Abstract
Investigation for motor system by magnetoencephalographic (MEG) recordings has focused on detecting the primary motor area. In order to collect data with high S/N ratio, selection of a motor paradigm and an analysis method to assure events time-locked to movement onset is important. Self-paced movement paradigm has been widely employed, because the same paradigm in electroencephalographic (EEG) and subdural recordings has provided bunch of physiological data. The motor field (MF) component in movement-related cortical magnetic fields (MRCFs) is believed to reflect the final stage of motor execution in MI. Frequency analysis on the background rhythm related to movement can be also utilized to estimate motor-related areas.
Considering the difficulties in performing the self-paced movement, easier motor paradigms such as isometric contraction or cyclic repetitive movements have been recently introduced. Although estimated sources from these paradigms have provided sources of reasonable locations, physiological significance should await for further study.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Movement-related cortical magnetic fields (MRCFs)
- Self-paced movement
- Frequency analysis
- Event-related desynchronization (ERD)/event-related synchronization (ERS)
- Coherence
1 Basic Principles and Physiology (Fig. 2.1)
1.1 Movement and Posture
The whole range of motor functions from voluntarily initiated precise grasping to reflexive reactions can be mainly characterized through a description of the temporal change of coordinates in space for each part of the body or the whole body. Each bodily motion is governed by muscle contraction, even if the body part keeps still in space, the placement of which is ruled by the motor system. These muscle contractions are without exception regulated by motor neurons situated in the anterior horn in the spinal cord or brainstem motor nucleus. The route originating from the motor neurons to a muscle is named the final common pathway, which receives various kinds of inputs from central sources.
Movement and posture are the two main features of motor function, whose space coordinates change and remain unchanged, respectively. As individuals, we can be vividly aware of our own movement, but we are rarely conscious of our posture.
1.2 Movement
Movement is categorized into three kinds of bodily motions: voluntary movement, automatic movement, and reflex.
Voluntary movement is a goal-directed behavior launched by volition and is generated by the cerebral cortex with associated activation of basal ganglia and the cerebellum.
Automatic movement is characterized by a stereotyped rhythmic movement with recursive elements, such as swallowing and walking. It is believed that a neural circuit called the “central pattern generator” exists in the spinal cord or brainstem to generate automatic movement.
Reflex is a stereotyped movement occurring unconsciously and caused by a specific stimulus. The relevant reflex center sits in the spinal cord or brainstem.
1.3 Voluntary Movement
Voluntary movement is initiated by volition and requires several steps, including, preparation, initiation, maintenance, and termination. Among these, the initiation step is represented by an abrupt change from the preceding resting position, which is usually caused by a drastic increase in activity in the primary motor area (MI). This change is projected to the periphery through the corticospinal or corticobulbar tract.
1.4 Involuntary Movements
Unwanted movements unsuitable for the conditions of body parts are a manifestation of disorders of motor control and categorized as involuntary movements. The site responsible in the nervous system spreads over various sites from peripheral to central areas, including the cerebral cortex.
2 Clinical Applications
2.1 Physiological Investigation of Control of Movement and Posture
For detecting electrical activity in cortical areas, self-paced movement has been commonly recorded using an EEG [1, 2]. Waveforms obtained using this approach are called movement-related cortical potentials (MRCPs). Various generators have been clarified by investigations with scalp recordings [3, 4] and subdural recordings [5, 6]. Following on from these recordings, the same approach has been adopted since the early era of magnetoencephalographic (MEG) recordings [7–12] to acquire movement-related cortical magnetic fields (MRCFs).
Compared with the investigation of sensory systems, the temporal sequence of neural activities related to motor function is not as well correlated with events visible to observers. In order to achieve the best possible MEG signals, short brisk movements are utilized to evoke alterations in brain activity correlated with movement onset.
Empirically, neural activities in the lower levels are more closely correlated with the onset of movement than those in higher levels. However, the detection of motor-related activities of spinal motor neurons or brainstem motor neurons is difficult because they do not produce large magnetic fields owing to their anatomical alignment, although they are tightly linked to the electromyography (EMG) activities in the temporal domain. Therefore, cortical activities in the MI, which are tightly linked to EMG activities after spinal motor neurons, are considered to be the best targets for MEG investigation. This tight connection between cortex and muscle activity is strengthened if we focus on the initiation of brisk movement, because rapid firing of pyramidal cells in the MI area becomes apparent.
