Abstract
Mesenchymal stem cells (MSCs) are a group of heterogeneous non-hematopoietic cells with self-renewal and multi-lineage differentiation potential, and have been widely used for cell-based therapies. While the mechanisms for the beneficial effects of MSCs on tissue repair and regeneration are complex and not fully understood, paracrine signaling is believed to be at least partially responsible for their therapeutic benefits. MSCs express and secret a large number of paracrine factors with a wide spectrum of biological functions including cell proliferation, differentiation, migration, anti-apoptosis, metabolism, immunomodulation, anti-inflammation, angiogenesis, and tissue remodeling. The regulation on the expression and production of the paracrine factors and related signaling molecules in MSCs are complex, and involves a variety of signaling pathways including Akt, STAT-3, p38 MAPK, and TNF receptors. The paracrine function of MSCs is closely associated with the species, age, and gender of the sources, and environmental factors like hypoxia, as well as the presence of stimuli such as tumor necrosis factor. Some disease conditions especially diabetes mellitus have significant impact on paracrine signaling of MSCs. Significant challenges remain on understanding how paracrine mechanisms work on the target tissues of MSCs, and how to design a therapeutic regimen with different paracrine factors to achieve an optimal outcome for tissue protection and regeneration.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
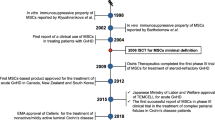
Cell therapy with stem cells remains a viable and attractive option for tissue repair and regeneration after injuries including myocardial infarction, stroke, and wound healing [21, 33, 52]. Mesenchymal stem cells (MSCs) are a group of heterogeneous non-hematopoietic cells that were first identified and isolated from the bone marrow in 1960s by Friedenstein and colleagues, and exhibit proliferative and self-renewal potential, and are able to differentiate into multilineage cell types of endodermal, ectodermal, and mesodermal origins including (but not limited to) osteocytes, chondrocytes, endothelial cells, adipocytes, myocytes, cardiomyocytes, neuron, and hepatocytes [36]. Over the past two decades, a number of cell populations with similar characteristics and multilineage differentiation potential have been successfully identified and characterized in many other adult and fetal tissues in addition to bone marrow, including (but not limited to) skin, dental pulp, adipose tissue, synovium, muscle, tonsil, brain, lung tissue, kidney, umbilical cord blood, peripheral blood, and placenta [38, 52]. MSC has been used to describe almost all the progenitor cells with multipotent differentiation potentials from these parenchymal nonhematopoietic tissues. Although there are currently no unique markers to exclusively identify and characterize MSCs or their subpopulation phenotypically, these cells are expected to express at least the stromal markers CD73 and CD105 without expression of the hematopoietic markers CD14, CD34, and CD45 based on the minimal criteria established by the International Society of Cellular Therapy on the nomenclature and definition of the adult tissue-derived undifferentiated progenitor cells with extended proliferative capability and multilineage differentiation potential [5, 12, 36].
Bone marrow-derived mesenchymal stem cells (BM-MSCs) are an attractive and ideal source for cell-based therapy due to the fact that these cells can be easily obtained without ethical concerns, and conveniently expanded ex vivo to clinical scales in a relatively short period of time with minimal loss of potency, and have little (if any) inherent immunogenicity for any adverse immune reactions (even in the setting of xenogeneic transplantation of MSCs) because of their immunosuppressive and/or immunomodulatory properties [4, 7, 36]. Therefore, in this focused review our efforts will be mainly directed to discuss the beneficial effects of cell therapy with BM-MSCs and the mechanism(s) especially the role of paracrine signaling.
Transplantation of MSCs Provides Promising Therapeutic Potential for Tissue Repair and Regeneration
BM-MSCs are considered to be the most utilized and extensively explored stem cell population for both pre-clinical studies and clinical trials on cell-based therapies due to their unique properties as highlighted above (easily isolated and amplified from the bone marrow, immunologically well tolerated, and their multilineage potential). Pre-clinical animal investigations have shown that transplantation of MSCs provides significant beneficial effects in the treatment of a variety of clinical conditions with significant restoration of tissue structures and improvement in organ function including (but not limited to) liver and kidney dysfunction, myocardial infarction, central nervous system disorders, osteoarthritis, autoimmune and inflammatory/degenerative disorders, and cutaneous wound repair [1, 19, 45, 55]. Clinical studies have demonstrated that administration of MSCs (both locally and systematically) in human subjects appeared to be safe, and exhibited promising therapeutic effects for a wide range of disease states like (but not limited to) myocardial infarction, ischemic and non-ischemic cardiomyopathy, ischemic stroke, spinal cord injury, liver diseases, ischemic intestinal diseases, and autoimmune and inflammatory disorders [1, 8, 21, 36, 55]. Obviously, it is beyond the scope of this review to detail all the clinical studies on every individual medical condition using MSCs.
