Abstract
In modern, high-density production systems, swine are challenged by pathogenic microorganisms—bacteria, viruses, and parasites that can cause infectious disease or pathology, especially for neonatal and weaned piglets (Yong-Gang et al. 2012). In these latter, immune system is not well developed in the first 4 weeks of life (Yang and Schultz 1986). Amino acids have been demonstrated to play important roles in immune responses by regulating (1) the activation of T lymphocytes, B lymphocytes, natural killer cells, and macrophages; (2) cellular redox state, gene expression, and lymphocyte proliferation; and (3) the production of antibodies, cytokines, and other cytotoxic substances (Li et al. 2007a, b; Kim et al. 2007). A number of studies have showed that dietary specific amino acids supplementation to pigs with malnutrition and infectious diseases enhance the immune status, thereby reducing morbidity and mortality (Ewaschuk et al. 2011; Johnsona et al. 2006; Liu et al. 2005, 2008; Han et al. 2008; Tan et al. 2009; Wenkai et al. 2012a, b). In this chapter, functions of amino acids in regulating the immune system and the amino acids requirements of immune system are described, in the hope of providing great promise in improving health and preventing infectious diseases in animals and humans.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Sulfur Amino Acid
- Amino Acid Requirement
- Weaned Piglet
- Apparent Ileal Digestibility
- Immune System Stimulation
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
In modern, high-density production systems, swine are challenged by pathogenic microorganisms—bacteria, viruses, and parasites that can cause infectious disease or pathology, especially for neonatal and weaned piglets (Zhang et al. 2012; Ren et al. 2012). In these latter, immune system is not well developed in the first 4 weeks of life (Yang and Schultz 1986). Amino acids have been demonstrated to play important roles in immune responses by regulating (1) the activation of T lymphocytes, B lymphocytes, natural killer cells, and macrophages; (2) cellular redox state, gene expression, and lymphocyte proliferation; and (3) the production of antibodies, cytokines, and other cytotoxic substances (Li et al. 2007b; Kim et al. 2007). A number of studies have showed that dietary specific amino acids supplementation to pigs with malnutrition and infectious diseases enhance the immune status, thereby reducing morbidity and mortality (Ewaschuk et al. 2011; Johnsona et al. 2006; Liu et al. 2008; Han et al. 2008; Tan et al. 2009; Ren et al. 2012a, b). In this chapter, functions of amino acids in regulating the immune system and the amino acids requirements of immune system are described, in the hope of providing great promise in improving health and preventing infectious diseases in animals and humans.
2 Porcine Immune System
The two primary immune responses to microorganisms and their antigens are generated by the innate and acquired or adaptive immune systems. The two immune systems interact intimately and fulfill the different needs of the host to control microorganisms. Innate immunity of pigs consists of the similar components described for other mammals. The effector functions are realized through two major mechanisms: (a) the recruitment and activation of cellular components, including macrophages, neutrophils, natural killer (NK) cells, and dendritic cells (DCs) and (b) the release of a broad spectrum of extracellular mediators such as cytokines, chemokines, complement, and antimicrobial peptides (AMPs). The cells of the immune system include the myeloid cells, monocytes, macrophages, dendritic cells, neutrophils, eosinophils, basophils and lymphocytes, of which there are two major types, the B and T lymphocytes. B cells and T cells are responsible for humoral and cell-mediated immunity, respectively, which sum to form adaptive immunity. The porcine immune system differs in many aspects from that of humans and mice, including morphological differences in the lymphatic system, and phenotypic differences in immune cells as well as functional differences in immune cell populations (Rothkötter et al. 2002). Unlike other most species, the lymphocytes enter into the lymphoid organs through the lymphatic vessels and exit directly into the blood in the pig. These differences might contribute to the predisposition to and outcomes of bacterial infections such as Salmonella serovars (Scharek and Tedin 2007).
The gastrointestinal tracts (GITs), one of the largest immunological organs of the body, contain greater than 1012 lymphocytes and has a greater concentration of antibodies than any other site in the body (Mayer 2000). With respect to immune function within the GITs, it may be equally important to achieve a homeostatic balance between immune tolerance and immune responsiveness (Artis 2008). The mucosal immune system is adequately equipped to generate a protective immune response directed at harmful pathogens, but it also has the capability to be tolerant of the ubiquitous dietary antigens and normal microbial flora while maintaining the ability to permit the absorption of nutrients. Therefore, the development of the gastrointestinal immune system is important for establishing an effective immunological response to a diverse milieu of dietary and microbial antigenic components (Brandtzaeg and Pabst 2004; Burkey et al. 2009).