At the termination stage of voluntary movement, a similar but opposite phenomenon must be happening. However, the tail-off of muscle activity is not so abrupt as to allow alignment of times across trials; therefore, few studies have explored this stage [13]. During the maintenance stage of voluntary movement, although there may be some continuing neural activities so as to maintain connection between cortical and muscular activities, they cannot be detected because they are only sustained for a rather short period in the case of voluntary movement.
If this maintenance stage of voluntary movement becomes elongated, it can be regarded as posture maintenance, which enables us to obtain a clear signal as for the correlation between cortex and muscle using coherence analysis (see Sect. 2.6.3).
2.2 Generator Sources for Involuntary Movement
In addition to physiological surveys of motor control, we can detect sources for some types of involuntary movements, if the generator responsible is situated in a limited area of the cerebral cortex. Because some types of cortical myoclonus are characterized by brisk contraction of the small body part, it is likely that the lesion responsible should be located in the cerebral cortex, which has been proven by several reports using jerk-locked back averaging [14–18]. There are reports dealing with non-cortical lesions in patients with tremor [19] and widespread lesions responsible in a patient with subacute sclerosing panencephalitis [20], although their relevant cortical lesions were not clearly demonstrated.
3 Principal Analysis Methods (Fig. 2.2)
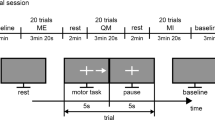
The self-paced movement method has been widely adopted. Subjects are requested to move their finger, hand, or foot on one side with intervals exceeding several seconds. Subjects should make a brisk and short contraction and keep still in between the movements. In order to delineate somatotopic organization, a distal part of a limb is often used.
Since some subjects experience difficulties in deciding when they have to move because of the long interval requested for this self-paced movement, some centers use assistance to indicate when movements should start. Delivery of cue signals such as a tone or light with intervals of several seconds can persuade subjects to start movement. Intervals can be either fixed or randomly assigned, and subjects do not have to be so strict in performing rapid responses.
Contingent negative variation (CNV) is a famous and well-utilized task in the investigation of motor control. A pair of stimuli (S1 and S2) with an interval of around 2 s serve as a warning and imperative stimuli, and they are repeated with an interval of 3–5 s between the stimulus pair. A time interval of 2 s between S1 and S2 is appropriate for subjects to predict the timing of S2, so subjects have to respond as soon as possible.
Isometric contraction maintained for longer than several seconds can be regarded as a task focusing the maintenance stage of voluntary movement. In order to verify the constant condition of muscle contraction, it is useful to employ some visual feedback or give guidance to adjust contraction.
Because conventional self-paced movements with a long interval are not easy for some subjects, rapid rate or short interval movement can be utilized. Repetitions of brisk movement up to 1–2-Hz can leave a rather silent period of muscle activity in between the repetitions.
Rhythmic and cyclic movement is similar but different from this rapid rate movement. Back-and-forth motion of 2–4 Hz does not leave an EMG silent period, allowing an assumption that it can mimic a sinusoidal profile, and coherence analysis between EMG and brain activity can be applied assuming brain activities also share a cyclic temporal sequence.
4 Recording and Analysis of Self-Paced Movement
4.1 Preparation
Besides usual preparations for MEG recording, it is important to ensure detection of alterations in motor output of the target body part. Selection of appropriate muscles and movements and methods varies across experiments. Surface EMG over the target muscle with cup electrodes is the most commonly used method. Electrodes can be placed on any part of the body and can be applied not only for recordings of movement but also for posture. Button pressing with a natural return designed without causing magnetic noise can be adopted. Light-emitting diodes are also utilized to check displacement of body parts. Adjustment of the allowance from the operating point is critical to define the time point to determine the initiation of movement.
Equally important is confirming the stillness of other body parts at other times except for the intended movement. For this purpose, EMG electrodes are placed on some body parts other than the target muscle, including the contralateral side.
Examiners should check the magnetic environment before actual measurement starts. When we find slow magnetic fluctuation, asking the subject to hold their breath is of help to check. Sometimes buttons on clothes or dental implants can cause magnetic noise. Screening conditions during the performance of an actual assessment is essential. Magnetized materials often cause large magnetic noise even if the movement is tiny. Putting a cushion under the return of a moving platform is useful to avoid noise caused by touchdown by the moving object. EMG cables should be fixed at several points so that they do not swing.
Eye movement can significantly distort the magnetic field related to movement, because its temporal profile is similar to movement. It is useful to set a visual target to which subjects are requested to fix their vision in order to avoid eye movement. Electrooculogram (EOG) monitoring is strongly advised.
