Abstract
Current challenges in the upper motor neuron syndrome (UMNS) management include identifying and establishing correct strategies to evaluate spasticity in clinical and research settings. There are a number of measures frequently used in a clinical environment. They are mainly qualitative tools that range from questionnaires to scales that are practical but imprecise. Alternative, quantitative measures that provide an accurate evaluation of spasticity are currently available for use, however they require specialist training and equipment. The advantage of quantitative assessments is that they can also differentiate between different components of spasticity and their contribution in the symptomatology. However, the use of these precise tools requires a longer time than is usually available in clinical practice. This chapter presents an overview of the different methods that exist to evaluate spasticity and proposes different management strategies. There is still a need to converge the efforts of researchers in different fields to develop accurate practical tools and algorithms that allow for precise evaluations in clinical practice.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Spasticity is one component of the upper motor neuron syndrome (UMNS), a central nervous system disorder usually caused by damage to nerve pathways within the brain or spinal cord. Clinically, spasticity is defined as “a velocity-dependent increase in the tonic stretch reflexes (muscle tone) with exaggerated tendon jerks, resulting from the hyperexcitability of the stretch reflex”. This definition was provided by Lance three decades ago (Lance 1980), and is still the most widely used. Spasticity may occur in association with conditions where the brain and/or spinal cord are damaged, such as in spinal cord injury, multiple sclerosis, stroke, traumatic brain injury, amyotrophic lateral sclerosis, or they fail to develop normally such as in cerebral palsy, hereditary spastic paraplegias, and metabolic diseases such as adrenoleukodystrophy, phenylketonuria, and Krabbe disease. Spasticity affects around 85 % of subjects with multiple sclerosis (Sommerfeld et al. 2004), 35 % of chronic hemiplegic stroke subjects (Sommerfeld et al. 2004) and between 65 and 78 % of subjects with spinal cord injury (Maynard et al. 1990).
Spasticity is a major problem that adversely impacts the quality of life of affected subjects, producing stiffness and ultimately may lead to muscle shortening (contractures) and musculoskeletal deformities. These changes interfere with voluntary movements and daily functions like ambulation, hand dexterity, balance, speech and swallowing amongst others. This increase in muscle tone or stiffness might also cause discomfort and pain, interfering with rehabilitation in patients with certain disorders. Symptoms may include hypertonicity (increased muscle tone), clonus (a series of oscillating muscle contractions), exaggerated deep tendon reflexes, muscle spasms, and scissoring (involuntary crossing of the legs).
There are several therapies to treat spasticity, including physical therapy, occupational therapy, pharmacological treatments and surgery. Despite the great variety of treatments, their effectiveness is still limited. Clinical methods to assess efficacy are very practical, but imprecise, in the measurement of spasticity or evaluation of therapy outcomes. Experimental methods are, on the other hand, very accurate but highly complex, often requiring very long preparation sessions with many complex and expensive experimental devices. In order to enhance the rehabilitation of patients suffering from spasticity, treatments should give measurable improvements. Therapy outcomes need to be accurately evaluated without requiring complex experimental procedures or equipment.
This chapter aims to introduce the reader to the challenges that are present in measurements of spasticity. In an attempt to illustrate the concepts in an easy to follow manner, the chapter has been organized as follows: first, we introduce the reader to the clinical aspects of spasticity, covering basic concepts of the neurophysiology of the disease and giving a more extended description of the problems of spasticity measurements. Next, we present a review of current methods for measurement of spasticity and therapy outcomes, as well as the characteristics of spasticity. Finally, we present the conclusions of this work.
2 Background
Spasticity is a common feature of muscle impairment in the UMNS. Although Lance’s definition of spasticity (given in the introduction) is the most widely accepted, it still makes it difficult for clinicians to understand the pathophysiology of this disease, and to quantify its severity. Confusion in the use of terminology complicates assessment and treatment planning by health professionals, and it results because clinicians often confuse the other signs of the UMNS and describe them indistinctly as spasticity (Ivanhoe and Reistetter 2004). The resistance of spastic muscle to stretch is dynamic and increases with the amount of stretch, and especially, with the velocity of the stretch.
2.1 Neurophysiology
The neurophysiological bases of spasticity have been widely discussed. Several theories ascribe the problem to an “abnormal process” of the signals arriving from the Central Nervous System (CNS) (Biering-Sorensen et al. 2006; Fleuren et al. 2010; Gómez-Soriano and Taylor 2010). Although the basic underlying mechanism of these abnormal processes is not clear, is likely that the major contribution is disruption in balance between the inhibitor and excitatory control signals coming from the CNS to modulate motoneuron excitability.
The basic neural circuit underlying spasticity is the stretch reflex arc, composed of the muscle spindle receptors, their afferent projections to spinal motoneurons, the spinal motoneurons themselves, the motor axons, and the muscle fibers they innervate. This reflex is important in coordinating normal movements in which muscles are contracted and relaxed. Stretch receptors in the muscles (muscle spindles) sense the amount of stretch in the muscle and send a signal to the spinal cord, via the sensory afferent pathways. The brain responds by sending a message back to contract or shorten the muscle. A loss of inhibitory control releases the hyperexcitability of the stretch reflex, and is generally thought to be the primary cause of spasticity.
The main components of spasticity are muscle stiffness (intrinsic biomechanical properties of the muscle) and hyperexcitability of the stretch reflex (Gottlieb et al. 1978; Rack et al. 1984). This augmented excitability of the stretch reflex could be explained by increased reflex gain after its activation or by decreased reflex threshold. A possible factor is an intrinsic decrement in α motoneuron excitability threshold, with a great increment in monosynaptic reflex excitability. There is also extensive evidence supporting the view that the reflex is triggered after smaller stretch stimuli (lower threshold), rather than by increases in reflex gain. There is still a need for practical measures that can differentiate between the contributions of the two components (intrinsic muscle stiffness and hyperexcitability) of spasticity to the symptomatology.
2.2 Measurements
Currently, there is no practical method providing an objective overall evaluation of spasticity. There are several available methods to assess the degree of spasticity of the patient, which can be classified as qualitative (clinical) methods or quantitative (experimental) methods.
2.2.1 Qualitative Methods
The principal advantage of the current qualitative methods is that they are relatively easy to use, quick to perform, and the clinician does not need novel instrumentation to make a measurement. They can be used in standard clinical environments without additional cost. However, these methods lack accuracy, precision and objectivity, instead providing a subjective way to track progress after therapy.
2.2.2 Quantitative Methods
The advantage of many quantitative methods is that they can assess different neurophysiological and biomechanical parameters, like EMG, joint torques and angles, allowing a deeper insight into physiological mechanisms of the disease. Quantitative methods also provide objective methods of assessment. The principal weakness of these methods is that they require complex instrumentation, such as mechanical devices, biosignal amplifiers, sensors and electrodes. These requirements increase costs, require personnel to perform measurements, and require additional preparation time, which makes sessions troublesome for patients and clinicians, and increases costs, hampering implementation in clinical environments.
The challenge in assessment of spasticity and the response to different therapies is to find the balance between practical clinical, and advanced experimental methods, in order to overcome the limitations imposed by both types of methods. Priorities for routine diagnosis are that methods should be fast and easy to perform rather than highly precise, as clinicians should examine patients in a functional context. The efficacy of uncomplicated clinical methods, such as the Ashworth and Tardieu scales to evaluate spasticity, has been proven over many years (see below). To evaluate and track the progression of spasticity with accuracy requires technical equipment and knowledge. If the measurement is too complicated, clinical professionals will not use it regularly. As an alternative, an appropriate and accurate way to assess spasticity and response to treatment might be to determine the threshold for stretch reflex, as it is sensitive to changes in response to treatment and other factors. However, simple and precise ways to assess stretch reflex are still lacking.
The following sections will review current clinical and experimental methods for the diagnosis and assessment of spasticity, highlighting their strengths and limitations.
