Abstract
Background
This study aimed to systematically review and compare the perioperative outcomes of video-assisted thoracoscopy (VATS) with open thoracotomy for chest trauma patients.
Methods
We conducted a systematic review and meta-analysis of randomized control trials and cohort studies comparing the perioperative outcomes of VATS with open thoracotomy for chest trauma patients. Clinical endpoints included postoperative complications, perioperative mortality rate, chest tube drainage volume, duration of tube drainage, duration of hospitalization, operation time, and amount of bleeding and transfusion volume in operation. A subgroup analysis was performed to explore the potential source of heterogeneity.
Results
Twenty-six studies were included. Pooled analyses showed significant reductions in the incidence of postoperative complications (risk ratio [RR] [95 % confidence interval (CI)], 0.47 [0.35, 0.64]), chest tube drainage volume (mean difference [MD] [95 % CI], −146.88 ml [−196.04, −97.72]), duration of tube drainage (MD, −1.71 days; 95 % CI −2.16 to −1.26), duration of hospitalization (MD, −4.67 days; 95 % CI −5.19 to−4.14), operation time (MD, −41.18 min; 95 % CI −52.85 to −29.51), and amount of bleeding (MD, −119.10 ml; 95 % CI −147.28 to −90.92) and transfusion volume (MD, −379.51 ml; 95 % CI −521.24 to−237.77) in chest trauma patients treated with VATS compared with open thoracotomy. The perioperative mortality rate was not significantly different between patients received VATS and open thoracotomy (RR, 0.52; 95 % CI 0.22–1.21).
Conclusions
Compared to open thoracotomy, VATS is an effective and even better treatment for improving perioperative outcomes of hemodynamically stable patients with chest trauma and reduce the complications. However, caution should also be exercised in certain clinical scenarios.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trauma is the leading cause of death in people aged under 45 worldwide, causing over 15 million deaths per year [1–3]. The morbidity rate of chest trauma in all trauma victims is about 25.2 % [4] and represents 25 % of all fatalities of trauma [5]. A retrospective review of 888 cases indicated that 5.7 % of chest trauma patients required thoracotomy [6]. Although the majority of hemodynamically stable patients with chest trauma can initially be treated with tube thoracostomy, it may be ineffective, leading to an increased risk of conversion to open thoracotomy or a prolonged duration of hospitalization [7]. Open thoracotomy is one of the major surgical maneuvers, but its large incisions have been labeled as the most morbid of surgical incisions and are usually associated with a long and painful recovery.
Since 1946, thoracoscopy has been used as a method of exploration in the cases with chest trauma [8]. In 1981, thoracoscopy has been proved to be a valuable diagnostic and therapeutic measure in patients with chest trauma [9, 10]. Due to the potential advantages of small incisions and less pain, video-assisted thoracoscopy (VATS) becomes increasingly popular in both diagnosis and treatment of trauma in the 1990s [11–13]. Furthermore, minithoracotomy with simultaneous video-assisted thoracoscopy (VAMT) has been proposed. Its procedure is similar to conventional VATS, but the minimal incision wounds for introduction of instruments into the chest are replaced by one muscle-sparing minithoracotomy for quick and complete removal of blood clot [14, 15].
In addition to smaller incision and less pain, perioperative outcomes such as effectiveness, postoperative complications, perioperative mortality, and duration of hospitalization for VATS seem to be superior to open thoracotomy in treating chest trauma [7, 16–18]. However, most of the studies comparing VATS with open thoracotomy in patients with chest trauma are case reports or case series with limited number of patients. Recently, some randomized controlled clinical trials (RCT) and cohort studies have been published. However, several studies reported that VATS caused some adverse effects such as pneumonias, atelectasis, and iatrogenic diaphragmatic hernia [2, 19], making the results of previous studies inconsistent. Therefore, these studies need to be systematically analyzed. In addition, most of these studies had a small sample size in a single institution. A meta-analysis overcomes the limitation of small sample sizes of individual studies and increases the numbers of observations and the statistical power. We therefore conducted a systematic review and meta-analysis to compare the perioperative outcomes of patients with chest trauma receiving VATS with those underwent open thoracotomy.
