Abstract
Retinal changes in patients with arterial hypertension have been described since the middle of the 19th century. From the famous work by Keith, Wagener, and Barker in 1939 until today, advanced retinal changes assessed by ophthalmoscopy, i.e., grades 3 and 4 of hypertensive retinopathy, as defined according to the traditional classification system established by the aforementioned authors, are indicative of adverse cardiovascular prognosis in patients with arterial hypertension. However, ophthalmoscopy has been repeatedly criticized over the last decades as it was found to be unreliable in mild and moderate arterial hypertension. Therefore, in the last decades, much research effort has been focused on the improvement of imaging technologies that can detect early vascular changes, i.e., arteriolar narrowing, microvascular rarefaction, arteriolar remodeling, and vascular dysfunction among others, in the retinal vascular bed and to assess the prognostic role of these early retinal vascular changes in arterial hypertension.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keyword
- Arterial hypertension
- Target organ damage
- Retina
- Ophthalmoscopy
- Digital retinal photography
- Scanning laser doppler flowmetry
- Arteriolar narrowing
- Microvascular rarefaction
- Arterial remodeling
- Vascular dysfunction
1 Introduction
As the cornea, lens, and vitreous humor lack blood vessels and are transparent, the retina offers the unique opportunity to examine the body’s microvasculature in vivo safely, repeatedly, and noninvasively. Retinal arterioles undergo similar changes as cerebral, coronary, and peripheral arterioles in hypertension indicating that retinal arteriolar abnormalities mirror structural and functional microvascular changes elsewhere in end-organ tissues [1, 2]. As retinal and cerebral circulation share common anatomical, physiological, and embryological features, retinal circulation might be a model for cerebral microvasculature. This was supported by an autopsy study of patients with stroke, which showed a close correlation between retinal and cerebral arteriolar findings [3]. Therefore, it is not surprising that retinal microvascular abnormalities present an important prognostic value, in particular with respect to cardiovascular events and cardiovascular mortality [4].
The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure lists retinopathy as one of several markers of target organ damage in hypertension [5]. In contrast, the current guidelines of the European Society of Hypertension and European Society of Cardiology 2007/2009 [6, 7] list retinopathy as target organ damage only for grades 3 and 4 of hypertensive retinopathy. This change in guidelines reflects the repeated criticism that arose over the last decade with respect to the usefulness of the traditional classification system of hypertensive retinopathy for current clinical practice [8–10]. As a result, much research effort has been focused on the development of new imaging techniques to analyze retinal arteriolar structure and function in subjects with hypertension more precisely.
2 Historical Context and Classification
Signs of hypertensive retinopathy were already described by Liebreich [11] in 1859 and then by Gunn [12] in 1892. The traditional classification of hypertensive retinopathy can be dated to a publication by Keith and colleagues in 1939 in which the authors classified hypertensive retinopathy into four grades of increasing severity [13]. In the last 20 years, retinal photographs were repeatedly used to assess the retinal microvasculature in patients with arterial hypertension. Further progress in imaging techniques [digital photography and scanning laser Doppler flowmetry (SLDF)] now allows the assessment of early structural [e.g., arteriole-to-venule ratio (AVR)] of retinal vessels, arteriolar length-to-diameter ratio, vessel density/rarefaction and tortuosity, the wall-to-lumen ratio of retinal arterioles and early functional parameters (e.g., vasoconstrictor and vasodilatory properties) of retinal microvasculature in arterial hypertension.
3 Assessment of Hypertensive Retinopathy
3.1 Hypertensive Retinopathy by Ophthalmoscopy
Direct ophthalmoscopy provides a magnified (x16) vision of the posterior pole of the retina. The procedure ought to be performed after the induction of pharmacological mydriasis and requires a certain degree of patient collaboration. It is an inexpensive method to assess retinal arteriolar structure. However, direct ophthalmoscopy has been shown to be subjective and unreliable [14–16], with significant interobserver (20–42 %) and intraobserver (10–33 %) variations in the assessment of different retinal lesions [16]. Moreover, it was found to be particularly unreliable in mild to moderate hypertension [15].