4.2 Recording Procedure
Before introducing subjects into a magnetically shielded room, recording baseline condition of magnetic fields without the subject is recommended (empty-room measurement). This data can be used for confirmation of background noise, essential data for noise reduction filters, and uncovering overlooked magnetic materials attached to the subject. Data acquisition parameters for MEG signals require a sampling rate of at least 500 Hz, with a band-pass filter set between 0.1 and 100 Hz. Depending on the necessity for detecting slow magnetic fields preceding movement, a high-pass filter can be widened to 0.03 Hz or narrowed to 1 Hz. When putting subjects adjusted to the MEG sensor, the examiner should check that subject’s head fits well around the sensorimotor area.
As for data collection, if an examiner sets an electronic pulse for averaging, it is possible to get only averaged data utilizing an automatic noise cancelation system to avoid large signals, including eye movement. It would also be useful to accumulate repetition-time segmented waveforms during the predetermined analysis time window. However, with these methods, we cannot properly exclude trials including unwanted noise segments. Therefore, it would be preferable to save all the continuous data including EMG, EOG, and trigger pulse.
Fifty to 100 repetitions of a movement are required to obtain averaged waveforms with a reasonable S/N ratio. Considering artifact rejection to exclude trials with contaminating noises, two or three sessions each with 30–50 movements are advised. Averaging procedures can be done either online or off-line. In case of recording continuous data and leaving final analysis to be done off-line, it would be preferable to obtain online averages to check recording conditions.
Because the task is rather simple and repetitive, adequate rest periods should be provided once the movement has been repeated 30–50 times. After a break, recording the head position with respect to the dewar should be done, because subjects tend to change their head position during the rest period.
4.3 Analysis
4.3.1 Trigger Point
Because MRCF aims to explore temporal changes in brain activity, an average across a certain number of repetitions of the movement is the first step. If continuous data is going to be processed, EMG onset should be visually tagged from continuous data. If the background EMG level serving as the resting condition becomes noisy, the triggering point may fluctuate. In this case, exclusion of data from the time period with increased EMG background from averaging could be considered.
4.3.2 Averaging Window
For off-line analysis, the time window for averaging can be adjusted by taking the shortest interval between two successive movements within the session. If the interval is short compared with the intended time window, the trials with a short interval should be excluded from the average. Depending on the purpose, settings for premovement and postmovement time periods vary from 2–4 s to 1–2 s, respectively. This assignment should be determined carefully, as the first 10–20 % of the total analysis window is usually assigned for the baseline period for amplitude calculation. Confirmation of reproducibility by superimposition of two different sessions can provide insight for contamination by noise elements. If these sets of averages show similarities, the sessions can be averaged to obtain group average waveforms to be used for further analysis.
4.3.3 Components of MRCF: (Figs. 2.3 and 2.4)
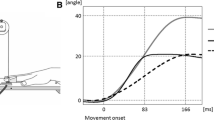
Sample movement-related cortical magnetic fields (MRCFs) after self-paced extension of the right middle finger. Upper panel: Magnetometer waveform over the left central area, low-pass filter set at 30 Hz and high-pass filter at 0.03 Hz, with a sampling rate of 603 Hz. Lower panel: Average of high-pass filter (1 Hz) and rectified electromyography (EMG) of the right extensor digitorum communis muscle. Open triangle: EMG onset. Solid triangle: readiness field (RF) onset
The components of MRCF have usually been named in accordance with Kristeva et al. [21]. The readiness field (RF) shown over the central area contralateral to the moving side corresponds to the first slow increasing magnetic activity prior to movement onset. The onset of RF is approximately several hundred milliseconds before movement onset, and it is usually later than the initiation of the slow EEG component starting 2–3 s before onset. This EEG component, Bereitschaftspotential (BP), is bilaterally distributed, and is followed by NS’ in the EEG starting several hundred milliseconds before movement onset, which is dominant over the contralateral side [3]. Taken together, it is most likely that the RF component is a counterpart of NS’ or BP2 rather than BP or BP1. This RF activity shows a peak around the onset of movement, and this is called the motor field (MF). It is considered that this is equivalent to motor potential (MP) in EEG recordings, which is sometimes clearly differentiated from the preceding slow cortical potential of NS’ or BP2 [22]. However, it is rare to encounter a prominent MF component emerging on top of the preceding RF. Hence, it is difficult to use these two terms differently, especially for the analysis for generator sources. Because RF is characterized by its onset time, it is advised to use in the temporal domain; how early this component appears etc. On the other hand, MF is better for use in cases of source localization. Following MF, a peak in the opposite direction at approximately 100 ms after EMG onset is noted as movement-evoked field I (MEFI) and the following peak at about 200 ms corresponds to movement-evoked field II (MEFII).
