Abstract
Mast cells are myeloid derived immune effector cells that have been most widely studied in the context of allergic disease. However, over recent years it has become apparent that they also play critical roles in the regulation of tissue remodelling and host defence. In solid tumors, mast cells are abundant at the tumor periphery in close proximity to blood vessels and are frequently considered to function in a tumor promoting capacity. They release potent angiogenic cytokines that augment tumor blood vessel formation, tumor enhancing growth factors and tissue-degrading enzymes that enable tumor metastasis. Mast cells can also release mediators in the tumor microenvironment that enhance aspects of immune suppression, such as interleukin 10. These observations have led to the consideration of inhibiting mast cells as an approach to cancer therapy. In marked contrast to this negative picture of mast cells in tumors, some studies of human disease have suggested that increased mast cell numbers can be associated with an improved prognosis. It has also been demonstrated, in mouse models, that mast cells might be important targets for immune activation during immunotherapy. Since mast cells are resistant to radiation and normally serve a sentinel cell role recruiting effector cells such as natural killer cells and T cells to sites of infection, they might have substantial potential as an additional target for therapy in the context of more traditional treatments. Our understanding of mast cells in human tumor settings is limited, but there remain excellent opportunities to attempt to modulate mast cell function as a new approach to therapy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Mast cells are highly granulated, tissue resident cells that were first described in 1878 by Paul Erhlich. They were identified by the reactivity of their metachromatic granules with aniline dyes and found in abundance around the blood vessels in loose connective tissue. Ehrlich was also the first to document large numbers of mast cells in solid tumors and subsequent work by his doctoral student, Westphal, demonstrated that mast cells predominately accumulated in the tumor stroma (reviewed in Crivellato et al. 2003). In more recent years, many histological studies have confirmed an abundance of mast cells in the tumor periphery where they often correlate with increased microvessel density (Esposito et al. 2004; Toth-Jakatics et al. 2000).
Interest in mast cells exploded in the 1950s, following the discovery by Riley and West that tissue mast cells serve as a repository for histamine (Riley and West 1953). Investigations linking histamine release from mast cells with anaphylactic response and studies examining the roles of other mediators released from degranulating mast cells (e.g., leukotrienes) in allergic disease took centre stage. Thus, mast cells are best known for their effector function following IgE/antigen mediated activation in allergic disease and response to parasitic infection. However, we have also come to recognize the multifaceted roles of mast cells in diverse biological processes including maintaining tissue homeostasis, regulating tissue remodelling events, and host defence where mast cells are particularly important as sentinel cells that recruit innate and adaptive immune cells during infection (Galli and Tsai 2008; Theoharides et al. 2012; Dawicki and Marshall 2007).
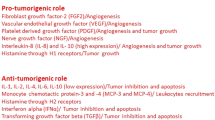
The aim of this chapter is to review the complex and sometimes conflicting literature on mast cells and the tumor microenvironment, highlighting the tumor enhancing roles of mast cells in promoting angiogenesis, tumor metastasis and immune suppression in the tumor microenvironment. In contrast, we will then discuss the sentinel role of mast cells in eliciting effective innate and adaptive immune responses and the therapeutic potential of targeting mast cells at tumor sites.
2 Mast Cell Biology
2.1 Mast Cell Origin
Mast cells are bone marrow derived, tissue resident myeloid cells that contain cytoplasmic granules with preformed, stored mediators (histamine, proteoglycans, neutral serine proteases and cytokines). In contrast to other myeloid-derived cells, which differentiate in the bone marrow and circulate as mature cells, mast cells are released from the bone marrow as committed progenitor cells that only fully differentiate within the tissues (reviewed in Gurish and Austen 2012). They are found throughout the body in close proximity to blood vessels and in large numbers at sites vulnerable to infection such as the skin, airways and gastrointestinal tract.
2.2 Mast Cell Mediators
Mast cells are unique immune cells that possess an array of mediators that can be selectively released, depending on the activation stimulus. Activated mast cells produce three major classes of mediators: (1) pre-formed granule associated mediators, (2) de novo synthesized lipid derived mediators, and (3) cytokines and chemokines (Fig. 20.1). Mast cells tightly control granule stored mediator release which can occur through complete degranulation or a slower and potentially more selective process of ‘piecemeal’ degranulation. A feature of mast cells is their ability to selectively release different mediator profiles in response to different stimuli. For example, human cord blood derived mast cells have been demonstrated to release IL-6 in the absence of degranulation following activation with the pro-inflammatory cytokine IL-1 (Kandere-Grzybowska et al. 2003) and display a highly selective release of cytokines and chemokines following activation through different Toll-like receptors (TLR) (McCurdy et al. 2003). Selective mediator release has also been demonstrated by rodent mast cells. Mast cells secrete a multitude of mediators which may have important functions in the tumor microenvironment (Table 20.1).
Mast cell mediator release. Following activation, mast cells release mediators via different mechanisms: (1) complete (anaphylactic) calcium dependent, degranulation occurs immediately following activation and results in fusion of granule membranes to each other and to the plasma membrane, resulting in release of granule contents into extracellular spaces; (2) piecemeal degranulation involves vesicular transport of mediators from cytoplasmic granules to the cell membrane to allow for slow, sustained release of selective mediators; (3) lipid mediators are synthesized within minutes of membrane perturbation following the release of arachadonic acid from membrane phospholipids; and (4) within the hours following activation mast cells undergo transcription and translation events to produce and secrete multiple cytokines, chemokines and growth factors
Proteases released from mast cell granules have important roles in the promotion of angiogenesis, extracellular matrix (ECM) remodelling and the release of ECM sequestered enzymes and growth factors. They also can degrade local cytokines and chemokines and act through protease activated receptors on multiple cell types (Stevens and Adachi 2007; Younan et al. 2010; Caughey 2011; Conti et al. 2007; Coussens et al. 1999). Proteoglycan–protease complexes and interactions of proteases with the coagulation cascade add to the influence of these potent mediators on the tissue microenvironment. Histamine has a substantial influence on tumor immunity, discussed later in this chapter, as well as on the local vasculature. In addition, certain preformed and stored cytokines such as tumor necrosis factor (TNF), add to the potent inflammatory response following mast cell degranulation.
Activated mast cells can synthesize lipid mediators from arachadonic acid. Prostanoids can add to the pro-angiogenic environment local to tumor sites while others lipid mediators, such as the leukotriene LTB4 and platelet activating factor (PAF), can have both vascular and immune modulatory effects in addition to providing a chemotactic signal for anti-tumor effector cells (Ott et al. 2003; Boyce 2007).
The vast array of different cytokines and chemokines that can be produced by mast cells, in many cases selectively, without granule-associated mediator release, provides enormous opportunity for mast cells to influence tumor growth and metastasis as well as the immune response to tumors. We are only at the beginning of exploring the importance of such mast cell mediators to host responses and the tumor microenvironment.
2.3 Mast Cell Subsets and Localization
MC progenitor cells differentiate in tissues into subsets with distinct functional characteristics. Classically these were referred to as connective tissue mast cells (CTMC) and mucosal mast cells (MMC). CTMC are found typically adjacent to blood vessels, lymphatic vessels and nerve endings in the connective tissue. MMC predominately associate with the epithelial lining of the mucosal tissue of the respiratory, digestive and urogenital tracts (reviewed in Gurish and Austen 2012).
Human mast cell subsets are often characterized based on the protease content of their cytoplasmic granules. MCTC cells contain tryptase together with chymase, cathepsin-G like protease, and mast cell carboxypeptidase and are found in the skin and submucosa. MCT cells contain tryptase, but lack the other neutral proteases present in MCTC cells and are localized to mucosal tissues (Irani et al. 1986, 1991). Importantly, mast cell protease content may be altered by the cytokine milieu and cell interactions within the tumor microenvironment. In human intestinal mast cell cultures IL-4 selectively increased tryptase positive mast cells (Bischoff et al. 1999), whereas co-culture with endothelial cells preferentially induced tryptase/chymase double positive cells (Mierke et al. 2000). Mast cell subsets display marked heterogeneity with respect to granule contents and differences in lipid mediator production in different tissues (Katz et al. 1985). Functional heterogeneity of mast cell subsets is also observed in mast cells isolated from different microenvironments within the same tissue (Finotto et al. 1994). Classical mast cell designations, such as the examples above, represent two extremes of a broad spectrum of mast cell subsets which display a large degree of phenotypic heterogeneity and functional plasticity in different microenvironments. Immature mast cells and those undergoing chronic activation may also display altered characteristics and further complicate the picture regarding heterogeneity within the tumor microenvironment.
It is important to note that mast cell infiltrates in tumor samples have sometimes been assessed using c-Kit specific antibodies. Mast cells express high levels of c-Kit and signalling through c-Kit is required for mast cell survival. However, c-Kit is also expressed at high levels on hematopoietic stem cells and common myeloid progenitors and has been reported on other cell types including innate lymphoid cells, endothelial cell precursors and some tumor cells. Care therefore has to be taken in interpreting the results of c-Kit based analyses. However, immunohistochemical or other analyses that rely on mast cell granule content can also be misleading. Macrophages may take up granule products and immature mast cells with few granules or degranulated mature mast cells may not stain sufficiently for detection. For many routine histological stains, formalin fixation of tissues can reduce metachromatic staining and alternate fixation approaches need to be employed.
3 Mast Cells in the Tumor Microenvironment
3.1 Experimental Models to Study the Role of Mast Cells
Commonly used in vitro models to study mast cells include mast cell lines such as the murine MC9, the rat RM3 or the human HMC-1 and LAD-2. Primary mast cell cultures typically derived from bone marrow for murine studies or from progenitor cells in cord blood or peripheral blood for human studies are also widely employed. These cells are often used in co-culture systems to assess mast cell interactions with tumor, stromal and immune cells. However, in vitro systems cannot fully replicate the complex structure of the tumor microenvironment in vivo. Much of what has been learned about the roles of mast cells in the tumor microenvironment has been gleaned from murine studies of mast cell deficient Kit mutant mice, ideally with complimentary tissue reconstitution of mast cell subsets. Kit mutant mice exhibit profound mast cell deficiency but possess other phenotypic abnormalities. Kit W/W−v mice have a compound deletional and truncated Kit mutation and are sterile, anemic, neutropenic, lack intestinal interstitial cells of Cajal and have a marked decrease in γδ T cells (Grimbaldeston et al. 2005). Kit W−sh/W−sh mice have an inversion mutation in the regulatory locus of the Kit gene and are neither sterile nor anemic, but exhibit neutrophilia, thromobocytosis, splenomegaly and cardiomegaly (Nigrovic et al. 2008).