Materials and methods
Search strategy
The meta-analysis was performed using the guidelines presented in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [20, 21]. Electronic database and manual searches were used to identify relevant studies. We systematically searched the PubMed, EMBASE, Web of Science, and Chinese Biomedical Literature database (CBM) for studies published up to December 2013 using a web-based search engine. Search terms were “thoracoscopy” or “thoracoscopic surgery,” “video-assisted thoracoscopic surgery” or “VATS,” “traumas,” “posttraumatic,” “traumatic,” “injuries,” and “wounds.” We also manually searched the journals known to publish data relevant to our search. The literature retrieval was performed in duplication by two independent reviewers (N.W. and L.W.). There was no restriction on publication language.
Selection of studies
Human studies, regardless of sample size, were included if they met the following criteria: (1) the studies compared the outcomes of VATS or VAMT with open thoracotomy in treating patients with chest trauma; (2) the study design was a cohort study or RCT. When multiple publications were based on the same or overlapping data, we used the most recent or largest population.
Quality assessment
Quality assessment of studies was conducted by two reviewers independently (N.W. and C.Q.). The quality of cohort studies was assessed based on the Newcastle–Ottawa criteria [22]. A “score system” was developed based on the Newcastle–Ottawa criteria (Supplementary Table 1). The total scores ranged from 0 (worst) to 9 (best) for cohort studies. The quality of RCT studies was assessed using the Cochrane Collaboration’s risk of bias assessment tool; selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), and reporting bias (selective outcome reporting) were evaluated for each study [23]. Each criterion for the bias risk was assessed as low, high, or uncertain risk. Any disagreements were discussed by two reviewers (J.J. and Y.L.).
Data extraction
Data extraction was performed independently by two reviewers (N.W. and L.W.) using a standardized data extraction form. First author’s name, publication year, demographics, patients’ characteristics, indications for VATS, and outcome information were extracted from each study. The numbers of patients with postoperative complications or perioperative mortality, and the means and standard deviations (SDs) of continuous variables in each group were also extracted. Any disagreements were discussed to reach a consensus.
Statistical analysis
We used the pooled risk ratio (RR) as a summary statistic to estimate the relative risk of postoperative complications and perioperative mortality after VATS compared with open thoracotomy. The mean difference (MD) was used as a summary statistic of continuous variables including chest tube drainage volume, duration of tube drainage, duration of hospitalization, operation time, and amount of bleeding and transfusion volume in operation. Statistical heterogeneity was tested using χ 2 test and the I 2 statistic. An I 2 ≥ 50 % indicated a significant heterogeneity between studies, and meta-analyses were conducted using a random effects model. An I 2 < 50 % suggested that the heterogeneity might be accepted, and a fixed effects model was applied. Subgroup analyses were performed to explore the potential source of heterogeneity from study design and subtypes of chest trauma. We evaluated the potential publication bias using Begg’s test [24]. All of the statistical analyses were conducted using RevMan 5.2 software (Cochrane Collaboration, RevMan software, Oxford, UK).
Results
Qualitative analysis
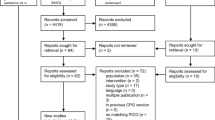
We identified a total of 2,132 potentially relevant studies. After reviewing the titles, abstracts, and full text, 26 studies [17, 25–49] met the study inclusion criteria and were included for the final analysis (Supplementary Fig. 1). The characteristics of the included studies were extracted (Table 1). Five studies were on VAMT, and 21 studies were on VATS. The type of chest trauma mainly involved in pneumothorax, hemothorax, rib fractures, lung contusion, diaphragm injury, and cardiac injury. The indications for VATS included hemostasis of bleeders, evacuation of clotted hemothorax, repair of lung laceration, wedge lung resection, repair of diaphragmatic laceration, removal of foreign body, widening of pericardial lacerations, decortication of empyema, and control of air leak.
Most studies indicated that injury severity and characteristics between two groups were comparable. The majority of studies included patients with multiple injuries involving both penetrating and blunt trauma. The investigated outcomes involved postoperative complications, perioperative mortality rate, tube drainage, duration of tube drainage, duration of hospitalization, operation time, and amount of bleeding in operation.
There were 14 cohort studies and 12 RCTs. For quality score of cohort studies, one study scored 6, two studies scored 7, and the others scored 8 (Supplementary Table 2). The risk of bias for each RCT was assessed, as shown in Supplementary Table 3. Most of RCTs did not report the detailed information about the methods of random sequence generation and allocation concealment.