3 Qualitative Measures
Qualitative methods to measure spasticity share some features that make them the most frequently used in clinical practice. They are fast to complete, easy to learn, relatively simple, and appropriate for most of the muscle groups. Most have been created so that a single evaluator can perform them manually, without requiring expensive and specialized equipment. On the other hand, they are subjective and validity and reproducibility of the technique depend on the experience of the assessor and on the control of potential influencing factors.
The contribution of both neural (stretch reflex) and mechanical components (elastic and viscous) should also be carefully considered when assessing spasticity. However, most of the methods available in clinical practice are qualitative methods with insufficient sensitivity to differentiate among different components of spasticity. These methods are mainly based on scales that evaluate different aspects of the pathophysiology of spasticity, such as the resistance produced by muscles against passive movements (Ashworth Scale) or the frequency of spasms (Penn Spasm Frequency Scale).
Other methods are based on questionnaires that assess the impact of the disease on the patient’s activities of daily life. Although these scales have been widely studied and tested, they may have limited reproducibility when comparing between different patients or when different clinicians perform the exams. In addition, many of them only focus on one single symptom or specific sign of spasticity, which hardly correlates with presence of other associated symptoms, hampering the assessment of the overall state of the patient.
3.1 Ashworth Scale and Modified Ashworth Scale
The Ashworth Scale (AS) and the Modified Ashworth Scale (MAS) are currently the most widely used methods to evaluate spasticity in both clinical practice and in advanced research settings (Pandyan et al. 2002). The original AS is an ordinal qualitative scale that was developed in 1964 to evaluate the response to a given antispastic medicine (Carisoprodol) on spasticity in Multiple Sclerosis (Ashworth 1964). This scale is a subjective graduation of the perception of the tone or resistance to manual externally imposed passive movements through the joint range of motion (ROM). This resistance is commonly used as a measure of spasticity, even though spasticity is only one of the factors that contribute to this tone. Changes in intrinsic properties of the muscle (contractures, composition modification with loss of sarcomeres and viscoelastic components) and joint, presence of pain, the activity of the agonists and antagonists and other factor are frequently involved in mediating this resistance (Kheder and Nair 2012). AS graduates tone in five categories ranging from 0 (normal state in absence of resistance) to 4 (the most severe rigidity with contractures).
Bohannon et al. described the modified Ashworth (MAS) in 1987 to raise the sensitivity of the AS in the evaluation of the lower levels of spasticity. The MAS adds an extra category between the grades 1 and 2, referred to as 1 + (Bohannon and Smith 1987). Some authors maintain that this new category brings ambiguity to the scale, and that the MAS should be considered a nominal assessment rather than an ordinal scale. The AS and MAS are non-instrumented and relatively simple and quick to execute. However, the reliability of these scales has been shown to be variable according to the examiner experience and to the limb, joint, and underlying pathologies being evaluated. AS have been reported to be more reliable than the MAS (Pandyan et al. 1999).
When assessing the lower extremities, the AS seems to have better inter-rater reliability in the distal than in the proximal muscle groups. Studies evaluating the intra-rater reliability of the MAS in CP have found conflicting results that range from low through moderate agreement, to good and very good (Numanoglu and Günel 2012). The inter-rater reliability of the MAS is better for upper limbs than for lower limbs (Pandyan et al. 1999), especially for wrist and elbow flexors. Both scales can detect changes after treatments in both upper and lower limbs and in different pathologies, although they have shown low sensitivity to change (Platz et al. 2005).
Despite the wide use of these scales, there is still a need to determine accurately, guidelines describing recommendations about the way to conduct the evaluation. While most authors agree the movement should be performed in less than a second, there is still variability in the speed, the starting limb positioning for the evaluations, the influence of pain and limited passive ROM, and the definition of catch and release. Detailed guidelines to use AS and MAS would be desirable to improve the reproducibility and reliability of these scales Table 7.1.
3.2 Tardieu Scale and Modified Tardieu Scale
The Tardieu Scale (TS) was developed on 1954 to assess spasticity considering the velocity dependent variability component that is included in the definition (Tardieu et al. 1954). Boyd et al. presented a modified version that is called the Modified Tardieu Scale (MTS) in 1999 (Boyd and Graham 1999). Although the scale can be used for adults and children with neurological conditions, these scales are more frequently used in practice in pediatric populations with Cerebral Palsy. The TS and the MTS assess the response of the muscle to stretch applied at three different speeds (V1, V2 and V3) Table 7.2.
When the examiner moves the joint at V1 we obtain the passive range of motion (R2). If the examiner moves the muscle quickly, (V2 or V3) we obtain R1. These scales emphasize the importance of the dynamic component of spasticity, represented by means of the difference between the angles (R2−R1) for a given joint. The difference R2−R1 is a useful tool to measure the severity of the disorder, and help the clinician to plan treatments for spasticity. The greater the difference, the higher the dynamic component, which means better response to antispastic treatments. The lower the difference R2−R1, the more likely it is that the stiffness comes from muscle contracture, which means that the expectation of response to antispastic treatments is poor.
The MTS has shown adequate to excellent intra-rater reliability for the majority of the muscle groups usually evaluated in patients with spasticity after brain injury (Mehrholz et al. 2005; Singh et al. 2011). The inter-rater reliability of the MTS ranges from low to adequate for the same muscles (Ansari et al. 2008). The inter-rater reliability of the TS is adequate to excellent and the test-retest reliability is excellent when using goniometry and inertial sensors (Paulis et al. 2011). The TS was able to detect changes over time in patients after a specific treatment for spasticity in one study, although there is still a lack of studies evaluating the actual responsiveness of the scale (Gracies et al. 2000).
3.3 Tendon Tap (Clinical Hammer)
Tendon hammers are commonly employed in clinical practice to elicit spinal reflexes. A muscle tendon percussion efficiently activates a reflex arc that leads to a momentary contraction of the specific muscle. This reflex response is correlated to stretch reflex threshold and provides information about the presence and the severity of the spasticity of the subject (Wood et al. 2005). It is routinely used in neurological examinations because it is a very simple and fast technique that provides valuable information at virtually no cost. The symmetry, or asymmetry, of the reflex between the two sides is suggestive of integrity, or abnormality, of the corticospinal tract, respectively.
There are a high number of classifications in the literature that try to grade the deep tendon reflex according to the intensity of the response, although there is not yet consensus about the use of any specific scale (Meythaler et al. 1996; Meythaler et al. 2001; Walker et al. 1990). The most common scales, the National Institute of Neurological Disorders and Stroke scale (NINDS) and Mayo Clinic scale, have both failed to provide better than fair inter-observer reliability (Manschot et al. 1998).
Tendon jerks are more easily elicited in people with spasticity and therefore it has been suggested that these could provide a means to quantify the phenomenon. However, there are some limitations in the magnitude of this response that varies with the force exerted by the tap, the position on which the tendon is hit, and with the subjectivity of the scoring Table 7.3.
3.4 Spasm Scores
A spasm is defined as the sudden extensor or flexion contraction of a muscle group. Spasms are highly correlated with the intensity of spasticity. The measurement of spasms and its changes provide a more comprehensive understanding of the spasticity. Penn et al. described the Penn Spasm Frequency Scale (PSFS) that aims to score the presence of spasms and their frequency and severity over a one-hour time span. This simple and fast, self-report measure assesses a patient’s self-perception of the frequency and severity of the spasticity (Penn et al. 1989). Subsequently, Priebe et al. introduced the modified PSFS that added a second part to score independently the spasm severity in spasticity secondary to spinal cord injury (Priebe et al. 1996) Table 7.4.
In general, qualitative clinical methods to assess spasticity or other symptoms of the UMN are poorly correlated. There is still a lack of consensus about the use of quantitative objective methods. Due to the complexity and the time-consuming nature of quantitative methods, most of the assessors still choose to evaluate spasticity by means of a combination of qualitative measures including assessment of different aspects of the UMNS that are tightly linked to spasticity.
4 Electrophysiological Measures
One of the most common methods to evaluate spasticity is to register the electrical activity of muscles, especially in a research environment. The rationale for this approach is that the mechanical properties and responses of muscles are closely related to their electrical activity.