The neonatal piglets have little active mucosal immune system with the low level of peripheral lymphocytes, underdeveloped lymphoid nodes, rudimentary jejunal Peyers patches, and the low numbers of effector/memory immune cells (Blecha 2001). Changes in activation of immune system by antigenic stimuli by commensal microbial flora, pathogens, and environmental influences result in the appearance of conventional, activated T and B cells and the influx and expansion of mucosal immune cells and those in the peripheral lymphoid pool (Sinkora et al. 1998, 2005). Piglets receive the passive immunity via colostral immunoglobulins intake. As time progresses up to weaning, the active mucosal system gradually gathers the ability to generate its own antibody molecules in the gut wall. In the first 2 weeks of life, the intestine rapidly becomes colonized with lymphoid cells. Between 14 and 28 days of age, the intestinal mucosa becomes colonized with CD4+ cells, and CD8+ cells begin to appear at 35 days age. The immunological architecture of piglet cannot be considered fully mature until 7 weeks of age (Sinkora and Butler 2009). In commercial practice, piglets are weaned at 3–4 weeks of age, and this results in an increased susceptibility to bacterial infection and acute diarrhea and high mortality rates. The obvious increase of the numbers of CD2+ leucocytes was observed in the intestine (Dréau et al. 1995), and piglets showed reduced ability to react to the lymphocyte mitogen phytohemagglutinin after weaning. With the reduction of IL-2 secreted from systemic T cells, production of specific antibody was also reduced (Butler et al. 2002; Sinkora et al. 2000).
3 Amino Acids Metabolism by Cells of the Immune System
The utilization of amino acids by immune cells plays an important role in the function of the immune system (Curi et al. 1997). Glutamine utilization has been linked to functional activities of immune cell function such as cytokine production, nitric oxide production, superoxide production, and phagocytosis. Many of cells of the immune system including lymphocytes, macrophages, and neutrophils utilize glutamine at high rates, which is related to the specific function of these cells in the inflammatory response (Curi et al. 1997, 1999; Wu et al. 2007; Wang et al. 2008; Newsholme et al. 1999; Ren et al. 2013). Therefore, glutamine had to be present at 10- to 100-fold in excess of any other amino acid in culture and cannot be replaced by glutamic acid or glucose. Although the activity of the first enzyme responsible for the metabolism of glutamine, glutaminase, is high in these cells, the rate of oxidation is low. Much of the glutamine is converted to glutamate, aspartate, lactate, and in appropriate conditions to CO2 (Newsholme 2001). Koch et al. (1990) demonstrated that glutamine provides N- and C-atoms required for the synthesis of macromolecules and energy while leucine provides more precursors for incorporation into protein in peripheral lymphocytes.
Cell culture studies have showed that BCAA are absolutely essential for lymphocytes to synthesize protein, RNA, and DNA and to divide in response to stimulation (Calder 2006). Immune cells are able to incorporate BCAA into proteins and oxidize BCAA (Calder 2006; Burns 1975). Walrand et al. (2004) reported that leucine incorporation into immune cell proteins was linear over time with a comparable slope. Incorporation of isoleucine into proteins by lymphocytes is greatest, followed by eosinophils, and then by neutrophils (Burns 1975). Immune cells express branched chain alpha keto acid dehydrogenase and decarboxylase activities and so can oxidize BCAA. Lymphocytes take up and oxidize leucine and isoleucine in vitro (Calder 2006). Mitogen stimulation of lymphocytes increases leucine transport by 270 %, leucine transamination by 195 %, and leucine oxidation by 122 % (Koch et al. 1990). Isoleucine is oxidized by neutrophils and lymphocytes through the Krebs cycle after decarboxylation and lymphocytes are able to oxidize isoleucine eight times more rapidly than neutrophils (Burns 1975). In a B cell line, the pattern of uptake of all three BCAAs through the cell cycle is the same, and the order of the rate of uptake is leucine, isoleucine, and valine (Glassy and Fur long 1981).
