Abstract
Coronary angioscopy or cardioscopy using biocompatible markers is one choice for evaluation of tissues, cells, or molecules which comprise the target lesions. Angioscopy using EB as a biomarker, namely, dye-staining angioscopy, has been developed and applied for molecular imaging of the substances that constitute atherosclerotic lesions.
By dye-staining angioscopy, coronary endothelial damage can be visualized. This technique could also provide discrimination of coronary fibrin from platelets and visualization of transparent fibrin thrombi, namely, a structure that was not visible by conventional angioscopy in patients with acute coronary syndrome (ACS). Fluffy coronary luminal surface without significant stenosis nor obstructive thrombus can be observed in patients with ACS.
Following percutaneous coronary intervention, this dye-staining angioscopy could detect damaged endothelial cells on coronary stent struts in chronic phase and evaluate characterization of band and web formation on the edges of coronary stents.
Dye-staining cardioscopy enabled visualization of blood flow through the subendocardial microvessels or myocardial tissue fluid flow. This technique is useful for evaluation of the effects of coronary interventions or angiogenic therapy on coronary microcirculation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Conventional coronary angioscopy (AS) has been proven to be more useful for evaluation of coronary plaque and thrombus than angiography. Also, cardioscopy (CS) has been proven to be more useful for the detection of intracardiac thrombi and myocardial diseases than ventriculography. However, visible light is used, both imaging modalities are limited to evaluate surface morphology and color of the target lesions, and therefore, it is beyond the scope for them to evaluate the compositions of the target lesions.
Coronary AS or CS using biocompatible markers is one choice for evaluation of tissues, cells, or molecules which comprise the target lesions.
In 1995, Uchida Y and his colleagues developed dye-staining angioscopy and applied it clinically to observation of the peripheral arteries using Evans blue (EB), which was used clinically for measurement of cardiac output and tissue permeability, as a biomarker for imaging fibrin and damaged endothelial cells [1]. They applied this imaging technique for evaluation of coronary, pulmonary, and aortic lesions in patients [2–9].
They also established dye-staining CS for examination of myocardial microcirculation using EB or fluorescein in patients [10, 11]. This article describes details of these novel imaging techniques.
2 Dye-Staining Coronary Angioscopy (AS)
2.1 Coronary AS Systems
Two AS systems were used by the present authors.
One AS system is composed of a light source (CTV-A, Olympus Corporation, Tokyo, Japan); a 5-F balloon guiding catheter with three channels, one for 0.5 mm fiberscope (AF-5, Olympus Company, Tokyo, Japan), one for 0.014 guidewire, and the remaining one for saline flush (Clinical Supply Co, Gifu, Japan); and color charge-coupled device (CCD) camera (OTV-A, Olympus Co) (Fig. 3.1a). Other AS system is composed of a light source, same as that described above, an angioscope of monorail type (VecMover, Clinical Supply Co), and a color (CCD) camera (CSVEC-10, Clinical Supply) (Fig. 3.1b).
2.2 Methods for Dye Staining
After coronary angiography, an angioscope was introduced into the targeted coronary artery. The balloon of the angioscope was inflated to stop the blood flow therein. The fiberscope incorporated into the angioscope was slowly advanced up to 7 cm distally to facilitate successive observations of the artery while displacing the blood by infusion of heparinized saline solution (10 IU/mL) at a rate of 2 mL/s for 10–20 s through the flush channel of the angioscope. To accurately confirm the location of the angioscope tip (and accordingly the observed portion), the angioscopic and fluoroscopic images were displayed simultaneously on a television monitor.
After observation by conventional AS, one mL of 2.5 % Evans blue (EB) solution was injected during balloon inflation into the artery through the flush channel of the angioscope to stain the damaged endothelial cells or fibrin, and then the balloon was deflated for blood flow restoration. One to 2 min later, the balloon was inflated again and the coronary luminal surface was observed by AS.
2.3 Imaging of Coronary Endothelial Damages Caused by Catheter Manipulation
Coronary endothelial cells protect the vascular wall against spasm and thrombus formation through release of vasodilating and antithrombotic substances. When the endothelial cells are damaged, thrombus is immediately formed on them. However, it has been difficult to visualize the damaged endothelial cells in patients in vivo.
