Abstract
Over the past few decades, dramatic advances in the treatment of childhood cancers have created a large and growing population of long-term survivors. Although many pediatric cancers can now be cured, the aggressive therapies employed in the recent era are associated with increased risks of a variety of adverse health effects, including subsequent malignant neoplasms (SMNs). Due to characteristics inherent to both the biology and treatment of Hodgkin’s lymphoma (HL), including the relatively high cure rate, a significant number of SMNs occur in HL survivors. The elevated risk of malignancy persists for decades after cure of HL is obtained, with no apparent plateau in risks over time. The cumulative mortality from second cancers exceeds deaths due to HL beyond 15–30 years after therapy for HL. The topic of SMNs after HL is broad and long-term data continue to accumulate. This chapter will specifically discuss second malignancies in survivors of childhood HL, focusing on gender and radiation dose.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Over the past few decades, dramatic advances in the treatment of childhood cancers have created a large and growing population of long-term survivors. In fact, it was recently estimated that one in every 640 young adults between the ages of 20 and 39 was a cancer survivor (Hewitt et al. 2003). Although many pediatric cancers can now be cured, the aggressive therapies employed in the recent era are associated with increased risks of a variety of adverse health effects, including subsequent malignant neoplasms (SMNs). Several large cohort studies conducted in North American and Europe have identified at least a sixfold increase in the risk of developing a new primary cancer in childhood cancer survivors relative to the general population (Inskip and Curtis 2007; Olsen et al. 1993).
Due to characteristics inherent to both the biology and treatment of Hodgkin’s lymphoma (HL), including the relatively high cure rate, a significant number of second malignancies occur in HL survivors (Inskip and Curtis 2007), with the elevated risk of malignancy persisting for decades after cure of HL is obtained and no apparent plateau (Hodgson et al. 2007; Ng et al. 2002). Due to the significant incidence of second cancer, the cumulative mortality from second cancers exceeds deaths due to HL beyond 15–30 years after therapy for HL (Ng et al. 2002).
Both radiation therapy (RT) and alkylating chemotherapy for HL increase the risks of SMN. Typical mantle radiation fields for HL encompass the thoracic mediastinal and cervical lymph nodes, resulting in radiation exposure to the breasts, normal lung, esophagus, and thyroid. In the era before chemotherapy, many patients received more comprehensive nodal radiation, encompassing the infradiaphragmatic lymph nodes in the para-aortic chain and pelvis. With a combined modality (RT and chemotherapy) approach to HL therapy, with less comprehensive nodal coverage, the infradiaphragmatic lymph nodes are only treated in patients with infradiaphragmatic disease, representing less than 10% of stage I-II HL. These patients are at increased risk of gastrointestinal malignancies. While the topic of SMN after HL is broad and long-term data continue to accumulate, this chapter will specifically discuss second malignancies in survivors of childhood HL focusing on gender and RT dose.
Incidence of Subsequent Malignant Neoplasms by Gender
In contrast to adults, in whom the risk of SMN is reportedly gender neutral or greater in men (van Leeuwen et al. 2000; Hancock et al. 1993), several studies have reported an increased incidence of SMN in girls with HL (Olsen et al. 1993; Tarbellet al. 1993), which has been attributed to the greater occurrence of subsequent breast cancer. A pooled analysis of 5,925 children with HL from 16 population-based international cancer registries calculated an overall observed/expected ratio for all SMN of 7.7 (95% CI, 6.6–8.8) with a value of 6.3 for males and 8.8 for females. However, when evaluating only solid-tumor, non-gender-specific SMN, there was no significant difference, with observed to expected values of 6.6 (95% CI, 4.8–8.9) for females and 5.2 (95% CI, 3.8–6.9) for males (Metayer et al. 2000).
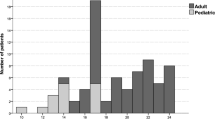
A recent report by Constine et al. (2008) from five institutions that included 930 children and adolescents treated for HL between 1960 and 1990 provided further evidence to support the increased incidence in SMN in female survivors of HL; however, it suggests that this difference is not due entirely to the differences in incidence of breast cancer and that there may be inherent differences between the genders in regards to susceptibility to SMN. After a mean follow-up of 16.8 years (maximum 39.4 years), the investigators found that SMNs occurred in 102 (11%) patients, with a 25-year actuarial rate of 19%. With 15,154 patient-years of follow-up, the expected number of solid tumors in the general population would be 7.18, resulting in a standardized incidence ratio (SIR) of 14.2 and an absolute excess risk (AER) of 63 cases per 10,000 years. Of the 102 children who developed a SMN, 30 (29%) were male and 72 (71%) were female (ratio, 0.42:1), The SIR of 19.93 (95% CI, 15.65–25.32) for females, was significantly greater than the 8.41 (95% CI, 5.68–12.03; p < 0.0001) SIR for males (Fig. 17.1). While there were 29 cases of breast cancer, other cancer types also occurred more frequently in females. If breast cancer was excluded from the risk analysis (Fig. 17.2), the SIR for females fell from 19.93 to 15.14 (95% CI, 9.71–22.0) (p = 0.0012 compared with males). In addition, if thyroid cancer was excluded from the risk analysis, the SIR for females fell from 19.28 to 17.28 (95% CI, 13.31–22.48), whereas the risk for males fell from 8.41 to 7.44 (95% CI, 4.90–10.86), which remains significantly different (p < 0.001). This data suggests that females may be inherently more vulnerable to SMNs than males.
