Abstract
Candida albicans—a common opportunistic fungal pathogen of humans—causes serious, disseminated invasive infections (candidiases) executed due to the action of several groups of virulence factors. One of the most critical is a family of secreted aspartic proteases involved in the destruction of host proteins and tissues. This chapter aims to characterize biochemical and structural properties of these enzymes that determine their functions and summarize their specific roles in the development and propagation of fungal infections. Candidal aspartic proteases deregulate the host biochemical homeostasis, by impairing the major proteolytic cascades such as the blood coagulation, the kallikrein-kinin system, and the complement system, by unleashing the activity of host proteases due to the degradation of specific endogenous inhibitors and by the inactivation of antimicrobial peptides and proteins produced by host cells. The degradation of important host proteins influences the fungal adhesion to the host cell surfaces, promotes the subsequent tissue damages, and enables the further dissemination of the pathogen. Confirmed multiple roles of candidal aspartic proteases in the host-pathogen interactions during candidiasis qualify these enzymes as promising potential targets for novel antifungal therapies.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Candida albicans
- Fungal infection
- Aspartic proteases (Saps)
- Protein degradation
- Host cell interaction
- Antibacterial peptides
- Kinins
1 Introduction
The current progress in the development of advanced health technologies, rescuing critically ill patients, has inevitably led to a considerable increase in the number of immunocompromised individuals who are particularly vulnerable to infections caused by opportunistic microorganisms including pathogenic fungi [1]. The catheterization and application of parenteral nutrition, hematologic malignancy, surgical treatments, including those related to cancer therapy and organ transplantation, HIV infection, the use of immunosuppressive therapies and broad-spectrum antibiotic treatment, as well as inherited immunodeficiency, old age and prematurity, are the main risk factors contributing to the development of opportunistic fungal infections [2,3,4,5].
The Candida spp. yeasts belongs to the most commonly identified fungal opportunistic pathogens of humans, responsible for serious, disseminated invasive infections [6, 7]. These fungi are also considered to be some of the major pathogens responsible for nosocomial bloodstream infections associated with high mortality rates in the range of 40–70% of infected patients [1, 2, 8]. Candida albicans—the most prevalent species from the Candida genus—is a part of normal human microbiota as a commensal microorganism that colonizes the skin and mucous membranes of the oral cavity, gastrointestinal tract, or genitourinary system [9, 10]. The genital or oral carriage of these yeasts is reported to be present in 20–65% of healthy individuals. However, when the delicate balance between microbial colonizers and the host is disturbed, Candida yeasts can cause annoying and painful superficial infections including thrush, oral candidosis, or candidal vulvovaginitis that can affect considerably large number of individuals colonized by these fungi [11,12,13,14].
The significant changes in the global distribution of particular Candida species and diversified prevalence among different groups of patients have been noticed over the last few decades [3, 15]. Despite the fact that C. albicans is still the major infectious agent from the genus Candida responsible for approximately 50% of all candidiases worldwide, other, so-called non-albicans Candida species have been emerging as fungal pathogens of humans, attributed to an increasing share in the overall number of candidal infections [16, 17]. This group includes mainly four species—C. glabrata, C. tropicalis, C. parapsilosis and C. krusei—that greatly differ in terms of the mechanisms of their pathogenicity [18].
Candida yeasts display a broad range of virulence attributes (Fig. 1) that allow them to successfully colonize and invade the host organism. During the infection, several mechanical, physical, and chemical protective barriers and biochemical defenses have to be affected by pathogens [19].
The candidal virulence factors primarily include two large groups of proteins: (i) an abundant set of cell surface-exposed proteins (adhesins and invasins) [22,23,24] and (ii) secreted hydrolytic enzymes such as lipases, phospholipases, and aspartic proteases [25,26,27]. The presence of such molecules, in a combination with other virulence-related fungal traits like a morphological polymorphism—i.e., the ability of the fungus to grow as unicellular, ovoid yeast-like forms or as filamentous forms (true hyphae or pseudohyphae)—the contact- and quorum-sensing, the phenotypic switching (“white” → “opaque”) and the biofilm formation greatly facilitates the initiation of the first contact of fungal cells with the host, followed by further dissemination within the human body and the subsequent development of infection [28]. All of these features and abilities contributing to the fungal pathogenicity work together to successfully combat or evade the host immune system and take control of the processes involved in maintaining physiological homeostasis of the host. In particular, the role of proteolytic enzymes in this phenomenon can hardly be overestimated [21, 26].
2 The Family of C. albicans Secreted Aspartic Proteases (Saps)
The proteolytic activity of C. albicans was first described in 1965 [29] and has more recently been assigned to 10 secreted aspartic proteases (Saps). The open reading frames (ORFs) for their genes, located on five different chromosomes, vary between 1173 and 1764 bp in length [26]. The products of their expression are preproenzymes longer by about 60–200 amino acids than active proteins due to the presence of the N-terminal signal peptide and the propeptide, which are proteolytically removed by the signal peptidase and Kex2 protease, respectively, during the classical secretory pathway in order to form the final products with a molecular mass within the range of 35–50 kDa [30, 31].
Although all C. albicans aspartic proteases are directed to the secretory pathway, only Sap1–Sap8 are secreted in the form of soluble enzymes. The other two, Sap9 and Sap10, are equipped with glycosylphosphatidylinositol (GPI) anchor that attaches them to the fungal cell wall or both, the cell wall and cell membrane [25, 32]. These enzymes are structurally similar to yapsins, proteases involved in maintaining the cell wall integrity in Saccharomyces cerevisiae [32].
Within the C. albicans Sap family, three separate groups can be distinguished according to the degree of amino acid sequence similarity [25]. Among them, Sap4–Sap6 and Sap1–Sap3 represent the highest similarity degree (Fig. 2). The expression of these proteases seems to be dependent on the specific morphological form of the yeast, because Sap1–Sap3 are expressed primarily by the yeast-like forms, whereas Sap4–Sap6 are characteristic for hyphal forms. Saps that belong to these groups have a high sequence similarity to Sap8 which constitutes the third group together with Sap7 that shares only 20–27% sequence identity with other proteases and with Sap9 and Sap10 which are slightly closer homologs [30, 33].
Dendrogram presenting the amino acid sequence similarity between the members of C. albicans aspartic protease family (Sap1–Sap10). A close relationship of Saps to S. cerevisiae yapsins (Yps) is also emphasized. The optimal pH for Sap action and the preferential hydrolysis sites are also specified [25, 30]
3 Biochemical Properties of C. albicans Aspartic Proteases
So far, for four out of ten Saps of C. albicans, the crystal structures have been solved, including Sap1 in an inhibitor-free form [34], the complexes of Sap2 with inhibitor A70450 [35, 36] and benzamidine [37], Sap3 in the free form and bound with pepstatin A [38], and the complex of Sap5 with pepstatin A [34]. The latter structure is presented in Fig. 3. All structurally characterized Sap isoenzymes show similar features that classify them as pepsin-like aspartic proteases. These kidney-shaped bilobed globular proteins predominantly consisting of β-sheets are clearly divided into N-terminal and C-terminal domains, each providing one catalytic Asp residue, belonging to highly conserved regions in aspartic proteases with the motifs Asp-Ser-Gly or Asp-Thr-Gly and the disulfide bridge. Another conserved region that overlaps the active center is a β-hairpin loop, commonly known as the active site flap, which contains a catalytically essential Tyr residue. The disulfide bridges tie together the N-terminal and C-terminal entrance loops. The presence of the N-terminal entrance loop, consisting of 11 amino acids and specified as the second site flap [39], distinguishes Saps from the other aspartic proteases [34, 38, 40].
