Abstract
18F-2-deoxy-d-glucose (FDG) has been the primary tracer for positron emission tomography (PET) in urologic malignancy. The primary clinical application of PET–CT in urology relates to the management of the urologic malignancies, including renal cancer, bladder cancer, prostate cancer, and testicular cancer.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
18F-2-deoxy-d-glucose (FDG) has been the primary tracer for positron emission tomography (PET) in urologic malignancy. The primary clinical application of PET–CT in urology relates to the management of the urologic malignancies, including renal cancer, bladder cancer, prostate cancer, and testicular cancer.
Renal Malignancy
Renal cell carcinoma constitutes 3 % of adult malignancies. The worldwide incidence is increasing at an annual rate of 2 %. Renal malignancies include renal cell carcinoma (RCC), transitional cell carcinoma, squamous cell carcinoma (SCC), lymphoma, and metastatic neoplasm, usually lung cancer or melanoma.
Renal cell carcinoma, the most common malignant neoplasm of the kidney, is primarily a surgically managed disease. In advanced disease, medical management offers little in terms of improved survival or palliation. Surgical extirpation is the mainstay of treatment if there is no diagnostic imaging evidence of local spread beyond Gerota’s fascia and distant metastasis. Metastases are present in about 50 % of patients at the time of presentation. Solitary metastasis may also be resected. RCC responds poorly to chemotherapy. Radiation therapy for RCC is used for palliation of metastatic sites, specifically the bone and brain. Immunotherapy with biologic response modifiers such as interleukin-2 and interferon alpha has the most impact on the treatment of metastatic disease. The 5-year survival is around 80–90 % for early stages of disease, while advanced disease carries a poor prognosis. Prognosis depends mainly on stage of the tumor at the time of presentation (Fig. 14.1)
Diagnostic imaging evaluation of a renal mass was performed as part of evaluation of hematuria, flank pain, or a palpable mass; however, incidental detection of malignant renal masses is also on surge due to widespread use of cross-sectional imaging. Characterization of renal masses from benign cysts, complex cysts, which can be malignant, and solid masses can be easily done on CECT.
Bosniak has classified the renal cysts based on morphological features on CECT. Bosniak category I are simple cysts, which do not require further evaluation. Category II complex cysts are usually followed up with anatomical imaging. Surgical removal and exploration are required in category III and IV cystic masses. Hence, PET–CT could potentially aid in the noninvasive evaluation and whole-body staging of Bosniak category III and IV renal masses.
PET–CT is mainly used for staging, response assessment, and surveillance in cases that have been operated. However, variants like clear cell carcinoma (CCC) are non-FDG avid. Other reasons for false negatives are small body size and interference from urinary activity as kidneys are the normal route of excretion. In oncocytomas, it is seen that FDG uptake is almost same as renal cell carcinoma. In one study with 11 Bosniak category III renal masses, 10 of 11 were benign, and the one containing RCC was false negative on FDG-PET. In another series of histopathologically proven 68 renal masses, it was found that the average standardized uptake value (SUV) for RCC to be 4.6, thus only slightly higher than adjacent nonmalignant renal parenchyma between 1 and 2 h after tracer injection.
In another series with 35 patients, it has been reported a sensitivity of 47 % and specificity of 80 % for FDG-PET characterization of renal masses. Hence, there may be inherent limitations in using the tracer FDG for evaluation of RCC in general, and renal masses in particular, because of the relatively modest FDG avidity of a significant fraction of malignant renal tumors. In the detection of locoregional and distant metastases, FDG-PET sensitivity and specificity have been estimated to be 63–77 % and 75–100 %, respectively. Positive predictive value appears to be high, in excess of 90 %, whereas generally, the negative predictive value is low to be clinically useful (e.g., a negative study does not exclude malignancy).
FDG PET–CT is superior to bone scan in evaluating osseous metastases as compared to bone scintigraphy. These observations are correlated with the heterogeneous expression of GLUT-1 in RCC, which may not correlate with the tumor grade or extent. FDG-PET can also alter clinical management in up to 40 % of patients with suspicious locally recurrent and metastatic renal cancer.
The normal route of excretion for FDG is urinary tract, so to avoid false negatives and false positives, newer tracers are being investigated, like amino acid analogs.
C-11-labeled acetate is one such tracer, which is retained by RCC but rapidly cleared from the renal parenchyma as carbon dioxide, and with no urinary excretion. Higher average SUV and tumor to renal cortex values are obtained within 10 min of tracer injection compared to FDG at 1 h postinjection, and the highest acetate tracer accumulation was found in granulocytic tumors. Although such tracers of amino acid transport or lipid-related metabolism may have a role in characterizing a small renal mass or response to therapy, detecting RCC in complex renal masses and metastatic disease requires high consistent tracer uptake. However, such consistency has not yet been demonstrated with this tracer.
The diagnostic accuracy of FDG-PET appears not to be improved by semiquantitative analysis, which is probably due to the fundamental variability of glucose metabolism in RCC. And delayed images 03 h postinjection with diuretic intervention helps us to delineate the tumor in a better way.
Thus, PET–CT has a role in staging (not in all histological types), response assessment, restaging, and surveillance in cases of renal cell carcinoma.
