggregation [102, 120, 121].
Mechanisms of other neurodegenerative disorders may also be influenced by PARK7. In addition to its role as a general thiol chaperone, PARK7 has also been identified as a copper chaperone with peroxidase activity involved in the transfer of copper ion to activate SOD-1 [122, 123]. The interaction between PARK7 and SOD-1 may be an important key to ALS treatment, as cell culture studies and animal models have shown PARK7 overexpression attenuates oxidative damage and increases cell viability in SOD-1 mutant neurons and mice [124].
20.4 Dementia and mTOR
A more recent therapeutic target for multiple dementias has been the inhibition of the serine/threonine protein kinase mechanistic target of rapamycin (mTOR). Both dementias and increased mTOR activity seem to create cells with an inability for cellular housekeeping of macromolecules, leading to protein aggregates in the case of dementias. Research into the mTOR pathway was launched in 1975 when rapamycin, an inhibitor to mTOR found in soil on Easter Island, was shown to act as an antifungal antibiotic [125]. Since that time, it has been elucidated that mTOR acts as a central detector coordinating cell action based on nutrient and stress sensing (Fig. 20.2). Rapamycin, hailed as a fountain of youth compound, has been found to increase lifespan in organisms ranging from yeast, to nematodes, to fruit flies, and in mice [125,126,127,128,129]. Lifespan increased by as much as 100% in mice, with an average increased lifespan of ~20% [130]. Caloric restriction, which is also known to decrease mTOR activity, likewise has been shown to increase lifespans across many genera, and recently a 30% calorically restricted diet has been shown to increase lifespan in rhesus monkeys by 15% [131, 132]. Resveratrol, a compound found in red wine among other foods, has been extensively investigated as a compound that promotes longevity and has been found to inhibit the mTOR pathway. While most of the work with resveratrol has investigated its ability to decrease DNA methylation thereby preventing genes such as tumor suppressors from being shut off, it has recently been shown the resveratrol directly binds to mTOR at the same site as ATP, which presents an elegant mechanism to mimic caloric restriction at a molecular level [133,134,135,136,137,138]. There have been 14 clinical trials of resveratrol for various dementias with eight in phase 1, three in phase 2, and three in phase 3 (clinicaltrials.gov as of February 21st, 2017). In general, resveratrol has proven safe but not very effective. Two of the phase 3 trails were targeted at AD, with one being withdrawn (clinicaltrails.gov NCT00743743) and the other completing but not yet reporting results (clinicaltrails.gov NCT00678431). There are promising phase 2 trials targeting AD. A 2015 study showed positive resveratrol dose-dependent effects even though only 1% of resveratrol passed the blood brain barrier to reach the nervous system (NCT01504854) [139]. More recently, a phase 4 study completed in December 2016 is comparing dietary interventions of resveratrol supplementation, omega-3 supplementation, and caloric restriction. In a second phase, the addition of physical/cognitive training in conjunction with the supplements is being assessed. Outcomes will measure any change in the Alzheimer Disease Assessment scale, functional/structural brain changes, and plasma biomarkers, but results have not been released yet (clinicaltrails.gov NCT01219244). The last phase 3 trial of resveratrol is targeting HD and is still in the recruiting phase (clinicaltrials.gov NCT02336633).
mTOR signaling and inhibitors: (a) Growth factors, food, and cancer all cause activation of PI3K and inactivation of AMPK which cause an increase in mTOR activity in both complexes mTORC1 and mTORC2 and decrease the level of cellular autophagy. Restoring autophagy either through mTOR inhibitors (rapalogs, ATP-competitive inhibitors, pan-mTOR inhibitors, or dual PI3K/mTOR inhibitors) or reduced caloric intake (growth signals) all restore autophagy which can clear Aß and Tau, thereby reducing amyloid plaques and tangles, respectively. (b) A simplified mTORC pathway showing the positive effects rapamycin and its analogs have by increasing autophagy compared to the detrimental outcomes of increased mTORC signaling. Beneficial and deleterious interactions or macromolecules are shown in green and red, respectively. Proteins found in both mTOR1 and mTOR2 are colored blue. Abbreviations: AMPK AMP-activated protein kinase, DEPTOR DEP domain containing mTOR-interacting protein, FKBP12 FK506/rapamycin binding protein, FOXO Forkhead box protein, mLST8 mammalian lethal with sec-13 protein 8 (also known as G𝛽L), mPMP mitochondrial permeability transition pore, mSin1 Mammalian Stress-activated map kinase-Interacting protein 1, mTOR Mammalian Target Of Rapamycin, mTORC Mammalian Target Of Rapamycin Complex, PTEN Phosphatase and tensin homolog, PRAS40 proline-rich Akt substrate 40 kDa, protor1/2 protein observed with rictor 1 and 2, RAPTOR Regulatory-Associated Protein of mammalian Target Of Rapamycin, RICTOR Rapamycin-Insensitive Companion of mTOR, Sirt1 Sirtuin-1, telO2 telomere maintenance 2, tti1 telO2-Interacting Protein 1
mTOR is actually a component of two protein complexes termed mechanistic target of rapamycin (mTORC1 and mTORC2), both of which contain DEPTOR, mLST8, telO2, and tti1 (DEP domain containing mTOR-interacting protein, mammalian lethal with sec-13 protein 8 [also known as G𝛽L], telomere maintenance 2, and telO2-Interacting Protein 1, respectively). The mTORCs differ in that mTORC1 alone contains mSIN1, RICTOR, and Protor (mammalian stress-activated map kinase-interacting protein 1, and rapamycin-insensitive companion of mTOR, and protein observed with rictor 1 and 2, respectively), while mTORC2 alone contains PRAS40 and RAPTOR (proline-rich Akt substrate 40 kDa, and regulatory-associated protein of mammalian target of rapamycin, respectively) (Fig. 20.2a). Much more is known about mTORC1 signaling compared to mTORC2; however, mTORC2 can activate mTORC1 through phosphorylation and activation of AKT. It has been reported that both amyloid-beta (Aß) increases mTOR activity and that mTOR increases Aß levels [140, 141]. Interestingly, Aß has been shown to induce mTOR hyperactivity through PRAS40 that is unique to mTORC1 [142].