The present authors succeeded in visualizing the damaged coronary endothelial cells. Namely, it became clear that coronary endothelial damages are caused by insertion of a catheter for percutaneous intervention, balloon inflation, and even by insertion of a guidewire (Fig. 3.2) [3, 5].
Visualization of coronary endothelial cell damages induced by catheterization
(a) A conventional angioscopic image of a coronary segment after balloon inflation of a guiding catheter
(a-1) Dye-staining angioscopic image of the same portion. Arrow: Circumscribed staining with EB, indicating balloon-induced endothelial damage
(b) Conventional angioscopic image of a coronary segment proximal to the target lesion which had been treated by stent deployment
(b-1) After EB injection. The entire luminal surface was stained blue, indicating extensive endothelial cell damage (arrow). Arrowhead: Guidewire
(c) Conventional angioscopic image of a coronary segment after single introduction of a guidewire
(c-1) After EB injection. Linear endothelial cell damage caused by guidewire (arrows)
Cited from Ref. [3] with permission
2.4 Discrimination of Coronary Fibrin from Platelets in Patients with Acute Coronary Syndrome (ACS)
Platelet thrombi play the key role in the genesis of ACS and it was generally considered that the white thrombus is platelet thrombus [9].
We performed dye-staining coronary AS study using EB as a marker of fibrin to examine whether white coronary thrombi in patients with ACS are composed of platelets alone. It became clear that the majority of white thrombi (so-called platelet thrombi) were clearly discriminated into fibrin-rich and platelet-rich thrombi (Fig. 3.3) [3].
Discrimination of fibrin from platelets in a coronary thrombus
(a) White coronary thrombi in a patient with acute myocardial infarction (arrows)
(a-1) After EB injection. The portions indicated by white arrows were stained blue, indicating presence of fibrin, but the portion indicated by a black arrow was not stained, indicating platelet aggregates
Cited from Ref. [10] with permission
This imaging modality may contribute to the selection of effective primary or adjunctive thrombolytic therapy.
2.5 Angiographically Obstructed but Angioscopically Not Obstructed Culprit Coronary Segment in Patients with Acute Coronary Syndrome (ACS)
Figure 3.4 shows a patient with unstable angina (UA) in whom the left anterior descending artery was totally occluded by angiography. However, a residual lumen was observed and nothing was seen in the lumen by conventional AS. Dye-staining AS exposed a blue structure occupying the residual lumen, indicating that it was a fibrin thrombus that caused total occlusion. Transparent fibrin thrombi, namely, a structure that was not visible by conventional AS and became visible by dye-staining AS, were observed in unstable angina or non-ST elevation myocardial infarction patients but not in ST-elevation myocardial infarction patients [12].
Angiographically obstructed but angioscopically not obstructed coronary segment in a patient with acute myocardial infarction
(a) Coronary angiogram (CAG). Obstructed proximal segment of the left anterior descending artery (arrow)
(a-1) Conventional angioscopic image of the angiographically obstructed segment. The segment was composed of disrupted plaque but residual lumen existed (arrow)
(a-2) After EB injection. The residual lumen was stained blue, indicating that the lumen was obstructed with a transparent fibrin thrombus (arrow)
Cited from Ref. [12] with permission
2.6 Detection of Damaged Endothelial Cells on Coronary Stent Struts in Chronic Phase
Coronary in-stent thrombosis is not infrequently observed by AS even 6 months or over after stenting, despite the use of ticlopidine and aspirin. However, the mechanisms underlying this late thrombosis are not well known. Endothelial cells are highly antithrombotic. Therefore, there is a possibility that neoendothelial cells covering stent struts are damaged.
