Abstract
Thoracic trauma is the second most common cause of mortality of all traumatic injuries, accounting for about 25 % of traumatic deaths. The present review focuses on the advances of the relevant literature regarding the most appropriate approach and definitive treatment of thoracic trauma . The universal clinical application of focused assessment with sonography for trauma (FAST) has greatly enhanced the tool for traumatic diagnosis, monitoring, and interventional procedural guidance. FAST has been used as an efficient triaging tool in blunt thoracic trauma patients. Additionally, video-assisted thoracoscopic surgery (VATS) has been established as safe and effective for managing thoracic trauma in hemodynamically stable patients. VATS for specific indications in thoracic trauma is associated with improved outcomes, decreased morbidity and mortality, and shortened hospital stay. Emergency resuscitative thoracotomy (ERT) is an accepted intervention for penetrating cardiothoracic trauma patient in extremis. However, its role in blunt trauma patient in extremis has been challenged and has been a subject of considerable debate. The treatment of flail chest injuries has undergone dramatic evolution over the last hundred years. Surgical stabilization of severe rib fractures offers several theoretical advantages, but the use of surgery for the treatment of flail chest is still controversial. For the treatment of deep pulmonary lacerations, the techniques that achieve hemostasis while preserving the maximal amount of pulmonary parenchyma are desirable. Lung-sparing technique is an less extensive surgical techniques of repair and resection surgical including suture pneumonorrhaphy, stapled and clamp pulmonary tractotomy with selective vessel ligation, and non-anatomic resection. The management of traumatic aortic injury has been transformed through the application of thoracic endovascular aortic repair (TEVAR) . TEVAR has been increasingly used for definitive treatment and its outcomes appear to be at least equally safe and effective as those of open repair. Finally, extracorporeal organ support is becoming more commonplace in trauma critical care management as clinical evidence for the merits of this approach builds.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Thoracic trauma
- Pulmonary injury
- Video-assisted thoracoscopic surgery (VATS)
- Focused assessment with sonography for trauma (FAST)
- Emergency resuscitative thoracotomy (ERT)
- Flail chest
- Lung-sparing techniques
- Pulmonary tractotomy
- Thoracic endovascular aortic repair (TEVAR)
Thoracic trauma is the second most common cause of mortality of all traumatic injuries, accounting for about 25 % of traumatic deaths [1]. Thoracic injury as a result of motor vehicle collisions throughout the world is extremely prevalent. Thoracic trauma is associated with high morbidity and mortality rates due to it can affect oxygenation, ventilation, and maintenance of circulation and may result in significant respiratory distress and shock . Many thoracic injuries cause death can be immediate or within the first minutes or hours after injury. Immediate deaths usually involve disruption of the heart or great vessel injury. Early deaths are frequently caused by airway obstruction, tension pneumothorax, pulmonary contusion, or cardiac tamponade. Injuries from chest trauma ranged from rib fractures requiring only pain control to cardiac lacerations with tamponade or exsanguinating hemorrhage. Given the range of injuries, acuity and clinical presentation, multiple diagnostic modalities, and treatment options, exist for thoracic trauma. Initial resuscitation is performed according to advanced trauma life support with immediate attention to airway, breathing, and circulation. During the primary survey, tracheal intubation, mechanical ventilation, closed chest tube thoracostomy and shock resuscitation can be crucial, time-sensitive therapies. Recently, much progress in the science of technologies in trauma critical care management and research-based advances improve outcomes for patients with major chest trauma.
1 Focused Assessment with Sonography for Trauma (FAST)
The injured patient should be rapidly evaluated and the treatments are prioritized based on the mechanism of injury, the patient’s presentation and physical examination. The first priority is to treat patients with unstable condition or dying patients. The principle of the initial assessment and resuscitation is according to the beginning of resuscitation while performing concurrent diagnostic procedures. It is important to avoid performing time-consuming auxiliary examination for severe unstable thoracic injury or dying patients due to the rapid changes of these patients condition. Currently, diagnostic thoracic/abdominal cavity puncture, FAST and emergency room bedside X-ray radiograph are three key component of primary diagnostic tool for unstable patients in most large institutions.
Primary assessment and management of thoracic trauma should follow the standard advanced trauma life support principles, starting with control of the airway. While it is obvious that a chest injury may affect breathing, the major effect of a tension pneumothorax and haemothorax is on circulation. A chest drain will be both diagnostic and therapeutic. During the initial hospital phase, the injured patient is rapidly assessed and the treatments are prioritized based on the mechanism of injury and the patient’s vital signs. The goal of the resuscitation is to improve organ and tissue perfusion by rapidly identifying and simultaneously treating life-threatening conditions.
Continued advances in imaging technology and the application of existing techniques are at the forefront of the initial evaluation of the trauma patient, particularly in patients who are critically injured. Radiographic diagnostics must be rapid and accurate. The initial radiographic evaluation screens for immediate life-threatening conditions. More sophisticated diagnostics then identify organ-specific injury and characterize its severity.
FAST and chest X-ray (CXR) are both rapid and repeatable bedside auxiliary examination and can help determine if indications for immediate operative intervention are present. Since its inception in the 1990s, the use of FAST scanning has assumed a key role in the rapid non-invasive assessment and subsequent management of patients suffering thoracoabdominal trauma [2]. The evolution of FAST has seen its incorporation into American College of Surgeons Advanced Trauma Life Support (ATLS) training and it is currently used by emergency physicians in resuscitation rooms worldwide to assist timely decision-making. FAST has proved to be a promising tool for pneumothorax. CXR and computed tomography (CT) scan are the two important investigations commonly used for the diagnosis. However, CXR has been shown to be an insensitive examination. The CT scan is the gold standard for the detection of pneumothorax, but it requires severely injured patients to be transported to the CT room, is time consuming and results in delayed diagnosis. FAST is easily performed at the bedside in the trauma resuscitation room and is used to perform rapid evaluation for severely injured patients. The use of FAST to detect pneumothorax has been studied by several trials to have a higher sensitivity and specificity compared to CXR [3–5]. Three meta-analyses provided a comprehensive analysis of the current literature evaluated the diagnostic accuracy of transthoracic ultrasonography for the diagnosis of pneumothorax in comparison CXR. Ding et al. [6] showed that pooled sensitivity and specificity were 0.88 and 0.99 respectively for ultrasonography, and 0.52 and 1.00 respectively for CXR. Alrajhi et al. [7] reported that ultrasonography was 90.9 % sensitive and 98.2 % specific for the detection of pneumothorax. Alrajab et al. [8] indicates that ultrasonography had a pooled sensitivity of 78.6 % and a specificity of 98.4 %. CXR had a pooled sensitivity of 39.8 % and a specificity of 99.3 %. These meta-analyses demonstrated that bedside ultrasonography performed by clinicians had higher sensitivity and similar specificity compared with CXR in the diagnosis of pneumothorax.
2 Minimally Invasive Techniques in Thoracic Trauma
Approximately 10–20 % of patients who sustain chest trauma will eventually need operative intervention [9, 10]. Although the majority of hemodynamically stable patients with chest trauma can initially be treated with closed tube thoracostomy, it may be ineffective, leading to an increased risk of conversion to open thoracotomy or a prolonged duration of hospitalization [11]. Open thoracotomy is a major surgical procedure and its large incisions are associated with a long and painful recovery [12]. Thoracoscopic evaluation of penetrating thoracic injuries was first described by Branco in Brazil in 1946 [13]. Video-assisted thoracic surgery (VATS) was then subsequently described by Jackson and Ferreira in 1976 to diagnose diaphragmatic injuries incurred by penetrating trauma to the left lower chest [14]. In 1981, Jones, et al. reported the performance of emergency thoracoscopy with local anesthetic in patients with ongoing bleeding following tube thoracostomy placement for traumatic hemothoraces [15, 16]. Over the past 20 years, the advent and increasing expertise in VATS has made it an effective and safe alternative in the assessment and management of thoracic surgery. VATS is associated with decreased morbidity and mortality, and shortened hospital stay [17].