Test–retest analyses revealed poor reliability in the early stages of hypertensive retinopathy, whereas grade 3 and 4 retinopathy as classified by Keith and colleagues [13] is still a valid diagnostic criteria of severe retinal damage [4, 17–19]. In 2004, Wong and Mitchell proposed a new and simple classification system of retinal microvascular signs, detectable by ophthalmoscopy, based on the strength of the reported associations of various retinopathy markers [8]. They graded retinal vascular signs into mild [generalized arteriolar narrowing, focal arteriolar narrowing, arteriovenous nicking, and arteriolar wall opacity (silver wiring)], moderate [hemorrhage (blot-, dot-, or flame-shaped), microaneurysm, cotton-wool spot and hard exudates], and malignant (moderate retinopathy plus optic disc swelling) [8].
3.2 Hypertensive Retinopathy by Retinal Photography
The use of retinal photographs in combination with standardized protocols, blinded grading, and special software has improved the reliability of assessing retinal microvascular abnormalities and has led to a more precise and objective quantification of retinal microvascular signs [20]. Retinal photography can be carried using standard film or with digital equipment. Both traditional fundus cameras and nonmydriatic models are widely used.
3.2.1 Arteriole-to-Venule Ratio
Digital nonmydriatic cameras allow computer-assisted or fully automated detection of different retinopathy lesions, and the calculation of the AVR of retinal vessels. The calculation of the AVR is of particular interest since the measurement of arteriolar narrowing cannot be quantified by ophthalmoscopy. The calculation of the AVR is based on the assumption that high blood pressure is associated with narrower retinal arteriolar diameters [21–24], though it does not affect retinal venular diameters. However, recent data suggest that venular diameter is also affected by several conditions including diabetes, metabolic syndrome, smoking, and inflammation [25–29], and therefore influence the AVR independently from changes in the diameter of retinal arterioles. Nonetheless, the narrowing of arterioles is considered to represent the earliest alteration of the microvasculature, including the retinal microvasculature, in hypertensive subjects [30–32].
3.2.2 Topological Changes in Retinal Vascular Architecture
The parameters of the arteriolar and venular network may also be altered in patients with primary hypertension. Several parameters have been suggested to assess arteriolar narrowing (e.g., the length-to-diameter ratio) calculated as the ratio of the length of a vessel segment between two branching points to its average diameter), vascular rarefaction (e.g., the number of terminal branches), or vessel tortuosity (e.g., the ratio of the actual length of the vessel segment to the straight line distance between two connected branching points) [33, 34]. However, these parameters, although scientifically very interesting, are as yet to be introduced into clinical practice.
3.3 Hypertensive Retinopathy by Scanning Laser Doppler Flowmetry
SLDF with automatic full-field perfusion imaging analysis (AFFPIA) allows the measurement of retinal capillary perfusion as well as the calculation of the inner and outer diameters of retinal arterioles, thereby allowing the precise analysis of retinal vascular function and arteriolar remodeling in hypertension [35–37]. Of clinical interest, both vascular dysfunction—at least when assessed in the peripheral [38, 39] and coronary [40] circulation—and arterial remodeling—at least when assessed in vitro in small subcutaneous arteries and arterioles [41–43]—have been found to be of prognostic significance with respect to cardiovascular events.
SLDF with AFFPIA is performed without the need for prior mydriasis. The method is safe, noninvasive, and has a short examination time of approximately 5 min. It is highly reliable [36, 44–46], but must be performed by a trained and certified observer.
3.4 Vascular Function of Retinal Vessels
Retinal vascular function can be assessed by examining the vasodilator capacity of retinal vessels, i.e., the increase in retinal capillary perfusion in response to flicker light exposure [37, 47–49], or more invasively, by examining the vasoconstrictor properties of retinal vessels by assessing the decrease in retinal capillary perfusion in response to the infusion of the nitric oxide synthase inhibitor NG-monomethyl-l-arginine (L-NMMA) [35, 37, 48, 49].