Mechanisms for the Therapeutic Effects of MSCs
It is clear that application of MSCs contributes to the repair and regeneration of damaged tissues with enhanced function and provides significant therapeutic benefits on a variety of disease conditions. However, it is much less clear on the primary mode(s) of action of these cells on achieving their beneficial effects on tissue repair. Initially, it is believed that transplanted MSCs home to the damaged areas, differentiate into the cells specific to the tissue and organ system, thus contributing to tissue repair and regeneration. Indeed, it is observed that the transplanted MSCs integrated into the damaged sites in a variety of tissues where they transform into the cells with the cell markers specific to the cell populations in a individual tissue and organ like hepatocytes in the liver, epithelial cells of the esophagus and small intestine, keratinocytes, and endothelial cells [16, 19, 42], supporting the idea that these cells are capable of homing to and integrating into the damaged tissues and directly contributing to their reconstruction and function recovery. There is no question that a direct engraftment and differentiation into the tissue specific cells and their supporting cells with transplanted MSCs represents an important mechanism for tissue repair and regeneration for some tissues like liver and lung.
MSCs have been shown to display a broad range of important immunomodulatory properties and attenuate tissue damages due to excessive inflammation in the early phase of injuries. These include suppression of T cell and B cell proliferation and terminal differentiation, modulating dendritic cell maturation and activities, and functional modulation of other cells critical to immune responses like natural killer cells and macrophages [40, 55]. The immuno-privileged and immuno-regulatory capabilities as well as anti-inflammatory properties of MSCs certainly contribute (at least partially) to their therapeutic benefits on repair and regeneration not only in autologous but also allogeneic recipients through modification of the local environment of damaged sites and argumentation of the survival and functional recovery of local resident cells with enhanced proliferation, migration, and differentiation, as well as decreased adverse inflammatory and immune reactions and cell apoptosis. This may be the primary mode of action of MSCs on the treatment of immune diseases such as graft-versus-host disease, rheumatoid arthritis, experimental autoimmune encephalomyelitis, sepsis, acute pancreatitis and multiple sclerosis. Although the exact mechanisms for the unusual immunomodulatory and anti-inflammatory effects of MSCs are far from fully understood, they are considered to be mediated through direct cell-cell interactions and/or secreting various immune-related soluble factors or cytokines such as interleukin 6 (IL-6), IL-10, IL-1 β, transforming growth factor-β (TGF-β), interferon-γ (INF- γ), and granulocyte-macrophage colony-stimulating factor (GM-CSF) [24, 36, 40, 55].
Paracrine Mechanisms as a Major Mode of Action for the Therapeutic Effects of MSCs
Recent studies have showed that less than 1% of systemically administered MSCs are still present for longer than a week in any organ system including lung, heart, kidney, liver, spleen, and gut following injection [6, 22, 23, 36, 39]. However, clinically, the beneficial effects are observed much longer than a week in patients who have ischemic heart diseases and receive transplantation of MSCs [46, 53]. It is observed that the differentiation of transplanted MSCs into cardiomyocytes is very inefficient. In some studies, when injected into the myocardium after infarction, MSCs are able to reduce the scar formation, improve angiogenesis, and preserve myocardial function without direct involvement of MSC engraftment into the cardiac compartment (either cardiomyocytes or supporting cells) [20, 37, 46, 53]. When administered to treat animals with acute renal failure, MSCs can prevent apoptosis and promote the proliferation of renal-tubule epithelial cells in a differentiation-independent manner [43, 44]. Cell-free products from human MSCs are reported to effectively enhance wound healing [32]. These observations suggest that paracrine factors and related signaling are a major mechanism responsible (at least partially) for the beneficial effects of MSCs on tissue repair and regeneration and alteration of disease pathophysiology.