To circumvent the functional defects observed in mast cell deficient models which are based on mutations of the c-Kit or stem cell factor (SCF) genes, newer models have been developed that target mast cell specific proteases. Inducible and constitutive CTMC deficiency was obtained by breeding the Mcpt5-Cre transgenic mice to the Cre-inducible diphtheria toxin receptor (iDTR) mice and to the R-DTA line which expresses diptheria toxin A in Cre-expressing cells, respectively. These models confirm the involvement of mast cells in contact mediated hypersensitivity (Dudeck et al. 2011). Mast cells were unexpectedly deleted in mice which express the Cre recombinase gene under the control of regulatory elements of the mast cell protease carboxypeptidase A3 gene as a result of Cre-mediated genotoxicity. Studies performed in these mice showed defects in passive local and systemic IgE-mediated anaphylaxis, but could not confirm previously reported roles for mast cells in passive autoantibody induced arthritis or experimentally induced autoimmune encephalitis (Feyerabend et al. 2011). While these discrepant findings may in part be influenced by differences in experimental design as suggested by others (Brown et al. 2012), they highlight that it will be crucial to utilize multiple models of mast cell deficiency in conjunction with other relevant and well established experimental approaches to both confirm and reveal roles for mast cells and mast cell specific mediators in tumorigenesis.
3.2 Mechanisms of Mast Cell Activation at Tumor Sites
The solid tumor microenvironment contains a number of stimuli which could activate mast cells (Fig. 20.2). Substantial evidence from both human in vitro and mouse in vivo studies indicates local mast cell activation with evidence of traditional and/or piecemeal degranulation processes and other indicators of mast cell activity, such as diffuse distribution of mast cell proteases and cytokine expression.
Mast cell activation within the tumor microenvironment. Several mast cell activation events are likely to occur within the tumor microenvironment. The tumor microenvironment is rich in damage associated molecular patterns and other endogenous alarmins such as IL-33 and tumor derived peptides, which can activate mast cells via ST2 and G-protein coupled receptors, respectively. Mast cells express Fc receptors and complement receptors and can be activated by circulating immune complexes and complement components. Mast cells can also be activated in the tumor microenvironment following engagement of receptors for SCF, adenosine and PGE2 and up-regulation of the transcription factor HIF-1α in the hypoxic tumor microenviroment. Mast cells secrete 3 classes of mediators: preformed granule associated mediators, de novo synthesized lipid mediators, and cytokines and chemokines. Different activators stimulate selective mediator release with some mediators primarily enhancing degranulation while others enhance eicosanoid and/or cytokine/chemokine production
Mast cells are known to respond to locally hypoxic conditions, found in the vicinity of growing solid tumors, directly through the function of hypoxia inducible factor (HIF)-1α (Sumbayev et al. 2012; Gulliksson et al. 2010). It has recently been demonstrated that HIF-1α mediates the antimicrobial impact of mast cells through regulation of several mechanisms, including antimicrobial peptide release and the development of extracellular traps (Branitzki-Heinemann et al. 2012). HIF-1α also plays a role in regulating responses to TLR-mediated mast cell activation, which could result from antimicrobial peptide release or tissue breakdown products (Sumbayev et al. 2012).
Adenosine and prostaglandin (PG)E2 are also observed in increased concentrations within the tumor microenvironment. PGE2 has been shown to be an effective stimulus for mast cell cytokine production including the generation of immunoregulatory cytokines such as IL-6 (Leal-Berumen et al. 1995) and the production of vascular endothelial growth factor (VEGF) (Abdel-Majid and Marshall 2004). Both of these events occur in the absence of mast cell degranulation.
Adenosine is found in increased concentrations within tumor sites as a consequence of local hypoxia and can be produced by some types of mast cells in response to IgE receptor-mediated activation (Lloyd et al. 1998). Mast cells express multiple adenosine receptors and have been described to respond to adenosine stimulation, especially through their A2b and A3 adenosine receptors. This leads to a pro-inflammatory response from mast cells that has been extensively studied in the context of allergic disease (recently reviewed in Rudich et al. 2012).
Mast cells can be activated via TLRs and other innate receptor systems to produce substantial amounts of cytokines including TNF and IL-6 as well as chemokines such as CCL3 and CXCL8. These types of responses may be initiated in certain tissue microenvironments by tissue breakdown products such as hyaluronan, the release of intracellular cell contents via necrotic cell death, or by the release of antimicrobial peptides by other cells that can signal via TLRs. Additional damage associated molecular patterns (DAMPs) that can be actively released from viable tumor cells and passively released from necrotic tumor cells within the tumor microenvironment include HSP60, 70 and 90 (Basu et al. 2000; Ciocca and Calderwood 2005).
Alarmins are up-regulated in a number of cancers and include such factors as tumor derived peptides (e.g., LL37), S100A8/S100A9 proteins, HMGB1, and cytokines such as IL-33. Some alarmins can act directly on cancer cells to induce tumor cell proliferation, migration and angiogenesis (reviewed in Chan et al. 2012). However, they can also act indirectly via immune effector cells such as mast cells. Adding to the complexity of this interaction, mast cells themselves have been shown to produce cathelicidins such as LL37 (Wang et al. 2012; Di Nardo et al. 2003) and the IL-1 family member IL-33 (Hsu et al. 2010). IL-33 is released by many cell types, especially epithelial cells, in response to tissue damage. Human skin explants and normal human skin derived fibroblasts and keratinocytes up-regulate IL-33 following exposure to physiological doses of UVB radiation. Murine studies have demonstrated that IL-33 is up-regulated in squamous cell carcinoma cells that evade immunological destruction (Byrne et al. 2011). Both human and murine mast cells express functional IL-33 receptors. IL-33 released from necrotic stromal cells induces murine mast cells to secrete pro-inflammatory cytokines (TNF and IL-6) and leukotrienes (Enoksson et al. 2011). Interestingly, mast cells associate with IL-33 expressing fibroblasts in UV-exposed murine skin samples (Byrne et al. 2011), suggesting mast cells may release such mediators in the tumor microenvironment of skin cancers and possibly other tumor subtypes. Since IL-33 is generally pro-inflammatory, the impact of such secretion would likely be to enhance some aspects of immune cell recruitment, with impacts on both the immune and angiogenic response to the tumor.
Many of the mechanisms whereby macrophages in the tumor microenvironment can become activated are likely shared by mast cells. These include the actions of several cytokines and chemokines (e.g., SCF, CXCL12) as well as aspects of innate immune signaling. Large amounts of SCF have been reported in tumor microenvironments and in other inflammatory settings. This enhances local mast cell survival and differentiation as well as potentially activating mast cells for enhanced secretion of VEGF and basic fibroblast growth factor (bFGF). CXCL12 has numerous impacts on mast cells including activation and chemotaxis. Enhanced levels of this chemokine may contribute particularly to immature mast cell recruitment as discussed in the context of mast cell impacts on tumor angiogenesis.
During allergic disease the predominant mechanism for mast cell activation is via allergen specific IgE bound to FcεRI. A number of studies have suggested that high serum levels of IgE are associated with a decreased cancer risk. The concept that IgE mediated mast cell activation may play a role in host defence against cancer has begun to emerge during recent years (Jensen-Jarolim et al. 2008). A recent rigorous examination of this concept using samples from a Norwegian cohort demonstrated a clear relationship between elevated allergen specific IgE and decreased risk of developing glioma (Schwartzbaum et al. 2012). These studies build on previous examinations of the potential for decreased cancer risk in allergic individuals. While such studies have had varying conclusions, evidence for a beneficial effect of allergy has been found for colorectal cancer (Negri et al. 1999) and a substantial meta-analysis concluded that there was an overall beneficial effect of allergic disease (Sherman et al. 2008). Notably however, a study of operable breast cancer concluded that lower IgE concentrations were also associated with longer survival, but only in patients whose tumors were E2R positive (Ownby et al. 1985), so care needs to be taken in developing general conclusions regarding cancer and IgE from current information.
Rodent mast cells normally express Fcγ receptors and human mast cells can also express a full range of IgG receptors in certain microenvironments, especially those rich in IFN-γ (Tkaczyk et al. 2004). IgG containing immune complexes therefore have the ability to activate mast cells leading to degranulation, lipid mediator production and cytokine/chemokine generation. Complement products produced as a result of IgG or IgM containing immune complex deposition may also induce mast cell activation with degranulation. The contribution of these processes to mast cell activation in tumor microenvironments is unknown. The impact of such mechanisms on mast cell activation needs to be considered, especially in the context of the increased use of antibody mediated therapies and fusion proteins containing Fc structures.
Mast cells are most efficiently activated via high affinity IgE receptors. The use of monoclonal IgE antibodies directed against tumor associated antigens has shown some success in experimental tumor models (Jensen-Jarolim et al. 2008). IgE-mediated mast cell degranulation can overcome allograft tolerance and elicit effector CD4+ and CD8+ T cell mediated rejection (de Vries et al. 2009). Therefore, local mast cell degranulation may be advantageous to subvert the immune suppressive microenvironment of solid tumors and elicit effective anti-tumor immunity. However, there are a number of safety concerns, such as the risk of anaphylaxis, that have been raised regarding the use of IgE antibodies in human therapy.
Notably, adhesion interactions, the cytokine and chemokine microenvironment and multiple other factors can affect not only the type and number of mast cells present within a given tumor setting or tissue location, but also the mediator response that will ensue following activation. It can therefore be difficult to predict from in vitro studies the full nature of the mast cell response. The consequences of chronic mast cell activation with specific mediators and adhesion interactions within a tissue setting may differ considerably from those of acute activation models used in the majority of experimental studies.
3.3 Mast Cell Recruitment to Solid Tumor Sites
Mast cells express a wide array of chemokine and growth factor receptors and migrate to sites of inflammation in response to chemotactic stimuli (reviewed in Halova et al. 2012). Mast cells are among the first cells recruited to tumor sites, are increased in precancerous lesions, further increase with cancer progression and are positively associated with microvessel density (Benitez-Bribiesca et al. 2001; Mohtasham et al. 2010; Kankkunen et al. 1997). Mediators released within the tumor microenvironment including SCF, transforming growth factor (TGF)-β, CCL5 and CXCL12 are thought to be important in the recruitment of mast cells to tumor sites.
SCF expression is highly elevated in human breast, gastric, colorectal, lung, ovarian, liver and esophageal tumor tissue as compared to adjacent normal tissue (Huang et al. 2008). SCF is important for the differentiation and activation of human mast cells, but has also been implicated in their recruitment. SCF has been demonstrated to be important for the recruitment of mast cells in several experimental tumor models including breast carcinoma and hepatocellular carcinoma (Huang et al. 2008; Zhang et al. 2000). Another factor found in abundance in solid tumors is TGF-β. TGF-β isoforms are chemotactic to murine cultured mast cells, rat peritoneal mast cells, the human mast cell line HMC-1 and cord blood derived cultured human mast cells (Olsson et al. 2000; Gruber et al. 1994). Other mediators expressed at high levels in tumors that are likely to be chemotactic to mast cells include VEGF isoforms, adenosine, complement components and lipid mediators (reviewed in Halova et al. 2012).