The present authors carried out angioscopic observation of the coronary segments 6 months after bare stent implantation in 44 patients. Stent struts were classified by conventional AS into subgroups: stent struts not covered by neointima (naked group), stent struts seen through the neointima (seen-through group), and those not seen through the neointima (not-seen-through group). Endothelial damages visualized by EB were observed in 13.3 % of not-seen-through group, while in 80 % of seen-through and naked groups (Fig. 3.5).The neoendothelial cells covering stent struts in the seen-through/naked group were stained blue with EB more frequently than in the not-seen-through group, indicating neoendothelial cell damage (Fig. 3.6). Neoendothelial cell damage was classified into localized damage or diffuse damage. Late stent thrombosis was observed in the latter type. In animals, late stent thrombosis was observed when the neointima thickness was within 100 μm. Neoendothelial cells may have been damaged by friction between them and the stent struts due to thin interposed neointima which might have acted as a cushion, resulting in the formation of late stent thrombosis [2, 7]. These findings suggest necessity of appropriate thickening of neointima for prevention of late stent thrombosis. Similar mechanism may participate in late stent thrombosis in patients to whom drug-eluting stent was implanted.
Staining of the endothelial cells covering stent struts 6 months after stent deployment
(a) Stent struts were seen through at 6 months after deployment (arrow)
(a-1) After EB injection. Endothelial cells on the struts but not those in other portions were stained blue, indicating endothelial cell damage (arrow)
Fluffy luminal surface of culprit non-stenotic coronary segment in a patient with acute coronary syndrome
(a) Coronary angiogram (CAG) of left anterior descending artery. Arrow: The segment where fluffy luminal surface was observed by AS
(a-1) Conventional angioscopy of the same segment. The luminal surface was fluffy as in the case of seagrass (arrow). Arrowhead: Guidewire
(a-2) After EB. The fluffy luminal surface was stained blue, suggesting presence of fibrin threads (arrow)
Cited from Ref. [7] with permission
2.7 Fluffy Coronary Luminal Surface Without Significant Stenosis nor Obstructive Thrombus in Patients with Acute Coronary Syndrome (ACS)
There are a considerable number of patients with ACS in whom no significant coronary obstructions are angiographically demonstrable. Hitherto, coronary spasm or accidental thrombosis was considered as underlying mechanism, however, without definite evidence. The present authors noticed that there is a certain group of patients with ACS in whom significant stenosis is not demonstrable and the suspected culprit coronary segment exhibits fluffy (or frosty glass-like) surface. In a few of these patients, a thrombus distal to the fluffy segment was detected. The fluffy surface was stained blue with EB, indicating the presence of fibrin and/or damaged endothelial cells (Fig. 3.7).
Band-like and membranous structures on the edges of stent
(a) The segment of left anterior coronary artery where angioscopy was performed immediately after bare-metal stent deployment (arrows)
(b-1) Band-like structure on the proximal edge of the stent (arrow)
(b-2) The band was stained blue with EB, indicating that the band was composed of fibrin
(b) Membranous structure on the distal edge of the stent (arrow)
(c-1) The membranous structure was easily displaced by a guidewire (arrow). Arrowhead: Guidewire
(c-2) The membranous structure was stained blue with EB, indicating that the structure was composed mainly with fibrin (arrow)
Cited from Ref. [11] with permission
Similar changes were reproduced by mechanical damages to the artery followed by blood perfusion to produce thrombus in dogs. Fluffy surface was exposed after removal of globular thrombus. Histologically, the fluffy surface was composed of fibrin threads arising from the damaged endothelial cells and adhered by platelets. Therefore, we consider that coronary segment with frosty glass-like surface is the site of surface disruption and resultant thrombosis and frosty glass-like changes are due to residual fibrin and platelets after autolysis of the thrombus [3, 5, 8].
2.8 Characterization of Band and Web Formation on the Edges of Coronary Stents
It is a known fact that in order to treat coronary artery disease, the technique of deployment of bare-metal or drug-eluting stents into the coronary artery is widely followed. However, it is also evident that this effective therapeutic modality brings about the occurrence of several unwonted phenomena in patients, for instance, the onset of in-stent restenosis and subacute or late stent thrombosis.
In the course of conducting routine evaluations of the implanted stents through coronary AS, the authors of the present study found a frequent appearance of band-like structures connecting two or more stent struts, namely, web (W), and/or membrane-like structure connecting multiple stent struts like a curtain and obstructing the lumen, namely, membrane (M), on the edges of the implanted stents. Therefore, the incidence of this phenomenon was further investigated in the acute and chronic phases of the deployment procedure of stents in patients suffering from ACS and from effort angina pectoris. Additionally, evaluation of experiments was conducted on animals in order to obtain further clarification of the mechanisms entailed in this phenomenon.