Growth factors activate mTORCs by binding growth factor receptors, which activate PI3K. While rapamycin inhibition of mTORC1 complex has proven beneficial for many disease states, long-term rapamycin use also inhibits mTORC2 which some have suggested could cause unforeseen deleterious side effects [143]. However, pan-mTOR inhibitors (which block both mTORC1 and mTORC2) have been shown to be beneficial [143]. There are now compounds which preferentially target mTORC1 (rapalogs), both mTORC1 and 2 over PI3K (pan-mTOR inhibitors), or target all three components equally (dual PI3K/mTOR inhibitors) (Fig. 20.2a).
A cellular theme that has been repeatedly supported is that, while mTOR and aging in general inhibit autophagy (cleaning up of macromolecules in a cell), maintaining a high level of autophagy via caloric restriction, sirtuin, or rapalogs promotes longevity [144]. Neurodegenerative diseases seem particularly susceptible to low autophagy activity, increasing the speed with which amyloid aggregates form. Calorically restricted cells increase autophagy via two well-established pathways. Cells in a low energy state have decreased PI3K activity, thereby lowering Akt activity, which in turn lowers mTORC1 (Akt inhibits Tsc1/2 which inhibits mTORC1). Normally mTORC1 inhibits sirtuin (Sirt1) which in turn activates FOXO, increasing, cellular autophagy. Calorically restricted cells also have increased AMPK activity, which activates Ulk1 also leading to increased autophagy. The increased cellular autophagy has multiple beneficial effects. Autophagy offers a molecular mechanism to alleviate the burden posed by the general phenomena of amyloid proteins in the various dementias. A low level of autophagy also leads to necrosis over apoptosis, which increases inflammation via the immune system. Intracellular stress is known to signal through Bcl-2 and cause increased calcium levels opening the mitochondrial permeability transition pore (mPTP) which can lead to caspase-dependent intrinsic apoptosis [145, 146]. The mPTP can exist in three states: closed, transiently open in low conductance, and permanently open in high conductance [147,148,149]. When excessively open, the mPTP causes an almost complete loss of ATP production, due to depolarization of the mitochondria, and leads to caspase-independent necrosis due to lack of energy to follow the controlled apoptotic path (Fig. 20.2a) [150].
While mitochondrial dysfunction has been implicated in various dementia including Parkinson disease, amyotrophic lateral sclerosis, Huntington disease, and Alzheimer disease, methods to target it have trailed [151,152,153,154]. Upregulation of the mTOR pathway is now known to increase oxidative stress. Oxidative stress has been targeted with antioxidant therapy and it has been found conjugating a cation compound to the antioxidant can greatly increase localization to the mitochondria due to its negative potential of 165 mV across the inner membrane [155]. Uptake of antioxidants has been shown to increase up to 80-fold while potency has increased up to 800-fold [156]. Most of the early targeting of the mTOR pathway was for cancer patients with many cancers showing increased mTOR pathway signaling. Not only is rapamycin FDA approved (Sirolimus) but follow on rapamycin analogs (rapalogs) are also FDA approved. For example, everolimus (Afinitor), temsirolimus (Torisel), and ridaforolimus are used for various cancers, with sirolimus and everolimus also particularly being used as immunosuppressants for use after organ transplants [130, 157]. There are 417 clinical trials listed as targeting mTOR, and of those 23 are targeting neurodegenerative diseases (clinicaltrials.gov as of February 21st, 2017). For example, tamoxifen has been shown to increase autophagy [158] like the mTOR inhibitors mentioned earlier, which is why there is a phase 1–2 clinical trial using tamoxifen for ALS (clinicaltrials.gov NCT02336633). The increased autophagy should decrease TDP-43 accumulation seen the in multiple neurogenerative diseases, but results have not yet been published for this trial. Interestingly, the combination of an anticancer therapeutic (CSC-3436) and tamoxifen was shown to synergistically kill cancer cells but switch cells from an autophagic to apoptotic state [159], suggesting combination therapies involving mTOR will likely take more time to elucidate. The fact that inhibition of mTOR seems to reduce dementia and extend lifespan raises the hope of not only longer life but also an increase in years of quality.
Conclusions
While the aforementioned disorders, on the surface, appear to be distinct and unrelated, many of the underlying mechanisms can offer insights into other diseases of neurodegeneration. The mitigation of oxidative stress has long been a focus in preventing the pathogenesis of many classes of neurodegenerative dysfunctions. In the past, with limited knowledge of mechanistic pathways leading to increased oxidative conditions, elevation of antioxidants, both exogenous and endogenous, has been the point of concentration. As seen above, a greater understanding of the pathways that either exacerbate or attenuate oxidative stress is revealing a number of regulation points to target for future therapy. A generation ago, the analogy of antioxidants being akin to a bullet-proof vest to intercept free-radicals was often evoked. Using this same analogy, we can equate the increasing understanding of signaling mechanisms and regulating pathways of oxidative stress as identifying the shooter, thus rather than trying to deflect damaging oxidative agents, by targeting these pathways, we can instead decrease the generation of these agents. As a greater understanding of the regulating pathways of neurodegeneration comes to light, the ability to develop pharmacotherapy to manipulate these pathways and improve treatment options will follow.
References
Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, Hentati A, et al. Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature. 1993;362(6415):59–62.
Shaw CE, Enayat ZE, Powell JF, Anderson VER, Radunovic A, Al-Sarraj S, et al. Familial amyotrophic lateral sclerosis: molecular pathology of a patient with a SOD1 mutation. Neurology. 1997;49(6):1612–6.