Chemokines likely play a crucial role in mediating the recruitment of mast cells to tumor sites. Chemokine receptor expression varies between immature and mature mast cells and among mast cell subsets. CCL5 induces chemotaxis of human cord blood derived mast cells via CCR1 and CCR4 in vitro (Juremalm et al. 2002). CCL5 is expressed in Hodgkin's lymphoma tumor tissue samples and CCL5 released from Hodgkin/Reed-Sternberg cell lines induces human mast cell chemotaxis in vitro (Fischer et al. 2003). Human mast cells also migrate to CCL5 released from human keratinocytes following exposure to UVB radiation (Van Nguyen et al. 2011). CCL5 expression by human uterine smooth muscle tumor cells correlates with mast cell density in the tumor tissue and the majority of infiltrating mast cells express the CCR3 receptor for CCL5 (Zhu et al. 2007). These data suggest CCL5 may be an important mast cell chemotactic mediator in several tumor settings.
Mast cells may also be attracted to the tumor microenvironment through the CXCL12/CXCR4 axis. CXCL12 protein is detected in solid tumors (Kryczek et al. 2005) and can be produced by both tumor cells and stromal cells. In human glioblastoma multiformes large numbers of CXCR4+ mast cells surround CXCL12 producing tumor cells (Polajeva et al. 2011). CXCL12 induces transendothelial migration of human cord blood derived mast cells in vitro and their selective release of the pro-angiogenic chemokine CXCL8 (Lin et al. 2001). In a xenograft model, carcinoma associated fibroblasts mobilize early endothelial progenitor cells (EPC), recruit them to implanted breast tumors and enhance tumor angiogenesis in a CXCL12 dependent manner (Orimo et al. 2005). Physiological concentrations of CXCL12 or VEGF alone were not sufficient to induce significant angiogenesis in an in vivo xenograft Matrigel model using ovarian cancer patient ascites. However, combined, the two mediators synergistically induced significant microvessel formation (Kryczek et al. 2005). Similarly, CXCL8 produced from pancreatic cancer cells acts cooperatively with fibroblast derived CXCL12 to enhance human endothelial cell angiogenesis in vitro (Matsuo et al. 2009). Thus, CXCL12 may coordinate the recruitment of EPC and mast cells to the leading edge of solid tumors whereby mast cell mediators such as VEGF and CXCL8 may synergize with CXCL12 in the tumor microenvironment to promote angiogenesis.
3.4 Prognostic Significance of Mast Cells in Solid Tumors
Mast cell density has been reported to associate with a poor outcome in many solid tumor types including Hodgkin’s lymphoma, melanoma, endometrial, cervical, esophageal, lung, gastric, colorectal and prostate carcinomas. The poor prognosis associated with mast cell infiltration has been linked to the positive correlations with microvessel density and metastasis (reviewed in Groot Kormelink et al. 2009).
While most studies suggest that mast cell infiltration of solid tumors is a poor prognostic indicator, others have failed to correlate mast cell infiltration with angiogenesis, metastasis and decreased survival (Xia et al. 2011). Moreover, in some studies, mast cell infiltration is correlated with improved survival (Fleischmann et al. 2009; Hedstrom et al. 2007; Rajput et al. 2008). Mast cells have demonstrated anti-tumor activities in vitro and in experimental tumor models. In vitro studies have demonstrated mast cells can mediate direct TNF-mediated tumor cell cytotoxicity (Benyon et al. 1991; Dery et al. 2000) and inhibit human breast tumor cell clonogenic growth in the presence of fibroblasts (Samoszuk et al. 2005). Anti-tumor roles for other mast cell derived mediators have also been described. In the tumor microenvironment, mast cells are a major source of histamine which can protect against tumor development as demonstrated by increased susceptibility to carcinogen-induced colorectal and skin tumors in histamine deficient mice (Yang et al. 2011).
The location of mast cells within the tumor microenvironment of different tumor subtypes may also be a crucial factor in their ability to provide a protective role against the growth of solid tumors. Studies in non-small cell carcinoma and prostate carcinoma have demonstrated that intratumoral, but not peritumoral, mast cells independently predict improved patient survival (Welsh et al. 2005; Johansson et al. 2010). In a large study of 4,444 breast tumors increased numbers of stromal mast cells independently predicted improved survival (Rajput et al. 2008). It is highly plausible that the prognostic significance of mast cells will be largely dependent on their activation status within the tumor microenvironment, as reflected by the diverse array of mediators that can be released from mast cells in a selective manner depending on the activation stimulus (Kandere-Grzybowska et al. 2003; McCurdy et al. 2003) and their functional interactions with blood vessels.
3.5 Mast Cells and Early Tumor Development
The contribution of mast cells to early tumor development is unclear. Only a few studies have evaluated the influence of mast cells on cancer incidence, with conflicting results. Mast cell deficient Kit W/W−v mice display decreased susceptibility to chemically induced intestinal tumors when compared with congenic WBB6F1-Kit+/+ wild-type mice, which could be normalized via wild type bone marrow reconstitution (Wedemeyer and Galli 2005). Similarly, studies using polyposis prone APC Δ468 mice, which have a mutation in the adenomatous polyposis coli (APC) gene, demonstrated that following lethal irradiation reconstitution with bone marrow from Kit W−sh/W−sh mice resulted in decreased polyp development compared to mice reconstituted with wild type bone marrow (Gounaris et al. 2007). These studies suggest an important role for mast cells in intestinal cancer development. In contrast, when mast cell deficient Kit W−sh/W−sh mice were crossed to the multiple intestinal neoplasia (APCMin/+) mice these mice developed significantly more adenomas than littermate controls (Sinnamon et al. 2008), suggesting a protective role for mast cells in this model of early-stage intestinal tumorigenesis. Differences in these studies may be attributable to genetic differences in mouse strains and developing tumors, additional immunological defects in c-Kit mutant mice or differences in gut microflora contributing to mast cell activation status. It will be useful to examine tumorigenesis in the recently developed, non c-Kit mutant, mast cell deficient models and other tumor subtypes to determine the true impact of mast cells on tumor incidence.
3.6 Mast Cells and Angiogenesis
Activated mast cells can secrete angiogenesis promoting factors including VEGF, bFGF, TGF-β, TNF and CXCL8 and release extracellular matrix (ECM) bound pro-angiogenic factors via action of granule associated proteases (Norrby 2002). Angiogenesis is required for macroscopic tumor expansion and metastasis (Folkman 1990). Mast cells are increased in most solid carcinomas and their numbers correlate with increased microvessel density, increased invasiveness and poor clinical outcome (reviewed in Groot Kormelink et al. 2009). Within the tumor microenvironment, mast cells produce many pro-angiogenic mediators including VEGF and bFGF and their expression correlates with microvessel density (Esposito et al. 2004; Toth-Jakatics et al. 2000). Several experimental model systems have demonstrated the pro-angiogenic activity of mast cells. Early animal studies that compared melanoma and bladder cancer cell growth in mast cell deficient Kit W/Wv mice and wild-type littermates demonstrated tumor angiogenesis was decreased in mast cell deficient mice (Starkey et al. 1988; Dethlefsen et al. 1994). In a xenograft model of human thyroid cancer, transferred human mast cells were recruited to tumor sites and enhanced tumor growth and angiogenesis (Melillo et al. 2010). In murine tumor models, co-transfer of bone marrow derived mast cells significantly enhanced angiogenesis in a murine plasmacytoma model via production of angiopoietin-1 (Nakayama et al. 2004) and mast cells were demonstrated to be critical for macroscopic tumor expansion in experimental models of human papilloma virus induced sarcoma (Coussens et al. 1999) and Myc-induced pancreatic carcinoma (Soucek et al. 2007).
Early studies using the chick chorioallantoic membrane assay demonstrated that degranulating rodent mast cells increased the angiogenic response via production of bFGF and VEGF (Ribatti et al. 2001; Rizzo and DeFouw 1996). Primary human lung mast cells, cord blood derived human mast cells and the HMC-1 and LAD-2 mast cell lines express several isoforms of VEGF (Abdel-Majid and Marshall 2004). Blocking antibody studies using a chick chorio allantoic membrane assay demonstrated human lung mast cells enhance the angiogenic response in a VEGF-A dependent manner (Detoraki et al. 2009) and have also identified pro-angiogenic roles for mast cell tryptase and chymase (Ribatti et al. 2011).
Mast cell degranulation at tumor sites has been detected immunohistochemically using anti-tryptase antibodies and ultrastructurally by electron microscopy (Samoszuk et al. 2005; Caruso et al. 2004). Mediators released by degranulating mast cells enhance angiogenesis in vitro and in experimental tumor models. Several in vitro experiments have identified roles for mast cell mediators in enhancing the angiogenic response. Mast cell tryptases (mMCP-6 and mMCP-7) induce endothelial spreading and tube formation in an in vitro angiogenesis assay (de Souza et al. 2012). Mast cell derived proteases can also contribute to the angiogenic process in the tumor microenvironment through their enzymatic release of ECM sequestered pro-angiogenic factors. For example, mMCP-4 chymase released from mast cells can enhance the angiogenic response in hyperplastic skin via activation of pro-MMP-9, which can liberate angiogenic factors such as VEGF and bFGF from neoplastic tissues (Coussens et al. 1999). Mast cell modulation of angiogenesis is likely altered throughout the course of tumorigenesis. Indeed, levels of the mast cell chymase (mMCP-5), mast cell tryptases (mMCP-6 and mMCP-7) and carboxypeptidase A increased progressively with tumorigenesis and correlated with increased angiogenic response in a murine model of chemically induced skin carcinoma (de Souza et al. 2012).
While there is an abundance of experimental data to support the angiogenesis promoting activities of mast cells in the context of tumorigenesis, experimental models have also identified anti-angiogenic factors that can be released from mast cells in the tumor microenvironment. Anti-angiogenic effects of mast cell derived PGD2 have been observed in a murine model of lung carcinoma where mast cell derived PGD2 inhibits production of the pro-angiogenic cytokine TNF and decreases vascular permeability in the developing tumor (Murata et al. 2011). These data provide additional support for the concept that mast cells can play a dual role in the tumor microenvironment (Theoharides and Conti 2004).