Cumulative proportion of second malignancies according to gender, with standard errors (Reprinted with permission from Constine et al. 2008)
Cumulative proportion of second malignancies according to gender, with standard errors, after excluding breast cancer (Reprinted with permission from Constine et al. 2008)
In contrast, other reports have not demonstrated an increased risk of SMNs for females treated for HL. Among 1,641 children in five Nordic countries, the SIRs for females and males were 8.9 (95% CI, 6.2–12) and 6.5 (95% CI, 4.3–9.6), respectively (Olsen et al. 1993). Similarly, two large single institution studies conducted in the US, one from Stanford University Medical Center reporting on 694 children (Wolden et al. 1998), and one from Roswell Park Cancer Institute reporting on 182 patients (Green et al. 2000) both provided statistically insignificant difference in SIRs between females and males of 15.4 (95% CI, 10.6–21.5) and 10.6 (95% CI, 6.6–16), and 10.16 (95% CI, 5.56–17.05) and 9.39 (95% CI, 4.05–18.49), respectively. A third trial from Harvard also did not demonstrate a difference in relative risk (RR) of SMN according to gender (Ng et al. 2002).
Breast Cancer
Mantle RT fields expose the medial breast tissue to radiation, resulting in a significantly increased risk of breast cancer. Breast cancer accounts for the largest absolute risk of SMNs among female survivors of HL. Radiation dose, chemotherapy administration, age at HL diagnosis, and treatment influence risk of breast cancer.
Radiation Dose
Earlier data suggested a roughly linear increase in breast cancer risk after exposure to RT in the low-dose range (Hildreth et al. 1989). Several more recent studies have analyzed RT dose after therapy for HL and provided quantitative information concerning RR and AER of breast cancer. van Leeuwen et al. (2003) conducted a case-control study of patients from the Netherlands who had been diagnosed with HL before age 41. They identified 48 cases of breast cancer and 175 matched control subjects treated for HL (of which 172 received RT). The RT dose was estimated to the area of the breast where the case patient’s tumor had developed and to a comparable location in the matched control subjects, in order to examine the association between individually estimated RT doses at the precise site of subsequent breast tumor development and breast cancer risk. The risk of breast cancer increased statistically significantly with RT dose, with patients who received 38.5 Gy or more having an RR of 4.5 (95% CI,1.3–16) times that of patients who received less than 4 Gy.
Of note, analysis of patients’ RT dose on risk of SMN must be done with attention to potential confounding factors, the most important of which appears to be ovarian functional status. For example, patients in this study who received both chemotherapy and RT had a statistically significantly lower risk of breast cancer than those treated with RT alone (RR = 0.45, 95% CI, 0.22–0.91). The RR for developing breast cancer in patients who received 38.5 Gy of more versus less than 4 Gy was 12.7 (95% CI, 1.8–86) for the subset of patients who received RT alone, but 0.45 (95% CI, 0.22–0.91) for those who received chemotherapy as well as RT. Reaching menopause before age 36 was associated with a strongly reduced risk of breast cancer (RR = 0.06, 95% CI, 0.01–0.45). Therefore, while breast cancer risk increases with increasing RT dose up to at least 38.5 Gy, chemotherapy was associated with a substantial risk reduction. It would appear that an alteration of the hormonal milieu brought about by early menopause is protective because it reduces exposure of RT-damaged breast cells to the stimulating effects of ovarian hormones.
Travis et al. (2003) conducted a similar population-based matched case-control study with a cohort of 3,817 female HL patients diagnosed at age 30 years or younger. Breast cancer occurred in 105 patients with HL, who were matched to 266 patients with HL but without breast cancer. A RT dose of 4 Gy or greater was associated with a RR of 3.2 (95% CI, 1.4–8.2), compared with the risk in patients who received lower doses and no alkylating agents, while the RR was 8.0 (95% CI, 2.6–26.4) with a dose of more than 40 Gy. Again, ovarian function greatly affected the RR of subsequent breast cancer. Treatment with alkylating agents alone resulted in a RR of 0.6 (95% CI, 0.2–2.0) of breast cancer, and patients who received both an alkylating agents and radiotherapy had a RR of 1.4 (95% CI, 0.6–3.5). The RR of breast cancer decreased with increasing number of alkylating agent cycles (P = .003 for trend). Similarly, a RT dose of 5 Gy or more to the ovaries was protective against breast cancer compared with those who received lower doses (RR of 0.4; 95% CI, 0.1–1.1).
A third case-control study conducted as part of the Childhood Cancer Survivor Study included 6, 647 women who were 5-year survivors of childhood cancer (all initial cancer types included), of whom 120 patients (65% of whom were initially diagnosed with HL) were identified with breast cancer and matched with 464 control patients (Inskip et al. 2009). A linear dose-response model fit the data well and demonstrated a slope of 0.27 per Gy (95% CI, 0.10–0.67) (Fig. 17.3). The estimated RRs were 6.4 at 20 Gy and 11.8 at 40 Gy. Again, the risk associated with breast irradiation was sharply reduced among women who received 5 Gy or more to the ovaries, with an excess odds ratio per Gy of 0.36 for those who received ovarian doses less than 5 Gy and 0.06 for those who received higher doses. Given the well-established increased risk of breast cancer in female children treated for HL, the Children’s Oncology Group has developed and studied a gender-specific, single modality chemotherapy regimen for high-risk HL patients that appears to maintain efficacy without RT, although follow-up is somewhat limited (Kelly et al. 2011).
Breast cancer risk by radiation dose to the breast (Reprinted with permission from Inskip et al. 2009)
Age at Diagnosis of HL
Two single institution retrospective cohort studies have demonstrated a strong relationship between age at diagnosis of HL, until the age of 30–35, and RR of breast cancer compared with the general female population. Data from Harvard on 1,319 patients demonstrates a continuous downward trend in the RR of breast cancer as age at diagnosis of HL increased, with a RR of 111.4 for those diagnosed before age 15, 31.1 for those diagnosed from ages 15–19, and an approximate decrease by half for the RR thereafter for every 5 year interval until a RR of 3.7, which is of borderline significance in women diagnosed between age 30 and 35 years. After age 35, the RR was not significantly increased (Ng et al. 2002). Data from Stanford on 885 patients is strikingly similar, with a RR of 33 for patients diagnosed before age 20, RR of 19 for patients treated between ages 20 and 24, and a RR of 7.3 for patients treated between the ages of 25 and 29. There was no increase in the RR after age 30 (Hancock et al. 1993).
