Abstract
Sustained high-intensity exercise demands time-dependent increases in ventilation and respiratory muscle work. Exercise-induced diaphragmatic fatigue commonly occurs because of a combination of the amount of diaphragmatic work required to support the exercise hyperpnea plus the increased propensity of the diaphragm for fatigue during exercise when it must compete with the locomotor muscles for the available cardiac output. The need for blood flow to be distributed to locomotor and respiratory muscles during whole-body exercise is a major determinant of diaphragmatic fatigue. Exercise-induced diaphragmatic fatigue does not generally result in an inadequate ventilatory response to exercise. Rather, high levels of respiratory muscle work leading to diaphragmatic fatigue were shown to cause sympathetically mediated vasoconstriction of resting limb vasculature and relieving most of this work of breathing during heavy exercise increased limb blood flow, reduced the severity of limb fatigue, and enhanced endurance exercise performance. Whether specific training of the respiratory muscles is sufficient to prevent or delay the activation of respiratory muscle metaboreflexes and blood flow redistribution during dynamic whole-body exercise remains unresolved.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Respiratory Muscle
- Exercise Performance
- Muscle Sympathetic Nerve Activity
- Inspiratory Muscle
- Heavy Exercise
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
This chapter describes the mechanical and metabolic costs of meeting the ventilatory requirements of exercise in healthy humans. We also deal with whether the respiratory muscles fatigue during exercise, what factors contribute to any such respiratory muscle fatigue, what the implications of these factors are for blood flow distribution and endurance exercise performance, and whether it is possible to overcome these potential respiratory limitations.
2 What Are the Ventilatory Costs of Exercise?
During whole-body exercise the respiratory control system functions to increase alveolar ventilation to a level sufficient to regulate arterial blood-gas tensions and acid–base balance at or near resting levels while minimizing the mechanical work performed by the respiratory muscles. These ventilatory demands are met by increases in tidal volume and airflow, requiring increases in negative intrapleural pressure. The peak dynamic pressure generated by the inspiratory muscles expressed relative to the subjects’ ability to generate pressure at the lung volumes and flow rates adopted during maximal exercise is only 40–60 % in moderately fit individuals [1]. In contrast, endurance-trained subjects elevate peak dynamic inspiratory muscle pressure to 90 % of capacity or greater [1].
The O2 consumption of the respiratory muscles \( (\dot{V}{\mathrm{rmO}}_2) \) during exercise increases progressively relative to minute ventilation (\( {\dot{V}}_E \)). However, the relationship is concave upward, i.e., a greater increment in \( \dot{V}{\mathrm{rmO}}_2 \) is required to establish a given increase in \( {\dot{V}}_E \) as work rate increases [2]. The \( \dot{V}{\mathrm{rmO}}_2 \) during near-maximal exercise requires approximately 10 % of \( \dot{V}{\mathrm{O}}_{2 \max } \) for moderately fit subjects, whereas in highly fit subjects at higher peak work rates and \( {\dot{V}}_E \), the \( \dot{V}{\mathrm{rmO}}_2 \) approaches 15 % of \( \dot{V}{\mathrm{O}}_{2 \max } \) [3]. Respiratory muscle perfusion naturally plays an important role in determining \( \dot{V}{\mathrm{rmO}}_2. \) By measuring the reduction in cardiac output achieved via mechanical ventilation, Harms et al. [4] estimated that the respiratory muscle work under normal physiological conditions at maximal exercise in fit subjects requires approximately 16 % of the cardiac output to be directed to the respiratory muscles to support their metabolic requirements (Fig. 2.1). These indirect estimates in humans are in agreement with microsphere studies in the exercising pony, which show large increases in blood flow to both inspiratory and expiratory muscles amounting to approximately 16 % of total cardiac output during maximal exercise [5].