W and M were observed in patients with ACS and those with EA (80.0 % vs 18.7 %) immediately after stent deployment and also 6 months later (55.5 % vs 28.5 %). They were stained in blue with EB immediately after stent deployment but not 6 months later. In beagles, W and M were observed in 75.0 % cases at 5 h and 66.6 % cases a month later. Histological studies revealed that W and M examined 5 h after stenting were composed of fibrin whereas those examined one month later were composed of collagen fibers (Fig. 3.8) [13].
These results indicate that W and M are frequently formed on the edges of coronary stents, and they are composed of fibrin in the acute phase, whereas this fibrin was replaced by collagen fibers in chronic phase. It is conceivable that they are formed due to blood flow turbulence and affinity of stent struts to platelets/fibrin.
The findings in this study indicated that pretreatment with heparin is not sufficient for prevention of W and M formation. Therefore, prophylactic fibrinolytic therapy just before stent deployment may be necessary for prevention of this unwanted phenomenon. Slow flow phenomenon occurs in the stented coronary artery. Distal embolism and endothelial dysfunction have been proposed as the main causative mechanisms of these unwanted hemodynamic changes [14]. Also, stent edge restenosis occurs in chronic phase [15]. There is a possibility that in addition to these mechanisms, the formation of W and M on the stent edges also contributes to slow or no flow and stent edge restenosis.
3 Dye-Staining Cardioscopy (CS)
Structurally, the left ventricular wall of the heart comprises three myocardial layers, namely, the inner oblique, middle circular, and outer oblique myocardial layers [16]. It is the inner oblique layer that is most susceptible to ischemia [17]. Till recently, the myocardial blood flow has been evaluated by contrast echocardiography, radionuclide imaging, magnetic resonance imaging, computed tomography, and electron beam computed tomography. However, selective evaluation of the blood flow in the individual myocardial layers, especially in the inner oblique layer, namely, the subendocardial myocardium, is often difficult for these imaging modalities.
A CS system using white light as the light source and obtaining color images of the heart from the inside, namely, conventional cardioscopy [18–20], was devised by the present authors. It was applied for the differential diagnosis of myocardial and valvular diseases. This imaging modality enabled the observation of subendocardial myocardial blood flow (SMBF). However, because endocardial color was used as an indicator, the assessment of SMBF was greatly influenced by the intensity of the light source. Therefore, a more reliable method for direct imaging of SMBF was required.
As the safety of the intravascular administration of EB became evident from all these studies, intracoronary administration of this dye was performed in coronary artery disease patients to observe SMBF disturbance by CS using EB as an indicator of SMBF, namely, “dye-staining CS.”
3.1 Cardioscopy System and Its Manipulation
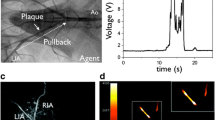
The CS system was composed of a light source (CLV-A, Olympus Corporation, Tokyo), 9-F balloon guiding catheter (Clinical Supply Co, Gifu, Japan), 4.2-F fiberscope (AF 14, Olympus), and a color charge-coupled device (CCD) camera (OTV-A, Olympus) (Fig. 3.8).
The patients were pretreated with oral diazepam (10 mg) before being transferred to the catheterization laboratory. Left ventriculography was performed after administering 50 mg of intravenous lidocaine and 5000 IU heparin. A 9-F guiding balloon was then introduced into the left ventricle and the balloon was inflated with CO2. Next, a 5-F fiberscope was advanced through the catheter so as to position the fiberscope tip at the tip of the catheter. The balloon was gently pushed against the targeted wall segment of the left ventricle, and 50–100 mL of saline solution (heparin 10 IU/mL, 37Co) was injected through the catheter at 10 mL/s to displace the blood between the balloon and the ventricular endocardial surface for observation. The anterior, apical, inferior, and lateral walls of the left ventricle were observed. The changes in the endocardial surface were recorded using a color CCD camera on a DVD recorder.
After control observation, the balloon catheter was replaced by a Judkins catheter and 1 ml of 2.5 % EB was injected into a coronary artery which irrigated the left ventricular wall segment under study. Then, the balloon catheter and fiberscope were reintroduced into the left ventricle, placing the balloon catheter tip at the same wall segment that had been previously observed, and luminal surface changes were observed again.