Secretion of Paracrine Factors in MSCs
It is well known that MSCs express and produce a wide spectrum of biologically active growth factors and cytokines including, but not limited to, fibroblast growth factor (FGF), IL-1 and 6, TGF-β, and VEGF, are expressed, produced, and released from MSCs [31, 34]. As early as 1996, it was observed that MSCs isolated from human bone marrow constitutively expressed and released G-CSF, SCF, LIF, M-CSF, IL-6, and IL-11 into the in vitro culture medium. These cytokines were reported to be involved in the regulation of the differentiation of cells derived from the bone marrow stroma through receptors that were linked to gp130-associated signal transduction pathways [10]. Since then, a long list of biologically active substances (and yet the list is still growing rapidly) such as (but not limited to) VEGF, FGF, MCP-1, HGF, IGF-I, SDF-1, TGF-β, nerve growth factor (NGF), and thrombopoietin have been identified to be expressed and secreted from MSCs derived from bone marrow and a variety of other sources. It has been observed that the conditioned medium from hypoxic MSCs overexpressing Akt gene (Akt-MSCs) markedly inhibits hypoxia-induced apoptosis and triggers vigorous spontaneous contraction of adult rat cardiomyocytes in vitro. Intramyocardial injection of the hypoxic conditioned medium from Akt-MSCs has been shown to significantly reduce the infarct size and improves ventricular function to the same extent as the Akt-MSCs in an acute myocardial infarction rodent model [9], confirming that paracrine actions exerted by the cells through the release of soluble factors are indeed important mechanisms for tissue repair and functional improvement after transplantation of the Akt-MSCs. Accumulating data have demonstrated that the growth factors and cytokines from MSCs exert their beneficial effects on the target cells in their vicinity to facilitate tissue repair and regeneration, including (not limited to) immune response modification, anti-apoptosis, cell survival, metabolism, proliferation, and differentiation, hematopoiesis, myogenesis, angiogenesis, collateral development, remodeling, neuroprotection, renal protection, hair growth, and wound healing [8, 19, 20, 24, 31]. Table 1 summarizes some of the major paracrine factors from MSCs and their actions on cell protection, tissue repair and regeneration. The actions of many other paracrine factors released from MSCs remain to be identified and characterized.
Possible Signaling Pathways Involved in the Secretion of Paracrine Factors in MSCs
Role of Akt Signaling in the Expression of Paracrine Factors
Since MSCs are a mixture of heterogeneous cell populations, and produce a large number of paracrine factors, it may be difficult to investigate the mechanism(s) responsible for the production of individual factors. However, a few signaling pathways have been shown to be critically involved in the expression and production of paracrine factors from MSCs. It has been reported that the expression of VEGF, FGF-2, HGF, IGF-I, and TB4 that are potential mediators of the effects exerted by the Akt-MSC conditioned medium, are significantly up-regulated in the Akt-MSCs especially in response to hypoxia, demonstrating that Akt signaling is important to the regulation on the expression of these factors in MSCs [9].
STAT-3 Signaling Is Important in the Expression of VEGF and TGF-β1 in MSCs
MSCs produce a significant amount of VEGF and TGF-β1 both at basal level and in response to stimuli. The regulation of VEGF expression or production is complex and involves many factors such as hypoxia. It is observed that mouse MSCs release VEGF under normoxia in association with constitutive STAT-3 activity. STAT3 deficiency in STAT-3 knockout mice resulted in a significantly decreased production of VEGF from MSCs. In response to hypoxia or TNF, MSCs produced significantly more VEGF in association with activated p38 MAPK and STAT-3. In addition, STAT-3 ablation neutralized hypoxia-induced release of VEGF from MSCs. Inhibition of p38 MAPK signaling alone has no effect on the release of VEGF from MSCs in normal mice [50].
Multipotent adult progenitor cells (MAPCs) are purified homogeneous MSCs from bone marrow, and are potent source of VEGF and TGF-β1. When the JAK2/STAT-3 signaling pathway in rat MAPCs is blocked with the selective JAK2 phosphorylation inhibitor AG490, VEGF gene expression and protein production are significantly suppressed in the cells [25]. These observations strongly suggest that VEGF expression in MSCs is mediated via JAK2/STAT3 signaling pathway. However, some studies suggest that TGF-α stimulated production of VEGF in human MSCs is mediated via MEK- and PI3-K- but not ERK- or JNK-dependent mechanisms [48]. Very likely, there are different pathways involved in the production of VEGF from MSCs in different species (murine vs human). STAT3 signaling is also critically involved in the regulation of TGF-β1 expression in rat MAPCs. A detectable level of TGF-β1 is expressed in rat MAPCs in culture system. Treatment of the cells with the specific STAT3 phosphorylation inhibitor AG490 significantly blocked STAT3 (Tyr705) phosphorylation, and increased TGF-β1 expression without change in ERK1/2 phosphorylation [26].
Activation of p38 MAPK Signaling Is Involved in the Expression of Paracrine Factors in MSCs
Studies using human MSCs and human adipose progenitor cells demonstrate the secretion of VEGF, HGF, and IGF-I in these cells is significantly increased by stimulation with TNF and is associated with increased activation of p38 mitogen-activated protein kinase (MAPK). Inhibition of p38 MAPK signaling with selective p38 MAPK inhibitor significantly decreased the TNF-stimulated production of VEGF, HGF, and IGF-I in these cells. However, p38 MAPK inhibitor alone had no effect on production of these growth factors without TNF stimulation. These data suggest that TNF enhances the production of paracrine factors in MSCs through a p38 MAPK-dependent mechanism [47]. Inactivation of p38 MAPK signaling is also reported to reduce the expression and production of IL-6, IL-8 and CXCL-1 in MSCs, and decrease wound healing [54], indicating that MSCs promote wound healing through releasing paracrine factors via activation of p38 MAPK signaling.
