Abstract
Fulminant type 1 diabetes is temporarily categorized as idiopathic type 1 diabetes mellitus (type 1B). It is characterized by an abrupt onset of the disease mostly with ketosis and ketoacidosis, accompanied by severe metabolic disorder, remarkably elevated blood glucose concentration, and almost complete, irreversible loss of islet function. In severe cases, the disease causes serious complications such as rhabdomyolysis, acute renal failure, and cerebral edema. Fulminant type 1 diabetes most commonly occurs in Asian countries. Timely diagnosis and treatment are the keys to improve the prognosis of patients. As a novel glucose monitoring technology, continuous glucose monitoring (CGM) is helpful to optimize the treatment regimen. This chapter will first briefly introduce fulminant type 1 diabetes with regard to the basic concept, diagnostic criteria, epidemiology, pathogenesis, clinical features, treatment, and prognosis. Also, we will continue to explain how CGM can be used to analyze the characteristics of blood glucose variability in fulminant type 1 diabetes and to guide the adjustment of individualized treatment through the presentation and analysis of typical cases.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Fulminant type 1 diabetes was first reported by Imagawa et al. [1] in 2000 and is characterized by a sudden onset of severe metabolic disorders, markedly elevated blood glucose with normal or slightly elevated glycated hemoglobin A1c (HbA1c), and almost complete, irreversible loss of islet function. Fulminant type 1 diabetes can be classified as one subtype of idiopathic type 1 diabetes (type 1B), with an acute onset of ketosis or ketoacidosis. The associated serious complications such as rhabdomyolysis, acute renal failure, and cerebral edema have been reported [2,3,4], and the outcomes could be fatal if without timely diagnose and treatment. Therefore, fulminant type 1 diabetes, as an acute and critical disease of the endocrine and metabolic system, requires special attention by all clinicians. In addition, due to almost complete, irreversible damage of islet function, patients exhibit large blood glucose variability and significantly increased risk of hypoglycemia and continue to need long-term therapy of insulin replacement. Therefore, it is necessary to comprehensively understand the characteristics of blood glucose variability through various monitoring techniques including self-monitoring of blood glucose (SMBG) and continuous glucose monitoring (CGM) technology in particular, in order to optimize the hypoglycemic regimen.
15.1 Overview of Fulminant Type 1 Diabetes Mellitus
15.1.1 The Concept of Fulminant Type 1 Diabetes
The 1997 American Diabetes Association (ADA) and the 1999 World Health Organization (WHO) have proposed the classification of diabetes mellitus [5,6,7], which divides diabetes into four types, namely, type 1 diabetes, type 2 diabetes, special types of diabetes, and gestational diabetes. Among them, type 1 diabetes is divided into two subtypes, namely, autoimmune-mediated diabetes (type 1A) and type 1B. Furthermore, three distinct stages of type 1 diabetes can be identified according to the latest ADA diabetes criteria (2017; Table 15.1) [8].
In 2000, Imagawa et al. [1] found a group of 11 patients with newly diagnosed type 1 diabetes that was characterized by a remarkably abrupt onset, the absence of insulitis and diabetes-related antibodies, and the high level of serum pancreatic enzyme concentrations. This was referred to a special type of type 1 diabetes and named “fulminant type 1 diabetes”.
15.1.2 Diagnostic Criteria for Fulminant Type 1 Diabetes
There is no uniform diagnosis criterion of fulminant type 1 diabetes. The 2012 Japan Diabetes Society (JDS) criteria (Table 15.2) are commonly used for the diagnosis of fulminant type 1 diabetes, which include the screening criteria and diagnostic criteria [9].
For the diagnosis of fulminant type 1 diabetes, the following aspects need to be supplemented:
-
1.
For patients with impaired glucose regulation, their HbA1c level is relatively high. Thus, the cutoff point [HbA1c < 8.7% (72 mmol/mol) (NGSP)] is not applicable to such patients.
-
2.
For patients with the manifestations of diabetic ketosis or ketoacidosis, fulminant type 1 diabetes should be routinely screened. Further tests for islet autoantibody, HbA1c, islet function, and liver function are required in patients with suspected fulminant type 1 diabetes.
-
3.
Fulminant type 1 diabetes can be diagnosed if three of the JDS diagnostic criteria are met; the diagnosis is highly suspected if two of the diagnostic criteria are met with a disease course exceeding 1 week.
-
4.
The onset of fulminant type 1 diabetes is often preceded by influenza-like symptoms or gastrointestinal symptoms and, thus, is often misdiagnosed as acute respiratory infection or acute gastroenteritis. Therefore, improvements are needed in the early detection, early diagnosis, and early treatment of fulminant type 1 diabetes.
15.1.3 Epidemiology of Fulminant Type 1 Diabetes
According to the previous case reports, fulminant type 1 diabetes most commonly occurs in Asian countries, with the highest incidence in Japan, followed by China and South Korea. It is rarely reported in Europe and the USA. Preliminary epidemiological studies show that the ketosis-onset fulminant type 1 diabetes accounted for 19.4% (43/222) [10] and 7.1% (7/99) [11] of cases of type 1 diabetes in Japan and South Korea. The prevalence rate in China was 9.1% among type 1 diabetes patients, accounting for 14.0% of type 1 diabetes with ketosis or ketoacidosis-onset over 18 years of age.
The existing evidence shows that fulminant type 1 diabetes has the following epidemiological characteristics:
-
1.
Sporadic distribution.
