Abstract
Deep brain stimulation (DBS) is a widely used, efficacious neurosurgical treatment for neurological movement disorders. For example, electrical stimulation in the ventral intermediate thalamic nucleus drastically reduces tremor in patients with essential tremor. Likewise, stimulation in the subthalamic nucleus or the internal globus pallidus significantly attenuates tremor, rigidity, bradykinesia, and gait complications of Parkinson’s disease. Its application is now rapidly expanding to a wide variety of conditions including epilepsy, neuropsychiatric disorders, Tourette syndrome, Alzheimer’s disease, and intractable pain. However, the exact underlying therapeutic mechanisms of action of DBS remain unclear. Despite this lack of understanding, clinical utility of DBS cannot be underappreciated, and there is a great need for studies that can elucidate patient-specific optimization of DBS parameters and targets. This chapter explores recent approaches for studying the underlying mechanisms of action of DBS. Additionally, it discusses the limitations of current open-loop approaches to DBS and accentuates the importance of developing a smart closed-loop DBS system that can optimize therapeutic parameters in real time to individual patients and symptoms.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Deep Brain Stimulation
- Essential Tremor
- Tourette Syndrome
- Stimulation Parameter
- High Frequency Stimulation
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
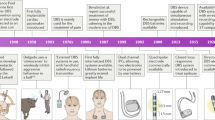
As recently as 30 years ago, surgical techniques for treating many neurologic disorders involved ablative procedures, potentially resulting in significant and sometimes generalized damage to the brain [26, 110]. The advent of thermal and cryogenic lesioning brought forth greater spatial selectivity during surgery; however, these procedures are irreversible and cannot be modulated if the treatment needs change [4, 10, 13]. In the early 1990’s, deep brain stimulation (DBS) became a reversible alternative to lesioning procedures for the treatment of movement disorders such as Parkinson disease and essential tremor [8, 9, 87]. Since then, the use of DBS has become more widespread for the effective treatment of other neurologic disorders such as dystonia [55, 64, 87, 96], Tourette syndrome [24, 46, 87, 104, 108], epilepsy [27, 52, 103], depression [25, 37, 72, 74], neuropathic pain [31, 48, 64, 87], and obsessive-compulsive disorder (OCD) [1, 33]. Additionally, DBS offers promising outcomes for the treatment of other neurological conditions ranging from bipolar disorder [45] and Alzheimer’s disease [58] to addiction [65], cerebral palsy [69, 107], and hyperphagic obesity [103] (Table 1). However, the underlying therapeutic mechanisms of DBS remain unknown despite years of research and successful clinical application.
The predominant hypothesis suggests that DBS modulates pathological activity via excitation of axonal fibers of passage and inhibition of local cell bodies [28, 73]. However, the integration of spatially and temporally distant signals suggests that the neural mechanisms underlying DBS efficacy may be far more complex [43]. Therefore, further advancement of DBS technology will require a greater understanding of the response to DBS on the molecular, biochemical, cellular, and circuitry levels. For example, the brain is a highly complex organ, with innumerable neural signals transmitted via distinct neurotransmitters capable of modulating neural activity across both local and global neural circuitry [40]. Thus, DBS may induce complex changes in synaptic plasticity that reorganize neural circuits and rectify neuropathological changes associated with neurological disorders. These changes could help explain the different timescales in therapeutic efficacy observed across different disorders. For example, DBS patients with Parkinson’s disease who experience immediate symptomatic relief, and patients with major depression who require longer intervals before symptomatic improvement can be observed [42].
2 Monitoring of Neural Activity
Numerous techniques are being utilized in clinical and preclinical studies to unravel the mechanisms of action of DBS and assist in target selection as well as optimization of stimulation parameters [35, 42]. These techniques allow examination of the neural responses to DBS at local and network-levels with high spatio-temporal resolutions. The most commonly utilized techniques include electrophysiological measurement of compound neural activity, electrochemical measurement of neurotransmitter signaling, and functional imaging techniques.
2.1 Electrophysiological Monitoring
Electrophysiological analysis has played an instrumental role in unraveling the function of the central nervous system (CNS) since the early 1950s, when Hodgkin and Huxley demonstrated the electrical nature of the action potential [44]. Since then, electrophysiological analysis techniques have evolved to enable the analysis of a broad range of neurological activity, from patch-clamp techniques that allowed the study of single ion channels, to single-unit recordings and global field potentials via multiunit recording arrays [75]. This technological diversity permits comprehensive evaluation of neurological activity from the subcellular to circuitry levels [35]. For example, electrophysiological techniques have been utilized to investigate the physiological mechanisms underlying DBS efficacy in the treatment of Tourette syndrome [47]. In this study, local field potential (LFP) recording electrodes were implanted into the thalamus, globus pallidus pars internal (GPi), or nucleus accumbens to analyze neural activity before, during, and after stimulation. Results from this study suggest that the pathophysiology of Tourette syndrome is related to dysfunctional synaptic transmission within deep brain nuclei, producing oscillations of inappropriate frequency and amplitude, and preventing the effective inhibition of stereotypical behaviors and tics such as blinking, head jerking, sniffing, throat clearing, and other vocalizations [2]. Similarly, excitatory postsynaptic potentials (EPSPs) evoked by high and low frequency stimulation of neurons within the subthalamic nucleus (STN) of 6-hydroxydopamine (6-OHDA)-lesioned rats revealed that high frequency stimulation produced significant EPSP depression in dopamine-depleted rats [115]. Similarly, low frequency stimulation resulted in EPSP augmentation in dopamine-intact rats [115].
2.2 Neurochemical Monitoring
Preclinical studies have demonstrated that neurotransmitter release is evoked by high frequency stimulation, and thus may be associated with the effects of DBS [60]. Fixed potential amperometry is a technique for measuring neurotransmitters and other analytes such as Glutamate, and involves the application of a constant voltage through a carbon fiber microelectrode implanted within the target of interest (Gale et al. 2013; Tye et al. 2013). Carbon fiber microelectrodes are coated with specific enzymes that react with non-electroactive analytes of interest, resulting in electroactive products that can be electrically measured [53]. The signals detected are caused by oxidative reactions between the applied voltage and the molecules of analyte within the extracellular space (Van Gompel et al. 2010). Unfortunately, the continuous enzyme delivery required to detect the neurotransmitter of interest makes this technique impractical for chronic in vivo detection of neurochemicals (Jacobs et al. 2010). Fast scan cyclic voltammetry (FSCV) is an alternative electroanalytical technique capable of real-time detection of electroactive neurotransmitters, hormones, and other metabolites [34, 51]. Previous studies have demonstrated that FSCV can effectively detect serotonin, norepinephrine, epinephrine, dopamine, and adenosine, as well as changes in oxygen and pH [41, 88, 106]. FSCV relies on the delivery of rapid voltage oscillations to allow oxidation and reduction of electrically active compounds of interest, resulting in the generation of unique electrical voltage versus current signatures specific for each analyte [88, 92]. By taking advantage of FSCV and a Wireless Instantaneous Neurotransmitter Concentration Sensing (WINCS) system designed to wirelessly measure neurochemical responses during DBS, Chang and colleagues showed that the immediate symptomatic relief induced by implantation of the DBS lead, also known as the microthalamotomy effect (Tasker 1998) was accompanied by a neurochemical signature resembling that of adenosine release [18, 19] (Fig. 1). Previous preclinical animal studies have demonstrated that administration of adenosine A1 agonists alleviates tremor symptoms in mice models of harmaline-induced essential tremor [7]. Therefore, it is possible that enhancement of adenosine signaling induced by the microthalamotomy effect, or by the administration of adenosine agonists, inhibits the maladaptive excitatory signaling producing uncontrolled movement in patients with essential tremor. However, the CNS contains multiple receptors for adenosine that operate through a variety of G-proteins, including Gs, Gq, and Gi. Variable effects in synaptic transmission are observed based on their localization on presynaptic, postsynaptic, or astrocytic membranes and the subsequent downstream signaling from the G-protein coupled receptor [79].