Recent studies have shown that the vasoconstrictor response of retinal vessels, assessed by the change in retinal capillary blood flow in response to the infusion of L-NMMA, is impaired in lean [35] and obese or overweight [37] subjects with primary hypertension. Blood pressure reduction induced pharmacologically by inhibitors of the renin–angiotensin system was found to improve the vasoconstrictor response of retinal vessels to L-NMMA infusion [35].
3.5 Remodeling of Retinal Arterioles
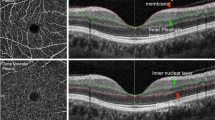
Remodeling of retinal arterioles is assessed by measuring the inner retinal arteriolar diameter in perfusion images and the outer retinal arteriolar diameter in reflection images, with subsequent calculation of the wall-to-lumen ratio [36, 37, 50, 51], wall cross-sectional area [37, 50, 51], and other parameters of retinal arteriolar remodeling according to previously described formulas [50, 51] (see Fig. 13.1).
Screenshot for the assessment of remodeling of retinal arterioles using scanning laser Doppler flowmetry with automatic full-field perfusion imaging analysis. The outer diameter is measured in reflexion images, whereby differences between the light intensity of reflected light between two points lying side by side, due to the acute angle at the outer vessel wall border, allow the detection of the outer diameter of the arteriole. The inner diameter is measured in perfusion images, whereby the bloodstream, due to high velocity in the center of the arteriolar lumen, and decreasing blood velocity toward to periphery of the arteriolar lumen allow the calculation of a parabolic velocity curve and thereby the measurement of the inner diameter of the arteriolar vessel. Subsequently, the wall-to-lumen ratio, wall cross-sectional area, and wall thickness can be calculated based on the measurements of the inner and outer diameter of the arteriole [37]
The wall-to-lumen ratio of retinal arterioles was found to be greater in hypertensive compared to normotensive patients and systolic and diastolic blood pressure levels were found to be related to the wall-to-lumen ratio of retinal arterioles [37]. Treated hypertensive patients with well-controlled hypertension revealed lower wall-to-lumen ratio of retinal arterioles than patients with uncontrolled hypertension [36]. Moreover, in hypertensive patients, the wall-to-lumen ratio of retinal arterioles was negatively related to the vasodilatory response of retinal vessels to flicker light exposure, indicating that hypertensive patients with a greater wall-to-lumen ratio might reveal impaired vasodilatory properties of their retinal vessels [48].
4 Retinal Microvascular Abnormalities and Hypertensive Organ Damage
4.1 Cerebrovascular Disease
The Atherosclerosis Risk in Communities (ARIC) study [17], the Cardiovascular Health Study [18], the Beaver Dam Eye Study [4], and the Shibata Study [19] revealed an increased risk of stroke in patients with hypertensive retinopathy, analysed by retinal photographs, than in patients without signs of hypertensive retinopathy. However, these population-based studies also indicate that earlier signs of hypertensive retinopathy (e.g., generalized and focal narrowing of arterioles and arteriovenous nicking) were weaker and less consistent when associated with stroke [17] and death from stroke [4]. The ARIC study demonstrated that hypertensive retinopathy adds additional predictive value for incident stroke in patients with cerebral white matter lesions [52]. Retinal microvascular alterations were also associated with magnetic resonance imaging-defined subclinical cerebral infarction [53], cerebral white matter lesions [52], cognitive impairment [54, 55], dementia [55], and cerebral atrophy [56]. The wall-to-lumen ratio [36] and wall cross-sectional area [57] of retinal arterioles have been found to be greater in hypertensive subjects with a history of a cerebrovascular event compared with uncomplicated hypertensive and normotensive subjects.
4.2 Cardiac Disease
Retinal microvascular abnormalities have been found to be associated with ischemic changes on electrocardiography [58], left ventricular hypertrophy [59], coronary heart disease [60–63], congestive heart failure [64], and lower hyperemic myocardial blood flow and perfusion reserve in subjects without coronary artery calcification [65].
