Abstract
During acute KD, the coronary artery lesions most frequently observed in pediatric Kawasaki disease (KD) patients are giant arterial aneurysms. Severely stenotic calcified lesions appear near the aneurysms when patients reach school age. Traditional balloon catheter treatment of stenotic lesions is hampered by the presence of calcification, which makes balloon expansion difficult. In addition, long-term patency is a problem for bypass surgery. Hence, standard treatment has been medical therapy with restrictions on physical activity. Rotablation has made it possible to safely perform catheterization of lesions in pediatric KD patients for which balloon catheter treatment is not indicated. The effects are maintained over the long term and provide benefits as the child grows and develops.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Clinical Outcomes for Rotablation for Kawasaki Disease Coronary Artery Lesions
We used rotablation to treat 33 lesions from 26 patients between May 1993 and December 2002.
Patients, Lesions, and Information on the Procedures
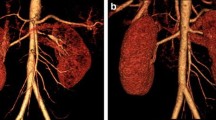
Patient age ranged from 8 to 28 years, and the average age was young, 15 years. Kawasaki disease (KD) was generally diagnosed between age 0 and 8 years, and average age at diagnosis was 2 years. Males represented 77 % of patients; 31 % of patients had multivessel disease, 8 % had a previous myocardial infarction (MI), and all patients were either asymptomatic or had only mild stable-effort angina. Lesion morphology was highly complex: 100 % had calcified lesions, 85 % had coronary aneurysms, 22 % had ostial lesions, and 100 % had lesions that were not balloon-expandable. The target vessel was the LAD in 58 %, RCA in 36 %, and LCX in 6 %. Average lesion length was 4.7 mm (vessel diameter, 3.82 mm). In other words, there were many focal lesions in large-diameter vessels and very few diffuse lesions, which made these patients suitable for rotablation. The average minimum vessel diameter was 1.26 mm, and average stenosis was 66 %. The number of burrs used per lesion was 1.5, and the final burr-to-artery ratio was 0.61. Because these patients had large-diameter vessels, the burrs used were larger than those used for adult patients. The final average burr size was 2.23 mm, and the largest burr size, 2.5 mm, was used for 37 % of the lesions. All patients underwent additional post-rotablation balloon dilatation, which was performed at a relatively low average of 9.5 ATM, although some patients required dilatation at high pressure, 20 ATM. Stents were implanted in only 9 % of patients, for whom coronary artery dissection led to decreased blood flow.
Acute Outcomes
The lesion dilatation technical success rate and clinical success rate were both 100 %. The procedures were conducted quite safely, and there were no primary complications, including death, emergency bypass, Q-wave MI, or acute coronary occlusion. The incidence rate of post-dilatation balloon rupture was 8 %, and complete expansion by balloon was possible in only 35 % of cases. Minimum vessel diameter increased from a pre-procedural 1.26 mm to a post-procedural 2.57 mm, and restenosis decreased from 66 to 33 %. There were no cases of coronary perforation, no-reflow, or spasm, which are complications particular to rotablation. There was one case in which the burr became trapped in the lesion but was subsequently removed. The diamond particles on the Rotablator are only attached to the front end of the burr, so if the burr passes the lesion without sufficient cutting, it sometimes get trapped in heavily calcified stenotic areas. To avoid this, it is important to cut in several steps, starting with a small burr, and to avoid using excessive pressure when advancing the burr. In contrast to treatment of atherosclerotic lesions in adults, we found that rotablation could be performed quite safely for these young patients, most likely because KD coronary artery lesions were focal, vessel diameters were large, and tortuous lesions were uncommon. We also found that, because high-pressure balloon post-dilatation could lead to balloon rupture, it is advisable to avoid excessively high pressures and to increase burr size as necessary. In children younger than 10 years, 6-Fr is the largest sheath that can be used, so only burrs smaller than 2 mm may be used. In some cases we waited 5 years for a child to grow enough to permit use of a 10-Fr sheath and 2.5-mm burr, for re-treatment.