Distribution of cardiac output at \( \dot{V}{\mathrm{O}}_{2 \max } \). Left panel: distribution of total cardiac output among legs, respiratory muscles, and other metabolically active tissues (skin, heart, brain, kidneys, and liver) at \( \dot{V}{\mathrm{O}}_{2 \max } \). Respiratory muscle blood flow at \( \dot{V}{\mathrm{O}}_{2 \max } \) was assumed to be equal to the fall in cardiac output obtained with respiratory muscle unloading at \( \dot{V}{\mathrm{O}}_{2 \max } \) and extrapolated to zero work of breathing. Right panel: total cardiac output and leg blood flow were measured under control conditions (normal work of breathing), with respiratory muscle unloading (low work of breathing) and with respiratory muscle loading (high work of breathing). Total blood flow was significantly lower with unloading and unchanged with loading, whereas leg blood flow and vascular conductance were significantly increased with unloading and decreased with loading (Data from Harms et al. [4, 26])
Nevertheless, the quantitation of respiratory muscle blood flow during exercise in the human remains controversial. Recent estimates of “trunk and head” blood flow based on the difference between cardiac output and flow to the arms plus legs (measured with dye dilution via catheterization of the subclavian and femoral veins) suggest that the lumped structure of the head, neck, heart, abdomen viscera, kidney, respiratory muscles, and gluteal muscles receives about 20 % of the cardiac output and 15 % of the \( \dot{V}{\mathrm{O}}_2 \) during maximal upright cycling exercise [6]. These data would attribute a substantially less than 15 % share of the cardiac output to the respiratory muscles. One problem not yet addressed in any study is the identification of all muscles – in the chest wall, abdomen, upper back, and shoulders – which are actually engaged (both dynamically and as fixators) in producing the hyperpnea accompanying heavy exercise.
3 Do the Respiratory Muscles Fatigue with Exercise?
Muscle fatigue has been defined as “a condition in which there is a loss in the capacity for developing force and/or velocity of a muscle, resulting from muscle activity under load and which is reversible by rest” [7]. Respiratory muscle fatigue thus defined and its significance to whole-body exercise performance were poorly documented and had generated little interest before the late 1970s. The seminal paper of Roussos and Macklem [8], however, illustrated that the diaphragm under resistive load exhibits task failure in a fashion similar to that expected of any other skeletal muscle.
More recently, nerve stimulation techniques have been used to provide objective evidence of exercise-induced respiratory muscle fatigue. In subjects with a wide range of fitness performing sustained exercise for more than 8–10 min at intensities greater than 80–85 % of \( \dot{V}{\mathrm{O}}_{2 \max }, \), reductions of 15–30 % in the transdiaphragmatic pressure response to supramaximal stimulation of the phrenic nerves were consistently obtained across a wide range of lung volumes and stimulation frequencies (1–100 Hz), and persisted for 1–2 h after exercise [9, 10]. These findings of diaphragmatic fatigue obtained at end-exercise have been confirmed using phrenic nerve stimulation “during” exercise, showing that significant fatigue occurs early during sustained, heavy exercise [11]. Like the diaphragm, the abdominal muscles are also susceptible to peripheral fatigue after sustained, heavy exercise (>90 % \( {\dot{\mathrm{V}}\mathrm{O}}_{2 \max } \), as demonstrated by 15–25 % reductions in the gastric pressure response to stimulation of the thoracic nerves [12].
4 What Are the Factors Contributing to Respiratory Muscle Fatigue?
There appear to be two general causes of exercise-induced diaphragmatic fatigue, namely, one cause attributable to the force production by the diaphragm itself and a second due to the effects of whole-body exercise, per se. Babcock et al. [13] examined the role that diaphragmatic pressure generation played in the fatigue process independent of the whole-body “exercise effect.” Subjects who demonstrated exercise-induced diaphragmatic fatigue were required to mimic at rest the essential mechanical components of breathing during exercise as well as the diaphragmatic pressure production for an identical time period as produced during exercise at 95 % of \( \dot{V}{\mathrm{O}}_{2 \max }. \) This mimicking protocol caused a less than 10 % decline in evoked diaphragmatic pressure. Furthermore, sustained force outputs of the diaphragm that were 1.5–2 times those normally experienced during exhaustive exercise were required to cause diaphragmatic fatigue when the subject was in the resting state and increased ventilation voluntarily. These data show that the influence of whole-body exercise on diaphragmatic fatigue is substantial. We believe that this whole-body exercise effect is likely due to less blood flow availability to the diaphragm during exercise (vs. hyperpnea during the resting state) in the face of high blood flow demands by the locomotor muscles.
A second study showed that greatly reducing the force output of the diaphragm during exhaustive prolonged exercise prevented exercise-induced diaphragmatic fatigue [14]. Thus, while the force output of the diaphragm experienced during exercise was insufficient to cause fatigue in the absence of locomotor muscle force output, it was critical to the development of diaphragmatic fatigue in the presence of whole-body exercise. These findings were consistent with the additional observation that the effect of exhaustive high-intensity whole-body exercise, per se, did not elicit fatigue in non-exercising muscles of the hand [13].
Based on the evidence summarized above, we postulate that the development of diaphragmatic fatigue during exercise is a function of the relationship between the magnitude of diaphragmatic work and the adequacy of its blood supply: the less blood flow is available, the less diaphragmatic work is required to produce fatigue. In healthy subjects of varying fitness levels [15], an imbalance of muscle force output versus blood flow and/or O2 transport availability to the diaphragm which favors fatigue appears to occur during exhaustive endurance exercise only when either the relative intensity of the exercise exceeds 85 % of \( \dot{V}{\mathrm{O}}_{2 \max } \) [9] or arterial hypoxemia is present [16].