Fast scan cyclic voltammetry recording during DBS electrode implantation into the VIM of the thalamus. a Pseudocolor plot collected from an awake patient. The plot depicts oxidation currents immediately on DBS electrode insertion. Black arrow indicates a second oxidation current peak. b Pseudocolor plot collected during electrical stimulation (130 Hz, 60 μsec pulse width, 2 V) through DBS electrode (in 4 out of 7 awake patients; no significant oxidation currents were not observed in the other 3 patients). The plot indicates oxidation current at a switching potential (1.5 V). Black arrow points to a much smaller second oxidation current. c, d Cyclic voltammograms (current versus voltage) at black dotted lines from A and B. Modified from [18]
2.3 Functional Imaging
Functional magnetic resonance imaging (fMRI) is an MRI technique that measures changes in blood flow [62]. The utility of this technique for characterizing the effects of DBS is based upon the principle that the magnitude of cerebral blood flow and oxygen consumption is proportional to the relative activity of individual brain regions due to differential energy requirements during periods of neural activity [105]. Specifically, the blood-oxygen-level dependent (BOLD) signal measures changes in the magnetization of hemoglobin following deoxygenation of blood within the CNS [77]. This enables the generation of an oxyhemoglobin/deoxyhemoglobin heat map based upon changes in oxygen consumption resulting from modulation of neural activity [94].
To this end, fMRI has been recently used to characterize the effects of high (130 Hz) and low (10 Hz) frequency stimulation on neural activity in a swine model of DBS [82]. In this study, modulation of activity in the sensorimotor cortex, basal ganglia, and cerebellum was observed as a function of the stimulus voltage applied to the ventrolateral (VL) thalamus. Specifically, Paek and colleagues showed that high frequency stimulation produced a negative BOLD response in the motor cortex, while low frequency stimulation produced a positive BOLD response. Additionally, they showed that by increasing the amplitude of the applied voltage, both the change in BOLD signal as well as the size of the affected brain region increased, correlating with an increase of neural activity (Fig. 2). This suggests that differences in BOLD response can be used to analyze brain responses to electrical stimulation and characterize these responses as a function of stimulation parameters.
Ventral lateral thalamus stimulation with different voltage intensities (3, 5, and 7 V). All voltages evoked increased BOLD signals in the ipsilateral prefrontal, primary somatosensory, insular cortices, and contralateral cerebellum. Also all voltages evoked decreased BOLD signal in the ipsilateral primary motor and premotor cortices. Abbreviations: BOLD, blood-oxygen-level dependent; CB, cerebellum; CC, cingulate cortex; DBS, deep brain stimulation; FDR, false discovery rate; IC, insular cortex; PFC, prefrontal cortex; PRIMC, primary motor cortex; PREMC, premotor cortex; V, voltage. Modified from [82]
In addition to characterization of the neural response to DBS, functional imaging may be also effectively utilized to facilitate identification of optimal DBS targets [87]. In this context, fMRI and positron emission tomography (PET) have already demonstrated clinical utility in the treatment of treatment-resistant depression. For example, an overactive subgenual cingulate cortex (Brodmann area 25) observed with PET has been shown in patients with acute sadness [71]. This overactivity has subsequently decreased in clinical responders following antidepressant treatments [25, 70, 71]. In 2005, Mayberg and colleagues used PET to show that chronic stimulation of the cingulate cortex in patients with treatment-resistant depression normalized metabolic hyperactivity and produced clinical benefits [72]. In that study, remission was accomplished in four out of six patients, with decreases in cerebral blood flow to subgenual cingulate, orbital frontal cortex, hypothalamus, anterior insula, and medial frontal cortex. At the same time, their results showed increases in cerebral blood flow within the dorsolateral prefrontal, dorsal anterior, posterior cingulate, premotor, and parietal regions.
3 Novel Stimulation Paradigms
While DBS has been used effectively to treat multiple disorders such as essential tremor and Parkinson disease, DBS technology must be further developed in order to improve patient care. For example, the existing DBS paradigm requires patients to return to the clinic for periodic adjustment of their stimulation parameters as their disease progresses [23, 35, 72]. Switching the existing DBS paradigm from an open-loop strategy where stimulation parameters are fixed, to an adaptive paradigm that relies on biological feedback to adjust stimulation parameters will be crucial for developing the next generation of DBS systems. Thus, closed-loop DBS systems equipped with electrophysiological, biochemical, and inertial sensors that monitor the molecular, cellular, and behavioral responses to DBS may allow for automated titration of stimulation parameters for sustained therapeutic benefits in the face of a changing environment. Developing a greater understanding of the cellular and molecular mechanisms of DBS by leveraging functional imaging in conjunction with neurochemical and electrophysiological techniques may also assist in optimizing DBS targets and stimulation parameters for specific disorders and individual patients [35]. Ultimately, adaptive, closed-loop DBS systems will extend battery life, reduce required hospital visits and associated healthcare costs [30].
Several key factors need to be investigated before automated adjustment of stimulation parameters can be clinically implemented. First, the complex relationships between clinical behavior and neural activity need to be elucidated. The advancement of electrochemical, electrophysiological, and functional imaging techniques from preclinical to clinical settings will be essential for the development of next-generation smart DBS systems. For example, optimal locations for recording of neural activity should be identified for specific disorders and specific patients. Furthermore, neurotransmitters critical for pathological activity and therapeutic response will need to be identified (Fitzgerald 2014). Additionally, specific neurotransmitter concentrations and their role in therapeutic efficacy will need to be elucidated. Second, the type of sensors that will be used to monitor the environment in order to effectively adjust stimulation parameters must be identified. The material of these sensors must be MRI safe and biocompatible for chronic implantation. For example, efforts are underway to develop electrochemical-sensing techniques capable of extending electrode longevity by renewing the electrochemically active surface following adsorption of chemical species [102]. This is paramount, as the carbon fiber microelectrodes typically used for FSCV are subject to electrode fouling due to the charge imbalance of the waveforms required for FSCV and are thus not suitable for chronic measurements [11]. Recent efforts to overcome this limitation have been focused on the use of boron-doped diamond microelectrodes that can be used over longer periods of time [15, 17, 39, 68, 83, 85, 93, 97, 99, 114, 116, 118]. Third, correlation of multimodal electrophysiological and neurochemical activity may provide new insight into the cellular and molecular mechanisms of therapeutic neuromodulation. Therefore, efforts should be directed toward developing smart DBS controllers that rely on the relationships between neural activity and the clinical effects of DBS to replace the trial-and-error process currently used for clinical DBS programming [35, 91, 100]. The versatility and adaptability of such controllers will allow optimization of DBS therapies to individual patients and symptoms. In turn, this will likely improve clinical outcomes, reduce the time and frequency of patient visits, and decrease overall health care costs.
