Abstract
Upon arriving above 2,500 m, the organism compensates the diminished inspired oxygen partial pressure by increasing ventilation and cardiac output. The pneumodynamic pump moves more rarefied air into the alveoli through an increase of the respiratory frequency and the tidal volume. Likewise, the hemodynamic pump increases both the cardiac frequency and the stroke volume, as if exercise were performed at sea level. The two pumps, one for air and the other for blood, carry out the essential role of supplying sufficient oxygen to the tissues and increasing the energy consumption until the red blood cells take over. The acid–base status, adequately interpreted at high altitude through the titratable hydrogen ion difference, along with the adaptation formula and multiple cellular changes, gives rise to adaptation. The tolerance to hypoxia formula reflects and explains the paradoxical concept that resistance to hypoxia grows as one goes higher. The possibility that man can adapt to live in the hypoxic environment of the summit of Mt. Everest is exposed. Furthermore, the knowledge of life at high altitude is proposed as an alternative to the environment of space travel. Herein, we describe our 43 years of experience and discoveries with fundamental concepts that change the way disease is treated in the hypoxic environment of high altitude.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- High Altitude
- Acute Mountain Sickness
- Chronic Mountain Sickness
- Oxygen Dissociation Curve
- Extreme Altitude
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The Earth is surrounded by an atmosphere that has an altitude of approximately 20 km. The air composition is the same at any altitude: 20.95 % oxygen, 78.09 % nitrogen, 0.93 % argon, and 0.039 % carbon dioxide. Small amounts of other gases are also present which are released upon industrial combustion and other natural events such as volcanic gas eruptions. It is actually the partial pressure of gases that decrease upon going higher. Nitrogen is an inert gas and its importance in respiration is transcendental, although currently lacking awareness. If the atmosphere was hypothetically only composed of oxygen (i.e., 100 %), the incidence of alveolar collapse, medically known as atelectasis, would greatly increase. Nitrogen and the lung surfactant aid in preventing this.
Adaptation to high altitude has three stages: (1) the acute altitude adaptation stage lasting 1 or 2 days, (2) the gradual subacute stage, and (3) the final chronic altitude adaptation stage [17]. In the acute and subacute stages, the immediate response to a diminished inspired oxygen tension (PIO2) is an increase in the pneumodynamic and hemodynamic pumps (Fig. 1).
The mechanisms of adaptation showing in the first stage: the increase of V = ventilation per minute composed of both the FR = respiratory frequency and Vt = tidal volume of the pneumodynamic pump and the Q = cardiac output, composed of both the FC = cardiac frequency and Vs = stroke volume of the hemodynamic pump. In the second stage: the increase in Hb = hemoglobin in the middle plays the fundamental role in the adaptation to high altitude
Both require a high energy demand that gradually decreases over time. Subsequently if the subject remains at the same altitude, the final optimal adaptation is achieved over a fixed amount of time. This time is directly proportional to the altitude. The adaptation formula described below is derived from these observations. In the second and third stages, molecular changes with a gradual increase in the number of red blood cells and hemoglobin occur. Concomitantly, the steroids and other biochemical metabolic changes play a secondary role. Chronic adaptation is achieved by reducing the expenditure of energy [18]. Hemoglobin increases but to a mean level suitable for the majority of the high-altitude residents, in the absence of illness. However, in some subjects with pulmonary shunts or uneven ventilation (sequel of pulmonary disease), the hemoglobin levels are higher. This has been previously referred to as “excessive polycythemia,” a term we are not in agreement with. As a consequence of these pulmonary alterations, blood flows through the organism with a lower oxygen tension. Upon reaching the kidney, erythropoietin production is stimulated which in turn induces an increase of red blood cells in the bone marrow.
Medicine is changing with time. Historically, we observed a much higher incidence of increased hemoglobin, which resulted from untreated and frequent bacterial pneumonias. The pulmonary alveoli were damaged, but the vessels and pulmonary capillary circulation remained unaffected. This resulted in shunts and subsequent low oxygen partial pressures in the blood. This has changed fundamentally due to the use of antibiotics. Currently, pneumococcus is treatable; however, new emerging diseases caused by virus that may not be as dramatic play a role not yet fully identified. Consequently, there are now fewer cases of what we call polyerythrocythemia formerly called polycythemia, increased polycythemia, erythrocythemia, or excessive erythrocytosis. The most appropriate term that we now use, based on the Greek terminology, is polyerythrocythemia: poly (many), erythrocyte (red blood cells), and hemia (in the blood).
Cardiorespiratory diseases at high altitude along with others have changed pathologically. For example, syphilis that affected a large number of people no longer exists. It turned out that Treponema pallidum was very sensitive to penicillin and was literally wiped out.
Much has been said about chronic mountain sickness. In this regard, we have had many discussions with world-renowned experts that still accept the term. We have stated that there is no such a thing as “chronic mountain sickness” at high altitude [5]. Diseases are the same, as at sea level, but they have been confused as chronic mountain sickness at altitude. These are mostly lung diseases of different etiopathogenesis, fundamentally with shunt production. The increase of hemoglobin above the normal at high altitude is due to respiratory insufficiency. Polyerythrocythemia has also been observed in cardiac arrhythmias, and after a pacemaker implantation, the number of red blood cells returned to normal values for that specific altitude.