Most electrophysiological-based methods register electrical activity of muscles by means of electromyography (EMG). There are different techniques to obtain and record this activity, most of which measure the neuromuscular reflex response to evoked stimuli. The main difference among these techniques lies in the way in which the stimulation is delivered: electrical stimulation to the peripheral nerve; biomechanical stimulation (pressure or changes in elongation by tendon tapping); or the response to external muscle stretch (Voerman et al. 2005).
The principal advantage of these methods is that they offer an understanding of what happens to the neuromuscular circuit when spastic reflexes occur: they are very important for the understanding of physiopathological mechanisms (Burridge et al. 2005).
The main limitation of these methods is that they do not have direct clinical relevance, when assessing spasticity, due to test response variability between subjects, and to the lack of correlation with the clinical scales. In addition, they require additional instrumentation and data analysis. Nevertheless, combined with biomechanical based methods, they can provide neuromuscular insight, in correlation with biomechanical properties, which allows features of spasticity such as the threshold angle at which spastic reaction is triggered, to be studied.
4.1 EMG Response to Electrical Stimulation
4.1.1 Hoffman Reflex and H/M Ratio
The Hoffman reflex (H-reflex) is a spinal reflex caused by a stimulation of the peripheral nerve and the subsequent activation of Ia afferent fiber bypassing the muscle spindle. This electrical pulse is conducted to the posterior horn of the spinal cord and is transmitted to the α-motoneuron, through a predominantly monosynaptic pathway. Next, the stimuli travels orthodromically to the muscle, generating a reflex response that constitutes the H-reflex and that can be registered. Amplitude and latency of the H-reflex are the most useful parameters in practice, offering information about the excitability of the α-motoneuron and its changes (Yates et al. 2011). The H-reflex is a low threshold reflex that is provoked at low stimulus intensities. If we gradually increase the intensity of the stimulation, the motor axon is also activated and we will progressively register another response that is called M-wave, which appears at a higher threshold. In the beginning of this increase of the intensity of the stimulation, initially the H-reflex will also increase and gradually the M-wave will appear. After that, if the stimulus is increased further, the H-reflex will decrease and the M-wave will rise, until a threshold is reached where the H-reflex will not be detected and the M-wave will be prominent (Hiersemenzel et al. 2000).
Several factors need careful consideration when assessing the H-reflex, in order to ensure correct accuracy, and reproducibility, of the technique. Among these factors, positioning (subject, head, join, limb), correct placement of the electrodes, differences in skin properties, subcutaneous fat, sensory input, duration and frequency of the stimulation, number of measurements, muscle activity, and subject age and height, need to be determined to ensure technique precision (Phadke et al. 2010). Due to these factors, the amplitude of the EMG signal has shown variability between subjects and between sessions. This amplitude is more comparable if expressed relative to the size of the EMG response evoked by a supramaximal stimulation of the motor axons in the nerve innervating a given muscle from which reflex response in measured (Hmax and Mmax). To decrease variability, some authors prefer the ratio Hmax/Mmax to evaluate α-motoneuron excitability with increased reliability (Gómez-Soriano et al. 2012).
4.1.2 F-Wave
The F-wave assesses spinal excitability by means of peripheral nervous system conduction. It is obtained by applying supramaximal electrical stimulation to the motor nerve that leads to the generation of an action potential in the muscle. In this method, the stimulation travels in two directions, orthodromically to the muscle provoke a contraction (generating the M-Wave) and antidromically to the spinal cord to activate the α-motoneuron cell body. Then, the impulse goes back orthodromically via the α-motoneuron to activate the muscle and generate a signal that is called F-wave (Blicher and Nielsen 2009). The F-wave is the second signal to register after stimulation (after the M-wave). The main properties of the F-wave evaluated are amplitude, latency and duration. Stroke patients have shown increased F-wave frequency, and this has been correlated with motoneuron hyperexcitability (Argyriou et al. 2010).
4.2 EMG Response to Mechanical Stimulation
4.2.1 Tendon Reflex (T-Reflex)
T-reflex or phasic stretch reflex implies the assessment of the electrical response to mechanical stimuli (tapping a tendon) with a hammer. The pressure made to the intrafusal fibers activates the Ia afferent fibers that generate signals transmitted directly to the ∝-motoneuron. This response is essentially equivalent to the H-reflex, with the difference being that the stimulation is elicited in the muscle spindle, rather than directly on the nerve. The T-reflex generates a contraction of the extrafusal fibers of the muscle (Liu et al. 2011) that can be recorded with surface electromyography. The most important parameters evaluated are latency and amplitude, although other parameters such as reflex duration, torque, and loop delay, are often used and correlate with clinical assessments. As described above for the H-reflex, positioning of the limbs and the electrodes, intensity and frequency of the stimulus, and other factors may influence the outcome, and affect accuracy and reproducibility of the technique (Heckman and Rymer 2008).
4.3 EMG Response to Movement
4.3.1 Stretch Reflex
The stretch reflex of the muscle has demonstrated spring-like behavior, which means that the muscle displays proportional changes in force as the muscle length varies (Powers et al. 1988). Hyperactive tonic stretch reflex has been widely recognized as one of the key features of spasticity. This hyperactivity is attributed mainly to a considerable reduction in stretch threshold that has been demonstrated in spastic muscles (Zhang et al. 2000). The stretch reflex is triggered at lower stimuli than non-spastic muscles, and this threshold decrease is correlated with increasing reflex joint torque (Chardon et al. 2010).
Some factors may increase the variability of the results and should be taken into account when evaluating the reflex response. Some of these factors are: the amount of force required to exert contraction, the velocity, the strength and the duration of the contraction/relaxation, the extension of the area to elicit the reflex response of the tested muscle and the concomitant contraction of non-tested muscles. There are some approaches to address the limitations brought by these factors including systems, such as an automated hammer, which will be described later in this chapter.
The majority of studies found augmented reflexes in people with UMNS, with or without spasticity, in comparison with healthy controls. Most of the studies failed to demonstrate the existence of a correlation between the amount of the increase in stretch responses and the severity of spasticity, especially when spasticity was assessed with clinical measures such as AS and MAS, although recent studies have reported more promising results (Biering-Sorensen et al. 2006). Therefore, electrophysiological techniques are not routinely useful tools for evaluation of spasticity in clinical practice. However, they are promising instruments to help reach a better understanding of the pathophysiology of spasticity and seek to characterize if changes in electrical stimulation in spasticity correlate with variations in the severity of spasticity (Min et al. 2012). These techniques are also unique to determine threshold and amplitude of stretch reflex, that in combination with the evaluation of torque responses through biomechanical techniques, represent a reliable and reproducible way to evaluate spasticity.
5 Biomechanical Measures
Biomechanical measures provide valuable information when quantitative data are necessary. However, they often require complex devices and considerably long setup time, which hinders their application in a clinical environment. They offer high repeatability, and objective, contrastable information, to the field of research and evaluation of treatments. Biomechanically based methods provide a more accurate assessment during passive movements than traditional clinical scales, allowing measures of velocity, angles, resistance to passive movements, and stiffness. A great advantage of these methods is that they can be correlated with clinical scales. The big pitfalls are the instrumentation needed for these methods, which must be coupled to the body, as well as the time required for data analysis, that makes their use in daily clinical practice unfeasible. In addition, their measures are highly dependent on the joint and the plane of movement, skipping other symptoms of spasticity such as spasms, clonus or hyperreflexia.
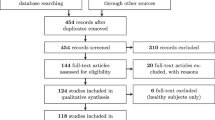
The methods proposed so far may be classified in a number of ways, depending on the joints involved, patient involvement, physical parameters being measured etc. The classification of those methods used in this chapter is presented in Fig. 7.1. The first distinction has been made based on various conditions in which increased muscle tone is observed: i.e. while stretching the muscle, tapping the tendon or voluntarily performing a functionally relevant movement.
5.1 Muscle Stretching
These methods may be considered, in most cases, as an instrumented way of performing typical clinical tests where the physician passively flexes or extends the limb in order to evaluate resistance. However, there are significant differences between the various methods proposed.