4 Conclusion
Despite its clinical efficacy, limitations in existing DBS technology make optimization of therapeutic benefits a difficult and expensive endeavor. However, combination of multimodal electrophysiological and neurochemical sensing with functional imaging techniques may provide new insight into the cellular and molecular mechanisms of therapeutic DBS. By focusing on these techniques that further the efforts in understanding the underlying therapeutic mechanisms of DBS, we may be able to tailor application of DBS to individual patients and symptoms. Furthermore, the development of closed-loop DBS strategies will likely lead to the improvement of therapeutic outcomes.
References
Abelson, J.L., Curtis, G.C., Sagher, O., Albucher, R.C., Harrigan, M., Taylor, S.F., Martis, B., Giordani, B.: Deep brain stimulation for refractory obsessive-compulsive disorder. Biol. Psychiatr. 57(5), 510–516 (2005). doi:10.1016/j.biopsych.2004.11.042
Albin, R.L., Mink, J.W.: Recent advances in Tourette syndrome research. Trends Neurosci. 29(3), 175–182 (2006). doi:10.1016/j.tins.2006.01.001
Amorim, B.O., Covolan, L., Ferreira, E., Brito, J.G., Nunes, D.P., de Morais, D.G., Nobrega, J.N., Rodrigues, A.M., deAlmeida, A.C., Hamani, C.: Deep brain stimulation induces antiapoptotic and anti-inflammatory effects in epileptic rats. J. neuroinflamm 12, 162 (2015). doi:10.1186/s12974-015-0384-7
Aziz, T.Z., Peggs, D., Sambrook, M.A., Crossman, A.R.: Lesion of the subthalamic nucleus for the alleviation of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced parkinsonism in the Primate. Mov. Disord. 6(4), 288–292 (1991). doi:10.1002/Mds.870060404
Barbas, H., Saha, S., Rempel-Clower, N., Ghashghaei, T.: Serial pathways from primate prefrontal cortex to autonomic areas may influence emotional expression. BMC neurosci. 4, 25 (2003). doi:10.1186/1471-2202-4-25
Bejjani, B.P., Arnulf, I., Vidailhet, M., Pidoux, B., Damier, P., Papadopoulos, S., Bonnet, A.M., Cornu, P., Dormont, D., Agid, Y.: Irregular jerky tremor, myoclonus, and thalamus: a study using low-frequency stimulation. Mov. Disord. 15(5), 919–924 (2000). doi:10.1002/1531-8257(200009)15:5<919:Aid-Mds1024>3.0.Co;2-0
Bekar, L., Libionka, W., Tian, G.F., Xu, Q., Torres, A., Wang, X., Lovatt, D., Williams, E., Takano, T., Schnermann, J., Bakos, R., Nedergaard, M.: Adenosine is crucial for deep brain stimulation-mediated attenuation of tremor. Nat. Med. 14(1), 75–80 (2008). doi:10.1038/nm1693
Benabid, A.L., Pollak, P., Gao, D., Hoffmann, D., Limousin, P., Gay, E., Payen, I., Benazzouz, A.: Chronic electrical stimulation of the ventralis intermedius nucleus of the thalamus as a treatment of movement disorders. J. Neurosurg. 84(2), 203–214 (1996). doi:10.3171/jns.1996.84.2.0203
Benabid, A.L., Pollak, P., Gervason, C., Hoffmann, D., Gao, D.M., Hommel, M., Perret, J.E., de Rougemont, J.: Long-term suppression of tremor by chronic stimulation of the ventral intermediate thalamic nucleus. Lancet 337(8738), 403–406 (1991)
Benazzouz, A., Gross, C., Feger, J., Boraud, T., Bioulac, B.: Reversal of rigidity and improvement in motor-performance by subthalamic high-frequency Stimulation in MPTP-treated monkeys. Eur. J. Neurosci. 5(4), 382–389 (1993). doi:10.1111/J.1460-9568.1993.Tb00505.X
Bennet, K.E., Tomshine, J.R., Min, H.K., Manciu, F.S., Marsh, M.P., Paek, S.B., Settell, M.L., Nicolai, E.N., Blaha, C.D., Kouzani, A.Z., Chang, S.Y., Lee, K.H.: A diamond-based electrode for detection of neurochemicals in the human brain. Front. Hum. Neurosci. 10, 102 (2016). doi:10.3389/fnhum.2016.00102
Bergey, G.K., Morrell, M.J., Mizrahi, E.M., Goldman, A., King-Stephens, D., Nair, D., Srinivasan, S., Jobst, B., Gross, R.E., Barkley, G., Salanova, V., Olejniczak, P., Cole, A., Cash, S.S., Noe, K., Wharen, R., Worrell, G., Murro, A.M., Edwards, J., Duchowny, M., Spencer, D., Smith, M., Geller, E., Gwinn, R., Skidmore, C., Eisenschenk, S., Berg, M., Heck, C., Van Ness, P., Fountain, N., Rutecki, P., Massey, A., O’Donovan, C., Labar, D., Duckrow, R.B., Hirsch, L.J., Courtney, T., Sun, F.T., Seale, C.G.: Long-term treatment with responsive brain stimulation in adults with refractory partial seizures. Neurology 84, 810–817 (2015)
Bergman, H., Wichmann, T., Delong, M.R.: Reversal of experimental parkinsonism by lesions of the subthalamic nucleus. Science 249(4975), 1436–1438 (1990). doi:10.1126/Science.2402638
Bewernick, B.H., Kayser, S., Sturm, V., Schlaepfer, T.E.: Long-term effects of nucleus accumbens deep brain stimulation in treatment-resistant depression: evidence for sustained efficacy. Neuropsychopharmacology 37, 1975–1985 (2012)
Bitziou, E., O’Hare, D., Patel, B.A.: Simultaneous detection of pH changes and histamine release from oxyntic glands in isolated stomach. Anal. Chem. 80(22), 8733–8740 (2008). doi:10.1021/ac801413b
Blomstedt, P., Sandvik, U., Tisch, S.: Deep brain stimulation in the posterior subthalamic area in the treatment of essential tremor. Mov. Disord. 25, 1350–1356 (2010)
Chan, H.Y., Aslam, D.M., Wiler, J.A., Casey, B.: A novel diamond microprobe for neuro-chemical and -electrical recording in neural prosthesis. J. Microelectromech. Syst. 18(3), 511–521 (2009). doi:10.1109/JMEMS.2009.2015493
Chang, S.Y., Kim, I., Marsh, M.P., Jang, D.P., Hwang, S.C., Van Gompel, J.J., Goerss, S.J., Kimble, C.J., Bennet, K.E., Garris, P.A., Blaha, C.D., Lee, K.H.: Wireless fast-scan cyclic voltammetry to monitor adenosine in patients with essential tremor during deep brain stimulation. Mayo Clin. Proc. 87(8), 760–765 (2012). doi:10.1016/j.mayocp.2012.05.006