Role of TNF Receptor-Mediated Mechanism in the Expression of Paracrine Factors in MSCs
Using TNF receptor type 1 (TNFR1) or type 2 (TNFR2) ablation model, it is observed that when MSCs are stimulated with TNF, LPS, or hypoxia for 24 hours, the production of TNF and IGF-1 is decreased in the cells from both knockouts (KOs) as compared with the cells from normal animals. On the other hand, IL-6 secretion is increased in the MSCs from both knockouts over the wild-type cells following TNF stimulation, but is significantly decreased with exposure to LPS. Hypoxia enhances the level of IL-6 in the cells from TNFR1 KO animals, but not in TNFR2 KO cells. TNF stimulation leads to a decreased production of VEGF in TNFR2KO cells, whereas no change in VEGF secretion is observed in TNFR1 KO cells. However, TNFR1 ablation resulted in a decrease in VEGF production in the cells following LPS stimulation with no change in TNFR2 KO cells. With hypoxia, VEGF expression is increased in the TNFR1 KO cells over the normal cells, whereas no difference is present in TNFR2KO cells [29]. These data suggest that TNF receptors and related signaling cascades play a complex role in the regulation on the expression and production of paracrine factors in MSCs in response to different stimuli.
It is also reported that TGF-α promotes the expression of HGF in human MSCs. TGF-α-stimulated production of HGF is effectively prevented by inhibition of MEK, p38, PI-3K signaling, or targeting TNF receptor 2 (TNFR2) using small interfering RNA (siRNA), but not by targeting TNF receptor 1 (TNFR1). However, inhibition of TNFR1 significantly increases basal level of HGF in MSCs. Further investigation indicates that there is a complex interactions between TNF receptors and TGF-α/EGF receptor in the regulation of HGF production in human MSCs via activation of MEK, p38, and PI-3K signaling [49].
Important Factors Associated with the Paracrine Function in MSCs
Paracrine mechanisms for the therapeutic effects of MSCs are very complex, and involve a large number of growth factors and cytokines and related receptors and signaling molecules with a broad range of biological functions. It is important to identify the factors that are critically involved in the regulation on the expression and production of these paracrine factors in MSCs to achieve an optimal therapeutic outcome. In the present focused review, the role of species, age, sex, and environmental factors like hypoxia in the expression of paracrine factors is briefly discussed.
Different Paracrine Factors Are Produced in MSCs from Different Species
Recently, the profiles of paracrine factors from swine and human bone marrow MSCs are characterized and compared in culture system under normoxic or hypoxic conditions [34]. It is shown that the cell markers of swine MSCs are comparable to those of human MSCs with minor differences phenotypically. The majority of paracrine factors including VEGF and Endothelin in the conditioned medium released from swine MSCs are similar to those from human MSCs under normoxic conditions. However, substantial differences in the levels for a number of growth factors and signaling molecules in the conditioned media exist between the two MSCs. Noticeably, a significant amount of FGF-16, frizzled-6, Galectin-3, IL-1 alpha, IL-17E, and Smad-5 are present in the conditioned medium of swine MSCs, while not much in the one of human MSCs. On the other hand, high level of TIMP-1 is detected in the conditioned medium of human MSCs, but not in the one of swine MSCs. When the cells are cultured under hypoxic conditions, only small changes in the paracrine factor profile is observed in the conditioned medium of swine MSCs compared with that under normoxic conditions, while significant changes occur in the paracrine factor profile in the medium of human MSCs. These data suggest that MSCs from different species express and produce different type and / or levels of paracrine factors, and respond differently to the environmental stimulation.
Age Plays an Important Role in the Expression of Paracrine Factors in MSCs
It is well known that the populations of bone marrow MSCs (BMSCs) are closely related to the age of the animal with higher level of MSCs in the younger ones. Although neonatal and adult BMSCs have similar pluripotent potentials and cell surface markers, neonatal bone marrow MSCs (nBMSCs) proliferate faster, and therefore, could be expanded more rapidly than adult bone marrow MSCs (aBMSCs) [30]. It is also reported that MSCs from older hosts are associated with telomere shortening and dysfunction, and a reduced capacity to maintain functional hematopoietic stem cells [15]. MSCs from animals with different ago have been shown to produce different levels of paracrine factors. When compared with aBMSCs, nBMSCs produce lower levels of IL-6 and VEGF, but higher levels of IGF-1 under basal conditions, and after stimulation with TNF. However, there are no differences in LPS-induced production of IL-6, VEGF, or IGF-1 between nBMSCs and adult cells. The difference in cytokine and growth factor production in nBMSCs is considered to be related to p38 and ERK signaling [30]. In a separate study, it is observed that inhibition of NFkB and IKK leads to a significant decrease in VEGF secretion in aBMSCs, but not in nBMSCs [35]. Higher expression of angiogenic growth factors (including HIF-1α, HO-1, VEGF, and FGF-2) is observed in the MSCs from young rats (8–12 weeks old) under anoxia as compared to the cells from old rats (24–26 months) [14]. Clearly, there is a significant difference in the expression and production of paracrine factors between neonatal and adult BMSCs.