The first difference is in the joint and muscles investigated. Most of the quantitative methods are applied to a limited number of joints. Usually spasticity is evaluated in the elbow, knee or ankle joint unilaterally. However, there have been systems proposed, that allow evaluation of spasticity in other joints, such as in the wrist (Walsh 1992) or metacarpophalangeal joints (Kamper and Rymer 2000). In general, subjects should remain passive and relaxed during the measurement. In a few cases, the subjects should voluntarily preactivate their muscles prior to stretch (e.g. (Powers et al. 1988; Powers et al. 1989)). This approach attempts to eliminate the influence of the difference in the stretch reflex threshold between various subjects.
Various parameters of the motion and of the reflex response may be measured. In most cases, the parameter of interest is the torque evoked at the joint versus the actual joint angle. Because spasticity is velocity-dependent, it is important to know the measurement velocity. Typically, motion is performed at a constant velocity (“isokinetic”). Usually, a constant angular velocity and not a constant muscle stretching velocity is applied, since the second depends on the relative location of muscle tendons. It is often assumed however, that the muscle is stretched at close to a constant velocity, and this is true for a good portion of the ROM in most cases.
The manual measures, in which tonic stretch reflexes are elicited by the examiner, (typically by manipulating the subject’s limb to cause rotation of the evaluated joint), may be considered a kind of isokinetic measure, provided that the examiner moves the limb smoothly. Such methods are considered quantitative, if the characteristic of movement is measured in an objective way. An example of such a system was developed by the Newcastle CREST group and is presented in Fig. 7.2. The clinician acts in the same manner as when performing the standard Ashworth test, except that instead of holding the patient’s arm directly, a small handle is used. The joint angle and force achieved during the pull are measured, and the spasticity is quantified by calculating the slope of the graph of applied force versus passive range of movement. The greater the resistance to the applied force the steeper the slope (Pandyan et al. 2001).
Schema of the manual device for spasticity measurement developed by the Newcastle CREST group (from (Pandyan et al. 2001))
Increased muscle stiffness, manifested as increased torque during passive movement, may be of muscular (i.e. due to changes of intrinsic muscle structure) or neural (i.e. due to altered reflex properties) origin. In order to be able to apply correct treatment, it is important to determine the source of the increased muscle tone correctly. For this reason biomechanical measures are often complemented by EMG measurement. If an increase in stiffness is accompanied by an increase in EMG activity, it suggests a reflex response. Other methods, which allow the distinction between various origins of the resistance, are discussed below.
Two distinct parameters of the reflex response may be altered by spasticity: the “set point”, (the angular threshold of resistance); and the “gain”, (the slope of the resistance versus joint angle curve) (Katz and Rymer 1989). Some systems, such as that proposed by the Newcastle CREST group, determine the level of spasticity based on the slope of the torque (or sometime force) versus joint angle curve. Katz and Rymer (1989) found that it is mostly the “set point” which is affected by the spastic hypertonia, and not the gain. Thus, it seems reasonable to determine the set point of the increased resistance, i.e. the angle where torque or EMG starts to increase significantly. Kim et al. (2011) have proposed a portable measurement system, equipped with flexible electrogoniometer and EMG sensors, which allows determination of the onset of the tonic stretch reflex while an examiner passively moves the limb. The use of an electrogoniometer allows the moment of the increased EMG activity to be correlated with a particular joint angle, and by the differentiation of the angular signals, determination of the angular velocity at which the test was performed.
The advantage of using instruments to record measurements during manually applied tests, is that they are simple to administer, whereas their accuracy is higher than qualitative tests. The main disadvantage is that if the movement is applied by the examiner, the characteristics of the movement (i.e. velocity versus angle profile) cannot be pre-defined or accurately repeated. This is the reason why, in the cases when higher repeatability of measurement conditions is required, powered devices are used. These are typically equipped with motors, which may drive and resist (active systems) or only resist (passive systems) the movement, ensuring that it follows the pre-defined profile.
Probably the most commonly used devices are isokinetic dynamometers, which are commercially available and used for multiple purposes (i.e. determining muscle strength, performing muscle strengthening exercises, rehabilitation). They are also often used for spasticity measurement. Typical tests incorporating isokinetic dynamometers are performed at two or three angular velocities. Testing at a lower velocity than the one at which reflex response is observed allows identification of the intrinsic resistance component and at a higher velocity allows identification of the reflex component. The great advantage of isokinetic dynamometry is that the velocity and amplitude of the applied movement, is standardized, however, some authors argue that the use of isokinetic dynamometers, increases repeatability only slightly compared to handheld dynamometers, whereas their use significantly increases complexity and costs of the measurement (Boiteau et al. 1995; Lamontagne et al. 1998; Lebiedowska et al. 2003).
Because the threshold velocity for eliciting the stretch reflex is not known, evaluators need to be careful when selecting the velocities used to perform the test (Boiteau et al. 1995), and the results obtained by various subjects cannot be easily compared (Biering-Sorensen et al. 2006). Rabita et al. (Rabita et al. 2005) have shown that normalization of the resistance observed at various velocities, by expressing it as a percentage of the values measured at the lowest velocity, gives results that correlate well with the AS score.
The angular range over which a constant velocity can be maintained is limited due to unavoidable acceleration at the beginning and deceleration at the end of the motion. It becomes especially significant when high velocities are applied over a short range of movement. Also it is not clear at which velocities isokinetic measurements should be performed. These are some of the arguments supporting performing measurements while motion is provided in a sinusoidal (e.g. (Lehmann et al. 1989; Rack et al. 1984; Stefanovska et al. 1989)) or random (e.g. (Hunter and Kearney 1982; Kearney et al. 1997; Powers et al. 1988)) waveform.
The simplest method of providing joint motion in a sinusoidal waveform is the pendulum test, however, it is not possible to perform this test at multiple frequencies. Wartenberg proposed this test in 1951 (Wartenberg 1951). The subject sits on a couch with lower leg hanging and is instructed to stay relaxed. The examiner extends the leg to the horizontal position and releases it, which allows the leg to swing freely due to gravity, and stopping after a few swings because of quadriceps femoris muscle resistance. The motion of the leg are measured by the electrogoniometers and the relaxation index, often calculated as the ratio between the initial flexion and the final position of the knee joint, is determined. The relaxation index is used to estimate the severity of spasticity, and it has been shown that, when computed in the way described above it has a good correlation with the AS score (Leslie et al. 1992).
Some alternative ways to determine the relaxation index have also been proposed (Johnson 2002). The pendulum test is easy to apply, and provides reliable results, but it is used only for evaluation of spasticity in the knee joint, and with adaption for the elbow joint as well (Lin et al. 2003; Liu et al. 2011). It is hard to use the pendulum test in cases of severe spasticity.
Performing measurements at various speeds and various frequencies allows better discrimination between intrinsic and reflex components of the stiffness. For this purpose mathematical models including mechanical properties of neuro-muscular system have been developed. Parameters are identified when performing movements at various velocities. The models and identification techniques being used differ in their complexity, and one of the most sophisticated techniques applied so far for spasticity quantification includes a parallel-cascade system identification method (Mirbagheri et al. 2007). In this work, the two components of the stiffness are split into parallel branches, an intrinsic and elastic one. A second-order model having inertia, viscous, and elastic parameters described the intrinsic stiffness. Reflex delay and a third-order model having gain, damping, and frequency parameters, described the reflex stiffness. In order to identify the parameters of this model the elbow joint is perturbated by applying pseudorandom binary sequence position inputs with low amplitude and a high switching-rate (150 ms).
The system identification techniques, such as the one described above, are very powerful in discriminating various components of resistance and in the quantification of spasticity, however, they require a complex set-up and fast movements at various velocities in random order. Although they allow precise identification of the system parameters, they may be very unpleasant for the subject. Furthermore, since strong motors are used, special attention must be paid to ensuring the safety of the subject.
5.2 Tendon Tapping
The stretch reflex may be elicited in a number of ways, e.g. by muscle stretching (similar to the Ashworth test, and the above described biomechanical methods), through electrical stimulation (as it is the case for some electrophysiological methods) or by short percussion of the muscle tendon. The clinical tendon tap method is an elegant way of eliciting a stretch reflex. However, in order to obtain repeatable results, the applied force and the position on which tendon is struck should be standardized.
