Abstract
The population in Asia has been rising since 2000 and is estimated to reach 932 million in 2050, making Asia the most populous elderly region in the world. The prevalence of hypertension is high even in Asia and it rises with age. In tandem with the aging population, Asia will have the largest population with hypertension in the world by the middle of this century.
While several of the mechanisms and pathophysiology responsible for the causation of hypertension are similar to younger adults, many differences also occur. The elderly have more arterial stiffness leading to a greater elevation of systolic blood pressure (BP) than the diastolic BP, resulting in a higher prevalence of isolated systolic hypertension which is more difficult to treat. The elderly is also more salt-sensitive and herein opportunities and evidence exist that lowering salt intake can lower BP. Evidence has also emerged that the white coat effect and masked hypertension are more common in the elderly and should be identified as they are associated with increased cardiovascular (CV) risk.
Hypertension in the elderly needs to be treated as reducing BP reduces CV mortality and morbidity. However, because the elderly is a more vulnerable group, usually having many other co-morbid conditions, including functional and cognitive impairments. Treatment may increase the occurrence of postural hypotension potentially leading to falls; thus, any treatment for the elderly has to be individualized. Target BP control for the elderly has to balance the benefits and adverse effects of anti-hypertensive therapy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hypertension
- Aging
- Elderly
- Arterial stiffness
- Salt sensitivity
- Isolated systolic hypertension
- Postural hypotension
17.1 The Aging Population in Asia
The definitions of elderly vary somewhat in Asia where some countries use age ≥ 60 to define “elderly” while others adopt age ≥ 65 years as a cut-off point to define the elderly group. Notwithstanding these arbitrary age definitions of elderly, the number of people age ≥ 60 is increasing rapidly. It is estimated that between 2015 and 2050, the proportion of the world’s population over 60 years will nearly double from 12 to 22% [1]. In Asia, with falling fertility rates and increased life expectancy, the population age 65 and older has been rising since 2000 (Fig. 17.1). The proportion of the population age ≥ 65 years in Asia was 4.8% in 2019 and is predicted to rise to 17.8% in 2050, with an increase in absolute numbers from 400 million to 900 million [2]. Due to this rapid rise, several countries in Asia will have between 15% to as high as 34% of the total their population being elderly (Figs. 17.2 and 17.3). In India and China with the largest populations in the world, the proportion of the population aged ≥65 years in India was 3.8% in 1990 and is predicted to rise to 13.7% in 2050. In China, the proportion of the population aged ≥65 years was 5.6% in 1990 and is predicted to rise to 26% in 2050 [2]. Japan is a country with the longest life expectancy in the world, the proportion of the Japanese population aged ≥65 years was 11.8% in 1990 and was predicted to rise to 37.7% in 2050. Japan may represent the possible future age structure in many Asian countries. As a result of this rapid rise in the aging population, Asia is on track in the next few decades to become one of the oldest in the world [3] by the middle of this century.
Population aged 65 and older in Asia 1950–2050. (Source: Asia Development Bank. https://data.adb.org/dataset/population-and-aging-asia-and-pacific (accessed 9 Aug 2021))
The proportion of population aged 60 or over in 2015 and 2050. (Source: Global Age Watch https://www.helpage.org/global-agewatch/about/about-global-agewatch/(accessed 9 Aug 2021). Map: https://www.helpage.org/global-agewatch/population-ageing-data/population-ageing-map/ (accessed 9 August 2021))
Prevalence of hypertension by age group in Malaysia 2019. (Source: National health and Morbidity Survey 2019 Volume ll Report on Non-communicable Diseases http://iku.moh.gov.my/images/IKU/Document/REPORT/NHMS2019/Report_NHMS2019-NCD_v2.pdf)
17.2 Prevalence of Hypertension in Asia
Globally, the prevalence of hypertension is high where in 2015, 1 in 4 men and 1 in 5 women had hypertension resulting in an estimated 1.13 billion people worldwide suffering from hypertension. Most of these people live in Asia which is the world’s most populous continent and most (two-thirds) living in low- and middle-income countries [4].
While it is recognized that high-income countries like the United States of America (USA) has a high prevalence of 47.1% of adults age 20 and older in 2017–2018 having hypertension [5], this also occurs in high-income countries in Asia where 60% and 32.9% of adult men in Japan and Korea, respectively, are hypertensive [6]. Furthermore it is equally high in many low- and middle-income economies in Asia where prevalence of hypertension is 42.3% in adults age 30 years or older in Malaysia and 50.3% in Pakistan [6,7,8,9] and notably, hypertension is more prevalent in people of East and South Asian ancestry [10, 11].
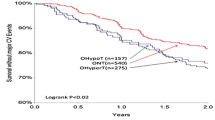
The prevalence of hypertension increases with age. In the USA, among those aged 60 years and older, the prevalence is 74.5% compared to lower prevalence of 54.5% among the 40–59 age group [5]. This higher prevalence in older adults is also observed in the low- and middle-income countries in Asia where in countries like Malaysia, the prevalence of hypertension in older adults is much higher than in younger adults, reaching a prevalence of 75.4% in those age between 74 and 75 years [7] (Fig. 17.3). Many governments in Asia are generally poorly prepared for this change. There will be implications not only on the health care system but also social and economic consequences [12].
17.3 Pathophysiology of Hypertension in the Elderly
Multiple systems like the cardiac, renal, sympathetic nervous system, and other CV control mechanisms interact and can affect cardiac and vascular homeostasis resulting in changes in blood pressure (BP).
17.3.1 The Renin-Angiotensin-Aldosterone System in the Elderly
The kidneys are an important regulator role of blood pressure [13, 14]. Parenchymal damage to the kidneys or any impairment of renal function almost invariably leads to the development of hypertension [15]. The kidneys control blood pressure via natriuresis and the renin-angiotensin-aldosterone system (RAAS) [13, 14, 16]. BP and salt excretion is regulated by the RAAS system. The RAAS system is activated by a low salt intake stimulating renal sodium reabsorption and preserving intravascular volume to maintain BP. Conversely, a high salt intake dampens the RAAS, facilitating natriuresis, excreting more sodium to reduce intravascular volume and BP. Many therapeutic agents targeting the RAAS had been developed over the past few decades, starting with captopril, the first angiotensin converting enzyme (ACE) inhibitor in 1981, followed by losartan, the first AT-ll angiotensin receptor blocker (ARB) in 1990 and the direct renin inhibitor, aliskiren in 2005 [17, 18]. Spironolactone has been available since the 1970s and used as a potassium-sparing diuretic initially but is now used in resistant hypertension as demonstrated in recent clinical trials [19,20,21], particularly in hyperaldosteronism.