Gender Is an Important Determinant in the Production of Paracrine Factors in MSCs
A recent study showed that treatment with MSCs from female donors is associated with greater cardiac protection against acute endotoxemic injury in rats compared with treatment with the cells from male animals [28]. Animal data have shown that MSCs from normal male mice produce significantly greater levels of TNF and IL-6 and significantly less amount of VEGF in response to LPS stimulation and hypoxia than the cells from female animals. A substantial change in the release of TNF, IL-6 and VEGF is observed in MSCs from male TNFR1 knockout mice compared with the cells from the male WT animals, but is not different from female WT MSCs. On the other hand, there is no significant difference in the production of TNF and IL-6 between female WT MSCs and female TNFR1KO MSCs [2, 3]. Apparently, gender differences exist in the therapeutic effects of MSCs and their paracrine function.
Role of Environmental Factors and Disease States in the Expression of Paracrine Factors in MSCs
Although bone marrow is a very hypoxic environment, bone marrow MSCs are very resistant to hypoxic culture condition, survive and function well in hypoxic environment with or without serum [27, 41]. As discussed in this chapter, MSCs produce and secrete a great variety of cytokines and growth factors with a wide spectrum of biological functions that are considered to be largely responsible for the beneficial actions when MSCs are used for tissue repair and regeneration. It is well documented that hypoxia significantly changes the profile of paracrine factors expressed and produced from MSCs. The changes in paracrine factors in response to hypoxia are highly variable and complex with some factors up-regulated, some ones down-regulated, and yet, some factors unchanged [34, 41]. For example, VEGF and TIMP-2 expression is usually up-regulated in bone marrow MSCs from rat, dog, and human under hypoxic condition, while LRP-6 and activin A expression is down-regulated, and no changes in the expression of a number of paracrine factors like (but not limited to) endothelin, frizzled-5, IL-7, IL-27, MMP-16, NCAM-1, and Smad5 in MSCs from both dog and human [34]. There are significant differences in the changes on the expression of some paracrine factors in MSCs from different species in response to hypoxia. It is reported that hypoxia leads to an increased expression of osteoprotegerin, TIMP-2, and IGFBP-7 in human MSCs, while a decrease in their expression in swine MSCs [34].
Some important disease states like hypercholesterolemia and diabetes mellitus (DM) may have significant impact on the paracrine function of MSCs. Indeed, bone marrow-derived progenitor cells from patients with hypercholesterolemia and/or DM exhibit a substantially reduced capacity for neovascularization and decreased paracrine secretion of proangiogenic factors [11, 18]. Recently, it is demonstrated that high glucose culture substantially suppresses VEGF expression in rat MAPCs through inhibition of JAK2/STAT3 signaling [25], and increases TGF-β1 expression in these cells via ERK1/2-induced inhibition of STAT3 signaling [26]. It has also been reported that the levels of IGF-1, FGF-2 and Akt pro-survival factors are significantly decreased in MSCs from type 1 diabetic mice [17]. The protein levels of HIF-1α, VEGF-A, and PDGF-B are shown to be significantly reduced in the conditioned media of mouse MSCs in the presence of high glucose in a dose-dependent manner in association with increased production of intracellular superoxide levels [13]. However, it is shown that high glucose concentration has no effect on the production of VEGF, HGF, or FGF2 from human MSCs at baseline and when treated with TNF-alpha, LPS, or hypoxia [51]. These apparent different results clearly implicate that the effect of high glucose on VEGF expression and production is dependent on specific cell type and/or species.
Conclusion and Future Directions
There is no question that paracrine factors and related signaling molecules represent an important mechanism for the beneficial effects of MSCs on tissue repair and regeneration. It is known that a great number of growth factors and cytokines (the numbers are still rapidly growing) with a broad spectrum of biological functions are expressed and produced in MSCs under different conditions and with different stimuli. A detailed knowledge on how these paracrine molecules mediate the complex protective and regenerative effects of MSCs is of great value to improve their function, viability, homing, retention and integration in the target tissues. Understanding the regulatory mechanisms for the expression and secretion of the paracrine function in MSCs is equally important, allowing engineering the cells for their optimal survival and function. New and more sensitive methods and technology are needed to detect, identify, and characterize new molecules from MSCs that are in small quantity and / or unstable in nature, and yet with powerful therapeutic potential on tissue repair and regeneration. Significant challenges remain on how to design an ideal therapeutic regimen with different paracrine factors to achieve an optimal outcome for tissue protection and regeneration.
References
Bernardo ME, Fibbe WE. Safety and efficacy of mesenchymal stromal cell therapy in autoimmune disorders. Ann N Y Acad Sci. 2012;1266:107–17.