4.3.4 Source Analysis with an Equivalent Current Dipole Model
For resolving the sources for intracranial sources for each component of MRCF, equivalent current dipole (ECD) assumption is widely used. At the MF, around 30 sensors covering the field extrema of opposing influx and efflux are sufficient to localize the ECD, whereas a smaller number of sensor locations with planar gradiometers centering on the field extrema are required for analysis. Compared with the prominent peak of N20m in somatosensory evoked fields, accepting a threshold of parameters indicating a correlation between observed and those estimated hypothetically can be set to a lower value for reliable ECDs. Correlation coefficients of 0.90–0.95 or goodness of fit of 0.80–0.90 are acceptable (Fig. 2.5).
Source location estimated by the assumption of a single dipole source, at 6 ms before the movement onset taken from the same data as Fig. 2.3. (a) Contour map and approximate source location. Red indicates an outward magnetic field and blue indicates an inward field. (b) Estimated current dipole location projected onto the subject’s own magnetic resonance imaging (MRI); the circle indicates the dipole location and the bar indicates the dipole orientation. A yellow triangle indicates the left central sulcus
Because slow magnetic artifacts largely distort the background baseline level, it can be reasonable to localize the MF component by setting a high-pass filter around 0.1 Hz at the expense of detecting the RF component [23]. Exploration with multiple generator sources has been performed using BESA [23, 24]. The MEFI component was located posterior to the central sulcus and may be different from N20m of the SEF [25, 26].
4.3.5 Spatial Filter
In modeling the source of MEG signals, the motor system can be a good target to introduce a spatial filter assuming sources are distributed within a certain volume or on a surface. Utilization of L1 minimum norm (minimum current estimate [MCE] [27]) or L2 minimum norm estimates (MNEs [28]) can be adopted, because we can start by making a minimum of assumptions. An example using MNE is shown in Fig. 2.6. These analytical methods do not require a priori information concerning the source structures. Spatial filters optimized to pass activity from a specific brain areas suppressing activity from other areas are called beamformers and can present narrower source distribution [29].
Source distribution by spatial filter (minimum norm estimate) projected onto the subject’s own MRI, 6 ms before the movement onset, taken from the same subject as Figs. 2.3 and 2.5. Pixels with an F-value threshold of 40 calculated from the baseline power are shown. Red areas indicates higher power than blue areas. A yellow triangle indicates the left central sulcus
5 Contingent Negative Variation
In EEG investigations, CNV is another well-known approach for surveying motor control, especially sensorimotor integration [30]. Using the same method, several MEG attempts have been reported. They demonstrated MI activity following the S2 time period [31–35]. As for the researcher recording using subdural electrodes, few reports have dealt with this sensorimotor integration [36]. This report demonstrated the involvement of areas other than the MI, whereas reports of conventional self-paced movement demonstrated activation of a rather restricted area of the MI. Therefore, source analysis as for CNV is required, and single ECD assumption may fail to provide an accurate location for the MI.
6 Advanced Techniques
6.1 Event-Related Desynchronization/Event-Related Synchronization
In the activities related to motor function, mu rhythm has been widely observed in routine EEG recordings [37]. Pfurtscheller’s group developed a method for the study of temporal changes in power in the EEG background oscillatory rhythm [38, 39]. Power decrease in alpha or beta bands in association with movement onset or a certain task was named event-related desynchronization (ERD) and was considered to indicate increased cortical excitability. The opposite phenomenon of a power increase was termed event-related synchronization (ERS), and this was believed to be related to decreased excitability (Fig. 2.7). Salmelin introduced this method to MEG by keeping the analysis time bin the same as that of the sampling rate, by adopting the name of temporal spatial evolution [40].
Time–frequency analysis. (a) Time–frequency representation of gradiometer activity over the left central area related to self-paced extension of the right middle finger (same data source as in Figs. 2.3, 2.5, and 2.6). Note event-related desynchronization (ERD) in the alpha to beta band starts around 2 s before movement onset, whereas beta frequency event-related synchronization (ERS) occurs 6–700 ms after movement onset. (b) Projection of the ERD source distribution at 12 Hz, 100 ms before movement onset, using a minimum norm estimate spatial filter. A yellow triangle indicates the left central sulcus
This analysis revealed other aspects of brain activity other than slow components. Usually, the RF of a slow magnetic shift precedes the movement by several hundred milliseconds, and ERD already starts 3 s before the onset [41]. This clear contrast between the slow and background activities indicate that these two components manifest completely different physiological events.
