Abstract
The observation that the Runx genes act as targets for transcriptional activation by retroviral insertion identified a new family of dominant oncogenes. However, it is now clear that Runx genes are ‘conditional’ oncogenes whose over-expression is growth inhibitory unless accompanied by another event such as concomitant over-expression of MYC or loss of p53 function. Remarkably, while the oncogenic activities of either MYC or RUNX over-expression are suppressed while p53 is intact, the combination of both neutralises p53 tumour suppression in vivo by as yet unknown mechanisms. Moreover, there is emerging evidence that endogenous, basal RUNX activity is important to maintain the viability and proliferation of MYC-driven lymphoma cells. There is also growing evidence that the human RUNX genes play a similar conditional oncogenic role and are selected for over-expression in end-stage cancers of multiple types. Paradoxically, reduced RUNX activity can also predispose to cell immortalisation and transformation, particularly by mutant Ras. These apparently conflicting observations may be reconciled in a stage-specific model of RUNX involvement in cancer. A question that has yet to be fully addressed is the extent to which the three Runx genes are functionally redundant in cancer promotion and suppression.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 The Murine Runx Genes as Targets for Insertional Mutagenesis
The discovery that the murine Runx genes can act as targets for transcriptional activation by murine leukaemia viruses (MLVs) provided evidence that they belong to the class of proto-oncogenes: genes normally involved in growth control that can be activated to play a dominant oncogenic role in cancer. MLVs are members of the gamma-retrovirus genus and induce tumours in mice primarily by insertional mutagenesis. Strong promoter/enhancer sequences in the long terminal repeats of these viruses affect the expression of genes near, or even at a considerable distance from, the insertion site. MLV induced tumours may display multiple insertions at complementing oncogenes; gene activation events predominate although tumour suppressor inactivation can also occur (reviewed in (Uren et al. 2005)). Completion of the mouse genome sequence has greatly increased the ease of mapping retroviral insertions in tumours, greatly extending the reach of mutagenesis screens for cancer –relevant genes (Hwang et al. 2002; Mikkers et al. 2002; Suzuki et al. 2002). While the process of retroviral integration into the host genome was previously thought to be random with regard to base sequence and location, it is now clear that some retroviruses display very significant and distinct biases. For MLV and related gamma-retroviruses, intrinsic integration preference arises at least in part from interaction of the viral integrase protein with the BET (bromodomain and extraterminal) host chromatin tethering factors Brd2,3 and 4 (De Rijck et al. 2013; Gupta et al. 2013; Sharma et al. 2013). This specificity is of interest with regard to oncogenic potential as BET binding is also a feature of ‘super-enhancers’ – highly cell-type specific tandem clusters of enhancer elements that appear to define cell identity and the cancer phenotype (Whyte et al. 2013). This intrinsic bias has to be allowed for, particularly when analysing and interpreting high throughput datasets (Cattoglio et al. 2010; LaFave et al. 2014). These findings led us to propose a two-stage model of gamma-retrovirus oncogenesis: selective integration at ‘dangerous’ sites, followed by clonal selection of collaborating mutations (Huser et al. 2014).
The first recorded example of Runx gene targeting by MLV arose from an early screen where a single case of Akv MLV insertion was recorded close to the P1 promoter of Runx1 in a case of myeloid leukaemia in a BXH2 mouse (Suzuki et al. 2002). This appears to have been a fortuitous observation, as subsequent studies have shown a relatively low frequency of targeting of the Runx genes in end-stage tumours of wild-type mice. However, frequent activation of Runx genes has been observed in mice where predisposition to tumour development is conferred, for example, by a germ-line MYC oncogene over-expressed under tissue-specific transcriptional controls. While all three Runx genes have been shown to be capable of acting as targets in MYC transgenic mice, the frequency varies according to model. Runx1 and Runx3 are targeted in B-cell lymphomas accelerated by neonatal infection with Moloney MLV in the Eμ-Myc model (Mikkers et al. 2002; Uren et al. 2008). All three Runx genes have been observed as targets in virus-accelerated T-cell lymphomas of CD2-MYC but with frequency of targeting Runx2>Runx3>Runx1 (Mikkers et al. 2002; Stewart et al. 2002; Stewart et al. 1997; Wotton et al. 2002). Moreover, a recent high throughput/NGS study confirmed the relative rarity of Runx gene insertions in clonally expanded cell populations in wild-type mice, and indicated that, in contrast, activation of a Runx family member is virtually obligatory in virus-accelerated CD2-MYC lymphomas (Huser et al. 2014).
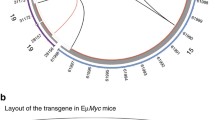
A diagram summarising the location and orientation of recorded proviral insertions at the murine Runx genes is presented in Fig. 16.1. We have included only those examples where significant clonal expansion has provided corroborating evidence that these insertions played a causal role in tumour outgrowth. A track showing H3K27Ac ‘enhancer’ marks in mouse thymus is included for comparison. While there is substantial correspondence between H3K27Ac marks and the peaks of insertion, this overlap is not seen at the Runx2 P1 promoter. However, it should be noted that available ChIP-Seq datasets may not reflect the target cell at the stage of development when retroviral integration occurred.
In vivo clonally expanded insertions of MLV and transposons at the Runx gene loci in murine tumours. The results of multiple studies have been collated. The top of each track shows gene structure, with solid vertical bars representing exons and lines representing introns, with arrows showing transcriptional start sites. Proviral insertions in the forward direction are coloured green while those in the reverse direction are coloured red. Sources of data for tracks (a–d) are as follows: (a) CD2-MYC transgenic T-cell lymphomas analysed by high throughput/NGS analysis (read number >100) (Huser et al. 2014). (b) CD2-MYC transgenic T-cell lymphomas from restriction mapping and direct sequence analyses (Cameron et al. 2003; Stewart et al. 2007; Wotton et al. 2002) (c) Common insertion sites from the retroviral tagged cancer gene database (ref) (d) Sleeping beauty transposon insertions in leukaemia/lymphomas from Rassf1a deficient mice (van der Weyden et al. 2012). Insertions with more than 100 copies are shown. The bottom of each track shows H3K27ac intensity in adult mouse thymus, obtained from the mouse ENCODE repository
In the CD2-MYC system it is clear that MLV induces transcriptional activation of Runx family genes, as cell lines established from these lymphomas show very high level expression of the targeted gene with no mutational changes in coding sequence (Stewart et al. 2002; Stewart et al. 1997; Wotton et al. 2002). Moreover, the strong statistical bias of proviral orientation where insertions have been observed at the Runx2 P1 promoter fits with the ‘enhancer mode’ of retroviral insertion, where the viral long terminal repeat is upstream and backwards with regard to the targeted promoter (Huser et al. 2014). Expanded clonal insertions far upstream of Runx2 in CD2-MYC lymphomas suggest that regulation of this gene in early T-cell development also involves distant cis-acting enhancer elements that serve as targets for long-range activation by retroviral insertions (Huser et al. 2014).
The pattern is somewhat less clear for Runx1. In the 6i lymphoma cell line derived from CD2-MYC lymphoma, MLV insertion is in the ‘promoter insertion’ mode and the result has been established as over-expression of the P1 isoform of RUNX1 (Wotton et al. 2002). Other examples from the RTCGD (retroviral tagged cancer gene database; http://variation.osu.edu/rtcgd/index.html) show insertions between the P1 and P2 promoters mainly in the opposite orientation to the gene, and the consequences for activation of either promoter have not been investigated.
In the case of Runx3, insertions appear to cluster at an upstream ‘super-enhancer.’ In the 1i CD2-MYC lymphoma cell line MLV insertion at this site is in the upstream and backwards mode and is associated with over-expression of the P1 isoform of RUNX3 (Stewart et al. 2002) and a similar location and orientation is evident in other lymphomas from the CD2-MYC series (Fig. 16.1). While other RTCGD database examples are less clearly biased in orientation, multiple insertions were reported at the homologue of this site in MLV-induced lymphomas in the rat. This site was originally designated Dsi1 before the discovery of the Runx genes, and it was noted that all insertions were in the same orientation, which we can now read as upstream and backwards with respect to Runx3. Notably, in the index case from which Dsi1 was cloned, there was also a proviral insertion at rat c-Myc (Vijaya et al. 1987). The Runx3 gene was also identified as a target for MLV insertion in two independent transplanted B-ALLs in a mouse model of BCR-ABL under selection for imatinib resistance. In this system over-expression of either RUNX3 or RUNX1 was shown to diminish imatinib-induced apoptosis (Miething et al. 2007).