A simple approach to standardizing the force is to allow the reflex hammer to swing through a measured arc before striking the tendon. However, if more precise control of the applied force is needed, a device equipped with electronic control of the applied force may be used. A few such systems have been proposed so far (Chardon et al. 2009; Fryer et al. 1972). In particular the device proposed by the Chardon et al. (Chardon et al. 2009) is an attractive option. It not only allows for standardization of the applied force, but it also allows measurement of the tension in the tendon at rest, and during a reflex response, thanks to the force sensor integrated into the tapper. When performing measurement using this system (see Fig. 7.3) a small linear actuator is fixed to the mechanical frame at an angle 90° to the tendon and aligned in such a way that the end of the tapper touches the skin. Then, a series of constant small amplitude stimuli is applied and the tendon tension and EMG activity of the muscle is measured. Afterward, the tapper is methodically lowered in increments of 1 mm, using a micrometer attached to the actuator, what allows for preactivation of the muscle. The same series of stimuli is generated at each tendon indentation. This approach allows an accurate estimation of the stretch reflex threshold as well as passive muscle properties, and thus quantifies spasticity in a rather simple and cost-effective way. However, the joint has to be immobilized in order to ensure reliable measurements. Thus, if the device is to measure reflex for various joints, a complex mechanical construction may be needed.
A device for automatized tendon tapping measure. Left experimental set up: a position-controlled linear actuator (Linmot, Inc.) is placed perpendicular to the tendon of the biceps brachii, while the tension in the stimulated muscle tendon and the EMG activity of that muscle are measured; Right exemplary force trace recorded by the force sensor during tapping (Chardon et al. 2009)
5.3 Functional Analyses
One of the main goals of spasticity treatment is to increase ability to perform voluntary movement. Therefore, it can be argued that it is necessary to investigate the behavior of spastic muscles during voluntary, and not passive movements. The most obvious way to perform such measurement is with movement analysis and energy expenditure measurement during gait (for lower extremities) or reaching and grasping activities (for upper extremities). Motion analysis systems, such as those described in Chap. 16 of this book, may be used. Such analyses provide comprehensive data, but also require employment of complex devices and time-demanding data processing. Performing such analyses would also be difficult in cases of severe spasticity. Furthermore, spasticity is only one of the components of the motor impairment caused by pathologies of the CNS. Other components are weakness and impaired motor coordination. Dysfunctional walking or reaching is an effect of all three impairments, and such functional analyses usually do not distinguish between the contributions of these factors. Thus, while functional analyses may provide useful information about the walking and reaching problems of people affected by spasticity, they should not be considered as a way of measuring spasticity per se (Johnson 2002; Wood et al. 2005).
6 Measuring the Effectiveness of Spasticity Treatment
To understand fully the importance of properly measuring the efficacy of treatments to overcome effects of spasticity, it is necessary to better understand what is required to adequately measure the changes that occur due to the treatment. One common treatment for spastic muscle behavior is the injection of Botulinum toxin type A (BtA). This treatment has been used for a number of years for cosmetic reasons as well as to treat other ailments. BtA injection is expensive, however it is generally considered safe (Kolaski et al. 2008) even when used for an extended period (Mejia et al. 2005). The effects and required dosages are well documented for those treatments where it is used extensively. More recently is has become widely accepted as a treatment for spastic muscles.
Botulinum toxins are a group the most lethal toxins known, however when injected into muscle in minute amounts, they can have beneficial therapeutic effects. Seven distinct serotypes are produced by Clostridium botulinum, with type A the one most commonly used therapeutically. BtA acts at the neuromuscular junction to inhibit the release of acetylcholine from the presynaptic nerve terminal without affecting the synthesis or storage of acetylcholine. The complete action of BtA is described in the literature (Davis and Barnes 2000; Dressler and Adib Saberi 2005) however, the effect is to cause muscle weakening (Blasi et al. 1993). When injected into a hyperactive muscle the weakening effect can reduce muscle size (Dressler and Adib Saberi 2005). Dosage is varied, depending on the size of the targeted muscle (Davis and Barnes 2000), while effectiveness may vary across patients (Pullman et al. 1996). Adverse systemic effects are rare, though they may occasionally be serious (Howell et al. 2007) and may include flu-like signs, transient fatigue, and nausea (Brin 1997). The muscle is progressively reinnervated by nerve sprouting making the action of the toxin temporary.
Many studies have assessed the effect of BtA injections on persons suffering from spasticity. It is not the purpose here to review them all, however those mentioned give an indication of the outcomes and methods of assessment commonly used. BtA has increasingly been considered a valuable treatment option for the management of muscle tone in children suffering from CP (Graham et al. 2000). These children are often at high risk of developing bone deformities during the growth phase which may require surgery to correct. BtA injections to the affected muscles can to delay or avoid surgery, as well as prevent secondary complications such as pain and other musculoskeletal problems while the child is growing.
In a report of three case studies Gooch and Sandell (1996) found that injection of BtA reduced pain, and improved ease of care in two children with CP, and reduced spasticity, and improved function temporarily in a third. Corry et al. (1997) performed a randomized, double blind study, on 14 patients with CP and found that BtA injection into the upper limb provided a modest functional change at 2 and 12 weeks, but the ability to pick up coins did not improve, and in some cases was worse. Vles et al. (2008) used a parent reported Visual Analogue Scale to evaluate the effect of BtA treatment of 55 children with CP, and found improvements in nursing, standing, and walking, but no significant improvement in pain. The treatment had no effect for 7 of the children, and 5 children had side effects. Moore et al. (2007) reported no long term cumulative or persisting benefit using BtA in leg spasticity over 2 years when 64 children with CP were assessed using PEDI and Gross Motor Function Measure (GMFM). They suggested that the measures may not have been sensitive in the situation, and that benefits perceived in other studies using impairment measures may be spurious. Py et al. (2009) used GMFM and clinical examination to assess the effectiveness of injecting BtA into the lower limbs of 54 children with CP, and found it clinically effective for 51 % with improved function for 24 % after one month. Lukban et al. (2009) reviewed trials between 1990 and 2008 that assessed the effectiveness of BtA for the treatment of CP. Outcomes were reported in terms of a variety of outcome scales which limit the comparison of results across trials. They also detail five systematic reviews of these trails. Four of these reviews concluded that the data was inadequate to support treatment.
BtA is also commonly used in the treatment of spasticity associated with other pathologies. Das and Park (1997) treated six post stroke hemiplegia patients with BtA injections and concluded that the treatment reduced spasticity in the upper limb with a subjective improvement in functional ability. Opara and colleagues (2007) reported that 20 patients following spinal cord injury (SCI), or suffering from MS, with moderate to severe spasticity in the lower extremities, showed improvements in pain measures, with side effects on only one patient. Marciniak et al. (2008) investigated the use of BtA with 28 patients following SCI and reported improvements in self-identified goals of function, hygiene, and pain.
Gait analysis (GA) has become a useful method for planning and assessment of treatments for spasticity especially in persons with CP (Boyd and Graham 1999; Boyd et al. 2000; Galli et al. 2007). This method allows a quantitative assessment of changes due to treatment, however the measurements are linked to assessments of the effect of the treatment on a joint or limb, and it is difficult to determine the specific effect of the injection on the treated muscle. Galli et al. (2007) reported a significant improvement in foot and ankle range of motion for 15 children with CP 1.5 months after injection of BtA into the calf muscles. Boyd et al. (Boyd and Graham 1999) devised new GA measures for ankle moments and reported improvements in ankle kinetics at 12 and 24 weeks after injection of BtA into the gastrocnemius-soleus muscles for 25 children.