6.2 Rapid Rate Movement
Self-paced movement methods have been regarded as the standard approach to detect the MI. However, because this approach requires several task regulations such as control of eye movement, brisk movement, and keeping relaxed muscles between the movements, some subjects cannot perform the task properly. In order to overcome this situation, methods with self-paced movement with shorter intervals have been introduced [42]. Because only a short time period of around 400 ms can be left as a baseline for amplitude measurement in the case of 2-Hz repetitive movements, a time period of 500 ms was introduced for baseline measurement. Because of its steadiness, this baseline period can be achieved by more subjects.
6.3 Corticomuscular Coherence (CMC)
Recent EEG studies of coherence between EEG and EMG showed corticomuscular oscillatory relations in humans [43–47] as well as in monkeys [48]. In a human MEG study, Salenius et al. demonstrated increased coherence in the frequency range of 15 ± 33 Hz between MEG signals from the primary sensorimotor cortex [44]. This activity was suppressed temporarily by transient ischemic sensory deafferentation [49] but regained its strength after the end of ischemia, indicating that sensory feedback is not essential for coherence.
This procedure enables researchers to examine speech [50] and tongue movement [51]. Because this method is easier compared with conventional self-paced movement especially for patients, this can be used extensively in clinical situations.
The source-level analysis of CMC is achieved either by using cross-correlogram [44] or by DICS [52] (Fig. 2.8).
Corticomuscular coherence analysis of right middle finger tonic extension. (a) Amplitude squared coherence between high-pass filtered (1 Hz) and rectified electromyography (EMG) and gradiometer over the left central area. A horizontal broken line indicates the 95 % confidence level. (b) Correlogram calculated by inverse Fourier transformation of the cross-spectra of the same data. A solid triangle indicates gradiometer activity precedes EMG by about 5 ms. (c) Contour map and approximate source location of correlogram activity at 5 ms time lead. (d) Estimated current dipole location projected onto the subject’s own MRI. (e) Source distribution of the coherent source by spatial filter (minimum norm estimate) projected onto the subject’s own MRI, 26 Hz, threshold set at the 95 % confidence level. A yellow triangle indicates the left central sulcus
6.4 Corticokinematic Coherence (CKC) [53]
Following the method of rapid rate movements, which still leaves silent period for EMG, repetitions of flexion-extensions of a body part produce steady-state movements without showing silent EMG activity. Bourguignon’s group developed a new method using a three-axis accelerometer that attaches to a finger, and subjects were instructed to make cyclic movements at a pace of 3 Hz. Cross-correlogram and coherence spectra demonstrated increased coherence at a driving frequency of 3 Hz and its harmonic frequency. The coherence was statistically significant with sources in the MI area close to the area representing the corresponding body part. Because this method is easy and straightforward for recording, it will become an easy and robust approach for MI surveys (Fig. 2.9).
Corticokinematic coherence. Magnetic field activities and accelerometer signals were measured with a bandpass of 0.1–300 Hz and sampled at 1012 Hz, while the subject performed repetitive flexion-extension of the left toe at 2 Hz. (a) Coherence between the central planar gradiometer sensor and accelerogram. Horizontal axis: frequency from 0 to 10 Hz, Vertical axis: coherence. There are two coherence peaks of 0.07 at 2 Hz and 0.2 at 4 Hz. (b) Cross-correlogram (c) Source estimated from the cross-correlogram at a peak of −74 ms (Courtesy of Dr Hidekazu Saito)
7 Future Directions
Without doubt, the most important target for clinical MEG of the motor system is to delineate the MI. Using these new techniques that utilize coherence, success rates for localizing the MI area have improved. However, compared with investigations for other systems, such as somatosensory systems, sampling a sufficient number of averages is not so easy owing to the difficulty to executing motor analyses, especially in patients. Physiological meaning for solutions obtained from these new techniques is to be clarified also.
For physiological investigations, analysis of the separation between the MI and non-primary motor areas is awaited. This development may be accomplished not only by analytical procedures, but these require advancements in hardware capable of higher spatial resolution.
References
Bates JA. Electrical activity of the cortex accompanying movement. J Physiol. 1951;113(2–3):240–57.