5 What Are the Consequences of Respiratory Muscle Fatigue?
5.1 Effects on Exercise Performance
Experiments that have deliberately fatigued the respiratory muscles prior to exercise using either voluntary hyperpnea [17, 18] or resistive loading [19, 20] have noted a decrease [17, 18, 20] or no change [19] in time-to-exhaustion during subsequent short-term, heavy exercise; the influence of fatigue upon more prolonged exercise remains untested. On balance, these findings suggest that there is potential for respiratory muscle fatigue to impair short-duration, high-intensity exercise performance. A potential limitation of pre-fatigue studies, however, is that the number and type of motor units recruited during loaded breathing may be substantially different than during subsequent exercise. There may also be an effect of prior fatigue on the breathing pattern during subsequent exercise, such that any changes in exercise performance could be due to changes in exertional dyspnea. Furthermore, it is difficult to determine the contribution of subject expectation because it is impossible to placebo the pre-fatigue condition.
Several studies have noted increases in exercise capacity with partial unloading of the respiratory muscles using either low-density gas mixtures [21] or proportional assist mechanical ventilation [22]. For example, mechanical unloading of the respiratory muscles by over 50 % of their total inspiratory and expiratory work during heavy exercise (>90 % of \( \dot{V}{\mathrm{O}}_{2 \max }) \) prevented diaphragmatic fatigue [14] and resulted in a statistically significant 14 % increase in exercise time-to-exhaustion in trained male cyclists, with reductions in oxygen uptake and the rate of rise in perceptions of respiratory and limb discomfort [22] (Fig. 2.2). Other studies have not found a significant effect of respiratory muscle unloading on exercise capacity in less fit subjects [23–25], although these studies were conducted at lower relative exercise intensities, and the respiratory muscle unloading did not affect oxygen uptake. Collectively, these findings suggest that the work of breathing normally encountered during heavy sustained exercise has a significant influence on exercise performance.
Effects of respiratory muscle unloading via mechanical ventilation upon endurance exercise capacity at a workload requiring ~90 % of \( \dot{V}{\mathrm{O}}_{2 \max } \) in trained male cyclists (n = 7). Group mean data are shown for minutes 1–5 of exercise and at exhaustion. Absolute time-to-exhaustion under control conditions averaged 9.1 ± 2.6 min. Unloading normal work of breathing by 50 % from control increased time-to-exhaustion in 76 % of trials by a mean ± SD of 1.3 ± 0.4 min (14 ± 5 %). Respiratory muscle unloading caused reductions in oxygen uptake and the rate of rise in perceptions of limb and respiratory discomfort throughout the duration of exercise. * Significantly different from control, p < 0.05 (Data from Harms et al. [22])
5.2 Cardiorespiratory Interactions
5.2.1 Respiratory Muscle Metaboreflex
Perhaps the most likely aspect of respiratory muscle work limiting exercise performance is a reflex effect from fatiguing respiratory muscles which increases sympathetic vasoconstrictor outflow and compromises perfusion of limb muscle during prolonged exercise, thereby limiting its ability to perform work. Harms et al. [26] used a proportional assist ventilator to decrease the work of breathing in endurance-trained cyclists exercising at greater than 80 % of \( \dot{V}{\mathrm{O}}_{2 \max }. \) An increase in limb blood flow was observed commensurate with a 50–60 % decrease in the work of breathing. Conversely, when the work of breathing was increased by a comparable amount, limb blood flow and vascular conductance fell (Fig. 2.1). It seems likely that the local reductions in vascular conductance were sympathetically mediated because these changes correlated inversely with changes in norepinephrine spillover across the limb. When the study was repeated at an exercise intensity of only 50–75 % of \( \dot{V}{\mathrm{O}}_{2 \max }, \), changes in limb blood flow, vascular conductance, and norepinephrine spillover did not occur, even though changes in respiratory muscle work were still sufficient to alter oxygen uptake and cardiac output [27].