Meta-analysis
Thirteen cohort studies and ten RCTs with adequate data were included in the meta-analysis (Table 1). The risk of postoperative complications in patients treated with VATS was significantly lower than that of patients who underwent open thoracotomy with a pooled RR of 0.47 (95 % CI 0.35–0.64; P < 0.001) (Fig. 1). The subgroup analysis showed consistent result between RCTs (RR, 0.34; 95 % CI 0.16–0.75; P = 0.007) and cohort studies (RR, 0.52; 95 % CI 0.37–0.72; P < 0.001) (Table 2).
Comparison of risk of postoperative complications of VATS with open thoracotomy in treating patients with chest trauma. Forest plots of RR and overall RR with 95 % CI between group of VATS and group of open thoracotomy. Blue square indicates the RR, with the size of the square inversely proportional to its variance, and horizontal lines represent 95 % CI. The pooled results are indicated by the black diamond. VATS video-assisted thoracoscopy, RR risk ratio, CI confidence interval
The perioperative mortality rate was not significantly different between the two groups with a pooled RR of 0.52 (95 % CI 0.22–1.21; P = 0.13) (Fig. 2). Consistent results were observed in RCTs (RR, 0.82; 95 % CI 0.22–2.99; P = 0.76) and cohort studies (RR, 0.39; 95 % CI 0.12–1.21; P = 0.10) (Table 2).
Comparison of perioperative mortality rate of VATS with open thoracotomy in treating patients with chest trauma. Forest plots of RR and overall RR with 95 % CI between group of VATS and group of open thoracotomy. Blue square indicates the RR, with the size of the square inversely proportional to its variance, and horizontal lines represent 95 % CI. The pooled results are indicated by the black diamond. VATS video-assisted thoracoscopy, RR risk ratio, CI confidence interval
Chest tube drainage volume and amount of bleeding and transfusion volume in operation were found significantly lower in patients with VATS compared to open thoracotomy with pooled MD −146.88 ml (95 % CI −196.04 to −97.72; P < 0.001), −119.10 ml (95 % CI −147.28 to −90.92; P < 0.001), and −379.51 ml (95 % CI −521.24 to −237.77; P < 0.001), respectively (Figs. 3, 4, 5). The duration of tube drainage, hospitalization, and operation time were significantly shorter in patients with VATS with pooled MD −1.71 days (95 % CI −2.16 to −1.26; P < 0.001), −4.67 days (95 % CI −5.19 to −4.14; P < 0.001), and −41.18 min (95 % CI −52.85 to −29.51; P < 0.001), respectively (Figs. 6, 7, 8). Consistent results were also found in both RCT and cohort studies for chest tube drainage volume, amount of bleeding, transfusion volume, and duration of tube drainage, hospitalization, and operation time (Table 2).
Comparison of chest tube drainage volume of VATS with open thoracotomy in treating patients with chest trauma. Forest plots of MD and overall MD with 95 % CI between group of VATS and group of open thoracotomy. Green square indicates the MD, with the size of the square inversely proportional to its variance, and horizontal lines represent 95 % CI. The pooled results are indicated by the black diamond. VATS video-assisted thoracoscopy, MD mean difference; CI confidence interval
Comparison of amount of bleeding of VATS with open thoracotomy in treating patients with chest trauma. Forest plots of MD and overall MD with 95 % CI between group of VATS and group of open thoracotomy. Green square indicates the MD, with the size of the square inversely proportional to its variance, and horizontal lines represent 95 % CI. The pooled results are indicated by the black diamond. VATS video-assisted thoracoscopy, MD mean difference, CI confidence interval
Comparison of transfusion volume of VATS with open thoracotomy in treating patients with chest trauma. Forest plots of MD and overall MD with 95 % CI between group of VATS and group of open thoracotomy. Green square indicates the MD, with the size of the square inversely proportional to its variance, and horizontal lines represent 95 % CI. The pooled results are indicated by the black diamond. VATS video-assisted thoracoscopy, MD mean difference, CI confidence interval
Comparison of duration of tube drainage of VATS with open thoracotomy in treating patients with chest trauma. Forest plots of MD and overall MD with 95 % CI between group of VATS and group of open thoracotomy. Green square indicates the MD, with the size of the square inversely proportional to its variance, and horizontal lines represent 95 % CI. The pooled results are indicated by the black diamond. VATS video-assisted thoracoscopy, MD mean difference, CI confidence interval
Comparison of duration of hospitalization of VATS with open thoracotomy in treating patients with chest trauma. Forest plots of MD and overall MD with 95 % CI between group of VATS and group of open thoracotomy. Green square indicates the MD, with the size of the square inversely proportional to its variance, and horizontal lines represent 95 % CI. The pooled results are indicated by the black diamond. VATS video-assisted thoracoscopy, MD mean difference, CI confidence interval
Comparison of operation time of VATS with open thoracotomy in treating patients with chest trauma. Forest plots of MD and overall MD with 95 % CI between group of VATS and group of open thoracotomy. Green square indicates the MD, with the size of the square inversely proportional to its variance, and horizontal lines represent 95 % CI. The pooled results are indicated by the black diamond. VATS video-assisted thoracoscopy, MD mean difference, CI confidence interval
Since there were different subtypes of chest trauma, we also performed a subgroup analysis of patients with traumatic hemothoraces and pneumothoraces. Results demonstrated that the perioperative outcomes of VATS group were significantly superior to open thoracotomy group for treating traumatic hemothoraces and pneumothoraces; VATS group had a lower risk of postoperative complications, smaller chest tube drainage volume, and amount of bleeding, and shorter duration of tube drainage, hospitalization, and operation time (Table 3).