Taylor JP, Brown RH Jr, Cleveland DW. Decoding ALS: from genes to mechanism. Nature. 2016;539(7628):197–206.
Bruijn LI, Houseweart MK, Kato S, Anderson KL, Anderson SD, Ohama E, et al. Aggregation and motor neuron toxicity of an ALS-linked SOD1 mutant independent from wild-type SOD1. Science. 1998;281(5384):1851.
Julien J-P, Kriz J. Transgenic mouse models of amyotrophic lateral sclerosis. Biochim Biophys Acta. 2006;1762(11–12):1013–24.
McGoldrick P, Joyce PI, Fisher EMC, Greensmith L. Rodent models of amyotrophic lateral sclerosis. Biochim Biophys Acta. 2013;1832(9):1421–36.
Sreedharan J, Blair IP, Tripathi VB, Hu X, Vance C, Rogelj B, et al. TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science. 2008;319(5870):1668.
Leigh P, Whitwell H, Garofalo O, Buller J, Swash M, Martin J, et al. Ubiquitin-immunoreactive intraneuronal inclusions in amyotrophic lateral sclerosis. Brain. 1991;114(2):775–88.
Arai T, Hasegawa M, Akiyama H, Ikeda K, Nonaka T, Mori H, et al. TDP-43 is a component of ubiquitin-positive tau-negative inclusions in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Biochem Biophys Res Commun. 2006;351(3):602–11.
Takalo M, Salminen A, Soininen H, Hiltunen M, Haapasalo A. Protein aggregation and degradation mechanisms in neurodegenerative diseases. Am J Neurodegener Dis. 2013;2(1):1–14.
James BD, Wilson RS, Boyle PA, Trojanowski JQ, Bennett DA, Schneider JA. TDP-43 stage, mixed pathologies, and clinical Alzheimer’s-type dementia. Brain. 2016;139(11):2983.
Parone PA, Da Cruz S, Han JS, McAlonis-Downes M, Vetto AP, Lee SK, et al. Enhancing mitochondrial calcium buffering capacity reduces aggregation of misfolded SOD1 and motor neuron cell death without extending survival in mouse models of inherited amyotrophic lateral sclerosis. J Neurosci. 2013;33(11):4657.
Saccon RA, Bunton-Stasyshyn RKA, Fisher EMC, Fratta P. Is SOD1 loss of function involved in amyotrophic lateral sclerosis? Brain. 2013;136(8):2342–58.
Ling S-C, Polymenidou M, Cleveland Don W. Converging mechanisms in ALS and FTD: disrupted RNA and protein homeostasis. Neuron. 2013;79(3):416–38.
Scotter EL, Chen H-J, Shaw CE. TDP-43 proteinopathy and ALS: insights into disease mechanisms and therapeutic targets. Neurotherapeutics. 2015;12(2):352–63.
Mackenzie IRA, Bigio EH, Ince PG, Geser F, Neumann M, Cairns NJ, et al. Pathological TDP-43 distinguishes sporadic amyotrophic lateral sclerosis from amyotrophic lateral sclerosis with SOD1 mutations. Ann Neurol. 2007;61(5):427–34.
Ou SH, Wu F, Harrich D, García-Martínez LF, Gaynor RB. Cloning and characterization of a novel cellular protein, TDP-43, that binds to human immunodeficiency virus type 1 TAR DNA sequence motifs. J Virol. 1995;69(6):3584–96.
Winton MJ, Igaz LM, Wong MM, Kwong LK, Trojanowski JQ, Lee VMY. Disturbance of nuclear and cytoplasmic TAR DNA-binding protein (TDP-43) induces disease-like redistribution, sequestration, and aggregate formation. J Biol Chem. 2008;283(19):13302–9.
Ayala YM, Zago P, Ambrogio A, Xu Y-F, Petrucelli L, Buratti E, et al. Structural determinants of the cellular localization and shuttling of TDP-43. J Cell Sci. 2008;121(22):3778.
Wang I, Wu LS, Chang HY, Shen CKJ. TDP-43, the signature protein of FTLD-U, is a neuronal activity-responsive factor. J Neurochem. 2008;105(3):797–806.
Neumann M, Sampathu DM, Kwong LK, Truax AC, Micsenyi MC, Chou TT, et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314(5796):130.
Barmada SJ, Skibinski G, Korb E, Rao EJ, Wu JY, Finkbeiner S. Cytoplasmic mislocalization of TDP-43 is toxic to neurons and enhanced by a mutation associated with familial ALS. J Neurosci. 2010;30(2):639.
Wils H, Kleinberger G, Janssens J, Pereson S, Joris G, Cuijt I, et al. TDP-43 transgenic mice develop spastic paralysis and neuronal inclusions characteristic of ALS and frontotemporal lobar degeneration. Proc Natl Acad Sci. 2010;107(8):3858–63.
Braak H, Del Tredici K. Where, when, and in what form does sporadic Alzheimer’s disease begin? Curr Opin Neurol. 2012;25(6):708–14.
Braak H, Tredici KD, Rüb U, de Vos RAI, Jansen Steur ENH, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003;24(2):197–211.
Cushman M, Johnson BS, King OD, Gitler AD, Shorter J. Prion-like disorders: blurring the divide between transmissibility and infectivity. J Cell Sci. 2010;123(8):1191.
Smethurst P, Newcombe J, Troakes C, Simone R, Chen Y-R, Patani R, et al. In vitro prion-like behaviour of TDP-43 in ALS. Neurobiol Dis. 2016;96:236–47.
Brettschneider J, Del Tredici K, Toledo JB, Robinson JL, Irwin DJ, Grossman M, et al. Stages of pTDP-43 pathology in amyotrophic lateral sclerosis. Ann Neurol. 2013;74(1):20–38.
Wu L-S, Cheng W-C, Shen CKJ. Targeted depletion of TDP-43 expression in the spinal cord motor neurons leads to the development of amyotrophic lateral sclerosis-like phenotypes in mice. J Biol Chem. 2012;287(33):27335–44.