What caused these sympathetically mediated changes in limb vascular conductance when respiratory muscle work was altered during maximal exercise? We postulate that reflex mechanisms of sympathoexcitation are triggered by metaboreceptors in the diaphragm and expiratory muscles that begin to accumulate metabolic end products during heavy exercise when cardiac output is insufficient to adequately meet the high metabolic requirements of both respiratory and limb musculature. Evidence in support of this postulate is fourfold. First, diaphragmatic fatigue caused a time-dependent increase in multiunit activity in small diameter phrenic afferents in anesthetized cats [28, 29] and in single-unit activity in group IV afferents in anesthetized rats [30]. Second, electrical or pharmacological stimulation of thin-fiber phrenic afferents in anesthetized animals using capsaicin, bradykinin or lactic acid injections, or diaphragm muscle ischemia elicited increases in efferent sympathetic nerve activity and/or vascular resistance in several vascular beds, including the limb musculature and renal and coronary vasculature [31–33]. Third, in the resting or mildly exercising canine, infusing lactic acid into the phrenic artery and diaphragm caused vasoconstriction and reduced blood flow in the contracting limb muscle, and this vasoconstrictive effect was prevented via adrenergic blockade [34]. Finally, in a series of studies in humans, high-intensity contractions of the diaphragm [35] or expiratory muscles [36] against airway resistance to the point of task failure and/or fatigue caused a time-dependent increase in muscle sympathetic nerve activity (MSNA) in the resting leg, despite a corresponding increase in systemic blood pressure. This time-dependent increase in MSNA was accompanied by a significant decrease in limb vascular conductance and limb blood flow along with an increase in mean arterial pressure and heart rate [37] (Fig. 2.3). A similar time-dependent increase in ulnar nerve MSNA elicited via voluntary increases in inspiratory muscle work has recently been shown during cycling exercise [38].
Upper panel (a): effects of fatiguing the diaphragm on muscle sympathetic nerve activity (MSNA) in the resting leg in one representative subject during eupnea and diaphragmatic breathing at 60 % of maximum inspiratory mouth pressure (MIP) with a TITTOT = 0.7 and f b = 15 breaths/min. Note that the frequency and amplitude of MSNA were unchanged at the onset of increased diaphragmatic force output but increased thereafter in a time-dependent manner. Lower panel (b): beat-by-beat velocity of femoral artery blood flow (VTI velocity time integral) in the resting leg in one representative subject during eupnea and fatiguing diaphragmatic work at 60 % MIP with a TITTOT = 0.7 and f b = 15 breaths/min and during recovery. Femoral artery diameter was unchanged during the experiment; therefore, any changes in measured blood velocity reflected those in blood flow. Note that leg blood flow decreased and leg vascular resistance increased during fatiguing diaphragmatic work, despite an increase in MAP (Data from St. Croix et al. [35] and Sheel et al. [37])
To determine the precise mechanisms responsible for these time-dependent increases in MSNA and vascular responses, additional experiments were conducted to differentiate the potential effect of diaphragmatic fatigue from associated changes in lung volume, intrathoracic pressure, mechanical deformation of muscle, and central respiratory motor output, all of which accompanied the fatiguing voluntary respiratory efforts carried out to task failure. These potential excitatory effects on MSNA were ruled out by showing no effect of non-fatiguing voluntary increases in central respiratory motor output per se and a vasodilatory effect of increasing tidal volume by itself [35, 36]. Furthermore, the increase in MSNA was gradual and time dependent and was not evident at the initiation of the fatiguing trial despite marked increases in effort, diaphragmatic force production, and negativity of intrathoracic pressure. A more recent study using multiple trials of gradually increasing inspiratory effort showed that limb vasoconstriction only occurred when the rhythmic contractions of the diaphragm were of sufficient force and frequency to cause fatigue [39]. Thus, the apparent threshold for activation of MSNA from rhythmic respiratory muscle contractions was surpassed, not at a specific intensity of muscle force output, but only by respiratory muscle fatigue or at least a regimen of rhythmic muscular contractions that was likely sufficient to cause significant accumulation of muscle metabolites.
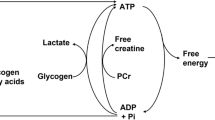
Collectively, the MSNA and blood flow data in humans and animals studied at rest and during exercise suggest that significant respiratory muscle metabolite accumulation will evoke a metaboreflex effect, which increases sympathetic vasoconstrictor outflow to limb locomotor muscle (Fig. 2.4), and perhaps explain the observed effects of changes in respiratory muscle work on limb vascular conductance, blood flow, and fatigue during maximal exercise [26, 40].