Structure of the complex of Sap5 with pepstatin A (pepA). a The overall structure of the Sap molecule, showing its kidney-shaped appearance and the predominance of β-sheets. The loops tied together by the disulfide bridges are specified as the N-terminal entrance loop (cysteine residues 47 and 59 showed as blue sticks) (N-ent loop) and the C-terminal entrance loops (cysteine residues 256 and 294) (C-ent loops). b A close-up view of the active site with marked conserved Asp32 and Asp218 residues and the disulfide bridge (Cys47 and Cys 59), Lys50, Trp51, and Arg52 residues forming the N-ent loop directed to the active site cleft and the residues Thr222, Ile223, Tyr225, Glu295, Arg 297, and Arg299 involved in substrate binding in the S4 pocket. Yellow dashed lines indicate hydrogen bonds between pepA and residues that form the substrate binding pocket. The figure was made with Pymol [41], PDB ID:2QZX
In addition, the structural and conformational differences allow the Sap isoenzyme structures to be divided into distinct subgroups. The most significant differences between Sap1–Sap3 and Sap5 regard the substrate binding site pockets, which have different characteristics, shapes, and sizes. On one hand, the S3 and S4 pockets, relatively large and with negative polar character in Sap1–Sap3, in Sap5 have a reduced size and the polar character is turned highly positive due to the substitutions of Leu297 (Sap1–Sap3), Asp299 (Sap2), Asp120 (Sap2, Sap3), and Gly299 (Sap1, Sap3) residues with Arg residues. On the other hand, the S2 pocket is enlarged in Sap5 because of the replacement of Asn131 (Sap1, Sap2) with Gly. The S1 and S2 substrate binding pockets in the central region of the enzymes show only a few differences, of which the formation of an extra cavity within the S1 pocket in Sap5 due to the substitution of Arg195 and Glu193 with Thr195 and Lys193 is the most important. Another significant difference is a narrowed entrance to the active site cleft in Sap5 relative to Sap1–Sap3 because the N-terminal loop in the former has larger residues, such as Lys50, Trp51, and Arg52, pointing down into the substrate binding cleft. Although the active site is strongly negative in all isoenzymes, the overall electrostatic charge of Sap5 is positive while Sap1, Sap2 and Sap3 are negatively charged. The difference in overall electrostatic charge of the molecule can underlie a rise of the optimal pH for Sap5 activity, compared to Sap1–Sap3 [34].
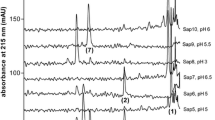
The pH dependence of Sap enzymatic activity was characterized for recombinant proteins [30, 42,43,44] as well as for Sap1–Sap3 purified from C. albicans culture supernatants [45] and determined using resorufin-labeled casein [30, 42], FRETS-25Ala library [30], bovine hemoglobin [43], bovine serum albumin [45], and a peptide, histatin 5 (His5) [44]. The analysis performed in the broad range of pH between 2.0 and 7.5 indicated that most of Saps displayed the optimum for proteolytic activities at pH 3.0–5.0 (Table 1), a feature typical for aspartic proteases; however, slightly variable results were obtained by different research groups. The pH optimal for Sap4–Sap6, Sap7, Sap9–Sap10 is less acidic, and the enzymes are still active at neutral pH. Sap3 and Sap8 differ from other Saps in showing substantial activity at pH 2.0. Interestingly, Sap8 shows the lowest pH optimum of 2.5, whereas Sap7, which is the less related with other Saps, shows the highest (6.5). The activity of all Saps, except Sap7, is inhibited by the classic aspartic protease inhibitor, pepstatin A. It has been suggested that pepstatin A insensitivity is due to the presence of Met242 and Thr467 residues which restrict the accessibility of pepstatin A to the binding site [46]. The biochemical characteristics of Sap isozymes are summarized in Table 1 [30].
Substrate specificities of all ten Sap isoenzymes (briefly summarized in Fig. 2) were determined by using FRETS-25Xaa libraries [30] or distinct peptide substrates [32, 43, 47]. A study of the substrate specificities at the P1 and P1′ sites for Sap1–Sap3 and Sap6 [43] showed that P1′ specificities are generally broader than those observed for P1. In general, Sap1–Sap6 and Sap8 have a broad substrate specificity and, like other aspartic proteases, prefer to hydrolyze peptide bonds after hydrophobic residues such as Leu, Phe, and Tyr, but also after positively charged residues such as Arg and Lys. In contrast, Sap7, Sap9, and Sap10 have narrower substrate specificities and prefer at the P1 site residues such as Met, Arg, and His Sap9 and Sap10 perform hydrolysis after dibasic (LysArg, LysLys) or monobasic (Lys, Arg) residues [32, 47], and almost all Saps hydrolyze peptide bonds before Ala [30]. Based on the similarities and differences in substrate specificities, Sap isozymes can be categorized into three groups [30]. Group 1 comprises Sap7 and Sap10, and most notably differs from other Saps in terms of substrate specificity, which here is narrowest. Sap4–Sap6 are categorized into group 2, and group 3 comprises Sap1–Sap3 and Sap8–Sap9, with a very similar, broad substrate specificity.
4 Functions of Saps in C. albicans Virulence
C. albicans exploits its proteolytic enzymes for host tissue invasion and inactivation of the host’s immune defense, to establish fungal infection. These factors are mandatory for the degradation of tissue barriers and acquiring nutrition at different host niches [48]. The adaptation to the host environment and the propagation of infections as well as further dissemination demand the involvement of the proteases in, for instance, combating the host immune cells like neutrophils or mononuclear phagocytes [49] as well as inactivating proteins of the complement system [50]. The roles of Saps during host infection, in terms of interactions of these pathogen proteases with major cellular, proteinaceous and peptide targets of the host, and the further consequences of these interactions, are briefly summarized in Fig. 4, and will be discussed in detail in the following subsections.
4.1 Expression of C. albicans Aspartic Protease Genes During Candidal Infection
As the individual members of C. albicans Sap family play diverse roles during both commensal and pathogenic interactions with the host, their genes are differentially expressed at various body sites, depending on the type, phase, and site of the infection [25, 51,52,53]. SAP1–SAP3 gene expression was detected in both yeast and hyphal cells. SAP1–SAP3 genes, predominantly expressed during mucosal infections [51, 54], were suggested to be significant for infection process in general, whereas the gene encoding Sap4, which belongs to the Sap4–Sap6 subfamily, was expressed in the hyphal phase during the adhesion to and penetration of epithelial cells [33, 52]. This Sap isoenzyme was suggested to be essential for the development of systemic infections and to be involved in avoiding the immune response [55]. In vivo, analysis of the expression of SAP1–SAP8 genes in oral candidiasis [25, 51, 52] showed the highest frequency of SAP2 expression both in colonized and infected patients. During oral infections, the expression of SAP1, SAP4, SAP7, and SAP8 genes was also detected at a significant level [25]. In the oral reconstituted human epithelium (RHE) model, SAP1 and SAP3 expression was detected, followed by SAP2 and SAP8 expression [57]. In contrast, in the RHE model of vaginal candidiasis, SAP2 and SAP9 expression preceded SAP1 expression [58]. Nevertheless, in both oral and vaginal RHE models, SAP1–SAP3 and SAP9 contributed to tissue damage [25, 58, 59]. In addition, an extensive expression of SAP1–SAP3 and SAP7–SAP8 genes was observed in a model that mimicked bloodstream infections [55, 60]. An investigation of SAP7 expression during C. albicans adhesion to the intestinal human cells indicated a meaningful role of Sap7 during the initial adaptation of C. albicans to intestinal tract which decreased over time [61]. Sap8 correlates mostly with oral or vaginal infections, with the expression of its gene detected in a RHE model together with SAP1–SAP3 [33]. SAP9 was one of the most expressed genes in vivo during human mucosal infections and in oral RHE models [54] and detected in both infectious and commensal forms of C. albicans. The Sap9 enzyme was suggested to play a role in the cell wall integrity, as well as the efficiency of yeast cells in contact with the mucosal surface of the host [32]. The clinical specimens of patients suffering from acute oral candidosis and from a lesion of chronic oral candidosis showed the expression of SAP1, SAP2, SAP3, and SAP6 genes [57]. The data regarding the expression of Sap-encoding genes, involving human samples and animal models, are summarized in Table 2.
4.2 Degradation of Main Functional Proteins of the Host
A broad spectrum of host substrates hydrolyzed by Saps, identified in early studies, included lactoferrin, lactoperoxidase, cathepsin D, albumin, hemoglobin, and the extracellular matrix components such as keratin, collagen, and vimentin [25, 48]. Sap2, produced in high amounts by yeast-like forms of C. albicans, was shown to contribute to the damage of mucin, the main component of protective layer for the mucous membrane [69]. The degradation of mucin can facilitate not only the penetration of mucous barrier enabling the further invasion of tissues, but can also provide carbon and nitrogen required for fungal growth [70].
The activity of Saps also affects the structural integrity of the epithelium. During the contact of C. albicans with the human oral mucosa, C. albicans uses its proteolytic potential to degrade E-cadherin in epithelial adherent junctions. Studies with protease mutant strains indicated that Sap5 is the major enzyme responsible for this process [71].
The invasion of host tissue can also be facilitated due to the degradation of proteinaceous components of subendothelial extracellular matrix, mainly laminin and fibronectin. Their proteolysis could presumably be important in the process of bloodstream penetration by the yeast [72]. Evidence suggested that strains that possessed a higher proteolytic activity strongly adhered to epidermal keratinocytes [73], corneocytes [74], and cells of the oral mucosa [75]. Although the role of Sap activity in this process was partly confirmed with the use of the specific inhibitor, pepstatin A, the mechanism of this effect was not fully elucidated. It was proposed that the increased adhesion to host cells resulted from the Sap-dependent degradation of certain host surface proteins which revealed additional potential binding sites for C. albicans [56].