3.2 Evaluation of Subendocardial Myocardial Blood Flow (SMBF) by Dye-Staining Cardioscopy (CS) Using Evans Blue (EB) as a Biomarker
The observed portion was anteroapical segment in chest pain syndrome, the wall segment which was irrigated by the artery in which spasm was evoked by intracoronary administration of acetylcholine in vasospastic angina, the wall segment irrigated by the stenotic artery in angina, and dys- or akinetic wall segment in old myocardial infarction.
In patients without coronary artery disease, endocardial surface was diffusely stained blue in color immediately after intracoronary injection of EB, indicating diffuse staining of subendocardial myocardium and accordingly normal SMBF in all the patients with CPS. In contrast, in patients with organic coronary artery disease due to organic coronary artery disease, patchy staining indicating patchy preservation of SMBF and no staining indicating absent SMBF were frequently observed. In addition, patchy staining was also observed in patients with VSA, a functional disease (Fig. 3.9).
Dye-staining cardioscopy
(a to a-1) A patient with chest pain syndrome without significant coronary stenosis
(a) Before EB intracoronary injection. Endocardial color was brown, indicating normal myocardial blood flow.
(a-1) After intracoronary EB injection. The endocardial surface was stained blue, indicating normal blood flow (arrow)
(b to b-1) A patient with old myocardial infarction
(b) The endocardial surface was white to yellowish brown
(b-1) After EB injection. The endocardial surface was partially stained blue, indicating partial myocardial blood flow (arrow)
Cited from Ref. [19] with permission
Effects of coronary stenting on SMBF were also investigated. Restoration of SMBF was confirmed by dye-staining CS in selected patients [4, 8].
3.3 Dye-Staining Cardioscopy Using Fluorescein as a Biomarker for Evaluation of Myocardial Tissue Fluid Flow (MTFF)
The subendocardial myocardial layer is most susceptible to ischemia. However, there is no clinically available imaging modality for selective and real-time evaluation of subendocardial myocardial microcirculation. Therefore, a fluorescent CS system which enables real-time and selective visualization of the subendocardial myocardial tissue fluid flow (MTFF) was developed by the present authors [9].
Fluorescein is a fluorescent dye and it is clinically used in the evaluation of retinal vessels [21]. When injected into the vessels, it diffuses through the microvessels of the arterial side into the interstitial spaces of the tissues and finally drains into the venous system. Therefore, if this dye in the myocardium is visualized in vivo, the real-time evaluation of myocardial microcirculation (tissue flow and accordingly regional blood flow in the microvessels) can be attained.
The present authors developed a fluorescent CS system, and using fluorescein as an indicator, the left ventricular subendocardial MTFF was evaluated in patients with coronary artery disease. Furthermore, the effects of percutaneous coronary interventions on the MTFF were evaluated.
3.3.1 Fluorescence Cardioscopy (FCS) System and Its Manipulation
The fluorescence cardioscopy (FCS) system was composed of a fluorescent excitation unit, angioscope, balloon guiding catheter, fluorescent emission unit, intensified CCD (ICCD) camera, camera controller, DVD recorder, and television monitor.
The fluorescent excitation unit (CLV-A, Olympus Co, Tokyo) comprised a xenon lamp and a filter disc with a band-pass filter (BP) of 470 nm for fluorescence excitation. The fluorescent emission unit (DD-2, Olympus Co, Tokyo) was composed of a dichroic membrane which cut the wavelength of light below 515 nm, a band absorption filter of 515 nm which allowed wavelength of light more than 515 nm, an intensified CCD (ICCD) camera (C3505, Hamamatsu Photonics Co, Hamamatsu), and a camera controller (C3510, Hamamatsu Photonics Co, Hamamatsu).
The cardioscope and balloon guiding catheter were the same as those used for CS using EB.
After conventional CS, the light and image guides were connected to the excitation and emission units, respectively. After setting the BP and BA filters, the light was irradiated onto the target through the BP filter and light guide. The consequently evoked autofluorescence of the target was received by the ICCD camera through the DM and BA filters.