Naturally, there may be very rare hematologic diseases, some yet undiscovered, but these would be exceptions. The carotid body disease can present with polyerythrocythemia. There is evidence of an increased incidence of carotid glomus at high altitude. Also, mistakenly it was thought that there was a relationship between age and polyerythrocythemia, but it has widely been disregarded. Some kidney diseases with renal artery narrowing also produce increased hematocrit. Some authors have sought other alterations in the gonads with hypoventilation, which led them to attempt treatments with progesterone. This only resulted in feminization of men without an effective and practical decrease in the number of red blood cells.
Others attempted to physically remove the RBCs. They even used cytotoxic drugs such as phenylhydrazine [19, 25]. Many died (and unfortunately continue to do so) due to this iatrogenic disease instead of the polyerythrocythemia. In Bolivia, one of the authors had to fight against the use of this internationally banned drug. He was initially misunderstood creating a social whirl but eventually won, resulting in the recognition and comprehension that the use of this drug is obviously prohibited by the World Health Organization.
Phlebotomy is still used as a treatment in these patients in order to physically reduce the number of RBCs. Our institute, IPPA, has never supported phlebotomy and because the fundamental concept is not to alter the perfect (energy-efficient) physiological balance of chronic adaptation [11]. When a phlebotomy is performed, with a consequent reduction of the optimal number of RBCs, it induces a condition similar to acute adaptation in the high-altitude patient, as if the high-altitude resident had gone to a higher altitude. The resulting increase in heart rate and ventilation is misinterpreted as an improvement. Patients with polyerythrocythemia have been found to hypoventilate. This was erroneously misinterpreted as the cause instead of an energy-efficient mechanism of oxygen transport [18]. After phlebotomy, there is an extra energy expenditure that is gradually reduced by again increasing the RBCs.
The high viscosity of blood is often feared as a possible cause of cerebrovascular accidents. Yet, an increase of RBCs does not necessarily lead to the formation of thrombus. This is somewhat conflicting with our studies. There are reports of hypercoagulability in other latitudes and longitudes, but we have not seen this phenomenon in Bolivia. It may partly be due to dehydration in newcomers to high altitude or the presence of some sort of undetected infection or even genetic tendencies.
The result of many years of study on polyerythrocythemia has led to a better understanding and hence improved therapy significantly reducing the concept of this previously considered evil disease. This was achieved in the laboratory, jumping to a practical and pragmatic use for health improvement of the inhabitants of high altitude. The essential concepts of our interpretation of hypoxia follow in the following paragraphs.
Chronic Mountain Sickness (CMS)
We consider that the increase of the hematocrit (above that of the normal residents) found in some high-altitude residents is not a disease in itself but rather a sign, i.e., a hematologic response to disease in the hypoxic environment of hypobaria at high altitude [21, 23]. What was previously known as chronic mountain sickness (CMS), a condition in which the hematocrit is increased above the normal level in residents at high altitude, is now referred to as polyerythrocythemia (PECH) from the Greek poly = increase, erythro = red, cyt = cells, and hemia = in the blood. Consequently, where the abbreviation PECH is used throughout, it refers to what was previously named CMS [18].
Chronic mountain sickness can occur in some long-term residents of altitudes above 2,500 m – the Andes and elsewhere. The number of red cells in the blood (Polyerythrocythemia) and the hematocrit develops to exceptionally high values. The high hematocrit and viscosity of the blood do not necessarily lead toward the formation of emboli, which occurs when there is concurrent phlebitis or other vascular disease. In patients with lung disease, pulmonary vasoconstriction maintained over the years can lead to pulmonary hypertension and enlargement of the right ventricle, resulting eventually in right-sided congestive heart failure – Latin: cor pulmonale. A large fraction of the cardiac output is shunted through vessels with hypoventilated alveoli, so the patient is cyanotic with congested ear lobes and some with finger clubbing. CMS is an inadequate denomination for pulmonary disease at high altitude, associated frequently to pulmonary shunts with increased erythropoietin and polyerythrocythemia.
In the article “Consensus Statement on Chronic and Subacute High Altitude Diseases” in 2005, we as coauthors held a minority point of view [5]. Our work of over 50 years in the city of La Paz located between 4,100 and 3,100 m gave us a lens through which we observed accurately and inquisitively, high-altitude pathology, on a daily basis.
In the aforementioned article, two essential points were a source of discussion:
-
1.
The use of a questionnaire to evaluate the symptoms of CMS.
-
2.
The use of the term “loss of adaptation” as opposed to “adaptation to disease in the hypoxic environment.” The concept “loss of adaptation” was incorrect since it was a mere attempt to avoid the explanation of the etiopathophysiology of the disease.