Indications for VATS in stable patients are based upon initial findings and the patient evolution. The immediate indications including significant hemothorax (>1500 ml at chest tube insertion), continuous bleeding (>300 ml/h within the first 3 h after chest tube insertion), suspected diaphragmatic injury, suspicion of a penetrating heart wound, and withdrawal of a stab in situ under direct vision [18–20]. Delayed (up to several days after the trauma) indications including retained or clotted hemothorax, prolonged air leak and/or recurrent pneumothorax, secondary empyema, thoracic duct injuries, and foreign body extraction such as bullets, wires, etc. [21–24]. In multiply-injured patients, VATS is used in a more delayed fashion; as other general surgical, neurosurgical and orthopaedic issues take priority before consideration is given to residual haemothorax [16]. Furthermore, ongoing chest drainage post-thoracostomy placement in the stable patient can be investigated and occasionally treated by VATS [25]. Expanded uses of VATS include: control of intercostal arterial bleeding, pulmonary resection, bronchoplasty, thoracic duct ligation, pericardial window creation, foreign body removal, evaluation and repair of diaphragmatic injury, evaluation of esophageal injury, and chest wall repair [26, 27]. The major and most frequent contraindication for using the VATS approach to addressing thoracic trauma is hemodynamic instability. Other relative, but not absolute, contraindications include suspected injuries to the heart or great vessels, inability to tolerate prolonged single lung ventilation, inability to tolerate lateral decubitus position, an obliterated pleural space, prior thoracotomy, other injuries with indication for emergency thoracotomy or sternotomy, and coagulopathy. In general, rules of patient safety and beneficial outcome should always be paramount to any dogma or focus on the type of surgical approach.
The most common urgent use of VATS following trauma is the drainage of residual hemothoraces greater than 500 ml or collections that result in the opacification of one-third of a hemithorax [28]. In many cases, the source of hemorrhage is either a bleeding intercostal artery or vein secondary to ribcage trauma or fracture. Other common causes of intrathoracic bleeding include parenchymal injuries such as pulmonary lacerations or pulmonary vascular injury from ballistic trauma. Many of these sources of bleeding can be managed thoracoscopically via direct coagulation, the placing of clips, or via suture. In cases of parenchymal injury, endoscopic surgical staplers have made the resection of segments or entire lobes of the lung reasonably facile.
Recently, a meta-analysis of randomized control trials and cohort studies comparing the perioperative outcomes of VATS with open thoracotomy for chest trauma patients demonstrated that VATS is an effective and even better treatment for improving perioperative outcomes of hemodynamically stable patients with chest trauma and reduce the complications [17]. Pooled analyses showed significant reductions in the incidence of postoperative complications, chest tube drainage volume, duration of tube drainage, duration of hospitalization, operation time, amount of bleeding and transfusion volume in chest trauma patients treated with VATS compared with open thoracotomy. The perioperative mortality rate was not significantly different between patients received VATS and open thoracotomy. In addition, VATS was also decrease the total cost of hospitalization when compared with tube thoracostomy in patients with blunt chest trauma [29].
3 Emergency Resuscitative Thoracotomy
A total of 72.4 % of patients of penetrating cardiac injuries die before reaching the hospital [30], and resuscitative thoracotomy becomes the only hope for the survival of traumatic cardiac arrest patients. Emergency department thoracotomy (EDT), also known as emergency resuscitative thoracotomy (ERT), has been considered a heroic, high-risk procedure for patients in extremis since its introduction in 1967, and over the last four decades, ERT has become well established technique for managing life-threatening thoracic trauma, the technique has been used with increasing selectivity.
A left anterolateral thoracotomy (LAT) is typically considered the standard incision for ERT, because it provides rapid access to the heart and the descending aorta, ability to perform in a supine patient, and ability to be extended to the right hemithorax (clamshell) or laparotomy if clinically warranted [31, 32]. Many surgeons have demonstrated that a stepwise approach to ERT incisions based on clinical presentation may be a reasonable approach, starting with LAT and extending the incision to clamshell if necessary [33, 34]. Others have suggested that the clamshell incision may instead be the standard initial ERT incision [35, 36]. Median sternotomy provided better access to intrathoracic structures than left and right anterior thoracotomies. Definitive control of the origin of the left subclavian artery was difficult with left 2nd or 3rd intercostal space incisions. Bilateral anterior thoracotomy, the clamshell incision, was easy to perform and gave superior access to all intrathoracic structures. In severe thoracic trauma, specific injuries are unknown, even if they can be anticipated. The best incision is therefore one that provides the most rapid and definitive access to all thoracic structures for assessment and control. While the right and left anterolateral incisions may be successfully employed by surgeons with extensive experience in ERT, the clamshell incision remains the superior incision choice [34].
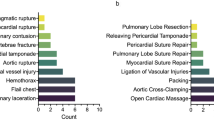
The goals of an EDT are draining of pericardial tamponade, controlling intrathoracic vascular or cardiac hemorrhage, cross-clamping the pulmonary hilum after massive air embolism or bronchopleural fistula, cross-clamping the descending aorta, performing open cardiac massage, and confirming proper endotracheal tube placement [33–35, 37]. Other objectives include vascular control for intra-abdominal hemorrhage and managing acute bronchovenous air embolism.
Emergency thoracotomy is an accepted intervention for penetrating cardiothoracic trauma patient in extremis. However, its role in blunt trauma patient in extremis has been challenged and has been a subject of considerable debate [38]. The challenge for today’s surgeon lies in determining whether a patient would benefit from EDT, a radical procedure that offers a chance of survival for patients who present in extremis. ATLS course states that patients with penetrating thoracic injuries arriving pulseless with myocardial activity should undergo immediate EDT, while those sustaining blunt trauma are not candidate for EDT based on extremely low survival rates.
In 2004, Powell and colleagues established indications for EDT based on 26 years of consecutive data [39]. The authors made three general recommendations for performing an EDT: EDT is indicated when there is witnessed penetrating chest trauma and <15 min of prehospital cardiopulmonary resuscitation (CPR); witnessed non-penetrating chest trauma and <5 min of prehospital CPR; or witnessed blunt trauma and <5 min of prehospital CPR. EDT should also be performed for severe hypotension (systolic blood pressure < 60 mmHg) due to cardiac tamponade, intrathoracic hemorrhage, air embolism, or active intra-abdominal hemorrhage. Contraindications for ERT include penetrating trauma and >15 min of CPR and no signs of life, and blunt trauma with >5 min of CPR and no signs of life or asystole [39]. Signs of life include detectable blood pressure, respiratory or motor effort, cardiac electrical activity, or pupillary activity. In 2011 the Western Trauma Association (WTA) paper, Moore et al. report survivors of blunt torso injuries with pre-hospital CPR up to 9 min and penetrating torso wounds up to 15 min, and recommended broadening the indications for EDT. Furthermore, the WTA multicenter experience suggests that resuscitative thoracotomy in the EDT is unlikely to yield productive survival when patients (1) sustain blunt trauma and require >10 min of prehospital CPR without response, (2) have penetrating wounds and undergo >15 min of prehospital CPR without response, or (3) manifest asystole without pericardial tamponade [40]. However, this multicenter study’s conclusion might have been limited because it does not provide the total number of EDTs performed, patient CPR time, or the characteristics of non-survivors [41].
According to the American College of Surgeons Committee on Trauma guidelines, EDT should rarely be performed on patients suffering blunt trauma [42]. This point may be disputed by data from a Scandinavian study that reported a survival rate of 12.2 % for blunt trauma EDT [43]. Lustenberger et al. and Kandler et al. reported similarly higher survival rates for blunt trauma (7.7 and 20 % respectively). Based on these studies and Moore et al.’s survivor analysis, the declaration of futility of EDT in blunt traumas should be reconsidered. Guidelines published by WTA in 2012 stating that patients undergoing CPR on presentation to the hospital should be stratified based on injury and transport time to ascertain whether EDT is advisable [44].
In 2015, with the support of recent data, Dayama et al. suggested revision to the guidelines for performing EDT as following: (1) EDT should be performed selectively in patients sustaining cardiopulmonary arrest secondary to blunt trauma after SOLs are lost in the emergency department or at the scene with transportation time equal to or less than 10 min. (2) EDT should be performed in patients sustaining penetrating thoracic injuries with loss of SOLs witnessed in the emergency department or at the scene with transportation time equal to or less than 15 min. Finally, as in all studies, the completeness and accuracy of the prehospital information is in question. In summarizing these data, EDT should be offered to patients who arrive in asystole to the hospital and are suspected to have a cardiac injury and tamponade [45].