Bladder Cancer
Bladder cancer is the most common malignant tumor of the urinary tract and more common in patients aged 50–80. The incidence doubles in men >75 years of age versus younger men. It is more common in males as compared to females and presents usually as painless hematuria. The various risk factors being occupational exposure like in case of aniline dye workers, smoking, pelvic irradiation, and drugs like cyclophosphamide. Depth of tumor penetration into the bladder wall forms the basis for disease staging and is the most important prognostic factor.
Transitional cell carcinoma is the most common histopathology, up to 90 % of cases; 8 % are squamous cell and other varieties being adenocarcinomas, sarcomas, lymphomas, and carcinoid tumor types. Diagnostic procedures may include cystoscopy with biopsy, excretory urography, or retrograde pyelogram; pelvis ultrasound; and CT of the chest, abdomen, and pelvis. Superficial lesions may be treated with endoscopic resection, fulguration, or photodynamic therapy. For invasive tumors, cystectomy with urinary diversion is usually done. Radiotherapy may be employed as adjuvant therapy, in combination with other therapies, or as a palliative measure. There is no established systemic chemotherapeutic regimen for the treatment of metastatic bladder carcinoma. The 5-year survival is about 90 % for superficial disease and about 60 % for invasive disease. Systemic disease has a bad prognosis.
FDG-PET has been found to be modestly accurate in the diagnosis of bladder cancer, as urinary bladder is a route of excretion for FDG, and in the detection of pelvic lymph node and distant metastases (Fig. 14.2).
However, dual time point imaging where images are taken after 1 and 3 h postinjection, post-diuretic administration, produces optimal images. Primary bladder carcinoma and the lymph node metastases may exhibit an SUV in the range 1.7–6.2. For lymph node staging, a sensitivity of 67 % and a specificity of 86 % have been reported. Other PET radiotracers including C-11 methionine and C-11 choline may also be potentially useful in the imaging evaluation of bladder carcinoma.
Locoregional nodal staging is an important prognostic marker for proper management of bladder cancer patients. The size criteria of nodal involvement used with anatomic imaging is of limited accuracy. Hence, PET with FDG or other tumor-specific tracers could provide increased accuracy in N stage of bladder cancer, as has been demonstrated with several other malignancies. Distant metastatic disease, most commonly osseous, pulmonary, and hepatic metastases, is important in patients with invasive bladder cancer. PET offers improvement in detection of osseous or hepatic metastases analogous to that observed in other malignancies such as lung or esophageal cancer.
Limited pilot studies have demonstrated that metastatic bladder cancer is FDG avid and that involved local lymph nodes as small as 9 mm could be detected, whereas smaller involved nodes (less than 5 mm) were false negative.
A recent study has reported a sensitivity of 67 % and a specificity of 86 % for FDG-PET detection of pelvic lymph node metastases of bladder cancer. Osseous metastases of bladder cancer are readily detected on FDG-PET, but the relative accuracy of FDG-PET versus conventional bone scintigraphy has yet to be fully addressed. Bladder cancer appears to have relatively consistent avidity for FDG, and adding FDG-PET to conventional anatomic evaluation of locoregional and distant spread of bladder cancer such as with PET–CT may well prove clinically valuable.
As elsewhere in the urinary tract, alternative tracers that do not undergo urinary excretion, or can be imaged before the arrival of the excreted urinary tracer activity, have been investigated in an attempt to obviate the confounding effects of urinary tract excretion. 11C-L methionine was used in a limited series to investigate the PET detection of primary bladder cancer. T4, most T3, and 2 of 4 of T2 primary bladder cancers were detected.
The T staging was not superior to anatomic imaging, and there were insufficient proven cases of nodal metastases to evaluate accuracy of local lymph node metastases. A preliminary study reported detection of 10 of 18 primary bladder cancers with 11C-choline PET. In two patients, pelvic lymph node metastases were visualized; however, again there were insufficient proven cases of nodal metastases in the series to evaluate the accuracy for local lymph node metastases. In addition to locoregional lymph node staging, differentiating post-radiation therapy scar from recurrent tumor in patients treated for locally advanced disease and assessment of neoadjuvant therapy response are areas warranting further investigation of PET with FDG and other tracers.
Prostate Cancer
As life expectancy increases, so will the incidence of this disease, creating what will become an epidemic male health problem. The commonest histology is adenocarcinoma. Digital rectal examination is considered the standard of reference for detection of prostate cancer. About 50 % of all palpable nodules are carcinomas. Neither prostatic acid phosphatase (PAP) nor prostate-specific antigen (PSA) is useful for screening prostate cancer, although elevated serum levels of these substances are usually suggestive of locally advanced or metastatic disease. The commonly used histopathological Gleason score, which ranges from a minimum of 2 to a maximum of 10, is based on both the tumor’s glandular differentiation and its growth pattern and has been shown to be associated with the clinical stage of disease. The role of diagnostic imaging in the management of prostate cancer is both as rapidly evolving and as controversial as the clinical management of the disease. Although two decades ago staging before prostatectomy with bone scintigraphy was common, today the management of prostate cancer is varied, with far less reliance on surgery and the routine use of serum markers (prostate-specific antigen) to assess disease progression and response to therapy. Because the prostate itself is easily accessed via the rectal vault, very high-resolution anatomic imaging by ultrasound or MRI is possible. Biopsy of all sectors of the prostate gland, either randomly or assisted by ultrasound guidance, is routine, and hence tumor histological grade is readily obtained at initial diagnosis.