Another important immuno-enhancing amino acid, arginine, is metabolized either by inducible nitric oxide synthases (iNOS) or by arginase 1 in immune cells. These enzymes are stimulated by T helper 1 or 2 cytokines, respectively. In the absence of immune stimulation, little arginine is used by immune cells due to a lack of expression of major arginine metabolizing enzymes, iNOS and arginase 1 (Bernard et al. 2001). Myeloid cells expressing arginase 1 are described in a growing number of disease processes, prominently in cancer, autoimmune diseases, and in graft vs. host disease (Bronte and Zanovello 2005; Rodriguez et al. 2005; Serafini et al. 2006; Popovic et al. 2007). The accumulation of arginase 1-expressing myeloid cells in spleens in mice after surgical trauma has also been observed (Makarenkova et al. 2006). Myeloid suppressor cells (MSC) efficiently deplete arginine and generate ornithine. Arginase 1 expression is also detected in mononuclear cells after trauma or surgery. Unlike arginase 1, iNOS is regulated by opposing stimuli. It has been shown that inflammatory stimuli induce the expression of iNOS in myeloid cells and other cell types (Hibbs 1991; Popovic et al. 2007; Johansson et al. 2002, 2010). iNOS can be induced in response to various cytokines such as IL-1, TNFα, and IFNγ, or bacterial products such as LPS. In vivo, IFNγ is the most potent and prevailing inducer of iNOS (Johansson et al. 2002). iNOS exerts a regulatory effect on arginase activity through the production of hydroxy-l-arginine, an intermediate product in the generation of NO. Arginase 1 in turn regulates NO through depletion of arginine availability (Morris 2004). Neither iNOS nor arginase 1 is induced in T lymphocytes, which represents a marked difference between these cells and myeloid cells. T lymphocytes depend on arginine for proliferation, ζ-chain peptide, and T cell receptor complex expression.
4 Impact of Amino Acids on Immune Function: Pig Studies
Amino acids affect immune system function usually through actions at several levels in the gastrointestinal tract, thymus, spleen, regional lymph nodes, and immune cells of the circulating blood (Cunningham-Rundles 2002). The regulation of amino acids on the immune function can be considered from two perspectives, namely, the enhancement of the immune response that protects individuals from infections and malignant neoplasms and the reduction of over-responses such as inflammation and autoimmunity (Yoneda et al. 2009). The roles of glutamine, arginine, threonine, methionine, cysteine, and tryptophan in enhancing the immune function in pigs have been well established (Johnsona et al. 2006; Ewaschuk et al. 2011; Tan et al. 2008; Li et al. 2007b; Wang et al. 2006; Grimble 2006; Le Floc’h and Sève 2007).
Glutamine is required to support optimal lymphocyte proliferation and production of cytokines by lymphocytes and macrophages (Wu 1996; Yoo et al. 1997; Yu et al. 2002; Calder and Yaqoob 1999). Adding glutamine to the weaning diet of pigs significantly modified immune cells in the mesenteric lymph nodes, in a potentially beneficial manner by preventing an increase in antigen naive CD4+ cells, increasing the proliferative response to pokeweed mitogen, and supporting a Th-1 type cytokine response after T cell stimulation (Johnsona et al. 2006). Glutamine is preferentially metabolized by the intestinal mucosa and by lymphocytes. As a precursor for glutathione (GSH) it helps maintain the antioxidant status of cells, improving the gut barrier function against bacterial infection. So glutamine supplementation is useful in reducing early steps in weaning-related gastrointestinal infections (Ewaschuk et al. 2011; Liu et al. 2002). Intestinal tissue from control, but not from Gln-supplemented, pigs responded to Escherichia coli with a significant increase in mucosal cytokine mRNA (IL-1β, IL-6, transforming growth factor-β, and IL-10) and a decrease in tight-junction protein expression (claudin-1 and occludin) (Ewaschuk et al. 2011).
As a precursor for nitric oxide and polyamine synthesis, arginine profoundly influences immune function (Kelly et al. 1995; Wu and Meininger 2002). Arginine has been demonstrated to exert beneficial effects on pregnant sows (Kim et al. 2006) and weaned pigs (Tan et al. 2009), on LPS-immunostimulated pigs (Liu et al. 2008), and on cyclophosphamide-immunosuppressed pigs (Han et al. 2009). This amino acid reduces morbidity and mortality in response to infectious pathogens. Administration of arginine increased thymus size, weight and cellularity, enhanced lymphocyte proliferation in response to mitogen and alloantigen, augmented macrophage and natural killer (NK)-cell-induced lysis of tumor cells, and increased IL-2 production by lymphocytes and receptor activity (Han et al. 2009; Kim et al. 2006; Tan et al. 2009). Arginine supplementation improves the development of digestive tract, prevents intestinal villous atrophy, and decreases the expression of intestinal pro-inflammatory cytokines, thereby enhancing the mucosal immune status in early-weaned piglets and alleviating mucosal injury of LPS-challenged pigs (Liu et al. 2008; Tan et al. 2008).
Threonine plays an important role in the production of antibodies and in providing overall immune system support. A significant part of the threonine intake is utilized by the gut itself and is used for the synthesis of endogenous secretions, particularly mucus, which is important to maintain the gut barrier. Threonine supplementation can regulate the innate immune function of IPEC-J2 cells infected with Pseudorabies Virus at molecular level, and can inhibit expression of genes corresponding to IL-1β, TNF-α, and TGF-β1, but enhance expression of gene corresponding to IL-6 and IL-15, while the effects were found to vary with time (Han et al. 2012). Dietary supplementation with threonine also has been demonstrated to promote serum levels of IgG in sows (Cuaron et al. 1984) and increase antibody production, serum IgG levels, and jejunal mucosal concentrations of IgG and IgA, while decreasing jejunal mucosal concentrations of IL-6 in young pigs challenged with E. coli (Li et al. 1999; Wang et al. 2006).