-
2.
Racial and ethnic variations in incidence rates. The incidence is higher in Asians than in Caucasians, with no reports so far in African American.
-
3.
Average age at onset of 39.1 years (most cases over 20 years old). Women showed a younger age at onset than men.
-
4.
No significant difference in the morbidity between men and women, although morbidity increases with age in males.
-
5.
Greater morbidity associated with pregnancy.
15.1.4 Etiology of Fulminant Type 1 Diabetes
The etiology and pathogenesis of fulminant type 1 diabetes are not yet clear and are currently thought to be associated with genetic, environmental (viral infection), and autoimmune factors (Fig. 15.1).
The etiology and pathogenesis of fulminant type 1 diabetes. HLA human leukocyte antigen, Foxp3 forkhead box protein 3, IRF7 interferon regulatory factor 7, CTLA-4 cytotoxic T-lymphocyte antigen 4, Th1 helper T cell 1, Th2 helper T cell 2, Th17 helper T cell 17, M∅ macrophage, IL-1β interleukin-1β, IL-4 interleukin-4, IL-10 interleukin-10, IL-17 interleukin-17, TNFα tumor necrosis factor α, TGFβ transforming growth factor β, iNOS inducible nitric oxide synthase, CpG DNA non-methylated DNA, TLR9 Toll-like receptor 9, Te effector T cell, GLP-1R glucagon like peptide-1 receptor, Tregs regulatory T cell, a-Tregs activated regulatory T cell, r-Tregs rest regulatory T cell
15.1.4.1 Genetic Susceptibility
The results of previous studies have shown that a genetic polymorphism of human leukocyte antigen II (HLA-II) is associated with the occurrence of fulminant type 1 diabetes (Table 15.3). The results indicate that HLA DR4-DQ4 is associated with the onset of Japanese fulminant type 1 diabetes mellitus, especially the DRB1*0405-DQB1*0401, DQA1*0303-DQB1*0401 and DQA1*0302-DQB1*0303 haplotypes. Tsutsumi et al. [12] found that 32.6% of fulminant type 1 diabetes patients carried the DRB1*0405-DQB1*0401 genotype, which was significantly higher than 14.2% of individuals in the normal control group. Therefore, the 2012 JDS diagnostic criteria for diagnosis of fulminant type 1 diabetes mellitus include the characteristic of “association with HLA DRB1*0405-DQB1*0401” [9]. Moreover, studies have shown that HLA DRB1*0405-DQB1*0401 is a susceptibility gene in Japanese patients with negative GAD-Ab, whereas the HLA DRB1*0901-DQB1*0303 genotype is more common in GAD-Ab positive and fulminant type 1 diabetes associated with pregnancy [12, 13]. The results of a study in South Korea also showed the involvement of HLA DRB1*0405-DQB1*0401 in fulminant type 1 diabetes [14]. HLA DQA1*0102-DQB1*0601 may be a susceptibility gene for the Chinese population [15].
In addition, there is evidence for genetic heterogeneity in fulminant type 1 diabetes. A pair of twins in South Korea had the same HLA DR-DQ haplotype but different phenotypes, namely, fulminant type 1 diabetes and autoimmune-mediated diabetes, type 1A [16].
15.1.4.2 Viral Infection
Most fulminant type 1 diabetes patients have a history of infection 2 weeks before onset, suggestive of an association between viral infection and the onset of fulminant type 1 diabetes. A Japanese national survey showed that 71.7% of fulminant type 1 diabetes patients had influenza-like symptoms before the onset and 72.5% had abdominal symptoms [17]. Also, some patients had significantly high titers of IgA antibodies to enterovirus [18]. The common viruses identified are herpes simplex virus (HSV), human herpesvirus 6 (HHV6), cytomegalovirus (CMV), coxsackie virus, etc. (Table 15.4).
Imagawa et al. [19] found elevations in a variety of antibodies after viral infection, suggesting that the virus-induced immune response, rather than viruses themselves, triggered the fulminant type 1 diabetes. Tanaka et al. [20] found the presence of enterovirus in islet cells and exocrine tissues, and immune response to enterovirus infection might be involved in the onset of fulminant type 1 diabetes.
15.1.4.3 Autoimmunity
At the initial discovery of fulminant type 1 diabetes, Imagawa et al. [1] found that islet autoantibody was negative in 11 fulminant type 1 diabetes patients and, thus, eliminated an association of fulminant type 1 diabetes with autoimmune disease, which distinguished it from type 1A diabetes. However, the follow-up study found some fulminant type 1 diabetes patients were positive for GAD-Ab or also had Graves’ disease or Hashimoto’s thyroiditis. A small number of patients presented with lymphocyte infiltration in pancreatic tissues [10, 21]. These data suggest that immune factors are involved in the occurrence of this disease.
A subsequent study has confirmed cellular or humoral immune abnormalities in a portion of fulminant type 1 diabetes patients. Aida et al. [22] found T cell and macrophage infiltration in and around the islets in three cases of fulminant type 1 diabetes, suggesting that both innate and acquired immunity are involved in the occurrence of this disease. It has also been reported that macrophage-mediated insulitis may be a more important cause of β-cell damage than T cells (CD8+ T cells were originally thought to cause fulminant type 1 diabetes) [23, 24].