3.7 Mast Cells, Tissue Remodelling and Metastasis
Mast cells are important regulators of tissue remodelling events in the tumor microenvironment through their interactions with stromal cells, such as fibroblasts and myofibroblasts and their release of tissue degrading enzymes (Fig. 20.3). Several mast cell mediators likely contribute to the increased fibroblast activity in the tumor microenvironment (Dvorak 1986). In vitro co-culture studies have demonstrated that mast cell tryptase can enhance human fibroblast chemotaxis, proliferation and pro-collagen synthesis (Gruber et al. 1997). Murine studies have demonstrated that mMCP-6 tryptase release from mast cells induces fibroblast proliferation in vitro and that tryptase expressing mast cell numbers correlate with increased fibroblast numbers and synthesis of α1 type I procollagen in dysplastic skin lesions (Coussens et al. 1999). Additional mediators, released from mast cells, are likely to contribute to fibroplasia in the tumor microenvironment. For example, human mast cells secrete bioactive TGF-β1 (Kanbe et al. 1999), which is a well-documented enhancer of fibrogenesis and ECM molecule synthesis in the tumor microenvironment (Bissell 2001). In addition to mast cell derived TGF-β, MMP activation by mast cell proteases is likely to induce the activation of ECM-bound forms of latent TGF-β in the tumor microenvironment potentiating the response.
Mast cells contribute to de-regulated tissue homeostasis in the tumor microenvironment. (1) Activated mast cells release many pro-angiogenic factors, which enhance endothelial cell migration, proliferation and blood vessel formation. (2) Mast cells secrete multiple proteases, which degrade the extracellular matrix (ECM) and release growth factors that have been sequestered in the ECM to enhance fibroblast proliferation and the angiogenic response. (3) Mast cells also enhance fibroplasia in the tumor microenvironment through their release of mediators that induce fibroblast proliferation and differentiation into myofibroblasts. (4) Fibroblasts and myofibroblasts activated by mast cell mediators synthesize ECM molecules, contributing to tissue remodelling events. (5) Mast cells indirectly modulate the tumor microenvironment through their release of multiple chemokines, which mediate the recruitment of additional immune effector cells to tumor sites
Myofibroblasts are contractile fibroblasts which express features of smooth muscle differentiation. They are important contributors to tissue remodelling through their release of mediators that interact with epithelial cells, production of ECM components and their ability to provide contractile force to facilitate wound closure. Tissue remodelling events in the tumor microenvironment are likely influenced via the direct actions of mast cell mediators on myofibroblasts. Numbers of α-smooth muscle actin (SMA) expressing myofibroblasts correlate with tryptase positive mast cells in human breast cancer tissue (Mangia et al. 2011). In vitro, human mast cell tryptase and histamine induce α-SMA expression in dermal fibroblasts and tryptase also stimulates their ability to contract a collagen matrix (Gailit et al. 2001). Thus, through direct release of ECM degrading enzymes and interactions with stromal cells mast cells are important contributors to the remodelling events that occur during tumorigenesis.
Tumor metastasis involves tissue remodelling events which enable tumor invasiveness and spread. Migration and invasiveness of tumor cells are considered prerequisites for tumor metastasis and a high mast cell density often correlates with lymph node metastases (Esposito et al. 2004; Cai et al. 2011; Elpek et al. 2001). Early evidence for a role of mast cells in tumor metastasis comes from experimental tumor models where metastasis incidence is decreased in mast cell deficient mice (Starkey et al. 1988; Dethlefsen et al. 1994). Several groups have demonstrated that mast cell mediators can increase tumor cell migration and invasiveness in vitro. For example, chymase degrades fibronectin and enhances cervical cancer cell detachment, while tryptase increases invasion and metastasis of breast cancer cells and activates the ECM degrading gelatinase pro-MMP-2 (Diaconu et al. 2011; Xiang et al. 2010). Many mediators released from mast cells (e.g., histamine, leukotrienes, TNF, VEGF, tryptase) can increase vascular permeability (Kunder et al. 2011) and may thereby enhance tumor cell extravasation and spread.
4 Mast Cell Regulation of Tumor Immunity Within the Tumor Microenvironment
4.1 Mast Cell Regulation of Anti-Tumor Immune Responses
Mast cells can have profound effects on immune regulation relevant to the tumor microenvironment through mediator production and potentially through direct interactions with effector cells. Mast cells are sentinel cells with the ability to alert and mobilize immune responses through both the recruitment of effector cells and the initiation of immune processes. In the context of a tumor microenvironment, however, mast cells are often not activated by pathways that lead to a full complement of mediator release. As a consequence, depending upon the available microenvironmental or therapy-derived signals mast cells can both enhance and inhibit effective anti-tumor immune responses through distinct pathways.
A number of pathways exist whereby mast cells can have immunosuppressive functions. These include the direct release of immunosuppressive cytokines, the enhancement of activity or recruitment of suppressive cell types such as regulatory T cells (Treg) and myeloid derived suppressor cells (MDSC) as well as the impact of preformed granule products such as proteases and histamine. Human and rodent mast cells can be substantial sources of a number of cytokines that could limit local or systemic anti-tumor immunity. These include both TGF-β and IL-10. While we have little information on microenvironmental factors that induce selective production of such mediators, the potential for them playing a role in limiting local immunity is clear. Vitamin D3 has been demonstrated to be an important factor in inducing selective mast cell production of IL-10 in the skin (Grimbaldeston et al. 2007) and intensive research is underway to identify other relevant factors with similar activity. The action of mast cell proteases in activating latent TGF-β could add to their immunosuppressive role following mast cell degranulation. An additional immunosuppressive activity of proteases may be in the degradation of other bioactive cytokines and chemokines rendering them inactive. This could limit the long term recruitment of certain cell types, although in murine models, mast cell proteases have been shown to be important for acute selective inflammatory cell recruitment by a separate mechanism (Shin et al. 2009; Huang et al. 1998).
Mast cell interactions with MDSCs may also impact effective tumor immunity. In a murine hepatocellular carcinoma model it was observed that mast cells could mobilize the infiltration of MDSCs and induce their production of IL-17. In turn, MDSC-derived IL-17 acted to mobilize Treg cells, enhancing their suppressor function and inducing IL-9 production. The IL-9 produced locally then had the capacity to promote the survival of mast cells in the tumor microenvironment (Yang et al. 2010). In marked contrast, a more recent study has demonstrated that the ability of monocyte–like MDSCs to exert an immune suppressive effect in a murine model of B16 melanoma metastasis was highly dependent on interactions with mast cells. This was further contrasted by a mast cell dependent immunostimulatory effect of granulocyte related MDSCs in a nematode parasite model (Saleem et al. 2012). Whether these mechanisms occur in a human tumor setting remains unclear.
Histamine has been widely studied as a potential inhibitor of effective anti-tumor immunity as in some situations it may reduce the development of effective acquired immune responses to tumors. In addition, histamine may impact more directly on tumor growth, since several tumor cell types express histamine receptors (Lieberman 2011). The high histamine content of many human tumors, largely as a result of associated tissue mast cells has been cited as having both pro- and anti-tumorigenic effects. Histamine is one of the major mediators leading to the pathologic events that follow allergic activation. Important immunomodulatory roles for histamine have been observed, controlling both innate and adaptive immune responses, through actions on H1 and H2 receptors on immune cells. Histamine acting via H2 on monocytes and phagocytes can block their cell-contact dependent immune suppression of natural killer (NK) cells to enhance natural and antibody mediated NK cell cytotoxicity (Hellstrand and Hermodsson 1991; Hellstrand et al. 1994) and prevent phagocyte derived reactive oxygen species down-regulation of NKp46 and NKG2D activating receptors (Romero et al. 2006). Histamine is also an important regulator of adaptive immune responses via its actions on dendritic cell (DC) and T cell subsets. Studies in H1R−/− mice have demonstrated that H1 engagement on DC is necessary for DC activation and subsequent priming of IFN-γ producing CD8+ T cells (Vanbervliet et al. 2011). Histamine, via H2, can modulate the differentiation, activation and functional activities of monocyte derived DC subsets (Simon et al. 2011), enhance antigen uptake by immature DC, induce the recruitment of CD11b+ DC and plasmacytoid DC (pDC) to draining lymph nodes (Dawicki et al. 2010) and modulate cytokine production in activated pDC (Mazzoni et al. 2003). Histamine is also a potent T cell regulator, which has been demonstrated to enhance TH1-type responses and inhibit Treg suppression via the H1 receptor but suppress both TH1 and TH2 T cell responses through the H2 receptor (Noubade et al. 2007; Forward et al. 2009; Jutel et al. 2001).
Levels of circulating histamine are three times higher in some groups of newly diagnosed cancer patients and remain high for two months post-surgical removal (Moriarty et al. 1988). In a long term follow-up study of solid malignancies, a progressive decrease in histamine blood levels preceded clinical relapse or detection of metastasis (Burtin et al. 1983). Clinically, histamine has shown promise as an immune stimulant when combined with IL-2 immunotherapy in clinical trials of acute myeloid leukemia and melanoma patients (Hellstrand et al. 1997). The enhanced efficacy of IL-2 immunotherapy in the presence of histamine has been attributed to enhanced NK cell mediated killing of tumor cells (Hellstrand et al. 1997; Brune et al. 1996) and enhanced type 1 T cell responses (Asemissen et al. 2005). The aforementioned immunomodulatory effects of histamine indicate histamine can enhance NK cytotoxicity indirectly in a H2 dependent manner and enhance type 1 T cell responses via interactions with H1 and H2 on T cells and DC. These findings are in keeping with the results of some animal models studies which demonstrate a role for histamine in regulating colorectal cancer development following treatment with carcinogenic agents (Yang et al. 2011). Within the tumor microenvironment, histamine and histamine receptor interactions have not been fully investigated and there is much work to be done to fully understand the role of histamine within the tumor setting. However, it is clear that there is great potential for mast cells to modulate tumor immunity and microenvironmental changes through histamine dependent mechanisms.
4.1.1 Mast Cells and Dendritic Cells Within the Tumor Microenvironment
A number of studies have shown that both histamine and mast cells have an important role in regulating DC populations and their mobilization. This work has been mainly carried out using models of infection or allergic disease. However, it has important implications for the potential impact on mast cells in the tumor microenvironment. A number of mast cell mediators including histamine and TNF have substantial effects on DC mobilization and polarization. DC migration from the tissue into the draining lymph node is a critical first step for the generation of an effective immune response. Early studies of Langerhan’s cells in the skin demonstrated that mast cell activation with IgE/antigen can lead to the mobilization of DC out of the epidermis and into the draining lymph node by a mechanism that was dependent on mast cells, TNF and histamine (Jawdat et al. 2004). Similarly, bacterial peptidoglycan treatment of the skin led to the mobilization of Langerhan’s cells by a mast cell dependent mechanism, although in this case the response was TNF independent. From more recent studies it has become apparent that mast cells also have important roles in the mobilization of other DC subsets of particular importance for the development of anti-tumor immunity including CD8+ DC and pDC (Dawicki et al. 2010). Interaction between mast cells and DC has also been shown to enhance TH1 and TH17 responses (Dudeck et al. 2011) which, depending upon the stage of tumor development and location, could either aid in effective tumor immunity development or promote inflammatory changes that enhance local angiogenesis. In other settings, it has been demonstrated that mast cell activators can serve as effective vaccine adjuvants with potential for cancer therapy (McLachlan et al. 2008). The recent recognition of important roles for c-Kit in DC biology may suggest that the direct impact of c-Kit on DCs needs to be considered in interpreting findings from mast cell deficient mouse models.