In the elderly, plasma renin activity declines with age and this has been attributed to the effect of age-associated nephrosclerosis [22, 23]. A study reported a reduced plasma renin activity in older adults age 65 years and older compared to younger individuals who were matched for mean arterial pressure, race, sex, height, and weight [24]. Nevertheless, a randomized control study comparing the efficacy of BP lowering of aliskiren to ramipril in the elderly found aliskiren lowered systolic and diastolic BP by 14 and 5.1 mmHg respectively, relative to baseline BP, while ramipril lowered systolic and diastolic BP by 11.76 and 3.6 mmHg respectively [25], indicating that aliskiren is able to lower BP in the elderly despite renin activity being reduced. However, to date no specific clinical outcome trials have been done on the efficacy and role of direct renin inhibitors in reducing cardiovascular mortality and morbidity in the hypertensive elderly.
Similarly, although plasma renin activity is decreased in the elderly, the fall in BP after ACE inhibitors is at least as great as in the younger age groups. One reason is due in part to a sustained ACE-inhibitor concentration as a consequence of slower clearance of the drug due to the poorer kidney function that is associated with aging.
Aging is also associated with a decline in renal function which may be amplified by intrinsic renal disease; for example, that caused by diabetes or other renovascular abnormalities. Hence, changes in tubular reabsorption of sodium will affect the ability and capacity of the kidney to adjust to fluctuations in normal sodium intake [26]. It has also been shown that compared to younger normal healthy individuals and normal older healthy individuals, the half-life for renal sodium excretion was prolonged. The elderly is less able to handle a high sodium load well, rendering them more salt-sensitive [27]. Herein suggests the role of diuretics for the treatment of hypertension in the elderly and is reflected in most guidelines for the management of hypertension.
17.3.2 Vascular Mechanism in the Elderly
Total peripheral resistance is one of the components determining BP. Structural and functional damage to the micro- or macrocirculation results in increased arterial stiffening [28] and total peripheral resistance causing a rise in BP. Microcirculatory damage could be a cause or a result of hypertension. Peripheral vascular resistance is controlled mainly at the arterioles and small arteries. Vascular tone is regulated by various factors including the sympathetic nervous system, humoral factors (the RAAS and endothelium), and auto-regulation. Endothelial damage and the resulting inflammation caused by low-density lipoprotein (LDL)-cholesterol, or hyperglycemia, stimulates the production of factors like the reactive oxygen species (ROS) and endothelin, leading to reduced nitric oxide and changes in the vasculature, and eventually raising BP.
Aging is associated with remodeling of large arteries leading to structural changes such as increased collagen deposition and rupture of elastin fibers [29] leading to a loss of elasticity, hypertrophy and sclerosis of muscular arteries and arterioles, and increasing arterial stiffness [30]. The loss of this elasticity with aging promotes the early return of reflected waves from the peripheral arterial circulation. Early wave reflection amplifies the systolic pressure wave generated with each heartbeat, leading to an increase in systolic pressure and a fall in diastolic pressure. These changes are responsible for the physiological changes in BP with aging, which is seen as a decline in diastolic BP and a rise in systolic BP, often presenting as isolated systolic hypertension (ISH), seen almost always in the elderly only. Abundant data has already confirmed that ISH is associated with at least twice the hazards ratio of increased CV mortality and morbidity compared to older individuals without ISH [31, 32]. Randomized clinical outcome trials have also demonstrated that treating ISH reduces CV mortality and morbidity [33, 34].
White coat hypertension (WCH) is a situation where in an untreated individual the BP measured in the clinic is ≥140/90 mmHg, while the day BP using ambulatory BP measurements or home BP measurements is <135/85 mmHg. WCH is common and is reported to be more common in the elderly [35, 36]. Although the term WCH was originally defined for individuals not on hypertensive medications, it is now being used to describe discrepancies between office and out-of-office BP in patients already on treatment for hypertension, with the term white coat uncontrolled hypertension (WUCH) or as white coat effect (WCE) [37]. WCE is reserved more for patients already on anti-hypertensive drugs, where similar to the WCH situation, the office BP is high but home is low [36, 38, 39]. These two terms are frequently used interchangeably.
Studies have found a correlation between WCE and arterial stiffness [36, 40, 41] and WCH/WCE is not uncommon. In a study involving many countries in Asia, WCE was as high as 40% in one country [42]. WCH WCE is more common in the elderly and was as high as 50% in the very old [35, 37, 38]. This has clinical implications especially in the elderly, as not identifying WCH/WCE may mean unnecessary anti-hypertensive therapy in an elderly who is often already burdened by many other co-morbidities or up-titrating hypertensive drugs giving rise to hypotension and/or postural hypotension leading to falls.
Masked hypertension (MH) is the reverse of WCH/WCE and is also referred to as isolated uncontrolled home hypertension. In this category, the clinic/office BP is normal, that is, <140/80 mmHg but the out-of-office home BP is ≥135/85 mmHg. MH is associated with increased risk of CV events and has been shown to be more common in the elderly [43,44,45,46,47]. In the Japanese J-HOME study, among a group of treated older hypertensive adults with mean age of 66 years, 23% had uncontrolled home hypertension [48]. As almost one in four treated older hypertensives adults have MH, it is important to identify such patients and modify management to reduce their cardiovascular risk.