Moreover, the recent study showed that the Toll-like receptor-9/interferon regulatory factor-7 (TLR9/IRF7) pathway is involved in the occurrence of fulminant type 1 diabetes, mainly through cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and transcription factor forkhead box P3 (Foxp3). Zhou et al. [25] found that Foxp3 promoter hypermethylation in human peripheral blood mononuclear cells prevented IRF-7 binding to the Foxp3 promoter, downregulated the expression of TLR9 and Foxp3, and thus impaired the function of regulatory T cells (Treg) and decreased CTLA-4. Treg immunodeficiency in peripheral blood and islets resulted in failure of the body to produce effective immune tolerance, which triggered a sustained autoimmune destruction of β-cells and finally led to fulminant type 1 diabetes.
15.1.4.4 Pregnancy
The fulminant type 1 diabetes can be divided into pregnancy-related fulminant type 1 diabetes and nonpregnancy-related fulminant type 1 diabetes according to its relationship with pregnancy. The study performed by Imagawa et al. [1] showed that almost all cases of abrupt onset of type 1 diabetes during pregnancy are fulminant type 1 diabetes, mostly occurring during late pregnancy or 2 weeks after delivery. Shimizu et al. [13] compared the clinical characteristics of the two types of the disease and found that fulminant type 1 diabetes associated with pregnancy might be related to the hormone levels and metabolic disorders of pregnant women: sex hormones during pregnancy can promote the Th2-type immune response and antagonize the Th1-type immune reaction. In addition, there is a case report of fulminant type 1 diabetes occurring 10 days after artificial abortion, revealing that abortion may also increase the risk of fulminant type 1 diabetes.
15.1.4.5 Others
Some medications (carbamazepine, mexiletine, ibuprofen, tegafur-uracil, pembrolizumab, etc.) may be involved in the occurrence of this disease by drug-induced hypersensitivity syndrome [26,27,28]. Onuma et al. [29] reported that compared with general population, patients with drug-induced hypersensitivity syndrome had a higher probability of developing fulminant type 1 diabetes, with a susceptibility gene HLA-B62, suggesting that in addition to genetic susceptibility, the use of specific drugs is associated with the occurrence of this disease.
15.1.5 Clinical Characteristics of Fulminant Type 1 Diabetes
Most fulminant type 1 diabetes patients are adults with no difference in the incidence between men and women. Pregnant women are at higher risk of this disease. Compared with type 1A diabetes, fulminant type 1 diabetes has the following clinical characteristics:
-
1.
Prodromal symptoms. Patients often develop prodromal symptoms 2 weeks before the onset of fulminant type 1 diabetes, for instance, influenza-like symptoms (fever, upper respiratory tract infection, etc.) or gastrointestinal symptoms (diarrhea, nausea, vomiting, etc.), with fever (60%) being most common.
-
2.
Hyperglycemia and ketoacidosis. The onset is very sudden, with typically <1 week from the presentation of typical hyperglycemic symptoms (polyuria, polyphagia, polydipsia, and weight loss) to the occurrence of ketosis or ketoacidosis. Sekine et al. [30] reported a case of a patient who had blood glucose within normal range 1 day before the onset, followed by a sudden increase in blood glucose and a sudden drop in C-peptide level the next day. Some researchers have even observed hypoglycemic events before the onset, probably due to a rapid release of synthesized insulin into the blood resulting from the rapid destruction of islets. As the course of the disease is very short, the HbA1c at onset is close to normal or only mildly increased.
-
3.
Severe metabolic disorders. Approximately 90% of fulminant type 1 diabetes begins with ketosis or ketoacidosis and half with disturbance of consciousness. At the onset, hyperglycemia, ketoacidosis, and electrolyte imbalance are more serious than type 1A diabetes.
-
4.
Almost complete, irreversible loss of islet function. The existing evidence shows permanent destruction of islet α- and β-cells in patients with fulminant type 1 diabetes.
-
5.
Serious complications such as rhabdomyolysis, liver dysfunction, and kidney dysfunction. Some patients exhibit multiple organ dysfunction such as loss of liver, kidney, heart, and striated muscle function, as manifested by an elevation in hepatic enzymes, pancreatic enzymes (amylase, lipase, elastase, etc.), and myokinases, or severe conditions like rhabdomyolysis, acute renal failure, cerebral edema, and even cardiac arrest [2,3,4] (Table 15.5).
-
6.
Others. Most cases of pregnancy-related type 1 diabetes are fulminant type 1 diabetes and mostly occur during the late pregnancy or 2 weeks after delivery [1, 17]. The clinical symptoms of fulminant type 1 diabetes associated with pregnancy appear to be much more serious, with lower HbA1c and arterial pH value. Fulminant type 1 diabetes associated with pregnancy can result in severe maternal and fetal complications, for instance, an extremely high incidence of abortion and stillbirth.
15.2 Treatment and Prognosis of Fulminant Type 1 Diabetes Mellitus
15.2.1 Treatment of Fulminant Type 1 Diabetes
At present, the evidence on the treatment of fulminant type 1 diabetes is mainly derived from case reports. According to its characteristics, the treatment is divided into acute-phase treatment and long-term insulin therapy.
15.2.1.1 Acute-Phase Treatment
Fulminant type 1 diabetes is characterized by an abrupt onset of the disease mostly with ketosis and ketoacidosis, accompanied by severe metabolic disorders and remarkably elevated blood glucose concentration. Once fulminant type 1 diabetes is suspected, the patient should be treated immediately for diabetic ketoacidosis including rehydration; small doses of intravenous insulin infusion; correction of electrolyte and acid-base imbalance, along with symptomatic and supportive treatment; and prevention and management of complications.