Yang C, Wang H, Qiao T, Yang B, Aliaga L, Qiu L, et al. Partial loss of TDP-43 function causes phenotypes of amyotrophic lateral sclerosis. Proc Natl Acad Sci. 2014;111(12):E1121–E9.
Kabashi E, Lin L, Tradewell ML, Dion PA, Bercier V, Bourgouin P, et al. Gain and loss of function of ALS-related mutations of TARDBP (TDP-43) cause motor deficits in vivo. Hum Mol Genet. 2010;19(4):671–83.
Diaper DC, Adachi Y, Lazarou L, Greenstein M, Simoes FA, Di Domenico A, et al. Drosophila TDP-43 dysfunction in glia and muscle cells cause cytological and behavioural phenotypes that characterize ALS and FTLD. Hum Mol Genet. 2013;22(19):3883–93.
van Eersel J, Ke YD, Gladbach A, Bi M, Götz J, Kril JJ, et al. Cytoplasmic accumulation and aggregation of TDP-43 upon proteasome inhibition in cultured neurons. PLoS One. 2011;6(7):e22850.
Colombrita C, Zennaro E, Fallini C, Weber M, Sommacal A, Buratti E, et al. TDP-43 is recruited to stress granules in conditions of oxidative insult. J Neurochem. 2009;111(4):1051–61.
Conti E, Izaurralde E. Nonsense-mediated mRNA decay: molecular insights and mechanistic variations across species. Curr Opin Cell Biol. 2005;17(3):316–25.
Frischmeyer PA, Dietz HC. Nonsense-mediated mRNA decay in health and disease. Hum Mol Genet. 1999;8(10):1893–900.
Polymenidou M, Lagier-Tourenne C, Hutt KR, Huelga SC, Moran J, Liang TY, et al. Long pre-mRNA depletion and RNA missplicing contribute to neuronal vulnerability from loss of TDP-43. Nat Neurosci. 2011;14(4):459–68.
Barmada SJ, Ju S, Arjun A, Batarse A, Archbold HC, Peisach D, et al. Amelioration of toxicity in neuronal models of amyotrophic lateral sclerosis by hUPF1. Proc Natl Acad Sci. 2015;112(25):7821–6.
Neumann M, Rademakers R, Roeber S, Baker M, Kretzschmar HA, Mackenzie IRA. A new subtype of frontotemporal lobar degeneration with FUS pathology. Brain. 2009;132(11):2922.
Lagier-Tourenne C, Polymenidou M, Hutt KR, Vu AQ, Baughn M, Huelga SC, et al. Divergent roles of ALS-linked proteins FUS/TLS and TDP-43 intersect in processing long pre-mRNAs. Nat Neurosci. 2012;15(11):1488–97.
Kim J-W, Kim H-C, Kim G-M, Yang J-M, Boeke JD, Nam K. Human RNA lariat debranching enzyme cDNA complements the phenotypes of Saccharomyces cerevisiae dbr1 and Schizosaccharomyces pombe dbr1 mutants. Nucleic Acids Res. 2000;28(18):3666–73.
Armakola M, Higgins MJ, Figley MD, Barmada SJ, Scarborough EA, Diaz Z, et al. Inhibition of RNA lariat debranching enzyme suppresses TDP-43 toxicity in ALS disease models. Nat Genet. 2012;44(12):1302–9.
Montemayor EJ, Katolik A, Clark NE, Taylor AB, Schuermann JP, Combs DJ, et al. Structural basis of lariat RNA recognition by the intron debranching enzyme Dbr1. Nucleic Acids Res. 2014;42(16):10845–55.
Merz Gregory E, Borbat Peter P, Pratt Ashley J, Getzoff Elizabeth D, Freed Jack H, Crane Brian R. Copper-based pulsed dipolar ESR spectroscopy as a probe of protein conformation linked to disease states. Biophys J. 2014;107(7):1669–74.
Pratt AJ, Shin DS, Merz GE, Rambo RP, Lancaster WA, Dyer KN, et al. Aggregation propensities of superoxide dismutase G93 hotspot mutants mirror ALS clinical phenotypes. Proc Natl Acad Sci. 2014;111(43):E4568–E76.
Lansbury PT, Lashuel HA. A century-old debate on protein aggregation and neurodegeneration enters the clinic. Nature. 2006;443(7113):774–9.
Yonashiro R, Tahara EB, Bengtson MH, Khokhrina M, Lorenz H, Chen K-C, et al. The Rqc2/Tae2 subunit of the ribosome-associated quality control (RQC) complex marks ribosome-stalled nascent polypeptide chains for aggregation. elife. 2016;5:e11794.
McCombe PA, Henderson RD. The role of immune and inflammatory mechanisms in ALS. Curr Mol Med. 2011;11(3):246–54.
Papadimitriou D, Le Verche V, Jacquier A, Ikiz B, Przedborski S, Re DB. Inflammation in ALS and SMA: sorting out the good from the evil. Neurobiol Dis. 2010;37(3):493–502.
Zhao W, Beers DR, Appel SH. Immune-mediated mechanisms in the pathoprogression of amyotrophic lateral sclerosis. J Neuroimmune Pharmacol. 2013;8(4):888–99.
Malaspina A, Puentes F, Amor S. Disease origin and progression in amyotrophic lateral sclerosis: an immunology perspective. Int Immunol. 2015;27(3):117–29.
Vaccaro A, Tauffenberger A, Aggad D, Rouleau G, Drapeau P, Parker JA. Mutant TDP-43 and FUS cause age-dependent paralysis and neurodegeneration in C. elegans. PLoS One. 2012;7(2):e31321.
Vérièpe J, Fossouo L, Parker JA. Neurodegeneration in C. elegans models of ALS requires TIR-1/Sarm1 immune pathway activation in neurons. Nat Commun. 2015;6:7319.
