Abstract
Metastatic tumor without systemic extension, so-called oligometastasis, is a good candidate for carbon ion radiotherapy (C-ion RT). Careful patient selection must be needed before starting C-ion RT. The fractionation schedule is variously dependent on the tumor site, size, extension, radiosensitivity, and previously irradiated site or not. In principle, 48 GyE in 12 fractions for lymph node is used. Tumor progressions at irradiated sites were 8 %, whereas at distant sites 55 %. C-ion RT for lymph node recurrence from various malignancies might be promising to have favorable local control with acceptable toxicities, although not affecting to reduce distant metastases.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Cancer metastasis is thought to be a part of a systemic disease, usually treated with systemic therapies, although solitary lymph node metastasis or distant metastasis without systemic extension, so-called oligometastasis, could be a candidate for C-ion RT. Most of patients with recurrence are treated with systemic chemotherapy before consulting C-ion RT and some are treated with chemo-radiotherapy. Careful patient selection must be needed for C-ion RT to avoid patients with systemic metastases during or just after RT.
2 Significance of C-Ion RT
C-ion RT for metastatic tumor is suitable for localized tumor without other tumor extension, resulting in long-term survival for patients. Because of high biological effectiveness and high dose conformity, C-ion provides a higher local control than photons. Therefore C-ion RT has a potential to control previously irradiated areas (see Chap. 29).
3 Clinical Futures and Diagnostic Work-Up
The cases with solitary or small regional lymph node metastasis and solitary lung, liver, and bone metastases with at least a 5-mm gap between the recurrent lesion and radiosensitive organs, including gastrointestinal tract, skin, spinal cord, and bladder, could be a candidate.
The diagnostic work-up including PET/CT could be considered.
4 General Management of Radiation Technique
The treatment system needs at least a 5-mm gap between the recurrent lesion and radiosensitive organs, including gastrointestinal tract and bladder, and irradiated field not exceeding 15 cm. In some cases, Gore-Tex-made spacer had been inserted surgically before carbon ion radiotherapy to make a gap between surrounding radiosensitive tissues. As a radiation technique, all sites were irradiated using 3-D conformal planning system with 2–4 portals, with respiratory gating if necessary. In target delineation, the involved node was defined as GTV, prophylactic lymph node area was defined as CTV, and CTV + 5 mm (excluding GI) was defined as PTV. Treatment was performed four times a week, up to a total dose of 48 GyE in 12 fractions for 3 weeks in principle.
5 Results of Therapy
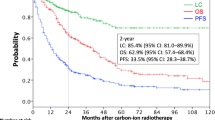
We treated 189 cases with 233 sites of metastatic lymph node from 1996 to February 2012. No acute grade 3 or higher adverse toxicities have been observed. Late adverse events were observed in one case, who developed duodenum bleeding at re-irradiated site. Tumor progressions were recognized at irradiated sites in 8 % and regional in 15 %, whereas distant sites in 55 %. The overall survival rates of the entire group were 77 % in 1 year, 53 % in 2 years, 43 % in 3 years, and 29 % in 4 years, respectively (median survival time, 2 years and 2 months).
6 Case Study
Case 1
-
A 54-year-old male presented a rib tumor and needle biopsy revealed that the tumor originated from thyroid cancer. It was judged unresectable by his orthopedic surgeon and he was referred to our hospital (Fig. 33.1 by courtesy of Dr. Reiko Imai).
Fig. 33.1 (a) CT image with a contrast medium before carbon ion radiotherapy. The tumor is located in the right tenth rib and he complained of back pain. (b) CT image with a contrast medium 8 years after carbon ion radiotherapy. The tumor shrank and partially calcified. He had no complain. (c) CT image with a contrast medium before C-ion RT. (d) Dose distribution for the patient: 70.4 GyE in 16 fractions over 4 weeks (Courtesy of Dr. Reiko Imai)
Case 2
-
A 65-year-old male with orbital squamous cell carcinoma was successfully treated with carbon ion. However, unfortunately, he had recurred at parotid lymph node. He received 52.8 GyE in 12 fraction by carbon ion radiotherapy and has been living without late adverse effect for 4 years (Fig. 33.2).
Case 3
-
A 57-year-old female with recurrent ovarian cancer (adenocarcinoma) was treated with carbon ion. She had recurred multiple para-aortic lymph nodes and received chemotherapy, although the effect was SD. She irradiated 52.8 GyE in 12 fractions and has been living well without late adverse effect for 6 years (Fig. 33.3).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Japan
About this chapter
Cite this chapter
Karasawa, K. (2014). Metastatic Tumors. In: Tsujii, H., Kamada, T., Shirai, T., Noda, K., Tsuji, H., Karasawa, K. (eds) Carbon-Ion Radiotherapy. Springer, Tokyo. https://doi.org/10.1007/978-4-431-54457-9_33
Download citation
DOI: https://doi.org/10.1007/978-4-431-54457-9_33
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-54456-2
Online ISBN: 978-4-431-54457-9
eBook Packages: MedicineMedicine (R0)