The role of EDT continues to be debated due to these data are largely derived from retrospective analyses of trauma registries that have not been specifically designed to evaluate the critical factors predictive of survival after ED thoracotomy. EDT is best applied in patients with penetrating cardiac injuries, and should be applied with penetrating cardiac injuries, and should be applied in patients with penetrating non-cardiac thoracic injuries and exsanguinating abdominal vascular injuries in accordance with the level II recommendations of the American College of Surgeons [42]. In general, patients who require EDT after penetrating trauma mechanisms have better outcomes than those who have suffered blunt trauma (comes than those who have suffered blunt trauma). The mechanism of injury is usually the strongest predictors of survival post-EDT [46]. Recently, in a meta-analysis performed by Dayama et al. [41], the overall survival rate in patients with EDT for penetrating traumas was 9.8 % (169 of the 1719, range 0–45.5); the survival rate in patients with EDT for blunt injuries was 5.2 % (24 of the 460, range 0–12.2). These data are compared with analysis by the American College of Surgeons Committee on Trauma, which demonstrated patients with penetrating injuries had a survival rate of 11.2 and 1.6 % in those with blunt trauma. Furthermore, an interesting finding in this review was a notable difference in the survivor outcome of US experience versus non-US experience with only 6.5 % surviving in the US as compared with 11.4 % outside the US. And also, this review shows a better survival rate of EDT in military (11.9 %) and in pre-hospital settings (16.3 %). Seamon et al. [47] investigated whether EDT versus resuscitation without EDT improves outcomes in patients who present to the hospital pulseless after critical thoracic injuries. Patients presenting pulseless after penetrating thoracic injury have the most favorable EDT outcomes both with (survival, 21.3 %; neurologically intact survival, 11.7 %) and without signs of life (survival, 8.3 %; neurologically intact survival, 3.9 %). In patients presenting pulseless after penetrating extrathoracic injury, EDT outcomes were more favorable with signs of life (survival, 15.6 %; neurologically intact survival, 16.5 %) than without (survival, 2.9 %; neurologically intact survival, 5.0 %). Outcomes after EDT in pulseless blunt injury patients were limited with signs of life (survival, 4.6 %; neurologically intact survival, 2.4 %) and dismal without signs of life (survival, 0.7 %; neurologically intact survival, 0.1 %).
Although most survival studies of EDT focus on neurologic outcome, a novel study by Keller et al. examined the long term social, cognitive, functional, and psychological consequences, and determined that of the 8.3 % of patients who survived hospitalization after EDT, the majority of EDT survivors had no evidence of cognitive, functional, or psychological long-term impairment. Seamon and colleagues strongly recommend that patients who present pulseless with signs of life after penetrating thoracic injury undergo EDT. Furthermore they conditionally recommend EDT for patients who present pulseless and have absent signs of life after penetrating thoracic injury, present or absent signs of life after penetrating extrathoracic injury, or present signs of life after blunt injury. Lastly, they conditionally recommend against EDT for pulseless patients without signs of life after blunt injury [47].
4 Surgical Fixation for Flail Chest
Flail chest cause chest wall instability, asynchronous movement of the flail segment, and paradoxical chest motion, which is result in deformity of the chest wall, loss of thoracic volume, decreased lung volume, atelectasis, chest tightness, dyspnea, and chronic pain [48–50]. Flail chest is a life-threatening injury, and is associated with significant morbidity and mortality [51]. Respiratory insufficiency as a result of paradoxical chest movement, lung collapse, and pulmonary contusion are the main factors leading to serious morbidity in patients with flail chest. Of all the above, pulmonary contusion is by far the most important single factor, along with paradoxical motion disrupts the mechanics of ventilation, which contributes to intra-alveolar hemorrhage and flooding resulting in ventilation/perfusion (V/Q) mismatch and hypoxemia. The treatment of flail chest injuries has undergone dramatic evolution over the last hundred years [52]. In the first half of the twentieth century, treatment was focused on mechanical stabilization of the chest wall. At the time, chest wall stabilization was performed by bracing or adhesive strapping or traction of the chest wall. In the second half of the century, the concept of internal pneumatic stabilization use of positive pressure mechanical ventilation became a critical treatment strategy for stabilization of flail chest injuries. Kirschner wires and Judet struts used for stabilization of flail chest injury are outdated modes of fixation compared to current modern technique of plates and screw fixation [53, 54]. The current modern treatment of flail chest injuries includes nonsurgical and surgical treatment strategies including mechanical ventilation, tube thoracostomy, pain control, chest physiotherapy and surgical fixation.
Mechanical ventilation is necessary which is usually for hypoxemia due to pulmonary dysfunction and gas exchange abnormalities, rather than treat chest wall instability [50, 55]. Mechanical ventilation should be weaned from the ventilator at the earliest time possible. Prolonged mechanical ventilation has been reported to leads to barotrauma and increases the risk for pneumonia, sepsis , extended time in the intensive care unit, and death [48–50, 56–58]. Decreasing the number of days on mechanical ventilation may result in decreased morbidity and mortality and may dramatically decrease medical costs [50]. However, patients with head injury and pulmonary contusion may require long-term mechanical ventilation and do not attain the benefits of early extubation [50]. Noninvasive ventilation (NIV) for patients with blunt chest trauma, which demonstrated that early use of NIV in appropriately identified patients with chest trauma and without respiratory distress may prevent intubation and decrease complications and ICU length of stay [59]. NIV may be considered in patients with blunt chest trauma who are neurologically intact, hemodynamically stable and not in respiratory distress. There is no apparent benefit of NIV in the prevention of intubation in patients with respiratory decompensation. In fact, delaying intubation in these patients leads to harm. Future studies need to be methodologically sound and focus on the use of NIV in patients with blunt chest trauma early in the course of the disease, prior to overt respiratory failure [59].
Surgical stabilization of severe rib fractures offers several theoretical advantages (Fig. 1), but the use of surgery for the treatment of flail chest is still controversial [60]. There have been a number of studies demonstrated that surgical fixation of flail chest injuries improved outcomes including fewer days on mechanical ventilation, decreased length of ICU stay, fewer chest infections and less chronic pain, and reduce mortality [61–64]. However, there are limited randomized controlled trials on this area [48, 58, 65]. These randomized controlled trials remain limited by antiquated fixation system, lack of prospective study design and small sample size, outdated methods of surgical fixation and vague study criteria. In 2015, Pieracci et al. conducted a prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. In this clinical evaluation found that surgical stabilization of rib fractures, as compared to best medical management, was associated independently with a 76 % decreased likelihood of respiratory failure and an 82 % decreased likelihood of tracheostomy, as well as 5 day decreased duration of mechanical ventilation, and significantly improved spirometry readings among extubated patients [66]. Surgical stabilization of severe rib fractures offers several advantages, however, there remains a lack of consensus regarding both indications and technique [67]. High-quality large, multicenter randomized controlled trial in this area are still need to better assess the benefits of surgical fixation versus non-operative care for trauma patients with flail chest injuries.
Surgical stabilization of severe rib fractures for a 53-years-old male patient with flail chest . The chest X-ray film showed severe ribs fractures on the left side (a); the surgical finding showed severe multiple ribs fractures (b). Surgical internal ribs fixation showed that shape memory alloy of nickel and titanium encircle rib bone plate is one of the best suitable choose for correction of chest wall floating (c)
There are no absolute indications for operative repair of a flail chest injury. Indications for surgical stabilization of severe rib fractures by Denver Health Medical Center were included: (1) Acute respiratory insufficiency despite optimal medical therapy: either need for mechanical ventilation or ≥2 of the following: tachypnea, hypercarbia, hypoxia, uncontrolled secretions, incentive spirometry <75 % predicted. (2) Uncontrolled pain despite optimal medical therapy: ≥2 of the following: numeric pain score ≥4/10, splinting, lung hypoexpansion on imaging. (3) Anticipated chronic pain/impaired pulmonary mechanics: ≥1 of the following: flail chest, ≥3 severely displaced fractures, hemithorax volume loss ≥30 % [67]. Whereas most reviews have listed four or five categories based mostly on anatomic diagnoses, the Denver Health Medical Center uniquely lists three categories based on the clinical situation. The indications emphasize the goal that the surgery is trying to achieve, but this categorization may promote overuse of this procedure [68].