Gerdts J, Summers DW, Sasaki Y, DiAntonio A, Milbrandt J. Sarm1-mediated axon degeneration requires both SAM and TIR interactions. J Neurosci. 2013;33(33):13569–80.
Osterloh JM, Yang J, Rooney TM, Fox AN, Adalbert R, Powell EH, et al. dSarm/Sarm1 is required for activation of an injury-induced axon death pathway. Science. 2012;337(6093):481.
Summers DW, DiAntonio A, Milbrandt J. Mitochondrial dysfunction induces Sarm1-dependent cell death in sensory neurons. J Neurosci. 2014;34(28):9338–50.
Gaudet AD, Popovich PG, Ramer MS. Wallerian degeneration: gaining perspective on inflammatory events after peripheral nerve injury. J Neuroinflammation. 2011;8:110.
Wang JT, Medress ZA, Barres BA. Axon degeneration: molecular mechanisms of a self-destruction pathway. J Cell Biol. 2012;196(1):7–18.
Gerdts J, Brace EJ, Sasaki Y, DiAntonio A, Milbrandt J. SARM1 activation triggers axon degeneration locally via NAD+ destruction. Science. 2015;348(6233):453.
Yang J, Wu Z, Renier N, Simon DJ, Uryu K, Park DS, et al. Pathological axonal death through a MAPK cascade that triggers a local energy deficit. Cell. 2015;160(1):161–76.
Verghese PB, Sasaki Y, Yang D, Stewart F, Sabar F, Finn MB, et al. Nicotinamide mononucleotide adenylyl transferase 1 protects against acute neurodegeneration in developing CNS by inhibiting excitotoxic-necrotic cell death. Proc Natl Acad Sci. 2011;108(47):19054–9.
Sasaki Y, Vohra BPS, Baloh RH, Milbrandt J. Transgenic mice expressing the Nmnat1 protein manifest robust delay in axonal degeneration in vivo. J Neurosci. 2009;29(20):6526–34.
Coleman MP, Conforti L, Buckmaster EA, Tarlton A, Ewing RM, Brown MC, et al. An 85-kb tandem triplication in the slow Wallerian degeneration (Wld(s)) mouse. Proc Natl Acad Sci U S A. 1998;95(17):9985–90.
Gerdts J, Summers Daniel W, Milbrandt J, DiAntonio A. Axon self-destruction: new links among SARM1, MAPKs, and NAD+ metabolism. Neuron. 2016;89(3):449–60.
Gilley J, Orsomando G, Nascimento-Ferreira I, Coleman Michael P. Absence of SARM1 rescues development and survival of NMNAT2-deficient axons. Cell Rep. 2015;10(12):1974–81.
Sasaki Y, Nakagawa T, Mao X, DiAntonio A. Milbrandt J. NMNAT1 inhibits axon degeneration via blockade of SARM1-mediated NAD+ depletion. elife. 2016;5:e19749.
Summers DW, Gibson DA, DiAntonio A. Milbrandt J. SARM1-specific motifs in the TIR domain enable NAD+ loss and regulate injury-induced SARM1 activation. Proc Natl Acad Sci. 2016;113(41):E6271–E80.
Haidet-Phillips AM, Hester ME, Miranda CJ, Meyer K, Braun L, Frakes A, et al. Astrocytes from familial and sporadic ALS patients are toxic to motor neurons. Nat Biotechnol. 2011;29(9):824–8.
Re DB, Verche VL, Yu C, Amoroso MW, Politi KA, Phani S, et al. Necroptosis drives motor neuron death in models of both sporadic and familial ALS. Neuron. 2014;81(5):1001–8.
Pasparakis M, Vandenabeele P. Necroptosis and its role in inflammation. Nature. 2015;517(7534):311–20.
Zhao H, Jaffer T, Eguchi S, Wang Z, Linkermann A, Ma D. Role of necroptosis in the pathogenesis of solid organ injury. Cell Death Dis. 2015;6:e1975.
Ofengeim D, Yuan J. Regulation of RIP1 kinase signalling at the crossroads of inflammation and cell death. Nat Rev Mol Cell Biol. 2013;14(11):727–36.
Ito Y, Ofengeim D, Najafov A, Das S, Saberi S, Li Y, et al. RIPK1 mediates axonal degeneration by promoting inflammation and necroptosis in ALS. Science. 2016;353(6299):603.
Maruyama H, Morino H, Ito H, Izumi Y, Kato H, Watanabe Y, et al. Mutations of optineurin in amyotrophic lateral sclerosis. Nature. 2010;465(7295):223–6.
Degterev A, Hitomi J, Germscheid M, Ch’en IL, Korkina O, Teng X, et al. Identification of RIP1 kinase as a specific cellular target of necrostatins. Nat Chem Biol. 2008;4(5):313–21.
Degterev A, Huang Z, Boyce M, Li Y, Jagtap P, Mizushima N, et al. Chemical inhibitor of nonapoptotic cell death with therapeutic potential for ischemic brain injury. Nat Chem Biol. 2005;1(2):112–9.
Kalia LV, Lang AE. Parkinson’s disease. Lancet. 2015;386(9996):896–912.
Lew M. Overview of Parkinson's disease. Pharmacotherapy. 2007;27(12P2):155S–60S.
Obeso JA, Rodríguez-Oroz MC, Benitez-Temino B, Blesa FJ, Guridi J, Marin C, et al. Functional organization of the basal ganglia: therapeutic implications for Parkinson’s disease. Mov Disord. 2008;23(S3):S548–S59.
Le W, Appel SH. Mutant genes responsible for Parkinson’s disease. Curr Opin Pharmacol. 2004;4(1):79–84.
Bonifati V, Rizzu P, van Baren MJ, Schaap O, Breedveld GJ, Krieger E, et al. Mutations in the DJ-1 gene associated with autosomal recessive early-onset parkinsonism. Science. 2003;299(5604):256–9.