Considering VAMT as a special type of VATS, a subgroup analysis was also conducted by VAMT and VATS. Lower perioperative mortality rate, smaller chest tube drainage volume, amount of bleeding and transfusion volume in operation, and shorter hospitalization and operation time were observed in patients who underwent VATS or VAMT compared with those who underwent open thoracotomy (Table 4).
There was no significant heterogeneity for studies investigating the risk of postoperative complications and perioperative mortality with I 2 = 0 % (Figs. 1, 2). However, significant heterogeneity was observed among studies on chest tube drainage volume, duration of tube drainage, duration of hospitalization, operation time, and amount of bleeding and transfusion volume in operation with I 2 values above 90 %. Heterogeneity was markedly reduced after grouping by study design, subtype of chest trauma, and operation method (Figs. 3, 4, 5, 6, 7, 8).
Discussion
This systematic review and meta-analysis explored whether the perioperative outcomes of VATS in treatment of patients with proper indications of chest trauma were superior to conventional open thoracotomy treatments. Our results suggested that VATS could significantly reduce the risk of postoperative complications, chest tube drainage volume, duration of tube drainage, duration of hospitalization, operation time, and amount of bleeding and transfusion volume in operation in the management of chest trauma. Subgroup analysis indicated that both VAMT (visualization through the incision) and VATS (visualization only through a monitor) were significantly superior to open thoracotomy.
A previous systematic review demonstrated that VATS was useful in the treatment of retained hemothoraces and persistent pneumothoraces which were two major subtypes of chest trauma, and it was able to reduce associated complications [2, 50]. However, meta-analysis was not performed in this study and the majority of included studies were case series. Up to now, there is no meta-analysis comparing the perioperative outcomes of patients who underwent VATS with those who underwent open thoracotomy. Our study for the first time provided quantitatively synthetical evidence on this issue.
For primary outcomes in our study, perioperative mortality rate was not significantly different between VATS group and conventional open thoracotomy group, verifying the safety of VATS. Infection of wound or thoracic cavity, atelectasis, and pneumonia were common postoperative complications of VATS and open thoracotomy. Our results indicated a lower rate of postoperative complications in group of VATS than open thoracotomy. For secondary outcomes, VATS could significantly reduce duration of tube drainage and hospitalization. Although the procedure of VATS costs more than open thoracotomy and VATS once had been considered as a luxury tool in the armamentarium of the trauma team, in fact, the total cost of hospitalization might be even lower for patients who underwent VATS due to the reduced duration of drainage and hospitalization. VATS had already been shown to decrease hospital length of stay and cost when compared with tube thoracostomy in patients with blunt chest trauma [51]. VATS was increasingly accepted mainly due to the potential benefits of small wounds and less pain to patients [52]. In our study, only two studies evaluated pain intensity [30, 47] and length of incision [34, 36], respectively, so meta-analysis was not performed on these two issues. But these studies showed that mean score of Visual Analog Scale was significantly lower [30, 47] and length of incision was significantly shorter for VATS [34, 36]. Our meta-analysis also demonstrated that the amount of bleeding, transfusion volume during operation, and the total operation time were smaller or shorter for VATS, suggesting smaller wounds and smoother process.