We opine that CMS is rather an adaptive reaction to an underlying malfunction of some organs and no specific symptoms could be quantified. To substantiate our line of reasoning, we reviewed 240 CMS cases seen at the High Altitude Pathology Institute in La Paz. Patients who had a high hematocrit (>58 %) underwent pulmonary function studies in search for the cause of hypoxia: hypoventilation, diffusion alteration, shunts, and uneven ventilation–perfusion. The tests included arterial blood gas tests, chest x-rays, spirometry, hyperoxic tests, flow–volume curves, ventilation studies at rest and during exercise, ECG, exercise testing, and Doppler color echocardiography to assess heart structure and function. When correlated with clinical history, these results revealed that CMS is practically always secondary to some type of anomaly in cardiorespiratory or renal function and very rarely other hematologic disease. Therefore, a questionnaire that tried to catalog symptoms common to many types of diseases that lead to hypoxia is flawed because it leads to incomplete diagnosis and inappropriate treatment. CMS, once again, was shown to be an adaptation of the blood transport system to a deficient organs’ function due to diverse disease processes, the adaptation aimed at sustaining normoxia at the cellular level in the hypoxic environment at high altitude.
Quoting Prof. Zubieta-Castillo (Sr): “The organic systems of human beings and all other species tend to adapt to any environmental change and circumstance, and never tend towards regression which would inevitably lead to death.”
The Triple Hypoxia Syndrome
Many patients with PECH at high altitude in the city of La Paz (3,600 m), with hematocrit greater than 55 % but not greater that 70 %, apparently can function normally. They work, play soccer, develop intellectual activities, and frequently perform better than sedentary normal people. They request medical attention, only when they present symptoms similar to those of acute mountain sickness (AMS), such as headache, dyspnea, nausea, lassitude, and indigestion. Without going higher, they have been said to experience “soro jchi (soroche) AMS in bed.” Their arterial blood gases may show extreme hypoxia with an oxygen arterial tension (PaO2) near 20 mmHg, with or without hypercapnia and a normal or acidotic pH. We have previously named this complication of PECH (formerly referred to as chronic mountain sickness (CMS)) triple hypoxia syndrome (THS). It is due to the addition of three hypoxias: (1) normal high-altitude adaptation to hypoxia, (2) PECH hypoxia (CMS), and (3) an acute additional hypoxia that can be reversed by oxygen. This is similar to “surviving” in the summit of Mt. Everest at a much lower altitude. It may be caused by viral infections (gripe) or some other acute respiratory disease, with malaise that lasts several days without treatment and typically is reversed by 24 h of oxygen to PaO2 baseline values of their chronic condition with polyerythrocythemia. The diagnosis is important, since THS is an acute transitory condition that when not recognized and treated with oxygen can possibly lead to cardiac, pulmonary, or cerebral complications and even death [22, 26].
The Increase in Hematocrit During the High-Altitude Adaptation Process
High-altitude adaptation is altitude and time dependent following the simplified equation:
where each concept stands for:
-
High-altitude adaptation = Time at altitude (days) / Altitude in kilometers (km) [17].
For a fixed altitude, the only variable that changes is time. Immediately upon ascent, the organism senses the lowering of the oxygen partial pressure due to a diminished barometric pressure. The initial acute phase usually lasts between 1 and 2 days, varying according to the health conditions of the subject and if he or she has previously been exposed to high altitude and learned how to “handle” it in complex macrosystemic and microsystemic mechanisms. The former implies cardiorespiratory compensation and the latter adaptation processes at the cellular and molecular level. The macrosystemic mechanisms attempt to raise the PaO2 to “sea level values” through increased ventilation and higher cardiac frequency, never being able to achieve it, thereby reducing the PaCO2 resulting in respiratory alkalosis, a negative action at the cellular level. The microsystemic mechanisms return the pH to normal, through kidney function, reducing the negative symptoms of acute mountain sickness through adequate cellular function. However, a permanent and stable adaptation is only achieved at around 4 weeks when the hematocrit reaches the optimal level for the altitude (3600 m). Consequently, high-altitude adaptation is defined as having three stages:
-
(A)
Acute, first 72 h, where acute mountain sickness (or high-altitude pulmonary edema, HAPE, and high-altitude cerebral edema, HACE) can occur.
-
(B)
Subacute, from 72 h until the slope of increase of the hematocrit rise with time is zero; here high-altitude subacute heart disease can occur, if excessive exercise is performed.
-
(C)
Chronic, where the hematocrit level is constant and the healthy high-altitude residents achieve their optimal hematocrit.
We have measured hematocrit changes in one high-altitude resident traveling several times between La Paz (3,510 m) and Copenhagen (35 m above sea level) for 3 years. We have also studied the fall in hematocrit values in three lowlanders traveling once from La Paz to Copenhagen [17].
A complete and optimal hematocrit adaptation is only achieved at around 40 days for a subject going from sea level to 3,510 m in La Paz as shown in Fig. 2. The time in days required to achieve full adaptation to any altitude, ascending from sea level, can be estimated by multiplying the adaptation factor of 11.4 by the altitude in km. Subjects with different cardiopulmonary deficiencies increase the hematocrit to levels above those of normal individuals.
Conversely, descending from high altitude in La Paz to sea level in Copenhagen, the hematocrit response is a linear fall over 18–23 days as shown in Fig. 3.