4.3 Renal Disease
In the ARIC study, subjects with retinopathy were more likely to develop renal dysfunction than individuals without [66]. This was confirmed by the Cardiovascular Health Study [67]. In a cross-sectional study, we found a close relationship between the wall-to-lumen ratio of retinal arterioles and urinary albumin excretion, and an estimated creatinine clearance >60 mL/min in 37 male subjects who were either normotensive or revealed primary hypertension [68].
5 Arterial Stiffness, Carotid Intima-Media Thickness, and Carotid Plaques
In the ARIC study, carotid arterial stiffness, estimated from high-resolution ultrasonic echo tracking of the left common carotid artery and defined as the adjusted arterial diameter change, was related to generalized retinal arteriolar narrowing, as assessed by examining the AVR of retinal vessels in subjects aged 45–64 [69]. In the Multi-Ethnic Study of Atherosclerosis, reduced aortic distensibility, as an indicator for aortic stiffness, was associated with reduced arteriolar caliber in participants free of cardiovascular disease [70]. In a small study in patients with primary hypertension, retinopathy was associated with carotid intima-media thickness and carotid plaque score [71].
All these trials clearly indicate a coincidental occurrence of microvascular retinal abnormalities and cardiovascular morbidity and hypertensive target organ damage, respectively. However, although some of these studies adjusted for other classic cardiovascular risk factors to a greater or lesser extent, none of them adequately evaluated whether the assessment of microvascular retinal changes is of additive value on top of the assessment of established parameters of target organ damage [6] (e.g., urinary albumin excretion, left ventricular hypertrophy, carotid artery intima-media thickness, and pulse wave velocity). This lack of inclusion of other measures of target organ damage limits the value of evaluating retinopathy in hypertension (unless in hypertensive emergency). Nonetheless, with the advancement of imaging technologies, changes in retinal microvascular circulation may be detected noninvasively at an early stage and more accurately than other subclinical target organ damage.
6 Retinal Microvascular Alterations and Mortality
Several studies performed in the middle of the 20th century or thereafter, which relied on ophthalmoscopy (with all its limitations), revealed that hypertensive patients with moderate to severe retinal microvascular abnormalities had an increased risk of mortality [13, 58, 72–78]. However, it can be problematic to generalize from these earlier studies, carried out in patients with uncontrolled and untreated hypertension to current patients with cardioprotective treatment, who present with less severe signs of hypertensive retinopathy.
In a nested case–control analysis of the Beaver Dam Eye Study, an increased risk of ischemic heart disease death was associated with a suboptimal relationship of retinal arteriolar diameter at bifurcation, even after adjusting for age, sex, past history of cardiovascular disease, and other known cardiovascular risk factors [79]. In another nested case–control analysis of the Beaver Dam Eye Study, a weak association between generalized retinal arteriolar narrowing, defined by the AVR of retinal vessels, and cardiovascular mortality was found for subjects aged 43–74 but not for subjects aged 75 years or older [4], whereas an analysis of the entire Beaver Dam cohort did not reveal an association between the AVR of retinal vessels or its components (arteriolar and venular diameter) and all-cause or vascular disease-related mortality [80]. However, adjustment for other parameters of hypertensive target organ damage was not performed in the aforementioned studies.
Unfortunately, studies analyzing the impact of retinal vascular function (i.e., the change of retinal capillary blood flow in response to flicker light exposure or to an infusion of L-NMMA) and/or precise analyses of retinal arteriolar remodeling (i.e., the calculation of the wall-to-lumen ratio and wall cross-sectional area of retinal arterioles) on cardiovascular mortality have not been conducted as these methodical approaches have only recently been introduced [35, 36].
7 Conclusions
There is an abundance of evidence that advanced retinopathy [grade 3 and 4 hypertensive retinopathy or moderate to severe (malignant) retinopathy] implies an increased risk of cardiovascular complications and mortality in hypertensive subjects. However, the evidence is weaker and inconsistent for the earlier signs of hypertensive retinopathy. Earlier signs of hypertensive retinopathy are very common among hypertensive subjects and appear to be among the earliest signs of vascular alterations in hypertension. Unfortunately, the detection of early retinopathy in hypertension is currently associated with several limitations.