Late Restenosis
Follow-up angiography was performed for 33 lesions (100 %) 3–6 months post-procedure. Minimum vessel diameter was 1.25 mm pre-procedure, 2.57 mm post-procedure, and 2.32 mm in the late phase. Late restenosis (≥50 %) was noted in 9 (27 %) lesions. Restenosis occurred in 17 % of cases for which the final burr size was 2.5 mm and 33 % of cases for which the burr was less than 2.5 mm. Although the difference was not statistically significant, there was less restenosis among patients for whom the largest possible size burr was used and the greatest diameter gained.
Late lumen loss was 0.25 mm, clearly lower than that for adult elective percutaneous coronary intervention (PCI), for which average late lumen loss is 0.90–1.00 mm. Restenosis is determined by initial diameter gain and late lumen loss, the latter of which is caused by neointimal hyperplasia triggered by inflammation resulting from vessel injury. Drug-eluting stents, which are coated with a drug meant to inhibit this, have dramatically reduced post-PCI restenosis and are used in clinical settings. It may be that in KD coronary lesions, because young coronary arteries are pathologically subject to severe inflammation, both the normal media and intima structures are destroyed, and the neointimal hyperplasia caused by smooth muscle cell proliferation and migration that is seen in adult atherosclerotic lesions does not occur so easily. The late lumen loss ratio, calculated by dividing late lumen loss by initial lumen gain, is 0.4 for balloon angioplasty, 0.6 for stenting, and 0.7 for rotablation when performed on adult atherosclerotic lesions. In contrast, the ratio for Rotablator-treated KD coronary artery lesions is 0.2, almost as low as the 0.1 ratio for drug-eluting stenting in adults. Therefore, in contrast to adult patients, restenosis prevention in KD artery lesions depends greatly on initial gain; thus, it is necessary to use as large a burr as possible. Vessel diameters of 3.8 mm and comparatively large lesions are common, so even using the largest burr size of 2.5 mm, the burr-to-artery ratio is 0.6, which suggests little risk of perforation.
Catheterization was repeated in 8 (24 %) patients with restenotic lesions. Of these, 44 % underwent repeat rotablation, 22 % received stents, 33 % were treated with balloon dilatation, and 11 % were treated conservatively. No patient who underwent repeat rotablation had received treatment using the largest (2.5 mm) burr during their initial rotablation. There was no repeat restenosis after the second rotablation.
New Coronary Aneurysms in the Late Period
In follow-up angiography performed 3–6 months post-procedure on all 33 lesions (100 %), four (12 %) patients had new coronary aneurysms at the treatment site; 60 % of these occurred in lesions with sufficient post-procedural stenosis (<25 %). This proportion was significantly higher than that for lesions with post-procedural stenosis of 25 % or greater (4 %). While there were no new coronary artery aneurysms found in lesions where intravascular ultrasound revealed circumferential calcification, aneurysms did develop in lesions in which high-pressure balloon dilatation caused cracks in post-procedural circumferential calcification. Because young coronary arteries are subject to pathologically severe inflammation in KD, the normal media and intima structures are destroyed, so it is likely that dilatation force from the vessel lumen reaches the adventitia, which may trigger coronary aneurysm formation.
While we recommend using the largest possible burr, to prevent restenosis, we believe that post-dilatation should be performed at a comparatively low pressure, aiming at 30–50 % post-procedural stenosis and refraining from excessively high-pressure dilatation. Furthermore, the development of new aneurysms is a phenomenon particular to KD patients [1]. Stent use may result in late-stage stent malapposition, so stenting should be undertaken only when absolutely necessary, and limited to bail-out situations.