The Runx2 gene has also been reported as a target for retroviral insertional mutagenesis in myeloid leukaemias of Cbfb-MYH11 (Inv16) mice where it was initially considered a candidate tumour suppressor on the basis that the insertions were intragenic and potentially disruptive (Castilla et al. 2004). However, further study revealed that reduced dosage of Runx2 suppressed disease in this model, while ectopic expression of full-length Runx2 cooperated with Cbfb-MYH11 in transplantation assays (Kuo et al. 2009), suggesting that the intragenic insertions may have been activating events. This conclusion appears to conflict with a recent report of intragenic Runx2 insertions of the transposon Sleeping Beauty in leukaemias/lymphomas of Rassfs1a −/− mice which were also interpreted as inactivating events (van der Weyden et al. 2012). However, in view of the location and orientation of these insertions in Runx2 (Fig. 16.1) and the lack of corroborating evidence that the gene is up-regulated by these insertions, it is difficult to judge which interpretation is correct. As discussed later (Fig. 16.6), other lines of evidence suggest that both may have credence, if reduced Runx expression is favoured in the early tumour development while high expression drives later stages.
2 The Human RUNX Genes Act as Frequent Targets for Retroviral Vector Insertion in CD34+ Cells
The development of vector-induced leukaemias in gene therapy trials (Hacein-Bey-Abina et al. 2008; Howe et al. 2008) demonstrated the mutagenic potential of murine gamma-retroviruses in human subjects and focused attention on the factors affecting this adverse event (Scobie et al. 2009). High throughput studies of MLV vector integration in human CD34+ cells revealed pronounced hot-spots or hyper-clusters, including the LMO2 gene that was the most frequently activated target in gene therapy-related leukaemias (Cattoglio et al. 2010). The selective targeting of MLV integration to regions of active chromatin marked by acetylated histones due to direct interaction of the viral integrase protein with Brd/BET chromatin tethers sheds light on these observations (Gupta et al. 2013; Sharma et al. 2013). As shown in Fig. 16.2, the human RUNX genes also serve as preferential targets for integration in CD34+ and K562 cells in vitro, with a distribution that mirrors H3K27Ac chromatin marks. There is an evident difference between the targeted sites for each RUNX gene. For RUNX3, the upstream ‘super-enhancer’ is most frequently targeted, while most insertions in RUNX1 and RUNX2 are intragenic. The lack of orientation bias of these insertions is consistent with the interpretation that the clustered pattern results from preferential integration and that no significant post-integration clonal selection has occurred during the limited culture period prior to harvesting for analysis (Huser et al. 2014).
Insertions at the RUNX gene loci in human haematopoietic cells transduced with MLV vector or infected with MLV/VSV pseudotypes. The top of each track shows gene structure, with solid vertical bars representing exons and lines representing introns, with arrows showing transcriptional start sites. Insertions in the forward direction are coloured green while those in the reverse direction are coloured red. Tracks (a–b) represent datasets: (a) MLV vector insertions in CD34+ cells (Cattoglio et al. 2010). (b) MLV Insertions in K562 cells (LaFave et al. 2014). The bottom of each track shows H3K27ac intensity in CD34+ primary cells, obtained from the human Epigenetics Roadmap
The frequent targeting of all three RUNX genes by retroviral vectors in CD34+ cells is also consistent with the fact that they are all transcriptionally active in early haematopoiesis, including RUNX2, providing a parallel with the targeting of Runx2 by retroviral insertion in the Inv16 leukaemia model (Castilla et al. 2004). Moreover, the sites of preferred integration overlap to some extent with those selected in clonal end-stage murine lymphomas induced by MLV (Fig. 16.1). Despite these common features, end-stage patient leukaemias have not yet revealed the RUNX genes as targets, nor have the RUNX genes emerged from monitoring of insertion sites in the blood of healthy trial subjects (Hacein-Bey-Abina et al. 2008; Schwarzwaelder et al. 2007). This is perhaps not surprising in light of the requirement for activation of MYC or loss of p53 to facilitate the oncogenic effects of RUNX over-expression in murine models.
3 Switching the Runx Genes from Growth Suppressors to Oncogenes In Vivo: The Roles of MYC and p53
The potent synergy between RUNX2 and MYC in transgenic mice over-expressing both genes in the T-cell compartment (CD2-MYC/CD2-Runx2 mice) confirmed the dominant oncogenic potential of RUNX2 (Vaillant et al. 1999). While the generality of the MYC/RUNX synergy was later confirmed by synergistic induction of B-cell lymphomas in vav-Runx1/Eμ-Myc mice (Blyth et al. 2009), most studies to date have been conducted with the CD2-Runx2 model. Under the control of the CD2 LCR, RUNX2 was shown to accelerate lymphoma development in Eμ-Pim1 and CD2-v-Myb transgenic mice as well as in p53null mice (Blyth et al. 2001; Cameron et al. 2003), indicating a non-redundant, unique role for RUNX in tumour development. However, the selective targeting of c-Myc and N-Myc in virus-accelerated tumours of CD2-Runx2 mice was a further indication of a special relationship between RUNX and MYC oncogenic functions (Blyth et al. 2001).
An unusual feature of the CD2-MYC model is the undetectable expression of the CD2-MYC transgene in the majority of mice that remain healthy (Stewart et al. 1993). To account for this phenotype it has been suggested that variegated expression of the hCD2 locus in early lymphoid development (Williams et al. 2008) leads to MYC-induced apoptosis in expressing cells and that compensatory expansion of transgene non-expressing cells leads to replenishment and generation of an apparently normal lymphoid compartment (Blyth et al. 2006). It seems likely that the potent oncogenicity of the CD2-MYC/CD2-Runx2 combination is at least partially explained by the simultaneous activation of both oncogenes at the same stage of early lymphoid development. Similarly, the efficiency of virus acceleration in CD2-MYC mice may be explained by the activation of collaborating genes by viral infection and integration in lymphoid progenitor cells that have yet to activate the CD2-MYC transgene (Stewart et al. 1993). The remarkably low apoptotic index of spontaneous CD2-Runx2 lymphomas and reduced apoptosis in compound transgenics compared to CD2-MYC alone in this setting indicates that the major selective advantage of RUNX2 in this context is survival and ablation of MYC-induced apoptosis (Blyth et al. 2006).
In the CD2-Runx2 model, where RUNX2 expression is initiated in early lymphoid development, there is a gene dose-dependent predisposition to thymic lymphoma development (Vaillant et al. 1999). However, analysis of thymic development in the transgenic mice revealed a marked deficit in fetal thymocyte numbers rather than a preneoplastic expansion, indicating that the initial response to ectopic RUNX2 expression is growth suppressive. Moreover, analysis of the immature CD8+ subset (CD8ISP) which was expanded in these mice showed that these were small cells with a markedly lower proliferation rate than CD8ISP from healthy mice (Vaillant et al. 2002). A similar though less marked phenotype was observed in vav-Runx1 mice which displayed reduced proliferation in haematopoietic stem/progenitor cells and B-cells, although with enhanced survival (Blyth et al. 2009). The ability of MYC to counteract the growth suppressive potential of ectopic RUNX expression is evident from the rapid onset of tumours in vav-Runx1/EμMyc and in CD2-Runx2/CD2-MYC, where the CD8ISP population observed in CD2-Runx2 mice is transformed to large blastic cells in the premalignant thymus (Blyth et al. 2009; Blyth et al. 2006; Vaillant et al. 1999). The rapid onset of lymphomas in CD2-Runx2/p53null mice shows that loss of the p53 pathway can also synergise with ectopic Runx expression (Blyth et al. 2001). A diagram summarising the collaboration of Myc and Runx genes in the context of T-cell lymphomas under the influence of CD2 LCR-driven gene expression is summarised in Fig. 16.3.