Chang, S.Y., Shon, Y.M., Agnesi, F., Lee, K.H.: Microthalamotomy effect during deep brain stimulation: potential involvement of adenosine and glutamate efflux. In: Conference Proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society IEEE Engineering in Medicine and Biology Society Conference, 2009, pp. 3294–3297 (2009). doi:10.1109/IEMBS.2009.5333735
Constantoyannis, C., Kumar, A., Stoessl, A.J., Honey, C.R.: Tremor induced by thalamic deep brain stimulation in patients with complex regional facial pain. Mov. Disord. Off. J. Mov. Disord. Soc. 19(8), 933–936 (2004). doi:10.1002/mds.20047
Denys, D., Mantione, M., Figee, M., van den Munckhof, P., Koerselman, F., Bosch, A., Schuurman, R.: Deep brain stimulation of the nucleus accumbens for treatment-refractory obsessive-compulsive disorder. Arch. Gen. Psychiatr. 67, 1061–1068 (2010)
Deuschl, G., Agid, Y.: Subthalamic neurostimulation for Parkinson’s disease with early fluctuations: balancing the risks and benefits. Lancet Neurol. 12, 1025–1034 (2013)
Deuschl, G., Herzog, J., Kleiner-Fisman, G., Kubu, C., Lozano, A.M., Lyons, K.E., Rodriguez-Oroz, M.C., Tamma, F., Troster, A.I., Vitek, J.L., Volkmann, J., Voon, V.: Deep brain stimulation: postoperative issues. Mov. Disord. Off. J. Mov. Disord. Soc. 21(Suppl 14), S219–S237 (2006). doi:10.1002/mds.20957
Diederich, N.J., Kalteis, K., Stamenkovic, M., Pieri, V., Alesch, F.: Efficient internal pallidal stimulation in Gilles de la Tourette syndrome: a case report. Mov. Disord. Off. J. Mov. Disord. Soc. 20(11), 1496–1499 (2005). doi:10.1002/mds.20551
Dougherty, D.D., Rezai, A.R., Carpenter, L.L., Howland, R.H., Bhati, M.T., O’Reardon, J.P., Eskandar, E.N., Baltuch, G.H., Machado, A.D., Kondziolka, D., Cusin, C., Evans, K.C., Price, L.H., Jacobs, K., Pandya, M., Denko, T., Tyrka, A.R., Brelje, T., Deckersbach, T., Kubu, C., Malone Jr., D.A.: A randomized sham-controlled trial of deep brain stimulation of the ventral capsule/ventral striatum for chronic treatment-resistant depression. Biol. Psychiatr. 78(4), 240–248 (2015). doi:10.1016/j.biopsych.2014.11.023
Faria, M.: Violence, mental illness, and the brain—a brief history of psychosurgery: part 2—from the limbic system and cingulotomy to deep brain stimulation. Surg. Neurol. Int. 4 (2013)
Fisher, R., Salanova, V., Witt, T., Worth, R., Henry, T., Gross, R., Oommen, K., Osorio, I., Nazzaro, J., Labar, D., Kaplitt, M., Sperling, M., Sandok, E., Neal, J., Handforth, A., Stern, J., De Salles, A., Chung, S., Shetter, A., Bergen, D., Bakay, R., Henderson, J., French, J., Baltuch, G., Rosenfeld, W., Youkilis, A., Marks, W., Garcia, P., Barbaro, N., Fountain, N., Bazil, C., Goodman, R., McKhann, G., Babu Krishnamurthy, K., Papavassiliou, S., Epstein, C., Pollard, J., Tonder, L., Grebin, J., Coffey, R., Graves, N., Group, S.S.: Electrical stimulation of the anterior nucleus of thalamus for treatment of refractory epilepsy. Epilepsia 51(5), 899–908 (2010). doi:10.1111/j.1528-1167.2010.02536.x
Florence, G., Sameshima, K., Fonoff, E.T., Hamani, C.: Deep brain stimulation: more complex than the inhibition of cells and excitation of fibers. Neurosci. Rev. J. Bring. Neurobiol. Neurol. Psychiatr. (2015). doi:10.1177/1073858415591964
Follett, K.A., Weaver, F.M., Stern, M., Hur, K., Harris, C.L., Luo, P., Marks, W.J., Rothlind, J., Sagher, O., Moy, C., Pahwa, R., Burchiel, K., Hogarth, P., Lai, E.C., Duda, J.E., Holloway, K., Samii, A., Horn, S., Bronstein, J.M., Stoner, G., Starr, P.A., Simpson, R., Baltuch, G., De Salles, A., Huang, G.D., Reda, D.J., CSP 468 Study Group: Pallidal versus subthalamic deep-brain stimulation for parkinson’s disease. New Engl. J. Med. 362, 2077–2091 (2010)
Fraix, V., Houeto, J.L., Lagrange, C., Le Pen, C., Krystkowiak, P., Guehl, D., Ardouin, C., Welter, M.L., Maurel, F., Defebvre, L., Rougier, A., Benabid, A.L., Mesnage, V., Ligier, M., Blond, S., Burbaud, P., Bioulac, B., Destee, A., Cornu, P., Pollak, P., Group, S.S.: Clinical and economic results of bilateral subthalamic nucleus stimulation in parkinson’s disease. J. Neurol. Neurosurg. Psychiatr. 77(4), 443–449 (2006). doi:10.1136/jnnp.2005.077677
Franzini, A., Ferroli, P., Leone, M., Broggi, G.: Stimulation of the posterior hypothalamus for treatment of chronic intractable cluster headaches: first reported series. Neurosurgery 52(5), 1095–1099; discussion 1099–1101 (2003)
Kuhn, J., Bührle, C.P., Lenartz, D., Sturm, V.: Deep brain stimulation in addiction due to psychoactive substance use. In: Handbook of Clinical Neurology, vol. 116, pp. 259–269 (2013)
Gabriels, L., Cosyns, P., Nuttin, B., Demeulemeester, H., Gybels, J.: Deep brain stimulation for treatment-refractory obsessive-compulsive disorder: psychopathological and neuropsychological outcome in three cases. Acta Psychiatr. Scand. 107(4), 275–282 (2003)
Glanowska, K.M., Venton, B.J., Moenter, S.M.: Fast scan cyclic voltammetry as a novel method for detection of real-time gonadotropin-releasing hormone release in mouse brain slices. J. Neurosci. Off. J. Soc. Neurosci. 32(42), 14664–14669 (2012). doi:10.1523/JNEUROSCI.1303-12.2012
Grahn, P.J., Mallory, G.W., Khurram, O.U., Berry, B.M., Hachmann, J.T., Bieber, A.J., Bennet, K.E., Min, H.K., Chang, S.Y., Lee, K.H., Lujan, J.L.: A neurochemical closed-loop controller for deep brain stimulation: toward individualized smart neuromodulation therapies. Front. Neurosci. 8, 169 (2014). doi:10.3389/fnins.2014.00169