Hypoventilation in Chronic Mountain Sickness
Patients diagnosed with chronic mountain sickness or rather PECH have repeatedly been found to hypoventilate. Low saturation in PECH is attributed to hypoventilation. Although this observation seems logical, a further understanding of the exact mechanism of hypoxia is mandatory. An exercise study using the Bruce Protocol in PECH subjects (n = 13) compared with normals N (n = 17), measuring ventilation (VE), pulse (P), and saturation by pulse oximetry (SaO2) was performed. Ventilation at rest while standing, prior to exercise in a treadmill, was indeed lower in PECH subjects (8.37 l/min compared with 9.54 l/min in N). However, during exercise at stages one (3′) through four (12′), ventilation and cardiac frequency both remained higher than in N. In spite of this, SaO2 gradually decreased. Although PECH subjects increased ventilation and heart rate more than N, saturation was not sustained, suggesting respiratory insufficiency. The degree of venoarterial shunting of blood is obviously higher in the PECH patients both at rest and during exercise as judged from the SaO2 values. The higher shunt fraction is probably due to a larger degree of trapped air in the lungs with uneven ventilation of the PECH patients.
One can infer that hypoventilation at rest is an energy-saving mechanism of the pneumodynamic and hemodynamic pumps [18]. Increased ventilation would cause an unnecessary high SaO2 at rest (low metabolism). This is particularly true during sleep.
A Biological and Mechanical Energy-Efficient Space Travel Alternative: Hypobaric Cabin Pressure
Astronauts in the microgravity environment of space suffer with conditions such as anemia [10]. Thus far unexplained, neocytolysis has been described as the possible underlying mechanism [2, 9]. The adaptation to space capsules involves less use of muscles and changes in ventilation–perfusion at lung level so that the organism finds it convenient to reduce the hematocrit following the least energy expenditure concept [18]. The knowledge and understanding of polycythemia and anemia resulting from altitude shifts [17] allows for a logical proposal to bloodletting of high-altitude residents on travel to sea level for periods longer than 20 days (an outstanding humanitarian blood resource) and similarly in astronauts when going into space. The logic is that they would economize energy, avoiding the destructive phase of adaptation. However, in astronauts, upon return to sea level, reinfusion of the phlebotomized blood could return the hematocrit to normal levels. Erythropoietin administration is also an option but not favored due to associated complications.
Original space flights were in a pure oxygen environment and one-third the sea level pressure until serious fire accidents were encountered. Currently, the cabin pressure is normal sea level pressure at 760 Torr with 20 % oxygen and 80 % nitrogen (NASA) [6].
An alternative to the complication of anemia would be to reduce the ambient oxygen tension within space vehicles, down to 2/3 the sea level pressure (similar to the altitude of the city of La Paz with over 1.5 million inhabitants), in order to maintain a hypoxic stimulus and sustain the number of red blood cells for re-entry to Earth. Furthermore, the weightlessness space conditions require less oxygen consumption as there is less muscular use and hence tolerance to hypoxia can be increased. Likewise, the Extravehicular Mobility Unit could benefit from a lower oxygen tension, less pressure difference between outside and within the space capsule, a speedier preparation, and additionally more autonomy. Long space flights in the near future would require less wasted resources in excess oxygen production. The return to the normal (relative hyperoxic) environment of sea level would ease adaptation, as there would presumably be no reduction of the hematocrit during space flight [15].
Man may undertake space travel in the future where oxygen tensions will be a crucial life-saving variable, and this proposal provides a physiological and physical energy-efficient alternative.
Adaptation to Life at the Extreme Altitude of Mt. Everest
Short permanence of humans, under acute conditions, with partial and incomplete adaptation with eminent risk of death demonstrates that even at the highest places of the planet Earth, enough mechanisms of tissue oxygenation are still present. The only objective of the ascent is the conquest of the summit, even for just a few minutes, demonstrating the extraordinary physical capacity of human beings. This is done even under adverse climatic conditions like extreme cold and storms.
As knowledge and technology improve, man is able to accomplish the most difficult challenges previously considered impossible. The conquest of the summit of Mt. Everest (8,848 m), the highest point of the planet, for example, was originally thought to be impossible. Careful preparation of the expeditions, experience, persistence, and extraordinary stamina allowed Sir Edmund Hillary and Tenzing to stand on top of the mountain. Up to the year 2006, hundreds have reached such extreme altitude and, after Messner and Habeler, some of them without supplementary oxygen. But the question remains: What is the highest possible point of permanent residence?
Based on the observation of man’s highest habitats, most scientists believe 5,000 m above sea level is the limit for adaptation to hypoxia. Likewise, it is well known that acute exposure of humans to this altitude and above, without any kind of adaptation for tissue oxygenation, can result in loss of conscience and even death.
In the study entitled “A consideration of the Possibility of Ascending Mt. Everest,” Kellas proposes that the “limits of permanent acclimatization to high altitudes,” based on his own experience, was 6,096 m. Curiously, several decades later, most physiologists believed it was much lower. In the north of Chile, the Aucanquilcha mine is at 5,950 m. The Indian Armed Forces have set up military posts in the border with Pakistan at around 6,000 m, residing there for long periods up to 6 months or more. Inder Anand reported that several soldiers suffered subacute heart disease. This can now be attributed to a fast ascent and inadequate time of adaptation (not disregarding possible previous cardiac pathologies not adequately diagnosed prior to the ascent, in some)
The hypothesis “man can adapt to the altitude of the summit of Mt. Everest” was conceived based on experience gained over 36 years (at the time of publication). Ever since its creation, in 1970, the High Altitude Pathology Institute, Clinica IPPA (3,510 m), has studied and treated patients (permanent residents and newcomers) in the cities of La Paz and El Alto (3,100–4,100 m) and the surrounding areas in Bolivia (4). It was estimated that in Bolivia, more than 5,000,000 people (2/3 of the total population) live above 2,000 m. Additionally, the proposed hypothesis was also based on a study of the history of high life and exponentially growing scientific literature on high altitude around the world.