Schematic representation of the proposed respiratory muscle metaboreflex from the diaphragm and expiratory muscles activated by fatiguing contractions of these muscles and eliciting increased sympathetic discharge and limb vasoconstriction during heavy exercise with consequences of enhanced rate of development of limb fatigue and reduced exercise performance (see text) (From Dempsey et al. [63])
5.2.2 Intrathoracic Pressures and Cardiac Output
In exercising humans and dogs, reducing the negativity of inspiratory intrapleural pressure reduces right ventricular preload and stroke volume in health [4]. On the other hand, increasing expiratory threshold pressure reduces stroke volume – presumably because left ventricular afterload is increased – thereby reducing transventricular pressure differences which would slow the rate of ventricular filling during diastole [41, 42]. Further, increasing abdominal versus intrathoracic pressure with predominantly diaphragm versus ribcage inspirations, respectively, has marked cyclical effects on femoral venous return from the limbs at rest and even during mild-intensity leg exercise [43]. Understanding how the cardiovascular effects of isolated alterations in pressures during various phases of the respiratory cycle translate into the complex effects of breathing during whole-body exercise will be a formidable task – especially in the elite athlete ventilating in excess of 150 l/min who experiences expiratory flow limitation, positive expiratory pressures which often exceed the critical closing pressure of the airways, and hyperinflation with inspiratory pressures that are approaching the limits of the dynamic capacity of the inspiratory muscles [1]. Equally intriguing and clinically relevant is why reducing the magnitude of negative pressure on inspiration increases stroke volume and cardiac output in a dose-dependent manner in heart failure animals [44] and humans [45] during exercise – effects which are in the opposite direction to those in the healthy subject.
6 Can These Respiratory Limitations Be Overcome?
Evidence from studies that have specifically trained the respiratory muscles of healthy subjects using strength (resistive/threshold) or endurance (hyperpnea) training suggests it might be possible to overcome the aforementioned respiratory limitations on exercise. Early studies produced contradictory findings, primarily due to poor research designs and inappropriate outcome measures [46]. More recent evidence from adequately controlled studies suggests that there might be small but significant effects on exercise performance during constant load tests, time trials, and intermittent tests [47–50].
The mechanisms by which respiratory muscle training might improve exercise performance are not entirely clear. Increases in respiratory muscle strength, velocity of shortening, and endurance have been consistently observed with respiratory muscle training in healthy subjects [51]. The functional significance of such improvements in respiratory muscle function would presumably be to prevent or delay the respiratory muscle fatigue that is known to occur during heavy sustained exercise (see above). Changes in respiratory muscle fiber size, subtype ratio, and myofiber contractile properties induced by respiratory muscle training may reduce the force contribution from each active myofiber or the number of myofibers at a given submaximal level of ventilation. In conjunction, a stronger type I fiber may allow individuals to delay the recruitment of less efficient type II fibers. Fatigue-resistant respiratory muscles may cause reductions in the rate of carbohydrate breakdown, lactate accumulation, and intracellular pH in these muscles, contributing to an overall improvement in cellular homeostasis. Fewer metabolic stimuli in the respiratory muscles would be expected to attenuate reflex activity from type III/IV receptors of these muscles and thereby reduce sympathetic vasoconstrictor activity in the limbs. The concomitant increase in limb blood flow would increase oxygen delivery to the limbs and potentially reduce both limb muscle fatigue and peripheral effort sensations. There is evidence that respiratory muscle training reduces exercise-induced respiratory muscle fatigue [52], increases the oxidative and/or lactate transport capacity of the inspiratory muscles [53], alleviates calf muscle fatigue during plantar flexion exercise [54], and increases the threshold for activation of the respiratory muscle metaboreflex [55]. However, direct evidence for a benefit of respiratory muscle training on blood flow redistribution during dynamic whole-body exercise is not yet available. In addition to the potential effects of respiratory muscle training on exercise-induced respiratory muscle fatigue and its associated vasoconstrictive effects on the locomotor muscle vasculature, there might also be perceptual benefits. Attenuation of sensory input to the central nervous system may be expected to occur in line with a decrease in inhibitory feedback from fatiguing respiratory muscles, an alteration in breathing pattern (e.g., reduce operating lung volumes), a delay in the recruitment of accessory respiratory muscles, an alteration in the motor recruitment within a given respiratory muscle, or a reduction in the fraction of maximum tension generated with each breath [56, 57].
To what extent should exercise performance be affected by respiratory muscle training? Several studies have noted increases in time-to-exhaustion with partial unloading of the respiratory muscles of healthy subjects [21, 22]. For example, mechanical unloading of the respiratory muscles by over 50 % of their total inspiratory and expiratory work during heavy exercise prevented diaphragmatic fatigue [14] and resulted in at most a 14 % improvement in endurance capacity in trained cyclists (Fig. 2.2) with no change in circulating lactate, a reduction in oxygen uptake and cardiac output, a decrease in the rate of rise of both respiratory and limb discomfort, and variable effects on ventilation [22]. Although some respiratory muscle training studies have reported huge improvements (25–50 %) in exercise capacity [47, 48], it seems inconceivable that the effects could surpass those seen with substantial mechanical unloading – unless respiratory muscle training imparts some additional influences on locomotor muscles that are not realized via substantial respiratory muscle unloading and the prevention of diaphragmatic fatigue. A potential reason why previous studies have found greater improvements in exercise capacity with respiratory muscle training may be due to a large intraindividual variance in exercise performance coupled with a failure to use carefully matched and designed placebo groups.