The potential roles for diagnostic imaging of prostate cancer include diagnosis of primary disease, determination of extracapsular spread, and detection of locoregional lymph node metastases and distant metastatic spread. Bone scintigraphy with SPECT/CT is very useful in detecting osseous metastases. However, bone scintigraphy cannot detect soft tissue or lymph nodal involvement, quite prevalent with metastatic spread of this disease.
Preliminary studies show that accumulation of FDG in prostate cancer is low, and also the uptake may overlap with the uptake in benign prostatic hyperplasia (BPH), in the normal gland, and in the operative site or local recurrence. However, animal and preliminary clinical studies have demonstrated that FDG-PET may be useful in the evaluation of advanced androgen-independent disease and in patients with high Gleason scores and serum PSA level, in the detection of active osseous and soft tissue metastases, and in the assessment of response after androgen ablation and treatment with novel chemotherapies. For metastatic disease, FDG localization in the lesions may display a standardized uptake value (SUV) of up to 5.7 at a positive predictive value of 98 %.
FDG-PET may be more useful than In-111 ProstaScint in the detection of metastatic disease in patients with high PSA or PSA velocity. FDG-PET appears to be more useful in the detection of soft tissue metastases than osseous metastases and also differentiates between active osseous diseases from the scintigraphically quiescent lesions. It also helps in restaging patients who have a rising PSA level despite treatment. Additionally, it has been suggested that FDG-PET has a better specificity but lower sensitivity for detecting osseous metastases in comparison to bone scintigraphy and is useful in differential diagnosis of flare reaction after endocrine therapy. FDG-PET has also shown a role in prognosticating patients undergoing radical prostatectomy. Lesions demonstrating higher FDG accumulation (i.e., high SUV) had poorer prognosis in comparison to those with low SUV.
In a series of 24 patients with organ-confined prostate cancer in which urinary tracer activity in the bladder was minimized, only 1 (4 % sensitivity) was detected. Tumor volume ranged from 1.2 to 10.4 ml with a mean of 6.9 ml. The failure of detection most likely reflects the low tumor to background achieved with FDG. Similar disappointing results were reported for the detection of local recurrence of prostate cancer in patients treated by prostatectomy, also attributed to the relatively low avidity of prostate cancer for FDG.
Novel PET radiotracers for imaging of prostate cancer are also in vogue. Acetate participates in cytoplasmic lipid synthesis, which is believed to be increased in tumors. Cellular retention of radiolabeled acetate in prostate cancer cell lines is primarily due to incorporation of the radiocarbon into phosphatidylcholine and neutral lipids of the cells. The lack of accumulation of acetate in urine is also advantageous to imaging prostate cancer in particular, because the prostate bed remains unobstructed by the adjacent high levels of radioactivity in the urinary bladder, commonly a problem with FDG. Although there can be a considerable overlap between the uptake level in primary cancer and in the normal prostate gland, generally, the uptake appears to be greater in the tumor than in the normal tissue. C-11 acetate may also be useful in detection of tumor recurrence in patients who had been treated previously with prostatectomy or radiation therapy.
Choline PET may also be useful in imaging prostate cancer. The biological basis for radiolabeled choline uptake in tumors is the malignancy-induced upregulation of choline kinase, which leads to the incorporation and trapping of choline in the form of phosphatidylcholine (lecithin) in the tumor cell membrane in proportion to the rate of tumor duplication. The tracer uptake has been noted to decrease in both the primary tumor and in the metastases after hormonal therapy and increase after relapse as measured by the increase in the serum PSA level. both acetate and choline appear to be more or less equally useful in imaging prostate cancer in individual patients and are more advantageous than FDG. in some clinical circumstances, such as detection of the locally recurrent disease, the diagnostic potential of other tracers such as radiolabeled androgen analog F-18 fluoro-5a-dihydrotestosterone (FDHT) for imaging androgen receptors may be necessary. However, this is yet to be clinically established.
In addition, emerging roles include guidance of local therapy in patients with organ-confined disease and assessment of tumor response to systemic therapy in patients with advanced metastatic disease.
In prospective series of 67 patients, C-choline PET was 80 % sensitive and 96 % specific in the staging of pelvic lymph node metastases. 18 F-labeled choline derivatives have subsequently been synthesized and tested, including 18 F-fluoromethyl choline and 18 F-fluoroethyl choline. Fluoromethyl choline most closely matches the in vivo phosphorylation rate of choline and appears to be the preferred 18 F-labeled choline analog for PET imaging. Both soft tissue and bone metastases are readily identified with fluorocholine, with SUVs ranging from 2.5 to as high as 10, but on average roughly 4.5 in untreated prostate cancer. In addition to high liver, pancreas, and bowel activity, fluorocholine undergoes urinary excretion. The rapid tumor uptake and blood pool clearance, however, does permit early imaging of the prostate and adjacent tissues before arrival of urinary tracer in the bladder. In comparison to FDG-PET, 18 F-fluorocholine PET was generally better in detection of primary lesions and osseous and soft tissue metastases on initial clinical evaluation.
As with acetate and choline PET tracers, amino acid tracers have been investigated both as a probe of an alternate metabolic pathway and as a strategy to avoid the confounding effects of urinary tracer in the bladder. In patients with progressive metastatic prostate cancer, l-methionine uptake in metastatic lesions was consistently higher than FDG uptake and demonstrated progressing metastatic lesions more consistently than did FDG on PET imaging. Some success was also reported in using 11C-l-methionine PET to direct biopsy in patients with rising serum prostate-specific antigen and negative routine biopsies.