The most common indication for surgical fixation of flail chest, and that with the strongest evidential support, is for respiratory failure with an anterolateral flail segment without severe underlying pulmonary contusion [58, 65, 69–71]. When contemplating surgical fixation of a chest wall injury, the absence of severe underlying pulmonary contusion (PC) may be particularly important. PC in turn is the most common injury identified in the setting of blunt thoracic trauma, occurring in 30–75 % of all cases [72]. Flail chest is typically accompanied by PC [55]. 54 % of the flail chest injuries patients had lung contusions [50]. Voggenreiter et al. [73] demonstrated that surgical fixation permits early extubation in patients with flail chest and respiratory insufficiency without pulmonary contusion, while patients with pulmonary contusion do not benefit from operative chest wall stabilization. These authors concluded that flail chest and respiratory insufficiency without underlying PC is an indication for surgical fixation. However, in recent, Zhang et al. retrospectively analyzed a study comparing the clinical efficacy of surgical fixation and nonsurgical management of flail chest and PC. These authors concluded that surgical fixation for flail chest with PC could reduce the hospital length of stay (38 vs. 60 days, p = 0.049) [74]. Those studies were a single-center, uncontrolled and retrospective and involved a small sample size. Consequently, although surgical fixation clearly corrects the anatomic chest deformity, the mortality and short term morbidity of flail chest combined with PC entity have not improved. Additional larger, multiple-center, prospective randomized controlled studies are needed further evaluation.
With the increasing technological advancements available in the trauma critical care management, conservative management, has become more common [71]. The optimal nonoperative treatment of patients with flail chest includes adequate pain management, via use of epidural catheters, intercostal nerve blocks, or patient-centered analgesia [55]. The use of epidural catheters seems to be the most preferred method, with improved outcomes and lower complications compared with other methods [52, 55, 75]. Compared with intravenous narcotic use, epidural catheters allow for improved subjective pain perception, pulmonary functions tests, lower rate of pneumonia, as well as decreased length of time on a mechanical ventilator or ICU stay [52, 55, 76]. They also have lower rate of complications such as respiratory depression, somnolence, and gastrointestinal symptoms [55]. Epidural catheters have also been compared with intrapleural catheters in a previous randomized controlled trial and have shown to decrease pain and improve tidal volume and negative inspiratory pressures [75]. Other modes of pain management include use of oral and intravenous narcotic administration and patient-centered analgesia [52, 55].
5 Deep Pulmonary Lacerations
Pulmonary lacerations secondary to either blunt trauma usually as result of displaced rib fractures puncturing the lung parenchyma or penetrating injuries directly to the lung. The natural history of blunt trauma is usually spontaneous resolution, as most are small and superficial and heal without any intervention. The vast majority of lung injuries requiring surgery are caused by penetrating trauma. Deep pulmonary laceration is typically associated with rupture of the visceral pleura and is a critical condition. Deep pulmonary laceration accounts for about 50 % of patients with intrathoracic hemorrhage and often results in death. If early and appropriate treatment is based on accurate diagnosis by rapid assessment of the pathology and by diagnostic imaging (Fig. 2), deep pulmonary laceration is a treatable condition in which the lives of these patients can be saved [77, 78]. VATS has been demonstrated to be an accurate, safe and reliable alternative method for the direct evaluation of the lung injuries.
In the past, major lung resection (lobectomy and pneumonectomy) when performed after traumatic lung injuries has been associated with high morbidity and mortality rates. Simple superficial oversewing of deep penetrating lung injuries potentially lead to postoperative lethality of hemoptysis [79, 80]. Therefore, techniques that achieve hemostasis while preserving the maximal amount of pulmonary parenchyma are desirable (Fig. 3). A major advance in lung-sparing techniques for the treatment of pulmonary penetrating injuries was introduced by Gao et al. [81], and Wall et al. [82] respectively in 1994. Lung-sparing technique is an less extensive surgical techniques of repair and resection surgical including suture pneumonorrhaphy, stapled and clamp pulmonary tractotomy with selective vessel ligation, and non-anatomic resection [83]. These resection techniques are indicated for control of hemorrhage, control of small air leaks, to preserve pulmonary tissue, and/or when the pulmonary injury is amenable to reconstruction [84]. It is estimated that approximately 85 % of all penetrating pulmonary injuries can be managed with these procedures [82, 85–87]. Lung tractotomy allows for rapid exposure and selective ligation of injured pulmonary structures, and thus reduces the need for emergent lung resection [86]. Tractotomy has allowed achieving rapid hemostasis with preservation of lung tissue. Use of stapling instruments has simplified the procedure. Smaller lung resections involving peripheral portions of a lobe were performed as nonanatomic wedge resections using surgical staplers. Lobectomy and pneumonectomy was required for resection of devitalized or destroyed pulmonary tissue in severe lung injuries.
6 Traumatic Aortic Injury
Injury to the aorta and the arch vessels can occur following blunt and penetrating trauma. Traumatic aortic injury (TAI) is the second most common cause of death after blunt trauma [88]. As many as one-third of fatalities in motor vehicle collisions can be attributed to TAI [88, 89]. Burkhart and colleagues reported that 57 % of the deaths occurred at the scene or on arrival to the hospital, 37 % died within the first 4 h of admission, and 6 % died 4 h after admission [90]. In autopsy study involving traffic accidents, 33 % of the victims had associated TAI, 80 % patients with blunt TAI die prior to hospital arrival and only 20 % in hospital [88].
The most common anatomical site of aortic injury is the medial aspect of the lumen, distal to the left subclavian artery. Injury at this site is found in about 93 % of hospital admissions and in about 80 % of autopsy studies [91]. These resulting from a combination of high shear stress, heterogeneity in the wall architecture possibly contributing to focal wall weakness and acute transient intraluminal pressure loading [92, 93]. The most common type of injury is a false aneurysm (58 %), followed by dissection (25 %) and intimal tear (20 %) [94].
For those patients with TAI, timely diagnosis and prompt aggressive blood pressure control are essential in preventing free rupture of the contained aortic injury. Digital substraction angiography (DSA) was the gold standard for diagnosis of TAI traditionally. CT angiography (CTA) is now the new standard modality for screening and definitive diagnosis of TAI [91]. The diagnosis of TAI by DSA and CTA were showed in Fig. 4. The sensitivity and negative predictive value of the CT scan in the diagnosis of blunt TAI approaches 100 % [95]. Advances in CT technology have significantly improved the sensitivity of CT for the detection of TAI. The new-generation multi-slice CT scanners with 3-dimensional reformation have almost 100 % sensitivity and specificity, a 90 % positive and 100 % negative predictive value, an overall diagnostic accuracy of 99.7 %, and provide impressive anatomical details of the aortic arch and the injury site [91, 96]. Transesophageal echocardiography (TEE) as a diagnostic tool might be useful in critically ill patients in the intensive care unit who cannot be transferred safely to the radiology suite for CT scan [91]. Additionally, with regards to long-term surveillance and more specifically the detection of endoleaks, pseudoaneurysms and stent graft material-related complications, recent clinical practice guidelines by the Task Force for the Diagnosis and Treatment of Aortic Diseases of the ESC recommend the combination of a chest X-ray with either MRI or CT scan. Although CT is currently the preferred modality, they advise considering the dangers of radiation , especially in younger patients, and suggest the use of MRI except in cases of magnetic resonance-incompatible grafts [97].
Once the diagnosis is made, treatment must be properly timed. In general, minimal aortic injuries (intimal tear of less than 1 cm with no or minimal peri-aortic haematoma) receive conservative management [98]. Treatment of patients with TAI may be interventional surgical or conservative therapy dependent on clinical judgment on an individual basis [99]. The timing of repair according to the extent of injury on the thoracic aorta and the presence or absence of other injuries [100]. With regards to the best timing of intervention, the decision should be made based on the presence and severity of symptoms and related complications, comorbidities and the presence or absence of other injuries [100].
Prevention of free rupture by means of rigorous blood pressure control is the most urgent priority. The risk of free rupture is highest in the first few hours after the injury, with 90 % of ruptures occurring within the first 24 h [91]. Without rigorous blood pressure control, risk of rupture is about 12 %, and rigorous blood pressure control reduces the risk to about 1.5 % [101, 102]. Systolic blood pressure should be kept as low as tolerated, in most patients at about 90–110 mmHg. In elderly or head-injury patients, optimal systolic pressure might be slightly higher [91]. It is important to avoid excessive administration of intravenous crystalloid, as controlled hypotension is preferred to avoid blood pressure elevation and to decrease the likelihood of aortic rupture [103]. β-blockers and antihypertensive are the most commonly used modalities to modulate the systolic blood pressure [91, 103].