Crisostomo PR, Wang M, Herring CM, Markel TA, Meldrum KK, Lillemoe KD, Meldrum DR. Gender differences in injury induced mesenchymal stem cell apoptosis and VEGF, TNF, IL-6 expression: role of the 55 kDa TNF receptor (TNFR1). J Mol Cell Cardiol. 2007;42(1):142–9.
Crisostomo PR, Wang M, Herring CM, Morrell ED, Seshadri P, Meldrum KK, Meldrum DR. Sex dimorphisms in activated mesenchymal stem cell function. Shock. 2006;26(6):571–4.
Djouad F, Bouffi C, Ghannam S, Noël D, Jorgensen C. Mesenchymal stem cells: innovative therapeutic tools for rheumatic diseases. Nat Rev Rheumatol. 2009;5(7):392–9.
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop DJ, Horwitz E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315–7.
Gao J, Dennis J, Muzic R, Lundberg M, Caplan A. The dynamic in vivo distribution of bone marrow-derived mesenchymal stem cells after infusion. Cells Tissues Organs. 2001;169:12–20.
García-Castro J, Trigueros C, Madrenas J, Pérez-Simón JA, Rodriguez R, Menendez P. Mesenchymal stem cells and their use as cell replacement therapy and disease modelling tool. J Cell Mol Med. 2008;12(6B):2552–65.
Gnecchi M, Danieli P, Cervio E. Mesenchymal stem cell therapy for heart disease. Vascul Pharmacol. 2012;57(1):48–55.
Gnecchi M, He H, Noiseux N, Liang OD, Zhang L, Morello F, Mu H, Melo LG, Pratt RE, Ingwall JS, Dzau VJ. Evidence supporting paracrine hypothesis for Akt-modified mesenchymal stem cell-mediated cardiac protection and functional improvement. FASEB J. 2006;20(6):661–9.
Haynesworth SE, Baber MA, Caplan AI. Cytokine expression by human marrow-derived mesenchymal progenitor cells in vitro: effects of dexamethasone and IL-1 alpha. J Cell Physiol. 1996;166(3):585–92.
Heeschen C, Lehmann R, Honold J, Assmus B, Aicher A, Walter DH, Martin H, Zeiher AM, Dimmeler S. Profoundly reduced neovascularization capacity of bone marrow mononuclear cells derived from patients with chronic ischemic heart disease. Circulation. 2004;109:1615–22.
Horwitz EM, Le Blanc K, Dominici M, Mueller I, Slaper-Cortenbach I, Marini FC, Deans RJ, Krause DS, Keating A. International Society for Cellular Therapy. Clarification of the nomenclature for MSC: The International Society for Cellular Therapy position statement. Cytotherapy. 2005;7(5):393–5.
Ishizuka T, Hinata T, Watanabe Y. Superoxide induced by a high-glucose concentration attenuates production of angiogenic growth factors in hypoxic mouse mesenchymal stem cells. J Endocrinol. 2011;208(2):147–59.
Jiang S, Kh Haider H, Ahmed RP, Idris NM, Salim A, Ashraf M. Transcriptional profiling of young and old mesenchymal stem cells in response to oxygen deprivation and reparability of the infarcted myocardium. J Mol Cell Cardiol. 2008;44(3):582–96.
Ju Z, Jiang H, Jaworski M, Rathinam C, Gompf A, Klein C, Trumpp A, Rudolph KL. Telomere dysfunction induces environmental alterations limiting hematopoietic stem cell function and engraftment. Nat Med. 2007;13:742–7.
Kallis YN, Alison MR, Forbes SJ. Bone marrow stem cells and liver disease. Gut. 2007;56(5):716–24.
Khan M, Akhtar S, Mohsin S, Khan S N, Riazuddin S. Growth factor preconditioning increases the function of diabetes-impaired mesenchymal stem cells. Stem Cells Dev. 2011;20(1):67–75.
Kränkel N, Adams V, Linke A, Gielen S, Erbs S, Lenk K, Schuler G, Hambrecht R. Hyperglycemia reduces survival and impairs function of circulating blood-derived progenitor cells. Arterioscler Thromb Vasc Biol. 2005;25:698–703.
Kuroda Y, Kitada M, Wakao S, Dezawa M. Bone marrow mesenchymal cells: how do they contribute to tissue repair and are they really stem cells? Arch Immunol Ther Exp (Warsz). 2011;59(5):369–78.
Lai RC, Chen TS, Lim SK. Mesenchymal stem cell exosome: a novel stem cell-based therapy for cardiovascular disease. Regen Med. 2011;6(4):481–92.
Lalu MM, McIntyre L, Pugliese C, Fergusson D, Winston BW, Marshall JC, Granton J, Stewart DJ. Canadian Critical Care Trials Group. Safety of cell therapy with mesenchymal stromal cells (SafeCell): a systematic review and meta-analysis of clinical trials. PLoS One. 2012;7(10):e47559.