Model of RUNX/MYC collaboration in lymphomagenesis. See text for explanation and supporting references. Panel A shows the key features of premalignant phenotype and disease in CD2-MYC, CD2-Runx2 and compound transgenic mice. Panel B shows the interaction between RUNX2, MYC and p53 in the early T-cell compartment. Both CD2-Runx2 and CD2-MYC transgenes are independently synergistic with germ-line inactivation of p53, suggesting that the oncogenic activity of both genes is antagonised by the tumour suppressor function of p53, while the combination of both oncogenes appears to overcome p53. We hypothesise that this phenomenon entails co-activation one or more genes that neutralises p53 function in T-lymphoma cells. CLP: common lymphoid progenitor
4 Over-Expression of RUNX and MYC Combine to Disarm the p53 Response In Vivo: A Dual Signal Hypothesis
While MYC and Runx transgenes are potently synergistic in lymphomagenesis, they also collaborate independently with germline inactivation of p53 (Blyth et al. 1995; Hsu et al. 1995). In accord with this observation, both MYC and RUNX induce p53 responses when ectopically expressed (Wolyniec et al. 2009; Zindy et al. 1998). Remarkably, the combination of transgenic MYC and RUNX2 appears to neutralise p53 activation, abolishing the selection to lose the wild-type Trp53 allele in primary and transplanted lymphomas on a CD2-MYC/ Runx2/ Trp53+/− background. The fact that the wild-type allele is rapidly lost on in vitro establishment of cell lines argues that it was intact but not active in the primary lymphomas (Blyth et al. 2006). These observations suggest that, in vivo, RUNX expression modifies the effects of MYC on the p53 pathway and vice versa. While the underlying mechanism has yet to be uncovered (Fig. 16.3b), it is notable that other oncogenes identified as potent MYC collaborators in retroviral mutagenesis screens impinge on the p53 pathway, including Bmi1, a repressor of Ink4a/Arf (Jacobs et al. 1999), and Gfi1, an indirect regulator of p53 activity via LSD1 mediated demethylation (Khandanpour and Moroy 2013).
Induction of MYC expression in primary fibroblasts leads to apoptosis unless pre-empted by a ‘dual signal’ provided by survival factors (Harrington et al. 1994) or relieved by inactivation of p53 (Hermeking and Eick 1994). It is interesting to compare this phenomenon to dual signalling hypotheses that evolved to account for shaping of the T-cell repertoire by positive and negative selection, and the proliferation of T-cells in response to foreign antigens (Zinkernagel et al. 1978). Notably, MYC expression enhances positive selection of thymocytes with functional T-cell receptors (Rudolph et al. 2000), while early studies showed that ectopic expression of RUNX1 could block TCR-signalling induced apoptosis of T-cell hybridomas (Fujii et al. 1998). It is tempting to suggest that the extremely potent synergy between Runx and Myc genes in driving lymphoma development is not merely a disordered response in the context of cancer, but an inherent feature of a signalling network that normally licenses lymphoid cells to proliferate in response to exogenous signals. The occurrence of autoimmune disease and hypersensitivity in Runx-deficient mice also provides indirect support for this hypothesis (Brenner et al. 2004; de Bruijn and Speck 2004; Wong et al. 2012).
5 Lymphoma Progression: Identification of Third Hit Genes in MYC/Runx2 Lymphomas
Analysis of rapid onset tumours arising in CD2-MYC/CD2-Runx2 transgenic mice showed that these are clonal outgrowths as indicated by their unique patterns of T-cell receptor rearrangement (Vaillant et al. 1999). This observation suggested that a further selective step is required to drive the end-stage lymphomas and led us to conduct further retroviral mutagenesis screens to identify the key target genes. Neonatal infection of CD2-MYC/CD2-Runx2 mice with Moloney MLV leads to even more rapid tumour onset, increased clonal complexity and increased dissemination of primary thymic lymphomas to peripheral lymphoid tissues (Stewart et al. 2007). As outlined in Table 16.1, analysis of the preferred RIM targets in the progressing lymphomas showed a strong bias towards G1 checkpoint genes (D cyclins) and other genes that overcome the requirement for exogenous growth factor signals (e.g. Pim kinases). A further deep profiling analysis of many thousands of insertion sites in these tumours (Huser et al. 2014) confirmed these core progression genes as part of a broader set enriched for T-cell receptor, PI3K and JAK-STAT pathways along with selected chemokine receptors involved in T-cell homing to thymus (Ccr7, Ccr9). Most of these genes were frequently targeted in tumours of wild type mice suggesting that this gene set is frequently recruited in the normal course of viral infection where unscheduled proliferation of the target cell provides a selective advantage. While the consequence in otherwise normal cells might be self-limiting proliferation, activation of these genes in a lymphoma stem cell transformed by MYC and RUNX over-expression is sustained proliferation in the absence of exogenous signals (Huser et al. 2014).
Potential parallels with this ‘three-hit’ model are emerging from recent studies on human cancer where a recent review highlighted evidence for RUNX2 synergy with PI3K/AKT signalling in multiple cancer types (Cohen-Solal et al. 2015). Moreover, it may be interesting to re-evaluate evidence for similar oncogene combinations that may have been overlooked e.g. in osteosarcomas where RUNX2 and CCND3 on chromosome 6p21 are frequently co-amplified and over-expressed (Lu et al. 2008) and MYC is also frequently over-expressed (Gamberi et al. 1998).
6 Evidence of RUNX Addiction in Lymphoma Development
Evidence that endogenous RUNX activity is important for lymphoma development was provided by the delayed onset of T-cell lymphomas in Runx1 +/− mice, whether these are induced by Moloney MLV infection or by the potent CD2-MYC/CD2-Runx2 combination. Moreover, the lack of evidence of loss of heterozygosity in these lymphomas argued strongly that the Runx1 gene was acting to promote tumour development rather than as a tumour suppressor (Wotton et al. 2002). Even more strikingly, the frequently occurring T-cell lymphomas in Trp53 null mice are virtually abolished on a Runx1 +/− background (Shimizu et al. 2013). While these observations suggested an important pro-oncogenic role for basal RUNX1 expression, it could not be excluded that the gene plays an essential role in T-cell development and influences lymphomagenesis only indirectly by controlling the size of the target cell population.
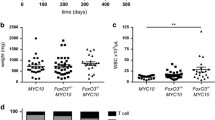
A recent study in Eμ-Myc/Runx1cKO mice has provided direct evidence of addiction to RUNX1 in primary lymphoma cells which, in contrast to normal splenic lymphocytes, resist even mono-allelic deletion in vivo. While established lymphoma cell lines that have lost p53 function become permissive for complete loss of Runx1, the Runx1 null cells display a proliferative disadvantage and become markedly more sensitive to chemotherapeutics including doxorubicin and dexamethasone (Borland et al. 2016). These findings validate the Runx genes and their downstream effectors as targets for lymphoma therapies. Another notable feature of this study is that the transcriptional signature conferred by deletion of Runx1 in these cells is enriched for genes involved in B-cell survival, proliferation and differentiation but does not include the ‘ribosomal biogenesis’ signature seen in Runx1 null haematopoietic progenitors (Cai et al. 2015) or the mitotic checkpoint signature observed in human AML cells after RUNX1 knockdown (Ben-Ami et al. 2013). While these findings again emphasise the cell context-dependent roles of RUNX, it should be noted that there are other players that may influence the outcome of loss of RUNX expression. In Eμ-Myc lymphomas, the cells over-express MYC, a major driver of ribosome biogenesis that may be able to rescue loss of RUNX1 expression (Borland et al. 2016), while Kasumi AML cells express RUNX1-ETO, a potential antagonist of RUNX-dependent gene expression (Ben-Ami et al. 2013).