VATS was recommended for a variety of therapeutic purposes following chest trauma. In our study, we found that VATS was mostly applied to chest trauma cases involving hemostasis of bleeders, evacuation of clotted hemothorax, repair of lung laceration, wedge lung resection, repair of diaphragmatic laceration, and control of air leak. Removal of foreign body, widening of pericardial lacerations and decortication of empyema were also applied. Manlulu AV et al. investigated the current indications of VATS in 2004 [13]. Compared with our results, these indications seemed not to change much during the last ten years. Most of the included studies in our systematic review indicated that in spite of the superior perioperative outcomes of VATS, surgeons should bear in mind that the application of VATS was conditional. Contraindications to VATS included obliterated pleural spaces, inability to tolerate single-lung ventilation, hemodynamic instability, circulatory shock, and life-threatening thoracic injury. Procedure of VATS required experienced surgeons, anesthetists, and nurses. The optimal timing for performing VATS and its effects on outcomes were not clearly understood. However, none of the studies in our systematic review investigated the timing of VATS. The majority of previous reports advocated the early use of VATS within 5 days after trauma and more operative difficulties in patients if VATS was performed at a later time point [2].
We conducted a critical quality assessment for each included study. All cohort studies scored at least 6, suggesting that all of them had moderate or high quality. However, the original RCTs had uneven quality. The vast majority of included RCT studies had a low risk on performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), and reporting bias (selective reporting). However, most of the included RCTs did not report the detailed information about methods of random sequence generation and allocation concealment. When randomization is not strictly carried out, characteristics of participants may not be comparable between two groups; bias may be introduced and may affect the reliability of the results. Thus, more high-quality RCTs are warranted in this field.
We need to acknowledge other limitations in this study. Firstly, the majority of included studies came from a single institution, and the number of participants in each study was limited. Only one study had more than 100 patients undergoing VATS. Secondly, most of the studies were from China, indicating VATS enjoyed great popularity in Chinese hospitals, but this limited the generalizability of our conclusion. More multi-center RCTs involving different counties are needed. Thirdly, VATS and open thoracotomy have different indications. The majority of patients suffered multiple injuries including both penetrating and blunt injury trauma. Injury severity might affect the eligibility for receiving VATS or thoracotomy and the outcomes of operation. Other factors such as age, sex, and medical history might also play a part. Although the majority of the cohort studies had reported that injury severity, age, and gender were comparable between two groups, other known and unknown confounding factors might introduce the bias. Included RCTs with poor randomization could not guarantee the comparability between two groups. High-quality RCTs with appropriate randomization can make up for this limitation in future studies.
In conclusion, our meta-analysis demonstrated that VATS was effective and superior for treatment of appropriate chest trauma than conventional open thoracotomy. But caution should also be exercised in certain clinical scenarios. Furthermore, well-designed, multi-center RCTs with large simple sizes need to be conducted to compare the efficacy of VATS with thoracotomy and identify the best indicators for VATS or VAMT treatment.
References
Injury prevention & control: data & statistics (WISQARS(TM)). http://www.cdc.gov/injury/wisqars/leading_causes_death.html. Center for Disease Control and Prevention, Accessed 28 Nov 2013
Billeter AT, Druen D, Franklin GA et al (2013) Video-assisted thoracoscopy as an important tool for trauma surgeons: a systematic review. Langenbecks Arch Surg 398:515–523
A leading cause of death and disability in China. http://www.wpro.who.int/china/sites/injury_prevention. Accessed 12 Jan 2013