Thus PET–CT could be valuable in the management of advanced prostate cancer.
Role of PET–CT in Testicular and Gynecological Malignancies
Testicular Cancer
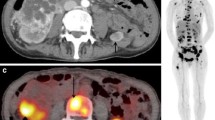
Role of imaging is vital in testicular and gynecologic malignancies as they are important cancers with significant morbidity. The incidence of testicular malignancy is increasing and is a cancer of relatively young men. Ovarian, uterine, and cervical cancer are among the most common tumors in women, with high morbidity and mortality rates. Despite early screening tests for cervical cancer, mortality from this tumor remains significant. Outcome in terms of long-term survival is based on staging. Imaging techniques have been fundamental in this process, and positron emission tomography (PET) is developing to be an important tool in pretreatment assessment, assessing early response to therapy, restaging, and in cases of tumor recurrence (Fig. 14.3).
A 33-year-old man with a history of testicular cancer treated 18 months back, now presented with rising tumor markers. There was no evidence of disease on conventional imaging. PET–CT imaging revealed FDG-avid lymph node lying close to the L2 vertebra, as shown on the transaxial image of CT (a), PET image (b), and PET–CT fusion image (c) (see arrows)
Testicular cancer (seminoma and non-seminoma, NSGCT) is a relatively rare tumor affecting only 1 % of men, but it is the commonest tumor in young males (aged 15–35), and its incidence is increasing. Biological behavior and potential for metastasis for the two tumors are different; however, the overall prognosis is good (Fig. 14.4).
A patient with known metastatic testicular cancer had an FDG-PET scan performed before chemotherapy (b). The transaxial images of CT (a), PET showed an FDG-avid nodal lesion (arrow). One week later following chemotherapy, there has been a rapid decrease in uptake in the tumor (c) (see arrow), indicating an early response to chemotherapy. The patient responded well to the current course of chemotherapy
Because of advances in chemotherapy, cure is now possible for the majority of patients with minimal metastatic disease. If tumor spread could be reliably assessed, some patients with NSGCT stage I (no evidence of metastases) could be clinically observed rather than undergo prophylactic chemotherapy.
Testicular cancers usually present as an asymptomatic lump and urgent orchidectomy is warranted. Usual histological diagnosis being seminoma and non-seminomatous germ cell tumor (NSGCT), 10 % can have mixed tumors as well. The tumors spread to the para-aortic region initially, although hematogenous spread is more common in NSGCT and metastases are seen in the lung, brain, liver, and bone also. At the time of diagnosis, all patients are staged by clinical examination and computed tomography (CT) scans of the chest and abdomen and pelvis. Tumor markers are measured for prognosticating and allowing monitoring of treatment response and assessment of recurrence.
In seminoma, conventional practice has been to perform retroperitoneal radiotherapy even in stage I disease, and about 15 % of patients at presentation have disease confined to the abdomen. Retroperitoneal and pelvic radiotherapy is a common practice and has a good rate of achieving local control. So, if there is nodal involvement, PET–CT can act as a guide for radiotherapy planning.
Anatomic staging techniques including CT, ultrasound, and lymphangiography have all been used to stage testicular cancer. The most widely used now is CT, which is routinely performed as part of the initial staging protocol. All staging procedures have limitations, and even for CT, false-negative rates of 59 % have been reported. The false-negative rates for lymphangiography and ultrasound are 64 and 70 %, respectively. The diagnosis of nodal metastases by CT is based on detection of nodal enlargement, with a 1-cm upper limit for normal lymph node size. Before nodal enlargement, the entire volume of lymph node may be replaced by malignant cells, whereas a large lymph node may contain only benign reactive cells. As a result, the false-positive rate of CT is also high at 40 %. This inaccuracy has led to search for more accurate imaging methods, including metabolic imaging with PET.
As 18 F-2-deoxy-d-glucose (FDG)-PET relies on metabolic uptake criteria rather than size criteria. It has the potential to identify small-volume disease in a lymph node that is normal in size; this may have a direct effect on patient management. Unnecessary treatment and morbidity is avoided in stage I tumors by more accurate classification of patients at high or low risk. Treatment plan is also changed in stage III and IV tumors if there is distant metastasis.
FDG-PET can clearly identify more sites of disease in patients with established metastatic disease than seen on CT.
There are only a few studies that have addressed the issue of improving the initial staging using PET. The sensitivity ranged between 70 and 87 % and the specificity between 94 and 100 %. The three major initial studies confirmed overall better sensitivity, positive predictive value (PPV), and negative predictive value (NPV) for PET than for CT. Both CT and PET missed small (approximately 1 cm) retroperitoneal lymph node metastases. However, one limitation of these studies was that not all patients had histological confirmation of findings on PET and assessment of true negativity or positivity.
FDG-PET potentially has the ability to detect small-volume tumors in solitary residual masses, to identify a specific mass as the site of relapse in patients with multiple masses, to detect other unsuspected sites of tumor, and to determine the site and extent of disease in patients with raised tumor markers.
In a recent study including 51 patients with seminomas and post chemotherapy residual masses, PET detected residual tumor in all masses greater than 3 cm and in 95 % of masses less than 3 cm, with PPVs and NPVs of 100 and 96 %, respectively, for PET versus 37 and 92 %, respectively, for CT. These findings showed that PET was a reliable predictor of residual tumor. Two problems emerged in the studies of residual masses. First, FDG-PET can miss some small-volume active disease. Overall, the numbers of false-negative PET studies were small, and the NPV was high.