Presumably, Sap9 and Sap10 can also participate in the regulation of adhesion due to the degradation of chitin synthases that participate in the process of cell wall formation, and a number of yeast surface proteins such as yeast-form cell wall protein 1 (Ywp1), agglutinin-like sequence protein 2 (Als2), and the protein repressed during hyphae development 3 (Rhd3) [32, 47].
4.3 The Interaction of Saps with the Complement System and the Antibodies
After invading host tissues, C. albicans encounters the innate immune system that acts against the pathogen through numerous antimicrobial peptides, the complement system, and specialized immune proteins and cells [50]. C. albicans aspartic proteases can prevent or modulate the functionality of immunoglobulins, in particular immunoglobulin A, resistant to the majority of bacterial proteases, which influences the attachment of C. albicans to buccal epithelial cells [76, 77].
The components of the complement system involved in pathogen removal were also shown to be targets of Saps [78, 79]. Sap1, Sap2, and Sap3 degraded complement proteins C3b, C4b, and C5, preventing both phagocytosis and the final formation of the terminal complement complex (TCC) and thus the activation of the selected mechanisms of the immune response [78]. Furthermore, Sap2 was able to degrade factor H, a complement system controller whose binding to the surface of C. albicans cells can increase the fungicidal response through bridging yeast and host immune cells. The same protease could also degrade CR3 and CR4, and FHR-1 receptor involved in the recognition of pathogens by the cells of the immune system [80].
4.4 Propelling the Host Proteolytic Cascades: The Kinin Production and Clot Formation
During fungal cell proliferation and further dissemination, Saps are able to degrade important components of proteolytic cascades involved in maintaining the biochemical homeostasis of the host organism, including proteins that comprise the contact system (i.e., the surface-activated kinin-generating system in plasma) and the blood clotting pathways [78, 80,81,82,83].
Primarily aimed at effectively defending against microbial infections, the activation of the contact system that results in the production of kinins can also, to some extent, be beneficial for pathogens [84]. The kinins are vasoactive peptides [85] and play an important role of inflammation mediators [86]. The increased permeabilization of blood vessels caused by kinins can not only support the migration of immune cells but can also increase the availability of nutrients for the pathogens and the possibility of disseminating the infection [87]. The contact system consists of two initially inactive serine proteases—factor XII and plasma prekallikrein—and a non-enzymatic protein, high-molecular-mass kininogen (HK). The factor XII is activated on a contact with negatively charged cell surfaces and subsequently activates prekallikrein. The active kallikrein releases a kinin—the nonapeptide bradykinin—from HK [88]. Kinins can also be released from the low-molecular-mass kininogen (LK), which does not belong to the contact system, but serves as the substrate for tissue kallikrein [89].
During the infection, C. albicans can trigger the release of kinins indirectly, by the activation of factor XII [90] or by direct action of Saps on HK molecule [81]. It was reported that mixtures of proteases secreted into a growth medium by both morphological forms of C. albicans released kinins from both HK and LK [81]. Studies with purified Sap2 confirmed its ability to release kinins from kininogens and also clearly indicated that LK is a protein much more susceptible to the direct proteolysis than HK [91]. The detailed analysis of LK degradation by all Saps showed that the majority of proteases, except Sap7, are able to produce kinins [92]. Sap3 released Met-Lys-bradykinin—a peptide able to exert the kinin-like biological effects through the activation of cellular kinin receptors—to a very high yield. Other Saps (except Sap9) could produce small amounts of the same kinin and bradykinin but primarily generated peptides comprising a kinin sequence extended at N- and/or C-termini. These peptides could be further processed by the action of Sap9, resulting in an efficient production of Met-Lys-bradykinin. The cooperative degradation of kininogens by several Saps can be exploited by C. albicans to produce an optimal amount of kinins at the site of the infection. However, Sap9 alone released des-Arg1-bradykinin, a peptide devoid of kinin-like biological activity [92].
The activation of coagulation factor XII by Saps can also initiate the process of blood clotting; however, this protein is not the only component of the cascade that is susceptible to a limited proteolysis by Saps. The process of fibrin clot formation can also be assisted by the Sap-dependent activation of factor X and prothrombin. A contribution of Saps to the development of the fibrin clot may underlie the septic coagulation and an insufficient peripheral circulation during infections [83, 93].
4.5 Deregulation of Host Proteases by Degradation of Their Inhibitors
Saps are able to degrade proteinaceous inhibitors that control the activity of main proteases of the host. Sap2 was shown to cleave α2-macroglobulin [94], cystatin A [95], and α1-protease inhibitor (A1PI), the latter also being susceptible to the action of Sap1, Sap3, Sap 4, and Sap9 [96]. By impairing the enzyme-inhibitor balance through the inactivation of the inhibitor molecule, Saps can indirectly contribute to the destruction of host tissues, supporting the process of infection. For instance, it was shown that the proteolytic cleavage of A1PI may assist in damaging epithelial and endothelial cells, caused by neutrophil extracellular traps (NETs). NETs are defense structures composed of DNA and microbicidal molecules released from neutrophil after a contact with a variety of microorganisms and molecules, which appear in response to infection, such as interleukin 8 (IL-8) [97]. Pathogens located within the NETs are exposed to direct contact with microbicidal molecules including neutrophil elastase (NE). The degradation of A1PI contributes to unrestrained NE activity, which might lead to the damage of host tissues, thereby supporting the colonization of the host by C. albicans cells that survived despite the killing properties of NETs. Furthermore, the degraded inhibitor had a reduced ability to complexation of IL-8 which can contribute to the increased influx of neutrophils to the site of infection and the progression of NET formation [96].
4.6 Interaction with Host Cells
The first host cells that come into contact with C. albicans but play an important function in preventing the fungal invasion are epithelial cells. Saps probably assist the adhesion of fungal cells to epithelium, acting as a ligand for the host cell receptors or modifying the surface components of both types of cells to allow for better interaction [25]. The E-cadherin cleavage by Saps resulted in epithelial integrity destruction and an increase of monolayer permeability [71, 98].
Sap4-Sap6 have the ability to bind to epithelial surface integrins. This interaction, mediated by Sap amino acid motif RGD/KGD, enables the internalization of proteases to endosomes and lysosomes by a still unknown mechanism. The location of these proteases in acidic interior of lysosomes leads to their activation, resulting in a partial permeabilization of the lysosome membrane and a subsequent caspase activation [99]. This kind of apoptotic pathway has been well established and occurs in many pathological conditions [100].
Proteases of C. albicans have the ability to induce cytokine expression by host cells. An increase in the production of interleukin-1β (IL-1β) and tumor necrosis factor (TNF-α) was observed in the macrophages after stimulation with Sap1–Sap3 and Sap6. Additionally, all these proteases except Sap3 increased the secretion of IL-6. The induction of cytokine secretion appeared to be regulated by the Akt/NF-κB activation and was independent of the Sap enzymatic activity [101]. It was also shown that aspartic proteases expressed by both morphological forms of C. albicans were able to produce IL-1β by direct, limited proteolysis of its precursor [102].
The formation of mature interleukin requires the involvement of apoptosis-associated speck-like protein (ASC), pro-caspase-1, and activated NLRP3 inflammasome, which is a pro-inflammatory complex presented in the monocytes, monocyte-derived macrophages, and dendritic cells (Fig. 5). It was shown that Sap2 and Sap6 were able to stimulate this inflammatory process, undergoing an internalization via the clathrin-dependent mechanism [103].
NLRP3 inflammasome activation by Sap2 and Sap6 that leads to IL-1β and IL-18 production [103 modified]
At the place of infection, the fungal pathogens are faced with locally presented or attracted phagocytes, mainly neutrophils and macrophages. Regardless of their efficiency, C. albicans cells have developed several mechanisms to evade phagocyte control, with the engagement of proteolytic enzymes (see the reviews: [104, 105]).
Neutrophils, equipped with many receptors sensitive to fungal pathogen-associated molecular patterns (PAMP), are the main immune cells involved in the host defense against C. albicans. These phagocytes migrate to the place of the fungal infection across Sap concentration gradient, in a dose-dependent manner [106]. The chemoattractant properties of those proteases, confirmed in a study of Candida mutant strains with selective deletion of Sap genes, were attributed to Sap9 [107]. The influx of neutrophils to the place of infection was also confirmed in vivo, in a mice model, in response to Sap2 [108].
Saps can also influence the ROS production by the activation of neutrophil oxidative burst, as was deduced from an observed decrease of ROS formation during the contact of neutrophils with C. albicans mutant strains with deleted Sap9-encoding gene [107]. Both processes seemed to depend on Sap proteolytic activity, because enzymatically inactive Saps did not cause neutrophil activation [108]. A further stimulation of neutrophils with Sap9 also triggered the apoptosis of these cells [107]. On the other hand, independently of their enzymatic activity, Saps induce interleukin release by epithelial cells. Interleukins, especially IL-8, are chemoattracting agents for neutrophils; therefore, inactive Saps can also indirectly modulate the influx of neutrophils to the infection foci [109].