If respiratory muscle training were to attenuate exercise-induced respiratory muscle fatigue, it is likely that the benefit would only occur in near-maximal exercise conditions. Increases in time-to-exhaustion with respiratory muscle unloading have been noted in healthy, fit subjects only at exercise intensities greater than 85 % of \( \dot{V}{\mathrm{O}}_{2 \max } \) [21, 22]. Interestingly, exercise-induced diaphragmatic fatigue also only occurred consistently at exercise intensities greater than 85 % of \( \dot{V}{\mathrm{O}}_{2 \max } \) [9], and the effects of respiratory muscle unloading on limb vascular resistance during exercise only occurred when the intensity exceeded 80 % of maximum [26, 27]. On the other hand, there are several examples where respiratory muscle work exerts significant cardiovascular effects, even during submaximal exercise. In patients with congestive heart failure [58] or those with chronic obstructive pulmonary disease [59], sustained exercise at only 50–60 % of maximum caused fatigue of limb locomotor muscles [60]. In rodent models of heart failure (vs. healthy controls), microsphere distribution studies showed a reduced limb blood flow and enhanced diaphragm blood flow during exercise [61]. In human chronic heart failure patients, respiratory muscle unloading [45] was shown to increase limb vascular conductance and limb blood flow and enhance exercise performance. These effects reflect the combination of increased respiratory muscle work with limited cardiac output in chronic heart failure. Finally, even the healthy person exercising submaximally in hypoxic environments undergoes hyperventilation and increased work of breathing; under these conditions, unloading the respiratory muscles significantly reduces the rate of development of limb fatigue and improves endurance performance [62].
References
Johnson BD, Saupe KW, Dempsey JA (1992) Mechanical constraints on exercise hyperpnea in endurance athletes. J Appl Physiol 73:874–886
Otis AB (1954) The work of breathing. Physiol Rev 34:449–458
Aaron EA, Seow KC, Johnson BD et al (1992) Oxygen cost of exercise hyperpnea: implications for performance. J Appl Physiol 72:1818–1825
Harms CA, Wetter TJ, McClaran SR et al (1998) Effects of respiratory muscle work on cardiac output and its distribution during maximal exercise. J Appl Physiol 85:609–618
Manohar M (1986) Blood flow to the respiratory and limb muscles and to abdominal organs during maximal exertion in ponies. J Physiol 377:25–35
Calbet JA, Gonzalez-Alonso J, Helge JW et al (2007) Cardiac output and leg and arm blood flow during incremental exercise to exhaustion on the cycle ergometer. J Appl Physiol 103:969–978
NHLBI Workshop summary. Respiratory muscle fatigue. Report of the Respiratory Muscle Fatigue Workshop Group (1990) Am Rev Respir Dis 142:474–480
Roussos CS, Macklem PT (1977) Diaphragmatic fatigue in man. J Appl Physiol 43:189–197
Johnson BJ, Babcock MA, Suman OE et al (1993) Exercise-induced diaphragmatic fatigue in healthy humans. J Physiol 460:385–405
Romer LM, Polkey MI (2008) Exercise-induced respiratory muscle fatigue: implications for performance. J Appl Physiol 104:879–888
Walker DJ, Walterspacher S, Schlager D et al (2011) Characteristics of diaphragmatic fatigue during exhaustive exercise until task failure. Respir Physiol Neurobiol 176:14–20
Taylor BJ, How SC, Romer LM (2006) Exercise-induced abdominal muscle fatigue in healthy humans. J Appl Physiol 100:1554–1562
Babcock MA, Pegelow DF, McClaran SR et al (1995) Contribution of diaphragmatic power output to exercise-induced diaphragm fatigue. J Appl Physiol 78:1710–1719
Babcock MA, Pegelow DF, Harms CA et al (2002) Effects of respiratory muscle unloading on exercise-induced diaphragm fatigue. J Appl Physiol 93:201–206
Babcock MA, Pegelow DF, Johnson BD et al (1996) Aerobic fitness effects on exercise-induced low-frequency diaphragm fatigue. J Appl Physiol 81:2156–2164
Babcock MA, Johnson BD, Pegelow DF et al (1995) Hypoxic effects on exercise-induced diaphragmatic fatigue in normal healthy humans. J Appl Physiol 78:82–92