Hodgson et al. (2007) conducted an international population-based retrospective cohort study using multivariate modeling to describe the age at HL diagnosis and attained age on both the RR and AER. Second malignant neoplasm risk was found to be strongly dependent on age at HL diagnosis and attained age. Consistent with the previous two studies, the RR of female breast cancer declined significantly with attained age; however, the baseline risk with advancing age led to a significant increase in AER, which suggests that the increased risk of breast cancer persists with increasing attained age. This was particularly notable for younger patients, as the AER at an attained age of 60 was 212 (95% CI, 108–401), 94 (95% CI, 61–140), and 24 (95% CI, 6.9–46) for women diagnosed at ages 20–29, 30–39, and greater than 40, respectively. At an attained age of 50, similar values were 139 (95% CI, 88–212), 61 (95% CI, 46–79), and 16 (95% CI, 4.5–30) for women diagnosed at ages 20–29, 30–39, and greater than 40, respectively. This study was based on analyses that simultaneously evaluated both age at HL diagnosis and attained age, which is important because the variables are highly correlated. Without adjustment for age at HL diagnosis, the AER for breast cancer decreased instead of increased with attained age.
Breast Cancer Survival After HL vs. De Novo Breast Cancer
Two recent reports have evaluated outcomes of patients who develop breast cancer after HL compared with those who have de novo breast cancer. A recent multi-institutional matched case-controlled study of 253 women with breast cancer and a history of RT for HL (HL-BC) and 741 patients with sporadic breast cancer (BC-1) similarly found inferior outcomes for HL-BC patients. Specifically, although HL-BC patients were more likely to be detected by screening mammography (40% vs. 33%) at an earlier stage (stage 0 or 1; 61% vs 42%) and to be postmenopausal at diagnosis (51% vs 31%), breast cancer–specific mortality had an elevated risk (adjusted HR, 1.6; 95% CI, 0.7–3.4), although this was not statistically significant. Of note, survivors of HL were more than four times more likely to be diagnosed with metachronous contralateral breast cancer (adjusted HR, 4.3; 95% CI, 1.7–11.0; p < .01). The most striking finding of this study was a near double risk of death from any cause among the HL-BC patients (adjusted HR, 1.9; 95% CI, 1.1–3.3) (Elkin et al. 2011).
Another similar U.S. population-based analysis by Milano et al. (2010) included 298 HL survivors who developed breast cancer and 405,223 women with a first or only breast cancer. It revealed significantly worse outcomes for HL-BC patients in several outcome measures. Fifteen year OS among patients with HL-BC was significantly inferior to that of patients with BC-1 both for localized (48% versus 69%; p < .0001) and regional/distant (33% versus 43%; p < .0001) BC. Additionally, HL-BC patients had a significantly increased sevenfold risk (P < .0001) of death from cancers other than breast cancer when compared with patients with BC-1. Ten year cause-specific survival was similar for patients with HL-BC and BC-1 with regional/distant disease, but it was inferior for patients with localized breast cancer (82% vs. 88%, respectively; P = .002). Of note, patients with HL-BC also experienced a two- to fourfold greater risk of cardiac death. The investigators hypothesized that these inferior outcomes were due to a combination of patient susceptibility, treatment-induced factors, and limitations in treatment options for breast cancer after HL.
Of note, two recent reports provided a pathologic evaluation and molecular profile of breast cancer specimens of survivors of HL compared with women who had de novo breast cancer and suggest that subsequent breast cancers may have quantitatively different biology. For example, the overall frequency of microsatellite alterations in the post-HL breast cancers was 4.2-fold greater than in the de novo specimens (P = .16), suggesting widespread genomic instability (Behrens et al. 2000). In another series, BC after HL as compared with de novo BC had a gene expression profile characterized by high proliferation and more aggressive tumor type (Broeks et al. 2010).
Lung Cancer
Lung cancer is the second most common SMN after HL, with a substantially increased3- to 20-fold relative risks compared with the general population (Dores et al. 2002; Ng et al. 2002; Swerdlow et al. 2000, 2001; Travis et al. 2002; van Leeuwen et al. 1995). Clearly established risk factors for lung cancer after treatment of HL include RT and alkylating chemotherapy (Travis et al. 2002), both of which demonstrate a dose-dependent response. However, cigarette smoking is by far the greatest risk factor; in fact, it appears that virtually all HL patients who develop lung cancer had a history of tobacco abuse (Travis et al. 2002).
The RR of lung cancer among pediatric HL survivors is similar to that of adult HL patients, ranging from 5.1 to 27.1, while AER is smaller in children (Bhatia et al. 2003; Castellino et al. 2011; Dores et al. 2002; Green et al. 2000; Metayer et al. 2000; Wolden et al. 1998). However, the incidence of second lung cancer is low among pediatric survivors. In a population-based long-term follow-up study by Dores et al. (2002), only four out of 157 solid tumors occurred in the lung. Similarly, the most recent analysis on the Childhood Cancer Survivorship Study HL cohort showed seven out of 277 second cancers occurring in the lung (Castellino et al. 2011).
Radiation Dose
Ionizing radiation is a well-known pulmonary carcinogen (UNSCEAR 2000). However, quantification of the carcinogenic effect of radiation specific to lung cancer is challenging due to multiple confounding agents such as chemotherapy and smoking (Swerdlow et al. 2001). A case-control study of 61 lung cancer patients and 120 control survivors among women treated with RT for breast cancer reported the RR of lung cancer associated with initial RT for breast cancer of 1.8 with excess RR of 0.20 per Gy to the ipsilateral lung (Inskip et al. 1994).