First, direct ophthalmoscopy is subjective and unreliable in patients with grade 1 and 2 hypertensive retinopathy. Second, grade 1 and 2 hypertensive retinopathy cannot be distinguished by most physicians, even when retinal photographs are analyzed. Third, the approach of calculating the AVR of retinal vessels, as a parameter of generalized retinal arteriolar narrowing, from digitized photographs has insufficient explanatory power since AVR is not only dependent on the arteriolar diameter but also on the venular diameter. However, a novel approach, SLDF with AFFPIA, might be useful in better characterizing early retinal microvascular alterations, since this method allows the detection of retinal vascular function and the detailed analysis of retinal arteriolar remodeling. Future studies with large cohorts that also adjust for other markers of target organ damage and cardiovascular risk factors are needed to assess the impact of retinal vascular function and arteriolar remodeling on clinical cardiovascular disease as well as mortality.
References
Tso MO, Jampol LM (1982) Pathophysiology of hypertensive retinopathy. Ophthalmology 89:1132–1145
Rizzoni D, De Ciuceis C, Porteri E et al (2011) Close relationship between media to lumen ratio of subcutaneous small arteries and wall to lumen ratio of retinal arterioles evaluated non invasively by scanning lasaer doppler flowmetry. J Hypertens 29(e-Supplement A):e11 (Abstract)
Goto I, Katsuki S, Ikui H et al (1975) Pathological studies on the intracerebral and retinal arteries in cerebrovascular and noncerebrovascular diseases. Stroke 6:263–269
Wong TY, Klein R, Nieto FJ et al (2003) Retinal microvascular abnormalities and 10-year cardiovascular mortality: a population-based case-control study. Ophthalmology 110:933–940
Chobanian AV, Bakris GL, Black HR et al (2003) Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42:1206–1252
Mancia G, De Backer G, Dominiczak A et al (2007) Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of hypertension (ESH) and of the European society of cardiology (ESC). J Hypertens 25:1105–1187
Mancia G, Laurent S, Agabiti-Rosei E et al (2009) Reappraisal of European guidelines on hypertension management: a European society of hypertension task force document. J Hypertens 27:2121–2158
Wong TY, Mitchell P (2004) Hypertensive retinopathy. N Engl J Med 351:2310–2317
van den Born BJ, Hulsman CA, Hoekstra JB et al (2005) Value of routine funduscopy in patients with hypertension: systematic review. BMJ 331:73
Chatterjee S, Chattopadhya S, Hope-Ross M et al (2002) Hypertension and the eye: changing perspectives. J Hum Hypertens 16:667–675
Liebreich R (1859) Ophthalmoskopischer Befund bei Morbus Brightii. Albrecht von Graefes Arch Ophthalmol 5:265–268
Gunn RM (1892) Ophthalmoscopic evidence of (1) arterial changes with chronic renal diseases and (2) of increased arterial tension. Trans Ophthalmol Soc U K 12:124–125
Keith NM, Wagener HP, Barker NW (1939) Some different types of essential hypertension: their course and prognosis. Am J Med Sci 197:332–343
Aoki N, Horibe H, Ohno Y et al (1977) Epidemiological evaluation of funduscopic findings in cerebrovascular diseases. III. Observer variability and reproducibility for funduscopic findings. Jpn Circ J 41:11–17
Dimmitt SB, West JN, Eames SM et al (1989) Usefulness of ophthalmoscopy in mild to moderate hypertension. Lancet 1:1103–1106
Kagan A, Aurell E, Tibblin G (1967) Signs in the fundus oculi and arterial hypertension: unconventional assessment and significance. Bull World Health Organ 36:231–241
Wong TY, Klein R, Couper DJ et al (2001) Retinal microvascular abnormalities and incident stroke: the atherosclerosis risk in communities study. Lancet 358:1134–1140