Dodd SL, Powers SK, Thompson D et al (1989) Exercise performance following intense, short-term ventilatory work. Int J Sports Med 10:48–52
Martin B, Heintzelman M, Chen HI (1982) Exercise performance after ventilatory work. J Appl Physiol 52:1581–1585
Mador MJ, Acevedo FA (1991) Effect of respiratory muscle fatigue on subsequent exercise performance. J Appl Physiol 70:2059–2065
Taylor BJ, Romer LM (2008) Effect of expiratory muscle fatigue on exercise tolerance and locomotor muscle fatigue in healthy humans. J Appl Physiol 104:1442–1451
Wilson GD, Welch HG (1980) Effects of varying concentrations of N2/O2 and He/O2 on exercise tolerance in man. Med Sci Sports Exerc 12:380–384
Harms CA, Wetter TJ, St Croix CM et al (2000) Effects of respiratory muscle work on exercise performance. J Appl Physiol 89:131–138
Gallagher CG, Younes M (1989) Effect of pressure assist on ventilation and respiratory mechanics in heavy exercise. J Appl Physiol 66:1824–1837
Krishnan B, Zintel T, McParland C et al (1996) Lack of importance of respiratory muscle load in ventilatory regulation during heavy exercise in humans. J Physiol 490(Pt 2):537–550
Marciniuk D, McKim D, Sanii R et al (1994) Role of central respiratory muscle fatigue in endurance exercise in normal subjects. J Appl Physiol 76:236–241
Harms CA, Babcock MA, McClaran SR et al (1997) Respiratory muscle work compromises leg blood flow during maximal exercise. J Appl Physiol 82:1573–1583
Wetter TJ, Harms CA, Nelson WB et al (1999) Influence of respiratory muscle work on VO2 and leg blood flow during submaximal exercise. J Appl Physiol 87:643–651
Balzamo E, Lagier-Tessonnier F, Jammes Y (1992) Fatigue-induced changes in diaphragmatic afferents and cortical activity in the cat. Respir Physiol 90:213–226
Jammes Y, Balzamo E (1992) Changes in afferent and efferent phrenic activities with electrically induced diaphragmatic fatigue. J Appl Physiol 73:894–902
Hill JM (2000) Discharge of group IV phrenic afferent fibers increases during diaphragmatic fatigue. Brain Res 856:240–244
Hussain SN, Chatillon A, Comtois A et al (1991) Chemical activation of thin-fiber phrenic afferents. 2. Cardiovascular responses. J Appl Physiol 70:77–86
Offner B, Dembowsky K, Czachurski J (1992) Characteristics of sympathetic reflexes evoked by electrical stimulation of phrenic nerve afferents. J Auton Nerv Syst 41:103–111
Szulczyk A, Szulczyk P, Zywuszko B (1988) Analysis of reflex activity in cardiac sympathetic nerve induced by myelinated phrenic nerve afferents. Brain Res 447:109–115
Rodman JR, Henderson KS, Smith CA et al (2003) Cardiovascular effects of the respiratory muscle metaboreflexes in dogs: rest and exercise. J Appl Physiol 95:1159–1169
St Croix CM, Morgan BJ, Wetter TJ et al (2000) Fatiguing inspiratory muscle work causes reflex sympathetic activation in humans. J Physiol 529(Pt 2):493–504
Derchak PA, Sheel AW, Morgan BJ et al (2002) Effects of expiratory muscle work on muscle sympathetic nerve activity. J Appl Physiol 92:1539–1552
Sheel AW, Derchak PA, Morgan BJ et al (2001) Fatiguing inspiratory muscle work causes reflex reduction in resting leg blood flow in humans. J Physiol 537(Pt 1):277–289
Katayama K, Iwamoto E, Ishida K et al (2012) Inspiratory muscle fatigue increases sympathetic vasomotor outflow and blood pressure during submaximal exercise. Am J Physiol Regul Integr Comp Physiol 302:R1167–R1175
Sheel AW, Derchak PA, Pegelow DF et al (2002) Threshold effects of respiratory muscle work on limb vascular resistance. Am J Physiol Heart Circ Physiol 282:H1732–H1738
Romer LM, Lovering AT, Haverkamp HC et al (2006) Effect of inspiratory muscle work on peripheral fatigue of locomotor muscles in healthy humans. J Physiol 571(Pt 2):425–439
Miller JD, Hemauer SJ, Smith CA et al (2006) Expiratory threshold loading impairs cardiovascular function in health and chronic heart failure during submaximal exercise. J Appl Physiol 101:213–227
Stark-Leyva KN, Beck KC, Johnson BD (2004) Influence of expiratory loading and hyperinflation on cardiac output during exercise. J Appl Physiol 96:1920–1927