Specific to HL treatment, van Leeuwen et al. (1995) conducted a case-control study from a cohort of 1,939 patients treated in the Netherlands. They identified 30 patients with lung cancer following HL and 82 matched control subjects. They used estimates of RT dose (<1, 1–5, 5–8, and >9 Gy) to the ipsilateral lobe of lung and reported dose and reported a statistically significant increase in risk of lung cancer with increasing RT dose and an RR of 9.6 for patients who received 9 Gy or more compared with those who received less than 1 Gy.
A more recent report by Travis et al. (2002) is the largest and most comprehensive study that describes the relationship between RT and chemotherapy as well as smoking in the occurrence of excess lung cancer among HL survivors. In this large case-control study among 19,046 HL patients from international population-based cancer registries, they identified 222 HL survivors who developed lung cancer and 444 matched controls without lung cancer. A RT dose of 5 Gy or more without chemotherapy was associated with increased lung cancer risk (RR = 5.9). Patients aged 40 or younger who were treated with RT had a RR of 3.8. There was a RT dose-dependent increase of risk with a peak RR of 8.6 in the 30–39 Gy dose range. It also reported dose-dependent risk with receipt of chemotherapy and effects appeared to be additive when patients received both chemotherapy and RT. Finally, smoking increased lung cancer risk more than 20-fold and appeared to multiply the risk from HL treatment. The authors estimated that of lung cancers after HL, ∼63% are due to the combined effect of treatment and smoking, ∼24% are due to smoking, ∼10% are due to treatment alone (including RT and/or chemotherapy), and the remaining ∼3% are due to causes unrelated to tobacco use or therapy. However, it is important to note that this comprehensive study was not specific to pediatric population as it did not do a separate analysis on patients treated before age 21.
Gender
Analysis of gender-related lung cancer risk among pediatric cancer survivors is challenging. Both gender-related smoking patterns and duration of exposure to tobacco affect risk of lung cancer and may act as confounders in lung cancer risk analysis subsequent to previous cancer treatment. In a study of atomic bomb survivors, Pierce et al. (2003) attempted adjusting for smoking, which removed a large female:male ratio of 1.6 in radiation relative risk due to the interaction between sex and smoking level. In the study by Milano et al. (2011) which compared disease characteristics of subsequent lung cancer among HL survivors versus first primary lung cancer in the general population, there was no difference in gender distribution between the two populations.
Lung Cancer Survival After HL versus De Novo Lung Cancer
A population-based analysis by Milano et al. (2011) that compared outcomes of 187 HL survivors who developed non small cell lung cancer and 178,431 patients with a first primary lung cancer from SEER data revealed significantly worse outcomes in the HL cohort. The multivariable Cox proportional hazard analysis showed that survival of HL cohort was inferior with hazard ratio of 1.60, 1.67, and 1,31 for localized, regional, and distant stage diseases respectively. However, only three out of 187 HL survivors were diagnosed of HL before age 20. Therefore, whether pediatric HL survivors with subsequent lung cancer would have inferior survival compared to age-matched patients with first primary lung cancer could not be answered with this analysis.
Subsequent Breast and Lung Cancer Risk in Modern RT Era
The above studies are most relevant to patients treated for HL decades ago in an era when much larger RT fields and doses were administered. It is almost certain that the reduced exposure of various organs to RT in the modern era will decrease subsequent neoplasms and other late effects. However, these data are informative for the tens of thousands of HL survivors treated decades ago, especially with data outlined above suggesting that their elevated risk of SMN and other late effects may be lifelong.
Although only time will tell to as what extent modern RT fields will reduce second cancer risk, Koh et al. (2007) recently performed a comparison of traditional mantle field versus involved-field radiotherapy for HL to quantify the reduction in normal tissue does and estimate the reduced risk of subsequent malignancies. In this study, organ-specific dose-volume histograms were generated for 41 patients receiving an antiquated dose and volume of 35 Gy to a traditional mantle field, 35 Gy IFRT, and a contemporary dose and volume of 20 Gy IFRT. Reduction of volume from 35 Gy mantle RT to 35 Gy IFRT resulted in a decrease in the mean RT dose to the breast and lung of 9.0 Gy to 3.2 Gy, and 14.7 Gy to 11.2 Gy, respectively, but given its equivalent inclusion in both fields there was no decrease in dose to the thyroid. Reducing dose from 35 Gy IFRT to 20 Gy IFRT resulted in an expected reduction in dose by the same proportion, with a value of 1.8 Gy to the breast and 6.4 Gy to the lung.
The use of 35 Gy IFRT rather than 35 Gy mantle field corresponded to a decrease in predicted excess relative risk (ERR) of approximately 65% for female breast and lung cancer and 35% for male lung cancer, while reduction of dose from 35 Gy IFRT to 20 Gy IFRT reduced predicted EER by an additional approximately 40%. The reduced dose and subsequent estimated risk of SMN for both breast and lung cancer was largely attributed to the omission of the axillary fields in IFRT, although the more superior placement of the inferior border in IFRT also contributed to the decreased lung dose and SMN risk.
Gastrointestinal Cancers
It is well established that HL survivors are at increased risk of developing SMN in the gastrointestinal (GI) system, with a RR of 1.7–6.0 compared with the general population (Birdwell et al. 1997; Dores et al. 2002; Ng et al. 2002; Swerdlow et al. 2000; van Leeuwen et al. 2000). The risks are higher for children with 7.2- to 35-fold increased incidence (Bhatia et al. 2003; Birdwell et al. 1997; Constine et al. 2008; Dores et al. 2002; Green et al. 2000; Metayer et al. 2000; van Leeuwen et al. 2000).While GI cancers are grouped together in many reports, several studies separately analyzed individual sites in GI system. The majority of the cancers occurred in the stomach or large intestine, while relatively few cases were observed in the esophagus, small intestine, and pancreas. However, the RRs in these sites were dramatically elevated due to low incidences in the general population. The latency period for SMN development is 10–20 years following the initial treatment, and increased risk seems to persist past 20 years (Metayer et al. 2000). Increased risk of second GI cancers leads to higher mortality from GI cancers compared with the general population. In a long-term follow-up study of 5-year survivors of HL from Childhood Cancer Survivor Study, Castellino et al. (2011) reported that GI system cancers werethe most common cancer cause of deaths along with breast cancer.