With adequate and gradual adaptation, life is possible even at the hypoxic levels of the summit of Mt. Everest [20, 24, 27]. We describe some further examples that provide proof of such a statement:
-
1.
Life at high altitude in the city of La Paz between 3,100 and 4,100 m where people sustain variable degrees of tissue hypoxia having a very low arterial oxygen tension (PaO2 = 37 mmHg) due to respiratory and/or cardiac disease.
-
2.
It is possible to perform maximal work at extreme altitudes, as evidenced by a soccer match played at 6,542 m on the summit of Mount Sajama.
-
3.
Severe high-altitude pulmonary edema (HAPE) occurred in a rugby player within 72 h at 3,600 m (PaO2 of 27 mmHg and a SaO2 of 45 %) upon arrival from Portugal.
-
4.
In the triple hypoxia syndrome (THS) where polyerythrocythemic (CMS) patients with gradual adaptation to hypoxia, with a high hematocrit, can occasionally tolerate a PaO2 of 30 mmHg for a week or longer, a severe hypoxic condition similar to that on the summit of Mt. Everest [22].
-
5.
Human fetus under normal conditions develop at oxygen tension values equal to the altitude of Mt. Everest until delivery (PaO2 = 28 mmHg). They are naturally capable of living in hypoxic environmental conditions present on our planet.
Consequently, normal subjects with full capacity for adaptation will show that life is possible at any existing altitude on planet Earth, provided that the following conditions are met: adequate environmental temperatures, heated lodging, adequate food, and slow and progressive adaptation to increasing altitudes. This seems possible in only one generation in a young perfectly healthy individual, as the human organism is provided with the adequate compensation mechanisms. Once adapted, the capacity for reproduction on site seems feasible.
Pregnancy and delivery, at the highest altitude on planet Earth, occurred in the city of La Paz. A young girl had an unwanted pregnancy at the city of El Alto (4,100 m), and consequently, she moved to an isolated place in Chacaltaya at 5,300 m for the rest of her pregnancy. She worked at a refuge there until the time of delivery that was carried out uneventfully (precariously at the resourceless refuge) giving birth to a healthy female.
Extreme Hypoxia in Newcomers to High Altitude: How Can It Be Tolerated?
Patients suffering from the acute effects of hypobaric hypoxia can have extremely low arterial oxygen tensions (PaO2), which are quite well tolerated. They can come to consultation with a PaO2 between 30 and 40 mmHg. Their recovery after a few days is uneventful following the efficient treatment of the underlying cause.
At sea level, these very low oxygen tensions are not tolerable. A patient presenting a PaO2 of 60 mmHg can be sent to an intensive care unit, as his or her life could be at risk. However at high altitude in the city of La Paz of 3,600 m, the normal acid–base values are as follows: PaO2 = 60 ± 2 mmHg, PaCO2 = 30 ± 2 mmHg and pH = 7.40 ± 0.02, and SpO2 = 91 % ± 1 %. The latter oscillates with irregular breathing and deep breaths can achieve even 98 % as has been previously described [12].
One out of four subjects, arriving to La Paz, has some form of acute mountain sickness. This implies headaches, shortness of breath, loss of appetite, malaise, nausea that can evolve to vomiting, and more severe neurological alterations in HACE or pulmonary alterations in HAPE.
Some can present extreme hypoxia. The pathologies that we have recently seen associated with this extreme hypoxia are pneumonia upon ascent, pulmonary thromboembolism, high-altitude pulmonary or cerebral edema, and several others.
For example, a 25-year-old Frenchman climbed Huayna Potosi at 6,000 m 2 days after arriving to La Paz 3,600 m from Paris. On the way down, he felt shortness of breath and was unable to sleep over the night. He came to consultation walking. A blood gas analyses reported a PaO2 = 35 mmHg, PaCO2 = 29 mmHg, and a pH = 7.53. This was diagnosed as severe hypoxia and respiratory alkalosis in high-altitude pulmonary edema. Would he have been alive if at sea level? What is the explanation for this extreme hypoxia tolerance?
The alkaline pH during acute high-altitude exposure shifts the oxygen dissociation curve to the left, allowing more capture and transport of oxygen. The other variable that can allow for the tolerance to extremely low PaO2 values is the normal low (relative to sea level) PaCO2. The acid–base balance in the human body is calculated by the Van Slyke equation based on sea level measurements. The maintenance of blood pH within a fairly strict range at/around pH 7.4, with due consideration of the effect of hyperventilation, is essential for cellular function at any altitude. This is because various chemical processes occurring in the body, e.g., those involving proteins and enzymes, are pH dependent. As is well known, oxygen and carbon dioxide partial pressures get lower as the altitude gets higher. At permanent low levels of the arterial carbon dioxide partial pressure (PaCO2), the acid–base balance begins to change. Mountaineering physiologists, unfortunately, assumed that the sea level equation for A–B balance would be equally applicable, without any critical thought, and never thought of appropriate equations valid for high-altitude calculations [14]. The pH effects are inextricably linked critically with hemoglobin and oxygen status that can be crucial at high altitudes. Therefore, for a more precise recalculation of the “titratable hydrogen ion difference,” that should use a Hb and HCO3 − values for a particular altitude, we have derived our modified Van Slyke equation [8]. An adequate acid–base balance is probably the fundamental metabolic adaptation that allows for mountaineers to tolerate extreme hypoxia and even reach the summit of Mt. Everest.