Greenberg, B.D., Gabriels, L.A., Malone, D.A., Rezai, A.R., Friehs, G.M., Okun, M.S., Shapira, N.A., Foote, K.D., Cosyns, P.R., Kubu, C.S., Malloy, P.F., Salloway, S.P., Giftakis, J.E., Rise, M.T., Machado, A.G., Baker, K.B., Stypulkowski, P.H., Goodman, W.K., Rasmussen, S.A., Nuttin, B.J.: Deep brain stimulation of the ventral internal capsule/ventral striatum for obsessive-compulsive disorder: worldwide experience. Mol. Psychiatr. 15, 64–79 (2010)
Grubert, C., Hurlemann, R., Bewernick, B.H., Kayser, S., Hadrysiewicz, B., Axmacher, N., Sturm, V., Schlaepfer, T.E.: Neuropsychological safety of nucleus accumbens deep brain stimulation for major depression: effects of 12-month stimulation. World J. Biol. Psychiatr. 12(7), 516–527 (2011). doi:10.3109/15622975.2011.583940
Halpern, C.H., Wolf, J.A., Bale, T.L., Stunkard, A.J., Danish, S.F., Grossman, M., Jaggi, J.L., Grady, M.S., Baltuch, G.H.: Deep brain stimulation in the treatment of obesity. J. Neurosurg. 109, 625–634 (2008)
Halpern, J.M., Xie, S.T., Sutton, G.P., Higashikubo, B.T., Chestek, C.A., Lu, H., Chiel, H.J., Martin, H.B.: Diamond electrodes for neurodynamic studies in Aplysia californica. Diam. Relat. Mater. 15(2–3), 183–187 (2006). doi:10.1016/j.diamond.2005.06.039
Hamani, C., Temel, Y.: Deep brain stimulation for psychiatric disease: contributions and validity of animal models. Sci. Trans. Med. 4(142), 142rv148 (2012). doi:10.1126/scitranslmed.3003722
Heien, M.L., Johnson, M.A., Wightman, R.M.: Resolving neurotransmitters detected by fast-scan cyclic voltammetry. Anal. Chem. 76(19), 5697–5704 (2004). doi:10.1021/ac0491509
Herrington, T.M., Cheng, J.J., Eskandar, E.N.: Mechanisms of deep brain stimulation. J. Neurophysiol. 115(1), 19–38 (2016). doi:10.1152/jn.00281.2015
Hess, C.W., Vaillancourt, D.E., Okun, M.S.: The temporal pattern of stimulation may be important to the mechanism of deep brain stimulation. Exp. Neurol. 247, 296–302 (2013). doi:10.1016/j.expneurol.2013.02.001
Hodgkin, A.L., Huxley, A.F.: A quantitative description of membrane current and its application to conduction and excitation in nerve. J. Physiol. 117(4), 500–544 (1952)
Holtzheimer, P.E., Kelley, M.E., Gross, R.E., Filkowski, M.M., Garlow, S.J., Barrocas, A., Wint, D., Craighead, M.C., Kozarsky, J., Chismar, R., Moreines, J.L., Mewes, K., Posse, P.R., Gutman, D.A., Mayberg, H.S.: Subcallosal cingulate deep brain stimulation for treatment-resistant unipolar and bipolar depression. Arch. Gen. Psychiatr. 69(2), 150–158 (2012). doi:10.1001/archgenpsychiatry.2011.1456
Houeto, J.L., Karachi, C., Mallet, L., Pillon, B., Yelnik, J., Mesnage, V., Welter, M.L., Navarro, S., Pelissolo, A., Damier, P., Pidoux, B., Dormont, D., Cornu, P., Agid, Y.: Tourette’s syndrome and deep brain stimulation. J. Neurol. Neurosurg. Psychiatr. 76(7), 992–995 (2005). doi:10.1136/jnnp.2004.043273
Israelashvili, M., Loewenstern, Y., Bar-Gad, I.: Abnormal neuronal activity in Tourette syndrome and its modulation using deep brain stimulation. J. Neurophysiol. 114(1), 6–20 (2015). doi:10.1152/jn.00277.2015
Katayama, Y., Yamamoto, T., Kobayashi, K., Kasai, M., Oshima, H., Fukaya, C.: Motor cortex stimulation for phantom limb pain: comprehensive therapy with spinal cord and thalamic stimulation. Stereotact. Funct. Neurosurg. 77(1–4), 159–162 (2001). 64593
Kennedy, S.H., Giacobbe, P., Rizvi, S.J., Placenza, F.M., Nishikawa, Y., Mayberg, H.S., Lozano, A.M.: Deep brain stimulation for treatment-resistant depression: follow-up after 3 to 6 years. Am. J. Psychiatr. 168, 502–510 (2011)
Kiss, Z.H., Doig-Beyaert, K., Eliasziw, M., Tsui, J., Haffenden, A., Suchowersky, O.: Functional and stereotactic section of the Canadian neurosurgical society, Canadian movement disorders group. The Canadian multicentre study of deep brain stimulation for cervical dystonia. Brain 130, 2879–2886 (2007)
Kita, J.M., Wightman, R.M.: Microelectrodes for studying neurobiology. Curr. Opin. Chem. Biol. 12(5), 491–496 (2008). doi:10.1016/j.cbpa.2008.06.035
Kocabicak, E., Temel, Y., Hollig, A., Falkenburger, B., Tan, S.: Current perspectives on deep brain stimulation for severe neurological and psychiatric disorders. Neuropsychiatr. Dis. Treat. 11, 1051–1066 (2015). doi:10.2147/NDT.S46583
Koehne, J., Marsh, M., Boakye, A., Douglas, B., Kim, I., Chang, S., Jang, D., Bennet, K., Kimble, C., Andrews, R., Meyyappan, M.: Carbon nanofiber electrode array for electrochemical detection of dopamine using fast scan cyclic voltammetry. Analyst 136(9), 1802–1805 (2011)
Koller, W., Pahwa, R., Busenbark, K., Hubble, J., Wilkinson, S., Lang, A., Tuite, P., Sime, E., Lazano, A., Hauser, R., Malapira, T., Smith, D., Tarsy, D., Miyawaki, E., Norregaard, T., Kormos, T., Olanow, C.W.: High-frequency unilateral thalamic stimulation in the treatment of essential and parkinsonian tremor. Ann. Neurol. 42, 292–299 (1997)
Kumar, R., Dagher, A., Hutchison, W.D., Lang, A.E., Lozano, A.M.: Globus pallidus deep brain stimulation for generalized dystonia: clinical and PET investigation. Neurology 53(4), 871–874 (1999)
Kuncel, A.M., Grill, W.M.: Selection of stimulus parameters for deep brain stimulation. Clin. Neurophysiol. Off. J. Int. Fed. Clin. Neurophysiol. 115(11), 2431–2441 (2004). doi:10.1016/j.clinph.2004.05.031
Kupsch, A., Benecke, R., Müller, J., Trottenberg, T., Schneider, G.H., Poewe, W., Eisner, W., Wolters, A., Müller, J.U., Deuschl, G.: Pallidal deep-brain stimulation in primary generalized or segmental dystonia. N. Engl. J. Med. 355, 1978–1990 (2006)
Laxton, A.W., Lozano, A.M.: Deep brain stimulation for the treatment of Alzheimer disease and dementias. World Neurosurg. 80 (3–4), S28 e21–28. doi:10.1016/j.wneu.2012.06.028