7 RUNX, p53 and Senescence: Insights from Primary Cells
Primary fibroblasts have provided many useful insights into the activities of cancer-relevant genes in the absence of the many genetic and epigenetic changes that affect the responses of established cancer cell lines (Etzold et al. 2016; Serrano et al. 1997). In primary murine embryonic fibroblasts (Fig. 16.4) or human foreskin fibroblasts (Hs68), ectopic expression of any of the three Runx genes (P1 or P2 isoforms) leads to senescence-like growth arrest (SLGA) (Kilbey et al. 2007; Wotton et al. 2004). Unlike cells undergoing Ras-induced SLGA which develops as a response to unscheduled proliferation and DNA damage (Di Micco et al. 2006), cells with enforced RUNX expression do not display nuclear DNA damage foci, and have a phenotype that instead resembles the effects of ectopic p53 expression. The requirements for induction of this failsafe response are not fully understood, but appear to engage both p53 and p16 (Cdkn2a) pathways. In primary MEFs lacking p53, the effect of ectopic RUNX1 is not growth arrest, but over-proliferation at confluence and increased tumorigenicity in nude mice (Wotton et al. 2004). In NIH3T3 cells, which have an abnormal p53 pathway response and lack p16 expression due to a large genomic deletion encompassing Cdkn2a/Cdkn2b (Wotton et al. 2004), the effect of ectopic RUNX expression is to promote an epitheloid morphology resembling mesenchymal to epithelial transition, and markedly enhanced survival under stress conditions (Wotton et al. 2008). This survival phenotype is associated with direct RUNX modulation of multiple enzymes involved in sphingolipid metabolism (Sgpp1, Ucgc, St3gal5), shifting the ‘rheostat’ from pro-apoptotic ceramides to pro-survival sphingosine-1-phospate (Kilbey et al. 2010). In human Hs68 cells, RUNX1 expression induces p53 despite the absence of detectable p14ARF expression, while the induction of SLGA is blocked by HPV E6. Moreover, Leiden fibroblasts (CDKN2A mutant) are resistant to RUNX1-induced SLGA (Wolyniec et al. 2009).
Contrasting effects of ectopic RUNX expression in wild-type and established mouse fibroblasts. In primary mouse embryonic fibroblasts, RUNX over-expression leads to a profound growth arrest with flattened morphology and accumulation of senescence-associated β-galactosidase. In p53 deficient MEFs or NIH3T3 cells, ectopic RUNX expression leads instead to a morphological change resembling mesenchymal to epithelial transition along with enhanced growth and/or survival (Kilbey et al. 2007; Wotton et al. 2008, 2004)
The strongly growth suppressive effect of RUNX over-expression in normal cells provides an important caveat to the interpretation of cancer cell inhibition by ectopic RUNX as evidence of a tumour suppressor function. This problem potentially compromises many publications on the RUNX genes and their putative roles in human cancer where in general only established cell lines are available for study. Moreover, the fact that the RUNX1-ETO fusion oncoprotein is also a potent inducer of senescence-like growth arrest in fibroblasts (Wolyniec et al. 2009) argues against a yin-yang interpretation of its functional relationship to RUNX1 mediated by regulation of p14/p19ARF (Linggi et al. 2002).
8 Translational Relevance: RUNX Genes as Dominant Oncogenes in Human Cancer
The relative rarity of copy number gains affecting the RUNX genes in human cancer and the widespread assumption that they are predominantly tumour suppressors has until recently diverted attention from their capacity to act as dominant oncogenes. Amplification of a large domain of chromosome 21 that encompasses RUNX1 has been observed in a poor prognostic subset of B-ALL, presenting an exception to this rule (Harrison et al. 2014). Although it has been argued that these leukaemias do not significantly over-express RUNX1 mRNA compared to ALLs lacking RUNX1 amplification (Strefford et al. 2006) it is conceivable that other leukaemias over-express RUNX1 by different mechanisms, as RUNX1 mRNA is highly elevated in many ALLs (Niini et al. 2002). Notably, gains of chromosome 21 and RUNX1 copies are also evident in progressing t(12;21) leukaemias that express the TEL-RUNX1 fusion oncoprotein, in contrast to the frequent loss of the normal, non-translocated TEL allele (Lilljebjorn et al. 2010). The requirement for activity of the RUNX1 protein expressed from the untranslocated RUNX1 allele for survival and proliferation of leukaemia cell lines harbouring RUNX1 fusion oncoproteins (Ben-Ami et al. 2013; Zaliova et al. 2011) also argues against a simple tumour suppressor role /dominant negative inhibitor relationship. It should also be noted that there are many ways in which RUNX expression can be dysregulated, including post-translational modification and translational controls via miRNA. Examples of RUNX oncogenic activity apparently mediated by such mechanisms have emerged from recent studies on human cancer cells of multiple types (Bledsoe et al. 2014; Browne et al. 2016; Shin et al. 2016).
9 The Runx Genes as Tumour Suppressors in Haematopoietic Cancers: Evidence from Mouse Models
The severe development defects resulting from germ-line deletion of the Runx genes has delayed assessment of their tumour suppressor activity in vivo, requiring the development of conditional knockout strains. As reviewed recently (Chin et al. 2015), conditional knockouts of Runx1, Runx3 or Cbfb have revealed mainly myeloproliferative or myelodysplastic disease and/or haematopoietic stem cell expansions of varying degree. Deletion of Runx1 in HSPC mediated by vav-Cre was shown to lead to reduced cell size as a result of diminished ribosome biogenesis, along with reduced apoptosis and resistance to genotoxic and ER stress, and it was suggested that this phenotype provides a selective advantage for null cells (Cai et al. 2015). Dual deletion of Runx1 and Runx3 using the Mx1-Cre system resulted mainly in bone marrow failure although this was preceded by expansion of haematopoietic stem/progenitor cells (HSPC) and almost 20 % of the mice developed fatal myeloproliferative disorder (Wang et al. 2014). While there are few reports of the development of spontaneous malignant disease in knockouts (Chin et al. 2015), Runx1 inactivation collaborates strongly with other oncogenic insults such as FLT3-ITD or N-Ras to induce AML-like disease (Mead et al. 2013; Motoda et al. 2007). The predisposition towards MDS/AML rather than other malignancies in familial platelet disorder due to RUNX1 mutation (Owen et al. 2008) suggests that the unique sensitivity of the myeloid lineage to RUNX1 mutation and loss of function is conserved from mouse to human.
However, RUNX1 mutations have also been found in some human lymphoid malignancies, notably in early T-ALLs (18 %) and a small subset of B-ALL also carrying BCR-ABL (Grossmann et al. 2011). Moreover, on the basis of a systems biology approach dubbed ‘reverse engineering’ of transcription networks, RUNX1 was predicted to act as a tumour suppressor in this lineage (Della Gatta et al. 2012). Evidence from mouse models in support of this designation is rather limited although one study of Mx1-Cre mediated deletion of Runx1 reported thymic lymphoma in a proportion of Runx1KO mice. However, the major phenotype observed in these mice was myelodysplasia and a block in T-cell development and it is unclear from the report whether the lymphomas actually arose from Runx1 null cells (Putz et al. 2006). Another early study in chimeric mice showed that Runx1KO cells were preferentially targeted in T-cell lymphomas induced by chemical mutagenesis (Kundu et al. 2005). As highlighted earlier, reduction to a single functional allele in Runx1 +/− slows onset of MLV-induced T-cell lymphomas (Wotton et al. 2002) and virtually ablates spontaneous T-cell lymphomas in p53-deficient mice (Shimizu et al. 2013), arguing for a pro-oncogenic role. Moreover, a recent study has provided evidence that primary B-cell lymphomas in the Eμ-Myc model are addicted to RUNX1, while established cell lines lacking p53 become permissive to Cre-mediated deletion and display Rag gene de-repression, providing a potential explanation for the apparent oncogene/tumour suppressor paradox in the lymphoid compartment (Borland et al. 2016).
10 RUNX2 and Oncogene-Induced Senescence: A Temporal Model for RUNX Function in Cancer
Murine primary embryonic fibroblasts and osteoblasts lacking RUNX2 are prone to spontaneous immortalisation and tumorigenic conversion (Kilbey et al. 2007; Zaidi et al. 2007). Both cell types display reduced basal expression of a number of negative regulators of cell cycle progression that have been implicated as effectors of oncogene-induced failsafe responses (p16Ink4a, p19Ink4a, p53 and p21Waf1). These observations provide a rationale for the failure of primary fibroblasts and osteoblasts to undergo early growth arrest in the oxidative conditions of cell culture (Parrinello et al. 2003) and suggest a non-redundant role for RUNX2, which is perhaps not surprising as RUNX2 is the predominant expressed family member in both cell types. Runx2 null MEFs also resist H-Ras oncogene-induced senescence and become tumorigenic (Kilbey et al. 2007). However, despite their failure to arrest in response to mutant H-Ras, failsafe effectors are induced in Runx2 null fibroblasts at levels comparable to wild-type cells. The basis of their continued proliferation in the presence of failsafe effector expression is not fully understood, but is associated with altered expression of chromatin remodelling factors that regulate cyclin gene expression (Kilbey et al. 2008). It has also been reported that loss of Runx1 impairs N-Ras-induced failsafe responses in haematopoietic progenitors (Motoda et al. 2007), while Runx3cKO mice show accelerated lung tumour development in a K-Ras knock-in model (Lee et al. 2013) suggesting that this may be a wider feature of Runx oncogenesis (Fig. 16.5).