The formation of NETs, composed of decondensed chromatin incrusted with a subset of granular proteins, is a relatively recently recognized mechanism used by neutrophils to capture and kill the microbial pathogens outside of the phagocyte cells [110]. We recently found SAP genes to be overexpressed in the yeast during the contact with NET-forming neutrophils [111]. On the other hand, the SAP-encoded proteins triggered the NET release in a dose-dependent manner, engaging two different mechanisms, which depended on fungal morphology and correlated with preference to secreted Sap type (Fig. 6). For Sap1–Sap2 and Sap8–Sap10, we observed the release of NETs in a ROS-dependent way. Sap5 and Sap7 acted similarly, but with lower efficiency. A ROS-independent mechanism of NETosis was observed for neutrophils treated with Sap4 and Sap6, for which the NADPH oxidase inhibition only partially lowered the NET release (unpublished data).
4.7 Sap Impact on the Action of Antimicrobial Peptides Produced by the Host
Besides degrading a vast number of the host proteins, the arsenal of ten C. albicans Saps effectively degrades and neutralizes some of human antimicrobial peptides (AMPs) which are key components of the innate immune system of the host, and represent a first, primitive line of defense against attacks of a wide range of microorganisms and are often called natural antibiotics.
It has been shown that C. albicans cells use Saps to hydrolytically inactivate His5, a histidine-rich cationic salivary component that possesses potent antimicrobial activities, in particular against C. albicans [112]. The investigation of four C. albicans aspartic proteases—Sap2, Sap5, Sap9, and Sap10—showed that His5 is effectively cleaved by all these enzymes except Sap5 and that the main protease responsible for His5 degradation is Sap9. A recent study expanded the known characteristic of His5 degradation on all ten C. albicans proteases using peptide chemistry methods [44] and indicated that seven Sap family members (Sap1–Sap4 and Sap7–Sap9, used as recombinant proteins) could rapidly degrade this salivary AMP under conditions corresponding to the oral cavity environment.
Human cathelicidin LL-37 was another human AMP shown to be prone to Sap-dependent degradation and inactivation [111]. This cationic α-helical AMP with antimicrobial and immunomodulatory properties [113], constitutively expressed in epithelial cells and the cells of the innate immune system such as human neutrophils, was cleaved into multiple products by six Sap enzymes, Sap1–Sap4 and Sap8–Sap9. The progress of degradation deprived this peptide from its fungicidal activity, thus enabling the pathogen to survive and propagate despite presence of AMP.
Nonetheless, at the initial stages of Sap treatment of two peptides, LL-37 and His5, truncated derivatives—LL-25, LL8-37, His-21, His-17, and His-13—that still possessed some antifungal activity were produced and, therefore, the body’s first line of defense against the infection was initially sustained [44, 111]. However, the LL-25 peptide, despite possessing antifungal properties, was devoid of the immunomodulatory properties of full-length LL-37, i.e., did not affect the generation of ROS by neutrophils, lowered the chemoattractant activity toward neutrophils by significantly decreased calcium flux and IL-8 production after neutrophil stimulation, and also lost the function of an inhibitor of neutrophil apoptosis [111].
It was recently demonstrated [114] that Saps can degrade and inactivate two antimicrobial peptides—designated NAT26 and HKH20—that can potentially be excised from human kininogens by host proteases such as NE [115, 116]. The NAT26, a helical and positively charged peptide responsible for the antimicrobial properties of the domain 3 of LK and HK, was effectively cleaved by all Saps except Sap10. In contrast, the HKH20, a histidine- and lysine-rich, positively charged peptide derived from domain 5 of HK, was completely cleaved only by Sap9.
A susceptibility of human AMPs to Sap action is schematically summarized in Fig. 7.
A detailed kinetic analysis of Sap-catalyzed degradation of LL-37 [111], His5 [44], and NAT26 and HKH20 [114] revealed that, despite the high hydrolytic activity of these proteases in an acidic environment, most of them were able to process the peptides over a broad pH range, with the highest activity at a neutral pH for Sap3, Sap4, and Sap9. These findings suggest that proteolytic processing of AMP can possibly proceed in the various niches of the body where C. albicans reside.
4.8 Involvement of Saps in the Formation and Resistance of Polymicrobial Biofilm
On mucosal or artificial surfaces, C. albicans forms three-dimensional polymicrobial communities with extracellular matrix layers also containing host immune cells. Such a complex biofilm is highly resistant to the host’s immune activity and antifungal drugs [117].
The role of Saps in biofilm formation is poorly recognized. In the simple artificial models, it was demonstrated that C. albicans biofilm secreted more Saps than the planktonic counterparts [118]. In the oral mucosal epithelia model coinfected with C. albicans and Streptococcus oralis, the microorganisms synergized to activate the host enzyme, calpain 1, involved in the cleavage of epithelial junction proteins and increased fungal invasion but the fungal protease activity was not required for this affect [119]. In the study of a biofilm, formed by C. albicans and oral streptococci, the cell wall-associated Sap9 was found to be required for the control of hyphal filamentation of C. albicans, and for the regulation of mixed species biofilm formation [120].
5 Secreted Aspartic Proteases of Other Candida Species and Their Roles in Candidal Infections
Apart from C. albicans, three non-albicans Candida species possess in their genome the genes that encode secreted aspartic proteases: C. parapsilosis (SAPP1–SAPP3), C. tropicalis (SAPT1–SAPT4), and C. dubliniensis (SAPCD1–SAPCD4, SAPCD7–SAPCD10).
C. parapsilosis possesses three SAPP genes (SAPP1–SAPP3) and two SAPP2 homologs that demonstrate 91.5% amino acid sequence identity. To date, only the products of SAPP1 and SAPP2 genes have been isolated and purified [121, 122]. Both Sapp1 and Sapp2 are extracellular enzymes; however, Sapp1 was also reported to occur in a cell wall-attached form [123]. They have an identical molecular mass of 37 kDa, and their amino acid sequence is 53% identical [124]. While the secretion of Sapp2 does not depend on the type of nitrogen source, the production of Sapp1 is induced by the presence of protein in the growth medium [121]. The optimal pH for Sapp1 and Sapp2 hydrolytic activity is in the acidic pH range, and Sapp1 possesses a broad substrate specificity [121, 125].
Currently, the tertiary structures of Sapp1 and of one of the Sapp2 homologs are known [122, 125]. During the maturation of proenzymes, they can be activated autocatalytically or by the action of endoproteinase Kex2, and only removed peptides possess potential glycosylation sites [124, 126].
It was reported that C. parapsilosis aspartic proteases demonstrated the ability to degrade several host proteins, i.e., Sapp1 hydrolyzed IgA and activated prothrombin and coagulation factor X, while Sapp2 degraded keratin and trypsinogen [121, 127]; both proteases had the ability to generate biologically active kinins from human kininogens [81, 128].
Sapt1 is the only secreted aspartic protease of the Sapt family that could be successfully isolated from C. tropicalis cultures. The amino acid sequence similarities between particular Sapts do not exceed 63% but they are closely related to the enzyme produced by C. albicans, with Sapt1 showing a large similarity to Sap8, while Sapt4 showed similarities to the Sap1–Sap3 subfamily [129]. A tertiary structure of Sapt1 is already known [130]. The production of this enzyme can be induced by the presence of an exogenous protein, such as bovine serum albumin, in the culturing medium [131]. C. tropicalis proteases might be directly involved in fungal invasion, with the destruction of the host tissues and degradation of the host proteins, e.g., of the human kininogens with generating of kinin-related peptides [81], and their activity may be also important for fungal cell adhesion and development of the disseminated candidiasis in patients with leukemia and neutropenia [132]. However, the expression of the SAPT genes during the colonization of the oral epithelium was not strictly correlated with the invasion [133].
C. tropicalis also produces tropiase, a protease that does not belong to the Sapt family. In contrast to the previously described enzymes, tropiase demonstrates the proteolytic activity in a broader pH range of 7–9 and is stable at pH between 3 and 12 and at high temperatures [134]. Tropiase is involved in the degradation of casein, keratin, and collagen. Moreover, this enzyme also hydrolyzes α and β chains of fibrinogen, but without demonstrated clotting activity and fibrin formation. Interestingly, the purified tropiase possesses hemorrhagic and capillary permeability-increasing activities which may highly contribute to the development of candidiasis [134, 135].