Richarme G, Mihoub M, Dairou J, Bui LC, Leger T, Lamouri A. Parkinsonism-associated protein DJ-1/Park7 is a major protein deglycase that repairs methylglyoxal-and glyoxal-glycated cysteine, arginine, and lysine residues. J Biol Chem. 2015;290(3):1885–97.
J-y L, Song J, Kwon K, Jang S, Kim C, Baek K, et al. Human DJ-1 and its homologs are novel glyoxalases. Hum Mol Genet. 2012;21(14):3215–25.
Vistoli G, De Maddis D, Cipak A, Zarkovic N, Carini M, Aldini G. Advanced glycoxidation and lipoxidation end products (AGEs and ALEs): an overview of their mechanisms of formation. Free Radic Res. 2013;47(Suppl 1):3–27.
Brownlee M. The pathobiology of diabetic complications a unifying mechanism. Diabetes. 2005;54(6):1615–25.
Simm A, Wagner J, Gursinsky T, Nass N, Friedrich I, Schinzel R, et al. Advanced glycation endproducts: a biomarker for age as an outcome predictor after cardiac surgery? Exp Gerontol. 2007;42(7):668–75.
Münch G, Lüth H, Wong A, Arendt T, Hirsch E, Ravid R, et al. Crosslinking of α-synuclein by advanced glycation endproducts—an early pathophysiological step in Lewy body formation? J Chem Neuroanat. 2000;20(3):253–7.
Spillantini MG, Schmidt ML, Lee VM-Y, Trojanowski JQ, Jakes R, Goedert M. α-Synuclein in Lewy bodies. Nature. 1997;388(6645):839–40.
Clayton DF, George JM. Synucleins in synaptic plasticity and neurodegenerative disorders. J Neurosci Res. 1999;58(1):120–9.
Vargas KJ, Makani S, Davis T, Westphal CH, Castillo PE, Chandra SS. Synucleins regulate the kinetics of synaptic vesicle endocytosis. J Neurosci. 2014;34(28):9364–76.
Luk B, Mohammed M, Liu F, Lee FJS. A physical interaction between the dopamine transporter and DJ-1 facilitates increased dopamine reuptake. PLoS One. 2015;10(8):e0136641.
Chandra S, Fornai F, Kwon H-B, Yazdani U, Atasoy D, Liu X, et al. Double-knockout mice for α-and β-synucleins: effect on synaptic functions. Proc Natl Acad Sci U S A. 2004;101(41):14966–71.
Conway KA, Harper JD, Lansbury PT. Accelerated in vitro fibril formation by a mutant α-synuclein linked to early-onset Parkinson disease. Nat Med. 1998;4(11):1318–20.
Conway KA, Lee S-J, Rochet J-C, Ding TT, Williamson RE, Lansbury PT. Acceleration of oligomerization, not fibrillization, is a shared property of both α-synuclein mutations linked to early-onset Parkinson’s disease: implications for pathogenesis and therapy. Proc Natl Acad Sci. 2000;97(2):571–6.
Cremades N, Cohen SI, Deas E, Abramov AY, Chen AY, Orte A, et al. Direct observation of the interconversion of normal and toxic forms of α-synuclein. Cell. 2012;149(5):1048–59.
Karpinar DP, Balija MBG, Kügler S, Opazo F, Rezaei-Ghaleh N, Wender N, et al. Pre-fibrillar α-synuclein variants with impaired β-structure increase neurotoxicity in Parkinson’s disease models. EMBO J. 2009;28(20):3256–68.
Kalia LV, Kalia SK, McLean PJ, Lozano AM, Lang AE. α-Synuclein oligomers and clinical implications for Parkinson disease. Ann Neurol. 2013;73(2):155–69.
Chen L, Wei Y, Wang X, He R. Ribosylation rapidly induces α-Synuclein to form highly cytotoxic molten globules of advanced glycation end products. PLoS One. 2010;5(2):e9052.
Iannuzzi C, Irace G, Sirangelo I. Differential effects of glycation on protein aggregation and amyloid formation. Front Mol Biosci. 2014;1:9.
Richard J. Mechanism for the formation of methylglyoxal from triosephosphates. Biochem Soc Trans. 1993;21(2):549–53.
Gautier V, Le H-T, Malki A, Messaoudi N, Caldas T, Kthiri F, et al. YajL, the prokaryotic homolog of the parkinsonism-associated protein DJ-1, protects cells against protein sulfenylation. J Mol Biol. 2012;421(4):662–70.
Le H-T, Gautier V, Kthiri F, Malki A, Messaoudi N, Mihoub M, et al. YajL, prokaryotic homolog of parkinsonism-associated protein DJ-1, functions as a covalent chaperone for thiol proteome. J Biol Chem. 2012;287(8):5861–70.
Clements CM, McNally RS, Conti BJ, Mak TW, Ting JP-Y. DJ-1, a cancer-and Parkinson's disease-associated protein, stabilizes the antioxidant transcriptional master regulator Nrf2. Proc Natl Acad Sci. 2006;103(41):15091–6.
Ariga H, Takahashi-Niki K, Kato I, Maita H, Niki T, Iguchi-Ariga SM. Neuroprotective function of DJ-1 in Parkinson’s disease. Oxidative Med Cell Longev. 2013;2013:1.
Kim J-M, Cha S-H, Choi YR, Jou I, Joe E-H, Park SM. DJ-1 deficiency impairs glutamate uptake into astrocytes via the regulation of flotillin-1 and caveolin-1 expression. Sci Rep. 2016;6:28823.
Meiser J, Delcambre S, Wegner A, Jäger C, Ghelfi J, d'Herouel AF, et al. Loss of DJ-1 impairs antioxidant response by altered glutamine and serine metabolism. Neurobiol Dis. 2016;89:112–25.
Richman P, Meister A. Regulation of gamma-glutamyl-cysteine synthetase by nonallosteric feedback inhibition by glutathione. J Biol Chem. 1975;250(4):1422–6.