Interventional treatment for blunt TAIs can be either open surgical repair (OSR) or thoracic endovascular aortic repair (TEVAR) . The TEVAR has been widely rapidly adopted as an alternative to the OSR for treatment of traumatic aortic injury (Fig. 5). TEVAR is minimally invasive compared to surgery and can be performed soon after the establishment of diagnosis prior to management of other concomitant severe injuries. TEVAR is an effective option for the treatment of blunt TAI, numerous reports have demonstrated that blunt TAI have benefits of lower blood loss, shorter hospital stay, and reduced mortality rate, which confirming the increased utilization of TEVAR as the primary approach in selected trauma patients. Unlike aneurysmal disease, TAI is usually a focal lesion in the setting of a relatively younger and healthier aorta. As a result, a properly sized, delivered, and deployed device may have a potentially lower rate of long-term complications compared with other aortic pathologies [104].
The same trauma patient showed in Fig. 4. Repeated examination by DSA and CTA after thoracic endovascular aortic repair
The first case report of endovascular stent-graft treatment of a blunt TAI was published in 1997 [105]. Recently published observational studies and meta-analyses favor the use of the endovascular method as definitive treatment over open surgery in patients with TAI and support delaying repair of the injuries where possible. Azizzadeh and colleagues described an estimated odds ratio of 0.33 for complications including in-hospital mortality with TEVAR compared with open repair (OR), similar costs, and similar length of hospital stay [106]. In 2014, Branco et al. after a 9 year analysis of the same data bank, described favorable outcomes of the endovascular approach compared with OR in terms of in-hospital mortality (12.9 % vs. 22.4 %) and sepsis (5.4 vs. 7.5 %) [107]. Estrera et al. found that TEVAR was statistically superior to OR with cross-clamping but not to OR with distal aortic perfusion, in terms of survival (4, 31 and 14 % respectively). In the same study survival at 1 and 5 years post-intervention was 76 and 75 % respectively for OR, and 92 and 87 % for TEVAR [108]. According to Di Eusanio and colleagues, Delayed repair was used as first-line treatment for blunt TAIs and was associated with a very low mortality (3.9 %), mortality and paraplegia rates were not different comparing TEVAR and OR groups [109]. At midterm follow-up (median follow-up 2.3 years, range 0–7 years), TEVAR is an effective and durable option for the treatment of TAI in properly selected patients [104]. The incidence of in-hospital mortality, stroke, and paraplegia were 5.0, 2.4 and 0 %, respectively. The rates of device-related adverse events (2.4 %), secondary procedures (4.8 %), and open conversion are rare (2.4 %). Survival was 95 % at 30 days, 88 % at 1 year, 87 % at 2 years, and 82 % at 5 years. The late outcomes (mean, 103.9 months) following open and endovascular repair of TAI was reported by Patel shows that the overall crude mortality rate was 14.7 % and freedom from aortic reintervention at 4 years was higher after open repair (DTAR 100 % vs. TEVAR 94 %; P = 0.03) [110]. A recent study by Canaud et al. [111] described data of follow-up of minimum 10 years post-TEVAR (mean 11.6 years) with very encouraging results. The authors showed that the favorable outcomes of TEVAR over OR in terms of mortality and complications last over time, follow-up computed tomography scans did not reveal any stent-graft migration or collapse, or secondary endoleaks [111]. The findings support the use of TEVAR over OR for patients with TAI. However, there are no RCTs conducted to determine whether use of TEVAR for the treatment of blunt TAI is associated with reduced mortality and morbidity when compared to conventional open repair. To perform a randomized controlled trial to clarify optimal management of blunt TAI would be very challenging to complete, mainly because of the natural history of the condition, usually seen in combination with other life-threatening injuries, the requirement for urgent intervention and the potential difficulties surrounding consent [112]. Despite lack of RCT evidence, clinicians are moving forward with endovascular treatment of blunt TAI on the basis of meta-analyses and large clinical series. Recent clinical practice guidelines of the Task Force for the Diagnosis and Treatment of Aortic Diseases of the ESC, that advise the use of TEVAR in suitable anatomies (Level of Evidence: C). There are still some unresolved issues and areas of concern.
There are currently some technical limitations to endografting. One of the most common problems in treating aortic arch pathologies is a short proximal landing zone. Injuries that occur adjacent to a sharp bend in the aorta may result in poor apposition of the covered stent to the aortic wall, which leads not only to failure in covering the injury but also to device collapse [113, 114]. Another technical issue relates to the management of the left subclavian artery. Lesions adjacent to the left subclavian artery may require covering this vessel in order to achieve adequate repair. Although usually well tolerated, coverage of the left subclavian artery can result in ischemia of the upper extremity or territory perfused by the left vertebral artery [98]. To further expand the applicability of endovascular repair of aortic arch and descending aortic pathology, alternatives have been proposed, such as the chimney graft technique, which involves placement of stents in side branches of the aorta alongside the main endovascular stent graft [115–117]. One advantage of the chimney technique is that readily available, on-the-shelf stents can be used. When these stents are placed in the side branches parallel to the aortic stent graft, a prolonged proximal landing zone can be created, and continued perfusion of the aortic side branches can be maintained [117]. Chimney graft use in the emergent setting is becoming widely accepted as a useful technique. Increasing amounts of data support the benefit of visceral and arch chimney graft techniques. In particular, the low early mortality and complication rates and high long-term patency seem advantageous in electively treated cases [118]. Elective TEVAR with the chimney technique is used more often and is a potential new technique to replace hybrid repair for thoracic aortic diseases.
7 Extracorporeal Lung Support in Trauma Patients
Acute respiratory distress syndrome (ARDS) is most frequently observed in the early course of intensive care in patients with severe trauma which has an associated mortality rate of 40–60 % despite many medical advances in its treatment [119–121]. The injury to the lungs in ARDS after trauma may be due to a direct pulmonary insult, such as pulmonary contusion or one that is indirect, as in severe sepsis , trauma, shock , and massive blood transfusion. Extracorporeal membrane oxygenation (ECMO) therapy presents a rescue therapy in severe trauma patients with concomitant chest injury suffering from refractory ARDS when conventional therapies have been exhausted [122, 123].
ECMO uses technology derived from cardiopulmonary bypass that allows gas exchange outside the body, circulatory support can also be provided. The first successful report use of ECMO as lifesaving treatment in respiratory failure was introduced by Robert Bartlett in 1972 and revolutionized the treatment of resistant hypoxemia in patients worldwide [124–126].
ECMO has been used for more than 40 years and its benefits in neonates with respiratory distress. The benefits of ECMO in adult patients with cardiac failure or refractory ARDS are still debated, as early studies demonstrated ECMO was initially associated with poor results [127]. However, with technological advances in the ECMO circuit including the use of polymethylpentene membrane oxygenators, centrifugal pumps, miniaturization of circuits, and heparin-bonded circuitry, which have led to a reduction in the rate of technical issues and complications. Moreover, improved understanding of the benefits of ECMO has emerged from its widespread use as a rescue therapy for patients with ARDS and refractory hypoxaemia associated with H1N1 (2009 influenza A). ECMO offers artificial temporary and respiratory support that should be maintained until the patient recovers from severe respiratory failure.
The management of severe ARDS in adult trauma patients presents a great challenge for physicians. In some ways, trauma patients are the ideal patients to undergo ECMO. Trauma patients often have recoverable injuries. Moreover, they are typically young and healthy, with good cardiopulmonary function at baseline [128]. ECMO more frequent considered as a viable treatment option for severe ARDS in the trauma patient. One potential contraindication to ECMO in the trauma population is the increased risk of hemorrhage during its use. However, this issue has recently been challenged, as advancements in ECMO circuits, specifically heparin-bonded systems and shorter circuit lengths, have allowed ECMO use with little or no anticoagulation. Several reports have shown that patients with traumatic intracranial hemorrhage and respiratory failure can be successfully managed on heparin-free ECMO without increasing the size of the lesion [129–131]. If the risk of bleeding is adequately reduced, trauma patients with severe pulmonary failure present an ideal population for treatment with ECMO. Cordell-Smith et al. reported a series showing a survival rate of 71 % in 28 trauma patients treated with ECMO [132]. In the report by Ried M showed that the overall survival rate in patients with required pumpless extracorporeal lung assist and veno-venous ECMO for primary post-traumatic respiratory failure was 79 % compared with the proposed Injury Severity Score-related mortality (59 %) [133]. Extracorporeal lung support (ELS) devices are an excellent and life-saving treatment option in severe thoracic trauma patients with ALF. Thoracic trauma patients with concomitant refractory pulmonary failure have a remarkable potential to recover under ELS. The utilization of the ELS devices was safe and effective in these severe multiple trauma patients. In recent, retrospective analysis of ECMO patients in the Extracorporeal Life Support Organization database, Jacobs JV et al. showed that, outcomes after the use of ECMO in blunt thoracic trauma can be favorable, the rate of survival to discharge was 74.1 % [128].