Age at treatment is strongly associated with risk of developing GI cancer. In 25-year follow-up studies of 32,591 long-term survivors of HL from 16 international population-based cancer registries, Dores et al. (2002) showed that pediatric HL survivors who were treated before age 20 had relative risk of 10.0, significantly higher compared with adult survivors whose risk is less than twofold in a large population-based analysis. Metayer et al. (2000) analyzed outcomes of 5,923 pediatric survivors from nine population-based cancer registries, including the effect of age at treatment within the pediatric survivors. Children who were treated before age of 16 had a RR of 19.3, while survivors who were treated between ages 17–21 seemed to have lower RR of six. There was also a threefold difference in AER between the two groups.
Cancer treatment is an important risk factor in development of GI cancer. Both chemotherapy and RT are known to be associated with an increased risk of GI cancer. While some have reported marginally increased risk due to RT, (Swerdlow et al. 2000) others found it highly significant (Birdwell et al. 1997; Dores et al. 2002; van Leeuwen et al. 2000). In general, combined modality treatment was associated with higher risk compared with RT alone. This pattern may suggest that the role of chemotherapy and RT is additive. However, there has been no conclusive study in this matter. Though not specific to GI cancer, RT field size was associated with second cancer risk. In a single institution long-term follow-up study, Ng et al. (2002) showed significant excesses of solid organ tumors following exposure to large radiation fields, such as total nodal irradiation on para-aortic/pelvic radiation. In an analysis of 930 children for HL, Constine et al. (2008) reported that 77% of second cancers, including GI cancers, occurred within the RT field. In a more recent analysis of the British Childhood Cancer Survivor Cohort, children who received abdominal or pelvic RT for selected childhood cancers, including HL, had 3.3-fold increased risk of developing cancers in the digestive system (Reulen et al. 2011).
Specific to stomach cancer, van den Belt-Dusebout et al. (2009) conducted a nested case-control study with a cohort of 5,142 HL or testicular cancer survivors to evaluate the roles of RT dose in the development of stomach cancer. Forty-two patients who developed stomach cancer were compared with 126 matched controls whose mean RT dose to the stomach was estimated. They found that RT increases the risk of stomach cancer by 8.8-fold. Use of the para-aortic field was associated with a higher risk compared with mantle field only. There was a dose-dependent escalation of risk where patients whose estimated stomach dose was higher than 20 Gy had a 9.9-fold increased risk compared with those who received less than 11 Gy. Estimated RR was 0.84 per Gy. On the other hand, no study has evaluated the relation between RT dose to colon and subsequent colon cancer risk.
In general, GI cancer incidence is reportedly higher in males than females. This pattern is site-dependent as stomach and esophagus cancers are highly associated with behavioral risk factors including tobacco and alcohol which may also have strong gender relations. Overall, it does not appear that one gender has a higher RR of GI cancer than the other (Birdwell et al. 1997; Dores et al. 2002). In the pediatric population, comparison of RR becomes more challenging as these values become inflated due to the low number of observed cases and low background incidence.
Thyroid Cancer
Thyroid cancer is another common SMN among children who were treated for HL. Relative risks of children developing thyroid cancer compared with the general population range from 13- to 53-fold (Bhatia et al. 2003; Constine et al. 2008; Dores et al. 2002; Green et al. 2000; Wolden et al. 1998), which is higher when compared with adult HL survivors (Dores et al. 2002; Ng et al. 2002; Swerdlow et al. 2000; van Leeuwen et al. 2000). While early studies based on single or multi-institution databases reported higher RRs due to a small number of reported cases, recent population-based studies with more than 20 years of followup repeatedly reported statistically significantly elevated RR as well as AER (Dores et al. 2002). The majority of cancers occur 10 years after diagnosis with a median time of 14–16 years for thyroid cancer (Bhatia et al. 2003; Constine et al. 2008). This is similar to the latent interval of 13–16 years for second thyroid cancer in an analysis of all childhood malignancy survivors (Sigurdson et al. 2005). Risks are elevated 10 years past diagnosis and remain elevated up to 30 years after diagnosis (Bhatia et al. 2003; Dores et al. 2002; Metayer et al. 2000), suggesting the role of cancer treatment in thyroid carcinogenesis.
Age at treatment has a strong association with risk of developing thyroid cancer (Bhatia et al. 2003; Dores et al. 2002; Metayer et al. 2000). Children who were treated before age 21 have significantly higher RR and AER compared with adult survivors whose RR is less than fivefold in most large-scale series (Dores et al. 2002; Ng et al. 2002; Swerdlow et al. 2000; van Leeuwen et al. 2000). Within the pediatric population, children who were treated before age 10 were found to have even higher RR and AER (Bhatia et al. 2003; Metayer et al. 2000). According to Bhatia et al. (2003), compared to children who were diagnosed with HL after age 10, there was a 3.7- and 1.6-fold increased risk of thyroid cancer among children who were diagnosed at age less than five, and between 5 and 10 years, respectively. Such a finding suggests that younger children whose thyroids are still developing have higher sensitivity to the carcinogenic effects of ionizing radiation.