Wong TY, Klein R, Sharrett AR et al (2003) The prevalence and risk factors of retinal microvascular abnormalities in older persons: the cardiovascular health study. Ophthalmology 110:658–666
Nakayama T, Date C, Yokoyama T et al (1997) A 15.5-year follow-up study of stroke in a Japanese provincial city. The Shibata Study. Stroke 28:45–52
Moss SE, Klein R, Kessler SD et al (1985) Comparison between ophthalmoscopy and fundus photography in determining severity of diabetic retinopathy. Ophthalmology 92:62–67
Hubbard LD, Brothers RJ, King WN et al (1999) Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the atherosclerosis risk in communities study. Ophthalmology 106:2269–2280
Sharrett AR, Hubbard LD, Cooper LS et al (1999) Retinal arteriolar diameters and elevated blood pressure: the atherosclerosis risk in communities study. Am J Epidemiol 150:263–270
Wong TY, Hubbard LD, Klein R et al (2002) Retinal microvascular abnormalities and blood pressure in older people: the cardiovascular health study. Br J Ophthalmol 86:1007–1013
Wong TY, Knudtson MD, Klein R et al (2004) Computer-assisted measurement of retinal vessel diameters in the Beaver Dam Eye Study: methodology, correlation between eyes, and effect of refractive errors. Ophthalmology 111:1183–1190
Nguyen TT, Wong TY (2006) Retinal vascular manifestations of metabolic disorders. Trends Endocrinol Metab 17:262–268
Ikram MK, de Jong FJ, Vingerling JR et al (2004) Are retinal arteriolar or venular diameters associated with markers for cardiovascular disorders? The Rotterdam Study. Invest Ophthalmol Vis Sci 45:2129–2134
Kawasaki R, Tielsch JM, Wang JJ et al (2008) The metabolic syndrome and retinal microvascular signs in a Japanese population: the funagata study. Br J Ophthalmol 92:161–166
Wong TY, Duncan BB, Golden SH et al (2004) Associations between the metabolic syndrome and retinal microvascular signs: the atherosclerosis risk in communities study. Invest Ophthalmol Vis Sci 45:2949–2954
Sun C, Liew G, Wang JJ et al (2008) Retinal vascular caliber, blood pressure, and cardiovascular risk factors in an Asian population: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci 49:1784–1790
Intengan HD, Schiffrin EL (2001) Vascular remodeling in hypertension: roles of apoptosis, inflammation, and fibrosis. Hypertension 38:581–587
Schiffrin EL (2004) Remodeling of resistance arteries in essential hypertension and effects of antihypertensive treatment. Am J Hypertens 17:1192–1200
Park JB, Schiffrin EL (2001) Small artery remodeling is the most prevalent (earliest?) form of target organ damage in mild essential hypertension. J Hypertens 19:921–930
Hughes AD, Stanton AV, Jabbar AS et al (2008) Effect of antihypertensive treatment on retinal microvascular changes in hypertension. J Hypertens 26:1703–1707
Hughes AD, Martinez-Perez ME, Jabbar AS et al (2006) Quantification of topological changes in retinal vascular architecture in essenital and malignant hypertension. J Hypertens 24:889–894
Delles C, Michelson G, Harazny J et al (2004) Impaired endothelial function of the retinal vasculature in hypertensive patients. Stroke 35:1289–1293
Harazny JM, Ritt M, Baleanu D et al (2007) Increased wall:lumen ratio of retinal arterioles in male patients with a history of a cerebrovascular event. Hypertension 50:623–629
Ritt M, Harazny JM, Ott C et al (2008) Analysis of retinal arteriolar structure in never-treated patients with essential hypertension. J Hypertens 26:1427–1434
Perticone F, Ceravolo R, Pujia A et al (2001) Prognostic significance of endothelial dysfunction in hypertensive patients. Circulation 104:191–196