Another useful role of PET–CT is in a scenario where there are rising tumor markers, and this may be the first indicator of disease recurrence. However, they are neither sensitive nor specific for tumor detection, and marker-negative relapse may occur even where the initial tumor was marker positive. Also, some patients with residual masses posttreatment may show modest elevation of markers even though the masses contain no active tumor, and a return of markers to normal, posttreatment, does not guarantee disease remission. Thus, PET–CT can help in lesion localization in such cases. In a recent study of 70 patients with known markers who underwent PET imaging, it was found that patients with raised tumor markers, including those with a residual mass, PET identified the site of disease in all patients but 1. In the group with raised tumor markers and no residual masses, PET demonstrated the tumor in all patients. In the group with raised tumor markers and residual masses, there was one false positive. Negative PET scans in the presence of raised tumor markers presented more of a problem as there were five patients with false-negative findings in this group. In three of these cases, all imaging was normal, and subsequent PET scans were the first studies to identify the site of recurrence. This finding suggests that, in the presence of raised tumor markers and negative imaging findings, the most appropriate follow-up procedure is repeating the PET study. These findings have important implications for the management of patients. It has been found that the ability of PET to find unsuspected disease resulted in management changes in 57 % of patients. Management changes involved changes from local therapy like radiotherapy/surgery to chemotherapy or surveillance. Many of their patients had multiple recurrences and had chemotherapy-resistant tumor, and in such cases local control of active sites may be the only chance of cure. In the first relapse, determination of whether there are one or multiple sites will help to determine the type of consolidation treatment.
PET–CT also plays a role in assessing response to treatment. A recent study evaluated the value of FDG-PET imaging compared to tumor markers and CT/MR in 23 patients with relapsed testicular cancer after two or three cycles of induction chemotherapy before high-dose chemotherapy. The outcome of high-dose chemotherapy was correctly predicted by PET–CT scan/serum tumor marker in 91, 59, and 48 % of patients, respectively. In those patients who showed response to induction chemotherapy according to CT scans or serum tumor marker evaluation, a positive PET study correctly predicted treatment failure. In addition, PET identified patients most likely to achieve favorable response to subsequent high-dose chemotherapy. It was suggested that FDG-PET is a valuable addition to the prognostic model of low-, intermediate-, and high-risk patients, particularly in the low and intermediate groups, for further selection of patients who would benefit from high-dose chemotherapy.
Cervical Cancer
Cervical carcinoma is a leading cause of death in females in India. The advent of routine Papanicolaou (Pap) smears has led to a substantial reduction in the incidence and greater than 70 % decrease in mortality of cervical cancer over the last 50 years. About 80 % are squamous cell carcinomas and about 20 % adenocarcinomas, in addition to other rare types of tumors. Uncommon subtypes are adenosquamous carcinoma, lymphoma, adenoma malignum, and small cell carcinoma, the latter tending to be locally invasive as well to have distant metastases. The International Federation of Gynecology and Obstetrics (FIGO) has defined a staging system for carcinoma of the cervix that uses a combination of clinical and radiologic findings. Although prognosis is related to stage, other factors are equally important in determining prognosis, including the extent of lymph node involvement. Only limited data is available on the use of imaging modalities, including FDG PET–CT in the primary detection of these malignancies.
FIGO staging of cervical cancer is done in accordance with the FIGO clinical criteria, which allows information obtained from physical examination, lesional biopsy, endocervical curettage, hysteroscopy, cystoscopy, proctoscopy, barium enema, intravenous pyelogram (IVP), and radiographs of the chest and skeleton, to be used for staging purposes. This criterion allows uniform staging evaluation of patients with cervical cancer. Cervical cancer spreads in a predictable pattern from the primary tumor to pelvic, para-aortic, supraclavicular lymph nodes, and then to non-nodal distant sites. Extrapelvic disease without pelvic lymph nodal involvement is rare. Lymphangiography and surgical staging have become obsolete, although surgical staging is still advocated as the gold standard to assess pelvic and para-aortic lymph node metastasis. The best methods for defining the status of lymph nodes are CT and MRI scanning. The less-invasive nature of CT/MR as well as the extra anatomic information provided on tumor extent has made the imaging procedures preferable; however, as far as lymph nodal assessment is concerned, CT and MRI have lower sensitivity and specificity as it depends on size-based criteria in comparison to functional imaging.
These problems with conventional imaging have led to evaluation of FDG-PET as an alternative for the staging of cervical carcinoma and for the evaluation of lymph nodes in particular. MR imaging had accuracies for detecting parametrial, pelvic sidewall, bladder, and rectal involvement of 88, 95, 96, and 100 %, respectively. The overall staging accuracy was 88 %.
FDG-PET has a superior ability to detect regional and distant metastatic disease in patients with cervical cancer as compared with CT and MR imaging, which has made FDG PET–CT a useful investigation. A recent study evaluated the usefulness of tumor volume measurement with PET in patients with advanced cervical cancer treated by radiation therapy. Conclusion made from this study was that tumor volume can be accurately measured by PET; the tumor volume separates patients with a good prognosis from those with a poorer prognosis; a subset of patients with relatively small tumors and no lymph node involvement does remarkably well; and tumor volume does not correlate with the presence of lymph node disease.