Radiotherapy to the neck has been recognized as the main risk factor of second thyroid cancer. In a pooled analysis of seven cohort studies, including atomic bomb survivors and populations who received RT for benign diseases of the head and neck, Ron et al. (1995) suggested linear relation between the doses to the thyroid and cancer risk. While thyroid doses as low as 9 cGy were found to be associated with a fourfold increased risk of malignant tumors, Tucker et al. (1991) showed that doses greater than 200 cGy were associated with a 13-fold increased risk in an analysis of 9,170 childhood cancer survivors. However, a flattening of the dose-response curve was observed in higher doses (>10 Gy) used for treatment of HL. In a more recent nested case-control study from the Childhood Cancer Survivor Study, Sigurdson et al. (2005) confirmed a similar trend with a linear increase of thyroid cancer risk in the low dose range to 20 Gy with a peak in risk in the 20–29 Gy range with an odds ratio of 9. However, it demonstrated a decreasing risk at doses above 30 Gy, consistent with the cell-killing hypothesis of high dose RT. This analysis also showed the ascending slope of the dose-response curve was steeper for children who were diagnosed with cancer at less than 10 years of age. These trends were confirmed in a subsequent update from the Childhood Cancer Survivor Study (Bhatti et al. 2010) (Fig. 17.4). The higher risk of thyroid cancer observed in the 20–29 Gy range suggests that children, particularly those treated at younger ages, will continue to be at significant risk of thyroid cancer despite the effort to decrease RT dose and field size in the treatment of HL.
Observed relative risk of thyroid cancer as a function of mean radiation dose to the thyroid gland for categories of dose and fitted values (Reprinted with permission from Bhatti et al. 2010)
It is well established that females within the general population have approximately a three times higher incidence rate of thyroid cancer compared with males. Following this pattern, there was increased incidence in female survivors of childhood HL (Bhatia et al. 2003; Constine et al. 2008; Dores et al. 2002; Green et al. 2000; Metayer et al. 2000; Wolden et al. 1998). In Metayer et al. (2000), six of 3,188 male survivors had thyroid cancer while 16 of 2,737 female survivors developed thyroid cancer. In a smaller series by Bhatia et al. (2003), males and females had an incidence rate of 0.9% and 2.3% respectively. However, females do not seem to have increased AER compared with males. In a multiple regression analysis by Bhatia et al. (2003), RR of thyroid cancer in male children with HL was 1.7 compared with females, though not statistically significant. A similar trend is seen in a population-based analysis by Metayer et al. (2000) where males and females had relative risk of 18.1 and 12.6, respectively.
Bone and Soft Tissue Sarcoma
Bone and soft tissues are another common site of second cancer development after HL. The reported RR of sarcoma ranges from 10 to 14.9 (Bhatia et al. 2003; Castellino et al. 2011; Metayer et al. 2000; Wolden et al. 1998). Common histologies include malignant fibrous histiocytoma, osteosarcoma, spindle cell sarcoma, and undifferentiated soft tissue sarcoma (Wolden et al. 1998).Latency from most series ranges from 10 to 15 years following treatment, while the significance of elevated RR past 20 years is questioned due to low number of observed cases (Bhatia et al. 2003; Metayer et al. 2000).Children are reported to have higher risk of developing sarcoma compared with adult survivors. Metayer et al. (2000) noted that children who were diagnosed between age 10–16 years have the greatest risk of sarcoma. Both alkylating agents and RT have been reported as risk factors. In particular, there was dose-dependent increase of sarcoma risk (Le Vu et al. 1998) and many of the sarcomas occurred within the radiation field such as in the thoracic vertebral body, clavicle, and scapula (Wolden et al. 1998).
In conclusion, although dramatic progress has been made in the treatment of pediatric HL, SMNs have remained a concern for the ever increasing cohort of long-term survivors. Female gender clearly increases risk of SMN, although it is not entirely clear whether all of the excess risk is attributable to the increased risk of breast cancer. Increased RT dose has unequivocally been shown to increase the risk of SMN in nearly all sites, with the notable exception of subsequent thyroid cancer, which displays a peak within the relative low dose range of 20–29 Gy.
Increasing awareness of SMNs continue to influence treatment strategies used in pediatric HL, with shorter courses of chemotherapy and decreasing RT dose and field size. There is a clinical need for improvements in screening guidelines for long-term survivors and for effective treatment strategies for those who develop SMNs. This is especially the case for the cohort of patients treated in previous eras, who are at an increased risk of developing SMNs relative to contemporary patients, and, for certain cancers, appear to have poorer outcomes compared to patients with similarly staged de novo cancers.