The mechanisms by which injection with BtA changes muscle behavior over longer periods are not yet adequately explained and precise measurements are necessary to fully understand the effect this treatment has on muscle mechanical behavior. It has been found that BtA reduces muscle spindle afferent discharge providing relief through partial motor paralysis and a decrease in reflex muscular tone without affecting muscle strength (Filippi et al. 1993). Pandyan et al. (2002) assessed elbow flexor spasticity following stroke 4 weeks after BtA injection to the elbow flexor muscles in 14 subjects using MAS, EMG, and elbow and grip strength measures. They observed that while MAS was unable to detect changes, EMG activity reduced while elbow and grip strength increased. They concluded that the MAS is an inappropriate measure of spasticity, and that BtA treatment reduces spasticity measured by EMG activity, but does not necessarily cause a reduction in force generating capabilities of the joint. There is however some suggestion that when BtA injections occur over a prolonged period, muscle atrophy (Dressler and Adib Saberi 2005; Fortuna et al. 2011) and a loss of contractile tissue occurs (Fortuna et al. 2011), while other authors (Naumann et al. 2006) suggest that there are no persistent histological changes in the nerve terminal or the target muscle.
Though there is some doubt regarding the reversibility of BtA (Gough et al. 2005) there are no current published studies looking at the long term effect of BtA on human muscle, but several animal studies have raised concerns that BtA may have long-term effects. Chen et al. (2002) looked at the effect of BtA on juvenile rat gastrocnemius muscle, and found that its use lead to decreased muscle fibre cross-sectional area and muscle mass. This was not reversed by exercise, and they suggested that BtA injections could compromise muscle growth. More recently a study using rabbits (Galli et al. 2007) suggested that repeated BtA injections could cause muscle atrophy and a loss of contractile tissue. Clearly more research is needed to assess the long-term effect of BtA injection in human muscle tissue.
In a review of the use of botulinum neurotoxins Koussoulakos (2009) states “The experimental clinical studies carried out so far to test the efficacy of botulinum neurotoxins in various pathological circumstances are not considered fully reliable on universal standards.” The author goes on to note that even for well-designed and well-performed experimental studies outcomes may be affected by placebo effects to the control group (Willis et al. 2007) or to a lack of objectivity in subjective evaluation that may be affected by the patients mood. Despite this the author suggests the reality of the nontoxicity of BtA and reported health improvements support its use. The description of the benefits of BtA injection to the large numbers of patients across many studies varies a great deal.
It is difficult to compare results due to the wide variety of assessments used such as pain, muscle tone, joint angles or walking speed, and the range of muscles and muscle groups (both upper and lower body) treated. While some level of flexibility is necessary for clinical studies especially in the face of limited numbers of patients suffering from highly variable pathologies a complete understanding of the efficacy of BtA injection is impossible without some consistence and highly repeatable form of measurement which is flexible enough to be used across multiple joints in both the upper and lower body. Koussoulakos (2009) suggests that the following questions need to be answered, “(a) which muscles are better targets for maximalization of functional profit for each patient, (b) what are the optimal doses, (c) does an increase in the injected dose restrict the number of treated muscles, and (d) what is the most effective combination of various treatments for each case?”
Discussions of the effect of BtA treatments are usually based on outcome measures such as walking speed or joint angle changes, which are accurate when measured in a gait laboratory, however such measurements do not have the specificity to adequately answer the questions posed above. The effect on muscle mechanics following treatment by BtA injection is also not well understood. For the treatment of CP the stated goal may be to weaken muscles (Gough et al. 2005), which may not be a desirable longterm outcome. The actual requirement may be to delay the onset of the heightened stretch reflex so that it occurs at greater joint angles or higher angular velocities when greater muscle strength may be beneficial.
When treating spasticity, it is important not only to focus on the spasticity, but to remember the other deficits which may be more functionally limiting than the spasticity itself. While many clinical studies have shown improvements from BtA treatments for spasticity one of the few quantitative studies (Chen et al. 2005) showed that changes in muscle behavior might be present following treatment that was not apparent to qualitative assessment. There is a potential benefit to those who treat spasticity through the use of BtA injection from a greater understanding of the short and longer term effects of such treatments on the angle and speed at which the stretch reflex becomes apparent as well as the long term effects on muscle structure and strength.
While BtA injection is by no means the only treatment of spasticity it is one that is common and gaining popularity. This review of how its effect has been measured and reported in the literature serves to highlight the importance of accurate and repeatable quantifiable measures not only for the most beneficial and cost effective treatment of spastic muscles but also for the assessment of any clinical treatment.
7 General Recommendations
The measures that may be most applicable in a given situation will depend on the purpose for which the measurement is to be used. Most of the reasons to perform spasticity measurement may be qualified to one of the following categories:
-
1.
Clinical
-
Diagnosis.
-
Assessment of severity.
-
Evaluation of response to therapy
-
-
2.
Research
-
Understanding biomechanical and electrophysiological features of spasticity in different pathologies.
-
Understanding the effect of different therapies on every component of spasticity.
-
Generation of models to standardize and optimize management of spasticity with different therapies and to make predictions of response to treatment.
-
Each measurement technique has different requirements for complexity and accuracy (and impact on the subject) ranging from a yes/no in the case of diagnosis, to an accurate assessment of the velocity or muscle length required for the onset of the stretch reflex in a particular muscle.
The goal of diagnosis is to identify the existence of spasticity in different parts of the body, as a result of the UMNS, or to assess the extent of symptoms following SCI. In this case it is important to determine if a particular muscle is affected by the spasticity, rather than to quantify with accuracy the severity of spasticity. Thus, the popular qualitative measures, such as Ashworth or Tardieu Scales, which give a basic indication of level of involvement, are suitable. The tendon tap method may also be applicable for assessments that are limited to the knee joint.
In order to apply the correct treatment, and to track the evolution of the disease, it is often necessary to assess the severity of spasticity. The measure used in this case must quantify the severity of spasticity accurately, provide repeatable results, be applicable for various muscles and should not be too complex to apply. In these cases the instrumented muscle stretching measures in which force is administered either manually, or by the device (e.g. isokinetic dynamometry), may be applicable. However, these measures should ideally be accompanied by EMG measurements in order to distinguish between the 22 neural and muscular origins of increased muscle stiffness, and to track changes in muscle tissue properties. An automated tendon tapping device could also be used for the above application, however, its reliability is not yet proven and its construction needs adaption to allow reflex measurement for various joints.
The same measures as used for assessment of spasticity severity, can often be used for the assessment of therapy outcomes, however, the therapy outcomes measurement may not need to focus on the spasticity itself, but instead on how the severity of spasticity, and the muscles involved, effect the quality of daily living. Thus, movement analysis and energy expenditure measurements during functionally relevant movements may also be applicable.
The goal of research is to obtain a better understanding of spasticity, its influence on movement, the origin of the increased muscle stiffness, and the influence of the body adaptation mechanisms to the new conditions. Here it is necessary to distinguish between various components of the stiffness. In such a case the reliability of the method is more important than its ease of application. In these cases system identification techniques, such as those where force is applied at various velocities in order to distinguish between various components of spasticity or electrophysiological methods, will be most appropriate. These techniques would also allow a better understanding of the way in which different agents act on the different components of spasticity.
8 Conclusions and Future Challenges
Quantifying spasticity is important for evaluating of the effects of the treatment, but although it is an easy to recognize the phenomenon, it is much more difficult to quantify it (Biering-Sorensen et al. 2006). It is not surprising, given the variations in understanding of what spasticity is, that there is no agreement on the way in which it should be measured (Wood et al. 2005).
Quantitative measurements are widely used for research purposes and are more accurate than qualitative clinical techniques. However, these procedures are less practical for use in a clinical environment, where test application requires rapid testing methods that do not cause significant delays in medical practice. When selecting the spasticity measurement method a trade-off has to be made between reliability and reproducibility of the obtained results on one side, and the complexity of the set-up used and time necessary to perform the measurement on the other side.
As new measuring devices and techniques are developed, they will gradually generate a better understanding of the causes and symptoms of spasticity, and this will in turn allow more targeted diagnostic tools to improve treatment and further our understanding of the condition.