The same group of investigators has evaluated a treatment planning method for dose escalation to the para-aortic lymph nodes based on PET with intensity modulated radiotherapy (IMRT) for cervical cancer patients with para-aortic lymph node involvement. They subsequently determined the guidelines regarding the selection of appropriate treatment parameters. A group of researchers developed a simple, rapid, and highly reproducible system for visual grading of characteristics of the primary tumor in patients with cervical cancer at the time of diagnosis. Another group evaluated the outcome of patients with FIGO clinical stage IIIb cervical carcinoma as a function of site of initial regional lymph node metastasis as detected by FDG-PET. They concluded that the cause-specific survival in this group was highly dependent on the extent of lymph node metastasis as identified on FDG-PET. FDG-PET imaging helps in predicting response in patients with cervical carcinoma pre- and post radiotherapy. A recent study evaluated 152 patients with cervical cancer who underwent radiotherapy and/or chemotherapy with pre- and posttreatment FDG-PET imaging. The 5-year survival of patients with positive FDG-PET scans (at previous or new sites) was of 32 % and with negative FDG-PET post-therapy scan was 80 %. They concluded that persistent or new FDG uptake on the post-therapy scan was the most significant prognostic factor for developing metastatic disease and for predicting death from cervical cancer. The main cause of false positives in FDG PET–CT is interference of activity from urinary bladder, which might cause difficulty in image interpretation or artifacts. Imaging patients pre- and post-void without furosemide intervention was found, however, to have 100 % sensitivity for tumor detection on post-void images.
As with other tumors, timing of the acquisition of the PET images post-administration of FDG may be important, and dual time point intervention is usually done and well documented in studies.
Several non-FDG tracers have been tried like imaging using both 11C-choline and 11C-methionine and evaluated in carcinoma of the cervix. Absence of significant renal excretion with subsequent little or no radioactivity in the urinary bladder makes this tracer more suitable than FDG for evaluation of gynecologic malignancies.
Despite significant advances, cervical cancer continues to be a major worldwide public health concern. Although no randomized trials have directly compared FDG imaging to surgical staging, there is substantial evidence supporting its clinical utility in the management of patients with cervical cancer. The robust data has led the Center for Medicare and Medicaid Services to make it a covered oncologic indication.
Uterine Cancer
Endometrial carcinoma is the most common gynecologic malignancy, with approximately 40,000 new cases diagnosed in the United States each year. The two main subtypes of endometrial cancer are endometrioid (type I) and non-endometrioid (type II) tumors. 80–90 % of patients are associated with endometrioid histology. Patients are usually perimenopausal and have risk factors associated with increased estrogen exposure such as nulliparity, chronic anovulation, and obesity. The tumors are confined, as a rule, to the uterus and have a good prognosis. On the other hand, non-endometrioid subtypes are seen in older multiparous women, usually without increased estrogen exposure. The most common forms are uterine papillary serous carcinoma and clear cell carcinoma. In view of high propensity for myometrial and vascular invasion as well as peritoneal carcinomatosis, these types of cancers carry a poorer prognosis than endometrioid carcinoma. Painless bleeding is the most frequent presenting symptom of endometrial cancer. Effective steps for the evaluation of patients’ postmenopausal bleeding (PMB) are transvaginal sonography (TVS), endometrial biopsy (EMB), and hysteroscopy. After the detection of malignancy, tumor bulk as well as local and distant spread can be assessed with this imaging modality before surgical staging (Fig. 14.5).
A 61-year-old woman with stage IV endometrial cancer had completed chemotherapy and radiotherapy and being considered for surgery. PET–CT was performed to exclude metastasis. There was evidence of disease outside the uterus. The transaxial CT images (a), PET image (b), as well as fusion image (c) showed persistent FDG uptake in the primary endometrial site indicating residual tumor (see arrows)
Routine surveillance imaging has not proved to be effective, and likely will not be until a curative treatment for this recurrent metastatic disease is found. Seven percent patients show vaginal recurrence, which presents as vaginal bleeding. So, clinical examination and MRI/CT are the important tools in this scenario.
FDG imaging has been shown to play an important role in the decision-making process for women with known recurrent endometrial cancer. For women with an isolated site of recurrence, surgery and/or radiotherapy may be either curative or provide effective palliation, but with multifocal recurrent disease, only palliative chemotherapy is indicated. A well-documented study on PET versus CT performance in 90 women with recurrent endometrial or cervical cancer found that PET improved the sensitivity and specificity for assessing the extent of disease when compared with CT. These investigators also noted that in 42 % of patients, PET results led to a change of management.
Studies using 18 F-17b-estradiol (FES) and FDG-PET showed that FES-PET are more useful in monitoring hormone therapy, especially in endometrial hyperplasia than FDG-PET. This differential monitoring of PET signals certainly could provide valuable insights into the management of recurrent disease or fertility-sparing interventions where hormone receptor status could inform the decision to treat a woman with progestin or antiestrogen therapy rather than chemotherapy. These treatment decision strategies, however, are only theoretical and have not yet been investigated. Endometrial cancer is a common malignancy that usually has a good prognosis. Given the favorable outcomes generally seen, there is no apparent benefit to extensive surgical or radiologic staging of these women. The utility of FDG PET–CT is confined to clarifying the extent and location of recurrent disease, thus assisting in the individualization of salvage therapy decisions.