Lee JW, Gupta N, Serikov V, Matthay MA. Potential application of mesenchymal stem cells in acute lung injury. Expert Opin Biol Ther. 2009;9(10):1259–70.
Lee RH, Pulin AA, Seo MJ, Kota DJ, Ylostalo J, Larson BL, Semprun-Prieto L, Delafontaine P, Prockop DJ. Intravenous hMSCs improve myocardial infarction in mice because cells embolized in lung are activated to secrete the anti-inflammatory protein TSG-6. Cell Stem Cell. 2009;5(1):54–63.
Li H, Fu X. Mechanisms of action of mesenchymal stem cells in cutaneous wound repair and regeneration. Cell Tissue Res. 2012;348(3):371–7.
Liu Z, Lei M, Jiang Y, Hao H, Chu L, Xu J, Luo M, Verfaillie CM, Zweier JL, Liu Z. High glucose attenuates VEGF expression in rat multipotent adult progenitor cells in association with inhibition of JAK2/STAT3 signaling. J Cell Mol Med. 2008;13:3427–36.
Luo M, Liu Z, Chen G, Hao H, Lu T, Cui Y, Lei M, Verfaillie CM, Liu Z. High glucose enhances TGF-β1 expression in rat bone marrow stem cells via ERK1/2-mediated inhibition of STAT3 signaling. Life Sci. 2012;90(13–14):509–18.
Mangi AA, Noiseux N, Kong D, He H, Rezvani M, Ingwall JS, Dzau VJ. Mesenchymal stem cells modified with Akt prevent remodeling and restore performance of infarcted hearts. Nat Med. 2003;9(9):1195–201.
Manukyan MC, Weil BR, Wang Y, Abarbanell AM, Herrmann JL, Poynter JA, Brewster BD, Meldrum DR. Female stem cells are superior to males in preserving myocardial function following endotoxemia. Am J Physiol Regul Integr Comp Physiol. 2011;300(6):R1506–14.
Markel TA, Crisostomo PR, Wang M, Herring CM, Meldrum DR. Activation of individual tumor necrosis factor receptors differentially affects stem cell growth factor and cytokine production. Am J Physiol Gastrointest Liver Physiol. 2007;293(4):G657–62.
Markel TA, Wang M, Crisostomo PR, Manukyan MC, Poynter JA, Meldrum DR. Neonatal stem cells exhibit specific characteristics in function, proliferation, and cellular signaling that distinguish them from their adult counterparts. Am J Physiol Regul Integr Comp Physiol. 2008;294(5):R1491–7.
Mirotsou M, Jayawardena TM, Schmeckpeper J, Gnecchi M, Dzau VJ. Paracrine mechanisms of stem cell reparative and regenerative actions in the heart. J Mol Cell Cardiol. 2011;50:280–9.
Mishra PJ, Mishra PJ, Banerjee D. Cell-free derivatives from mesenchymal stem cells are effective in wound therapy. World J Stem Cells. 2012;4(5):35–43.
Mundra V, Gerling IC, Mahato RI. Mesenchymal stem cell-based therapy. Mol Pharm. 2013;10(1):77–89.
Nguyen BK, Maltais S, Perrault LP, Tanguay JF, Tardif JC, Stevens LM, Borie M, Harel F, Mansour S, Noiseux N. Improved function and myocardial repair of infarcted heart by intracoronary injection of mesenchymal stem cell-derived growth factors. J Cardiovasc Transl Res. 2010;3(5):547–58.
Novotny NM, Markel TA, Crisostomo PR, Meldrum DR. Differential IL-6 and VEGF secretion in adult and neonatal mesenchymal stem cells: role of NFkB. Cytokine. 2008;43(2):215–9.
Parekkadan B, Milwid JM. Mesenchymal stem cells as therapeutics. Annu Rev Biomed Eng. 2010;12:87–117.
Pelacho B, Nakamura Y, Zhang J, Ross J, Heremans Y, Nelson-Holte M, Lemke B, Hagenbrock J, Jiang Y, Prosper F, Luttun A, Verfaillie CM. Multipotent adult progenitor cell transplantation increases vascularity and improves left ventricular function after myocardial infarction. J Tissue Eng Regen Med. 2007;1:51–9.
Rastegar F, Shenaq D, Huang J, Zhang W, Zhang BQ, He BC, Chen L, Zuo GW, Luo Q, Shi Q, Wagner ER, Huang E, Gao Y, Gao JL, Kim SH, Zhou JZ, Bi Y, Su Y, Zhu G, Luo J, Luo X, Qin J, Reid RR, Luu HH, Haydon RC, Deng ZL, He TC. Mesenchymal stem cells: Molecular characteristics and clinical applications. World J Stem Cells. 2010;2(4):67–80.