In addition, the following points need to be noted:
-
1.
Given the acute onset with severe metabolic disorders, fulminant type 1 diabetes should be diagnosed and treated in a timely manner with (1) rapid establishment of two intravenous accesses, one for continuous intravenous insulin infusion and the other for rehydration and anti-infection treatment, and (2) due to severe dehydration and poor subcutaneous absorption of insulin, it is recommended to use intravenous insulin infusion rather than insulin pump therapy.
-
2.
In serious cases, rhabdomyolysis and resultant acute renal failure may occur. (1) Pay attention to the presence or absence of muscle weakness, swelling, pain, and brown urine; (2) the serum creatine kinase level is the most specific indicator of rhabdomyolysis, which should be routinely tested and used for constant monitoring of dynamic changes during the early diagnosis and treatment of fulminant type 1 diabetes.
-
3.
Fulminant type 1 diabetes associated with pregnancy can result in severe maternal complications and stillbirth. Key measures to save the fetus include shortening of hyperglycemia-lasting duration, timely correction of ketoacidosis, and performing a cesarean section in a timely manner.
15.2.1.2 Long-Term Insulin Therapy
As there is almost complete, irreversible destruction of islet α- and β-cells in fulminant type 1 diabetes, the patient usually has extremely poor islet function, large blood glucose variability, and increased incidence of hypoglycemia. Therefore, patients usually require four times of intensive treatment with subcutaneous rapid-acting or short-acting insulin combined with intermediate-acting or long-acting insulin. In addition, an insulin pump, which simulates the physiological insulin secretion, can be used to improve blood glucose control in patients [3]. It improves inter- and intraday glucose variability [3, 31]. The use of an insulin pump as long-term insulin replacement therapy is suggested, with a significantly higher insulin dosage than that used for type 1A diabetes [32].
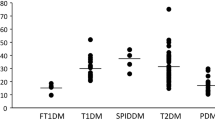
15.2.2 Prognosis of Fulminant Type 1 Diabetes
Due to the sudden onset and severe metabolic disorders of fulminant type 1 diabetes, the mortality rate is high in the absence of early diagnosis and timely treatment. After correction of ketosis or ketoacidosis, abnormal hepatic enzyme, pancreatic enzyme, and myokinase levels will return to normal within 2–3 weeks; however, fulminant type 1 diabetes causes permanent destruction of islet α- and β-cells, which requires long-term insulin replacement therapy. Compared with type 1A diabetes, fulminant type 1 diabetes results in worse islet function, more severe β-cell destruction, higher insulin requirement, and increased risk of hypoglycemia and diabetic microvascular diseases. However, Koyano et al. [33] reported the partial recovery of pancreatic α-cells after treatment from fulminant type 1 diabetes in a case of 34-year-old male, but his serum C-peptide level was still under the detection limit. Also, it was reported that early intensive treatment achieved partial recovery of β-cell function in a 44-year-old female patient who developed acute pancreatitis and concomitant fulminant type 1 diabetes [34]. Recently, a case of idiopathic type 1 diabetes with subsequent recovery of β-cell function has also been reported [35].
15.3 Use of CGM for Patients with Fulminant Type 1 Diabetes
Due to the almost complete destruction of islet β-cells, the blood glucose level is more easily influenced by exogenous insulin, and the patients exhibit large blood glucose variability and increased risks of hypoglycemia and diabetic microvascular diseases. Thus, glucose monitoring is particularly important.
At present, SMBG and CGM are commonly used glucose monitoring methods for diabetes patients. HbA1c, glycated albumin (GA), and other indicators can also reflect the recent glycemic control. SMBG represents the glucose concentration at a specific time-point, and it cannot reflect continuous, dynamic changes in blood glucose. CGM can detect occult hypoglycemia and hyperglycemia, which may be not easily detected by traditional methods. Thus, CGM is an effective supplement to traditional glucose monitoring methods. Moreover, CGM facilitates the understanding of trends in blood glucose variability and determination of the influences of meal uptake, exercise, and medication on blood glucose, so as to guide better improvements in lifestyle and adjustment of the treatment regimen. According to the Chinese clinical guideline for CGM (2012), CGM is desirable for type 1 diabetes patients [36]. Given that fulminant type 1 diabetes is a subtype of type 1 diabetes, CGM is also applicable to fulminant type 1 diabetes patients. CGM supports the management of type 1 diabetes by effectively detecting hyperglycemic and hypoglycemic events, providing data for blood glucose variability, and guiding the adjustment of treatment plan.
15.3.1 CGM Is an Effective Tool for Detecting Blood Glucose Variability
15.3.1.1 Detection of Hyperglycemic and Hypoglycemic Events
The results of the study performed by Melki et al. [37] showed that two-thirds of daily utilization of CGM was applied to monitor asymptomatic nocturnal hypoglycemia. Accumulating evidence has shown that CGM can detect asymptomatic nocturnal hypoglycemic events. Cheyne et al. [38] conducted a CGM study in ten type 1 diabetes patients with poor glycemic control and found that eight patients experienced asymptomatic hypoglycemia with blood glucose <3 mmol/L. For children with type 1 diabetes, CGM measurements suggested that about 70% of subjects had nocturnal hypoglycemia and 20% experienced nocturnal hypoglycemia for three consecutive nights [39]. CGM not only detects nocturnal hypoglycemia but also contributes to the detection of asymptomatic hypoglycemia during daytime [38, 39].