Demirhan R, Onan B, Oz K et al (2009) Comprehensive analysis of 4,205 patients with chest trauma: a 10-year experience. Interact CardioVasc Thorac Surg 9:450–453
Ziegler DW, Agarwal NN (1994) The morbidity and mortality of rib fractures. J Trauma 37:975–979
Al-Koudmani I, Darwish B, Al-Kateb K et al (2012) Chest trauma experience over eleven-year period at al-mouassat university teaching hospital-Damascus: a retrospective review of 888 cases. J Cardiothorac Surg 7:35
Meyer DM, Jessen ME, Wait MA et al (1997) Early evacuation of traumatic retained hemothoraces using thoracoscopy: a prospective, randomized trial. Ann Thorac Surg 64:1396–1400
Martins Castello Branco J (1946) Thoracoscopy as a method of exploration in penetrating injuries of the thorax. Dis Chest 12:330–335
Jones JW, Kitahama A, Webb WR et al (1981) Emergency thoracoscopy: a logical approach to chest trauma management. J Trauma 21:280–284
Ahmed N, Jones D (2004) Video-assisted thoracic surgery: state of the art in trauma care. Injury 35:479–489
Bagheri R, Tavassoli A, Sadrizadeh A et al (2009) The role of thoracoscopy for the diagnosis of hidden diaphragmatic injuries in penetrating thoracoabdominal trauma. Interact CardioVasc Thorac Surg 9:195–197
Uribe RA, Pachon CE, Frame SB et al (1994) A prospective evaluation of thoracoscopy for the diagnosis of penetrating thoracoabdominal trauma. J Trauma 37:650–654
Manlulu AV, Lee TW, Thung KH et al (2004) Current indications and results of VATS in the evaluation and management of hemodynamically stable thoracic injuries. Eur J Cardiothorac Surg 25:1048–1053
Hsiao CW, Lee SC, Tzao C et al (2003) Minithoracotomy with simultaneous video-assisted thoracoscopic surgery vs. video-assisted thoracoscopic surgery for spontaneous hemopneumothorax. Thorac Cardiovasc Surg 51:288–290
Hsiao C-W, Tzao C, Lee S-C et al (2003) Video-assisted thoracoscopic surgery with simultaneous minithoracotomy for spontaneous hemopneumothorax. J Med Sci Taipei 23:191–194
Ahmed N, Chung R (2010) Role of early thoracoscopy for management of penetrating wounds of the chest. Am Surg 76:1236–1239
Ben-Nun A, Orlovsky M, Best LA (2007) Video-assisted thoracoscopic surgery in the treatment of chest trauma: long-term benefit. Ann Thorac Surg 83:383–387
Fabbrucci P, Nocentini L, Secci S et al (2008) Video-assisted thoracoscopy in the early diagnosis and management of post-traumatic pneumothorax and hemothorax. Surg Endosc 22:1227–1231
Fukami T, Konoeda C, Kitano K et al (2010) Iatrogenic diaphragmatic hernia following partial resection of the lung via video-assisted thoracoscopy. Kyobu Geka 63:1151–1154 (in Japanese)
Moher D, Liberati A, Tetzlaff J et al (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34
Wells G, Shea B, O’Connell D et al (2011) The Newcastle–Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses, http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 20 Nov 2013
Higgins J, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343: d5928
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Long C (2010) A comparison of the effectiveness of minithoracotomy with simultaneous video-assisted thoracoscopy with open thoracotomy. Chin Med Treat 29:72 (in Chinese)
Jiang J, Li G, Zhang Y et al (2010) Clinical observation of IL-2 and WBC/HB of patients with thoracic trauma after thoracoscopy. Mod Hosp 10:58–60 (in Chinese)
Li F, Zhou Q, Zhang Z (2009) Controlled clinical trial of video-assisted thoracoscopic surgery in treating chest trauma. Acta Acad Med Zunyi 32:460–461 (in Chinese)
Peng Y, Yuan S (2008) Analysis of effectiveness of video-assisted thoracoscopic surgery in treating 64 patients with chest trauma. Shandong Med 48:44 (in Chinese)
Li G, Zhang Y, Jiang J et al (2008) Profiles of IL-2 and IL-10 in chest trauma before and after treated with video-assisted thoracoscopic surgery. Acad J Guangzhou Med Coll 36:16–19 (in Chinese)
Liao F, Ye G, Gu W et al (2012) The application of video-assisted thoracoscopic in thoracic trauma. Lingnan Emerg Med 17:276–278 (in Chinese)
Zhao Q (2010) To compare the clinical effect of video-assisted thoracoscopic surgery and conventional lobectomy surgery in treating of chest trauma. Chin Pract Med 33:32–33 (in Chinese)