Runx2 null mouse fibroblasts are prone to spontaneous immortalisation and resist Ras-induced senescence. RUNX2 deficient primary embryonic fibroblasts express low levels of markers of aging and failsafe senescence (p16/p19Cdkn2a, p53, p21Cdkn1a), resist early growth arrest in normoxic culture and have an increased propensity for spontaneous immortalisation after 3T3 passage. Introduction of HRasV12 results in senescence-like growth arrest with nuclear DNA damage foci (green) in wild-type MEFs while Runx2 null cells proliferate and become tumorigenic, despite apparent induction of failsafe mediators (Kilbey et al. 2007)
However, at this point knockout mouse models have supported a pro-oncogenic rather than a suppressor role for RUNX2 in vivo (Ferrari et al. 2015) as have many recent studies of human cancer. A rare co-occurrence of cleido-cranial dysplasia and AML suggested a possible loss-of-function scenario but instead the authors of that study found that RUNX2 was actually over-expressed, a phenomenon they suggested might be explained by compensatory up-regulation of the wild-type allele (Schnerch et al. 2014). As the RUNX genes can cross-regulate (Brady et al. 2009) it should also be kept in mind that functional loss of one family member may have consequences for other members, and that the point mutations of RUNX1 in AML and a handful of other cancers may affect more than merely RUNX1. These observations also invite us to propose a temporal model to explain the dualistic behaviour of the Runx genes in cancer. We hypothesise that reduced levels of RUNX expression may act early to promote cancer development in a number of ways; by facilitating the growth of cells carrying initiator mutations (including mutant Ras alleles), preventing exit from stem cell/progenitor compartments, promoting genomic instability, impairing DNA repair and finally by de-repressing potentially mutagenic Rag genes. In contrast, in the later stages of cancer where Myc drives proliferation and the p53 pathway is compromised, Runx gene activity drives tumour cell growth and metastatic potential. This temporal model is also compatible with the apparent addiction of AML cells with RUNX1-ETO to expression of the wild-type allele of RUNX1 (Ben-Ami et al. 2013) and the copy number gains of the unaffected RUNX1 allele in progressing TEL-RUNX1 leukaemias (Lilljebjorn et al. 2012) (Fig. 16.6).
A temporal model for RUNX function in cancer. In this model, RUNX expression is required for tumour suppressive cell fate decisions and protection against mutational damage in early tumorigenesis where compromised expression increases the probability of transformation. At later stages, over-expression of MYC and/or loss of p53 function unmask the latent oncogenic potential of RUNX and increased expression is selected in end-stage tumours
11 The RUNX Genes: Isoforms or Functionally Divergent Genes?
For historical reasons, the field has focused heavily on RUNX1 in haemato-oncology, RUNX2 in bone development, and RUNX3 in immune cell function and tumour suppression. However, given the evidence of functional overlap as well as cross-regulation between family members (Spender et al. 2005) maintaining a singular focus on one family member while ignoring its relatives appears myopic. The fact that only RUNX1 has emerged as a common target for chromosomal translocation events in human leukaemia appears suggestive of a unique function for this family member. However, it should be noted that this bias could arise instead due to the relatively high expression of RUNX1 in haematopoietic progenitors where initiating events occur and/or to specific features of the RUNX1 locus on chromosome 21 that confer susceptibility to rearrangement (Levanon et al. 2001).
Despite their unique roles in specific biological niches, indications of functional overlap between family members can be seen in the T-cell lineage where RUNX1 and RUNX3 act sequentially to silence CD4 (Taniuchi et al. 2002) and in bone where both RUNX1 and RUNX3 are required in addition to the bone ‘master regulator’ RUNX2 for full osteoblast function and skeletal development (Bauer et al. 2015; Liakhovitskaia et al. 2010). These observations prompt the question of redundancy and whether the products of all Runx genes should be regarded as isoforms that play unique roles in development only because of their tissue-specific expression patterns. An analogy may be drawn from the Myc gene family where the entire N-Myc coding sequence can replace c-Myc in murine development despite their significant sequence divergence (Malynn et al. 2000). While this type of experiment has not been fully recapitulated for the Runx family, substitution of the C-terminus of RUNX1 with equivalent domains of RUNX2 and RUNX3 to create chimeric proteins led to at least partial rescue of haematopoietic development in vivo (Fukushima-Nakase et al. 2005). Moreover, all three genes appeared equally efficient in rescuing haematopoietic development of Runx1 null cells in an in vitro co-culture system (Goyama et al. 2004).
Direct comparison of all three genes by ectopic expression in murine fibroblasts and gene expression microarray analysis showed a very high degree of redundancy, with a strong overlap in the signature gene expression changes and no examples of opposing regulation. However, there were clearly differences with regard to the relative potency of regulation for individual target genes that could conceivably translate into functional differences in specific niches in vivo (Wotton et al. 2008). In our view the degree of RUNX redundancy and the biological contexts in which it may operate largely remains to be addressed.
12 Conclusions and Prospects
There is growing evidence that the oncogenic potential of the Runx gene family revealed by their powerful co-operation with MYC over-expression or p53 loss in mouse models is highly relevant to human cancer, where a growing body of literature attests to the important roles that RUNX family members play in supporting the oncogenic phenotypes of end-stage cancers and cell lines. The tumour suppressor features of the Runx genes have been less amenable to dissection in in vivo models, but are now being elucidated using conditional knockout models. Evidence that the Runx genes operate in a complex integrated regulatory network suggests that future studies should address effects on all three genes where any single gene is affected.
References
Bauer, O., Sharir, A., Kimura, A., Hantisteanu, S., Takeda, S., & Groner, Y. (2015). Loss of osteoblast Runx3 produces severe congenital osteopenia. Molecular and Cellular Biology, 35, 1097–1109.
Ben-Ami, O., Friedman, D., Leshkowitz, D., Goldenberg, D., Orlovsky, K., Pencovich, N., et al. (2013). Addiction of t(8;21) and inv(16) acute myeloid leukemia to native RUNX1. Cell Reports, 4, 1131–1143.
Bledsoe, K. L., McGee-Lawrence, M. E., Camilleri, E. T., Wang, X., Riester, S. M., van Wijnen, A. J., et al. (2014). RUNX3 facilitates growth of Ewing sarcoma cells. Journal of Cellular Physiology, 229, 2049–2056.
Blyth, K., Terry, A., O’Hara, M., Baxter, E. W., Campbell, M., Stewart, M., et al. (1995). Synergy between a human c-myc transgene and p53 null genotype in murine thymic lymphomas: Contrasting effects of homozygous and heterozygous p53 loss. Oncogene, 10, 1717–1723.
Blyth, K., Terry, A., Mackay, N., Vaillant, F., Bell, M., Cameron, E. R., et al. (2001). Runx2: A novel oncogenic effector revealed by in vivo complementation and retroviral tagging. Oncogene, 20, 295–302.
Blyth, K., Vaillant, F., Hanlon, L., Mackay, N., Bell, M., Jenkins, A., et al. (2006). Runx2 and MYC collaborate in lymphoma development by suppressing apoptotic and growth arrest pathways in vivo. Cancer Research, 66, 2195–2201.
Blyth, K., Slater, N., Hanlon, L., Bell, M., Mackay, N., Stewart, M., et al. (2009). Runx1 promotes B-cell survival and lymphoma development. Blood Cells, Molecules & Diseases, 43, 12–19.
Borland, G., Kilbey, A., Hay, J., Gilroy, K., Terry, A., Mackay, N., et al. (2016). Addiction to Runx1 is partially attenuated by loss of p53 in the Emu-Myc lymphoma model. Oncotarget, 7, 22973–22987.