There is no established standard of care regarding the use of ECMO in patients with blunt thoracic trauma . It would be difficult for any single institution with ECMO capabilities to collect a large number of trauma patients requiring the use of ECMO. Standardizing ECMO therapy and evaluating its efficacy in patients with multiple injuries is also problematic. Further study is needed, and multi-institutional collaboration will be paramount to make progress in this field.
In conclusion, new technology innovation and application significantly change the traditional path and method in treatment of chest trauma. Guidelines for trauma care seek to set achievable standards for trauma treatment services which should constantly update to propose important and evidence-based recommendations regarding chest trauma.
References
DuBose JA, O’Connor JV, Scalea TM. Lung, Trachea, and Esophagus. In: Mattox KL, Moore EE, Feliciano DV, editors. Trauma (eBook). 7th ed. New York: The McGraw-Hill Companies, Inc.; 2013. p. 1118–60.
Smith ZA, Wood D. Emergency focussed assessment with sonography in trauma (FAST) and haemodynamic stability. Emerg Med J. 2014;31(4):273–7.
Kirkpatrick AW, Sirois M, Laupland KB, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the extended focused assessment with sonography for trauma (EFAST). J Trauma. 2004;57(2):288–95.
Knudtson JL, Dort JM, Helmer SD, et al. Surgeon-performed ultrasound for pneumothorax in the trauma suite. J Trauma. 2004;56(3):527–30.
Volpicelli G. Sonographic diagnosis of pneumothorax. Intensive Care Med. 2011;37(2):224–32.
Ding W, Shen Y, Yang J, et al. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest. 2011;140(4):859–66.
Alrajhi K, Woo MY, Vaillancourt C. Test characteristics of ultrasonography for the detection of pneumothorax: a systematic review and meta-analysis. Chest. 2012;141(3):703–8.
Alrajab S, Youssef AM, Akkus NI, et al. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Crit Care. 2013;17(5):R208.
Mattox KL, Wall MJ Jr. Newer diagnostic measures and emergency management. Chest Surg Clin N Am. 1997;7(2):213–26.
Lowdermilk GA, Naunheim KS. Thoracoscopic evaluation and treatment of thoracic trauma. Surg Clin North Am. 2000;80(5):1535–42.
Meyer DM, Jessen ME, Wait MA, et al. Early evacuation of traumatic retained hemothoraces using thoracoscopy: a prospective, randomized trial. Ann Thorac Surg. 1997;64(5):1396–400.
Ben-Nun A, Orlovsky M, Best LA. Video-assisted thoracoscopic surgery in the treatment of chest trauma: long-term benefit. Ann Thorac Surg. 2007;83(2):383–7.
Martins Castello Branco J. Thoracoscopy as a method of exploration in penetrating injuries of the thorax. Dis Chest. 1946;12:330–5.
Jackson AM, Ferreira AA. Thoracoscopy as an aid to the diagnosis of diaphragmatic injury in penetrating wounds of the left lower chest: a preliminary report. Injury. 1976;7(3):213–7.
Jones JW, Kitahama A, Webb WR, et al. Emergency thoracoscopy: a logical approach to chest trauma management. J Trauma. 1981;21(4):280–4.
Ahmed N, Jones D. Video-assisted thoracic surgery: state of the art in trauma care. Injury. 2004;35(5):479–89.
Wu N, Wu L, Qiu C, et al. A comparison of video-assisted thoracoscopic surgery with open thoracotomy for the management of chest trauma: a systematic review and meta-analysis. World J Surg. 2015;39(4):940–52.
Freeman RK, Al-Dossari G, Hutcheson KA, et al. Indications for using video-assisted thoracoscopic surgery to diagnose diaphragmatic injuries after penetrating chest trauma. Ann Thorac Surg. 2001;72(2):342–7.
Pons F, Lang-Lazdunski L, de Kerangal X, et al. The role of videothoracoscopy in management of precordial thoracic penetrating injuries. Eur J Cardiothorac Surg. 2002;22(1):7–12.
Hanvesakul R, Momin A, Gee MJ, et al. A role for video assisted thoracoscopy in stable penetrating chest trauma. Emerg Med J. 2005;22(5):386–7.
Navsaria PH, Vogel RJ, Nicol AJ. Thoracoscopic evacuation of retained posttraumatic hemothorax. Ann Thorac Surg. 2004;78(1):282–5.
Edil BH, Trachte AL, Knott-Craig C, et al. Video-assisted thoracoscopic retrieval of an intrapleural foreign body after penetrating chest trauma. J Trauma. 2007;63(1):E5–6.
Schermer CR, Matteson BD, Demarest GB 3rd, et al. A prospective evaluation of video-assisted thoracic surgery for persistent air leak due to trauma. Am J Surg. 1999;177(6):480–4.
Landreneau RJ, Keenan RJ, Hazelrigg SR, et al. Thoracoscopy for empyema and hemothorax. Chest. 1996;109(1):18–24.
Reddy VS. Minimally invasive techniques in thoracic trauma. Semin Thorac Cardiovasc Surg. 2008;20(1):72–7.
Milanchi S, Makey I, McKenna R, et al. Video-assisted thoracoscopic surgery in the management of penetrating and blunt thoracic trauma. J Minim Access Surg. 2009;5(3):63–6.
Goodman M, Lewis J, Guitron J, et al. Video-assisted thoracoscopic surgery for acute thoracic trauma. J Emerg Trauma Shock. 2013;6(2):106–9.
Heniford BT, Carrillo EH, Spain DA, et al. The role of thoracoscopy in the management of retained thoracic collections after trauma. Ann Thorac Surg. 1997;63(4):940–3.
Smith JW, Franklin GA, Harbrecht BG, et al. Early VATS for blunt chest trauma: a management technique underutilized by acute care surgeons. J Trauma. 2011;71(1):102–5.
Tyburski JG, Astra L, Wilson RF, et al. Factors affecting prognosis with penetrating wounds of the heart. J Trauma. 2000;48(4):587–90.
Morgan BS, Garner JP. Emergency thoracotomy–the indications, contraindications and evidence. J R Army Med Corps. 2009;155(2):87–93.
Tm S. The shock trauma manual of operative techniques. New York: Springer; 2015.
Hunt PA, Greaves I, Owens WA. Emergency thoracotomy in thoracic trauma-a review. Injury. 2006;37(1):1–19.
Simms ER, Flaris AN, Franchino X, et al. Bilateral anterior thoracotomy (clamshell incision) is the ideal emergency thoracotomy incision: an anatomic study. World J Surg. 2013;37(6):1277–85.
Voiglio EJ, Coats TJ, Baudoin YP, et al. Resuscitative transverse thoracotomy. Ann Chir. 2003;128(10):728–33.
Wise D, Davies G, Coats T, et al. Emergency thoracotomy: “how to do it”. Emerg Med J. 2005;22(1):22–4.
Grove CA, Lemmon G, Anderson G, et al. Emergency thoracotomy: appropriate use in the resuscitation of trauma patients. Am Surg. 2002;68(4):313–6.
Khorsandi M, Skouras C, Shah R. Is there any role for resuscitative emergency department thoracotomy in blunt trauma? Interact CardioVasc Thorac Surg. 2013;16(4):509–16.
Powell DW, Moore EE, Cothren CC, et al. Is emergency department resuscitative thoracotomy futile care for the critically injured patient requiring prehospital cardiopulmonary resuscitation? J Am Coll Surg. 2004;199(2):211–5.
Moore EE, Knudson MM, Burlew CC, et al. Defining the limits of resuscitative emergency department thoracotomy: a contemporary Western Trauma Association perspective. J Trauma. 2011;70(2):334–9.
Dayama A, Sugano D, Spielman D, et al. Basic data underlying clinical decision-making and outcomes in emergency department thoracotomy: tabular review. ANZ J Surg. 2016;86(1–2):21–6.
Practice management guidelines for emergency department thoracotomy. Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons-Committee on Trauma. J Am Coll Surg. 2001;193(3):303–9.