Zhou W, Freed CR. DJ-1 up-regulates glutathione synthesis during oxidative stress and inhibits A53T α-synuclein toxicity. J Biol Chem. 2005;280(52):43150–8.
Fan J, Ye J, Kamphorst JJ, Shlomi T, Thompson CB, Rabinowitz JD. Quantitative flux analysis reveals folate-dependent NADPH production. Nature. 2014;510(7504):298.
Ishikawa S, Taira T, Takahashi-Niki K, Niki T, Ariga H, Iguchi-Ariga SM. Human DJ-1-specific transcriptional activation of tyrosine hydroxylase gene. J Biol Chem. 2010;285(51):39718–31.
Takahashi-Niki K, Niki T, Iguchi-Ariga S, Ariga H. [Function of DJ-1 in mitochondria]. Yakugaku Zasshi. 2011;132(10):1105–10.
González MI, Krizman-Genda E, Robinson MB. Caveolin-1 regulates the delivery and endocytosis of the glutamate transporter, excitatory amino acid carrier 1. J Biol Chem. 2007;282(41):29855–65.
Abousaab A, Warsi J, Elvira B, Lang F. Caveolin-1 sensitivity of excitatory amino acid transporters EAAT1, EAAT2, EAAT3, and EAAT4. J Membr Biol. 2016;249(3):239–49.
Cremona ML, Matthies HJ, Pau K, Bowton E, Speed N, Lute BJ, et al. Flotillin-1 is essential for PKC-triggered endocytosis and membrane microdomain localization of DAT. Nat Neurosci. 2011;14(4):469–77.
Callaghan RC, Cunningham JK, Sykes J, Kish SJ. Increased risk of Parkinson's disease in individuals hospitalized with conditions related to the use of methamphetamine or other amphetamine-type drugs. Drug Alcohol Depend. 2012;120(1):35–40.
Curtin K, Fleckenstein AE, Robison RJ, Crookston MJ, Smith KR, Hanson GR. Methamphetamine/amphetamine abuse and risk of Parkinson’s disease in Utah: a population-based assessment. Drug Alcohol Depend. 2015;146:30–8.
Underhill SM, Wheeler DS, Li M, Watts SD, Ingram SL, Amara SG. Amphetamine modulates excitatory neurotransmission through endocytosis of the glutamate transporter EAAT3 in dopamine neurons. Neuron. 2014;83(2):404–16.
Hong WC, Amara SG. Differential targeting of the dopamine transporter to recycling or degradative pathways during amphetamine-or PKC-regulated endocytosis in dopamine neurons. FASEB J. 2013;27(8):2995–3007.
Hayashi T, Ishimori C, Takahashi-Niki K, Taira T, Y-c K, Maita H, et al. DJ-1 binds to mitochondrial complex I and maintains its activity. Biochem Biophys Res Commun. 2009;390(3):667–72.
Shendelman S, Jonason A, Martinat C, Leete T, Abeliovich A. DJ-1 is a redox-dependent molecular chaperone that inhibits α-synuclein aggregate formation. PLoS Biol. 2004;2(11):e362.
Zhou W, Zhu M, Wilson MA, Petsko GA, Fink AL. The oxidation state of DJ-1 regulates its chaperone activity toward α-synuclein. J Mol Biol. 2006;356(4):1036–48.
Andres-Mateos E, Perier C, Zhang L, Blanchard-Fillion B, Greco TM, Thomas B, et al. DJ-1 gene deletion reveals that DJ-1 is an atypical peroxiredoxin-like peroxidase. Proc Natl Acad Sci. 2007;104(37):14807–12.
Girotto S, Cendron L, Bisaglia M, Tessari I, Mammi S, Zanotti G, et al. DJ-1 is a copper chaperone acting on SOD1 activation. J Biol Chem. 2014;289(15):10887–99.
Yamashita S, Mori A, Kimura E, Mita S, Maeda Y, Hirano T, et al. DJ-1 forms complexes with mutant SOD1 and ameliorates its toxicity. J Neurochem. 2010;113(4):860–70.
Vezina C, Kudelski A, Sehgal S. Rapamycin (AY-22,989), a new antifungal antibiotic. I. Taxonomy of the producing streptomycete and isolation of the active principle. J Antibiot. 1975;28(10):721–6.
Yanos ME, Bennett CF, Kaeberlein M. Genome-wide RNAi longevity screens in Caenorhabditis elegans. Curr Genomics. 2012;13(7):508–18.
Johnson TE. 25years after age-1: genes, interventions and the revolution in aging research. Exp Gerontol. 2013;48(7):640–3.
Bartke A. Single-gene mutations and healthy ageing in mammals. Philos Trans Roy Soc Lond B Biol Sci. 2011;366(1561):28–34.
Partridge L. Some highlights of research on aging with invertebrates, 2010. Aging cell. 2011;10(1):5–9.
Apelo SIA, Lamming DW. Rapamycin: an InhibiTOR of aging emerges from the soil of Easter Island. J Gerontol Ser A Biol Med Sci. 2016;71(7):841–9. https://doi.org/10.1093/gerona/glw090.
Colman RJ, Beasley TM, Kemnitz JW, Johnson SC, Weindruch R, Anderson RM. Caloric restriction reduces age-related and all-cause mortality in rhesus monkeys. Nat Commun. 2014;5:3557.
Colman RJ, Anderson RM, Johnson SC, Kastman EK, Kosmatka KJ, Beasley TM, et al. Caloric restriction delays disease onset and mortality in rhesus monkeys. Science. 2009;325(5937):201–4.
Borra MT, Smith BC, Denu JM. Mechanism of human SIRT1 activation by resveratrol. J Biol Chem. 2005;280(17):17187–95.
Sin TK, Yung BY, Siu PM. Modulation of SIRT1-Foxo1 signaling axis by resveratrol: implications in skeletal muscle aging and insulin resistance. Cell Physiol Biochem. 2015;35(2):541–52.