Brady, G., Whiteman, H. J., Spender, L. C., & Farrell, P. J. (2009). Downregulation of RUNX1 by RUNX3 requires the RUNX3 VWRPY sequence and is essential for Epstein-Barr virus-driven B-cell proliferation. Journal of Virology, 83, 6909–6916.
Brenner, O., Levanon, D., Negreanu, V., Golubkov, O., Fainaru, O., Woolf, E., & Groner, Y. (2004). Loss of Runx3 function in leukocytes is associated with spontaneously developed colitis and gastric mucosal hyperplasia. Proceedings of the National Academy of Sciences of the United States of America, 101, 16016–16021.
Browne, G., Dragon, J. A., Hong, D., Messier, T. L., Gordon, J. A., Farina, N. H., et al. (2016). MicroRNA-378-mediated suppression of Runx1 alleviates the aggressive phenotype of triple-negative MDA-MB-231 human breast cancer cells. Tumour Biology, 37, 8825–8839.
Cai, X., Gao, L., Teng, L., Ge, J., Oo, Z. M., Kumar, A. R., et al. (2015). Runx1 deficiency decreases ribosome biogenesis and confers stress resistance to hematopoietic stem and progenitor cells. Cell Stem Cell, 17, 165–177.
Cameron, E. R., Blyth, K., Hanlon, L., Kilbey, A., Mackay, N., Stewart, M., et al. (2003). The Runx genes as dominant oncogenes. Blood Cells, Molecules & Diseases, 30, 194–200.
Castilla, L. H., Perrat, P., Martinez, N. J., Landrette, S. F., Keys, R., Oikemus, S., et al. (2004). Identification of genes that synergize with Cbfb-MYH11 in the pathogenesis of acute myeloid leukemia. Proceedings of the National Academy of Sciences of the United States of America, 101, 4924–4929.
Cattoglio, C., Pellin, D., Rizzi, E., Maruggi, G., Corti, G., Miselli, F., et al. (2010). High-definition mapping of retroviral integration sites identifies active regulatory elements in human multipotent hematopoietic progenitors. Blood, 116, 5507–5517.
Chin, D. W., Watanabe-Okochi, N., Wang, C. Q., Tergaonkar, V., & Osato, M. (2015). Mouse models for core binding factor leukemia. Leukemia, 29, 1970–1980.
Cohen-Solal, K. A., Boregowda, R. K., & Lasfar, A. (2015). RUNX2 and the PI3K/AKT axis reciprocal activation as a driving force for tumor progression. Molecular Cancer, 14, 137.
de Bruijn, M. F., & Speck, N. A. (2004). Core-binding factors in hematopoiesis and immune function. Oncogene, 23, 4238–4248.
De Rijck, J., de Kogel, C., Demeulemeester, J., Vets, S., El Ashkar, S., Malani, N., et al. (2013). The BET family of proteins targets moloney murine leukemia virus integration near transcription start sites. Cell Reports, 5, 886–894.
Della Gatta, G., Palomero, T., Perez-Garcia, A., Ambesi-Impiombato, A., Bansal, M., Carpenter, Z. W., et al. (2012). Reverse engineering of TLX oncogenic transcriptional networks identifies RUNX1 as tumor suppressor in T-ALL. Nature Medicine, 18, 436–440.
Di Micco, R., Fumagalli, M., Cicalese, A., Piccinin, S., Gasparini, P., Luise, C., et al. (2006). Oncogene-induced senescence is a DNA damage response triggered by DNA hyper-replication. Nature, 444, 638–642.
Etzold, A., Galetzka, D., Weis, E., Bartsch, O., Haaf, T., Spix, C., et al. (2016). CAF-like state in primary skin fibroblasts with constitutional BRCA1 epimutation sheds new light on tumor suppressor deficiency-related changes in healthy tissue. Epigenetics, 11, 1–12.
Ferrari, N., Riggio, A. I., Mason, S., McDonald, L., King, A., Higgins, T., et al. (2015). Runx2 contributes to the regenerative potential of the mammary epithelium. Scientific Reports, 5, 15658.
Fujii, M., Hayashi, K., Niki, M., Chiba, N., Meguro, K., Endo, K., et al. (1998). Overexpression of AML1 renders a T hybridoma resistant to T cell receptor-mediated apoptosis. Oncogene, 17, 1813–1820.
Fukushima-Nakase, Y., Naoe, Y., Taniuchi, I., Hosoi, H., Sugimoto, T., & Okuda, T. (2005). Shared and distinct roles mediated through C-terminal subdomains of acute myeloid leukemia/Runt-related transcription factor molecules in murine development. Blood, 105, 4298–4307.
Gamberi, G., Benassi, M. S., Bohling, T., Ragazzini, P., Molendini, L., Sollazzo, M. R., et al. (1998). C-myc and c-fos in human osteosarcoma: Prognostic value of mRNA and protein expression. Oncology, 55, 556–563.
Goyama, S., Yamaguchi, Y., Imai, Y., Kawazu, M., Nakagawa, M., Asai, T., et al. (2004). The transcriptionally active form of AML1 is required for hematopoietic rescue of the AML1-deficient embryonic para-aortic splanchnopleural (P-Sp) region. Blood, 104, 3558–3564.
Grossmann, V., Kern, W., Harbich, S., Alpermann, T., Jeromin, S., Schnittger, S., et al. (2011). Prognostic relevance of RUNX1 mutations in T-cell acute lymphoblastic leukemia. Haematologica, 96, 1874–1877.
Gupta, S. S., Maetzig, T., Maertens, G. N., Sharif, A., Rothe, M., Weidner-Glunde, M., et al. (2013). Bromo- and extraterminal domain chromatin regulators serve as cofactors for murine leukemia virus integration. Journal of Virology, 87, 12721–12736.
Hacein-Bey-Abina, S., Garrigue, A., Wang, G. P., Soulier, J., Lim, A., Morillon, E., et al. (2008). Insertional oncogenesis in 4 patients after retrovirus-mediated gene therapy of SCID-X1. The Journal of Clinical Investigation, 118, 3132–3142.
Harrington, E. A., Bennett, M. R., Fanidi, A., & Evan, G. I. (1994). c-Myc-induced apoptosis in fibroblasts is inhibited by specific cytokines. The EMBO Journal, 13, 3286–3295.
Harrison, C. J., Moorman, A. V., Schwab, C., Carroll, A. J., Raetz, E. A., Devidas, M., et al. (2014). An international study of intrachromosomal amplification of chromosome 21 (iAMP21): Cytogenetic characterization and outcome. Leukemia, 28, 1015–1021.
Hermeking, H., & Eick, D. (1994). Mediation of c-Myc-induced apoptosis by p53. Science, 265, 2091–2093.
Howe, S. J., Mansour, M. R., Schwarzwaelder, K., Bartholomae, C., Hubank, M., Kempski, H., et al. (2008). Insertional mutagenesis combined with acquired somatic mutations causes leukemogenesis following gene therapy of SCID-X1 patients. The Journal of Clinical Investigation, 118, 3143–3150.
Hsu, B., Marin, M. C., el-Naggar, A. K., Stephens, L. C., Brisbay, S., & McDonnell, T. J. (1995). Evidence that c-myc mediated apoptosis does not require wild-type p53 during lymphomagenesis. Oncogene, 11, 175–179.
Huser, C. A., Gilroy, K. L., de Ridder, J., Kilbey, A., Borland, G., Mackay, N., et al. (2014). Insertional mutagenesis and deep profiling reveals gene hierarchies and a Myc/p53-dependent bottleneck in lymphomagenesis. PLoS Genetics, 10, e1004167.
Hwang, H. C., Martins, C. P., Bronkhorst, Y., Randel, E., Berns, A., Fero, M., & Clurman, B. E. (2002). Identification of oncogenes collaborating with p27Kip1 loss by insertional mutagenesis and high-throughput insertion site analysis. Proceedings of the National Academy of Sciences of the United States of America, 99, 11293–11298.