References
Ansari NN, Naghdi S, Hasson S, Azarsa MH, Azarnia S (2008) The modified Tardieu scale for the measurement of elbow flexor spasticity in adult patients with hemiplegia. Brain Inj 22(13–14):1007–1012
Argyriou AA, Karanasios P, Makridou A, Makris N (2010) F-wave characteristic as surrogate markers of spasticity in patients with secondary progressive multiple sclerosis. J Clin Neurophysiol 27(2):120–125
Ashworth B (1964) Preliminary trial of carisoprodal in multiple sclerosis. Practitioner 192:540–542
Biering-Sorensen F, Nielsen JB, Kling K (2006) Spasticity-assessment: a review. Spinal Cord 44:708–722
Blasi J, Chapman ER, Link E, Binz T, Yamasaki P, De Camilli S, Südhof TC, Niemann H, Jahn R (1993) Botulinum neurotoxin A selectively cleaves the synaptic protein SNAP-25. Nature 365(6442):160–163
Blicher JU, Nielsen JF (2009) Evidence of increased motoneuron exciltability in stroke patients without clinical spasticity. Neurorehabil Neural Repair 23(1):14–16
Bohannon RW, Smith MB (1987) Interrater reliability of a modified Ashworth Scale of muscle spasticity. Phys Ther 67:206–207
Boiteau M, Richards F, Malouin CL (1995) Use of a hand-held dynamometer and a Kin-Com dynamometer for evaluating spastic hypertonia in children: a reliability study. Phys Ther 75:796–802
Boyd NR, Graham HK (1999) Objective measurement of clinical findings in the use of botulinum toxin type A for the management of children with cerebral palsy. Eur J Neurol 6:223–235
Boyd RN, Pliatsios V, Starr R, Wolfe R, Graham HK (2000) Biomechanical transformation of the gastroc-soleus muscle with botulinum toxin A in children with cerebral palsy. Dev Med Child Neurol 42(1):32–41
Brin MF (1997) Botulinum toxin: chemistry, pharmacology, toxicity, and immunology. Muscle Nerve Suppl 6:S146–S168
Burridge JH, Wood DE, Hermens HJ, Voerman GE, Johnson GR, Van Wijck F, Platz T, Gregoric M, Hitchcock R, Pandyan AD (2005) Theoretical and methodological considerations in the measurement of spasticity. Disabil Rehabil 27(1/2):69–80
Chardon M, Suresh NL, Rymer WZ (2009) A new method for reflex threshold estimation in spastic muscles. In: Conference proceeding of IEEE Engineering in Medicine and Biology Society, pp 5300–5303
Chardon MK, Suresh NL, Rymer WZ (2010) An evaluation of passive properties of spastic muscles in hemiparetic stroke survivors. In: Conference proceeding of IEEE Engineering in Medicine and Biology Society, pp 2993–2996
Chen CM, Stott NS, Smith HK (2002) Effects of botulinum toxin A injection and exercise on the growth of juvenile rat gastrocnemius muscle. J Appl Physiol 93(4):1437–1447
Chen JJ, Wu YN, Huang SC, Lee HM, Wang YL (2005) The use of a portable muscle tone measurement device to measure the effects of botulinum toxin type A on elbow flexor spasticity. Arch Phys Med Rehabil 86(8):1655–1660
Corry IS, Cosgrove AP, Walsh EG, McClean D, Graham HK (1997) Botulinum toxin A in the hemiplegic upper limb: a double-blind trial. Dev Med Child Neurol 39(3):185–193
Das TK, Park DM (1997) Effect of treatment with botulinum toxin on spasticity. Postgrad Med J 65(762):208–210
Davis EC, Barnes MP (2000) Botulinum toxin and spasticity. J Neurol Neurosurg Psychiatr 69(2):143–147
Dressler D, Adib Saberi F (2005) Botulinum toxin: mechanisms of action. Eur Neurol 53(1):3–9
Filippi GM, Errico P, Santarelli R, Bagolini B, Manni E (1993) Botulinum A toxin effects on rat jaw muscle spindles. Acta Otolaryngol 113(3):400–404
Fleuren JF, Voerman GE, Erren-Wolters CV, Snoek GJ, Rietman JS, Hermens HJ et al (2010) Stop using the Ashworth Scale for the assessment of spasticity. J Neurol Neurosurg Psychiatry 81:46–52
Fortuna R, Vaz MA, Youssef AR, Longino D, Herzog W (2011) Changes in contractile properties of muscles receiving repeat injections of botulinum toxin (Botox). J Biomech 44(1):39–44
Fryer G, Lamonte RJ, Simons DG (1972) An electronically controlled automatic reflex hammer. Med Biol Eng 10:125–129
Galli M, Cimolin V, Valente EM, Crivellini M, Ialongo T, Albertini G (2007) Computerized gait analysis of botulinum toxin treatment in children with cerebral palsy. Disabil Rehabil 29(8):659–664
Gómez-Soriano J, Taylor J (2010) Spasticity after a spinal cord injury: review of the pathophysiology mechanisms, diagnostic techniques and current physiotherapy treatments. Fisioterapia 32:89–98
Gómez-Soriano J, Cano-de-la- Cuerda R, Muñoz-Hellín E, Ortiz- Gutiérrez R, Taylor JS (2012) Valoración y cuantificación de la espasticidad: revisión de los métodos clínicos, biomecánicos y neurofisiológicos. Rev Neurol 55:217–226
Gooch JL, Sandell TV (1996) Botulinum toxin for spasticity and athetosis in children with cerebral palsy. Arch Phys Med Rehabil 77(5):508–511
Gottlieb GL, Agarwal GC, Penn R (1978) Sinusoidal oscillation of the ankle as a means of evaluating the spastic patient. J Neurol Neurosurg Psychiatry 41:32–33
Gough M, Fairhurst C, Shortland AP (2005) Botulinum toxin and cerebral palsy: time for reflection? Dev Med Child Neurol 47(10):709–712
Gracies JM, Marosszeky JE, Renton R, Sandanam J, Gandevia SC, Burke D (2000) Short-term effects of dynamic lycra splnts on upper limb in hemiplegic patients. Arch Phys Med Rehabil 81:1547–1555
Graham HK, Aoki KR, Autti-Rämö I, Boyd RN, Delgado MR, Gaebler-Spira DJ, Gormley ME, Guyer BM, Heinen F, Holton AF, Matthews D, Molenaers G, Motta F, PGarcía Ruiz PJ, Wissel J (2000) Recommendations for the use of botulinum toxin type A in the management of cerebral palsy. Gait Post 11(1): 67–79
Heckman CJ, Rymer WZ (2008) Spinal mechanisms for control of muscle length and force. In: Conn PM (ed) Neuroscience in medicine, 3rd edn. Humana Press, Totowa, pp 443–448
Hiersemenzel LP, Curt A, Dietz V (2000) From spinal shock to spasticity. Neuronal adaptations to a spinal cord injury. Neurology 54:1574–1582
Howell K, Selber P, Graham HK, Reddihough D (2007) Botulinum neurotoxin A: an unusual systemic effect. J Paediatr Child Health 43(6):499–501
Hunter IW, Kearney RE (1982) Dynamics of human ankle stiffness: variation with mean ankle torque. J Biomech 15:747–752
Ivanhoe CB, Reistetter TA (2004) Spasticity: the misunderstood part of the upper motor neuron syndrome. Am J Phys Med Rehabil 83:S3–S9
Johnson GR (2002) Outcome measures of spasticity. Eur J Neurol 9(Suppl 1):10–16
Kamper DG, Rymer WZ (2000) Quantitative features of the stretch response of extrinsic finger muscles in hemiparetic stroke. Muscle Nerve 23:954–961
Katz RT, Rymer WZ (1989) Spastic hypertonia: mechanisms and measurement. Arch Phys Med Rehabil 70:144–155
Kearney RE, Stein RB, Parameswaran L (1997) Identification of intrinsic and reflex contributions to human ankle stiffness dynamics. IEEE Trans Biomed Eng 44:493–504
Kheder A, Nair KP (2012) Spasticity: pathophysiology, evaluation and management. Pract Neurol 12(5):289–298
Kim KS, Seo JH, Song CG (2011) Portable measurement system for the objective evaluation of the spasticity of hemiplegic patients based on the tonic stretch reflex threshold. Med Eng Phys 33:62–69