4.1.2 Mast Cell Effects on Local T Cell Populations
The role of mast cells may not always be to enhance tumor immunity through interactions with DCs. For example, prostanoids produced by mast cells in response to IgE-mediated activation, while potentially limiting angiogenesis (Murata et al. 2011) could act on DP1 receptors on dendritic cells to promote Treg development (Hammad et al. 2007). PGD2 has also been shown to inhibit IL-12 responses by DC leading to increased TH2 polarization (Theiner et al. 2006), potentially further restricting the development of an effective anti-tumor T cell response.
Mast cells may modulate T cell responses by mechanisms that are independent of effects on dendritic cell function (Nakae et al. 2006). Such interactions can include the direct effects of mast cell mediators such as TNF and histamine as well as cell contact dependent events. Mast cell modulation of local Treg populations within the tumor microenvironment may be of particular importance in dictating the effectiveness of T cell responses to tumors. Mast cells are an excellent source of IL-6 following activation with multiple different stimuli. In particular, mast cell IL-6 can be produced selectively following TLR-mediated activation or following IgE mediated mast cell activation, in the latter case associated with degranulation. IL-6 plays a critical role in regulating the function of Treg cells and can alter the activities of such cells so that they develop pro-inflammatory TH17 characteristics. Since an abundance of Treg cells within the tumor microenvironment is one mechanism whereby immune responses to tumors are thought to be frequently suppressed, activation of mast cells could provide opportunities to reduce local Treg activities.
4.1.3 Cell Recruitment via Chemokine Production
During early infection and inflammation mast cells bring effector cells to local tissue sites (reviewed in Marshall 2004). This occurs as a consequence of a multi-step recruitment process that involves increased adhesion interactions, altered vascular permeability as well as direct chemoattractant actions. Although mast cells can influence all of these steps, the extent to which these processes occur in a tumor microenvironment, in the absence of immunotherapy, remains unclear. Mast cell influence on many immune responses has frequently been associated with production of TNF. This cytokine is produced following mast cell activation and has also been reported to be preformed and associated with mast cell granules and released immediately upon degranulation. One of the major actions of TNF is the up-regulation of adhesion molecules on the vascular endothelium. IL-1 produced by mast cells would also contribute to such vascular effects.
Multiple chemokines can be produced by mast cells, however, they are known to be a particularly potent tissue source of CXCL8, CCL3, CCL4, CCL5 and CXCL10 and also produce other key chemokines such as CCL2 and CXCL9. Mast cell derived CXCL8 can not only recruit neutrophils, but has more recently been shown to be a potent and selective inducer of human NK cell recruitment in the context of virally activated mast cells (Burke et al. 2008). In contrast, CCR3 and CCR5 ligands have been shown to be more important for the recruitment of CD56+ T cells, including invariant NKT cells as well as cytotoxic T cells (McAlpine et al. 2012). In granulomas, neutrophils recruited as a result of mast cell derived TNF production, have also been implicated as an important source of CCL3 (von Stebut et al. 2003). This illustrates the types of complex cell–cell interactions that can lead to a chemokine rich microenvironment. In the B16 mouse melanoma model CCL2 and CCL3 have been demonstrated to have important roles in host immunity and prevention of metastasis (Nakasone et al. 2012). Notably CCL2 is also active in mast cell recruitment. CCL3 has also been shown to be critical for the development of immune responses following tumor cell apoptosis (Iida et al. 2008). Both mast cells and macrophages probably contribute to such critical chemokine responses.
CXCR3 ligands (CXCL9, CXCL10 and CXCL11) are all found in tissue microenvironments and contribute to angiogenic responses as well as to the recruitment of T cells to tumor sites. Human mast cells can produce CXCL10 in response to IFN-γ or to viral infection. IFN-γ is frequently increased at local tumor sites, as are CXCR3 ligands. Recently, it has been shown that CXCR3 ligands can also cause partial mast cell degranulation and activate several signaling pathways that could result in cytokine and chemokine production from mast cells (Willox et al. 2010). This could be an important mechanism for local mast cell activation within a tumor setting with CXCR3 ligands providing a regulatory link between the processes of angiogenesis and cell recruitment.
4.2 Mast Cells and Tumor Immunotherapy
Mast cells represent attractive targets for anti-cancer immunotherapy due to their abundance at the periphery of many solid tumors and ideal location in close proximity to blood vessels. In concordance with the well documented pro-tumorigenic roles of mast cells, several groups have suggested that therapeutic strategies that are designed to inhibit mast cells and their mediators are viable approaches for the treatment of solid tumors (Groot Kormelink et al. 2009; Maltby et al. 2009). Indeed, therapeutic success has been achieved in experimental tumor models using anti-inflammatory approaches that have impact on mast cell numbers. For example infliximab treatment of experimental colitis reduced both mast cell responses and the development of later tumors (Kim et al. 2010). In a model of mast cell enhanced human thyroid tumor growth mast cell stabilization was also shown to effectively reduce tumor growth (Melillo et al. 2010). We have recently demonstrated that mast cells can play a critical role in mediating the anti-tumor effects of TLR2 targeted immunotherapy in a murine model of melanoma and that TLR2 activated mast cells can recruit NK cells and T cells in a CCL3-dependent manner (Oldford et al. 2010). Mast cells have also been demonstrated to be crucial for the recruitment of pDC via CCL2 production and regulation of anti-tumor immunity following TLR7 targeted immunotherapy of murine melanoma (Drobits et al. 2012). These data suggest an alternate approach that harnesses the immune potential of mast cells and specifically targets the sentinel role of mast cells using innate immune activator based immunotherapy strategies. In contrast to other immune cells, mast cells are relatively radioresistant (Soule et al. 2007), which makes them prime candidates for combined treatment modalities. Furthermore, widespread inhibition of mast cell function may not be advantageous for all tumor types. Inhibition of mast cell function by administration of imatinib mesylate (GLEEVEC™), a receptor tyrosine kinase inhibitor which inhibits c-Kit, resulted in increased mammary cancer development and peritumoral blood clotting in a murine model of breast carcinoma (Samoszuk and Corwin 2003). In a murine model of prostate carcinoma imatinib administration decreased the incidence of prototypical prostate carcinoma, but increased the incidence of prostate carcinomas with the more aggressive neuroendocrine phenotype (Pittoni et al. 2011). Thus, it is evident that the influence of mast cells on the tumor microenvironment is complex and is likely dependent on the state of mast cell activation at the tumor site. Selective mast cell activation therefore provides a novel opportunity to modify the tumor microenvironment for successful cancer immunotherapy.
The use of monoclonal IgE antibodies directed against tumor associated antigens has shown some success in experimental tumor models (Jensen-Jarolim et al. 2008). The effectiveness of this treatment may be the result of a variety of mechanisms including the enhanced recruitment of effector cells, the direct impact of mediators on tumor cells and impact on immune regulation. IgE-mediated mast cell degranulation can overcome allograft tolerance and elicit effector CD4+ and CD8+ T cell mediated rejection (de Vries et al. 2009). Therefore, local mast cell degranulation may be advantageous to subvert the immune suppressive microenvironment of solid tumors and elicit effective anti-tumor immunity. However, IgE mediated mast cell activation does not always overcome tolerance and in models of oral tolerance it has been shown to be ineffective in altering Treg responses (Tunis et al. 2012). More work is required to directly assess the impact of such mechanisms on T cell responses to tumors.
5 Concluding Remarks
From the discussion above, it is clear that mast cells can have multiple roles within the tumor microenvironment. These extend from the most widely known pro-tumorigenic effects of mast cells in the promotion of angiogenesis through to immune activating impacts of mast cells that could enhance effective host defence and even the use of mast cells as potential triggers for immunotherapy. The challenges we currently face in understanding and exploiting these responses therapeutically are twofold. First, we need to determine which interactions are of importance in a human tumor setting, since much of the available data has been obtained from animal models. Second, to develop strategies to exploit or alter human mast cell responses within the tumor microenvironment appropriately and selectively such that their positive roles can be enhanced and their pro-tumorigenic and pro-metastatic effects can be reduced. Mast cells have enormous potential as targets to selectively alter both tissue remodelling events and immune responses if we are willing to take on these challenges.