Kornhuber HH, Deecke L. Changes in the brain potential in voluntary movements and passive movements in man: readiness potential and reafferent potentials. Pflugers Arch Gesamten Physiol Menschen Tiere. 1965;284:1–17.
Shibasaki H, Barrett G, Halliday E, Halliday AM. Components of the movement-related cortical potential and their scalp topography. Electroencephalogr Clin Neurophysiol. 1980;49(3–4):213–26.
Vaughan Jr HG, Costa LD, Ritter W. Topography of the human motor potential. Electroencephalogr Clin Neurophysiol. 1968;25(1):1–10.
Ikeda A, Luders HO, Burgess RC, Shibasaki H. Movement-related potentials recorded from supplementary motor area and primary motor area. Role of supplementary motor area in voluntary movements. Brain: J Neurol. 1992;115(Pt 4):1017–43.
Neshige R, Luders H, Shibasaki H. Recording of movement-related potentials from scalp and cortex in man. Brain: J Neurol. 1988;111(Pt 3):719–36.
Deecke L, Boschert J, Weinberg H, Brickett P. Magnetic fields of the human brain (Bereitschaftsmagnetfeld) preceding voluntary foot and toe movements. Exp Brain Res. 1983;52(1):81–6.
Antervo A, Hari R, Katila T, Poutanen T, Seppanen M, Tuomisto T. Cerebral magnetic fields preceding self-paced plantar flexions of the foot. Acta Neurol Scand. 1983;68(4):213–7.
Hari R, Antervo A, Salmi T. Slow EEG potentials preceding self-paced plantar flexions of hand and foot. Acta Physiol Scand. 1983;119(1):55–9. doi:10.1111/j.1748-1716.1983.tb07305.x.
Cheyne D, Weinberg H. Neuromagnetic fields accompanying unilateral finger movements: pre-movement and movement-evoked fields. Exp Brain Res. 1989;78(3):604–12.
Kristeva-Feige R, Walter H, Lutkenhoner B, Hampson S, Ross B, Knorr U, Steinmetz H, Cheyne D. A neuromagnetic study of the functional organization of the sensorimotor cortex. Eur J Neurosci. 1994;6(4):632–9.
Nagamine T, Toro C, Balish M, Deuschl G, Wang B, Sato S, Shibasaki H, Hallett M. Cortical magnetic and electric fields associated with voluntary finger movements. Brain Topogr. 1994;6(3):175–83.
Toma K, Nagamine T, Yazawa S, Terada K, Ikeda A, Honda M, Oga T, Shibasaki H. Desynchronization and synchronization of central 20-Hz rhythms associated with voluntary muscle relaxation: a magnetoencephalographic study. Exp Brain Res. 2000;134(4):417–25. doi:10.1007/s002210000483.
Ugawa Y, Uesaka Y, Terao Y, Yumoto M, Hnajima R, Sakai K. Pathophysiology of sensorimotor cortex in cortical myoclonus. Clin Neurosci. 1995;3(4):198–202.
Mima T, Nagamine T, Ikeda A, Yazawa S, Kimura J, Shibasaki H. Pathogenesis of cortical myoclonus studied by magnetoencephalography. Ann Neurol. 1998;43(5):598–607. doi:10.1002/ana.410430507.
Timmermann L, Gross J, Schmitz F, Freund HJ, Schnitzler A. Involvement of the motor cortex in pseudochoreoathetosis. Mov Disord: Off J Mov Disord Soc. 2001;16(5):876–81.
Sudmeyer M, Pollok B, Hefter H, Gross J, Wojtecki L, Butz M, Timmermann L, Schnitzler A. Postural tremor in Wilson’s disease: a magnetoencephalographic study. Mov Disord: Off J Mov Disord Soc. 2004;19(12):1476–82. doi:10.1002/mds.20240.
Butz M, Timmermann L, Gross J, Pollok B, Sudmeyer M, Kircheis G, Haussinger D, Schnitzler A. Cortical activation associated with asterixis in manifest hepatic encephalopathy. Acta Neurol Scand. 2014;130(4):260–7. doi:10.1111/ane.12217.
Volkmann J, Joliot M, Mogilner A, Ioannides AA, Lado F, Fazzini E, Ribary U, Llinas R. Central motor loop oscillations in parkinsonian resting tremor revealed by magnetoencephalography. Neurology. 1996;46(5):1359–70.
Oga T, Ikeda A, Nagamine T, Sumi E, Matsumoto R, Akiguchi I, Kimura J, Shibasaki H. Implication of sensorimotor integration in the generation of periodic dystonic myoclonus in subacute sclerosing panencephalitis (SSPE). Mov Disord: Off J Mov Disord Soc. 2000;15(6):1173–83.