After control observation, 3 ml of 10 % fluorescein (Fluorescite®, Alcon Japan Co, Tokyo) was injected into the right femoral vein. Fluorescence images were obtained at 30 s and 1, 3, and 6 min after finishing fluorescein injection.
3.3.2 MTFF in Patients with Coronary Artery Disease
The fluorescence images were classified as follows: diffuse with high intensity indicating normal MTFF, diffuse but with low intensity indicating decreased MTFF, no fluorescence indicating absent MTFF, and patchy fluorescence indicating patchy preservation of MTFF. MTFF was normal in all 18 patients with chest pain syndrome; patchy, decreased, or absent MTFF in 16 of 20 patients with angina pectoris and/or old myocardial infarction due to organic coronary artery disease; and patchy MTFF in 21 of 28 patients with vasospastic angina pectoris. Ten of 20 patients underwent coronary stenting with successful angiographic results in all. However, MTFF disturbance frequently remained (Fig. 3.10) [9].
Cardioscopy using fluorescein as a biomarker (fluorescence cardioscopy)
(a to a-2) A patient with chest pain syndrome (CPS) without demonstrable coronary stenosis
(a) Left ventriculogram showed normal contraction. Arrow: The portion observed by cardioscopy
(a-1) Conventional cardioscopy revealed normal brown color of the endocardial surface, suggesting normal myocardial blood flow
(a-2) After intravenous fluorescein injection. The endocardial surface exhibited strong and diffuse fluorescence, indicating normal myocardial tissue fluid flow
(b) Left ventriculogram of a patient with old myocardial infarction (three-vessel disease). Left ventricular contraction was severely disturbed. Arrow: The portion observed by cardioscopy
(b-1) The endocardial surface was white, indicating fibrosis and/or severe ischemia
(b-2) After fluorescein injection. The endocardial surface was partially stained with fluorescein, indicating severely disturbed myocardial tissue fluid flow (arrow)
Cited from Ref. [20] with permission
4 Conclusion
Angioscopy using EB as a biomarker, namely, dye-staining angioscopy, clarified hitherto unrecognized mechanisms of coronary artery disease by discriminating fibrin or damaged endothelial cells. This technique was also applied for diagnosis and treatment of aortic, pulmonary, and venous diseases. Using new biocompatible markers, this technique is now used for molecular imaging of the substances that constitute atherosclerotic lesions [22, 23].
Cardioscopy using dyes as biomarkers of blood or tissue fluid flow, namely, dye-staining cardioscopy, enabled visualization of blood flow through the subendocardial microvessels or myocardial tissue fluid flow. This technique will be useful for evaluation of the effects of coronary interventions or angiogenic therapy on coronary microcirculation.
References
Uchida Y, Nakamura F, Tomaru T. Observation of atherosclerotic lesions by an intravascular microscope in patients with arteriosclerosis obliterans. Am Heart J. 1995;130:1114–7.
Uchida Y. Recent advances in coronary angioscopy. J Cardiol. 2011;57:18–30.
Uchida Y. Physiological and histological basis for understanding blood stream, vascular endothelial cell damage, thrombosis, and thrombolysis. In: Uchida Y, editor. Coronary angioscopy. Armonk: Futura Publishing Ltd; 2001. p. 57–70.
Uchida Y. Recent advances in percutaneous cardioscopy. Curr Cardiovasc Imaging Rep. 2011;4:317–27.
Uchida Y, Uchida Y. Angioscopic evaluation of neointimal coverage of coronary stents. Curr Cardiovasc Imaging Rep. 2010;3:317–23.
Terasawa K, Fujimori Y, Morio H, Ozegawa T, Uchida Y. Evaluation of coronary endothelial damages caused by PTCA guidewire: in vivo dye staining angioscopy. J Jpn Coll Angiol. 2000;40:159–64.
Uchida Y, Uchida Y, Sakurai T, Kanai M, Shirai S, Oshima T, Koga A, Matsuyama A. Possible role of damaged neoendothelial cells in the genesis of coronary stent thrombus in chronic phase. Int Heart J. 2011;52:12–6.