Another non-albicans Candida species, C. glabrata, which is more closely related to baker’s yeast S. cerevisiae than to other pathogenic species of Candida genus, possesses in its genome at least 11 YPS genes which are similar in structure to SAP genes [136]. The YPS-encoded proteins (yapsins) constitute a family of aspartic proteinases with a GPI-anchor, involved in the maintenance of cell wall integrity and cell–cell interactions. C. glabrata yapsins are considered to have a strong structural similarity to Sap9 and Sap10 [32].
6 Fungal Aspartic Proteases as Drug Targets—Future Application
From the perspective of Saps’ contribution to the fungal pathogenicity, they are ideal drug targets, especially in the context of increasing resistance of C. albicans strains against the commonly used antifungal agents. The inactivation of Saps could successfully stop the infections on different levels correlated with the facets of the infection process. They can be the targets for the process of tissue barrier degradation, destruction of the host’s defense molecules, acquiring nutrients for pathogen propagation, the adhesion, and biofilm formation on the host tissues or abiotic surfaces [39, 137,138,139,140].
However, due to their wide substrate specificity and broad range of pH operation [30], it is difficult to find a universal inhibitor, working with high efficiency. Pepstatin A, the most popular inhibitor of aspartic proteases like pepsin and cathepsin D, is also effective toward C. albicans Saps as was presented in many in vitro studies [141]. In the model of human oral candidiasis, it was shown that the inhibition of Saps with pepstatin A can influence the fungal adhesion and invasion, associated with a reduction of tissue damages [142]. However, its inhibition profile toward Saps is not universal. The activity of Sap9 and Sap10, GPI-anchored to the fungal cell membrane, was only partially blocked by pepstatin A [47], and Sap7 was proven to be insensitive to pepstatin A [46]. Some researchers also suggested that the effectiveness of pepstatin A action can be restricted to the used models or conditions [143]. Moreover, the possible therapeutic application of pepstatin A in mice model failed due to its metabolism in the liver and rapid clearance from the blood [144].
An interesting opportunity has opened for finding Saps inhibitors since an observation of declined Candida infections in AIDS patients after the application of antiretroviral therapy that included HIV protease inhibitors (HIV PIs). Since Candida Saps and HIV proteinase belong to the same class of aspartic proteases, it was postulated that HIV PIs can be also effective against Saps in vivo [36, 145]. Among analyzed compounds, ritonavir was the most potent inhibitor of Sap2, the main candidal protease active in fungal infection, while saquinavir, indinavir, and nelfinavir inhibited Sap2 activity with lower efficiency [72, 146]. The inhibitory activity of these compounds toward Sap1–Sap3 and the attenuation of Candida cell adhesion were observed in RHE model of oral candidiasis and in a model of experimental rat vaginitis [147]. However, it is not clear whether the modulation of Candida adhesion to epithelial cells, observed in vitro, results only from proteolytic activity of Saps, that can affect some proteinaceous targets on the surface of epithelial cells, allowing for better adherence of fungus to them. The current results also pointed out a possible interruption of some specific interactions of aspartic proteases, not connected with their enzymatic activity, with the host proteins located on the surface of these cells. Such drugs, blocking the adhesion of Candida cells, would be particularly attractive. However, this issue was addressed by only one report for oral candidiasis [148].
Currently used antifungal drugs, which take advantage of their inhibitory activity toward Candida aspartic proteases, do not satisfy the medical standards, due to their potency, pharmacokinetic properties, and increased toxicity at higher concentration [149]. Therefore, new sources of Sap inhibitors are being sought including programmed, variable domain antibodies, produced against Sap2, whose protective properties were observed in experimental rat vaginal candidiasis [150]. Many peptidomimetic inhibitors have been developed that are derived from the structure of pepstatin A, which inhibited proteases of different Candida species [148]. Also the molecular modeling and new key structural information about Saps’ active centers have been adopted for a design and synthesis of new Sap inhibitors [151,152,153]. Research was also focused on natural sources of inhibitors, including the extracts of plants [154], bacteria [155], and marine organisms [156] or artificial materials such as triangular gold nanoparticles [157].
The current progressive increase in fungal resistance to the available drugs, a noticeable shift of the infection profiles toward non-albicans Candida species, as well as the problems with toxicity and delivery of existing drugs to the place of infection should prompt the search for various fungal targets. At this point, candidal aspartic proteases, with their broad spectrum of engagement in physiological and pathological processes, seem to be among the best candidates.
References
Yapar N (2014) Epidemiology and risk factors for invasive candidiasis. Ther Clin Risk Manag 10:95–105
Pfaller MA, Diekema DJ (2007) Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev 20:133–163
Horn DL, Neofytos D, Anaissie EJ et al (2009) Epidemiology and outcomes of candidemia in 2019 patients: data from the prospective antifungal therapy alliance registry. Clin Infect Dis 48:1695–1703
Pana ZD, Farmaki E, Roilides E (2014) Host genetics and opportunistic fungal infections. Clin Microbiol Infect 20:1254–1264
Eggimann P, Que YA, Revelly JP, Pagani JL (2015) Preventing invasive Candida infections. Where could we do better? J Hosp Infect 89:302–308
Perlroth J, Choi B, Spellberg B (2007) Nosocomial fungal infections: epidemiology, diagnosis, and treatment. Med Mycol 45:321–346
Kullberg BJ, Arendrup MC (2016) Invasive candidiasis. N Engl J Med 374:794–795
Gudlaugsson O, Gillespie S, Lee K et al (2003) Attributable mortality of nosocomial candidemia, revisited. Clin Infect Dis 37:1172–1177
Soll DR, Galask R, Schmid J et al (1991) Genetic dissimilarity of commensal strains of Candida spp. carried in different anatomical locations of the same healthy women. J Clin Microbiol 29:1702–1710
Cannon RD, Chaffin WL (1999) Oral colonization by Candida albicans. Crit Rev Oral Biol Med 10:359–383
Akpan A, Morgan R (2002) Oral candidiasis. Postgrad Med J 78:455–459
Achkar JM, Fries BC (2010) Candida infections of the genitourinary tract. Clin Microbiol Rev 23:253–273
Mendling W, Brasch J, Cornely OA et al (2015) Guideline: vulvovaginal candidosis (AWMF 015/072), S2k (excluding chronic mucocutaneous candidosis). Mycoses S1:1–15
Patil S, Rao RS, Majumdar B, Anil S (2015) Clinical appearance of oral Candida infection and therapeutic strategies. Front Microbiol 6:1391
Lewis RE (2009) Overview of the changing epidemiology of candidemia. Curr Med Res Opin 25:1732–1740
Diekema D, Arbefeville S, Boyken L et al (2012) The changing epidemiology of healthcare-associated candidemia over three decades. Diagn Microbiol Infect Dis 73:45–48
Arendrup MC (2013) Candida and candidaemia. Susceptibility and epidemiology. Dan Med J 60:B4698
Krcmery V, Barnes AJ (2002) Non-albicans Candida spp. causing fungaemia: pathogenicity and antifungal resistance. J Hosp Infect 50:243–260
Karkowska-Kuleta J, Rapala-Kozik M, Kozik A (2009) Fungi pathogenic to humans: molecular bases of virulence of Candida albicans, Cryptococcus neoformans and Aspergillus fumigatus. Acta Biochim Pol 56:211–224
Naglik JR, Moyes DL, Wächtler B, Hube B (2011) Candida albicans interactions with epithelial cells and mucosal immunity. Microbes Infect 13:963–976
Polke M, Hube B, Jacobsen ID (2015) Candida survival strategies. Adv Appl Microbiol 91:139–235
Liu Y, Filler SG (2011) Candida albicans Als3, a multifunctional adhesin and invasin. Eukaryot Cell 10:168–173