Jacobs, J. J., Scheijen, B., Voncken, J. W., Kieboom, K., Berns, A., & van Lohuizen, M. (1999). Bmi-1 collaborates with c-Myc in tumorigenesis by inhibiting c-Myc-induced apoptosis via INK4a/ARF. Genes & Development, 13, 2678–2690.
Khandanpour, C., & Moroy, T. (2013). Growth factor independence 1 (Gfi1) as a regulator of p53 activity and a new therapeutical target for ALL. Oncotarget, 4, 374–375.
Kilbey, A., Blyth, K., Wotton, S., Terry, A., Jenkins, A., Bell, M., et al. (2007). Runx2 disruption promotes immortalization and confers resistance to oncogene-induced senescence in primary murine fibroblasts. Cancer Research, 67, 11263–11271.
Kilbey, A., Terry, A., Cameron, E. R., & Neil, J. C. (2008). Oncogene-induced senescence: An essential role for Runx. Cell Cycle, 7, 2333–2340.
Kilbey, A., Terry, A., Jenkins, A., Borland, G., Zhang, Q., Wakelam, M. J., et al. (2010). Runx regulation of sphingolipid metabolism and survival signaling. Cancer Research, 70, 5860–5869.
Kundu, M., Compton, S., Garrett-Beal, L., Stacy, T., Starost, M. F., Eckhaus, M., et al. (2005). Runx1 deficiency predisposes mice to T-lymphoblastic lymphoma. Blood, 106, 3621–3624.
Kuo, Y. H., Zaidi, S. K., Gornostaeva, S., Komori, T., Stein, G. S., & Castilla, L. H. (2009). Runx2 induces acute myeloid leukemia in cooperation with Cbfbeta-SMMHC in mice. Blood, 113, 3323–3332.
LaFave, M. C., Varshney, G. K., Gildea, D. E., Wolfsberg, T. G., Baxevanis, A. D., & Burgess, S. M. (2014). MLV integration site selection is driven by strong enhancers and active promoters. Nucleic Acids Research, 42, 4257–4269.
Lee, Y. S., Lee, J. W., Jang, J. W., Chi, X. Z., Kim, J. H., Li, Y. H., et al. (2013). Runx3 inactivation is a crucial early event in the development of lung adenocarcinoma. Cancer Cell, 24, 603–616.
Levanon, D., Glusman, G., Bangsow, T., Ben-Asher, E., Male, D. A., Avidan, N., et al. (2001). Architecture and anatomy of the genomic locus encoding the human leukemia-associated transcription factor RUNX1/AML1. Gene, 262, 23–33.
Liakhovitskaia, A., Lana-Elola, E., Stamateris, E., Rice, D. P., van’t Hof, R. J., & Medvinsky, A. (2010). The essential requirement for Runx1 in the development of the sternum. Developmental Biology, 340, 539–546.
Lilljebjorn, H., Soneson, C., Andersson, A., Heldrup, J., Behrendtz, M., Kawamata, N., et al. (2010). The correlation pattern of acquired copy number changes in 164 ETV6/RUNX1-positive childhood acute lymphoblastic leukemias. Human Molecular Genetics, 19, 3150–3158.
Lilljebjorn, H., Rissler, M., Lassen, C., Heldrup, J., Behrendtz, M., Mitelman, F., et al. (2012). Whole-exome sequencing of pediatric acute lymphoblastic leukemia. Leukemia, 26, 1602–1607.
Linggi, B., Muller-Tidow, C., van de Locht, L., Hu, M., Nip, J., Serve, H., et al. (2002). The t(8;21) fusion protein, AML1 ETO, specifically represses the transcription of the p14(ARF) tumor suppressor in acute myeloid leukemia. Nature Medicine, 8, 743–750.
Lu, X. Y., Lu, Y., Zhao, Y. J., Jaeweon, K., Kang, J., Xiao-Nan, L., et al. (2008). Cell cycle regulator gene CDC5L, a potential target for 6p12-p21 amplicon in osteosarcoma. Molecular Cancer Research, 6, 937–946.
Malynn, B. A., de Alboran, I. M., O’Hagan, R. C., Bronson, R., Davidson, L., DePinho, R. A., & Alt, F. W. (2000). N-myc can functionally replace c-myc in murine development, cellular growth, and differentiation. Genes & Development, 14, 1390–1399.
Mead, A. J., Kharazi, S., Atkinson, D., Macaulay, I., Pecquet, C., Loughran, S., et al. (2013). FLT3-ITDs instruct a myeloid differentiation and transformation bias in lymphomyeloid multipotent progenitors. Cell Reports, 3, 1766–1776.
Miething, C., Grundler, R., Mugler, C., Brero, S., Hoepfl, J., Geigl, J., et al. (2007). Retroviral insertional mutagenesis identifies RUNX genes involved in chronic myeloid leukemia disease persistence under imatinib treatment. Proceedings of the National Academy of Sciences of the United States of America, 104, 4594–4599.
Mikkers, H., Allen, J., Knipscheer, P., Romeijn, L., Hart, A., Vink, E., & Berns, A. (2002). High-throughput retroviral tagging to identify components of specific signaling pathways in cancer. Nature Genetics, 32, 153–159.
Motoda, L., Osato, M., Yamashita, N., Jacob, B., Chen, L. Q., Yanagida, M., et al. (2007). Runx1 protects hematopoietic stem/progenitor cells from oncogenic insult. Stem Cells, 25, 2976–2986.
Niini, T., Vettenranta, K., Hollmen, J., Larramendy, M. L., Aalto, Y., Wikman, H., et al. (2002). Expression of myeloid-specific genes in childhood acute lymphoblastic leukemia – A cDNA array study. Leukemia, 16, 2213–2221.
Owen, C. J., Toze, C. L., Koochin, A., Forrest, D. L., Smith, C. A., Stevens, J. M., et al. (2008). Five new pedigrees with inherited RUNX1 mutations causing familial platelet disorder with propensity to myeloid malignancy. Blood, 112, 4639–4645.
Parrinello, S., Samper, E., Krtolica, A., Goldstein, J., Melov, S., & Campisi, J. (2003). Oxygen sensitivity severely limits the replicative lifespan of murine fibroblasts. Nature Cell Biology, 5, 741–747.
Putz, G., Rosner, A., Nuesslein, I., Schmitz, N., & Buchholz, F. (2006). AML1 deletion in adult mice causes splenomegaly and lymphomas. Oncogene, 25, 929–939.
Rudolph, B., Hueber, A. O., & Evan, G. I. (2000). Reversible activation of c-Myc in thymocytes enhances positive selection and induces proliferation and apoptosis in vitro. Oncogene, 19, 1891–1900.
Schnerch, D., Lausch, E., Becker, H., Felthaus, J., Pfeifer, D., Mundlos, S., et al. (2014). Up-regulation of RUNX2 in acute myeloid leukemia in a patient with an inherent RUNX2 haploinsufficiency and cleidocranial dysplasia. Leukemia & Lymphoma, 55, 1930–1932.
Schwarzwaelder, K., Howe, S. J., Schmidt, M., Brugman, M. H., Deichmann, A., Glimm, H., et al. (2007). Gammaretrovirus-mediated correction of SCID-X1 is associated with skewed vector integration site distribution in vivo. The Journal of Clinical Investigation, 117, 2241–2249.
Scobie, L., Hector, R. D., Grant, L., Bell, M., Nielsen, A. A., Meikle, S., et al. (2009). A novel model of SCID-X1 reconstitution reveals predisposition to retrovirus-induced lymphoma but no evidence of gammaC gene oncogenicity. Molecular Therapy, 17, 1031–1038.
Serrano, M., Lin, A. W., McCurrach, M. E., Beach, D., & Lowe, S. W. (1997). Oncogenic ras provokes premature cell senescence associated with accumulation of p53 and p16INK4a. Cell, 88, 593–602.
Sharma, A., Larue, R. C., Plumb, M. R., Malani, N., Male, F., Slaughter, A., et al. (2013). BET proteins promote efficient murine leukemia virus integration at transcription start sites. Proceedings of the National Academy of Sciences of the United States of America, 110, 12036–12041.
Shimizu, K., Yamagata, K., Kurokawa, M., Mizutani, S., Tsunematsu, Y., & Kitabayashi, I. (2013). Roles of AML1/RUNX1 in T-cell malignancy induced by loss of p53. Cancer Science, 104, 1033–1038.