References
Behrens C, Travis LB, Wistuba II, Davis S, Maitra A, Clarke EA, Lynch CF, Glimelius B, Wiklund T, Tarone R, Gazdar AF (2000) Molecular changes in second primary lung and breast cancers after therapy for Hodgkin’s disease. Cancer Epidemiol Biomark Prev 9:1027–1035
Bhatia S, Yasui Y, Robison LL, Birch JM, Bogue MK, Diller L, DeLaat C, Fossati-Bellani F, Morgan E, Oberlin O, Reaman G, Ruymann FB, Tersak J, Meadows AT, Late Effects Study Group (2003) High risk of subsequent neoplasms continues with extended follow-up of childhood Hodgkin’s disease: report from the Late Effects Study Group. J Clin Oncol 21:4386–4394
Bhatti P, Veiga LH, Ronckers CM, Sigurdson AJ, Stovall M, Smith SA, Weathers R, Leisenring W, Mertens AC, Hammond S, Friedman DL, Neglia JP, Meadows AT, Donaldson SS, Sklar CA, Robison LL, Inskip PD (2010) Risk of second primary thyroid cancer after radiotherapy for a childhood cancer in a large cohort study: an update from the Childhood Cancer Survivor Study. Radiat Res 174:741–752
Birdwell SH, Hancock SL, Varghese A, Cox RS, Hoppe RT (1997) Gastrointestinal cancer after treatment of Hodgkin’s disease. Int J Radiat Oncol Biol Phys 37:67–73
Broeks A, Braaf LM, Wessels LF, van de Vijver M, De Bruin ML, Stovall M, Russell NS, van Leeuwen FE, Van ’t Veer LJ (2010) Radiation-associated breast tumors display a distinct gene expression profile. Int J Radiat Oncol Biol Phys 76:540–547
Castellino SM, Geiger AM, Mertens AC, Leisenring WM, Tooze JA, Goodman P, Stovall M, Robison LL, Hudson MM (2011) Morbidity and mortality in long-term survivors of Hodgkin lymphoma: a report from the Childhood Cancer Survivor Study. Blood 117:1806–1816
Constine LS, Tarbell N, Hudson MM, Schwartz C, Fisher SG, Muhs AG, Basu SK, Kun LE, Ng A, Mauch P, Sandhu A, Culakova E, Lyman G, Mendenhall N (2008) Subsequent malignancies in children treated for Hodgkin’s disease: associations with gender and radiation dose. Int J Radiat Oncol Biol Phys 72:24–33
Dores GM, Metayer C, Curtis RE, Lynch CF, Clarke EA, Glimelius B, Storm H, Pukkala E, van Leeuwen FE, Holowaty EJ, Andersson M, Wiklund T, Joensuu T, Van’t Veer MB, Stovall M, Gospodarowicz M, Travis LB (2002) Second malignant neoplasms among long-term survivors of Hodgkin’s disease: a population-based evaluation over 25 years. J Clin Oncol 20:3484–3494
Elkin EB, Klem ML, Gonzales AM, Ishill NM, Hodgson D, Ng AK, Marks LB, Weidhaas J, Freedman GM, Miller RC, Constine LS, Myrehaug S, Yahalom J (2011) Characteristics and outcomes of breast cancer in women with and without a history of radiation for Hodgkin’s lymphoma: a multi-institutional, matched cohort study. J Clin Oncol 29:2466–2473
Green DM, Hyland A, Barcos MP, Reynolds JA, Lee RJ, Hall BC, Zevon MA (2000) Second malignant neoplasms after treatment for Hodgkin’s disease in childhood or adolescence. J Clin Oncol 18:1492–1499
Hancock SL, Tucker MA, Hoppe RT (1993) Breast cancer after treatment of Hodgkin’s disease. J Natl Cancer Inst 85:25–31
Hewitt M, Weiner S, Simone J (2003) Childhood cancer survivorship: improving care and quality of life. The National Academies Press, Washington, DC. Accessed at http://www.nap.edu/openbook.php?record_id=10767&page=R1
Hildreth NG, Shore RE, Dvoretsky PM (1989) The risk of breast cancer after irradiation of the thymus in infancy. N Engl J Med 321:1281–1284
Hodgson DC, Gilbert ES, Dores GM, Schonfeld SJ, Lynch CF, Storm H, Hall P, Langmark F, Pukkala E, Andersson M, Kaijser M, Joensuu H, Fossa SD, Travis LB (2007) Long-term solid cancer risk among 5-year survivors of Hodgkin’s lymphoma. J Clin Oncol 25:1489–1497
Inskip PD, Curtis RE (2007) New malignancies following childhood cancer in the United States, 1973–2002. Int J Cancer 121:2233–2240
Inskip PD, Robison LL, Stovall M, Smith SA, Hammond S, Mertens AC, Whitton JA, Diller L, Kenney L, Donaldson SS, Meadows AT, Neglia JP (2009) Radiation dose and breast cancer risk in the childhood cancer survivor study. J Clin Oncol 27:3901–3907
Inskip PD, Stovall M, Flannery JT (1994) Lung cancer risk and radiation dose among women treated for breast cancer. J Natl Cancer Inst 86:983–988
Kelly KM, Sposto R, Hutchinson R, Massey V, McCarten K, Perkins S, Lones M, Villaluna D, Weiner M (2011) BEACOPP chemotherapy is a highly effective regimen in children and adolescents with high-risk Hodgkin lymphoma: a report from the Children’s Oncology Group. Blood 117:2596–2603
Koh ES, Tran TH, Heydarian M, Sachs RK, Tsang RW, Brenner DJ, Pintilie M, Xu T, Chung J, Paul N, Hodgson DC (2007) A comparison of mantle versus involved-field radiotherapy for Hodgkin’s lymphoma: reduction in normal tissue dose and second cancer risk. Radiat Oncol 2:13
Le Vu B, de Vathaire F, Shamsaldin A, Hawkins MM, Grimaud E, Hardiman C, Diallo I, Vassal G, Bessa E, Campbell S, Panis X, Daly-Schveitzer N, Lagrange JL, Zucker JM, Eschwege F, Chavaudra J, Lemerle J (1998) Radiation dose, chemotherapy, and risk of osteosarcoma after solid tumours during childhood. Int J Cancer 77:370–377
Metayer C, Lynch CF, Clarke EA, Glimelius B, Storm H, Pukkala E, Joensuu T, van Leeuwen FE, Van’t Veer MB, Curtis RE, Holowaty EJ, Andersson M, Wiklund T, Gospodarowicz M, Travis LB (2000) Second cancers among long-term survivors of Hodgkin’s disease diagnosed in childhood and adolescence. J Clin Oncol 18:2435–2443