Uchida Y, Uchida Y, Sakurai T, Kanai M, Shirai S, Oshima T, Koga A, Matsuyama A, Tabata T. Fluffy luminal surface of the non-stenotic culprit coronary artery in patients with acute coronary syndrome.-An angioscopic study. Circ J. 2010;75:2379–85.
Uchida Y, Uchida Y, Shirai S, Oshima T, Shimizu K, Tomaru T, Sakurai T, Kanai M. Angioscopic detection of pulmonary thromboemboli: with special reference to comparison with angiography, intravascular ultrasonography and computed tomography angiography. J Interven Cardiol. 2010;23:470–8.
Uchida Y, Uchida Y, Sakurai T, Kanai M, Sugiyama Y. Imaging of subendocardial blood flow by dye-staining cardioscopy in patients with coronary artery disease. Int Heart J. 2010;51:308–11.
Uchida Y, Uchida Y, Kanai M, Tomaru T, Noike F, Sakurai T. Evaluation of myocardial tissue fluid flow by fluorescence cardioscopy in patients with coronary artery disease. Int Heart J. 2010;51:153–8.
Uchida Y, Uchida Y, Sakurai T, Kanai M, Shirai S, Morita T. Characterization of coronary fibrin thrombus in patients with acute coronary syndrome using dye-staining angioscopy. Arterioscler Thromb Vasc Biol. 2011;31:1452–60.
Uchida Y, Uchida Y, Matsuyama A, Koga A, Kanai M, Sakurai T. Formation of web- and membrane-like structures on the edges of bare-metal coronary stents. Circ J. 2010;74:1830–6.
Airoldi F, Buriguori C, Cianflone D, Cosgrave J, Sankovic G, Godino C. Frequency of slow flow following stent implantation and effect of nitroprusside. Am J Cardiol. 2007;99:916–20.
Jensen LO, Maeng M, Mintz GS, Christiansen EH, Hansen KN, Galloe H. Serial intravascular ultrasound analysis of peri-stent remodeling and proximal and distal edge effects after sirolimus-eluting or paclitaxel-eluting stent implantation in patients with diabetes mellitus. Am J Cardiol. 2009;103:1083–8.
Bhatis S, Levi M. The pathology of congenital heart disease, vol. 1. Armonk: Futura Publishing Ltd; 1996. p. 40–1.
Fujita T. Myocardial anatomy. In: Human anatomy. Tokyo: Nankodo CO; 1993. p. 310.
Uchida Y, Nakamura F, Oshima T, Fujimori Y, Hirose J. Percutaneous fiberoptic angioscopy of the left ventricle in patients with idiopathic dilated cardiomyopathy and acute myocarditis. Am Heart J. 1990;120:677–87.
Uchida Y. Atlas of cardioangioscopy. Tokyo: Mrdical View Co; 1995. p. 93–161.
Uchida Y. Percutaneous fiberoptic angioscopy of cardiac chambers and valves. In: Zipes DP, Rowlands BJ, editors. Progress in cardiology. Philadelphia: Lea & Febiger; 1991. p. 163–91.
Albert DM, Jakobiec FA. Fluorescein angiography. Principles and practice of ophthalmology, vol. 2. Toronto: W.B. Saunders Co; 1994. p. 697–717.
Uchida Y, Maezawa Y. Molecular imaging of atherosclerotic coronary plaques by fluorescent angioscopy. In: Schaller B, editor. Molecular imaging. Rijeka: Intech; 2012. p. 247–68.
Uchida Y, Uchida Y, Hiruta N, Shimoyama E, Sugiyama E. Molecular imaging of native high-density lipoprotein in human coronary plaques by fluorescent angioscopy. JACC Cardiovasc Imaging. 2013;6:1015–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Japan
About this chapter
Cite this chapter
Tomaru, T., Nakamura, F., Fujimori, Y., Uchida, Y. (2015). Dye-Staining Coronary Angioscopy and Cardioscopy. In: Mizuno, K., Takano, M. (eds) Coronary Angioscopy. Springer, Tokyo. https://doi.org/10.1007/978-4-431-55546-9_3
Download citation
DOI: https://doi.org/10.1007/978-4-431-55546-9_3
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-55545-2
Online ISBN: 978-4-431-55546-9
eBook Packages: MedicineMedicine (R0)