Shin, M. H., He, Y., Marrogi, E., Piperdi, S., Ren, L., Khanna, C., et al. (2016). A RUNX2-mediated epigenetic regulation of the survival of p53 defective cancer cells. PLoS Genetics, 12, e1005884.
Spender, L. C., Whiteman, H. J., Karstegl, C. E., & Farrell, P. J. (2005). Transcriptional cross-regulation of RUNX1 by RUNX3 in human B cells. Oncogene, 24, 1873–1881.
Stewart, M., Cameron, E., Campbell, M., McFarlane, R., Toth, S., Lang, K., et al. (1993). Conditional expression and oncogenicity of c-myc linked to a CD2 gene dominant control region. International Journal of Cancer, 53, 1023–1030.
Stewart, M., Terry, A., Hu, M., O’Hara, M., Blyth, K., Baxter, E., et al. (1997). Proviral insertions induce the expression of bone-specific isoforms of PEBP2alphaA (CBFA1): Evidence for a new myc collaborating oncogene. Proceedings of the National Academy of Sciences of the United States of America, 94, 8646–8651.
Stewart, M., MacKay, N., Cameron, E. R., & Neil, J. C. (2002). The common retroviral insertion locus Dsi1 maps 30 kilobases upstream of the P1 promoter of the murine Runx3/Cbfa3/Aml2 gene. Journal of Virology, 76, 4364–4369.
Stewart, M., Mackay, N., Hanlon, L., Blyth, K., Scobie, L., Cameron, E., & Neil, J. C. (2007). Insertional mutagenesis reveals progression genes and checkpoints in MYC/Runx2 lymphomas. Cancer Research, 67, 5126–5133.
Strefford, J. C., van Delft, F. W., Robinson, H. M., Worley, H., Yiannikouris, O., Selzer, R., et al. (2006). Complex genomic alterations and gene expression in acute lymphoblastic leukemia with intrachromosomal amplification of chromosome 21. Proceedings of the National Academy of Sciences of the United States of America, 103, 8167–8172.
Suzuki, T., Shen, H., Akagi, K., Morse, H. C., Malley, J. D., Naiman, D. Q., et al. (2002). New genes involved in cancer identified by retroviral tagging. Nature Genetics, 32, 166–174.
Taniuchi, I., Osato, M., Egawa, T., Sunshine, M. J., Bae, S. C., Komori, T., et al. (2002). Differential requirements for Runx proteins in CD4 repression and epigenetic silencing during T lymphocyte development. Cell, 111, 621–633.
Uren, A. G., Kool, J., Berns, A., & van Lohuizen, M. (2005). Retroviral insertional mutagenesis: Past, present and future. Oncogene, 24, 7656–7672.
Uren, A. G., Kool, J., Matentzoglu, K., de Ridder, J., Mattison, J., van Uitert, M., et al. (2008). Large-scale mutagenesis in p19(ARF)- and p53-deficient mice identifies cancer genes and their collaborative networks. Cell, 133, 727–741.
Vaillant, F., Blyth, K., Terry, A., Bell, M., Cameron, E. R., Neil, J., & Stewart, M. (1999). A full-length Cbfa1 gene product perturbs T-cell development and promotes lymphomagenesis in synergy with myc. Oncogene, 18, 7124–7134.
Vaillant, F., Blyth, K., Andrew, L., Neil, J. C., & Cameron, E. R. (2002). Enforced expression of Runx2 perturbs T cell development at a stage coincident with beta-selection. Journal of Immunology, 169, 2866–2874.
van der Weyden, L., Papaspyropoulos, A., Poulogiannis, G., Rust, A. G., Rashid, M., Adams, D. J., et al. (2012). Loss of RASSF1A synergizes with deregulated RUNX2 signaling in tumorigenesis. Cancer Research, 72, 3817–3827.
Vijaya, S., Steffen, D. L., Kozak, C., & Robinson, H. L. (1987). Dsi-1, a region with frequent proviral insertions in Moloney murine leukemia virus-induced rat thymomas. Journal of Virology, 61, 1164–1170.
Wang, C. Q., Krishnan, V., Tay, L. S., Chin, D. W., Koh, C. P., Chooi, J. Y., et al. (2014). Disruption of Runx1 and Runx3 leads to bone marrow failure and leukemia predisposition due to transcriptional and DNA repair defects. Cell Reports, 8, 767–782.
Whyte, W. A., Orlando, D. A., Hnisz, D., Abraham, B. J., Lin, C. Y., Kagey, M. H., et al. (2013). Master transcription factors and mediator establish super-enhancers at key cell identity genes. Cell, 153, 307–319.
Williams, A., Harker, N., Ktistaki, E., Veiga-Fernandes, H., Roderick, K., Tolaini, M., et al. (2008). Position effect variegation and imprinting of transgenes in lymphocytes. Nucleic Acids Research, 36, 2320–2329.
Wolyniec, K., Wotton, S., Kilbey, A., Jenkins, A., Terry, A., Peters, G., et al. (2009). RUNX1 and its fusion oncoprotein derivative, RUNX1-ETO, induce senescence-like growth arrest independently of replicative stress. Oncogene, 28, 2502–2512.
Wong, W. F., Kohu, K., Nakamura, A., Ebina, M., Kikuchi, T., Tazawa, R., et al. (2012). Runx1 deficiency in CD4+ T cells causes fatal autoimmune inflammatory lung disease due to spontaneous hyperactivation of cells. Journal of Immunology, 188, 5408–5420.
Wotton, S., Stewart, M., Blyth, K., Vaillant, F., Kilbey, A., Neil, J. C., & Cameron, E. R. (2002). Proviral insertion indicates a dominant oncogenic role for Runx1/AML-1 in T-cell lymphoma. Cancer Research, 62, 7181–7185.
Wotton, S. F., Blyth, K., Kilbey, A., Jenkins, A., Terry, A., Bernardin-Fried, F., et al. (2004). RUNX1 transformation of primary embryonic fibroblasts is revealed in the absence of p53. Oncogene, 23, 5476–5486.
Wotton, S., Terry, A., Kilbey, A., Jenkins, A., Herzyk, P., Cameron, E., & Neil, J. C. (2008). Gene array analysis reveals a common Runx transcriptional programme controlling cell adhesion and survival. Oncogene, 27, 5856–5866.
Zaidi, S. K., Pande, S., Pratap, J., Gaur, T., Grigoriu, S., Ali, S. A., et al. (2007). Runx2 deficiency and defective subnuclear targeting bypass senescence to promote immortalization and tumorigenic potential. Proceedings of the National Academy of Sciences of the United States of America, 104, 19861–19866.
Zaliova, M., Madzo, J., Cario, G., & Trka, J. (2011). Revealing the role of TEL/AML1 for leukemic cell survival by RNAi-mediated silencing. Leukemia, 25, 313–320.
Zindy, F., Eischen, C. M., Randle, D. H., Kamijo, T., Cleveland, J. L., Sherr, C. J., & Roussel, M. F. (1998). Myc signaling via the ARF tumor suppressor regulates p53-dependent apoptosis and immortalization. Genes & Development, 12, 2424–2433.
Zinkernagel, R. M., Callahan, G. N., Althage, A., Cooper, S., Klein, P. A., & Klein, J. (1978). On the thymus in the differentiation of “H-2 self-recognition” by T cells: Evidence for dual recognition? The Journal of Experimental Medicine, 147, 882–896.
Acknowledgements
Our work was supported by a joint programme grant from Bloodwise (grant number 13046) and Cancer Research UK (grant number A11951).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Neil, J.C., Gilroy, K., Borland, G., Hay, J., Terry, A., Kilbey, A. (2017). The RUNX Genes as Conditional Oncogenes: Insights from Retroviral Targeting and Mouse Models. In: Groner, Y., Ito, Y., Liu, P., Neil, J., Speck, N., van Wijnen, A. (eds) RUNX Proteins in Development and Cancer. Advances in Experimental Medicine and Biology, vol 962. Springer, Singapore. https://doi.org/10.1007/978-981-10-3233-2_16
Download citation
DOI: https://doi.org/10.1007/978-981-10-3233-2_16
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-3231-8
Online ISBN: 978-981-10-3233-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)