Miller JD, Pegelow DF, Jacques AJ et al (2005) Skeletal muscle pump versus respiratory muscle pump: modulation of venous return from the locomotor limb in humans. J Physiol 563(Pt 3):925–943
Miller JD, Smith CA, Hemauer SJ et al (2007) The effects of inspiratory intrathoracic pressure production on the cardiovascular response to submaximal exercise in health and chronic heart failure. Am J Physiol Heart Circ Physiol 292:H580–H592
Olson TP, Joyner MJ, Dietz NM et al (2010) Effects of respiratory muscle work on blood flow distribution during exercise in heart failure. J Physiol 588:2487–2501
McConnell AK, Romer LM (2004) Respiratory muscle training in healthy humans: resolving the controversy. Int J Sports Med 25:284–293
HajGhanbari B, Yamabayashi C, Buna T et al (2012) Effects of respiratory muscle training on performance in athletes: a systematic review with meta-analyses. J Strength Cond Res. doi:10.1519/JSC.0b013e318269f73f
Illi SK, Held U, Frank I et al (2012) Effect of respiratory muscle training on exercise performance in healthy individuals: a systematic review and meta-analysis. Sports Med 42(8):707–724
McConnell AK (2012) CrossTalk opposing view: respiratory muscle training does improve exercise tolerance. J Physiol 590:3397–3398
Patel MS, Hart N, Polkey MI (2012) CrossTalk proposal: training the respiratory muscles does not improve exercise tolerance. J Physiol 590:3393–3395
Leith DE, Bradley M (1976) Ventilatory muscle strength and endurance training. J Appl Physiol 41:508–516
Verges S, Lenherr O, Haner AC (2007) Increased fatigue resistance of respiratory muscles during exercise after respiratory muscle endurance training. Am J Physiol Regul Comp Physiol 292(3):R1246–R1253
Brown PI, Sharpe GR, Johnson MA (2012) Inspiratory muscle training abolishes the blood lactate increase associated with volitional hyperpnoea superimposed on exercise and accelerates lactate and oxygen uptake kinetics at the onset of exercise. Eur J Appl Physiol 112:2117–2129
McConnell AK, Lomax M (2006) The influence of inspiratory muscle work history and specific inspiratory muscle training upon human limb muscle fatigue. J Physiol 577(Pt 1):445–457
Witt JD, Guenette JA, Rupert JL et al (2007) Inspiratory muscle training attenuates the human respiratory muscle metaboreflex. J Physiol 584(Pt 3):1019–1028
McConnell AK, Romer LM (2004) Dyspnoea in health and obstructive pulmonary disease: the role of respiratory muscle function and training. Sports Med 34(2):117–132
Sheel AW, Foster GE, Romer LM (2004) Exercise and its impact on dyspnea. Curr Opin Pharmacol 11(3):195–203
O’Donnell DE, D’Arsigny C, Raj S et al (1999) Ventilatory assistance improves exercise endurance in stable congestive heart failure. Am J Respir Crit Care Med 160:1804–1811
Richardson RS, Sheldon J, Poole DC et al (1999) Evidence of skeletal muscle metabolic reserve during whole-body exercise in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 159:881–885
Amann M, Regan MS, Kobitary M et al (2010) Impact of pulmonary system limitations on locomotor muscle fatigue in patients with COPD. Am J Physiol Regul Integr Comp Physiol 299:R314–R324
Musch TI (1993) Elevated diaphragmatic blood flow during submaximal exercise in rats with chronic heart failure. Am J Physiol 265:H1721–H1726
Amann M, Pegelow DF, Jacques AJ et al (2007) Inspiratory muscle work in acute hypoxia influences locomotor muscle fatigue and exercise performance of healthy humans. Am J Physiol Regul Integr Comp Physiol 293:R2036–R2045
Dempsey JA, Romer L, Rodman J et al (2006) Consequences of exercise-induced respiratory muscle work. Respir Physiol Neurobiol 151:242–250
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Italia
About this chapter
Cite this chapter
Romer, L.M., Dempsey, J.A. (2014). Work of Breathing During Exercise: Implications for Performance. In: Aliverti, A., Pedotti, A. (eds) Mechanics of Breathing. Springer, Milano. https://doi.org/10.1007/978-88-470-5647-3_2
Download citation
DOI: https://doi.org/10.1007/978-88-470-5647-3_2
Published:
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-5646-6
Online ISBN: 978-88-470-5647-3
eBook Packages: MedicineMedicine (R0)