The Tolerance to Hypoxia Formula
People living at high altitude in the city of La Paz (3,600 m), with diverse types of lung disease, exhibit extremely low arterial oxygen tensions (PaO2). Their arterial oxygen partial pressure of oxygen (PaO2) can range between 30 and 40 mmHg (normal values—PaO2 = 60 ± 2 mmHg, arterial carbon dioxide tension (PaCO2) = 30 ± 2 mmHg, and pH = 7.40 ± 0.02; oxyhemoglobin saturation by pulse oximetry (SpO2) is 91 % ± 1 %). The SpO2 oscillates with irregular breathing and taking a deep breath can result in even 98 % (like at sea level) provided there is a normal pulmonary function, as previously described [12]. This results from a decrease in the ratio between pulmonary dead space and alveolar ventilation. When the medical reports from people in La Paz were shown to physicians at sea level, they often asked, “Were these people conscious?” This clearly shows that people at sea level cannot tolerate such low arterial PO2. A patient presenting a PaO2 below 60 mmHg at the sea level is usually sent to an intensive care unit, as his life could be in peril.
Importance of Arterial PCO2: The First Factor
The other variable that can allow for the tolerance to extremely low PaO2 values is the low PaCO2 values at high altitude relative to sea level. As is well known, oxygen and carbon dioxide partial pressures descend as the altitude increases. The distribution of PaCO2 in arterial blood gases at the city of La Paz (3,510 m) shows clearly that the average is around 30 mmHg. Furthermore, it is evident that the highest PaCO2 reached is 72 mmHg in an isolated critically terminally ill patient. The great majority hardly reach a PaCO2 above 53 mmHg. At high altitude, high PaCO2 levels as those seen at sea level are not compatible with life.
Hypocapnia and the ensuing alkaline pH during high-altitude exposure shift the oxygen dissociation curve to the left, in an attempt to increase the efficiency of the capture and transport of oxygen. In reality, the curve’s P-50 is dynamic moving to the left at the pulmonary capillaries and to the right at the tissue level. The acid–base balance in the human body is calculated by the Van Slyke equation based on sea level measurements. The maintenance of blood pH within a fairly strict range at around pH 7.4, with due consideration of the effect of hyperventilation, is essential for cellular function at any altitude. This is because various chemical processes occurring in the body, e.g., those involving proteins and enzymes, are pH dependent. With chronic low levels of the arterial carbon dioxide partial pressure (PaCO2), the acid–base balance begins to change. Mountaineering physiologists employed the sea level equation for estimations of acid–base balance in high-altitude subjects without critical appraisal of its validity. The pH effects are inextricably linked critically with hemoglobin and oxygen status that can be crucial at high altitudes.
Therefore, for a more precise recalculation of the “titratable hydrogen ion difference” (THID) that should use Hb and HCO3 −values for a particular altitude, we have derived our modified Van Slyke equation: THID in eECF = (1 − [Hb]/43) × (Δ[HCO3 −] + ßB) × (pH-7.4) [8]. An adequate acid–base balance is probably the fundamental metabolic adaptation that allows for mountaineers to tolerate extreme hypoxia and even reach the summit of Mt. Everest [14].
Hemoglobin: The Other Factor
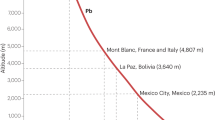
Hemoglobin (Hb) increases with altitude as shown in Fig. 4. This data is from permanent residents at different altitude cities or towns. From the trend curve, one can attempt to estimate the optimal hemoglobin value upon the summit of Mt. Everest, if complete adaptation could be achieved.
Hemoglobin values found at different altitudes in resident populations. The red dot is the calculated Hb from the trend equation: Hb = 2E-07x2 - 0.0003x + 14.45 with an R = 0.9718. The Hb values for residents at 2,500, 3,600, and 4,100 m for the Bolivia cities of Cochabamba, La Paz, and El Alto, respectively, are the normal values in our labs. The Hb values of residents at 4,355, 4,660, and 5,500 m were obtained from bibliographic data [4]
It becomes evident from the observation of a longer breath holding time at high altitude in polyerythrocythemia (PECH) patients with low PaO2, compared with normal-high altitude subjects, that they are more tolerant to hypoxia [13]. The greater oxygen content of blood in PECH, as a result of the increase in Hb, allows for a better tolerance to hypoxia. This is also demonstrated by plotting the oxygen consumption of yeast cells against time after full saturation with 100 % oxygen [7]. The resulting oxygen dissociation curve of PECH patients has a much broader oxygen content area when exposed to 100 % oxygen [16].