Ovarian Cancer
About two-thirds of patients present with advanced FIGO Stage III or IV disease; ovarian cancer accounts for a greater number of deaths than all other gynecologic malignancies. Epithelial tumors account for approximately 90 % of ovarian cancers and can have serous, mucinous, endometrioid, clear cell, and undifferentiated histologies. Serous carcinoma represents approximately 80 % of all ovarian cancers and is histologically graded as low or high grade. Low-grade serous carcinomas arise from borderline tumors, whereas high-grade tumors do not have a definite precursor lesion, are more frequent, and have a poorer prognosis. Borderline tumors lack stromal invasion and occur at a younger age group than invasive cancer. Primary ovarian mucinous carcinoma is uncommon and is diagnosed after excluding metastatic disease to the ovary (Fig. 14.6).
A 40-year-old woman was diagnosed with ovarian cancer and was treated with radical surgery. On follow-up, she was found to have rising tumor marker (CA-125). MRI was stable without evidence of recurrence. The transaxial images of CT, (a) PET (b), and PET–CT fusion image (c) showed FDG-avid lesion in the pelvis that were proven to be recurrent disease (see arrows)
Imaging is used to characterize an adnexal mass and assess for metastatic disease following the diagnosis of malignancy. USG is the first-line approach for lesion characterization, with MR imaging as a problem-solving tool. CT or MR imaging can be used to stage patients for metastatic disease. Adnexal lesions are common findings on imaging procedures, and the key is to distinguish benign from potentially malignant lesions.
There are several possible diagnostic tasks for FDG-PET imaging in ovarian cancer, including noninvasive characterization of an ovarian mass as malignant or benign early diagnosis and defining the extent of localized ovarian cancer; staging and initial treatment planning (which often includes debulking surgery) after the diagnosis; predicting whether response will occur and determining whether the disease is responding to treatment; and determining whether there is residual tumor (restaging) or recurrence after the treatment. There are critical diagnostic points because the treatments for ovarian cancer can be aggressive and difficult for patients to tolerate. FDG-PET has been evaluated, to some extent, in each of these settings, but the role of PET in detecting recurrent disease and in monitoring response to tumors is the major area of focus. Multimodality screening using serum CA-125 and pelvic USG or TVS is used. Ovarian cancer primarily recurs in the peritoneal cavity and retroperitoneal lymph nodes. Patients are monitored for recurrence with periodic physical examinations, serum CA-125 level measurements, and USG examinations. Additional imaging (CT, MR, and FDG-PET or PET–CT) is commonly performed when there are signs or symptoms suggestive of recurrence.
However, both morphologic (CT and MR imaging) and metabolic FDG-PET imaging are limited in their ability to detect small-volume (<5–10 mm) disease. Rising CA-125 levels may precede the clinical detection of recurrence in 56–94 % of cases, with a median lead time of 3–5 months. Recent data suggest FDG-PET to be more sensitive than CA-125 levels, in some instances.
There is increased use of PET–CT for evaluating response to neoadjuvant, adjuvant, or standard chemotherapy or radiotherapy, but the literature is just evolving and studies are small. In a prospective study of 33 patients with advanced-stage ovarian cancer (FIGO stage IIIC and IV), receiving neoadjuvant chemotherapy before cytoreductive surgery, FDG-PET of the abdomen and pelvis was obtained before treatment and after the first and third cycles of chemotherapy. A significant correlation was observed between FDG-PET metabolic response after the first (threshold of 20 % decline in standardized uptake value [SUV]) and third cycle of chemotherapy (threshold of 55 % decline in SUV) and overall survival. The investigators concluded that FDG-PET seems to be a promising tool for early prediction of response to chemotherapy.
PET–CT is the established hybrid imaging method for ovarian carcinoma, but combinations of PET and MR imaging are being explored and this technology is evolving rapidly. The combination of PET and MR imaging using software fusion techniques has been examined in 31 patients with ovarian cancer. The investigators concluded that anatomic localization was superior for PET–MR imaging fusion than for PET–CT. However, diagnostic accuracy was not formally evaluated. Nonetheless, although PET–MR imaging could play a growing role in ovarian cancer imaging in the future, it is still in its infancy.
Uterine Sarcomas
Uterine sarcomas are mainly classified into three subtypes: leiomyosarcoma, carcinosarcoma, and endometrial stromal sarcoma. They constitute less than 8 % of uterine carcinomas. In a small study of five patients, it has been reported that FDG-PET detected leiomyosarcoma with an accuracy of 100 % compared with an accuracy of 80 % for MR imaging. However, FDG-PET was unable to detect metastases in subcentimeter lymph nodes. Because of their aggressive tumor biology, leiomyosarcoma typically recurs within 2 years of initial treatment. FDG PET–CT has a better detection rate as compared to CT for extrapelvic recurrences.
Vaginal Cancer
It constitutes less than 3 % of gynecological malignancy. It is usually diagnosed by Pap smear and staged according to FIGO classification system. Squamous cell carcinomas constitute 80 % of the histological variants. The usual presentation is bleeding. Tumor usually spreads by local invasion, lymphatic dissemination to inguinal and pelvic lymph nodes, and hematogenous spread to the lungs. Depending upon the anatomical involvement, like in cases where upper third of the vagina is involved, drainage is into the pelvic lymph nodes, internal and external iliac chain, and obturator nodes, whereas tumors of the lower third drain into deep pelvic lymph nodes, femoral, and inguinal nodes. A comparison of CT and FDG-PET in 23 patients with stages II and IV vaginal carcinoma found that FDG-PET identified all metabolically active primary tumors with a sensitivity of 100 % and detected metastatic lymph nodes in 35 % of patients in comparison to 17 % by CT. Lymph node involvement usually indicates poor prognosis.