17.3.3 The Nervous System and Hypertension in the Elderly
Both short- and long-term control of BP are regulated by the sympathetic system. Studies have shown a significant decline in sympathetic and para-sympathetic response with aging [49, 50]. Postural hypotension occurs due to age-related impairment in baroreflex-mediated vasoconstriction, cardiac chronotropic responses, and deterioration of the diastolic filling of the heart [51, 52]. Postural hypotension increases with age where, in community dwelling individuals ≥65 years of age, its prevalence is approximately 20%; in those ≥75 years of age it is as high as 30% and in frail elderly individuals living in nursing homes, the prevalence is up to 50% [51, 53].
Patients with apparent and true resistant hypertension (RHT) often have increased sympathetic activity [54, 55]. Based on these findings, technology was developed to treat RHT by suppressing sympathetic activity with electrical stimulation of the carotid baroreflex and catheter-based renal denervation (RDN). Initial studies of renal nerve denervation (RDN) showed good decreases in BP with minimal adverse effects [56,57,58]. However, in sham-control trials, RDN was found to be not better at lowering BP compared with use of anti-hypertensive drugs alone [59]. One of the reasons for the failure of this study was that RDN was not standardized and many operators of RDN did not have any experience before the study.
17.3.4 Hypertension, Left Ventricular Hypertrophy, and Heart Failure in the Elderly
The prevalence of left ventricular hypertrophy (LVH) based on echocardiographic studies in hypertensive patients ranged from 36 to 41% [60]. In Asian hypertensive patients attending a primary care clinic with a mean age of 59.2 ± 7.7 years, 1 in 4 had echocardiography evidence of LVH [61]. The concentric LVH seen in hypertension makes the myocardium less compliant and results in diastolic dysfunction. This is more common in women, the elderly, and patents with diabetes [62, 63]. Also it is reported that isolated systolic hypertension, almost exclusively seen in the elderly, is associated more with concentric LVH [64, 65]. Hypertension with LVH and diastolic dysfunction when left untreated or not controlled well, leads to heart failure with preserved ejection fraction (HFpEF) [66].
Hypertensive heart failure (HF) is common in patients with hypertension in general and it is more common in the elderly than younger adults [67, 68]. The incidence of HF is strongly dependent on age, with an estimated incidence of 1% at age 65 that approximately doubles with each decade of age thereafter [69]. The prevalence of HF was about ten times higher in those aged ≥80 years (12.8% in men and 12% in women), compared to those aged 40–59 years (1.2% in men and 1.7% in women) [68]. Mortality and hospitalization rates due to HF is also higher in those aged ≥65 years than those aged <65 years [68, 69].
Several large HF registries showed that hypertension was the primary cause of HF in 11–23% of the patients [70, 71]. In an Asian HF registry, one-third of the patients with HF had hypertensive HF [72, 73]. A more recent study hypertensive HF accounted for 4% of HF, suggesting better control of hypertension [74]. The diagnosis and management of HF in the elderly is more challenging than for younger adults due to multi-comorbid diseases, polypharmacy, cognitive impairment, functional ability, and frailty. Studies have shown that 60% of elderly with HF usually have three or more other co-morbid conditions and 17% had cognitive impairment [75,76,77].
Many clinical trials on HF did not include patients over 75 years. HFpEF in the elderly remains without definitive treatment as most clinical trials were performed in HF patients with reduced ejection fraction (HFrEF). As hypertension is often the pre-disposing cause of HF in the elderly, control of hypertension is critical. Reduction in salt consumption is also important as the elderly are more salt-sensitive and even more so in elderly Asians with HF as Asians have been shown to not only have a higher salt intake but are also more salt-sensitive than their European counter-parts (see Sec. 17.4.3 on Salt Intake and Hypertension in the Elderly) (see Chap. 13 on HF for more details).
17.4 Atrial Fibrillation
The prevalence of atrial fibrillation (AF) increases with age, and is the most common arrhythmia in adults age 65 years and older [78]. The prevalence in individuals aged ≥75 years is 10% [79,80,81]. As high as 70% of individuals with AF were between 65 and 85 of age [78, 82]. AF often co-exists with hypertension and hypertension increases the risk of AF, with 60–80% of patients with AF also having hypertension [83, 84].
Although the epidemiological association between hypertension and AF is well established, the pathogenic mechanisms explaining the higher propensity of hypertensive patients to develop AF are still incompletely known. Experimental animal studies seem to suggest that it is due to a remodeling of the left atrium caused by hypertension. Although the entire mechanism is not well understood, it stands to reason that hypertension should be treated early and controlled well to prevent the progression to left atrium dilatation [84].
17.4.1 Genetic Factors and Hypertension in the Elderly
Hypertension develops because of an interaction between genetic and multiple environmental factors. Familial clustering of hypertension is well recognized and a family history of hypertension in an individual is a determinant of not only future hypertension but an earlier onset in the said individual. This implies that genetic factors are at play in the causation of hypertension.
Although gene analyses have identified many gene variants that predispose an individual to the development of hypertension, they are of modest effect. It has been estimated that the combination of different gene variants associated with the risk of hypertension contribute only around 3.5% of the trait variance [85]. Besides genetic predisposition to future risk of hypertension, there is the interaction between genes with epigenetics where environmental and life-style factors may influence the actual and potential onset of hypertension. This has been evaluated in a recent genome-wide association (GWAS) and replication study of BP phenotypes in 320,251 East and South Asian and European ancestry that suggested an interaction of genomic with epigenomic in the regulation of BP [86]. One of the suggested use of these GWAS studies is that it could generate a genetic risk score to predict future cardiovascular risk [87].
17.4.2 Environmental and Life-Style Factors and Hypertension in the Elderly
The prevalence of obesity is increasing rapidly worldwide [88]. Asia is not spared from this “epidemic” in spite of several countries being in the low-middle income group, with prevalence of obesity along with the metabolic syndrome, being just as high as in developed countries [89, 90]. Risk factors for CV disease like diabetes and even actual coronary heart disease occur at lower body mass index in Asians than in Europeans [11, 90, 91]. Obesity predisposes to an increased risk of diabetes mellitus and sleep apnea, which are both associated with higher prevalence of hypertension, and is independently associated with risk of CV and cerebrovascular events [92].