Sulfur amino acids, methionine and cysteine, have indeed been shown to be beneficial for the immune system, aside from their role in protein synthesis (Grimble 2006). Additional dietary intake of methionine plus cysteine can reduce the adverse effects of immune system stimulation on whole body protein deposition in growing pigs, and probably accelerates the recovery (Litvak et al. 2011). Dietary supplementation with N-acetylcysteine (a stable precursor of cysteine) is highly effective in enhancing immune functions under various disease states (Geudens et al. 2008; Grimble 2001). However, improvement of immune function in pigs challenged with aflatoxin was not observed with supplementation of 0, 0.15, 0.30, or 0.45 % methionine to a basal diet containing 0.33 % methionine (Van Heugten et al. 1994). Methionine and cysteine are precursors of important molecules and important for intestinal mucosal function. We recently demonstrated that a sulfur amino acid-free diet administered enterally to piglets for 7 days led to a reduced intestinal mucosal growth associated with villus atrophy, reduced epithelial cell proliferation, lower goblet cell number, and diminished small intestinal redox capacity (Bauchart-Thevret et al. 2009).
Tryptophan plays an important role in the defense of the body and immune response modulation (Moffet and Namboodiri 2003; Le Floc’h and Sève 2007), in relation with the kynurenine pathway. In pigs, Melchior et al. (2004, 2005) showed that this metabolic pathway is involved in tryptophan metabolism disturbances associated with an inflammatory response. Pigs suffering from lung inflammation had lower plasma tryptophan concentrations and higher IDO activity in lungs and associated lymph nodes, than pair-fed healthy control piglets (Le Floc’h et al. 2004; Melchior et al. 2004, 2005).
5 Amino Acids Requirements to Optimize Immunity
A deficiency of dietary protein or amino acids has long been demonstrated to impair immune function and increase the sensitivity of animals to infectious challenges or stressful conditions (Le Floc’h et al. 2004). For example, deficiency of branched chain amino acids and of arginine + lysine increased splenocyte proliferation, but sulfur amino acid deficiency decreased splenocyte and lymphocyte proliferation (Konashi et al. 2000). The study with piglets has shown that threonine deficiency caused higher nitrogen excretion, blood urea, and lower number of acidic mucin-producing goblet cells in the small intestine (Wang et al. 2007). Dietary supplementation with amino acids beyond their requirements for growth deposition might thus be useful depending on environmental conditions particularly during periods of stress and when the immune system is challenged (Reeds and Jahoor 2001).
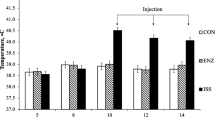
It is now clear that immune system stimulation (ISS) can cause morphological and physiological changes in the gastrointestinal tract and impact nutrient utilization in pigs (Le Floc’h et al. 2004; Mani et al. 2012). During immunological stress, amino acids are redistributed away from protein production towards tissues involved in inflammation and immune response (Bruins et al. 2000, 2002; Webster et al. 2002). They are used for the synthesis of inflammatory and immune proteins, to support immune cell proliferation, and for the synthesis of other compounds important for body defense functions (Le Floc’h et al. 2004; Webster et al. 2002). Immune activation appears to alter glutamine and arginine metabolism. Bruins et al. (2000) and Deutz et al. (1992) have shown that surgery and endotoxemia induced by LPS injection results in an increase in glutamine efflux from the hindquarter and intestine and in glutamine uptake by the liver and spleen. During the peak of an immune response, the requirement for those nonessential amino acids (glutamine, arginine, cysteine, and so on) increases 2- to 3-fold (Wilmore and Shabert 1998; Pond and Newsholme 1999), becoming, at least potentially, limiting (Reeds and Jahoor 2001). ISS does not change the apparent ileal digestibility (AID) of amino acids but alters the partitioning of sulfur amino acids in favor of nonprotein body stores in growing pigs (Rakhshandeh et al. 2010). These findings reflect an increased need for dietary sulfur amino acids to support the immune response during immune system stimulation in growing pigs (Rakhshandeh et al. 2010). In pigs injected with turpentine, fibrinogen plasma concentrations increase by 30 % and fibrinogen synthesis increases by 140 % (Jahoor et al. 1999). And in pigs with a lung inflammation induced by intravenous injection of complete Freund’s adjuvant, plasma tryptophan concentrations declined for 10 days. Therefore, the increase in protein synthesis may require a great quantity of tyrosine, phenylalanine, and tryptophan (Le Floc’h et al. 2004; Melchior et al. 2004, 2005). Li et al. (1999) reported that although maximum growth rate of 17–31 kg pigs occurred at a dietary threonine level of 6.8 g kg−1, higher threonine levels were needed to maximize humoral antibody production and IgG levels. To optimize immunity of 10–25 kg pigs, 6.6 g per day of true ileal digestible threonine should be fed (Wang et al. 2006). Li et al. (2007a) showed that the ideal amino acid pattern of lysine/methionine/threonine/tryptophan on the digestible basis was 100:27:29:59 for 10 kg pigs under immune stress and 100:30:21:61 for piglets under normal conditions.