CGM also helps to detect postprandial hyperglycemia [40]. SMBG only represents the glucose concentration at a specific time-point, not the blood glucose levels throughout the day. Thus, it cannot detect all hyperglycemic events in a timely manner, especially postprandial hyperglycemia. Boland et al. [39] emphasized that CGM is an effective tool for detecting postprandial hyperglycemia in patients who only monitor fasting and bedtime blood glucose. Schaepelynck-Bélicar et al. [41] applied CGM in 12 patients with poor glycemic control and found that there were 24 postprandial hyperglycemic episodes in ten patients; five patients experienced prolonged nocturnal hyperglycemia; and four had the dawn phenomenon. Also, CGM facilitates the distinction between asymptomatic hypoglycemia and the dawn phenomenon [42].
15.3.1.2 Comprehensive Understanding of Glucose Variability
CGM not only detects hyperglycemic and hypoglycemic events but also contributes to the understanding of the characteristics of blood glucose variability [40,41,42,43]. Bhide et al. [44] believe that the biggest advantage of CGM is that it is capable of revealing the dynamic trends of blood glucose concentration so that practitioners can guide the adjustment of the treatment plan accordingly. Moreover, CGM also provides information about the causes of glycemic variability in diabetes patients.
15.3.2 Use of CGM to Guide Adjustments to Therapy
In clinical practice, CGM can be used to monitor the detailed changes in blood glucose variability throughout the day. It can improve the management of blood glucose levels and reduce hypoglycemic events by guiding the fine regulation of blood glucose. Long-term use of CGM helps improving the HbA1c [45,46,47,48,49,50,51]. However, improper use of CGM may also have a potentially negative impact: CGM provides interstitial fluid glucose readings, which lag behind capillary glucose levels. Moreover, overtreatment of hyperglycemia or hypoglycemia may increase blood glucose variability.
Fulminant type 1 diabetes developed rapidly and accompanied with more severe dysfunction of islets when compared with type 1A diabetes mellitus resulted in dramatic glycemic variability. However, HbA1c levels are more commonly normal at the early stage of the disease. Thus, the application of CGM mainly focuses on improving and maintaining the stability of blood glucose levels at the initial stage. CGM can also help improving the HbA1c when HbA1c is markedly elevated.
In our previous study, we analyzed the CGM results of three patients with fulminant type 1 diabetes who were treated in our hospital from January 2007 to March 2008, and the therapeutic regimens were adjusted accordingly (Table 15.6) [3].
Case 1 (Fig. 15.2): A patient treated with subcutaneous insulin injection four times daily with insulin dose of 0.67 U/(kg·d). The mean blood glucose (MBG) was 8.9 mmol/L, and standard deviation of blood glucose (SDBG) was 3.6 mmol/L, indicating the presence of high glycemic variability. The patient also had hypoglycemia, and the percentage of time (PT) spent with glucose ≤3.9 mmol/L was 4% with no time spent with blood glucose ≤2.8 mmol/L (Fig. 15.2a). Six months later, the glucose variation was still quite large (SDBG was 3.0 mmol/L), and MBG decreased to 6.5 mmol/L. Thus, the patient had a potentially increased risk of hypoglycemia. The PT spent with glucose ≤3.9 mmol/L and ≤2.8 mmol/L were 21% and 6%, respectively (Fig. 15.2b).
Case 2 (Fig. 15.3): A patient was treated with an insulin pump with insulin dose of 0.57 U/(kg·d). CGM revealed good glycemic control. The MBG was 6.3 mmol/L, SDBG was 2.2 mmol/L, and the PT spent with glucose ≤3.9 mmol/L was 10% with no time spent with blood glucose ≤2.8 mmol/L (Fig. 15.3a). After follow-up for 6 months, the MBG was reduced to 5.5 mmol/L, and the SDBG was unchanged (2.2 mmol/L). Thus, the PT spent with glucose ≤3.9 mmol/L and ≤2.8 mmol/L were 27% and 9%, respectively, indicating an increased duration of hypoglycemic events, which were mainly concentrated in the period after dinner and before bedtime (Fig. 15.3b). These data demonstrated that hypoglycemia was associated with MBG, and a lower blood glucose level caused an increased risk of hypoglycemia, if the blood glucose fluctuation was basically unchanged. In conclusion, the blood glucose level of the patient was kept too low. Thus, we adjusted the therapy by reducing the basal rate of the insulin pump from before dinner to bedtime, in order to increase the target glucose level.
Case 3 (Fig. 15.4): A patient was initially treated with four times daily subcutaneous insulin injections with insulin dose of 0.95 U/(kg·d), but the patient had poor control of blood glucose, with MBG of 11.5 mmol/L, SDBG of 5.0 mmol/L, and largest amplitude of glycemic excursion (LAGE) of 6.1 mmol/L (reference range < 1.4 mmol/L), and the occurrence of asymptomatic nocturnal hypoglycemia (Fig. 15.4a). After transferring to insulin pump treatment with an insulin dose of 0.9 U/(kg·d), there were significant improvements in the blood glucose levels and the degree of variability. The MBG was 8.7 mmol/L, SDBG was 2.3 mmol/L, and LAGE was decreased to 2.9 mmol/L (Fig. 15.4b). The results showed that the CGM facilitated the understanding of the patient’s blood glucose variability, and the insulin pump might help to control blood glucose variability in fulminant type 1 diabetes patients, thereby reducing the incidence of hypoglycemia and achieving satisfactory glycemic control.