Milano MT, Li H, Constine LS, Travis LB (2011) Survival after second primary lung cancer: a population-based study of 187 Hodgkin lymphoma patients. Cancer 117:5538–5547
Milano MT, Li H, Gail MH, Constine LS, Travis LB (2010) Long-term survival among patients with Hodgkin’s lymphoma who developed breast cancer: a population-based study. J Clin Oncol 28:5088–5096
Ng AK, Bernardo MV, Weller E, Backstrand K, Silver B, Marcus KC, Tarbell NJ, Stevenson MA, Friedberg JW, Mauch PM (2002) Second malignancy after Hodgkin disease treated with radiation therapy with or without chemotherapy: long-term risks and risk factors. Blood 100:1989–1996
Olsen JH, Garwicz S, Hertz H, Jonmundsson G, Langmark F, Lanning M, Lie SO, Moe PJ, Moller T, Sankila R (1993) Second malignant neoplasms after cancer in childhood or adolescence. Nordic society of paediatric haematology and oncology association of the nordic cancer registries. BMJ 307:1030–1036
Pierce DA, Sharp GB, Mabuchi K (2003) Joint effects of radiation and smoking on lung cancer risk among atomic bomb survivors. Radiat Res 159:511–520
Reulen RC, Frobisher C, Winter DL, Kelly J, Lancashire ER, Stiller CA, Pritchard-Jones K, Jenkinson HC, Hawkins MM, British Childhood Cancer Survivor Study Steering Group (2011) Long-term risks of subsequent primary neoplasms among survivors of childhood cancer. JAMA 305:2311–2319
Ron E, Lubin JH, Shore RE, Mabuchi K, Modan B, Pottern LM, Schneider AB, Tucker MA, Boice JD Jr (1995) Thyroid cancer after exposure to external radiation: a pooled analysis of seven studies. Radiat Res 141:259–277
Sigurdson AJ, Ronckers CM, Mertens AC, Stovall M, Smith SA, Liu Y, Berkow RL, Hammond S, Neglia JP, Meadows AT, Sklar CA, Robison LL, Inskip PD (2005) Primary thyroid cancer after a first tumour in childhood (the Childhood Cancer Survivor Study: a nested case-control study. Lancet 365:2014–2023
Swerdlow AJ, Barber JA, Hudson GV, Cunningham D, Gupta RK, Hancock BW, Horwich A, Lister TA, Linch DC (2000) Risk of second malignancy after Hodgkin’s disease in a collaborative British cohort: the relation to age at treatment. J Clin Oncol 18:498–509
Swerdlow AJ, Schoemaker MJ, Allerton R, Horwich A, Barber JA, Cunningham D, Lister TA, Rohatiner AZ, Vaughan Hudson G, Williams MV, Linch DC (2001) Lung cancer after Hodgkin’s disease: a nested case-control study of the relation to treatment. J Clin Oncol 19:1610–1618
Tarbell NJ, Gelber RD, Weinstein HJ, Mauch P (1993) Sex differences in risk of second malignant tumours after Hodgkin’s disease in childhood. Lancet 341:1428–1432
Travis LB, Gospodarowicz M, Curtis RE, Clarke EA, Andersson M, Glimelius B, Joensuu T, Lynch CF, van Leeuwen FE, Holowaty E, Storm H, Glimelius I, Pukkala E, Stovall M, Fraumeni JF Jr, Boice JD Jr, Gilbert E (2002) Lung cancer following chemotherapy and radiotherapy for Hodgkin’s disease. J Natl Cancer Inst 94:182–192
Travis LB, Hill DA, Dores GM, Gospodarowicz M, van Leeuwen FE, Holowaty E, Glimelius B, Andersson M, Wiklund T, Lynch CF, Van’t Veer MB, Glimelius I, Storm H, Pukkala E, Stovall M, Curtis R, Boice JD Jr, Gilbert E (2003) Breast cancer following radiotherapy and chemotherapy among young women with Hodgkin disease. JAMA 290:465–475
Tucker MA, Jones PH, Boice JD Jr, Robison LL, Stone BJ, Stovall M, Jenkin RD, Lubin JH, Baum ES, Siegel SE (1991) Therapeutic radiation at a young age is linked to subsequent thyroid cancer. The Late Effects Study Group. Cancer Res 51:2885–2888
UNSCEAR 2000 report: sources and effects of ionizing radiation [report to General Assembly, with scientific annexes]. http://www.unscear.org/unscear/en/publications.html
van den Belt-Dusebout AW, Aleman BM, Besseling G, de Bruin ML, Hauptmann M, Van’t Veer MB, de Wit R, Ribot JG, Noordijk EM, Kerst JM, Gietema JA, van Leeuwen FE (2009) Roles of radiation dose and chemotherapy in the etiology of stomach cancer as a second malignancy. Int J Radiat Oncol Biol Phys 75:1420–1429
Van Leeuwen FE, Klokman WJ, Stovall M, Hagenbeek A, van den Belt-Dusebout AW, Noyon R, Boice JD Jr, Burgers JM, Somers R (1995) Roles of radiotherapy and smoking in lung cancer following Hodgkin’s disease. J Natl Cancer Inst 87:1530–1537
van Leeuwen FE, Klokman WJ, Veer MB, Hagenbeek A, Krol AD, Vetter UA, Schaapveld M, van Heerde P, Burgers JM, Somers R, Aleman BM (2000) Long-term risk of second malignancy in survivors of Hodgkin’s disease treated during adolescence or young adulthood. J Clin Oncol 18:487–497
van Leeuwen FE, Klokman WJ, Stovall M, Dahler EC, Van’t Veer MB, Noordijk EM, Crommelin MA, Aleman BM, Broeks A, Gospodarowicz M, Travis LB, Russell NS (2003) Roles of radiation dose, chemotherapy, and hormonal factors in breast cancer following Hodgkin’s disease. J Natl Cancer Inst 95:971–980
Wolden SL, Lamborn KR, Cleary SF, Tate DJ, Donaldson SS (1998) Second cancers following pediatric Hodgkin’s disease. J Clin Oncol 16:536–544
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Dhakal, S., Youn, P., Milano, M.T., Constine, L.S. (2013). Survivors of Childhood Hodgkin’s Lymphoma After Treatment: Subsequent Solid Tumor Malignancies Based on Gender and Radiation Dose. In: Hayat, M. (eds) Pediatric Cancer, Volume 4. Pediatric Cancer, vol 4. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-6591-7_17
Download citation
DOI: https://doi.org/10.1007/978-94-007-6591-7_17
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-6590-0
Online ISBN: 978-94-007-6591-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)