This increase in prevalence of obesity is also seen in the elderly, for example in the USA, to more than 30% in men and women aged 60 years and over [93, 94]. Similarly an Asian country also reports obesity rate of 30.2% in those aged 60 and above [95].
17.4.3 Salt Consumption and Hypertension in the Elderly
The daily average intake of salt globally is 9.8 g (equivalent to 3.95 g of sodium) [96]. This is much higher than the recommended daily intake of 5 g of salt by the World Health Organization (WHO) [97]. Asians consume more salt than populations in the USA and the United Kingdom [98] and studies have shown that higher salt consumption is associated with higher BP [99,100,101,102,103] and that different individuals have different salt sensitivity [100, 104,105,106].
Salt sensitivity is associated with reduced blood pressure dipping at night [107, 108], insulin resistance [109, 110], and increased sympathetic nerve activity [109, 111]. In the elderly, there is less nocturnal BP decline [112, 113] and this could be related to salt sensitivity and/or amount of salt intake. That salt sensitivity and/or high salt load in the elderly has been studied and when salt intake was reduced, there was a shift from non-dipping to a dipping state [114, 115]. Furthermore salt sensitivity is seen more commonly in hypertensives, blacks, women [116, 117], the elderly [116, 118], the obese [117, 119], and in Asians. Genetic studies done in Asia identified higher prevalence of salt sensitivity among the Chinese [120] and Japanese [104]. Due to the high intake of salt in Asia coupled with higher salt sensitivity in Asians and the elderly, and the evidence that salt reduction does indeed reduce BP, it would be beneficial to advise reduction in salt intake in elderly Asians.
17.4.4 Clinical Significance of the Pathophysiological Differences of Hypertension in the Elderly in Asia
The elderly is a vulnerable group with a high burden of diseases [75, 76, 121, 122] necessitating multiple drugs. Hence, it is not uncommon to see polypharmacy in the elderly. In Korea, 86.4% of elderly age 65 years and older were on multiple drugs, and similarly, in Japan the number of drugs ranged from 4.8 to 5.6 [123,124,125]. Because of multi-morbidity and differences in the pathophysiology of hypertension in the elderly, management of hypertension has to be adjusted accordingly when compared to younger individuals.
The differences between younger and older hypertensive patients can be summarized:
-
Isolated systolic hypertension is more common in the elderly and in the very old adults aged 75 years and older [31, 32].
-
Heart failure, HFpEF, is more common in the elderly [66, 69, 72, 73].
-
Elderly patients have more atrial fibrillation [79,80,81, 83, 84].
-
Renin concentrations are lower in the elderly [24].
-
White coat effect (isolated office hypertension) is more common in the elderly [35,36,37,38].
-
Masked hypertension is more common in the elderly [43, 47, 48].
-
Postural hypotension is more common in the elderly [45, 51,52,53].
-
Nocturnal dipping is commonly absent in elderly patients [112, 113].
-
Multi-comorbidities, more functional and cognitive impairments occur in the elderly [75, 76, 121, 122].
The clinical diagnosis of hypertension in the elderly is universally the same as for younger adults, ie a BP ≥140/90 mmHg [126,127,128] except for the recommendations by the USA where in 2017, their cut-off point for diagnosis was lowered by 10 mmHg to 130/80 irrespective of age [129]. Similarly, the diagnosis of isolated systolic hypertension is based on a systolic BP of ≥140 and diastolic BP of <90 mmHg while the USA uses systolic BP ≥130 and diastolic BP <80 mmHg.
Hypertension guidelines recommend assessing total CV risk rather than relying on the BP alone to decide on treatment. This is useful as often several mildly raised CV risk factors in someone with BP in the range of SBP of 140–150 mmHg may appear to be at low risk and hence dismissed as not needing treatment when in fact a formal calculation shows the patient actually to be at medium to high risk, thus necessitating treatment [130]. Most assessments in older patients for total/global CV risk invariably will be of medium or high risk, and a formal calculation is usually not needed. However, it is useful to do a global CV risk as it helps to decide how far to treat and the target BP. It is also helpful when there is uncertainty as to whether one really need to put a patient on anti-hypertensive therapy especially if patient is frail, has many other co-morbid conditions and a limited life span.
The elderly with hypertension of various forms will benefit from treatment [33, 34], and even the very elderly aged 80 and older also benefit [131, 132]. Several of the Asian guidelines do not differentiate between the “old” (≥65–74 years) and the “very old” (≥75 years) elderly. Most of the Asian guidelines for the management of hypertension in the elderly recommend a target that is similar to younger adults, <140/90 mmHg but not going below systolic BP of 130 mmHg for the old, and a target of <150/90 mmHg for the very old [127] (Table 17.1).
The recommended drug of choice for treatment of hypertension in the elderly is based on the mechanistic and pathophysiologic differences between younger and older adults and on clinical outcome trials. In Asia, all the guidelines recommend diuretics and calcium blockers for the elderly while a few countries included the RAS blockers [127, 133,134,135,136,137,138].
Many commonly used classes of anti-hypertensive drugs are generic, and more affordable to treat hypertension, even in the low middle-income countries in Asia. Despite this, BP control rates in Asia are all <50%, except for countries like Korea, Taiwan, and Singapore [6, 9].
In summary, hypertension in the elderly should be treated. However, the management of hypertension in the elderly needs to be individualized, where in healthier, ambulant elderly who are community dwelling, greater efforts could be made to achieve target BP. Rather than base treatment on chronological age, we should be using biological age as our guide on the management of hypertension in the elderly.
References
WHO. Ageing and health fact sheet. WHO Publication. 2018. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed 9 Aug 2021.
Department of Economic and Social Affairs, Population Division, United Nations. World Population Prospects 2019. https://population.un.org/wpp/. Accessed 9 Aug 2021.
Population and aging in Asia: the growing elderly population. Asia Development Bank. 2018. https://data.adb.org/dataset/population-and-aging-asia-and-pacific. Accessed 9 Aug 2021.
WHO. Hypertension fact sheet. WHO Publication. 2021. https://www.who.int/news-room/fact-sheets/detail/hypertension. Accessed 9 Aug 2021.