References
Artis D (2008) Epithelial-cell recognition of commensal bacteria and maintenance of immune homeostasis in the gut. Nat Rev Immunol 8:411–420
Bauchart-Thevret C, Stoll B, Chacko S, Burrin DG (2009) Sulfur amino acid deficiency upregulates intestinal methionine cycle activity and suppresses epithelial growth in neonatal pigs. Am J Physiol Endocrinol Metab 296:E1239–E1250
Bernard AC, Mistry SK, Morris SM Jr, O’Brien WE, Tsuei BJ, Maley ME, Shirley LA, Kearney PA, Boulanger BR, Ochoa JB (2001) Alterations in arginine metabolic enzymes in trauma. Shock 15:215–219
Blecha F (2001) Immunology. In: Pond WG, Mersmann HJ (eds) Biology of the domestic pig. Cornell University Press, Ithaca, NY, pp 688–711
Brandtzaeg P, Pabst R (2004) Let’s go mucosal: communication on slippery ground. Trends Immunol 25:570–577
Bronte V, Zanovello P (2005) Regulation of immune responses by L-arginine metabolism. Nat Rev Immunol 5:641–654
Bruins MJ, Soeters PB, Deutz NE (2000) Endotoxemia affects organ protein metabolism differently during prolonged feeding in pigs. J Nutr 130:3003–3013
Bruins MJ, Soeters PB, Lamers WH, Deutz NE (2002) L-arginine supplementation in pigs decreases liver protein turnover and increases hindquarter protein turnover both during and after endotoxemia. Am J Clin Nutr 75:1031–1044
Burkey TE, Skjolaas KA, Minton JE (2009) BOARD-INVITED REVIEW: Porcine mucosal immunity of the gastrointestinal tract. J Anim Sci 87:1493–1501
Burns CP (1975) Isoleucine metabolism by leukemic and normal human leukocytes in relation to cell maturity and type. Blood 45:643–651
Butler JE, Weber P, Sinkora M, Baker D, Schoenherr A, Mayer B, Francis D (2002) Antibody repertoire development in fetal and neonatal piglets. VIII. Colonization is required for newborn piglets to make serum antibodies to T-dependent and type 2 T-independent antigens. J Immunol 169(12):6822–6830
Calder PC (2006) Branched-chain amino acids and immunity. J Nutr 136:288S–293S
Calder PC, Yaqoob P (1999) Glutamine and the immune system. Amino Acids 17:227–241
Cuaron JA, Chapple RP, Easter RA (1984) Effect of lysine and threonine supplementation of sorghum gestation diets on nitrogen balance and plasma constituents in first-litter gilts. J Anim Sci 58:631–637
Cunningham-Rundles S (2002) Evaluation of the effects of nutrients on immune function. In: Calder PC, Field CJ, Gill HS (eds) Nutrition and immune function. CABI Publishing, Wallingford, UK, pp 57–92
Curi TCP, Demelo MP, Deazevedo RB, Zorn TMT, Curi R (1997) Glutamine utilization by rat neutrophils: presence of phosphate-dependent glutaminase. Am J Physiol 42:Cl124–Cl129
Curi R, Newsholme P, Pithon-Curi TC, Pires-de-Melo M, Garcia C, Homem-de-Bittencourt PI Jr, Guimarães ARP (1999) Metabolic fate of glutamine in lymphocytes, macrophages and neutrophils. Braz J Med Biol 32:15–21
Deutz NE, Reijven PL, Athanasas G, Soeters PB (1992) Post-operative changes in hepatic, intestinal, splenic and muscle fluxes of amino acids and ammonia in pigs. Clin Sci 83:607–614
Dréau D, Lallès JP, Toullec R, Salmon H (1995) B and T lymphocytes are enhanced in the gut of piglets fed heat-treated soyabean proteins. Vet Immunol Immunopathol 47:69–79
Ewaschuk JB, Murdoch GK, Johnson IR, Madsen KL, Field CJ (2011) Glutamine supplementation improves intestinal barrier function in a weaned piglet model of Escherichia coli infection. Br J Nutr 106:870–877
Geudens N, Wuyts WA, Rega FR, Vanaudenaerde BM, Neyrinck AP, Verleden GM, Lerut TE, Van Raemdonck DEM (2008) N-acetyl cysteine attenuates the inflammatory response in warm ischemic pig lungs. J Surg Res 146(2):177–183
Glassy MC, Fur long CE (1981) Neutral amino acid transport during the cell cycle of cultured human lymphocytes. J Cell Physiol 107:69–74