Karkowska-Kuleta J, Kozik A (2014) Moonlighting proteins as virulence factors of pathogenic fungi, parasitic protozoa and multicellular parasites. Mol Oral Microbiol 29:270–283
Karkowska-Kuleta J, Kozik A (2015) Cell wall proteome of pathogenic fungi. Acta Biochim Pol 62:339–351
Naglik JR, Challacombe SJ, Hube B (2003) Candida albicans secreted aspartyl proteinases in virulence and pathogenesis. Microbiol Mol Biol Rev 67:400–428
Schaller M, Borelli C, Korting HC, Hube B (2005) Hydrolytic enzymes as virulence factors of Candida albicans. Mycoses 48:365–377
Hruskova-Heidingsfeldova O (2008) Secreted proteins of Candida albicans. Front Biosci 13:7227–7242
Höfs S, Mogavero S, Hube B (2016) Interaction of Candida albicans with host cells: virulence factors, host defense, escape strategies, and the microbiota. J Microbiol 54:149–169
Staib F (1965) Serum-proteins as nitrogen source for yeastlike fungi. Sabouraudia 4:187–193
Aoki W, Kitahara N, Miura N et al (2011) Comprehensive characterization of secreted aspartic proteases encoded by a virulence gene family in Candida albicans. J Biochem 150:431–438
Dos Santos ALS (2010) HIV aspartyl protease inhibitors as promising compounds against Candida albicans. World J Biol Chem 1:21–30
Albrecht A, Felk A, Pichova I (2006) Glycosylphosphatidylinositol-anchored proteases of Candida albicans target proteins necessary for both cellular processes and host-pathogen interactions. J Biol Chem 281:688–694
Silva NC, Nery JM, Dias ALT (2014) Aspartic proteinases of Candida spp.: role in pathogenicity and antifungal resistance. Mycoses 57:1–11
Borelli C, Ruge E, Lee JH et al (2008) X-ray structures of Sap1 and Sap5: structural comparison of the secreted aspartic proteinases from Candida albicans. Proteins 72:1308–1319
Cutfield SM, Dodson EJ, Anderson BF et al (1995) The crystal structure of a major secreted aspartic proteinase from Candida albicans in complexes with two inhibitors. Structure 3:1261–1271
Abad-Zapatero C, Goldman R, Muchmore SW et al (1996) Structure of a secreted aspartic protease from C. albicans complexed with a potent inhibitor: implications for the design of antifungal agents. Protein Sci 5:640–652
Behnen J, Koster H, Neudert G et al (2012) Experimental and computational active site mapping as a starting point to fragment-based lead discovery. Chem Med Chem 7:248–261
Borelli C, Ruge E, Schaller M et al (2007) The crystal structure of the secreted aspartic proteinase 3 from Candida albicans and its complex with pepstatin A. Proteins 68:738–748
Stewart K, Abad-Zapatero C (2001) Candida proteases and their inhibition: prospects for antifungal therapy. Curr Med Chem 8:941–948
Monod M, Staib P, Borelli C (2013) Candidapepsin. In: Handbook of proteolytic enzymes, vol 1, pp 159–166
Delano WL (2006) The PyMol molecular graphics system. Delano Scientific LLC, San Carlos
Borg-von Zepelin M, Beggah S, Boggian K et al (1998) The expression of the secreted aspartyl proteinases Sap4 to Sap6 from Candida albicans in murine macrophages. Mol Microbiol 28:543–554
Koelsch G, Tang J, Loy JA et al (2000) Enzymic characteristics of secreted aspartic proteases of Candida albicans. Biochim Biophys Acta 1480:117–131
Bochenska O, Rapala-Kozik M, Wolak N et al (2016) The action of ten secreted aspartic proteases of pathogenic yeast Candida albicans on major human salivary antimicrobial peptide, histatin 5. Act Biochi Pol 63:1–8
Smolenski G, Sullivan PA, Cutfield SM, Cutfield JF (1997) Analysis of secreted aspartic proteinases from Candida albicans: purification and characterization of individual Sap1, Sap2 and Sap3 isoenzymes. Microbiology 143:349–356
Aoki W, Kitahara N, Miura N et al (2012) Candida albicans possesses Sap7 as a pepstatin A-insensitive secreted aspartic protease. PLoS ONE 7:1–9
Schild L, Heyken A, de Groot PWJ et al (2011) Proteolytic cleavage of covalently linked cell wall proteins by Candida albicans Sap9 and Sap10. Eukaryot Cell 10:98–109
Hube B (1998) Possible role of secreted proteinases in Candida albicans infections. Rev Iberoam Micol 15:65–68
Cheng SC, Joosten LA, Kullberg BJ et al (2012) Interplay between Candida albicans and the mammalian innate host defense. Infect Immun 80:1304–1313
Zipfel PF, Hallström T, Riesbeck K (2013) Human complement control and complement evasion by pathogenic microbes–tipping the balance. Mol Immunol 56:152–160
Naglik JR, Newport G, White TC et al (1999) In vivo analysis of secreted aspartyl proteinase expression in human oral candidiasis. Infect Immun 67:2482–2490
Schaller M, Januschke E, Schackert C et al (2001) Different isoforms of secreted aspartyl proteinases (Sap) are expressed by Candida albicans during oral and cutaneous candidosis in vivo. J Med Microbiol 50:743–747
Staniszewska M, Siennicka K, Pilat J et al (2012) Role of aspartic proteinases in Candida albicans virulence. Part II: Expression of SAP1-10 aspartic proteinase during Candida albicans infections in vivo. Post Mikrobiol 51:137–142
Naglik JR, Moyes D, Makwana J et al (2008) Quantitative expression of the Candida albicans secreted aspartyl proteinase gene family in human oral and vaginal candidiasis. Microbiology 154:3266–3280
Staniszewska M, Bondarczyk MM, Siennicka K et al (2012) In vitro study of secreted aspartyl proteinases Sap1 to Sap3 and Sap4 to Sap6 expression in Candida albicans pleomorphic forms. Pol J Microbiol 61:247–256
Naglik JR, Rodgers C, Shirlaw PJ et al (2003) Differential expression of Candida albicans secreted aspartyl proteinase and phospholipase B genes in humans correlates with active oral and vaginal infections. J Infect Dis 188:469–479
Schaller M, Korting HC, Schafer W et al (1998) Investigations on the regulation of secreted aspartyl proteases in a model of oral candidiasis in vivo. Mycoses 41:69–73
Schaller M, Bein M, Korting HC et al (2003) The secreted aspartyl proteinases Sap1 and Sap2 cause tissue damage in an in vitro model of vaginal candidiasis based on reconstituted human vaginal epithelium. Infect Immun 71:3227–3234
Schaller M, Hube B, Ollert MW et al (1999) In vivo expression and localization of Candida albicans secreted aspartyl proteinases during oral candidiasis in HIV-infected patients. J Invest Dermatol 112:383–386
Staniszewska M, Bondaryk M, Malewski T, Kurzatkowski W (2014) Quantitative expression of Candida albicans aspartyl proteinase genes SAP7, SAP8, SAP9, SAP10 in human serum in vitro. Pol J Microbiol 63:15–20
Staniszewska M, Bondaryk M, Zukowski K, Chudy M (2015) Role of SAP7-10 and morphological regulators (EFG1, CPH1) in Candida albicans hypha formation and adhesion to colorectal carcinoma Caco-2. Pol J Microbiol 64:203–210
Sanglard D, Hube B, Monod M et al (1997) A triple deletion of the secreted aspartyl proteinase genes SAP4, SAP5, and SAP6 of Candida albicans causes attenuated virulence. Infect Immun 65:3539–3546
Hube B, Sanglard D, Odds FC et al (1997) Disruption of each of the secreted aspartyl proteinase genes SAP1, SAP2 and SAP3 of Candida albicans attenuates virulence. Infect Immun 65:3529–3538
Kretschmar M, Felk A, Staib P et al (2002) Individual acid aspartic proteinases (Saps) 1–6 of Candida albicans are not essential for invasion and colonization of the gastrointestinal tract in mice. Microb Pathog 32:61–70
Felk A, Kretschmar M, Albrecht A et al (2002) Candida albicans hyphal formation and the expression of the Efg1-regulated proteinases Sap4 to Sap6 are required for the invasion of parenchymal organs. Infect Immun 70:3689–3700
Correia A, Lermann U, Teixeira L et al (2010) Limited role of secreted aspartyl proteinases Sap1 to Sap6 in Candida albicans virulence and host immune response in murine hematogenously disseminated candidiasis. Infect Immun 78:4839–4849
Jackson BE, Wilhelmus KR, Hube B (2007) The role of secreted aspartyl proteinases in Candida albicans keratitis. Invest Ophthalmol Vis Sci 48:3559–3565
Stringaro A, Crateri P, Pellegrini G et al (1997) Ultrastructural localization of the secretory aspartyl proteinase in Candida albicans cell wall in vitro and in experimentally infected rat vagina. Mycopathologia 137:95–105
Hube B, Monod M, Schofield DA et al (1994) Expression of seven members of the gene family encoding secretory aspartyl proteinases in Candida albicans. Mol Microbiol 14:87–99