Vulvar Carcinoma
It accounts for less than 4 % of the malignancies. Usual age of presentation is 70 years, and the most common histology is Squamous cell carcinoma. The lymphatic drainage is usually to the inguinal lymph nodes. The presence of lymph node metastases decreased 5-year survival from 97 % (stage I) to 50 % (stage III). As inguinal femoral lymph nodal dissection carries chances of increased morbidity, preoperative evaluation helps in proper management of these patients. Pre-op evaluation of patients with FDG-PET with respect to nodal metastases to the groin reported an overall sensitivity of 80 %, specificity 90 %, PPV 80 %, and NPV of 90 %. Given the low sensitivity and high NPV, a negative scan result does not preclude surgical resection. Given the high specificity, FDG imaging identifies metastatic pelvic lymph nodes and can be used to plan preoperative chemoradiation or spare extensive groin dissection. A sensitivity of 75 % and specificity of 62 % have been reported for inguinofemoral nodal metastasis by using the new agent (11C) tyrosine. a number of new agents are being investigated for staging of vulvar cancer.
For Further Reading
Aide N, Cappele O, Bottet P, Bensadoun H, Regeasse A, Comoz F, et al. Efficiency of [(18)F] FDG PET in characterizing renal cancer and detecting distant metastases: a comparison with CT. Eur J Nucl Med Mol Imaging. 2003;30:1236–45.
De Hullu JA, Pruim J, Que TH, et al. Noninvasive detection of inguinofemoral lymph node metastases in squamous cell cancer of the vulva by L-[1e11C] tyrosine positron emission tomography. Int J Gynecol Cancer. 1999;9(2):141e6.
De Jong IJ, Pruim J, Elsinga PH, Jongen MM, Mensink HJ, Vaalburg W. Visualisation of bladder cancer using C-11-choline PET: first clinical experience. Eur J Nucl Med Mol Imaging. 2002;29:1283–8.
Grigsby PW, Siegel BA, Dehdashti F, Rader J, Zoberi I. Posttherapy [18F] fluorodeoxyglucose positron emission tomography in carcinoma of the cervix: response and outcome. J Clin Oncol. 2004;22:2167–71.
Hain SF, O’Doherty MJ, Timothy AR, et al. Fluoro deoxyglucose positron emission tomography in the evaluation of germ cell tumours at relapse. Br J Cancer. 2000;83:863–9.
Ho KC, Lai CH, Wu TI, et al. 18F-fluorodeoxyglucose positron emission tomography in uterine carcinosarcoma. Eur J Nucl Med Mol Imaging. 2008;35(3):484–92.
Kitajima K, Murakami K, Yamasaki E, et al. Performance of integrated FDG-PET/contrast enhanced CT in the diagnosis of recurrent uterine cancer: comparison with PET and enhanced CT. Eur J Nucl Med Mol Imaging. 2009;36(3):362–72.
Lamoreaux WT, Grigsby PW, Dehdashti F, et al. FDG-PET evaluation of vaginal carcinoma. Int J Radiat Oncol Biol Phys. 2005;62(3):733–7.
Lassen U, Daugaard G, Eigtved A, et al. Whole body FDG-PET in patients with stage I non-seminomatous germ cell tumours. Eur J Nucl Med Mol Imaging. 2003;30:396–402.
Price DT, Coleman RE, Liano RP, Robertson CN, Polascik TJ, DeGrado TR. Comparison of [18F] fluorocholine and (18F) fluoro deoxyglucose for positron emission tomography of androgen dependent and androgen independent prostate cancer. J Urol. 2002;168:273–80.
Risum S, Hogdall C, Loft A, et al. The diagnostic value of PET-CT for primary ovarian cancer- a prospective study. Gynecol Oncol. 2007;105(1):145–9.
Safaei A, Figlin R, Hoh CK, Silverman DH, Seltzer M, Phelps ME, Czernin J. The usefulness of F-18 deoxyglucose whole-body positron emission tomography (PET) for re-staging of renal cell cancer. Clin Nephrol. 2002;57:56–62.
Singh AK, Grigsby PW, Dehdashti F, Herzog TJ, Siegel BA. FDGPET lymph node staging and survival of patients with FIGO stage IIIb cervical carcinoma. Int J Radiat Oncol Biol Phys. 2003;56(2):489–93.
Toth G, Lengyel Z, Balkay L, Salah MA, Tron L, Toth C. Detection of prostate cancer with 11C-methionine positron emission tomography. J Urol. 2005;173:66–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer India
About this chapter
Cite this chapter
Pradhan, P.K., Mubalsha, R. (2015). Application of PET–CT in Genitourinary Malignancies. In: Das, B. (eds) Positron Emission Tomography. Springer, New Delhi. https://doi.org/10.1007/978-81-322-2098-5_14
Download citation
DOI: https://doi.org/10.1007/978-81-322-2098-5_14
Published:
Publisher Name: Springer, New Delhi
Print ISBN: 978-81-322-2097-8
Online ISBN: 978-81-322-2098-5
eBook Packages: MedicineMedicine (R0)