Laxton, A.W., Tang-Wai, D.F., McAndrews, M.P., Zumsteg, D., Wennberg, R., Keren, R., Wherrett, J., Naglie, G., Hamani, C., Smith, G.S., Lozano, A.M.: A phase I trial of deep brain stimulation of memory circuits in Alzheimer’s disease. Ann. Neurol. 68, 521–534 (2010)
Lee, K.H., Chang, S.Y., Roberts, D.W., Kim, U.: Neurotransmitter release from high-frequency stimulation of the subthalamic nucleus. J. Neurosurg. 101(3), 511–517 (2004). doi:10.3171/jns.2004.101.3.0511
Limousin, P., Speelman, J.D., Gielen, F., Janssens, M.: Multicentre European study of thalamic stimulation in parkinsonian and essential tremor. J. Neurol. Neurosurg. Psychiatr. 66, 289–296 (1999)
Logothetis, N.K.: The neural basis of the blood-oxygen-level-dependent functional magnetic resonance imaging signal. Philos. Trans. R. Soc. Lond. B Biol. Sci. 357(1424), 1003–1037 (2002). doi:10.1098/rstb.2002.1114
Lozano, A.M., Giacobbe, P., Hamani, C., Rizvi, S.J., Kennedy, S.H., Kolivakis, T.T., Debonnel, G., Sadikot, A.F., Lam, R.W., Howard, A.K., Ilcewicz-Klimek, M., Honey, C.R., Mayberg, H.S.: A multicenter pilot study of subcallosal cingulate area deep brain stimulation for treatment-resistant depression. J. Neurosurg. 116, 315–322 (2012)
Lozano, A.M., Kumar, R., Gross, R.E., Giladi, N., Hutchison, W.D., Dostrovsky, J.O., Lang, A.E.: Globus pallidus internus pallidotomy for generalized dystonia. Mov. Disord. Off. J. Mov. Disord. Soc. 12(6), 865–870 (1997). doi:10.1002/mds.870120606
Luigjes, J., van den Brink, W., Feenstra, M., van den Munckhof, P., Schuurman, P.R., Schippers, R., Mazaheri, A., De Vries, T.J., Denys, D.: Deep brain stimulation in addiction: a review of potential brain targets. Mol. Psychiatr. 17(6), 572–583 (2012). doi:10.1038/mp.2011.114
Mallet, L., Polosan, M., Jaafari, N., Baup, N., Welter, M.L., Fontaine, D., du Montcel, S.T., Yelnik, J., Chéreau, I., Arbus, C., Raoul, S., Aouizerate, B., Damier, P., Chabardès, S., Czernecki, V., Ardouin, C., Krebs, M.O., Bardinet, E., Chaynes, P., Burbaud, P., Cornu, P., Derost, P., Bougerol, T., Bataille, B., Mattei, V., Dormont, D., Devaux, B., Vérin, M., Houeto, J.L., Pollak, P., Benabid, A.L., Agid, Y., Krack, P., Millet, B., Pelissolo, A., STOC Study Group: Subthalamic nucleus stimulation in severe obsessive-compulsive disorder. N. Engl. J. Med. 359, 2121–2134 (2008)
Malone, D.A., Dougherty, D.D., Rezai, A.R., Carpenter, L.L., Friehs, G.M., Eskandar, E.N., Rauch, S.L., Rasmussen, S.A., Machado, A.G., Kubu, C.S., Tyrka, A.R., Price, L.H., Stypulkowski, P.H., Giftakis, J.E., Rise, M.T., Malloy, P.F., Salloway, S.P., Greenberg, B.D.: Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Biol. Psychiatr. 65, 267–275 (2009)
Marcelli, G., Patel, B.A.: Understanding changes in uptake and release of serotonin from gastrointestinal tissue using a novel electroanalytical approach. Analyst 135(9), 2340–2347 (2010). doi:10.1039/c0an00260g
Marks, W.A., Honeycutt, J., Acosta Jr., F., Reed, M., Bailey, L., Pomykal, A., Mercer, M.: Dystonia due to cerebral palsy responds to deep brain stimulation of the globus pallidus internus. Mov. Disord. Off. J. Mov. Disord. Soc. 26(9), 1748–1751 (2011). doi:10.1002/mds.23723
Mayberg, H.S., Brannan, S.K., Tekell, J.L., Silva, J.A., Mahurin, R.K., McGinnis, S., Jerabek, P.A.: Regional metabolic effects of fluoxetine in major depression: serial changes and relationship to clinical response. Biol. Psychiatr. 48(8), 830–843 (2000)
Mayberg, H.S., Liotti, M., Brannan, S.K., McGinnis, S., Mahurin, R.K., Jerabek, P.A., Silva, J.A., Tekell, J.L., Martin, C.C., Lancaster, J.L., Fox, P.T.: Reciprocal limbic-cortical function and negative mood: converging PET findings in depression and normal sadness. Am. J. Psychiatr. 156(5), 675–682 (1999). doi:10.1176/ajp.156.5.675
Mayberg, H.S., Lozano, A.M., Voon, V., McNeely, H.E., Seminowicz, D., Hamani, C., Schwalb, J.M., Kennedy, S.H.: Deep brain stimulation for treatment-resistant depression. Neuron 45(5), 651–660 (2005). doi:10.1016/j.neuron.2005.02.014
McIntyre, C.C., Thakor, N.V.: Uncovering the mechanisms of deep brain stimulation for Parkinson’s disease through functional imaging, neural recording, and neural modeling. Crit. Rev. Biomed. Eng. 30(4–6), 249–281 (2002)
Merkl, A., Schneider, G.H., Schonecker, T., Aust, S., Kuhl, K.P., Kupsch, A., Kuhn, A.A., Bajbouj, M.: Antidepressant effects after short-term and chronic stimulation of the subgenual cingulate gyrus in treatment-resistant depression. Exp. Neurol. 249, 160–168 (2013). doi:10.1016/j.expneurol.2013.08.017
Neher, E., Sakmann, B., Steinbach, J.H.: The extracellular patch clamp: a method for resolving currents through individual open channels in biological membranes. Pflugers Arch. 375(2), 219–228 (1978)
Odekerken, V.J., van Laar, T., Staal, M.J., Mosch, A., Hoffmann, C.F., Nijssen, P.C., Beute, G.N., van Vugt, J.P., Lenders, M.W., Contarino, M.F., Mink, M.S., Bour, L.J., van den Munckhof, P., Schmand, B.A., de Haan, R.J., Schuurman, P.R., de Bie, R.M.: Subthalamic nucleus versus globus pallidus bilateral deep brain stimulation for advanced parkinson’s disease (NSTAPS study): a randomised controlled trial. Lancet Neurol. 12, 37–44 (2013)
Ogawa, S., Menon, R.S., Tank, D.W., Kim, S.G., Merkle, H., Ellermann, J.M., Ugurbil, K.: Functional brain mapping by blood oxygenation level-dependent contrast magnetic resonance imaging. A comparison of signal characteristics with a biophysical model. Biophys. J. 64(3), 803–812 (1993). doi:10.1016/S0006-3495(93)81441-3