CDC. Prevalence of select measures among adults aged 20 and over: United States, 1999–2000 through 2017–2018. NHANES Interactive Data Visualizations. 2018. https://www.cdc.gov/nchs/nhanes/visualization/. Accessed 9 Aug 2021.
Chia Y-C, Buranakitjaroen P, Chen C-H, Divinagracia R, Hoshide S, Park S, et al. Current status of home blood pressure monitoring in Asia: statement from the HOPE Asia Network. J Clin Hypertens. 2017;19(11):1192–201.
Malaysia National Health and Morbidity Survey 2015. Non-communicable diseases, risk factors and other health related problems, Vol. II. Ministry of Health Malaysia. 2015. http://www.moh.gov.my/moh/resources/nhmsreport2015vol2.pdf. Accessed 9 Aug 2021.
Pakistan Health Research Council. Non-communicable Diseases Risk Factors Survey––Pakistan. Islamabad: World Health Organization; 2016. ISBN 978-969-499-008-8.
Kario K, Wang J-G. Could 130/80 mmHg be adopted as the diagnostic threshold and management goal of hypertension in consideration of the characteristics of Asian populations? Hypertension. 2018;71(6):979–84.
Ueshima H, Sekikawa A, Miura K, Turin TC, Takashima N, Kita Y, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008;118(25):2702–9.
Forouhi NG, Sattar N, Tillin T, McKeigue PM, Chaturvedi N. Do known risk factors explain the higher coronary heart disease mortality in South Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabetologia. 2006;49(11):2580–8.
Dou L, Liu X, Zhang T, Wu Y. Health care utilization in older people with cardiovascular disease in China. Int J Equity Health. 2015;14(1):59.
Coffman TM. The inextricable role of the kidney in hypertension. J Clin Invest. 2014;124(6):2341–7.
Coffman TM, Crowley SD. Kidney in hypertension. Hypertension. 2008;51(4):811–6.
Bidani AK, Griffin KA. Pathophysiology of hypertensive renal damage. Hypertension. 2004;44(5):595–601.
Hall JE, Granger JP, do Carmo JM, da Silva AA, Dubinion J, George E, et al. Hypertension: physiology and pathophysiology. Compr Physiol. 2012;2(4):2393–442.
Kotchen TA. Historical trends and milestones in hypertension research. Hypertension. 2011;58(4):522–38.
Sever PS, Messerli FH. Hypertension management 2011: optimal combination therapy. Eur Heart J. 2011;32(20):2499–506.
Zhao D, Liu H, Dong P, Zhao J. A meta-analysis of add-on use of spironolactone in patients with resistant hypertension. Int J Cardiol. 2017;233:113–7.
Wang C, Xiong B, Huang J. Efficacy and safety of spironolactone in patients with resistant hypertension: a meta-analysis of randomised controlled trials. Heart Lung Circ. 2016;25(10):1021–30.
Williams B, MacDonald TM, Morant SV, Webb DJ, Sever P, McInnes GT, et al. Endocrine and haemodynamic changes in resistant hypertension, and blood pressure responses to spironolactone or amiloride: the PATHWAY-2 mechanisms substudies. Lancet Diabet Endocrinol. 2018;6(6):464–75.
Weidmann P, De Myttenaere-Bursztein S, Maxwell MH, de Lima J. Effect on aging on plasma renin and aldosterone in normal man. Kidney Int. 1975;8(5):325–33.
Bauer JH. Age-related changes in the renin-aldosterone system. Physiological effects and clinical implications. Drugs Aging. 1993;3(3):238–45.
Messerli FH, Sundgaard-Riise K, Ventura HO, Dunn FG, Glade LB, Frohlich ED. Essential hypertension in the elderly: haemodynamics, intravascular volume, plasma renin activity, and circulating catecholamine levels. Lancet. 1983;2(8357):983–6.
Duprez DA, Munger MA, Botha J, Keefe DL, Charney AN. Aliskiren for geriatric lowering of systolic hypertension: a randomized controlled trial. J Hum Hypertens. 2010;24(9):600–8.
Mimran A, Ribstein J, Jover B. Aging and sodium homeostasis. Kidney Int Suppl. 1992;37:S107–13.
Epstein M, Hollenberg NK. Age as a determinant of renal sodium conservation in normal man. J Lab Clin Med. 1976;87(3):411–7.
Laurent S, Boutouyrie P. Arterial stiffness and hypertension in the elderly. Front Cardiovasc Med. 2020;7(202):544302.
Safar ME, Levy BI, Struijker-Boudier H. Current perspectives on arterial stiffness and pulse pressure in hypertension and cardiovascular diseases. Circulation. 2003;107(22):2864–9.
Deakin CD, Nolan JP, Soar J, Sunde K, Koster RW, Smith GB, et al. European Resuscitation Council guidelines for resuscitation 2010 section 4. Adult advanced life support. Resuscitation. 2010;81(10):1305–52.
Kannel WB, Dawber TR, McGee DL. Perspectives on systolic hypertension. The Framingham study. Circulation. 1980;61(6):1179–82.
Himmelmann A, Hedner T, Hansson L, O’Donnell CJ, Levy D. Isolated systolic hypertension: an important cardiovascular risk factor. Blood Press. 1998;7(4):197–207.
Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhäger WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet. 1997;350(9080):757–64.
Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA. 1991;265(24):3255–64.
Tanner RM, Shimbo D, Seals SR, Reynolds K, Bowling CB, Ogedegbe G, et al. White-coat effect among older adults: data from the Jackson heart study. J Clin Hypertens (Greenwich). 2016;18(2):139–45.
Pioli MR, Ritter AM, de Faria AP, Modolo R. White coat syndrome and its variations: differences and clinical impact. Integr Blood Press Control. 2018;11:73–9.
Williams B, Mancia G, Spiering W. ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;2018:39.
Helvaci MR, Seyhanli M. What a high prevalence of white coat hypertension in society! Intern Med. 2006;45(10):671–4.
Reddy AK, Jogendra MR, Rosendorff C. Blood pressure measurement in the geriatric population. Blood Press Monit. 2014;19(2):59–63.
de Simone G, Schillaci G, Chinali M, Angeli F, Reboldi GP, Verdecchia P. Estimate of white-coat effect and arterial stiffness. J Hypertens. 2007;25(4):827–31.