Statement on Consent for Participation
All the clinical trials carried out by the authors in this book have been reported to the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital already and were in accordance with the Good Clinical Practice and Standards of China Association for Ethical Studies (approval number: 2007-45).
References
Imagawa A, Hanafusa T, Miyagawa J, Matsuzawa Y. A novel subtype of type 1 diabetes mellitus characterized by a rapid onset and an absence of diabetes-related antibodies. Osaka IDDM Study Group. N Engl J Med. 2000;342:301–7. https://doi.org/10.1056/NEJM200002033420501.
Deng D, Xia L, Chen M, Xu M, Wang Y, Wang C. A case of fulminant type 1 diabetes associated with acute renal failure. Neuro Endocrinol Lett. 2015;36:115–8.
Zhou J, Bao YQ, Li M, Liu F, Chen HB, Han JF, Lu W, Ma XJ, Hu C, Xiang KS, Jia WP. Fulminant type 1 diabetes: the clinical features and treatment strategy. Chin J Diabetes Mellitus. 2009;1:34–8. https://doi.org/10.3760/cma.j.issn.1674-5809.2009.01.011.
Dong H, Liu L, Zhou Y, Mu J, Zhang J. Sudden death of a 15-year-old girl due to fulminant type 1 diabetes mellitus-diabetic ketoacidosis induced cerebral edema? J Forensic Legal Med. 2014;26:5–9. https://doi.org/10.1016/j.jflm.2014.05.001.
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):5–20.
The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 1997;20:1183–97.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53. https://doi.org/10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S.
American Diabetes Association. Standards of Medical Care in Diabetes-2017. Diabetes Care. 2017;40(Suppl 1):1–135.
Imagawa A, Hanafusa T, Awata T, Ikegami H, Uchigata Y, Osawa H, Kawasaki E, Kawabata Y, Kobayashi T, Shimada A, Shimizu I, Takahashi K, Nagata M, Makino H, Maruyama T. Report of the Committee of the Japan Diabetes Society on the research of fulminant and acute-onset type 1 diabetes mellitus: new diagnostic criteria of fulminant type 1 diabetes mellitus (2012). J Diabetes Investig. 2012;3:536–9. https://doi.org/10.1111/jdi.12024.
Imagawa A, Hanafusa T. Series: clinical study from Japan and its reflections; a nationwide survey of fulminant type 1 diabetes. Nippon Naika Gakkai Zasshi. 2013;102:1829–35.
Cho YM, Kim JT, Ko KS, Koo BK, Yang SW, Park MH, Lee HK, Park KS. Fulminant type 1 diabetes in Korea: high prevalence among patients with adult-onset type 1 diabetes. Diabetologia. 2007;50:2276–9. https://doi.org/10.1007/s00125-007-0812-z.
Tsutsumi C, Imagawa A, Ikegami H, Makino H, Kobayashi T, Hanafusa T, Japan Diabetes Society Committee on Type 1 Diabetes Mellitus Research. Class II HLA genotype in fulminant type 1 diabetes: a nationwide survey with reference to glutamic acid decarboxylase antibodies. J Diabetes Investig. 2012;3:62–9. https://doi.org/10.1111/j.2040-1124.2011.00139.x.
Shimizu I, Makino H, Imagawa A, Iwahashi H, Uchigata Y, Kanatsuka A, Kawasaki E, Kobayashi T, Shimada A, Maruyama T, Hanafusa T. Clinical and immunogenetic characteristics of fulminant type 1 diabetes associated with pregnancy. J Clin Endocrinol Metab. 2006;91:471–6. https://doi.org/10.1210/jc.2005-1943.
Kwak SH, Kim YJ, Chae J, Lee CH, Han B, Kim JI, Jung HS, Cho YM, Park KS. Association of HLA genotype and fulminant type 1 diabetes in Koreans. Genomics Inform. 2015;13:126–31. https://doi.org/10.5808/GI.2015.13.4.126.
Zheng C, Zhou Z, Yang L, Lin J, Huang G, Li X, Zhou W, Wang X, Liu Z. Fulminant type 1 diabetes mellitus exhibits distinct clinical and autoimmunity features from classical type l diabetes mellitus in Chinese. Diabetes Metab Res Rev. 2011;27:70–8. https://doi.org/10.1002/dmrr.1148.
Jung JH, Hahm JR, Kim MA, Park MH, Kim DR, Jung TS, Chung SI. Fulminant autoantibody-negative and type 1A diabetes phenotypes in a Korean HLA identical dizygotic twin. Diabetes Care. 2005;28:2330–1.
Imagawa A, Hanafusa T, Uchigata Y, Kanatsuka A, Kawasaki E, Kobayashi T, Shimada A, Shimizu I, Toyoda T, Maruyama T, Makino H. Fulminant type 1 diabetes: a nationwide survey in Japan. Diabetes Care. 2003;26:2345–52.
Imagawa A, Hanafusa T, Makino H, Miyagawa JI, Juto P. High titres of IgA antibodies to enterovirus in fulminant type-1 diabetes. Diabetologia. 2005;48:290–3. https://doi.org/10.1007/s00125-004-1624-z.
Imagawa A, Hanafusa T. Fulminant type 1 diabetes--an important subtype in East Asia. Diabetes Metab Res Rev. 2011;27:959–64. https://doi.org/10.1002/dmrr.1236.