Okun, M.S., Gallo, B.V., Mandybur, G., Jagid, J., Foote, K.D., Revilla, F.J., Alterman, R., Jankovic, J., Simpson, R., Junn, F., Verhagen, L., Arle, J.E., Ford, B., Goodman, R.R., Stewart, R.M., Horn, S., Baltuch, G.H., Kopell, B.H., Marshall, F., Peichel, D., Pahwa, R., Lyons, K.E., Tröster, A.I., Vitek, J.L., Tagliati, M.: Subthalamic deep brain stimulation with a constant-current device in Parkinson’s disease: an open-label randomised controlled trial. Lancet Neurol. 11, 140–149 (2012)
Olah, M.E., Stiles, G.L.: Adenosine receptor subtypes: characterization and therapeutic regulation. Ann. Rev. Pharmacol. Toxicol. 35, 581–606 (1995). doi:10.1146/annurev.pa.35.040195.003053
Ongur, D., An, X., Price, J.L.: Prefrontal cortical projections to the hypothalamus in macaque monkeys. J. Comp. Neurol. 401(4), 480–505 (1998)
Ostrem, J.L., Racine, C.A., Glass, G.A., Grace, J.K., Volz, M.M., Heath, S.L., Starr, P.A.: Subthalamic nucleus deep brain stimulation in primary cervical dystonia. Neurology 76, 870–878 (2011)
Paek, S.B., Min, H.K., Kim, I., Knight, E.J., Baek, J.J., Bieber, A.J., Lee, K.H., Chang, S.Y.: Frequency-dependent functional neuromodulatory effects on the motor network by ventral lateral thalamic deep brain stimulation in swine. NeuroImage 105, 181–188 (2015). doi:10.1016/j.neuroimage.2014.09.064
Park, J., Quaiserova-Mocko, V., Patel, B.A., Novotny, M., Liu, A., Bian, X., Galligan, J.J., Swain, G.M.: Diamond microelectrodes for in vitro electroanalytical measurements: current status and remaining challenges. Analyst 133(1), 17–24 (2008). doi:10.1039/b710236b
Pahwa, R., Lyons, K.E., Wilkinson, S.B., Simpson, R.K., Ondo, W.G., Tarsy, D., Norregaard, T., Hubble, J.P., Smith, D.A., Hauser, R.A., Jankovic, J.: Long-term evaluation of deep brain stimulation of the thalamus. J. Neurosurg. 104, 506–512 (2006)
Park, J., Show, Y., Quaiserova, V., Galligan, J.J., Fink, G.D., Swain, G.M.: Diamond microelectrodes for use in biological environments. J. Electroanal. Chem. 583(1), 56–68 (2005). doi:10.1016/j.jelechem.2005.04.032
Pereira, E.A., Green, A.L., Aziz, T.Z.: Deep brain stimulation for pain. In: Handbook of Clinical Neurology, vol. 116, pp. 277–294 (2013)
Perlmutter, J.S., Mink, J.W.: Deep brain stimulation. Annu. Rev. Neurosci. 29, 229–257 (2006). doi:10.1146/annurev.neuro.29.051605.112824
Perry, M., Li, Q., Kennedy, R.T.: Review of recent advances in analytical techniques for the determination of neurotransmitters. Anal. Chim. Acta 653(1), 1–22 (2009). doi:10.1016/j.aca.2009.08.038
Pienaar, I.S., Lee, C.H., Elson, J.L., McGuinness, L., Gentleman, S.M., Kalaria, R.N., Dexter, D.T.: Deep-brain stimulation associates with improved microvascular integrity in the subthalamic nucleus in Parkinson’s disease. Neurobiol. Dis. 74, 392–405 (2015). doi:10.1016/j.nbd.2014.12.006
Priori, A., Foffani, G., Rossi, L., Marceglia, S.: Adaptive deep brain stimulation (aDBS) controlled by local field potential oscillations. Exp. Neurol. 245, 77–86 (2013). doi:10.1016/j.expneurol.2012.09.013
Pulliam, C.L., Heldman, D.A., Orcutt, T.H., Mera, T.O., Giuffrida, J.P., Vitek, J.L.: Motion sensor strategies for automated optimization of deep brain stimulation in Parkinson’s disease. Parkinsonism Relat. Disord. 21(4), 378–382 (2015). doi:10.1016/j.parkreldis.2015.01.018. Epub 2015 Feb 11
Robinson, D.L., Venton, B.J., Heien, M.L., Wightman, R.M.: Detecting subsecond dopamine release with fast-scan cyclic voltammetry in vivo. Clin. Chem. 49(10), 1763–1773 (2003)
Roham, M., Halpern, J.M., Martin, H.B., Chiel, H.J., Mohseni, P.: Diamond microelectrodes and CMOS microelectronics for wireless transmission of fast-scan cyclic voltammetry. In: Conference Proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society IEEE Engineering in Medicine and Biology Society Conference 2007, pp. 6044–6047 (2007). doi:10.1109/IEMBS.2007.4353726
Rosen, B.R., Buckner, R.L., Dale, A.M.: Event-related functional MRI: past, present, and future. Proc. Natl. Acad. Sci. U.S.A. 95(3), 773–780 (1998)
Schlaepfer, T.E., Cohen, M.X., Frick, C., Kosel, M., Brodesser, D., Axmacher, N., Joe, A.Y., Kreft, M., Lenartz, D., Sturm, V.: Deep brain stimulation to reward circuitry alleviates anhedonia in refractory major depression. Neuropsycho-pharmacology 33, 368–377 (2008)
Sellal, F., Hirsch, E., Barth, P., Blond, S., Marescaux, C.: A case of symptomatic hemidystonia improved by ventroposterolateral thalamic electrostimulation. Mov. Disord. Off. J. Mov. Disord. Soc. 8(4), 515–518 (1993). doi:10.1002/mds.870080418
Singh, Y.S., Sawarynski, L.E., Michael, H.M., Ferrell, R.E., Murphey-Corb, M.A., Swain, G.M., Patel, B.A., Andrews, A.M.: Boron-doped diamond microelectrodes reveal reduced serotonin uptake rates in lymphocytes from adult rhesus monkeys carrying the short allele of the 5-HTTLPR. ACS Chem. Neurosci. 1(1), 49–64 (2010). doi:10.1021/cn900012y
Schüpbach, W.M., Maltête, D., Houeto, J.L., du Montcel, S.T., Mallet, L., Welter, M.L., Gargiulo, M., Béhar, C., Bonnet, A.M., Czernecki, V., Pidoux, B., Navarro, S., Dormont, D., Cornu, P., Agid, Y.: Neurosurgery at an earlier stage of parkinson disease: a randomized, controlled trial. Neurology 68, 267–271 (2007)
Suzuki, A., Ivandini, T.A., Yoshimi, K., Fujishima, A., Oyama, G., Nakazato, T., Hattori, N., Kitazawa, S., Einaga, Y.: Fabrication, characterization, and application of boron-doped diamond microelectrodes for in vivo dopamine detection. Anal. Chem. 79(22), 8608–8615 (2007). doi:10.1021/ac071519h
Swann, N.C., de Hemptinne, C., Miocinovic, S., Qasim, S., Wang, S.S., Ziman, N., Ostrem, J.L., San Luciano, M., Galifianakis, N.B., Starr, P.A.: Gamma oscillations in the hyperkinetic state detected with chronic human brain recordings in parkinson’s disease. J. Neurosci. 36(24), 6445–6458 (2016). doi:10.1523/JNEUROSCI.1128-16.2016