Grimble RF (2001) Nutritional modulation of immune function. Proc Nutr Soc 60:389–397
Grimble RF (2006) The effects of sulfur amino acid intake on immune function in humans. J Nutr 136:1660S–1665S
Han J, Liu YL, Fan W, Chao J, Hou YQ, Yin YL, Zhu HL, Meng GQ, Che ZQ (2009) Dietary L-arginine supplementation alleviates immunosuppression induced by cyclophosphamide in weaned pigs. Amino Acids 37:643–651
Han GQ, Yu B, Chen DW, Xiang ZT, Chen Y, Chen H, Mao Q (2012) Effects of threonine on expression of immune-related genes of porcine intestinal epithelial cell infected with Pseudorabies virus in vitro. Chin J Anim Nutr 3:487–496
Hibbs JB (1991) Synthesis of nitric oxide from L-arginine: a recently discovered pathway induced by cytokines with antitumour and antimicrobial activity. Res Immunol 142:565–569
Jahoor F, Wykes L, del Rosario MP, Frazer ME, Reeds PJ (1999) Chronic protein undernutrition and an acute inflammatory stimulus elicit different protein kinetic responses in plasma but not in muscle of piglets. J Nutr 129:693–699
Johansson AC, Hegardt P, Janelidze S, Visse E, Widegren B, Siesjö P (2002) Enhanced expression of iNOS intra-tumorally and at the immunization site after immunization with IFNγ -secreting rat glioma cells. J Neuroimmunol 123:135–143
Johansson CC, Mougiakakos D, Trocme E, All-Ericsson C, Economou MA, Larsson O, Seregard S, Kiessling R (2010) Expression and prognostic significance of iNOS in uveal melanoma. Int J Cancer 126:2682–2689
Johnsona IR, Ball RO, Baracos VE, Field CJ (2006) Glutamine supplementation influences immune development in the newly weaned piglet. Dev Comp Immunol 30:1191–1202
Kelly E, Morris SM Jr, Billiar TR (1995) Nitric oxide, sepsis, and arginine metabolism. J Parenter Enteral Nutr 19:234–238
Kim SW, Mateo RD, Wu G, Carroll JA, Shinzato I (2006) Dietary L-arginine supplementation affects immune status of pregnant gilts. FASEB J A266.1
Kim SW, Mateo RD, Yin YL, Wu GY (2007) Functional amino acids and fatty acids for enhancing production performance of sows and piglets. Asian-Australas J Anim Sci 20:295–306
Koch B, Schroder MT, Schafer G, Schauder P (1990) Comparison between transport and degradation of leucine and glutamine by peripheral human lymphocytes exposed to concanavalin A. J Cell Physiol 143:94–99
Konashi S, Takahashi K, Akiba Y (2000) Effects of dietary essential amino acid deficiencies on immunological variables in broiler chickens. Br J Nutr 83:449–456
Le Floc’h N, Sève B (2007) Biological roles of tryptophan and its metabolism: potential implications for pig feeding. Livest Sci 112:23–32
Le Floc’h N, Melchiora D, Obledb C (2004) Modifications of protein and amino acid metabolism during inflammation and immune system activation. Livest Prod Sci 87(1):37–45
Li DF, Xiao CH, Qiao SY, Zhang JH, Johnsonb EW, Thacker PA (1999) Effects of dietary threonine on performance, plasma parameters and immune function of growing pigs. Anim Feed Sci Technol 78:179–188
Li JW, Chen DW, Zhang KY, Long DB (2007a) The effect of immune stress on ideal amino acid pattern for piglets. Front Agric China 1(2):210–213
Li P, Yin YL, Li DF, Kim SW, Wu G (2007b) Amino acids and immune function. Br J Nutr 98:237–252
Litvak N, Rakhshandeh A, Htoo J, de Lange CFM (2011) Optimal dietary methionine to methionine plus cysteine ratio is increased during immune system stimulation in growing pigs. In: Proceedings of Mid-West American society of animal science meeting, Des Moines, Iowa
Liu T, Peng J, Xiong Y, Zhou S, Cheng X (2002) Effects of dietary glutamine and glutamate supplementation on small intestinal structure, active absorption and DNA, RNA concentrations in skeletal muscle tissue of weaned piglets during d 28 to 42 of age. Asian-Australas J Anim Sci 15:238–242