Kristeva R, Cheyne D, Deecke L. Neuromagnetic fields accompanying unilateral and bilateral voluntary movements: topography and analysis of cortical sources. Electroencephalogr Clin Neurophysiol. 1991;81(4):284–98.
Shibasaki H, Hallett M. What is the Bereitschaftspotential? Clin Neurophysiol: Off J Int Fed Clin Neurophysiol. 2006;117(11):2341–56. doi:10.1016/j.clinph.2006.04.025.
Hoshiyama M, Kakigi R, Berg P, Koyama S, Kitamura Y, Shimojo M, Watanabe S, Nakamura A. Identification of motor and sensory brain activities during unilateral finger movement: spatiotemporal source analysis of movement-associated magnetic fields. Exp Brain Res. 1997;115(1):6–14.
Onishi H, Sugawara K, Yamashiro K, Sato D, Suzuki M, Kirimoto H, Tamaki H, Murakami H, Kameyama S. Neuromagnetic activation following active and passive finger movements. Brain Behav. 2013;3(2):178–92. doi:10.1002/brb3.126.
Niimi M, Ohira T, Akiyama T, Hiraga K, Kaneko Y, Ochiai M, Fukunaga A, Kobayashi M, Kawase T. Source analysis of the magnetic field evoked during self-paced finger movements. Neurol Res. 2008;30(3):239–43. doi:10.1179/016164107X230801.
Weinberg H, Cheyne D, Crisp D. Electroencephalographic and magnetoencephalographic studies of motor function. Adv Neurol. 1990;54:193–205.
Uutela K, Hamalainen M, Somersalo E. Visualization of magnetoencephalographic data using minimum current estimates. NeuroImage. 1999;10(2):173–80. doi:10.1006/nimg.1999.0454.
Hamalainen MS, Ilmoniemi RJ. Interpreting magnetic fields of the brain: minimum norm estimates. Med Biol Eng Comput. 1994;32(1):35–42.
Hillebrand A, Barnes GR. Beamformer analysis of MEG data. Int Rev Neurobiol. 2005;68:149–71. doi:10.1016/S0074-7742(05)68006-3.
Walter WG. The contingent negative variation: an electro-cortical sign of sensori-motor reflex association in man. Prog Brain Res. 1968;22:364–77. doi:10.1016/S0079-6123(08)63519-0.
Basile LF, Rogers RL, Bourbon WT, Papanicolaou AC. Slow magnetic flux from human frontal cortex. Electroencephalogr Clin Neurophysiol. 1994;90(2):157–65.
Elbert T, Rockstroh B, Hampson S, Pantev C, Hoke M. The magnetic counterpart of the contingent negative variation. Electroencephalogr Clin Neurophysiol. 1994;92(3):262–72.
Hultin L, Rossini P, Romani GL, Hogstedt P, Tecchio F, Pizzella V. Neuromagnetic localization of the late component of the contingent negative variation. Electroencephalogr Clin Neurophysiol. 1996;98(6):435–48.
Gomez CM, Fernandez A, Maestu F, Amo C, Gonzalez-Rosa JJ, Vaquero E, Ortiz T. Task-specific sensory and motor preparatory activation revealed by contingent magnetic variation. Brain Res Cogn Brain Res. 2004;21(1):59–68. doi:10.1016/j.cogbrainres.2004.05.005.
Babiloni C, Brancucci A, Pizzella V, Romani GL, Tecchio F, Torquati K, Zappasodi F, Arendt-Nielsen L, Chen AC, Rossini PM. Contingent negative variation in the parasylvian cortex increases during expectancy of painful sensorimotor events: a magnetoencephalographic study. Behav Neurosci. 2005;119(2):491–502. doi:10.1037/0735-7044.119.2.491.
Matsumoto R, Ikeda A, Ohara S, Matsuhashi M, Baba K, Yamane F, Hori T, Mihara T, Nagamine T, Shibasaki H. Motor-related functional subdivisions of human lateral premotor cortex: epicortical recording in conditional visuomotor task. Clin Neurophysiol: Off J Int Fed Clin Neurophysiol. 2003;114(6):1102–15.
Chatrian GE, Petersen MC, Lazarte JA. The blocking of the rolandic wicket rhythm and some central changes related to movement. Electroencephalogr Clin Neurophysiol. 1959;11(3):497–510.