Sydow, O., Thobois, S., Alesch, F., Speelman, J.D.: Multicentre European study of thalamic stimulation in essential tremor: a six year follow up. J. Neurol. Neurosurg. Psychiatr. 74, 1387–1391 (2003)
Takmakov, P., Zachek, M.K., Keithley, R.B., Walsh, P.L., Donley, C., McCarty, G.S., Wightman, R.M.: Carbon microelectrodes with a renewable surface. Anal. Chem. 82(5), 2020–2028 (2010). doi:10.1021/ac902753x
Tekriwal, A., Baltuch, G.: deep brain stimulation: expanding applications. Neurol Med-Chir. 55(12), 861–877 (2015). doi:10.2176/nmc.ra.2015-0172
Temel, Y., Visser-Vandewalle, V.: Surgery in tourette syndrome. Mov. Disord. Off. J. Mov. Disord. Soc. 19(1), 3–14 (2004). doi:10.1002/mds.10649
Uludag, K., Dubowitz, D.J., Yoder, E.J., Restom, K., Liu, T.T., Buxton, R.B.: Coupling of cerebral blood flow and oxygen consumption during physiological activation and deactivation measured with fMRI. NeuroImage 23(1), 148–155 (2004). doi:10.1016/j.neuroimage.2004.05.013
Venton, B.J., Michael, D.J., Wightman, R.M.: Correlation of local changes in extracellular oxygen and pH that accompany dopaminergic terminal activity in the rat caudate-putamen. J. Neurochem. 84(2), 373–381 (2003)
Vidailhet, M., Yelnik, J., Lagrange, C., Fraix, V., Grabli, D., Thobois, S., Burbaud, P., Welter, M.L., Xie-Brustolin, J., Braga, M.C., Ardouin, C., Czernecki, V., Klinger, H., Chabardes, S., Seigneuret, E., Mertens, P., Cuny, E., Navarro, S., Cornu, P., Benabid, A.L., Le Bas, J.F., Dormont, D., Hermier, M., Dujardin, K., Blond, S., Krystkowiak, P., Destee, A., Bardinet, E., Agid, Y., Krack, P., Broussolle, E., Pollak, P., French, S.-S.G.: Bilateral pallidal deep brain stimulation for the treatment of patients with dystonia-choreoathetosis cerebral palsy: a prospective pilot study. Lancet Neurol. 8(8), 709–717 (2009). doi:10.1016/S1474-4422(09)70151-6
Visser-Vandewalle, V., Temel, Y., Boon, P., Vreeling, F., Colle, H., Hoogland, G., Groenewegen, H.J., van der Linden, C.: Chronic bilateral thalamic stimulation: a new therapeutic approach in intractable tourette syndrome—report of three cases. J. Neurosurg. 99(6), 1094–1100 (2003). doi:10.3171/Jns.2003.99.6.1094
Viswanathan, A., Jimenez-Shahed, J., Baizabal Carvallo, J.F., Jankovic, J.: Deep brain stimulation for tourette syndrome: target selection. Stereotact Funct. Neurosurg. 90, 213–224 (2012)
Walter, B.L., Vitek, J.L.: Surgical treatment for parkinson’s disease. Lancet Neurol. 3(12), 719–728 (2004). doi:10.1016/S1474-4422(04)00934-2
Weaver, F.M., Follett, K., Stern, M., Hur, K., Harris, C., Marks, W.J., Rothlind, J., Sagher, O., Reda, D., Moy, C.S., Pahwa, R., Burchiel, K., Hogarth, P., Lai, E.C., Duda, J.E., Holloway, K., Samii, A., Horn, S., Bronstein, J., Stoner, G., Heemskerk, J., Huang, G.D.: CSP 468 Study Group. Bilateral deep brain stimulation vs. best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. JAMA 301, 63–73 (2009)
Whiting, D.M., Tomycz, N.D., Bailes, J., de Jonge, L., Lecoultre, V., Wilent, B., Alcindor, D., Prostko, E.R., Cheng, B.C., Angle, C., Cantella, D., Whiting, B.B., Mizes, J.S., Finnis, K.W., Ravussin, E., Oh, M.Y.: Lateral hypothalamic area deep brain stimulation for refractory obesity: a pilot study with preliminary data on safety, body weight, and energy metabolism. J. Neurosurg. 119, 56–63 (2013)
Williams, A., Gill, S., Varma, T., Jenkinson, C., Quinn, N., Mitchell, R., Scott, R., Ives, N., Rick, C., Daniels, J., Patel, S., Wheatley, K.: PD SURG Collaborative Group. Deep brain stimulation plus best medical therapy versus best medical therapy alone for advanced Parkinson’s disease (PD SURG trial): a randomised, open-label trial. Lancet Neurol. 9, 581–591 (2010)
Xie, S.T., Shafer, G., Wilson, C.G., Martin, H.B.: In vitro adenosine detection with a diamond-based sensor. Diam. Relat. Mater. 15(2–3), 225–228 (2006). doi:10.1016/j.diamond.2005.08.018
Yamawaki, N., Magill, P.J., Woodhall, G.L., Hall, S.D., Stanford, I.M.: Frequency selectivity and dopamine-dependence of plasticity at glutamatergic synapses in the subthalamic nucleus. Neuroscience 203, 1–11 (2012). doi:10.1016/j.neuroscience.2011.12.027
Yoshimi, K., Naya, Y., Mitani, N., Kato, T., Inoue, M., Natori, S., Takahashi, T., Weitemier, A., Nishikawa, N., McHugh, T., Einaga, Y., Kitazawa, S.: Phasic reward responses in the monkey striatum as detected by voltammetry with diamond microelectrodes. Neurosci. Res. 71(1), 49–62 (2011). doi:10.1016/j.neures.2011.05.013
Zhang, K., Bhatia, S., Oh, M.Y., Cohen, D., Angle, C., Whiting, D.: Long-term results of thalamic deep brain stimulation for essential tremor. J. Neurosurg. 112, 1271–1276 (2010)
Zhao, H., Bian, X.C., Galligan, J.J., Swain, G.M.: Electrochemical measurements of serotonin (5-HT) release from the guinea pig mucosa using continuous amperometry with a boron-doped diamond microelectrode. Diam. Relat. Mater. 19(2–3), 182–185 (2010). doi:10.1016/j.diamond.2009.10.004
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
(Brian) Paek, S., Kale, R.P., Wininger, K.M., Lujan, J.L. (2017). Physiological Monitoring in Deep Brain Stimulation: Toward Closed-Loop Neuromodulation Therapies. In: Bhatti, A., Lee, K., Garmestani, H., Lim, C. (eds) Emerging Trends in Neuro Engineering and Neural Computation. Series in BioEngineering. Springer, Singapore. https://doi.org/10.1007/978-981-10-3957-7_4
Download citation
DOI: https://doi.org/10.1007/978-981-10-3957-7_4
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-3955-3
Online ISBN: 978-981-10-3957-7
eBook Packages: EngineeringEngineering (R0)