Abbreviations
- APC:
-
Adenomatous polyposis coli
- bFGF :
-
basic fibroblast growth factor
- CTMC:
-
Connective tissue mast cell
- DAMPs:
-
Danger associated molecular patterns
- DC:
-
Dendritic cells
- ECM:
-
Extracellular matrix
- EPC:
-
Endothelial progenitor cells
- H1 :
-
Histamine receptor 1
- H2 :
-
Histamine receptor 2
- HIF-1α:
-
Hypoxia inducible factor alpha
- HMGB1:
-
High-mobility group protein B1
- IFN-γ:
-
Interferon gamma
- Ig:
-
Immunoglobulin
- IL:
-
Interleukin
- LT:
-
Leukotriene
- MCP:
-
Mast cell protease
- MDSC:
-
Myeloid derived suppressor cells
- MMC:
-
Mucosal mast cell
- MMP:
-
Matrix metalloproteinase
- NK:
-
Natural killer cells
- NKT:
-
Natural killer T cells
- PAF:
-
Platelet activating factor
- pDC:
-
Plasmacytoid Dendritic cells
- PG:
-
Prostaglandin
- ROS:
-
Reactive oxygen species
- SCF:
-
Stem cell factor
- SMA:
-
Smooth muscle actin
- TGF-β:
-
Transforming growth factor beta
- TLR:
-
Toll-like receptor
- TNF:
-
Tumor necrosis factor
- TH :
-
Helper T cells
- Treg :
-
Regulatory T cells
- VEGF:
-
Vascular endothelial growth factor
References
Abdel-Majid RM, Marshall JS (2004) Prostaglandin E2 induces degranulation-independent production of vascular endothelial growth factor by human mast cells. J Immunol 172:1227–1236
Asemissen AM, Scheibenbogen C, Letsch A, Hellstrand K, Thoren F, Gehlsen K et al (2005) Addition of histamine to interleukin 2 treatment augments type 1 T-cell responses in patients with melanoma in vivo: immunologic results from a randomized clinical trial of interleukin 2 with or without histamine (MP 104). Clin Cancer Res 11:290–297
Basu S, Binder RJ, Suto R, Anderson KM, Srivastava PK (2000) Necrotic but not apoptotic cell death releases heat shock proteins, which deliver a partial maturation signal to dendritic cells and activate the NF-kappa B pathway. Int Immunol 12:1539–1546
Benitez-Bribiesca L, Wong A, Utrera D, Castellanos E (2001) The role of mast cell tryptase in neoangiogenesis of premalignant and malignant lesions of the uterine cervix. J Histochem Cytochem Off J Histochem Soc 49:1061–1062
Benyon RC, Bissonnette EY, Befus AD (1991) Tumor necrosis factor-alpha dependent cytotoxicity of human skin mast cells is enhanced by anti-IgE antibodies. J Immunol 147:2253–2258
Bischoff SC, Sellge G, Lorentz A, Sebald W, Raab R, Manns MP (1999) IL-4 enhances proliferation and mediator release in mature human mast cells. Proc Natl Acad Sci U S A 96:8080–8085
Bissell DM (2001) Chronic liver injury, TGF-beta, and cancer. Exp Mol Med 33:179–190
Boyce JA (2007) Mast cells and eicosanoid mediators: a system of reciprocal paracrine and autocrine regulation. Immunol Rev 217:168–185
Branitzki-Heinemann K, Okumura CY, Vollger L, Kawakami Y, Kawakami T, Naim HY et al (2012) A novel role for the transcription factor HIF-1alpha in the formation of mast cell extracellular traps. Biochem J 446:159–163
Brown MA, Hatfield JK, Walker ME, Sayed BA (2012) A game of kit and mouse: the Kit is still in the bag. Immunity 36:891–892 (author reply 3-4)
Brune M, Hansson M, Mellqvist UH, Hermodsson S, Hellstrand K (1996) NK cell-mediated killing of AML blasts: role of histamine, monocytes and reactive oxygen metabolites. Eur J Haematol 57:312–319
Burke SM, Issekutz TB, Mohan K, Lee PW, Shmulevitz M, Marshall JS (2008) Human mast cell activation with virus-associated stimuli leads to the selective chemotaxis of natural killer cells by a CXCL8-dependent mechanism. Blood 111:5467–5476
Burtin C, Noirot C, Paupe J, Scheinmann P (1983) Decreased blood histamine levels in patients with solid malignant tumours. Br J Cancer 47:367–372
Byrne SN, Beaugie C, O’Sullivan C, Leighton S, Halliday GM (2011) The immune-modulating cytokine and endogenous Alarmin interleukin-33 is upregulated in skin exposed to inflammatory UVB radiation. Am J Pathol 179:211–222
Cai SW, Yang SZ, Gao J, Pan K, Chen JY, Wang YL et al (2011) Prognostic significance of mast cell count following curative resection for pancreatic ductal adenocarcinoma. Surgery 149:576–584
Caruso RA, Ieni A, Fabiano V, Basile G, Inferrera C (2004) Perivascular mast cells in advanced gastric adenocarcinomas: an electron microscopic study. Anticancer Res 24:2257–2263
Caughey GH (2011) Mast cell proteases as protective and inflammatory mediators. Adv Exp Med Biol 716:212–234
Chan JK, Roth J, Oppenheim JJ, Tracey KJ, Vogl T, Feldmann M et al (2012) Alarmins: awaiting a clinical response. J Clin Investig 122:2711–2719
Ciocca DR, Calderwood SK (2005) Heat shock proteins in cancer: diagnostic, prognostic, predictive, and treatment implications. Cell Stress Chaperones 10:86–103
Conti P, Castellani ML, Kempuraj D, Salini V, Vecchiet J, Tete S et al (2007) Role of mast cells in tumor growth. Ann Clin Lab Sci 37:315–322
Coussens LM, Raymond WW, Bergers G, Laig-Webster M, Behrendtsen O, Werb Z et al (1999) Inflammatory mast cells up-regulate angiogenesis during squamous epithelial carcinogenesis. Genes Dev 13:1382–1397
Crivellato E, Beltrami C, Mallardi F, Ribatti D (2003) Paul Ehrlich’s doctoral thesis: a milestone in the study of mast cells. Br J Haematol 123:19–21
Dawicki W, Marshall JS (2007) New and emerging roles for mast cells in host defence. Curr Opin Immunol 19:31–38
Dawicki W, Jawdat DW, Xu N, Marshall JS (2010) Mast cells, histamine, and IL-6 regulate the selective influx of dendritic cell subsets into an inflamed lymph node. J Immunol 184:2116–2123
de Souza DA Jr, Toso VD, Campos MR, Lara VS, Oliver C, Jamur MC (2012) Expression of mast cell proteases correlates with mast cell maturation and angiogenesis during tumor progression. PloS ONE 7:e40790
de Vries VC, Wasiuk A, Bennett KA, Benson MJ, Elgueta R, Waldschmidt TJ et al (2009) Mast cell degranulation breaks peripheral tolerance. Am J Transpl Off J Am Soc Transpl Am Soc Transpl Surg 9:2270–2280
Dery RE, Lin TJ, Befus AD, Milne CD, Moqbel R, Menard G et al (2000) Redundancy or cell-type-specific regulation? Tumour necrosis factor in alveolar macrophages and mast cells. Immunology 99:427–434
Dethlefsen SM, Matsuura N, Zetter BR (1994) Mast cell accumulation at sites of murine tumor implantation: implications for angiogenesis and tumor metastasis. Invasion Metastasis 14:395–408
Detoraki A, Staiano RI, Granata F, Giannattasio G, Prevete N, de Paulis A et al (2009) Vascular endothelial growth factors synthesized by human lung mast cells exert angiogenic effects. J Allergy Clin Immunol 123:1142–1149, 9 e1-5
Di Nardo A, Vitiello A, Gallo RL (2003) Cutting edge: mast cell antimicrobial activity is mediated by expression of cathelicidin antimicrobial peptide. J Immunol 170:2274–2278
Diaconu NC, Rummukainen J, Naukkarinen A, Matto M, Harvima RJ, Pelkonen J et al (2011) Mast cell chymase is present in uterine cervical carcinoma and it detaches viable and growing cervical squamous carcinoma cells from substratum in vitro. Arch Dermatol Res 303:499–512
Drobits B, Holcmann M, Amberg N, Swiecki M, Grundtner R, Hammer M et al (2012) Imiquimod clears tumors in mice independent of adaptive immunity by converting pDCs into tumor-killing effector cells. J Clin Investig 122:575–585
Dudeck A, Dudeck J, Scholten J, Petzold A, Surianarayanan S, Kohler A et al (2011) Mast cells are key promoters of contact allergy that mediate the adjuvant effects of haptens. Immunity 34:973–984
Dvorak HF (1986) Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med 315:1650–1659
Elpek GO, Gelen T, Aksoy NH, Erdogan A, Dertsiz L, Demircan A et al (2001) The prognostic relevance of angiogenesis and mast cells in squamous cell carcinoma of the oesophagus. J Clin Pathol 54:940–944
Enoksson M, Lyberg K, Moller-Westerberg C, Fallon PG, Nilsson G, Lunderius-Andersson C (2011) Mast cells as sensors of cell injury through IL-33 recognition. J Immunol 186:2523–2528
Esposito I, Menicagli M, Funel N, Bergmann F, Boggi U, Mosca F et al (2004) Inflammatory cells contribute to the generation of an angiogenic phenotype in pancreatic ductal adenocarcinoma. J Clin Pathol 57:630–636
Feyerabend TB, Weiser A, Tietz A, Stassen M, Harris N, Kopf M et al (2011) Cre-mediated cell ablation contests mast cell contribution in models of antibody- and T cell-mediated autoimmunity. Immunity 35:832–844
Finotto S, Dolovich J, Denburg JA, Jordana M, Marshall JS (1994) Functional heterogeneity of mast cells isolated from different microenvironments within nasal polyp tissue. Clin Exp Immunol 95:343–350
Fischer M, Juremalm M, Olsson N, Backlin C, Sundstrom C, Nilsson K et al (2003) Expression of CCL5/RANTES by Hodgkin and Reed-Sternberg cells and its possible role in the recruitment of mast cells into lymphomatous tissue. Int J Cancer J Int du Cancer 107:197–201
Fleischmann A, Schlomm T, Kollermann J, Sekulic N, Huland H, Mirlacher M et al (2009) Immunological microenvironment in prostate cancer: high mast cell densities are associated with favorable tumor characteristics and good prognosis. Prostate 69:976–981
Folkman J (1990) What is the evidence that tumors are angiogenesis dependent? J Natl Cancer Inst 82:4–6
Forward NA, Furlong SJ, Yang Y, Lin TJ, Hoskin DW (2009) Mast cells down-regulate CD4+CD25+ T regulatory cell suppressor function via histamine H1 receptor interaction. J Immunol 183:3014–3022
Gailit J, Marchese MJ, Kew RR, Gruber BL (2001) The differentiation and function of myofibroblasts is regulated by mast cell mediators. J Invest Dermatol 117:1113–1119
Galli SJ, Tsai M (2008) Mast cells: versatile regulators of inflammation, tissue remodeling, host defense and homeostasis. J Dermatol Sci 49:7–19
Galli SJ, Nakae S, Tsai M (2005) Mast cells in the development of adaptive immune responses. Nat Immunol 6:135–142
Gounaris E, Erdman SE, Restaino C, Gurish MF, Friend DS, Gounari F et al (2007) Mast cells are an essential hematopoietic component for polyp development. Proc Natl Acad Sci U S A 104:19977–19982