Pfurtscheller G, Aranibar A. Event-related cortical desynchronization detected by power measurements of scalp EEG. Electroencephalogr Clin Neurophysiol. 1977;42(6):817–26.
Pfurtscheller G, Lopes da Silva FH. Event-related EEG/MEG synchronization and desynchronization: basic principles. Clin Neurophysiol: Off J Int Fed Clin Neurophysiol. 1999;110(11):1842–57.
Salmelin R, Hari R. Spatiotemporal characteristics of sensorimotor neuromagnetic rhythms related to thumb movement. Neuroscience. 1994;60(2):537–50.
Nagamine T, Kajola M, Salmelin R, Shibasaki H, Hari R. Movement-related slow cortical magnetic fields and changes of spontaneous MEG- and EEG-brain rhythms. Electroencephalogr Clin Neurophysiol. 1996;99(3):274–86.
Gerloff C, Uenishi N, Nagamine T, Kunieda T, Hallett M, Shibasaki H. Cortical activation during fast repetitive finger movements in humans: steady-state movement-related magnetic fields and their cortical generators. Electroencephalogr Clin Neurophysiol. 1998;109(5):444–53.
Conway BA, Halliday DM, Farmer SF, Shahani U, Maas P, Weir AI, Rosenberg JR. Synchronization between motor cortex and spinal motoneuronal pool during the performance of a maintained motor task in man. J Physiol. 1995;489(Pt 3):917–24.
Salenius S, Portin K, Kajola M, Salmelin R, Hari R. Cortical control of human motoneuron firing during isometric contraction. J Neurophysiol. 1997;77(6):3401–5.
Salenius S, Salmelin R, Neuper C, Pfurtscheller G, Hari R. Human cortical 40 Hz rhythm is closely related to EMG rhythmicity. Neurosci Lett. 1996;213(2):75–8.
Brown P, Salenius S, Rothwell JC, Hari R. Cortical correlate of the Piper rhythm in humans. J Neurophysiol. 1998;80(6):2911–7.
Halliday DM, Conway BA, Farmer SF, Rosenberg JR. Using electroencephalography to study functional coupling between cortical activity and electromyograms during voluntary contractions in humans. Neurosci Lett. 1998;241(1):5–8.
Baker SN, Olivier E, Lemon RN. Coherent oscillations in monkey motor cortex and hand muscle EMG show task-dependent modulation. J Physiol. 1997;501(Pt 1):225–41.
Pohja M, Salenius S. Modulation of cortex-muscle oscillatory interaction by ischaemia-induced deafferentation. Neuroreport. 2003;14(3):321–4. doi:10.1097/01.wnr.0000058518.74643.96.
Ruspantini I, Saarinen T, Belardinelli P, Jalava A, Parviainen T, Kujala J, Salmelin R. Corticomuscular coherence is tuned to the spontaneous rhythmicity of speech at 2–3 Hz. J Neurosci: Off J Soc Neurosci. 2012;32(11):3786–90. doi:10.1523/JNEUROSCI.3191-11.2012.
Maezawa H, Mima T, Yazawa S, Matsuhashi M, Shiraishi H, Hirai Y, Funahashi M. Contralateral dominance of corticomuscular coherence for both sides of the tongue during human tongue protrusion: an MEG study. NeuroImage. 2014;101:245–55. doi:10.1016/j.neuroimage.2014.07.018.
Gross J, Kujala J, Hamalainen M, Timmermann L, Schnitzler A, Salmelin R. Dynamic imaging of coherent sources: studying neural interactions in the human brain. Proc Natl Acad Sci U S A. 2001;98(2):694–9. doi:10.1073/pnas.98.2.694.
Bourguignon M, De Tiege X, Op de Beeck M, Pirotte B, Van Bogaert P, Goldman S, Hari R, Jousmaki V. Functional motor-cortex mapping using corticokinematic coherence. NeuroImage. 2011;55(4):1475–9. doi:10.1016/j.neuroimage.2011.01.031.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Japan
About this chapter
Cite this chapter
Nagamine, T., Matsuhashi, M. (2016). Basic Functions and Clinical Applications. In: Tobimatsu, S., Kakigi, R. (eds) Clinical Applications of Magnetoencephalography. Springer, Tokyo. https://doi.org/10.1007/978-4-431-55729-6_2
Download citation
DOI: https://doi.org/10.1007/978-4-431-55729-6_2
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-55728-9
Online ISBN: 978-4-431-55729-6
eBook Packages: MedicineMedicine (R0)