Cai P, Peng Y, Wang Y, Wang X. Effect of white-coat hypertension on arterial stiffness: a meta-analysis. Medicine. 2018;97(42):e12888.
Kario K, Tomitani N, Buranakitjaroen P, Chia YC, Park S, Chen CH, et al. Home blood pressure control status in 2017-2018 for hypertension specialist centers in Asia: results of the Asia BP@Home study. J Clin Hypertens. 2018;20(12):1686–95.
Cacciolati C, Hanon O, Alpérovitch A, Dufouil C, Tzourio C. Masked hypertension in the elderly: cross-sectional analysis of a population-based sample. Am J Hypertens. 2011;24(6):674–80.
Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007;25(11):2193–8.
Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens. 2011;24(1):52–8.
Mallion J-M, Clerson P, Bobrie G, Genes N, Vaisse B, Chatellier G. Predictive factors for masked hypertension within a population of controlled hypertensives. J Hypertens. 2006;24(12):2365–70.
Gorostidi M, Vinyoles E, Banegas JR, de la Sierra A. Prevalence of white-coat and masked hypertension in national and international registries. Hypertens Res. 2015;38(1):1–7.
Obara T, Ohkubo T, Funahashi J, Kikuya M, Asayama K, Metoki H, et al. Isolated uncontrolled hypertension at home and in the office among treated hypertensive patients from the J-HOME study. J Hypertens. 2005;23(9):1653–60.
Parashar R, Amir M, Pakhare A, Rathi P, Chaudhary L. Age related changes in autonomic functions. J Clin Diagn Res. 2016;10(3):CC11–C5.
Baker SE, Limberg JK, Dillon GA, Curry TB, Joyner MJ, Nicholson WT. Aging alters the relative contributions of the sympathetic and parasympathetic nervous system to blood pressure control in women. Hypertension. 2018;72(5):1236–42.
Gupta V, Lipsitz LA. Orthostatic hypotension in the elderly: diagnosis and treatment. Am J Med. 2007;120(10):841–7.
Brignole M. Progressive orthostatic hypotension in the elderly. e-journal of the ESC Council for Cardiology Practice 2006;5(10). https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-5/Progressive-orthostatic-hypotension-in-the-elderly-Title-Progressive-orthosta. Accessed 9 Aug 2021.
Saedon NI, Pin Tan M, Frith J. The prevalence of orthostatic hypotension: a systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci. 2020;75(1):117–22.
Grassi G, Mark A, Esler M. The sympathetic nervous system alterations in human hypertension. Circ Res. 2015;116(6):976–90.
Esler M. The sympathetic nervous system in hypertension: back to the future? Curr Hypertens Rep. 2015;17(2):11.
Catheter-based renal sympathetic denervation for resistant hypertension: Durability of blood pressure reduction out to 24 months. Hypertension 2011;57(5):911–7.
Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Böhm M. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet. 2010;376(9756):1903–9.
Courand PY, Feugier P, Workineh S, Harbaoui B, Bricca G, Lantelme P. Baroreceptor stimulation for resistant hypertension: first implantation in France and literature review. Arch Cardiovasc Dis. 2014;107(12):690–6.
Bhatt DL, Kandzari DE, O’Neill WW, D’Agostino R, Flack JM, Katzen BT, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370(15):1393–401.
Cuspidi C, Sala C, Negri F, Mancia G, Morganti A. Prevalence of left-ventricular hypertrophy in hypertension: an updated review of echocardiographic studies. J Hum Hypertens. 2012;26(6):343–9.
Ching S, Chia Y, Azman WW. Prevalence and determinants of left ventricular hypertrophy in hypertensive patients at a primary care clinic. Malays Fam Physician. 2012;7(2–3):2.
Krumholz HM, Larson M, Levy D. Sex differences in cardiac adaptation to isolated systolic hypertension. Am J Cardiol. 1993;72(3):310–3.
Chahal NS, Lim TK, Jain P, Chambers JC, Kooner JS, Senior R. New insights into the relationship of left ventricular geometry and left ventricular mass with cardiac function: a population study of hypertensive subjects. Eur Heart J. 2010;31(5):588–94.
Ganau A, Devereux RB, Roman MJ, de Simone G, Pickering TG, Saba PS, et al. Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. J Am Coll Cardiol. 1992;19(7):1550–8.
Devereux RB, James GD, Pickering TG. What is normal blood pressure? Comparison of ambulatory pressure level and variability in patients with normal or abnormal left ventricular geometry. Am J Hypertens. 1993;6(6 Pt 2):211s–5s.
Sweitzer NK, Lopatin M, Yancy CW, Mills RM, Stevenson LW. Comparison of clinical features and outcomes of patients hospitalized with heart failure and normal ejection fraction (> or =55%) versus those with mildly reduced (40% to 55%) and moderately to severely reduced (<40%) fractions. Am J Cardiol. 2008;101(8):1151–6.
Goldberg RJ, Spencer FA, Farmer C, Meyer TE, Pezzella S. Incidence and hospital death rates associated with heart failure: a community-wide perspective. Am J Med. 2005;118(7):728–34.
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics 2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139–596.
Butrous H, Hummel SL. Heart failure in older adults. Can J Cardiol. 2016;32(9):1140–7.
Nieminen MS, Brutsaert D, Dickstein K, Drexler H, Follath F, Harjola VP, et al. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27(22):2725–36.
Gheorghiade M, Abraham WT, Albert NM, Greenberg BH, O’Connor CM, She L, et al. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006;296(18):2217–26.
Oh GC, Cho H-J. Blood pressure and heart failure. Clin Hypertens. 2020;26(1):1.
Choi DJ, Han S, Jeon ES, Cho MC, Kim JJ, Yoo BS, et al. Characteristics, outcomes and predictors of long-term mortality for patients hospitalized for acute heart failure: a report from the Korean Heart Failure Registry. Korean Circ J. 2011;41(7):363–71.