Tanaka S, Aida K, Nishida Y, Kobayashi T. Pathophysiological mechanisms involving aggressive islet cell destruction in fulminant type 1 diabetes. Endocr J. 2013;60:837–45.
Minegaki Y, Higashida Y, Ogawa M, Miyachi Y, Fujii H, Kabashima K. Drug-induced hypersensitivity syndrome complicated with concurrent fulminant type 1 diabetes mellitus and Hashimoto’s thyroiditis. Int J Dermatol. 2013;52:355–7. https://doi.org/10.1111/j.1365-4632.2011.05213.x.
Aida K, Nishida Y, Tanaka S, Maruyama T, Shimada A, Awata T, Suzuki M, Shimura H, Takizawa S, Ichijo M, Akiyama D, Furuya F, Kawaguchi A, Kaneshige M, Itakura J, Fujii H, Endo T, Kobayashi T. RIG-I-and MDA5-initiated innate immunity linked with adaptive immunity accelerates beta-cell death in fulminant type 1 diabetes. Diabetes. 2011;60:884–9. https://doi.org/10.2337/db10-0795.
Mizutani T, Yoshimoto T, Kaneko R, Ishii A. Diagnosis of fulminant type 1 diabetes mellitus in an autopsy case with postmortem changes. Leg Med (Tokyo). 2011;13:250–3. https://doi.org/10.1016/j.legalmed.2011.05.007.
Shibasaki S, Imagawa A, Tauriainen S, Iino M, Oikarinen M, Abiru H, Tamaki K, Seino H, Nishi K, Takase I, Okada Y, Uno S, Murase-Mishiba Y, Terasaki J, Makino H, Shimomura I, Hyöty H, Hanafusa T. Expression of toll-like receptors in the pancreas of recent-onset fulminant type 1 diabetes. Endocr J. 2010;57:211–9.
Wang Z, Zheng Y, Hou C, Yang L, Li X, Lin J, Huang G, Lu Q, Wang CY, Zhou Z. DNA methylation impairs TLR9 induced Foxp3 expression by attenuating IRF-7 binding activity in fulminant type 1 diabetes. J Autoimmun. 2013;41:50–9. https://doi.org/10.1016/j.jaut.2013.01.009.
Adachi J, Mimura M, Gotyo N, Watanabe T. The development of fulminant type 1 diabetes during chemotherapy for rectal cancer. Intern Med. 2015;54:819–22. https://doi.org/10.2169/internalmedicine.54.3413.
Gaudy C, Clévy C, Monestier S, Dubois N, Préau Y, Mallet S, Richard MA, Grob JJ, Valéro R, Béliard S. Anti-PD1 pembrolizumab can induce exceptional fulminant type 1 diabetes. Diabetes Care. 2015;38:e182–3. https://doi.org/10.2337/dc15-1331.
Hughes J, Vudattu N, Sznol M, Gettinger S, Kluger H, Lupsa B, Herold KC. Precipitation of autoimmune diabetes with anti-PD-1 immunotherapy. Diabetes Care. 2015;38:e55–7. https://doi.org/10.2337/dc14-2349.
Onuma H, Tohyama M, Imagawa A, Hanafusa T, Kobayashi T, Kano Y, Ohashi J, Hashimoto K, Osawa H, Makino H, Japan Diabetes Society Committee on Type 1 Diabetes Mellitus Research, Japanese Dermatological Association. High frequency of HLA B62 in fulminant type l diabetes with the drug-induced hypersensitivity syndrome. J Clin Endocrinol Metab. 2012;97:E2277–81. https://doi.org/10.1210/jc.2012-2054.
Sekine N, Motokura T, Oki T, Umeda Y, Sasaki N, Hayashi M, Sato H, Fujita T, Kaneko T, Asano Y, Kikuchi K. Rapid loss of insulin secretion in a patient with fulminant type 1 diabetes mellitus and carbamazepine hypersensitivity syndrome. JAMA. 2001;285:1153–4. https://doi.org/10.1001/jama.285.9.1153.
Imagawa A, Hanafusa T. Fulminant type 1 diabetes mellitus. Endocr J. 2006;53:577–84.
Murase Y, Imagawa A, Hanafusa T, Iwahashi H, Uchigata Y, Kanatsuka A, Kawasaki E, Kobayashi T, Shimada A, Shimizu I, Maruyama T, Makino H. Fulminant type 1 diabetes as a high risk group for diabetic microangiopathy--a nationwide 5-year-study in Japan. Diabetologia. 2007;50:531–7. https://doi.org/10.1007/s00125-006-0575-y.
Koyano HM, Matsumoto T. Recovery from exocrine pancreatic insufficiency in a patient with fulminant type 1 diabetes. Intern Med. 2013;52:573–5. https://doi.org/10.2169/internalmedicine.52.9019.
Yamashita K, Sato Y, Seki K, Asano J, Funase Y, Yamauchi K, Aizawa T. Fulminant type 1 diabetes with robust recovery of insulin secretion: a case report. Diabetes Res Clin Pract. 2013;100:e34–8. https://doi.org/10.1016/j.diabres.2013.01.032.
Kaneko K, Satake C, Yamamoto J, Takahashi H, Sawada S, Imai J, Yamada T, Katagiri H. A case of idiopathic type 1 diabetes with subsequent recovery of endogenous insulin secretion despite initial diagnosis of fulminant type 1 diabetes. Endocr J. 2017;64:369–74. https://doi.org/10.1507/endocrj.EJ16-0245.