Grimbaldeston MA, Chen CC, Piliponsky AM, Tsai M, Tam SY, Galli SJ (2005) Mast cell-deficient W-sash c-kit mutant Kit W-sh/W-sh mice as a model for investigating mast cell biology in vivo. Am J Pathol 167:835–848
Grimbaldeston MA, Nakae S, Kalesnikoff J, Tsai M, Galli SJ (2007) Mast cell-derived interleukin 10 limits skin pathology in contact dermatitis and chronic irradiation with ultraviolet B. Nat Immunol 8:1095–1104
Groot Kormelink T, Abudukelimu A, Redegeld FA (2009) Mast cells as target in cancer therapy. Current Pharm Design 15:1868–1878
Gruber BL, Marchese MJ, Kew RR (1994) Transforming growth factor-beta 1 mediates mast cell chemotaxis. J Immunol 152:5860–5867
Gruber BL, Kew RR, Jelaska A, Marchese MJ, Garlick J, Ren S et al (1997) Human mast cells activate fibroblasts: tryptase is a fibrogenic factor stimulating collagen messenger ribonucleic acid synthesis and fibroblast chemotaxis. J Immunol 158:2310–2317
Gulliksson M, Carvalho RF, Ulleras E, Nilsson G (2010) Mast cell survival and mediator secretion in response to hypoxia. PLoS ONE 5:e12360
Gurish MF, Austen KF (2012) Developmental origin and functional specialization of mast cell subsets. Immunity 37:25–33
Halova I, Draberova L, Draber P (2012) Mast cell chemotaxis—chemoattractants and signaling pathways. Frontiers Immunol 3:119
Hammad H, Kool M, Soullie T, Narumiya S, Trottein F, Hoogsteden HC et al (2007) Activation of the D prostanoid 1 receptor suppresses asthma by modulation of lung dendritic cell function and induction of regulatory T cells. J Exp Med 204:357–367
Hedstrom G, Berglund M, Molin D, Fischer M, Nilsson G, Thunberg U et al (2007) Mast cell infiltration is a favourable prognostic factor in diffuse large B-cell lymphoma. Br J Haematol 138:68–71
Hellstrand K, Hermodsson S (1991) Cell-to-cell mediated inhibition of natural killer cell proliferation by monocytes and its regulation by histamine H2-receptors. Scand J Immunol 34:741–752
Hellstrand K, Asea A, Hermodsson S (1994) Histaminergic regulation of antibody-dependent cellular cytotoxicity of granulocytes, monocytes, and natural killer cells. J Leukoc Biol 55:392–397
Hellstrand K, Hermodsson S, Brune M, Naredi P, Carneskog J, Mellqvist UH (1997) Histamine in cancer immunotherapy. Scand J Clin Lab Invest 57:193–202
Hsu CL, Neilsen CV, Bryce PJ (2010) IL-33 is produced by mast cells and regulates IgE-dependent inflammation. PLoS ONE 5:e11944
Huang C, Friend DS, Qiu WT, Wong GW, Morales G, Hunt J et al (1998) Induction of a selective and persistent extravasation of neutrophils into the peritoneal cavity by tryptase mouse mast cell protease 6. J Immunol 160:1910–1919
Huang B, Lei Z, Zhang GM, Li D, Song C, Li B et al (2008) SCF-mediated mast cell infiltration and activation exacerbate the inflammation and immunosuppression in tumor microenvironment. Blood 112:1269–1279
Iida N, Nakamoto Y, Baba T, Kakinoki K, Li YY, Wu Y et al (2008) Tumor cell apoptosis induces tumor-specific immunity in a CC chemokine receptor 1- and 5-dependent manner in mice. J Leukoc Biol 84:1001–1010
Irani AA, Schechter NM, Craig SS, DeBlois G, Schwartz LB (1986) Two types of human mast cells that have distinct neutral protease compositions. Proc Natl Acad Sci U S A 83:4464–4468
Irani AM, Goldstein SM, Wintroub BU, Bradford T, Schwartz LB (1991) Human mast cell carboxypeptidase. Selective localization to MCTC cells. J Immunol 147:247–253
Jawdat DM, Albert EJ, Rowden G, Haidl ID, Marshall JS (2004) IgE-mediated mast cell activation induces Langerhans cell migration in vivo. J Immunol 173:5275–5282
Jensen-Jarolim E, Achatz G, Turner MC, Karagiannis S, Legrand F, Capron M et al (2008) AllergoOncology: the role of IgE-mediated allergy in cancer. Allergy 63:1255–1266
Johansson A, Rudolfsson S, Hammarsten P, Halin S, Pietras K, Jones J et al (2010) Mast cells are novel independent prognostic markers in prostate cancer and represent a target for therapy. Am J Pathol 177:1031–1041
Juremalm M, Olsson N, Nilsson G (2002) Selective CCL5/RANTES-induced mast cell migration through interactions with chemokine receptors CCR1 and CCR4. Biochem Biophys Res Commun 297:480–485
Jutel M, Watanabe T, Klunker S, Akdis M, Thomet OA, Malolepszy J et al (2001) Histamine regulates T-cell and antibody responses by differential expression of H1 and H2 receptors. Nature 413:420–425
Kanbe N, Kurosawa M, Nagata H, Saitoh H, Miyachi Y (1999) Cord blood-derived human cultured mast cells produce transforming growth factor beta1. Clin Exp Allergy J British Soc Allergy Clinical Immunol 29:105–113
Kandere-Grzybowska K, Letourneau R, Kempuraj D, Donelan J, Poplawski S, Boucher W et al (2003) IL-1 induces vesicular secretion of IL-6 without degranulation from human mast cells. J Immunol 171:4830–4836
Kankkunen JP, Harvima IT, Naukkarinen A (1997) Quantitative analysis of tryptase and chymase containing mast cells in benign and malignant breast lesions. Int J Cancer J Int du Cancer 72:385–388
Katz HR, Stevens RL, Austen KF (1985) Heterogeneity of mammalian mast cells differentiated in vivo and in vitro. J Allergy Clin Immunol 76:250–259
Kim YJ, Hong KS, Chung JW, Kim JH, Hahm KB (2010) Prevention of colitis-associated carcinogenesis with infliximab. Cancer Prev Res 3:1314–1333
Kryczek I, Lange A, Mottram P, Alvarez X, Cheng P, Hogan M et al (2005) CXCL12 and vascular endothelial growth factor synergistically induce neoangiogenesis in human ovarian cancers. Cancer Res 65:465–472
Kunder CA, St John AL, Abraham SN (2011) Mast cell modulation of the vascular and lymphatic endothelium. Blood 118:5383–5393
Leal-Berumen I, O’Byrne P, Gupta A, Richards CD, Marshall JS (1995) Prostanoid enhancement of interleukin-6 production by rat peritoneal mast cells. J Immunol 154:4759–4767
Lieberman P (2011) The basics of histamine biology. Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol 106:S2–S5
Lin TJ, Issekutz TB, Marshall JS (2001) SDF-1 induces IL-8 production and transendothelial migration of human cord blood-derived mast cells. Int Arch Allergy Immunol 124:142–145
Lloyd HG, Ross L, Li KM, Ludowyke RI (1998) Evidence that IgE receptor stimulation increases adenosine release from rat basophilic leukaemia (RBL-2H3) cells. Pulm Pharmacol Ther 11:41–46
Maltby S, Khazaie K, McNagny KM (2009) Mast cells in tumor growth: angiogenesis, tissue remodelling and immune-modulation. Biochim Biophys Acta 1796:19–26
Mangia A, Malfettone A, Rossi R, Paradiso A, Ranieri G, Simone G et al (2011) Tissue remodelling in breast cancer: human mast cell tryptase as an initiator of myofibroblast differentiation. Histopathology 58:1096–1106
Marshall JS (2004) Mast-cell responses to pathogens. Nat Rev Immunol 4:787–799
Matsuo Y, Ochi N, Sawai H, Yasuda A, Takahashi H, Funahashi H et al (2009) CXCL8/IL-8 and CXCL12/SDF-1alpha co-operatively promote invasiveness and angiogenesis in pancreatic cancer. Int J Cancer J Int du Cancer 124:853–861
Mazzoni A, Leifer CA, Mullen GE, Kennedy MN, Klinman DM, Segal DM (2003) Cutting edge: histamine inhibits IFN-alpha release from plasmacytoid dendritic cells. J Immunol 170:2269–2273
McAlpine SM, Issekutz TB, Marshall JS (2012) Virus stimulation of human mast cells results in the recruitment of CD56(+) T cells by a mechanism dependent on CCR5 ligands. FASEB J 26:1280–1289
McCurdy JD, Olynych TJ, Maher LH, Marshall JS (2003) Cutting edge: distinct toll-like receptor 2 activators selectively induce different classes of mediator production from human mast cells. J Immunol 170:1625–1629
McLachlan JB, Shelburne CP, Hart JP, Pizzo SV, Goyal R, Brooking-Dixon R et al (2008) Mast cell activators: a new class of highly effective vaccine adjuvants. Nat Med 14:536–541
Melillo RM, Guarino V, Avilla E, Galdiero MR, Liotti F, Prevete N et al (2010) Mast cells have a protumorigenic role in human thyroid cancer. Oncogene 29:6203–6215
Mierke CT, Ballmaier M, Werner U, Manns MP, Welte K, Bischoff SC (2000) Human endothelial cells regulate survival and proliferation of human mast cells. J Exp Med 192:801–811
Mohtasham N, Babakoohi S, Salehinejad J, Montaser-Kouhsari L, Shakeri MT, Shojaee S et al (2010) Mast cell density and angiogenesis in oral dysplastic epithelium and low- and high-grade oral squamous cell carcinoma. Acta Odontol Scand 68:300–304
Moriarty CM, Stucky JL, Hamburger KW, Patil KD, Foley JF, Koefoot RR (1988) Blood histamine and solid malignant tumors. J Cancer Res Clin Oncol 114:588–592
Murata T, Aritake K, Matsumoto S, Kamauchi S, Nakagawa T, Hori M et al (2011) Prostagladin D2 is a mast cell-derived antiangiogenic factor in lung carcinoma. Proc Natl Acad Sci U S A 108:19802–19807
Nakae S, Suto H, Iikura M, Kakurai M, Sedgwick JD, Tsai M et al (2006) Mast cells enhance T cell activation: importance of mast cell costimulatory molecules and secreted TNF. J Immunol 176:2238–2248
Nakasone Y, Fujimoto M, Matsushita T, Hamaguchi Y, Huu DL, Yanaba M et al (2012) Host-derived MCP-1 and MIP-1alpha regulate protective anti-tumor immunity to localized and metastatic B16 melanoma. Am J Pathol 180:365–374
Nakayama T, Yao L, Tosato G (2004) Mast cell-derived angiopoietin-1 plays a critical role in the growth of plasma cell tumors. J Clin Investig 114:1317–1325
Negri E, Bosetti C, La Vecchia C, Levi F, Tomei F, Franceschi S (1999) Allergy and other selected diseases and risk of colorectal cancer. Eur J Cancer 35:1838–1841
Nigrovic PA, Gray DH, Jones T, Hallgren J, Kuo FC, Chaletzky B et al (2008) Genetic inversion in mast cell-deficient (Wsh) mice interrupts corin and manifests as hematopoietic and cardiac aberrancy. Am J Pathol 173:1693–1701
Norrby K (2002) Mast cells and angiogenesis. APMIS: Acta Pathologica, Microbiologica, et Immunologica Scandinavica 110:355–371