Pahle AS, Pedersen BL, Skaga NO, et al. Emergency thoracotomy saves lives in a Scandinavian hospital setting. J Trauma. 2010;68(3):599–603.
Burlew CC, Moore EE, Moore FA, et al. Western Trauma Association critical decisions in trauma: resuscitative thoracotomy. J Trauma Acute Care Surg. 2012;73(6):1359–63.
Codner PA, Brasel KJ. Emergency Department Thoracotomy: an Update. Curr Trauma Rep. 2015;1:212–8.
Molina EJ, Gaughan JP, Kulp H, et al. Outcomes after emergency department thoracotomy for penetrating cardiac injuries: a new perspective. Interact CardioVasc Thorac Surg. 2008;7(5):845–8.
Seamon MJ, Haut ER, Van Arendonk K, et al. An evidence-based approach to patient selection for emergency department thoracotomy: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015;79(1):159–73.
Granetzny A, Abd El-Aal M, Emam E, et al. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact CardioVasc Thorac Surg. 2005;4(6):583–7.
Engel C, Krieg JC, Madey SM, et al. Operative chest wall fixation with osteosynthesis plates. J Trauma. 2005;58(1):181–6.
Dehghan N, de Mestral C, McKee MD, et al. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76(2):462–8.
Ciraulo DL, Elliott D, Mitchell KA, et al. Flail chest as a marker for significant injuries. J Am Coll Surg. 1994;178(5):466–70.
Simon BJ, Cushman J, Barraco R, et al. Pain management guidelines for blunt thoracic trauma. J Trauma. 2005;59(5):1256–67.
Oyarzun JR, Bush AP, McCormick JR, et al. Use of 3.5-mm acetabular reconstruction plates for internal fixation of flail chest injuries. Ann Thorac Surg. 1998;65(5):1471–4.
Lafferty PM, Anavian J, Will RE, et al. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Joint Surg Am. 2011;93(1):97–110.
Simon B, Ebert J, Bokhari F, et al. Management of pulmonary contusion and flail chest: an Eastern Association for the Surgery of Trauma practice management guideline. 2012;73(5 Suppl 4):S351–61.
Nirula R, Diaz JJ Jr, Trunkey DD, et al. Rib fracture repair: indications, technical issues, and future directions. World J Surg. 2009;33(1):14–22.
Ahmed Z, Mohyuddin Z. Management of flail chest injury: internal fixation versus endotracheal intubation and ventilation. J Thorac Cardiovasc Surg. 1995;110(6):1676–80.
Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52(4):727–32.
Duggal A, Perez P, Golan E, et al. Safety and efficacy of noninvasive ventilation in patients with blunt chest trauma: a systematic review. Crit Care. 2013;17(4):R142.
Nirula R, Mayberry JC. Rib fracture fixation: controversies and technical challenges. Am Surg. 2010;76(8):793–802.
Du DY, Su HJ, Tan YK, et al. Comparison between surgical and conservative treatment for flail chest. J Trauma Surg. 2009;11(3):196–9 (in Chinese).
Leinicke JA, Elmore L, Freeman BD, et al. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg. 2013;258(6):914–21.
Slobogean GP, MacPherson CA, Sun T, et al. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg. 2013;216(2):302–11.
Doben AR, Eriksson EA, Denlinger CE, et al. Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J Crit Care. 2014;29(1):139–43.
Marasco SF, Davies AR, Cooper J, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013;216(5):924–32.
Pieracci FM, Lin Y, Rodil M, et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg. 2016;80(2):187–94.
Pieracci FM, Rodil M, Stovall RT, et al. Surgical stabilization of severe rib fractures. J Trauma Acute Care Surg. 2015;78(4):883–7.
Mayberry J. Surgical stabilization of severe rib fractures: several caveats. J Trauma Acute Care Surg. 2015;79(3):515.
Althausen PL, Shannon S, Watts C, et al. Early surgical stabilization of flail chest with locked plate fixation. J Orthop Trauma. 2011;25(11):641–7.
Lardinois D, Krueger T, Dusmet M, et al. Pulmonary function testing after operative stabilisation of the chest wall for flail chest. Eur J Cardiothorac Surg. 2001;20(3):496–501.
Davignon K, Kwo J, Bigatello LM. Pathophysiology and management of the flail chest. Minerva Anestesiol. 2004;70(4):193–9.
Allen GS, Coates NE. Pulmonary contusion: a collective review. Am Surg. 1996;62(11):895–900.
Voggenreiter G, Neudeck F, Aufmkolk M, et al. Operative chest wall stabilization in flail chest–outcomes of patients with or without pulmonary contusion. J Am Coll Surg. 1998;187(2):130–8.
Zhang Y, Tang X, Xie H, et al. Comparison of surgical fixation and nonsurgical management of flail chest and pulmonary contusion. Am J Emerg Med. 2015;33(7):937–40.
Luchette FA, Radafshar SM, Kaiser R, et al. Prospective evaluation of epidural versus intrapleural catheters for analgesia in chest wall trauma. J Trauma. 1994;36(6):865–9.
Bulger EM, Edwards T, Klotz P, et al. Epidural analgesia improves outcome after multiple rib fractures. Surgery. 2004;136(2):426–30.
Nishiumi N, Maitani F, Tsurumi T, et al. Blunt chest trauma with deep pulmonary laceration. Ann Thorac Surg. 2001;71(1):314–8.
Gaer JA, Tsang V, Khaghani A, et al. Use of endotracheal silicone stents for relief of tracheobronchial obstruction. Ann Thorac Surg. 1992;54(3):512–6.
Smith RS. Disruptive technology in the treatment of thoracic trauma. Am J Surg. 2013;206(6):826–33.
Gao JM, Du DY, Yang J, et al. Penetrating chest trauma: analysis of 711 cases. Chin J Trauma. 2003;19(3):187–8 (in Chinese).
Gao JM, Li BC, Zhang K, et al. Management of chest trauma: experience in 666 cases. Chin J Traumatol. 1994;10(2):85–6 (in Chinese).
Wall MJ Jr, Hirshberg A, Mattox KL. Pulmonary tractotomy with selective vascular ligation for penetrating injuries to the lung. Am J Surg. 1994;168(6):665–9.
Petrone P, Asensio JA. Surgical management of penetrating pulmonary injuries. Scand J Trauma Resusc Emerg Med. 2009;17:8.
Tan YK, Kong LW, Du DY, et al. Management standards for traumatic intrapulmonary hematoma and hematocele. Chin J Trauma. 2012;28(7):613–6 (in Chinese).
Velmahos GC, Baker C, Demetriades D, et al. Lung-sparing surgery after penetrating trauma using tractotomy, partial lobectomy, and pneumonorrhaphy. Arch Surg. 1999;134(2):186–9.
Cothren C, Moore EE, Biffl WL, et al. Lung-sparing techniques are associated with improved outcome compared with anatomic resection for severe lung injuries. J Trauma. 2002;53(3):483–7.
Karmy-Jones R, Jurkovich GJ, Shatz DV, et al. Management of traumatic lung injury: a Western Trauma Association Multicenter review. J Trauma. 2001;51(6):1049–53.
Teixeira PG, Inaba K, Barmparas G, et al. Blunt thoracic aortic injuries: an autopsy study. J Trauma. 2011;70(1):197–202.
Bertrand S, Cuny S, Petit P, et al. Traumatic rupture of thoracic aorta in real-world motor vehicle crashes. Traffic Inj Prev. 2008;9(2):153–61.
Burkhart HM, Gomez GA, Jacobson LE, et al. Fatal blunt aortic injuries: a review of 242 autopsy cases. J Trauma. 2001;50(1):113–5.
Demetriades D. Blunt thoracic aortic injuries: crossing the Rubicon. J Am Coll Surg. 2012;214(3):247–59.
Pearson R, Philips N, Hancock R, et al. Regional wall mechanics and blunt traumatic aortic rupture at the isthmus. Eur J Cardiothorac Surg. 2008;34(3):616–22.
Siegel JH, Belwadi A, Smith JA, et al. Analysis of the mechanism of lateral impact aortic isthmus disruption in real-life motor vehicle crashes using a computer-based finite element numeric model: with simulation of prevention strategies. J Trauma. 2010;68(6):1375–95.
Demetriades D, Velmahos GC, Scalea TM, et al. Operative repair or endovascular stent graft in blunt traumatic thoracic aortic injuries: results of an American Association for the Surgery of Trauma Multicenter study. J Trauma. 2008;64(3):561–70.