Chinese Diabetes Society. Chinese clinical guideline for continuous glucose monitoring (2012). Chin Med J. 2012;125:4167–74. https://doi.org/10.3760/cma.j.issn.0366-6999.2012.23.002.
Melki V, Ayon F, Fernandez M, Hanaire-Broutin H. Value and limitations of the Continuous Glucose Monitoring System in the management of type 1 diabetes. Diabetes Metab. 2006;32:123–9.
Cheyne EH, Kerr D. Making “sense” of diabetes: using a continuous glucose sensor in clinical practice. Diabetes Metab Res Rev. 2002;18(Suppl 1):43–8. https://doi.org/10.1002/dmrr.209.
Boland E, Monsod T, Delucia M, Brandt CA, Fernando S, Tamborlane WV. Limitations of conventional methods of self-monitoring of blood glucose: lessons learned from 3 days of continuous glucose sensing in pediatric patients with type 1 diabetes. Diabetes Care. 2001;24:1858–62.
Edelman SV, Bailey TS. Continuous glucose monitoring health outcomes. Diabetes Technol Ther. 2009;11(Suppl 1):68–74. https://doi.org/10.1089/dia.2009.0012.
Schaepelynck-Bélicar P, Vague P, Simonin G, Lassmann-Vague V. Improved metabolic control in diabetic adolescents using the continuous glucose monitoring system (CGMS). Diabetes Metab. 2003;29:608–12.
Kaufman FR, Gibson LC, Halvorson M, Carpenter S, Fisher LK, Pitukcheewanont P. A pilot study of the continuous glucose monitoring system: clinical decisions and glycemic control after its use in pediatric type 1 diabetic subjects. Diabetes Care. 2001;24:2030–4.
Jensen MH, Christensen TF, Tarnow L, Seto E, Dencker Johansen M, Hejlesen OK. Real-time hypoglycemia detection from continuous glucose monitoring data of subjects with type 1 diabetes. Diabetes Technol Ther. 2013;15:538–43. https://doi.org/10.1089/dia.2013.0069.
Bhide M, Grey JM, Moser EG, Garg SK. A primary care perspective on the use of continuous glucose monitoring in clinical practice. Diabetes Technol Ther. 2013;15:533–7. https://doi.org/10.1089/dia.2013.0169.
Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Effectiveness of continuous glucose monitoring in a clinical care environment: evidence from the Juvenile Diabetes Research Foundation continuous glucose monitoring (JDRF-CGM) trial. Diabetes Care. 2010;33:17–22. https://doi.org/10.2337/dc09-1502.
Battelino T, Phillip M, Bratina N, Nimri R, Oskarsson P, Bolinder J. Effect of continuous glucose monitoring on hypoglycemia in type 1 diabetes. Diabetes Care. 2011;34:795–800. https://doi.org/10.2337/dc10-1989.
Sachedina N, Pickup JC. Performance assessment of the Medtronic-MiniMed Continuous Glucose Monitoring System and its use for measurement of glycaemic control in Type 1 diabetic subjects. Diabet Med. 2003;20:1012–5. https://doi.org/10.1046/j.1464-5491.2003.01037.x.
Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group, Tamborlane WV, Beck RW, Bode BW, Buckingham B, Chase HP, Clemons R, Fiallo-Scharer R, Fox LA, Gilliam LK, Hirsch IB, Huang ES, Kollman C, Kowalski AJ, Laffel L, Lawrence JM, Lee J, Mauras N, O'Grady M, Ruedy KJ, Tansey M, Tsalikian E, Weinzimer S, Wilson DM, Wolpert H, Wysocki T, Xing D. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med. 2008;359:1464–76. https://doi.org/10.1056/NEJMoa0805017.
Garg SK, Voelmle MK, Beatson CR, Miller HA, Crew LB, Freson BJ, Hazenfield RM. Use of continuous glucose monitoring in subjects with type 1 diabetes on multiple daily injections versus continuous subcutaneous insulin infusion therapy: a prospective 6-month study. Diabetes Care. 2011;34:574–9. https://doi.org/10.2337/dc10-1852.
Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group, Beck RW, Buckingham B, Miller K, Wolpert H, Xing D, Block JM, Chase HP, Hirsch I, Kollman C, Laffel L, Lawrence JM, Milaszewski K, Ruedy KJ, Tamborlane WV. Factors predictive of use and of benefit from continuous glucose monitoring in type 1 diabetes. Diabetes Care. 2009;32:1947–53. https://doi.org/10.2337/dc09-0889.
Bergenstal RM, Tamborlane WV, Ahmann A, Buse JB, Dailey G, Davis SN, Joyce C, Peoples T, Perkins BA, Welsh JB, Willi SM, Wood MA, STAR 3 Study Group. Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med. 2010;363:311–20. https://doi.org/10.1056/NEJMoa1002853.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd. and Shanghai Scientific and Technical Publishers
About this chapter
Cite this chapter
Zhou, J. (2018). Using Continuous Glucose Monitoring for Patients with Fulminant Type 1 Diabetes. In: Jia, W. (eds) Continuous Glucose Monitoring. Springer, Singapore. https://doi.org/10.1007/978-981-10-7074-7_15
Download citation
DOI: https://doi.org/10.1007/978-981-10-7074-7_15
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-7073-0
Online ISBN: 978-981-10-7074-7
eBook Packages: MedicineMedicine (R0)