The above observations on PaCO2 and Hb prompted us to propose the hypothesis [16] that the tolerance to hypoxia (TH) formula can be defined as
The constant factor is obtained by using the Hb and PaCO2 normal sea level values and equating to 1. This way, the tolerance to hypoxia for comparison purposes becomes 1 at sea level. From then on, the values at different altitudes are calculated as shown in Table 1. In this table, the Mt. Everest value is obtained from the paper by Grocott et al. [3] taken on the Cauldwell Expedition to Mt. Everest. Blood gases were measured at 8,400 m, and the Hb values were obtained from four subjects averaging the measurements at 5,300 m before and after the climb to the summit. This value should have been measured at higher altitudes and without averaging before and after climb as it reduces the true value. Only the value obtained after the ascent could be a more appropriate measure. However since the subjects were climbing and changing altitudes and the body has a fixed production of red blood cells, there was not enough time for full hematologic adaptation [17]. An optimal hemoglobin value for the summit of Mt. Everest is not known. However, based on Fig. 4, it is estimated that the optimal hemoglobin for oxygen transport at the summit of Mt. Everest would be around 26 g%. This roughly corresponds to a hematocrit of 78 %. In our medical practice, we have seen patients with PECH even above 80 % [12, 18, 19]. Hence, although it seems that these are surprising high values, they are within biological limits for humans. It is noteworthy that the maximum possible increase of Hb is double the sea level value, hence the tolerance to hypoxia formula is also is ruled by this.
Our formula links Hb with PaCO2, the hematologic and respiratory (including acid–base parameter) responses to hypoxia, respectively. These biological responses to hypoxia in humans will also apply to animals. This is clearly demonstrated when a normal average sea level Hb in males of 13.3 g% rises to an average of 16.6 g% in the city of La Paz, Bolivia, at 3,510 m of altitude, for example. The formula also includes the PaCO2 where it is showing the hyperventilatory response to hypoxia. For example, a sea level normal PaCO2 of 40 mmHg upon arrival to high altitude immediately is decreased to a PaCO2 of 30 mmHg, again, in the city of La Paz (3,510 m). Although this is a tolerance to hypoxia formula, the PIO2 is not included in the formula as it is directly related to the barometric pressure, as originally described by Paul Bert in 1878 [1]. The barometric pressure, a physical atmospheric parameter, is indirectly included with the PaCO2 which is equal to the FaCO2 * PB − PH20.
Other factors of adaptation to hypoxia, such as HIF, VEGF, increase in the density of the mitochondria, increase in capillary density, increase in pulmonary artery pressure, and increase in heart rate and ventilatory rate, are not included in this formula, as they are linked to the two biological factors included. Adaptation to hypoxia is complex, but this formula uses only two essential variables sufficient for the adequate interpretation of the concept in our criteria.
Conclusion
Adaptation to life at high altitude is possible, even at extreme environments such as the summit of Mt. Everest. The practice of medicine and observation over 44 years has taught us much about hypoxia. During a congress in Lhasa, Tibet, several physicians visited an intensive care unit where there was a subject suffering from pulmonary edema. He was in bed and receiving oxygen by mask. We wanted to see what his SpO2 would be when breathing ambient air. After a few minutes, the SPO2 started decreasing, and much to our surprise, one of the physicians who never had any experience in dealing with patients living in high altitude panicked and immediately ordered that the oxygen be restored. He was terribly alarmed by the ensuing hypoxia. This is understandable at sea level. A normal PaO2 of the city of La Paz, 60 mmHg if seen at sea level, would produce tremendous alarm and possibly immediate hospitalization and intensive care. Paradoxically, the higher one goes, the more tolerant the subject is to hypoxia. Please don’t misunderstand us, as we are talking of chronic adapted individuals and not acute exposure that can certainly produce symptomatology and even progress to high-altitude pulmonary edema or high-altitude cerebral edema. Life under chronic hypoxia is normal as at sea level. Diseases at high altitude, particularly in the cardiorespiratory areas, behave differently because the organism adapts to chronic hypoxia, even deviating from the normal and optimal status of good health.