Colina AR, Aumont F, Deslauriers N et al (1996) Evidence for degradation of gastrointestinal mucin by Candida albicans secretory aspartyl proteinase. Infect Immun 64:4514–4519
Villar CC, Kashleva H, Nobile CJ et al (2007) Mucosal tissue invasion by Candida albicans is associated with E-cadherin degradation, mediated by transcription factor Rim101p and protease Sap5p. Infect Immun 75:2126–2135
Morschhäuser J, Virkola R, Korhonen TK, Hacker J (1997) Degradation of human subendothelial extracellular matrix by proteinase-secreting Candida albicans. FEMS Microbiol Lett 153:349–355
Ollert MW, Söhnchen R, Korting HC et al (1993) Mechanisms of adherence of Candida albicans to cultured human epidermal keratinocytes. Infect Immun 61:4560–4568
Ray TL, Payne CD (1988) Scanning electron microscopy of epidermal adherence and cavitation in murine candidiasis: a role for Candida acid proteinase. Infect Immun 56:1942–1949
Borg M, Rüchel R (1988) Expression of extracellular acid proteinase by proteolytic Candida spp. during experimental infection of oral mucosa. Infect Immun 56:626–631
Rüchel R (1986) Cleavage of immunoglobulins by pathogenic yeasts of the genus Candida. Microbiol Sci 3:316–319
Marcotte H, Lavoie MC (1998) Oral microbial ecology and the role of salivary immunoglobulin A. Microbiol Mol Biol Rev 62:71–109
Gropp K, Schild L, Schindler S et al (2009) The yeast Candida albicans evades human complement attack by secretion of aspartic proteases. Mol Immunol 47:465–475
Luo S, Skerka C, Kurzai O, Zipfel PF (2013) Complement and innate immune evasion strategies of the human pathogenic fungus Candida albicans. Mol Immunol 56:161–169
Svoboda E, Schneider AE, Sándor N et al (2015) Secreted aspartic protease 2 of Candida albicans inactivates factor H and the macrophage factor H-receptors CR3 (CD11b/CD18) and CR4 (CD11c/CD18). Immunol Lett 168:13–21
Rapala-Kozik M, Karkowska-Kuleta J, Ryzanowska A et al (2010) Degradation of human kininogens with the release of kinin peptides by extracellular proteinases of Candida spp. Biol Chem 391:823–830
Rüchel R (1983) On the renin-like activity of Candida proteinases and activation of blood coagulation in vitro. Zentralbl Bakteriol Mikrobiol Hyg A 255:368–379
Kaminishi H, Hamatake H, Cho T et al (1994) Activation of blood clotting factors by microbial proteinases. FEMS Microbiol Lett 121:327–332
Frick IM, Björck L, Herwald H (2007) The dual role of the contact system in bacterial infectious disease. Thromb Haemost 98:497–502
Cockcroft JR, Chowienczyk PJ, Brett SE, Ritter JM (1994) Effect of NG-monomethyl-L-arginine on kinin-induced vasodilation in the human forearm. Br J Clin Pharmacol 38:307–310
Golias C, Charalabopoulos A, Stagikas D el al (2007) The kinin system-bradykinin: biological effects and clinical implications. Multiple role of the kinin system-bradykinin. Hippokratia 11:124–128
Imamura T, Tanase S, Szmyd G et al (2005) Induction of vascular leakage through release of bradykinin and a novel kinin by cysteine proteinases from Staphylococcus aureus. J Exp Med 201:1669–1676
Wu Y (2015) Contact pathway of coagulation and inflammation. Thromb J 13:17
Lalmanach G, Naudin C, Lecaille F, Fritz H (2010) Kininogens: more than cysteine protease inhibitors and kinin precursors. Biochimie 92:1568–1579
Kaminishi H, Tanaka M, Cho T et al (1990) Activation of the plasma kallikrein-kinin system by Candida albicans proteinase. Infect Immun 58:2139–2143
Bras G, Bochenska O, Rapala-Kozik M et al (2012) Extracellular aspartic protease SAP2 of Candida albicans yeast cleaves human kininogens and releases proinflammatory peptides, Met-Lys-bradykinin and des-Arg(9)-Met-Lys-bradykinin. Biol Chem 393:829–839
Kozik A, Gogol M, Bochenska O et al (2015) Kinin release from human kininogen by 10 aspartic proteases produced by pathogenic yeast Candida albicans. BMC Microbiol 15:60
Rüchel R (1983) On the role of proteinases from Candida albicans in the pathogenesis of acronecrosis. Zentralbl Bakteriol Mikrobiol Hyg A 255:524–536
Kaminishi H, Miyaguchi H, Tamaki T et al (1995) Degradation of humoral host defense by Candida albicans proteinase. Infect Immun 63:984–988
Tsushima H, Mine H, Kawakami Y et al (1994) Candida albicans aspartic proteinase cleaves and inactivates human epidermal cysteine proteinase inhibitor, cystatin A. Microbiology 140:167–171
Gogol M, Ostrowska D, Klaga K et al (2016) Inactivation of α1-proteinase inhibitor by Candida albicans aspartic proteases favors the epithelial and endothelial cell colonization in the presence of neutrophil extracellular traps. Acta Biochim Pol 63:1163
Zawrotniak M, Rapala-Kozik M (2013) Neutrophil extracellular traps (NETs)—formation and implications. Acta Biochim Pol 60:277–284
Moyes DL, Richardson JP, Naglik JR (2015) Candida albicans-epithelial interactions and pathogenicity mechanisms: scratching the surface. Virulence 6:338–346
Wu H, Downs D, Ghosh K et al (2013) Candida albicans secreted aspartic proteases 4–6 induce apoptosis of epithelial cells by a novel Trojan horse mechanism. FASEB J 27:2132–2144
Johansson AC, Appelqvist H, Nilsson C et al (2010) Regulation of apoptosis-associated lysosomal membrane permeabilization. Apoptosis 15:527–540
Pietrella D, Rachini A, Pandey N et al (2010) The inflammatory response induced by aspartic proteases of Candida albicans is independent of proteolytic activity. Infect Immun 78:4754–4762
Beauséjour A, Grenier D, Goulet JP, Deslauriers N (1998) Proteolytic activation of the interleukin-1beta precursor by Candida albicans. Infect Immun 66:676–681
Pietrella D, Pandey N, Gabrielli E et al (2013) Secreted aspartic proteases of Candida albicans activate the NLRP3 inflammasome. Eur J Immunol 43:679–692
Jiménez-López C, Lorenz MC (2013) Fungal immune evasion in a model host-pathogen interaction: candida albicans versus macrophages. PLoS Pathog 9(11):e1003741
Cheng SC, Sprong T, Joosten LA et al (2012) Complement plays a central role in Candida albicans-induced cytokine production by human PBMCs. Eur J Immunol 42:993–1004
Ran Y, Iwabuchi K, Yamazaki M et al (2013) Secreted aspartic proteinase from Candida albicans acts as a chemoattractant for peripheral neutrophils. J Dermatol Sci 72:191–193
Hornbach A, Heyken A, Schild L et al (2009) The glycosylphosphatidylinositol-anchored protease Sap9 modulates the interaction of Candida albicans with human neutrophils. Infect Immun 77:5216–5224
Pericolini E, Gabrielli E, Amacker M et al (2015) Secretory aspartyl proteinases cause vaginitis and can mediate vaginitis caused by Candida albicans in mice. MBio 6:e00724–15
Gabrielli E, Sabbatini S, Roselletti E et al (2016) In vivo induction of neutrophil chemotaxis by secretory aspartyl proteinases of Candida albicans. Virulence 29:1–7
Brinkmann V, Reichard U, Goosmann C et al (2004) Neutrophil extracellular traps kill bacteria. Science 303:1532–1535
Rapala-Kozik M, Bochenska O, Zawrotniak M et al (2015) Inactivation of the antifungal and immunomodulatory properties of human cathelicidin LL-37 by aspartic proteases produced by the pathogenic yeast Candida albicans. Infect Immun 83:2518–2530
Meiller TF, Hube B, Schild L et al (2009) A novel immune evasion strategy of Candida albicans: proteolytic cleavage of a salivary antimicrobial peptide. PLoS ONE 4:e5039
Vandamme D, Landuyt B, Luyten W, Schoofs L (2012) A comprehensive summary of LL-37, the factotum human cathelicidin peptide. Cell Immunol 280:22–35
Bochenska O, Rapala-Kozik M, Wolak N et al (2015) Inactivation of human kininogen-derived antimicrobial peptides by secreted aspartic proteases produced by the pathogenic yeast Candida albicans. Biol Chem 396:1369–1375
Frick IM, Akesson P, Herwald H et al (2006) The contact system—A novel branch of innate immunity generating antibacterial peptides. EMBO J 25:5569–5578
Nordahl EA, Rydengård V, Mörgelin M, Schmidtchen A (2005) Domain 5 of high molecular weight kininogen is antibacterial. J Biol Chem 280:34832–34839
Ganguly S, Mitchell AP (2011) Mucosal biofilm of Candida albicans. Curr Opin Microbiol 14:380–385
Mendes A, Mores AU, Carvalho AP et al (2007) Candida albicans biofilms produce more secreted aspartyl protease than the planktonic cells. Biol Pharm Bull 30:1813–1815