Schrepfer S, Deuse T, Reichenspurner H, Fischbein M, Robbins R, Pelletier M. Stem cell transplantation: the lung barrier. Transplant Proc. 2007;39:573–6.
Shi M, Liu ZW, Wang FS. Immunomodulatory properties and therapeutic application of mesenchymal stem cells. Clin Exp Immunol. 2011;164(1):1–8.
Takahashi M, Li TS, Suzuki R, Kobayashi T, Ito H, Ikeda Y, Matsuzaki M, Hamano K. Cytokines produced by bone marrow cells can contribute to functional improvement of the infarcted heart by protecting cardiomyocytes from ischemic injury. Am J Physiol Heart Circ Physiol. 2006;291(2):H886–93.
Terai S, Sakaida I, Yamamoto N, Omori K, Watanabe T, Ohata S, Katada T, Miyamoto K, Shinoda K, Nishina H, Okita K. An in vivo model for monitoring trans-differentiation of bone marrow cells into functional hepatocytes. J Biochem. 2003;134(4):551–8.
Togel F, Hu Z, Weiss K, Isaac J, Lange C, Westenfelder C. Administered mesenchymal stem cells protect against ischemic acute renal failure through differentiation-independent mechanisms. Am J Physiol Renal Physiol. 2005;289:F31–42.
Togel F, Weiss K, Yang Y, Hu Z, Zhang P, Westenfelder C. Vasculotropic, paracrine actions of infused mesenchymal stem cells are important to the recovery from acute kidney injury. Am J Physiol Renal Physiol. 2007;292:F1626–35.
Tolar J, Le Blanc K, Keating A, Blazar BR. Concise review: hitting the right spot with mesenchymal stromal cells. Stem Cells. 2010;28(8):1446–55.
Tongers J, Losordo DW, Landmesser U. Stem and progenitor cell-based therapy in ischaemic heart disease: promise, uncertainties, and challenges. Eur Heart J. 2011;32(10):1197–206.
Wang M, Crisostomo PR, Herring C, Meldrum KK, Meldrum DR. Human progenitor cells from bone marrow or adipose tissue produce VEGF, HGF, and IGF-I in response to TNF by a p38 MAPK-dependent mechanism. Am J Physiol Regul Integr Comp Physiol. 2006;291(4):R880–4.
Wang Y, Crisostomo PR, Wang M, Markel TA, Novotny NM, Meldrum DR. TGF-alpha increases human mesenchymal stem cell-secreted VEGF by MEK- and PI3-K- but not JNK- or ERK-dependent mechanisms. Am J Physiol Regul Integr Comp Physiol. 2008;295(4):R1115–23.
Wang Y, Weil BR, Herrmann JL, Abarbanell AM, Tan J, Markel TA, Kelly ML, Meldrum DR. MEK, p38, and PI-3K mediate cross talk between EGFR and TNFR in enhancing hepatocyte growth factor production from human mesenchymal stem cells. Am J Physiol Cell Physiol. 2009;297(5):C1284–93.
Wang M, Zhang W, Crisostomo P, Markel T, Meldrum KK, Fu XY, Meldrum DR. STAT3 mediates bone marrow mesenchymal stem cell VEGF production. J Mol Cell Cardiol. 2007;42:1009–15.
Weil BR, Abarbanell AM, Herrmann JL, Wang Y, Meldrum DR. High glucose concentration in cell culture medium does not acutely affect human mesenchymal stem cell growth factor production or proliferation. Am J Physiol Regul Integr Comp Physiol. 2009;296:R1735–43.
Williams AR, Hare JM. Mesenchymal stem cells: biology, pathophysiology, translational findings, and therapeutic implications for cardiac disease. Circ Res. 2011;109:923–40.
Wollert KC, Drexler H. Cell therapy for the treatment of coronary heart disease: a critical appraisal. Nat Rev Cardiol. 2010;7(4):204–15.
Yew TL, Hung YT, Li HY, Chen HW, Chen LL, Tsai KS, Chiou SH, Chao KC, Huang TF, Chen HL, Hung SC. Enhancement of wound healing by human multipotent stromal cell conditioned medium: the paracrine factors and p38 MAPK activation. Cell Transplant. 2011;20(5):693–706.
Yi T, Song SU. Immunomodulatory properties of mesenchymal stem cells and their therapeutic applications. Arch Pharm Res. 2012;35(2):213–21.
Acknowledgements
This work was supported by a grant from NIH R01 HL094650 (ZGL).
Disclosures
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Xiao, Y. et al. (2013). Secretome of Mesenchymal Stem Cells. In: Zhao, R. (eds) Essentials of Mesenchymal Stem Cell Biology and Its Clinical Translation. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-6716-4_3
Download citation
DOI: https://doi.org/10.1007/978-94-007-6716-4_3
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-6715-7
Online ISBN: 978-94-007-6716-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)