Liu YL, Huang JJ, Hou YQ, Zhu H, Zhao S, Ding B, Yin Y, Yi G, Shi J, Fan W (2008) Dietary arginine supplementation alleviates intestinal mucosal disruption induced by Escherichia coli lipopolysaccharide in weaned pigs. Bri J Nutr 100:552–560
Makarenkova VP, Bansal V, Matta BM, Perez LA, Ochoa JB (2006) CD11b+/Gr-1+ myeloid suppressor cells cause T cell dysfunction after traumatic stress. J Immunol 176:2085–2094
Mani V, Weber TE, Baumgard LH, Gabler NK (2012) Endotoxin inflammation and intestinal function in livestock. J Anim Sci. doi:10.2527/jas.2011-4627
Mayer L (2000) Mucosal immunity and gastrointestinal antigen processing. J Pediatr Gastroenterol Nutr 30:S4–S12
Melchior D, Sève B, Le Floc’h N (2004) Chronic lung inflammation affects plasma amino acid concentrations in pigs. J Anim Sci 82:1091–1099
Melchior D, Mézière N, Sève B, Le Floc’h N (2005) Is tryptophan catabolism increased under indoleamine 2,3 dioxygenase activity during chronic lung inflammation in pigs? Reprod Nutr Dev 45:175–183
Moffet JR, Namboodiri MA (2003) Tryptophan and immune response. Immunol Cell Biol 81:247–265
Morris SM Jr (2004) Enzymes of arginine metabolism. J Nutr 134(10):S2743–S2747
Newsholme P (2001) Why is L-glutamine metabolism important to cells of the immune system in health, postinjury, surgery or infection? J Nutr 131:S2515–S2522
Newsholme P, Curi R, Pithon-Curi TC, Murphy CJ, Garcia C, Pires-de-Melo M (1999) Glutamine metabolism by lymphocytes, macrophages and neutrophils. Its importance in health and disease. J Nutr Biochem 10:316–324
Pond CM, Newsholme EA (1999) Coping with metabolic stress in wild and domestic animals. Brit Soc Anim Sci Publ Ser 24:9–20
Popovic PJ, Zeh HJ III, Ochoa JB (2007) Arginine and immunity. J Nutr 137:S1681–S1686
Rakhshandeh A, Htoo JK, de Lange CFM (2010) Immune system stimulation of growing pigs does not alter apparent ileal amino acid digestibility but reduces the ratio between whole body nitrogen and sulfur retention. Livest Sci 134(1):21–23
Reeds PJ, Jahoor F (2001) The amino acid requirement of disease. Clin Nutr 20:15–22
Ren WK, Yin YL, Liu G, Yu XL, Li YH, Yang G, Li TJ, Wu GY (2012a) Effect of dietary arginine supplementation on reproductive performance of mice with porcine circovirus type 2 (PCV2) infection. Amino Acids 42:2089–2094
Ren WK, Luo W, Wu MM, Liu G, Yu XL, Fang J, Li TJ, Yin YL, Wu GY (2012b) Dietary L-glutamine supplementation improves pregnancy outcome in mice infected with type-2 porcine circovirus. Amino Acids. doi:10.1007/s00726-011-1134-5
Ren W, Zou L, Li N, Wang Y, Gang L, Peng Y, Ding J, Yin Y, Wu G (2013) Dietary arginine supplementation enhances immune responses to inactivated Pasteure llamultocid avaccination in mice. Br J Nutr 109:867–872
Rodriguez PC, Hernandez CP, Quiceno D, Dubinett SM, Zabaleta J, Ochoa JB, Gilbert J, Ochoa AC (2005) Arginase I in myeloid suppressor cells is induced by COX-2 in lung carcinoma. J Exp Med 202:931–939
Rothkötter HJ, Sowa E, Pabst R (2002) The pig as a model of developmental immunology. Hum Exp Toxicol 21:533–536
Scharek L, Tedin K (2007) The porcine immune system—differences compared to man and mouse and possible consequences for infections by Salmonella serovars. Berl Munch Tierarztl Wochenschr 120(7–8):347–354
Serafini P, Borrello I, Bronte V (2006) Myeloid suppressor cells in cancer: recruitment, phenotype, properties, and mechanisms of immune suppression. Semin Cancer Biol 16:53–65
Sinkora M, Butler JE (2009) The ontogeny of the porcine immune system. Dev Comp Immunol 33(3):273–283
Sinkora M, Sinkora J, Rehakova Z, Splichal I, Yang H, Parkhouse RM, Trebichavsky I (1998) Prenatal ontogeny of lymphocyte subpopulations in pigs. Immunology 95(4):595–603