Heitzer T, Schlinzig T, Krohn K et al (2001) Endothelial dysfunction, oxidative stress, and risk of cardiovascular events in patients with coronary artery disease. Circulation 104:2673–2678
Schachinger V, Britten MB, Zeiher AM (2000) Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation 101:1899–1906
Mathiassen ON, Buus NH, Sihm I et al (2007) Small artery structure is an independent predictor of cardiovascular events in essential hypertension. J Hypertens 25:1021–1026
De Ciuceis C, Porteri E, Rizzoni D et al (2007) Structural alterations of subcutaneous small-resistance arteries may predict major cardiovascular events in patients with hypertension. Am J Hypertens 20:846–852
Rizzoni D, Porteri E, Boari GE et al (2003) Prognostic significance of small-artery structure in hypertension. Circulation 108:2230–2235
Michelson G, Schmauss B, Langhans MJ et al (1996) Principle, validity, and reliability of scanning laser Doppler flowmetry. J Glaucoma 5:99–105
Kreis AJ, Nguyen T, Rogers S et al (2008) Reliability of different image analysis methods for scanning laser Doppler flowmetry. Curr Eye Res 33:493–499
Harazny JM, Raff U, Welzenbach J et al (2011) New software analyses increase the reliability of measurements of retinal arterioles morphology by scanning laser Doppler flowmentry in humans. J Hypertens 29:777–782
Ott C, Schlaich MP, Harazny J et al (2008) Effects of angiotensin II type 1-receptor blockade on retinal endothelial function. J Hypertens 26:516–522
Ritt M, Harazny JM, Ott C et al. (2012) Influence of blood flow on arteriolar wall-to-lumen ratio in the human retinal circulation in vivo. Microvasc Res, In Press
Ritt M, Harazny JM, Ott C et al (2011) Basal nitric oxide activity is an independent determinant of arteriolar structure in the human retinal circulation. J Hypertens 29:123–129
Heagerty AM, Aalkjaer C, Bund SJ et al (1993) Small artery structure in hypertension. Dual processes of remodeling and growth. Hypertension 21:391–397
Baumbach GL, Heistad DD (1989) Remodeling of cerebral arterioles in chronic hypertension. Hypertension 13:968–972
Wong TY, Klein R, Sharrett AR et al (2002) Cerebral white matter lesions, retinopathy, and incident clinical stroke. JAMA 288:67–74
Cooper LS, Wong TY, Klein R et al (2006) Retinal microvascular abnormalities and MRI-defined subclinical cerebral infarction: the atherosclerosis risk in communities study. Stroke 37:82–86
Wong TY, Klein R, Sharrett AR et al (2002) Retinal microvascular abnormalities and cognitive impairment in middle-aged persons: the atherosclerosis risk in communities study. Stroke 33:1487–1492
Baker ML, Marino Larsen EK, Kuller LH et al (2007) Retinal microvascular signs, cognitive function, and dementia in older persons: the cardiovascular health study. Stroke 38:2041–2047
Wong TY, Mosley TH Jr, Klein R et al (2003) Retinal microvascular changes and MRI signs of cerebral atrophy in healthy, middle-aged people. Neurology 61:806–811
Baleanu D, Ritt M, Harazny J et al (2009) Wall-to-lumen ratio of retinal arterioles and arteriole-to-venule ratio of retinal vessels in patients with cerebrovascular damage. Invest Ophthalmol Vis Sci 50:4351–4359
Breslin DJ, Gifford RW Jr, Fairbairn JF 2nd (1966) Essential hypertension a twenty-year follow-up study. Circulation 33:87–97
Tikellis G, Arnett DK, Skelton TN et al (2008) Retinal arteriolar narrowing and left ventricular hypertrophy in African Americans. The atherosclerosis risk in communities (ARIC) study. Am J Hypertens 21:352–359
Michelson EL, Morganroth J, Nichols CW et al (1979) Retinal arteriolar changes as an indicator of coronary artery disease. Arch Intern Med 139:1139–1141
Duncan BB, Wong TY, Tyroler HA et al (2002) Hypertensive retinopathy and incident coronary heart disease in high risk men. Br J Ophthalmol 86:1002–1006