Long-Term Prognosis for Patients Undergoing PCI on KD Coronary Artery Lesions
We investigated long-term outcomes (follow-up period: 13 years) for initial elective PCI in 39 KD pediatric patients (44 lesions). The mean age at time of treatment was 16 years. In 37 stenotic lesions (90 %) with marked calcification near the coronary aneurysm, we performed rotablation and POBA (balloon dilatation); bare metal stents were placed in 4 lesions (10 %). The rate of reintervention for restenosis was 35 % during a period of 5 years, and most of these procedures were performed within 1 year of the initial intervention. No reinterventions were performed during years 5 through 15. These patients continued periodic follow-up during their school years and were maintained on aspirin and warfarin (in cases of residual aneurysm); almost none required repeat (non-medical) treatment for the initially treated area during adulthood. Additionally, no aneurysm progression or rupture was seen, and, as reported by Suda et al. [2], outcomes were good for giant aneurysms as well. Only two patients (5.6 %) had cardiac-vessel events in adulthood, after the 10-year mark. The first patient, who underwent stent placement at age 27 years, did not undergo regular check-ups thereafter and developed recurrent chest pain at age 38 years. A new lesion was found in a location different from that of the previously treated lesion and the patient underwent stent placement. The second patient did not undergo regular check-ups after rotablation and POBA treatment, at age 14 years, and experienced cardiopulmonary arrest during exercise, at age 25 years. The patient was rushed to the hospital, where targeted temperature management and coronary bypass saved his life. This patient also presented with a new lesion in a location different from that of the previously treated lesion.
The above findings suggest that while restenosis can occur within 1 year of PCI treatment in school-aged patients, re-treatment prognosis is good, aneurysms do not progress even as the patient enters adulthood, and lesions remain stable. However, these findings do indicate that continued antiplatelet therapy and anticoagulant therapy (in patients with aneurysms) are necessary, that new lesions appear earlier than in non-KD patients of similar age, and that medical therapy is required for more stringent atherosclerosis prevention. For these reasons it seems that ongoing medical observation, even into adulthood, is necessary. In their 30-year follow-up of 60 pediatric KD patients with a history of MI, Tsuda et al. [3] found that many patients with low cardiac function had died from life-threatening ventricular arrhythmias, which led the authors to stress the importance of rigorous control.
Summary
Catheter-based treatment of KD coronary artery lesions can be performed safely with a Rotablator, and the effects are maintained over the long-term. Furthermore, the effects were not limited to treatment of focal coronary lesions but extend over time as KD patients mature. As long as a guidewire can cross the lesion, KD coronary artery lesions should be treated with less invasive catheter treatment rather than by surgery.
References
Akagi T. Interventions in Kawasaki disease. Pediatr Cardiol. 2005;26(2):206–12. http://dx.doi.org/10.1007/s00246-004-0964-2. PMID:15868317.
Suda K, Iemura M, Nishiono H, Teramachi Y, Koteda Y, Kishimoto S, et al. Long-term prognosis of patients with Kawasaki disease complicated by giant coronary aneurysms: a single-institution experience. Circulation. 2011;123(17):1836–42. http://dx.doi.org/10.1161/CIRCULATIONAHA.110.978213. PMID:21502578.
Tsuda E, Hirata T, Matsuo O, Abe T, Sugiyama H, Yamada O. The 30-year outcome for patients after myocardial infarction due to coronary artery lesions caused by Kawasaki disease. Pediatr Cardiol. 2011;32(2):176–82. http://dx.doi.org/10.1007/s00246-010-9838-y. PMID:21120463.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Japan
About this chapter
Cite this chapter
Yokoi, H. (2017). Long-Term Clinical Follow-Up After Rotational Atherectomy for Coronary Arterial Stenosis in Kawasaki Disease. In: Saji, B., Newburger, J., Burns, J., Takahashi, M. (eds) Kawasaki Disease. Springer, Tokyo. https://doi.org/10.1007/978-4-431-56039-5_41
Download citation
DOI: https://doi.org/10.1007/978-4-431-56039-5_41
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-56037-1
Online ISBN: 978-4-431-56039-5
eBook Packages: MedicineMedicine (R0)