Lee SE, Lee HY, Cho HJ, Choe WS, Kim H, Choi JO, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure Registry (KorAHF). Korean Circ J. 2017;47(3):341–53.
Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162(20):2269–76.
Murad K, Goff DC Jr, Morgan TM, Burke GL, Bartz TM, Kizer JR, et al. Burden of comorbidities and functional and cognitive impairments in elderly patients at the initial diagnosis of heart failure and their impact on total mortality: the cardiovascular health study. JACC Heart Fail. 2015;3(7):542–50.
Marengoni A, Tazzeo C, Calderón-Larrañaga A, Roso-Llorach A, Onder G, Zucchelli A, et al. Multimorbidity patterns and 6-year risk of institutionalization in older persons: the role of social formal and informal care. J Am Med Dir Assoc. 2021;22:2184.
Karamichalakis N, Letsas KP, Vlachos K, Georgopoulos S, Bakalakos A, Efremidis M, et al. Managing atrial fibrillation in the very elderly patient: challenges and solutions. Vasc Health Risk Manag. 2015;11:555–62.
Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285(18):2370–5.
Krijthe BP, Kunst A, Benjamin EJ, Lip GY, Franco OH, Hofman A, et al. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur Heart J. 2013;34(35):2746–51.
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation. Circulation. 2014;129(8):837–47.
Kistler PM, Sanders P, Fynn SP, Stevenson IH, Spence SJ, Vohra JK, et al. Electrophysiologic and electroanatomic changes in the human atrium associated with age. J Am Coll Cardiol. 2004;44(1):109–16.
Nabauer M, Gerth A, Limbourg T, Schneider S, Oeff M, Kirchhof P, et al. The Registry of the German competence NETwork on atrial fibrillation: patient characteristics and initial management. Europace. 2009;11(4):423–34.
Verdecchia P, Angeli F, Reboldi G. Hypertension and atrial fibrillation. Circ Res. 2018;122(2):352–68.
Dominiczak A, Delles C, Padmanabhan S. Genomics and precision medicine for clinicians and scientists in hypertension. Hypertension. 2017;69(4):e10–e3.
Kato N, Loh M, Takeuchi F, Verweij N, Wang X, Zhang W, et al. Trans-ancestry genome-wide association study identifies 12 genetic loci influencing blood pressure and implicates a role for DNA methylation. Nat Genet. 2015;47(11):1282–93.
Mattson DL, Liang M. Hypertension: from GWAS to functional genomics-based precision medicine. Nat Rev Nephrol. 2017;13(4):195–6.
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15(5):288–98.
Cameron AJ, Shaw JE, Zimmet PZ. The metabolic syndrome: prevalence in worldwide populations. Endocrinol Metab Clin N Am. 2004;33(2):351–75.
Ramachandran A, Chamukuttan S, Shetty SA, Arun N, Susairaj P. Obesity in Asia – is it different from rest of the world. Diabetes Metab Res Rev. 2012;28(s2):47–51.
McKeigue PM, Shah B, Marmot MG. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet. 1991;337(8738):382–6.
Larsson SC, Bäck M, Rees JMB, Mason AM, Burgess S. Body mass index and body composition in relation to 14 cardiovascular conditions in UK Biobank: a Mendelian randomization study. Eur Heart J. 2020;41(2):221–6.
Zamboni M, Mazzali G. Obesity in the elderly: an emerging health issue. Int J Obes. 2012;36(9):1151–2.
Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307(5):491–7.
Ariaratnam S, Rodzlan Hasani WS, Krishnapillai AD, Abd Hamid HA, Jane Ling MY, Ho BK, et al. Prevalence of obesity and its associated risk factors among the elderly in Malaysia: findings from The National Health and Morbidity Survey (NHMS) 2015. PLoS One. 2020;15(9):e0238566.
Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371(7):624–34.
WHO. Fact sheet on salt reduction. WHO Publication. 2020. https://www.who.int/news-room/fact-sheets/detail/salt-reduction. Accessed 9 Aug 2021.
INTERSALT study an international co-operative study on the relation of blood pressure to electrolyte excretion in populations. I. Design and methods. The INTERSALT Co-operative Research Group. J Hypertens. 1986;4(6):781–7.
Dahl. Possible role of salt intake in the development of essential hypertension. In: Cottier P, Bock D, editors. Essential hypertension: an international symposium. Berlin: Springer; 1960. p. 52–65.
Stamler J. The INTERSALT Study: background, methods, findings, and implications. Am J Clin Nutr. 1997;65(2 Suppl):626s–42s.
Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ. 1988;297(6644):319–28.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N Engl J Med. 2001;344(1):3–10.
Zhou BF, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C, et al. Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. J Hum Hypertens. 2003;17(9):623–30.
Katsuya T, Ishikawa K, Sugimoto K, Rakugi H, Ogihara T. Salt sensitivity of Japanese from the viewpoint of gene polymorphism. Hypertens Res. 2003;26(7):521–5.
Obarzanek E, Proschan MA, Vollmer WM, Moore TJ, Sacks FM, Appel LJ, et al. Individual blood pressure responses to changes in salt intake. Hypertension. 2003;42(4):459–67.
Stamler J, Rose G, Stamler R, Elliott P, Dyer A, Marmot M. INTERSALT study findings. Public health and medical care implications. Hypertension. 1989;14(5):570–7.
Higashi Y, Oshima T, Ozono R, Nakano Y, Matsuura H, Kambe M, et al. Nocturnal decline in blood pressure is attenuated by NaCl loading in salt-sensitive patients with essential hypertension: noninvasive 24-hour ambulatory blood pressure monitoring. Hypertension. 1997;30(2 Pt 1):163–7.
Takakuwa H, Shimizu K, Izumiya Y, Kato T, Nakaya I, Yokoyama H, et al. Dietary sodium restriction restores nocturnal reduction of blood pressure in patients with primary aldosteronism. Hypertens Res. 2002;25(5):737–42.
Yatabe MS, Yatabe J, Yoneda M, Watanabe T, Otsuki M, Felder RA, et al. Salt sensitivity is associated with insulin resistance, sympathetic overactivity, and decreased suppression of circulating renin activity in lean patients with essential hypertension. Am J Clin Nutr. 2010;92(1):77–82.