Mirvis SE, Shanmuganathan K. Diagnosis of blunt traumatic aortic injury 2007: still a nemesis. Eur J Radiol. 2007;64(1):27–40.
Parker MS, Matheson TL, Rao AV, et al. Making the transition: the role of helical CT in the evaluation of potentially acute thoracic aortic injuries. AJR Am J Roentgenol. 2001;176(5):1267–72.
Erbel R, Aboyans V, Boileau C, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The task force for the diagnosis and treatment of aortic diseases of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(41):2873–926.
Neschis DG, Scalea TM, Flinn WR, et al. Blunt aortic injury. N Engl J Med. 2008;359(16):1708–16.
Arjun RH, Goni V, John R, et al. Comment on the case report “bilateral atraumatic tibial tubercle avulsion fractures: case report and review of the literature” published in Injury, Int J Care Injured. 2015;46:767–69. Injury. 2015;46(10):2083.
O’Connor JV, Byrne C, Scalea TM, et al. Vascular injuries after blunt chest trauma: diagnosis and management. Scand J Trauma Resusc Emerg Med. 2009;17:42.
Fabian TC, Richardson JD, Croce MA, et al. Prospective study of blunt aortic injury: Multicenter Trial of the American Association for the Surgery of Trauma. J Trauma. 1997;42(3):374–80.
Hemmila MR, Arbabi S, Rowe SA, et al. Delayed repair for blunt thoracic aortic injury: is it really equivalent to early repair? J Trauma. 2004;56(1):13–23.
Kwolek CJ, Blazick E. Current management of traumatic thoracic aortic injury. Semin Vasc Surg. 2010;23(4):215–20.
Azizzadeh A, Ray HM, Dubose JJ, et al. Outcomes of endovascular repair for patients with blunt traumatic aortic injury. J Trauma Acute Care Surg. 2014;76(2):510–6.
Kato N, Dake MD, Miller DC, et al. Traumatic thoracic aortic aneurysm: treatment with endovascular stent-grafts. Radiology. 1997;205(3):657–62.
Azizzadeh A, Charlton-Ouw KM, Chen Z, et al. An outcome analysis of endovascular versus open repair of blunt traumatic aortic injuries. J Vasc Surg. 2013;57(1):108–14.
Branco BC, DuBose JJ, Zhan LX, et al. Trends and outcomes of endovascular therapy in the management of civilian vascular injuries. J Vasc Surg. 2014;60(5):1297–307, 1307.e1.
Estrera AL, Miller CC 3rd, Guajardo-Salinas G, et al. Update on blunt thoracic aortic injury: fifteen-year single-institution experience. J Thorac Cardiovasc Surg. 2013;145(3 Suppl):S154–8.
Di Eusanio M, Folesani G, Berretta P, et al. Delayed management of blunt traumatic aortic injury: open surgical versus endovascular repair. Ann Thorac Surg. 2013;95(5):1591–7.
Granke K, Hollier LH, Zdrahal P, et al. Longitudinal study of cerebral spinal fluid drainage in polyethylene glycol-conjugated superoxide dismutase in paraplegia associated with thoracic aortic cross-clamping. J Vasc Surg. 1991;13(5):615–21.
Canaud L, Marty-Ane C, Ziza V, et al. Minimum 10-year follow-up of endovascular repair for acute traumatic transection of the thoracic aorta. J Thorac Cardiovasc Surg. 2015;149(3):825–9.
Pang D, Hildebrand D, Bachoo P. Thoracic endovascular repair (TEVAR) versus open surgery for blunt traumatic thoracic aortic injury. Cochrane Database Syst Rev. 2015;9:CD006642.
Neschis DG, Moaine S, Gutta R, et al. Twenty consecutive cases of endograft repair of traumatic aortic disruption: lessons learned. J Vasc Surg. 2007;45(3):487–92.
Idu MM, Reekers JA, Balm R, et al. Collapse of a stent-graft following treatment of a traumatic thoracic aortic rupture. J Endovasc Ther. 2005;12(4):503–7.
Greenberg RK, Clair D, Srivastava S, et al. Should patients with challenging anatomy be offered endovascular aneurysm repair? J Vasc Surg. 2003;38(5):990–6.
Schlosser FJ, Aruny JE, Freiburg CB, et al. The chimney procedure is an emergently available endovascular solution for visceral aortic aneurysm rupture. J Vasc Surg. 2011;53(5):1386–90.
Hogendoorn W, Schlosser FJ, Moll FL, et al. Thoracic endovascular aortic repair with the chimney graft technique. J Vasc Surg. 2013;58(2):502–11.
Lindblad B, Bin Jabr A, Holst J, et al. Chimney grafts in aortic stent grafting: hazardous or useful technique? Systematic review of current data. Eur J Vasc Endovasc Surg. 2015;50(6):722–31.
Taylor MM. ARDS diagnosis and management: implications for the critical care nurse. Dimens Crit Care Nurs. 2005;24(5):197–207.
Rubenfeld GD, Herridge MS. Epidemiology and outcomes of acute lung injury. Chest. 2007;131(2):554–62.
Yuan KC, Fang JF, Chen MF. Treatment of endobronchial hemorrhage after blunt chest trauma with extracorporeal membrane oxygenation (ECMO). J Trauma. 2008;65(5):1151–4.
Huang YK, Liu KS, Lu MS, et al. Extracorporeal life support in post-traumatic respiratory distress patients. Resuscitation. 2009;80(5):535–9.
Arlt M, Philipp A, Voelkel S, et al. Extracorporeal membrane oxygenation in severe trauma patients with bleeding shock. 2010;81(7):804–9.
Bartlett RH, Gazzaniga AB, Jefferies MR, et al. Extracorporeal membrane oxygenation (ECMO) cardiopulmonary support in infancy. Trans Am Soc Artif Intern Organs. 1976;22:80–93.
Arlt M, Philipp A, Zimmermann M, et al. First experiences with a new miniaturised life support system for mobile percutaneous cardiopulmonary bypass. Resuscitation. 2008;77(3):345–50.
Arlt M, Philipp A, Zimmermann M, et al. Emergency use of extracorporeal membrane oxygenation in cardiopulmonary failure. Artif Organs. 2009;33(9):696–703.
Morris AH, Wallace CJ, Menlove RL, et al. Randomized clinical trial of pressure-controlled inverse ratio ventilation and extracorporeal CO2 removal for adult respiratory distress syndrome. Am J Respir Crit Care Med. 1994;149(2 Pt 1):295–305.
Jacobs JV, Hooft NM, Robinson BR, et al. The use of extracorporeal membrane oxygenation in blunt thoracic trauma: a study of the Extracorporeal Life Support Organization database. J Trauma Acute Care Surg. 2015;79(6):1049–54.
Reynolds HN, Cottingham C, McCunn M, et al. Extracorporeal lung support in a patient with traumatic brain injury: the benefit of heparin-bonded circuitry. Perfusion. 1999;14(6):489–93.
Muellenbach RM, Kredel M, Kunze E, et al. Prolonged heparin-free extracorporeal membrane oxygenation in multiple injured acute respiratory distress syndrome patients with traumatic brain injury. J Trauma Acute Care Surg. 2012;72(5):1444–7.
Yen TS, Liau CC, Chen YS, et al. Extracorporeal membrane oxygenation resuscitation for traumatic brain injury after decompressive craniotomy. Clin Neurol Neurosurg. 2008;110(3):295–7.
Cordell-Smith JA, Roberts N, Peek GJ, et al. Traumatic lung injury treated by extracorporeal membrane oxygenation (ECMO). Injury. 2006;37(1):29–32.
Ried M, Bein T, Philipp A, et al. Extracorporeal lung support in trauma patients with severe chest injury and acute lung failure: a 10-year institutional experience. Crit Care. 2013;17(3):R110.
Acknowledgments
This work was financially supported by the Nature Science Foundation of Chongqing Municipality (Grant No. 2012jjB10021), the Medical Science Research Foundation of Chongqing Health Bureau (Grant No. 2010-1-52).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Du, D. (2017). Advances in the Management of Thoracic Trauma. In: Fu, X., Liu, L. (eds) Advanced Trauma and Surgery. Springer, Singapore. https://doi.org/10.1007/978-981-10-2425-2_3
Download citation
DOI: https://doi.org/10.1007/978-981-10-2425-2_3
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-2424-5
Online ISBN: 978-981-10-2425-2
eBook Packages: MedicineMedicine (R0)