Sinkora M, Sinkora J, Rehakova Z, Butler JE (2000) Early ontogeny of thymoctes in pigs: sequential colonization of the thymus by T cell progenitors. J Immunol 165(4):1832–1839
Sinkora M, Butler JE, Holtmeier W, Sinkorova J (2005) Lymphocyte development in fetal piglets: facts and surprises. Vet Immunol Immunopathol 108(1–2):177–184
Tan BE, Li XG, Kong XF, Yao K, Wu GY, Yin YL (2008) Effect of arginine on development, mucosal morphology and IL-2 gene expression levels of digestive tract in early-weaned piglets. Scientia Agricultura Sinica 41(9):2783–2788
Tan BE, Li XG, Kong XF, Huang RL, Ruan Z, Yao K, Deng ZY, Xie MY, Shinzato I, Yin YL, GY W (2009) Dietary L-arginine supplementation enhances the immune status in early-weaned piglets. Amino Acids 37:323–331
Van Heugten E, Spears JW, Coffey MT, Kegley EB, Qureshi MA (1994) The effect of methionine and aflatoxin on immune function in weanling pigs. J Anim Sci 72:658–664
Walrand S, Guillet C, Gachon P, Rousset P, Giraudet C, Vasson MP, Boirie Y (2004) Protein synthesis rates of human PBMC and PMN can be determined simultaneously in vivo using small blood samples. Am J Physiol Cell Physiol 286:C1474–C1478
Wang X, Qiao SY, Liu M, Ma YX (2006) Effects of graded levels of true ileal digestible threonine on performance, serum parameters and immune function of 10–25 kg pigs. Anim Feed Sci Technol 129:264–278
Wang X, Qiao SY, Yin YL, Yue LY, Wang ZY, Wu GY (2007) A deficiency or excess of dietary threonine reduces protein synthesis in jejunum and skeletal muscle of young pigs. J Nutr 137:1442–1446
Wang JJ, Chen LX, Li P, Li XL, Zhou HJ, Wang FL, Li DF, Yin YL, Wu GY (2008) Gene expression is altered in piglet small intestine by weaning and dietary glutamine supplementation. J Nutr 138:1025–1032
Webster JI, Tonelli L, Sternberg EM (2002) Neuroendocrine regulation of immunity. Annu Rev Immunol 20:125–163
Wilmore DW, Shabert JK (1998) Role of glutamine in immunologic responses. Nutrition 14:618–626
Wu G (1996) Effects of concanavalin A and phorbolmyristate acetate on glutamine metabolism and proliferation of porcine intraepithelial lymphocytes. Comp Biochem Physiol 114:363–368
Wu G, Meininger CJ (2002) Regulation of nitric oxide synthesis by dietary factors. Annu Rev Nutr 22:61–86
Wu GY, Bazer FW, Davis TA, Johnson GA, Kim SW, Knabe DA, Spencer TE, Yin YL (2007) Important roles for arginine-family amino acids in swine nutrition and production. Livest Sci 122:8–22
Yang WC, Schultz RD (1986) Ontogeny of natural killer cell activity and antibody dependent cell-mediated cytotoxicity in pigs. Dev Comp Immunol 10:405–418
Yoneda J, Andou A, Takehana K (2009) Regulatory roles of amino acids in immune response. Curr Rheumatol Rev 5:252–258
Yoo SS, Field CJ, McBurney MI (1997) Glutamine supplementation maintains intramuscular glutamine concentrations and normalizes lymphocyte function in infected early-weaned pigs. J Nutr 127:2253–2259
Yu IT, Wu JF, Yang PC, Liu CY, Lee DN, Yen HT (2002) Roles of glutamine and nucleotides in combination in growth, immune responses and FMD antibody titres of weaned pigs. Anim Sci 75:379–385
Zhang Y, Yin Y, Fang J, Wang Q (2012) Pig production in subtropical agriculture. J Sci Food Agric 92:1016–1024
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Wien
About this chapter
Cite this chapter
Tan, B., Xie, M., Yin, Y. (2013). Amino Acids and Immune Functions. In: Blachier, F., Wu, G., Yin, Y. (eds) Nutritional and Physiological Functions of Amino Acids in Pigs. Springer, Vienna. https://doi.org/10.1007/978-3-7091-1328-8_12
Download citation
DOI: https://doi.org/10.1007/978-3-7091-1328-8_12
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-1327-1
Online ISBN: 978-3-7091-1328-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)