Noubade R, Milligan G, Zachary JF, Blankenhorn EP, del Rio R, Rincon M et al (2007) Histamine receptor H1 is required for TCR-mediated p38 MAPK activation and optimal IFN-gamma production in mice. J Clin Investig 117:3507–3518
Oldford SA, Haidl ID, Howatt MA, Leiva CA, Johnston B, Marshall JS (2010) A critical role for mast cells and mast cell-derived IL-6 in TLR2-mediated inhibition of tumor growth. J Immunol 185:7067–7076
Olsson N, Piek E, ten Dijke P, Nilsson G (2000) Human mast cell migration in response to members of the transforming growth factor-beta family. J Leukoc Biol 67:350–356
Orimo A, Gupta PB, Sgroi DC, Arenzana-Seisdedos F, Delaunay T, Naeem R et al (2005) Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell 121:335–348
Ott VL, Cambier JC, Kappler J, Marrack P, Swanson BJ (2003) Mast cell-dependent migration of effector CD8+ T cells through production of leukotriene B4. Nat Immunol 4:974–981
Ownby DR, Ownby HE, Bailey J, Frederick J, Tilley B, Brooks SC et al (1985) Presurgical serum immunoglobulin concentrations and the prognosis of operable breast cancer in women. J Natl Cancer Inst 75:655–663
Pittoni P, Piconese S, Tripodo C, Colombo MP (2011) Tumor-intrinsic and -extrinsic roles of c-Kit: mast cells as the primary off-target of tyrosine kinase inhibitors. Oncogene 30:757–769
Polajeva J, Sjosten AM, Lager N, Kastemar M, Waern I, Alafuzoff I et al (2011) Mast cell accumulation in glioblastoma with a potential role for stem cell factor and chemokine CXCL12. PLoS ONE 6:e25222
Rajput AB, Turbin DA, Cheang MC, Voduc DK, Leung S, Gelmon KA et al (2008) Stromal mast cells in invasive breast cancer are a marker of favourable prognosis: a study of 4,444 cases. Breast Cancer Res Treat 107:249–257
Ribatti D, Crivellato E, Candussio L, Nico B, Vacca A, Roncali L et al (2001) Mast cells and their secretory granules are angiogenic in the chick embryo chorioallantoic membrane. Clin Exp Allergy J British Soc Allergy Clin Immunol 31:602–608
Ribatti D, Ranieri G, Nico B, Benagiano V, Crivellato E (2011) Tryptase and chymase are angiogenic in vivo in the chorioallantoic membrane assay. Int J Dev Biol 55:99–102
Riley JF, West GB (1953) The presence of histamine in tissue mast cells. J Physiol 120:528–537
Rizzo V, DeFouw DO (1996) Mast cell activation accelerates the normal rate of angiogenesis in the chick chorioallantoic membrane. Microvasc Res 52:245–257
Romero AI, Thoren FB, Brune M, Hellstrand K (2006) NKp46 and NKG2D receptor expression in NK cells with CD56dim and CD56bright phenotype: regulation by histamine and reactive oxygen species. Br J Haematol 132:91–98
Rudich N, Ravid K, Sagi-Eisenberg R (2012) Mast cell adenosine receptors function: a focus on the a3 adenosine receptor and inflammation. Frontiers Immunol 3:134
Saleem SJ, Martin RK, Morales JK, Sturgill JL, Gibb DR, Graham L et al (2012) Cutting edge: mast cells critically augment myeloid-derived suppressor cell activity. J Immunol 189:511–515
Samoszuk M, Corwin MA (2003) Acceleration of tumor growth and peri-tumoral blood clotting by imatinib mesylate (Gleevec). Int J Cancer J Int du Cancer 106:647–652
Samoszuk M, Kanakubo E, Chan JK (2005) Degranulating mast cells in fibrotic regions of human tumors and evidence that mast cell heparin interferes with the growth of tumor cells through a mechanism involving fibroblasts. BMC Cancer 5:121
Sarchio SN, Kok LF, O’Sullivan C, Halliday GM, Byrne SN (2012) Dermal mast cells affect the development of sunlight-induced skin tumours. Exp Dermatol 21:241–248
Schwartzbaum J, Ding B, Johannesen TB, Osnes LT, Karavodin L, Ahlbom A et al (2012) Association between prediagnostic IgE levels and risk of glioma. J Natl Cancer Inst 104:1251–1259
Sherman PW, Holland E, Sherman JS (2008) Allergies: their role in cancer prevention. Q Rev Biol 83:339–362
Shin K, Nigrovic PA, Crish J, Boilard E, McNeil HP, Larabee KS et al (2009) Mast cells contribute to autoimmune inflammatory arthritis via their tryptase/heparin complexes. J Immunol 182:647–656
Simon T, Laszlo V, Falus A (2011) Impact of histamine on dendritic cell functions. Cell Biol Int 35:997–1000
Sinnamon MJ, Carter KJ, Sims LP, Lafleur B, Fingleton B, Matrisian LM (2008) A protective role of mast cells in intestinal tumorigenesis. Carcinogenesis 29:880–886
Soucek L, Lawlor ER, Soto D, Shchors K, Swigart LB, Evan GI (2007) Mast cells are required for angiogenesis and macroscopic expansion of Myc-induced pancreatic islet tumors. Nat Med 13:1211–1218
Soule BP, Brown JM, Kushnir-Sukhov NM, Simone NL, Mitchell JB, Metcalfe DD (2007) Effects of gamma radiation on FcepsilonRI and TLR-mediated mast cell activation. J Immunol 179:3276–3286
Starkey JR, Crowle PK, Taubenberger S (1988) Mast-cell-deficient W/Wv mice exhibit a decreased rate of tumor angiogenesis. Int J Cancer J Int du Cancer 42:48–52
Stevens RL, Adachi R (2007) Protease–proteoglycan complexes of mouse and human mast cells and importance of their beta-tryptase-heparin complexes in inflammation and innate immunity. Immunol Rev 217:155–167
Sumbayev VV, Yasinska I, Oniku AE, Streatfield CL, Gibbs BF (2012) Involvement of hypoxia-inducible factor-1 in the inflammatory responses of human LAD2 mast cells and basophils. PLoS ONE 7:e34259
Theiner G, Gessner A, Lutz MB (2006) The mast cell mediator PGD2 suppresses IL-12 release by dendritic cells leading to Th2 polarized immune responses in vivo. Immunobiology 211:463–472
Theoharides TC, Conti P (2004) Mast cells: the Jekyll and Hyde of tumor growth. Trends Immunol 25:235–241
Theoharides TC, Alysandratos KD, Angelidou A, Delivanis DA, Sismanopoulos N, Zhang B et al (2012) Mast cells and inflammation. Biochim Biophys Acta 1822:21–33
Tkaczyk C, Okayama Y, Metcalfe DD, Gilfillan AM (2004) Fcgamma receptors on mast cells: activatory and inhibitory regulation of mediator release. Int Arch Allergy Immunol 133:305–315
Toth-Jakatics R, Jimi S, Takebayashi S, Kawamoto N (2000) Cutaneous malignant melanoma: correlation between neovascularization and peritumor accumulation of mast cells overexpressing vascular endothelial growth factor. Hum Pathol 31:955–960
Tunis MC, Dawicki W, Carson KR, Wang J, Marshall JS (2012) Mast cells and IgE activation do not alter the development of oral tolerance in a murine model. J Allergy Clin Immunol 130:705–15 e1
Van Nguyen H, Di Girolamo N, Jackson N, Hampartzoumian T, Bullpitt P, Tedla N et al (2011) Ultraviolet radiation-induced cytokines promote mast cell accumulation and matrix metalloproteinase production: potential role in cutaneous lupus erythematosus. Scand J Rheumatol 40:197–204
Vanbervliet B, Akdis M, Vocanson M, Rozieres A, Benetiere J, Rouzaire P et al (2011) Histamine receptor H1 signaling on dendritic cells plays a key role in the IFN-gamma/IL-17 balance in T cell-mediated skin inflammation. J Allergy Clin Immunol 127:943–953 e1-10
von Stebut E, Metz M, Milon G, Knop J, Maurer M (2003) Early macrophage influx to sites of cutaneous granuloma formation is dependent on MIP-1alpha/beta released from neutrophils recruited by mast cell-derived TNFalpha. Blood 101:210–215
Wang Z, Macleod DT, Di Nardo A (2012) Commensal bacteria lipoteichoic acid increases skin mast cell antimicrobial activity against vaccinia viruses. J Immunol 189:1551–1558
Wedemeyer J, Galli SJ (2005) Decreased susceptibility of mast cell-deficient Kit(W)/Kit(W−v) mice to the development of 1, 2-dimethylhydrazine-induced intestinal tumors. Lab Investig J Tech Methods Pathol 85:388–396
Welsh TJ, Green RH, Richardson D, Waller DA, O’Byrne KJ, Bradding P (2005) Macrophage and mast-cell invasion of tumor cell islets confers a marked survival advantage in non-small-cell lung cancer. J Clin Oncol 23:8959–8967
Willox I, Mirkina I, Westwick J, Ward SG (2010) Evidence for PI3K-dependent CXCR3 agonist-induced degranulation of human cord blood-derived mast cells. Mol Immunol 47:2367–2377
Xia Q, Wu XJ, Zhou Q, Jing Z, Hou JH, Pan ZZ et al (2011) No relationship between the distribution of mast cells and the survival of stage IIIB colon cancer patients. J Transl Med 9:88
Xiang M, Gu Y, Zhao F, Lu H, Chen S, Yin L (2010) Mast cell tryptase promotes breast cancer migration and invasion. Oncol Rep 23:615–619
Yang Z, Zhang B, Li D, Lv M, Huang C, Shen GX et al (2010) Mast cells mobilize myeloid-derived suppressor cells and Treg cells in tumor microenvironment via IL-17 pathway in murine hepatocarcinoma model. PLoS ONE 5:e8922
Yang XD, Ai W, Asfaha S, Bhagat G, Friedman RA, Jin G et al (2011) Histamine deficiency promotes inflammation-associated carcinogenesis through reduced myeloid maturation and accumulation of CD11b+Ly6G+ immature myeloid cells. Nat Med 17:87–95
Younan G, Suber F, Xing W, Shi T, Kunori Y, Abrink M et al (2010) The inflammatory response after an epidermal burn depends on the activities of mouse mast cell proteases 4 and 5. J Immunol 185:7681–7690
Zhang W, Stoica G, Tasca SI, Kelly KA, Meininger CJ (2000) Modulation of tumor angiogenesis by stem cell factor. Cancer Res 60:6757–6762
Zhu XQ, Lv JQ, Lin Y, Xiang M, Gao BH, Shi YF (2007) Expression of chemokines CCL5 and CCL11 by smooth muscle tumor cells of the uterus and its possible role in the recruitment of mast cells. Gynecol Oncol 105:650–656
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Oldford, S.A., Marshall, J.S. (2013). Mast Cell Modulation of the Tumor Microenvironment. In: Shurin, M., Umansky, V., Malyguine, A. (eds) The Tumor Immunoenvironment. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-6217-6_20
Download citation
DOI: https://doi.org/10.1007/978-94-007-6217-6_20
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-6216-9
Online ISBN: 978-94-007-6217-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)