Latruffe N, Rifler J-P. Bioactive polyphenols from grapes and wine emphasized with resveratrol. Curr Pharm Des. 2013;19(34):6053–63.
Moridi H, Karimi J, Sheikh N, Goodarzi MT, Saidijam M, Yadegarazari R, et al. Resveratrol-dependent down-regulation of receptor for advanced glycation end-products and oxidative stress in kidney of rats with diabetes. Int J Endocrinol Metab. 2015;13(2):e23542.
Park D, Jeong H, Lee MN, Koh A, Kwon O, Yang YR, et al. Resveratrol induces autophagy by directly inhibiting mTOR through ATP competition. Sci Rep. 2016;6:21772.
Chung JH, Manganiello V, Dyck JR. Resveratrol as a calorie restriction mimetic: therapeutic implications. Trends Cell Biol. 2012;22(10):546–54.
Turner RS, Thomas RG, Craft S, van Dyck CH, Mintzer J, Reynolds BA, et al. A randomized, double-blind, placebo-controlled trial of resveratrol for Alzheimer disease. Neurology. 2015;85(16):1383–91.
Ito S, Kimura K, Haneda M, Ishida Y, Sawada M, Isobe K-i. Induction of matrix metalloproteinases (MMP3, MMP12 and MMP13) expression in the microglia by amyloid-β stimulation via the PI3K/Akt pathway. Exp Gerontol. 2007;42(6):532–7.
Ito S, Sawada M, Haneda M, Ishida Y, Isobe K-i. Amyloid-β peptides induce several chemokine mRNA expressions in the primary microglia and Ra2 cell line via the PI3K/Akt and/or ERK pathway. Neurosci Res. 2006;56(3):294–9.
Caccamo A, Maldonado MA, Majumder S, Medina DX, Holbein W, Magrí A, et al. Naturally secreted amyloid-β increases mammalian target of rapamycin (mTOR) activity via a PRAS40-mediated mechanism. J Biol Chem. 2011;286(11):8924–32.
Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell. 2012;149(2):274–93.
Hands S, Proud C, Wyttenbach A. mTOR’s role in ageing: protein synthesis or autophagy? Aging (Albany, NY). 2009;1(7):586–97.
Beau I, Mehrpour M, Codogno P. Autophagosomes and human diseases. Int J Biochem Cell Biol. 2011;43(4):460–4.
Rao VK, Carlson EA, Yan SS. Mitochondrial permeability transition pore is a potential drug target for neurodegeneration. Biochim Biophys Acta. 2014;1842(8):1267–72.
Bernardi P, Di Lisa F. The mitochondrial permeability transition pore: molecular nature and role as a target in cardioprotection. J Mol Cell Cardiol. 2015;78:100–6.
Oster AM, Thomas B, Terman D, Fall CP. The low conductance mitochondrial permeability transition pore confers excitability and CICR wave propagation in a computational model. J Theor Biol. 2011;273(1):216–31.
Wacquier B, Combettes L, Van Nhieu GT, Dupont G. Interplay between intracellular Ca2+ oscillations and Ca2+−stimulated mitochondrial metabolism. Sci Rep 2016;6.
Wang K. Autophagy and apoptosis in liver injury. Cell Cycle. 2015;14(11):1631–42.
Narendra DP, Youle RJ. Targeting mitochondrial dysfunction: role for PINK1 and Parkin in mitochondrial quality control. Antioxid Redox Signal. 2011;14(10):1929–38.
Manfredi G, Xu Z. Mitochondrial dysfunction and its role in motor neuron degeneration in ALS. Mitochondrion. 2005;5(2):77–87.
Song W, Chen J, Petrilli A, Liot G, Klinglmayr E, Zhou Y, et al. Mutant huntingtin binds the mitochondrial fission GTPase dynamin-related protein-1 and increases its enzymatic activity. Nat Med. 2011;17(3):377–82.
Yao J, Irwin RW, Zhao L, Nilsen J, Hamilton RT, Brinton RD. Mitochondrial bioenergetic deficit precedes Alzheimer’s pathology in female mouse model of Alzheimer’s disease. Proc Natl Acad Sci. 2009;106(34):14670–5.
Murphy MP, Smith RA. Drug delivery to mitochondria: the key to mitochondrial medicine. Adv Drug Deliv Rev. 2000;41(2):235–50.
Jauslin ML, Meier T, Smith RA, Murphy MP. Mitochondria-targeted antioxidants protect Friedreich Ataxia fibroblasts from endogenous oxidative stress more effectively than untargeted antioxidants. FASEB J. 2003;17(13):1972–4.
Zanardi E, Verzoni E, Grassi P, Necchi A, Giannatempo P, Raggi D, et al. Clinical experience with temsirolimus in the treatment of advanced renal cell carcinoma. Ther Adv Urol. 2015;7(3):152–61.
Graham CD, Kaza N, Klocke BJ, Gillespie GY, Shevde LA, Carroll SL, et al. Tamoxifen induces cytotoxic autophagy in glioblastoma. J Neuropathol Exp Neurol. 2016;75(10):946–54.
Wu S-T, Sun G-H, Cha T-L, Kao C-C, Chang S-Y, Kuo S-C, et al. CSC-3436 switched tamoxifen-induced autophagy to apoptosis through the inhibition of AMPK/mTOR pathway. J Biomed Sci. 2016;23(1):60.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Cumbay, M., LaFontaine, M., Arbor, S. (2019). Mechanistic Insights into Neurodegenerative Diseases: The Potential for the Development of Novel Therapeutics. In: Singh, S., Joshi, N. (eds) Pathology, Prevention and Therapeutics of Neurodegenerative Disease. Springer, Singapore. https://doi.org/10.1007/978-981-13-0944-1_20
Download citation
DOI: https://doi.org/10.1007/978-981-13-0944-1_20
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-0943-4
Online ISBN: 978-981-13-0944-1
eBook Packages: MedicineMedicine (R0)