Melander O, Groop L, Hulthén UL. Effect of salt on insulin sensitivity differs according to gender and degree of salt sensitivity. Hypertension. 2000;35(3):827–31.
Ebata H, Hojo Y, Ikeda U, Ishida H, Natsume T, Shimada K. Differential effects of an alpha 1-blocker (doxazosin) on diurnal blood pressure variation in dipper and non-dipper type hypertension. Hypertens Res. 1995;18(2):125–30.
O’Sullivan C, Duggan J, Atkins N, O’Brien E. Twenty-four-hour ambulatory blood pressure in community-dwelling elderly men and women, aged 60-102 years. J Hypertens. 2003;21(9):1641–7.
Imai Y, Nagai K, Sakuma M, Sakuma H, Nakatsuka H, Satoh H, et al. Ambulatory blood pressure of adults in Ohasama, Japan. Hypertension. 1993;22(6):900–12.
Uzu T, Ishikawa K, Fujii T, Nakamura S, Inenaga T, Kimura G. Sodium restriction shifts circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation. 1997;96(6):1859–62.
Uzu T, Kimura G, Yamauchi A, Kanasaki M, Isshiki K, Araki SI. Enhanced sodium sensitivity and disturbed circadian rhythm of blood pressure in essential hypertension. J Hypertens. 2006;24:1627.
He J, Gu D, Chen J, Jaquish CE, Rao DC, Hixson JE, et al. Gender difference in blood pressure responses to dietary sodium intervention in the GenSalt study. J Hypertens. 2009;27(1):48–54.
Vollmer WM, Sacks FM, Ard J, Appel LJ, Bray GA, Simons-Morton DG, et al. Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med. 2001;135(12):1019–28.
Weinberger MH, Fineberg NS. Sodium and volume sensitivity of blood pressure. Age and pressure change over time. Hypertension. 1991;18(1):67–71.
Elijovich F, Weinberger MH, Anderson CA, Appel LJ, Bursztyn M, Cook NR, et al. Salt sensitivity of blood pressure: a scientific statement from the American Heart Association. Hypertension. 2016;68(3):e7–e46.
Liu Y, Shi M, Dolan J, He J. Sodium sensitivity of blood pressure in Chinese populations. J Hum Hypertens. 2020;34(2):94–107.
Mitsutake SIT, Teramoto C, Shimizu S, Ito H. Patterns of co-occurrence of chronic disease among older adults in Tokyo, Japan. Prev Chronic Dis. 2019;16(180170) https://doi.org/10.5888/pcd16.180170. Accessed 9 Aug 2021.
Jang I-Y, Lee HY, Lee E. Th anniversary Committee of Korean Geriatrics S. geriatrics fact sheet in Korea 2018 from National Statistics. Ann Geriatr Med Res. 2019;23(2):50–3.
Kim H-A, Shin J-Y, Kim M-H, Park B-J. Prevalence and predictors of polypharmacy among Korean elderly. PLoS One. 2014;9(6):e98043.
Mabuchi T, Hosomi K, Yokoyama S, Takada M. Polypharmacy in elderly patients in Japan: analysis of Japanese real-world databases. J Clin Pharm Ther. 2020;45(5):991–6.
Morin L, Johnell K, Laroche M-L, Fastbom J, Wastesson JW. The epidemiology of polypharmacy in older adults: register-based prospective cohort study. Clin Epidemiol. 2018;10:289–98.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39(33):3021–104.
Chia Y-C, Turana Y, Sukonthasarn A, Zhang Y, Shin J, Cheng H-M, et al. Comparison of guidelines for the management of hypertension: similarities and differences between international and Asian countries; perspectives from HOPE-Asia Network. J Clin Hypertens. 2021;23(3):422–34.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334–57.
Whelton PK, Williams B. The 2018 European Society of Cardiology/European Society of Hypertension and 2017 American College of Cardiology/American Heart Association blood pressure guidelines: more similar than DifferentComparison of the 2018 ESC/ESH and 2017 ACC/AHA hypertension GuidelinesComparison of the 2018 ESC/ESH and 2017 ACC/AHA hypertension guidelines. JAMA. 2018;320(17):1749–50.
Chia Y. Review of tools of cardiovascular disease risk stratification: interpretation, customisation and application in clinical practice. Singap Med J. 2011;52(2):116–23.
Bulpitt C, Fletcher A, Beckett N, Coope J, Gil-Extremera B, Forette F, et al. Hypertension in the very elderly trial (HYVET): protocol for the main trial. Drugs Aging. 2001;18(3):151–64.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–98.
Liu J. Highlights of the 2018 Chinese hypertension guidelines. Clin Hypertens. 2020;26(1):8.
Kim HC, Ihm S-H, Kim G-H, Kim JH, Kim K-i, Lee H-Y, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part I-epidemiology of hypertension. Clin Hyperten. 2019;25(1):16.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42(9):1235–481.
Philippines clinical practice guideline for adult hypertension-prevention, screening, counseling and management. 2018. www.mahealthcare.com/pdf/practice_guidelines.
2018 Vietnam National Heart Association/Vietnam Society of Hypertension guidelines on diagnosis and treatment of arterial hypertension in adults. 2018 VNHA/VSH guidelines for diagnosis and treatment of hypertension … slideshare.net. Accessed 9 Aug 2021.
2018 Pakistan Hypertension League 3rd National Guideline for the prevention, detection, evaluation and Managment of hypertension 2018. PHL 2018 Magazine Final 1. phlpk.org. Accessed 9 Aug 2021.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chia, YC. (2022). Hypertension in the Elderly: Pathophysiology and Clinical Significance. In: Ram, C.V.S., Teo, B.W.J., Wander, G.S. (eds) Hypertension and Cardiovascular Disease in Asia. Updates in Hypertension and Cardiovascular Protection. Springer, Cham. https://doi.org/10.1007/978-3-030-95734-6_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-95734-6_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-95733-9
Online ISBN: 978-3-030-95734-6
eBook Packages: MedicineMedicine (R0)