References
Bert P (1978) Barometric pressure. Undersea Medical Society, Bethesda
De Santo NG, Cirillo M, Kirsch KA, Correale G, Drummer C, Frassl W et al (2005) Anemia and erythropoietin in space flights. Semin Nephrol 25:379–387
Grocott MP, Martin DS, Levett DZ, McMorrow R, Windsor J, Montgomery HE (2009) Arterial blood gases and oxygen content in climbers on Mount Everest. N Engl J Med 360:140–149
Leon-Velarde F, Gamboa A, Chuquiza JA, Esteba WA, Rivera-Chira M, Monge CC (2000) Hematological parameters in high altitude residents living at 4,355, 4,660, and 5,500 meters above sea level. High Alt Med Biol 1:97–104
Leon-Velarde F, Maggiorini M, Reeves JT, Aldashev A, Asmus I, Bernardi L et al (2005) Consensus statement on chronic and subacute high altitude diseases. High Alt Med Biol 6:147–157
NASA Crew Compartment Cabin Pressurization (2007) spaceflight.nasa.gov/shuttle/reference/shutref/orbiter/eclss/cabinpress.html. Accessed 15 Jun 2014
Neville J (1974) Hemoglobin oxygen affinity measurement using biotonometry. J Appl Physiol 37:961–971
Paulev PE, Zubieta-Calleja GR (2005) Essentials in the diagnosis of acid-base disorders and their high altitude application. J Physiol Pharmacol 56(Suppl 4):155–170
Rice L, Alfrey CP (2005) The negative regulation of red cell mass by neocytolysis: physiologic and pathophysiologic manifestations. Cell Physiol Biochem 15:245–250
Tavassoli M (1982) Anemia of spaceflight. Blood 60:1059–1067
Zubieta-Calleja G (2004) Bloodletting: a medical resource since the stone age. J Qinghai Med Coll 25:273–275
Zubieta-Calleja G, Zubieta-Castillo G (1998) Changes in oximetry during breath holding in normal residents of high altitude. In: Hideki Ohno, Toshio Kobayashi, Shigeru Masuyama and Michiro Nakashima (eds) Progress in mountain medicine and high altitude physiology. Press Committee of the 3rd World Congress on Mountain Medicine and High Altitude Physiology, Matsumoto, pp 343–348
Zubieta-Calleja G, Zubieta-Castillo G, Zubieta-Calleja L, Zubieta N (2002) Measurement of circulatory time using pulse oximetry during breath holding in chronic hypoxia. HAMB 3:115
Zubieta-Calleja GJ, Paulev P-E, Mehrishi JN, Zubieta-Castillo G Sr (2012) Extremely high altitude hypoxic conditions during Mount Everest expeditions, residence at South Pole stations, in Tibet and among the Andes: Van Slyke equation modification is crucially important for acid–base measurements. JBPC 12:103–112
Zubieta-Calleja GR (2007) Human adaptation to high altitude and to sea level: acid-base equilibrium, ventilation, and circulation in chronic hypoxia. Thesis. University of Copenhagen, Copenhagen
Zubieta-Calleja GR, Ardaya G, Zubieta N, Paulev PE, Zubieta-Castillo G (2013) Tolerance to hypoxia. J Fisiol 59(4): 65–72
Zubieta-Calleja GR, Paulev P-E, Zubieta-Calleja L, Zubieta-Castillo G (2007) Altitude adaptation through hematocrit changes. J Physiol Pharmacol 58:811–818
Zubieta-Calleja GR, Paulev PE, Zubieta-Calleja L, Zubieta-Calleja N, Zubieta-Castillo G (2006) Hypoventilation in chronic mountain sickness: a mechanism to preserve energy. J Physiol Pharmacol 57(Suppl 4):425–430
Zubieta-Calleja GR, Zubieta-Castillo G, Zubieta-Calleja L (1995) Inadequate treatment of excessive erythrocytosis. Acta Andina 4:123–126
Zubieta-Castillo G Sr, Zubieta-Calleja GR Jr, Zubieta-Calleja L, Zubieta N (2004) How chronic mountain sickness (cms) contributed to the theory of life at the hypoxic levels of the summit of mount Everest. HAMB 5:291–292
Zubieta-Castillo G Sr, Zubieta-Calleja GR Jr, Zubieta-Calleja L (2006) Chronic mountain sickness: the reaction of physical disorders to chronic hypoxia. J Physiol Pharmacol 57(Suppl 4):431–442
Zubieta-Castillo G, Zubieta-Calleja G (1996) Triple hypoxia syndrome. Acta Andina 5:15–18
Zubieta-Castillo G, Zubieta-Calleja G, Arano E, Zubieta-Calleja L (1998) Respiratory disease, chronic mountain sickness and gender differences at high altitude. In: Ohno H, Kobayashi T, Masuyama S, Nakashima M (eds) Progress in mountain medicine and high altitude physiology. Press Committee of the 3rd World Congress on Mountain Medicine and High Altitude Physiology, Matsumoto, pp 132–137
Zubieta-Castillo G, Zubieta-Calleja GR (2007) Facts that prove that adaptation to life at extreme altitude (8848 m) is possible. In: Lukyanova L, Takeda N, Singal PK (eds) Adaptation biology and medicine: health potentials, vol 5. Narossa Publishing House, New Dehli
Zubieta-Castillo G, Zubieta-Calleja GR (1988) Iatrogenic disease in a polycythemic patient at altitude. Am Rev Respir Dis 137:509
Zubieta-Castillo G, Zubieta-Calleja GR (1988) The triple hypoxia syndrome at altitude (abstract). Am Rev Respir Dis 137:509
Zubieta-Castillo G, Zubieta-Calleja GR, Zubieta-Calleja L, Zubieta C, Nancy (2003) Adaptation to life at the altitude of the summit of Everest. Fiziol Zh 49:110–117
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer India
About this chapter
Cite this chapter
Zubieta-Castillo, G., Zubieta-Calleja, G. (2014). High-Altitude Research and Its Practical Clinical Application. In: Singh, S., Prabhakar, N., Pentyala, S. (eds) Translational Research in Environmental and Occupational Stress. Springer, New Delhi. https://doi.org/10.1007/978-81-322-1928-6_5
Download citation
DOI: https://doi.org/10.1007/978-81-322-1928-6_5
Published:
Publisher Name: Springer, New Delhi
Print ISBN: 978-81-322-1927-9
Online ISBN: 978-81-322-1928-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)