Xu H, Sobue T, Bertolini M, Thompson A, Dongari-Bagtzoglou A (2016) Streptocuccus oralis and Candida albicans synergistically activate calpain to degrade E-cadherin from oral epithelial junctions. J Infect Dis 13:pii:jiw201
Dutton LC, Jenkinson HF, Lamont RJ, Nobbs AH (2016) Role of Candida albicans secreted aspartyl protease Sap9 in interkingdom biofilm formation. Pathog Dis 74:pii:ftw005
Hrusková-Heidingsfeldová O, Dostál J, Majer F et al (2009) Two aspartic proteinases secreted by the pathogenic yeast Candida parapsilosis differ in expression pattern and catalytic properties. Biol Chem 390:259–268
Dostál J, Pecina A, Hrusková-Heidingsfeldová O et al (2015) Atomic resolution crystal structure of Sapp2p, a secreted aspartic protease from Candida parapsilosis. Acta Cryst D 71:2494–2504
Vinterová Z, Sanda M, Dostál J et al (2011) Evidence for the presence of proteolytically active secreted aspartic proteinase 1 of Candida parapsilosis in the cell wall. Protein Sci 20:2004–2012
Hrušková-Heidingsfeldová O, Dostál J, Hamal P et al (2001) Enzymological characterization of secreted proteinases from Candida parapsilosis and Candida lusitaniae. Collect Czech Chem Commun 66:1707–1719
Dostál J, Brynda J, Hrusková-Heidingsfeldová O et al (2009) The crystal structure of the secreted aspartic protease 1 from Candida parapsilosis in complex with pepstatin A. J Struct Biol 167:145–152
Horváth P, Nosanchuk JD, Hamari Z et al (2012) The identification of gene duplication and the role of secreted aspartyl proteinase 1 in Candida parapsilosis virulence. J Infect Dis 205:923–933
Merkerová M, Dostál J, Hradilek M et al (2006) Cloning and characterization of Sapp2p, the second aspartic proteinase isoenzyme from Candida parapsilosis. FEMS Yeast Res 6:1018–1026
Bras G, Bochenska O, Rapala-Kozik M et al (2013) Release of biologically active kinin peptides, Met-Lys-bradykinin and Leu-Met-Lys-bradykinin from human kininogens by two major secreted aspartic proteases of Candida parapsilosis. Peptides 48:114–123
Parra-Ortega B, Cruz-Torres H, Villa-Tanaca L, Hernández-Rodríguez C (2009) Phylogeny and evolution of the aspartyl protease family from clinically relevant Candida species. Mem Inst Oswaldo Cruz 104:505–512
Symersky J, Monod M, Foundling SI (1997) High-resolution structure of the extracellular aspartic proteinase from Candida tropicalis yeast. Biochemistry 36:12700–12710
Zaugg C, Borg-Von Zepelin M, Reichard U et al (2001) Secreted aspartic proteinase family of Candida tropicalis. Infect Immun 69:405–412
Kontoyiannis D, Vaziri I, Hanna H et al (2001) Risk factors for Candida tropicalis fungemia in patients with cancer. Clin Infect Dis 33:1676–1681
Silva S, Negri M, Henriques M et al (2010) Silicone colonization by non-Candida albicans Candida species in the presence of urine. J Med Microbiol 59:747–754
Okumura Y, Inoue N, Nikai T (2007) Isolation and characterization of a novel acid proteinase, tropiase, from Candida tropicalis IFO 0589. Nihon Ishinkin Gakkai Zasshi 48:19–25
Chen YV, Rosli R, Fong SH et al (2012) Histopathological characteristics of experimental Candida tropicalis induced acute systemic candidiasis in BALB/c Mice. Int J Zool Res 1:12–22
Kaur R, Ma B, Cormack BP (2007) A family of glycosylphosphatidylinositol-linked aspartyl proteases is required for virulence of Candida glabrata. Proc Natl AcadSci USA 104:7628–7633
Nguyen JT, Hamada Y, Kimura T, Kiso Y (2008) Design of potent aspartic protease inhibitors to treat various diseases. Arch Pharm 341:523–535
Braga-Silva LA, Santos ALS (2011) Aspartic protease inhibitors as potential anti-Candida albicans drugs: impacts on fungal biology, virulence and pathogenesis. Curr Med Chem 18:2401–2419
Santos ALS (2011) Aspartic proteases of human pathogenic fungi are prospective targets for the generation of novel and effective antifungal inhibitors. Curr Enz Inhib 7:96–118
Bondaryk M, Kurzątkowski W, Staniszewska M (2013) Antifungal agents commonly used in the superficial and mucosal candidiasis treatment: mode of action and resistance development. Postępy Dermatol Alergol 30:293–301
Kuriyama T, Williams DW, Lewis MA (2003) In vitro secreted aspartyl proteinase activity of Candida albicans isolated from oral diseases and healthy oral cavities. Oral Microbiol Immunol 18:405–407
Schaller M, Schäfer W, Korting HC, Hube B (1998) Differential expression of secreted aspartyl proteinases in a model of human oral candidiosis and in patient samples from oral cavity. Mol Microbiol 29:605–615
Lermann U, Morschhäuser J (2008) Secreted aspartic proteases are not required for invasion of reconstituted human epithelia by Candida albicans. Microbiol 154:3281–3295
Rüchel R, Ritter B, Schaffrinski M (1990) Modulation of experimental systemic murine candidosis by intravenous pepstatin. Zentralbl Bakteriol Mikrobiol Hyg 273:391–403
Cauda R, Tacconelli M, Tumbarello M et al (1999) Role of protease inhibitors in preventing recurrent oral candidosis in patients with HIV infection: a prospective case-control study. J Acquir Immun Defic Syndr 21:20–25
Borg-Von Zeppelin M, Meyer I, Thomssen R et al (1999) HIV-protease inhibitors reduce cell adherence of Candida albicans strains by inhibition of yeast secreted aspartic proteases. J Investig Dermatol 113:747–751
Cassone A, De Bernardis F, Torosantucci A et al (1999) In vitro and in vivo anticandidal activity of human immunodeficiency vírus protease inhibitors. J Infect Dis 180:448
Pichova I, Pavlickova L, Dostal J et al (2001) Secreted aspartic proteases of Candida albicans, Candida tropicalis, Candida parapsilosis and Candida lusitaneae. Inhibition with peptidomimetic inhibitors. Eur J Biochem 268:2669–2677
Santos A, Braga-Silva L (2013) Aspartic protease inhibitors: effective drugs against the human fungal pathogen Candida albicans. Mini Rev Med Chem 13:155–162
De Bernardis F, Liu H, O’Mahony R et al (2007) Human domain antibodies against virulence traits of candida albicans inhibits fungus adherence to vaginal epithelium and protect against experimental vaginal candidiasis. J Infect Dis 195:149–157
Fear G, Komarnytsky S, Raskin I (2007) Protease inhibitors and their peptidomimetic derivatives as potential drugs. Pharmacol Ther 113:354–368
Cadicamo C, Mortier J, Wolber G et al (2013) Design, synthesis, inhibition studies, and molecular modeling of pepstatin analogs addressing different secreted aspartic proteases of Candida albicans. Biochem Pharmacol 85:881–887
Zielinska P, Staniszewska M, Bondaryk M et al (2015) Design and studies o multiple mechanism of anti-Candida activity of new potent-Trp-rich peptide dendrimers. Eur J Med Chem 105:106–119
Höfling JF, Mardegan RC, Anibal PC et al (2011) Evaluation of antifungal activity of medicinal plant extracts against oral Candida albicans and proteinases. Mycopathologia 172:117–124
Sato T, Nagai K, Shibazaki M et al (1994) Novel aspartyl protease inhibitors, YF-0200R-A and B. J Antibiot (Tokyo) 47:566–570
Christopeit T, Øverbø K, Danielson H, Nilsen IW (2013) Efficient screening of marine, FRET extracts for protease inhibitors by combining fret based activity assays and surface plasmon resonance spectroscopy based binding assays. Mar Drugs 11:4279–4293
Hajjar FHE, Jebali A, Hekmatimoghaddam S (2015) The inhibition of Candida albicans secreted aspartyl proteinase by triangular gold nanoparticles. Nanomedicine J 2:54–59
Acknowledgements
This work was supported in part by the National Science Centre of Poland (grant no. 571 UMO-2012/05/B/NZ1/00003 awarded to M.R.-K). Faculty of Biochemistry, Biophysics, and Biotechnology of Jagiellonian University is a partner of the Leading National Research Center (KNOW) supported by the Ministry of Science and Higher Education.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Gogol, M., Bochenska, O., Zawrotniak, M., Karkowska-Kuleta, J., Zajac, D., Rapala-Kozik, M. (2017). Roles of Candida albicans Aspartic Proteases in Host-Pathogen Interactions. In: Chakraborti, S., Dhalla, N. (eds) Pathophysiological Aspects of Proteases. Springer, Singapore. https://doi.org/10.1007/978-981-10-6141-7_15
Download citation
DOI: https://doi.org/10.1007/978-981-10-6141-7_15
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-6140-0
Online ISBN: 978-981-10-6141-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)