Cao Y, Zong S, Yang Q (2011) Comparison of effectiveness of minithoracotomy with simultaneous video-assisted thoracoscopy with open thoracotomy. Chin Rehabil Med 2:120 (in Chinese)
Lian A (2008) Clinical study of vedio-assisted thoracoscic in treating of chest trauma. Med Inf 21:1573–1575 (in Chinese)
Xie X, Wu W, Long J (2009) Comparative study of minithoracotomy with simultaneous video-assisted thoracoscopy in treating chest trauma. J Taishan Med Coll 30:706–707 (in Chinese)
Hao Q, Wen Y, Wan B et al (2010) Efficacy of video-assisted thoracoscopy in the treatment of traumatic hemothoraces. Asia-Pac Trad Med 6:70–71 (in Chinese)
Li X, Xu R, Wang Q et al (2012) Comparative study of video-assisted mini-thoracotomy and traditional thoracotomy in the treatment of traumatic hemopneumothorax. J Yanan Univ (Med Sci) 2:24–26 (in Chinese)
Yuan K (2012) Comparative efficacy of traditional thoracotomy and thoracoscopy assisted small incision in the treatment of chest trauma. Sichuan Med J 33:1760–1761 (in Chinese)
Liu W, Yu C (2012) Research of video-assisted thoracoscopic operation diagnosis and treatment value of traumatic hemopneumothorax. J Chin Med Pract 16:69–71 (in Chinese)
Yang L (2012) Comparison of the efficacy and nursing of video-assisted thoracoscopic with open thoracotomy for the treatment of traumatic hemothoraces. Chin Med Res 10:95–96 (in Chinese)
Hu W, Chen S, Wang F (2009) Comparison between traditional thoracotomy and video-assisted thoracoscopy for traumatic hemothorax. Chin Pract Med 4:37–38 (in Chinese)
Chen J (2013) Effect of TV laparoscopy in the diagnosis and treatment of traumatic hemopneumothorax. Clin Lung J 18:480–490 (in Chinese)
Lu H, Wu D, Lin L (2011) Value of video-assisted thoracoscopic in the treatment of traumatic hemothoraces. Zhejiang Trau Surg 16:806–807 (in Chinese)
Lu T, Zheng S (2013) Comparison of the effectiveness of video-assisted thoracoscopic with open thoracotomy for the treatment of traumatic hemothoraces. Chin J Prim Med Pharm 6:910–911 (in Chinese)
Wang Y, Yong H, Zhang X (2011) To compare the clinical effect of video-assisted thoracoscopic surgery and conventional lobectomy surgery in treatment of chest trauma. Ningxia Med J 2011:1180–1182 (in Chinese)
Yu X, Jiang Z, Zheng W et al (2012) Comparison between video-assisted and open thoracoscopic surgeries for traumatic hemopneumothorax. Chin J Min Inv Surg 12:1110–1112 (in Chinese)
Yu H, Li S, Zhao J et al (2013) Comparison of video-assisted thoracoscopic with open thoracotomy for treating traumatic hemothoraces and pneumothoraces. Chin J Clin Thorac Cardiovasc Surg 1:116–118 (in Chinese)
Li Y (2012) Comparative study of video-assisted thoracoscopic surgery and conventional surgical thoracotomy in treatment of post-traumatic hemothorax. Chin Med Sci 2:251–252 (in Chinese)
Huang S, Li Z, Chen L et al (2012) Analysis of video-assisted thoracoscopic in treating 50 patients with traumatic diaphragmatic hernia. Chin Med 10:150–151 (in Chinese)
Samiatina D, Rubikas R (2004) Video-assisted thoracoscopic surgery as an alternative to urgent thoracotomy following open chest trauma in selected cases. Medicina (Kaunas) 40(Suppl 1):134–138 (in Lithuanian)
Morrison CA, Lee TC, Wall MJ Jr et al (2009) Use of a trauma service clinical pathway to improve patient outcomes for retained traumatic hemothorax. World J Surg 33:1851–1856. doi:10.1007/s00268-009-0141-0
Smith JW, Franklin GA, Harbrecht BG et al (2011) Early VATS for blunt chest trauma: a management technique underutilized by acute care surgeons. J Trauma 71:102–105
Villavicencio RT, Aucar JA, Wall MJ Jr (1999) Analysis of thoracoscopy in trauma. Surg Endosc 13:3–9
Acknowledgments
This work was supported by the Special Project Fund of Health Research from National Health and Family Planning Commission, China (No. 201302016).
Disclosures
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Na Wu and Long Wu have contributed equally to this work and co-first authors.
Jun Jiang and Yafei Li have jointly directed the project.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, N., Wu, L., Qiu, C. et al. A comparison of Video-Assisted Thoracoscopic Surgery with Open Thoracotomy for the Management of Chest Trauma: A Systematic Review and Meta-analysis. World J Surg 39, 940–952 (2015). https://doi.org/10.1007/s00268-014-2900-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2900-9