Wong TY, Klein R, Sharrett AR et al (2002) Retinal arteriolar narrowing and risk of coronary heart disease in men and women. The atherosclerosis risk in communities study. JAMA 287:1153–1159
Gillum RF (1991) Retinal arteriolar findings and coronary heart disease. Am Heart J 122:262–263
Wong TY, Rosamond W, Chang PP et al (2005) Retinopathy and risk of congestive heart failure. JAMA 293:63–69
Wang L, Wong TY, Sharrett AR et al (2008) Relationship between retinal arteriolar narrowing and myocardial perfusion: multi-ethnic study of atherosclerosis. Hypertension 51:119–126
Wong TY, Coresh J, Klein R et al (2004) Retinal microvascular abnormalities and renal dysfunction: the atherosclerosis risk in communities study. J Am Soc Nephrol 15:2469–2476
Edwards MS, Wilson DB, Craven TE et al (2005) Associations between retinal microvascular abnormalities and declining renal function in the elderly population: the cardiovascular health study. Am J Kidney Dis 46:214–224
Ritt M, Harazny JM, Ott C et al (2009) Wall-to-lumen ratio of retinal arterioles is related with urinary albumin excretion and altered vascular reactivity to infusion of the nitric oxide synthase inhibitor N-monomethyl-l-arginine. J Hypertens 27:2201–2208
Liao D, Wong TY, Klein R et al (2004) Relationship between carotid artery stiffness and retinal arteriolar narrowing in healthy middle-aged persons. Stroke 35:837–842
Cheung N, Sharrett AR, Klein R et al (2007) Aortic distensibility and retinal arteriolar narrowing: the multi-ethnic study of atherosclerosis. Hypertension 50:617–622
Takiuchi S, Kamide K, Miwa Y et al (2004) Diagnostic value of carotid intima-media thickness and plaque score for predicting target organ damage in patients with essential hypertension. J Hum Hypertens 18:17–23
Frant R, Groen J (1950) Prognosis of vascular hypertension; a 9 year follow-up study of 418 cases. Arch Intern Med (Chic) 85:727–750
Breslin DJ, Gifford RW Jr, Fairbairn JF 2nd et al (1966) Prognostic importance of ophthalmoscopic findings in essential hypertension. JAMA 195:335–338
Breckenridge A, Dollery CT, Parry EH (1970) Prognosis of treated hypertension. Changes in life expectancy and causes of death between 1952 and 1967. Q J Med 39:411–429
Palmer RS, Loofbourow D, Doering CR (1948) Prognosis in essential hypertension: eight year follow-up study of 430 patients on conventional medical treatment. N Engl J Med 239:990
Shelbourne SA (1957) The retina in hypertensive diseases. Ann Intern Med 47:1154–1164
Svardsudd K, Wedel H, Aurell E et al (1978) Hypertensive eye ground changes. Prevalences, relation to blood pressure and prognostic significance. The study of men born in 1913. Acta Med Scand 204:159–167
Schouten EG, Vandenbroucke JP, Van der Heide-Wessel C et al (1986) Retinopathy as an indicator of all-causes mortality. Int J Epidemiol 15:234–236
Witt N, Wong TY, Hughes AD et al (2006) Abnormalities of retinal microvascular structure and risk of mortality from ischemic heart disease and stroke. Hypertension 47:975–981
Wong TY, Knudtson MD, Klein R et al (2004) A prospective cohort study of retinal arteriolar narrowing and mortality. Am J Epidemiol 159:819–825
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag Italia
About this chapter
Cite this chapter
Ritt, M., Schmieder, R.E. (2012). The Optic Fundus and Retinal Circulation: New Technology for an Old Examination. In: Berbari, A., Mancia, G. (eds) Special Issues in Hypertension. Springer, Milano. https://doi.org/10.1007/978-88-470-2601-8_13
Download citation
DOI: https://doi.org/10.1007/978-88-470-2601-8_13
Published:
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-2600-1
Online ISBN: 978-88-470-2601-8
eBook Packages: MedicineMedicine (R0)