Kolaski K, Ajizian SJ, Passmore L, Pasutharnchat N, Koman LA, Smith BP (2008) Safety profile of multilevel chemical denervation procedures using phenol or botulinum toxin or both in a pediatric population. Am J Phys Med Rehabil 87(7):556–566
Koussoulakos S (2009) Botulinum neurotoxin: the ugly duckling. Eur Neurol 61(6):331–342
Lamontagne A, Malouin F, Richards CL, Dumas F (1998) Evaluation of reflex- and nonreflex-induced muscle resistance to stretch in adults with spinal cord injury using hand-held and isokinetic dynamometry. Phys Ther 78:964–975; discussion 976–978
Lance J (1980) Symposium synopsis. In: Feldman RG, Young RR, Koella WP (eds). Spasticity: disordered motor control. Year Book Medical Publishers, Chicago, pp 485–494 (Med Eng Phys, 2011 33:62–69)
Lebiedowska M, Fisk J, Spira-Gaebler D, Burns R (2003) The resistance of a knee joint to externally imposed movement in patients with cerebral palsy. In: Conference proceeding eighth annual meeting GCMAS, pp 6–9
Lehmann JF, Price R, de Lateur BJ, Hinderer S, Traynor C (1989) Spasticity: quantitative measurements as a basis for assessing effectiveness of therapeutic intervention. Arch Phys Med Rehabil 70:6–15
Leslie G, Muir C, Part N, Roberts RA (1992) Comparison of the assessment of spasticity by the Wartenberg pendulum test and the Ashworth grading scale in patients with multiple sclerosis. Clin Rehabil 6:41–48
Lin CC, Ju MS, Lin CW (2003) The pendulum test for evaluating spasticity of the elbow joint. Arch Phys Med Rehabil 84:69–74
Liu J, Xu D, Ren Y, Zhang LQ (2011) Evaluations of neuromuscular dynamics of hyperactive reflexes poststroke. J Rehabil Res Dev 48(5):577–586
Lukban MB, Rosales RL, Dressler D (2009) Effectiveness of botulinum toxin A for upper and lower limb spasticity in children with cerebral palsy: a summary of evidence. J Neural Transm 116(3):319–331
Manschot A, van Passel L, Algra A, van Gijn J (1998) Mayo and NINDS scales for assessment of tendon reflexes: between observer agreement and implications for communication. J Neurol Neurosurg Psychiatry 64:253–255
Marciniak C, Rader L, Gagnon C (2008) The use of botulinum toxin for spasticity after spinal cord injury. Am J Phys Med Rehabil 87(4):312–317
Maynard FM, Karunas RS, Waring WP 3rd (1990) Epidemiology of spasticity following traumatic spinal cord injury. Arch Phys Med Rehabil 71:566–569
Mehrholz J, Wagner K, Meissner D, Grundmann K, Zange C, Kock R, Pohl M (2005) Reliability of the Modified Tardieu Scale and the Modified Ashworth Scale in adult patients with severe brain injury: a comparison study. Clin Rehabil 19(7):751–759
Mejia NI, Vuong KD, Jankovic J (2005) Long-term botulinum toxin efficacy, safety, and immunogenicity. Mov Disord 20(5):592–597
Meythaler JM, DeVivo MJ, Hadley M (1996) Prospective study on the use of bolus intrathecal baclofen for spastic hypertonia due to acquired brain injury. Arch Phys Med Rehab 77:461–466
Meythaler JM, Guin-Renfroe S, Johnson A, Brunner RM (2001) Prospective assessment of tizanidine for spasticity due to acquired brain injury. Arch Phys Med Rehabil 82:1155–1163
Min JH, Shin YI, Joa KL, Ko SH, Shin MJ, Chang JH, Ko HY (2012) The correlation between modified Ashworth scale and biceps T-reflex and inter-rater and intra-rater reliability of biceps T-reflex. Ann Rehabil Med 36(4):538–543
Mirbagheri MM, Settle K, Harvey R, Rymer WZ (2007) Neuromuscular abnormalities associated with spasticity of upper extremity muscles in hemiparetic stroke. J Neurophysiol 98:629–637
Moore ST, MacDougall HG, Gracies JM, Cohen HS, Ondo WG (2007) Long-term monitoring of gait in Parkinson’s disease. Gait Post 26(2):200–207
National institute of neurological disorders and stroke. http://www.ninds.nih.gov
Naumann M, Albanese A, Heinen F, Molenaers G, Relja M (2006) Safety and efficacy of botulinum toxin type A following long-term use. Eur J Neurol 13(Suppl 4):35–40
Numanoglu A, Günel MK (2012) Intraobserver reliability of modified Ashworth scale and modified Tardieu scale in the assessment of spasticity in children with cerebral palsy. Acta Orthop Traumatol Turc 46(3):196–200
Opara J, Hordyńska E, Swoboda A (2007) Effectiveness of botulinum toxin A in the treatment of spasticity of the lower extremities in adults—preliminary report. Ortop Traumatol Rehabil 9(3):277–285
Pandyan AD, Johnson GR, Price CIM, Curless RH, Rodgers H, Barnes MP (1999) A review of the properties and limitations of the Ashworth and modified Ashworth Scales as measures of spasticity. Clin Rehab 13:373–383
Pandyan AD, Price CI, Rodgers H, Barnes MP, Johnson GR (2001) Biomechanical examination of a commonly used measure of spasticity. Clin Biomech 16:859–865
Pandyan AD, Vuadens P, van Wijck FMJ, Stark S, Johnson GR, Barnes MP (2002) Are we underestimating the clinical efficacy of botulinum toxin (type A)? Quantifying changes in spasticity, strength and upper limb function after injections of Botox® to the elbow flexors in a unilateral stroke population. Clin Rehabil 16:654–660
Paulis WD, Horemans HLD, Brouwer BS, Stam HJ (2011) Excellent test-retest and inter-rater reliability for Tardieu Scale measurements with inertial sensors in elbow flexors for stroke patients. Gait Post 33:185–189
Penn RD, Savoy SM, Corcos DM, Latash M, Gottlieb G, Parke B et al (1989) Intrathecal baclofen for severe spinal spasticity. N Engl J Med 320:1517–1522
Phadke CP, Thompson FJ, Kukulka CG, Nair PM, Bowden MG, Madhavan S, Trimble MH, Behrman AL (2010) Soleus H-reflex modulation after motor incomplete spinal cord injury: effects of body position and walking speed. J Spinal Cord Med 33(4):371–378
Platz T, Eickhof C, Nuyens G, Vuadens P (2005) Clinical scales for the assessment of spasticity, associated phenomena and function: a systematic review of the literature. Disabil Rehabil 27(1–2):7–18
Powers RK, Marder-Meyer J, Rymer WZ (1988) Quantitative relations between hypertonia and stretch reflex threshold in spastic hemiparesis. Ann Neurol 23:115–124
Powers RK, Campbell DL, Rymer WZ (1989) Stretch reflex dynamics in spastic elbow flexor muscles. Ann Neurol Sens Mot Perform Program 25:32–42
Priebe MM, Sherwood AM, Thornby JI, Kharas NF, Markowski J (1996) Clinical assessment of spasticity in spinal cord injury: a multidimensional problem. Arch Phys Med Rehabil 77:713–716
Pullman SL, Greene P, Fahn S, Pedersen SF (1996) Approach to the treatment of limb disorders with botulinum toxin A. Experience with 187 patients. Arch Neurol 53(7):617
Py AG, Zein Addeen G, Perrier Y, Carlier RY, Picard A (2009) Evaluation of the effectiveness of botulinum toxin injections in the lower limb muscles of children with cerebral palsy. Preliminary prospective study of the advantages of ultrasound guidance. Ann Phys Rehabil Med 52(3):215–223
Rabita G, Dupont L, Thevenon A, Lensel-Corbeil G, Pérot C, Vanvelcenaher J (2005) Quantitative assessment of the velocity-dependent increase in resistance to passive stretch in spastic plantarflexors. Clin Biomech 20:745–753
Rack PM, Ross HF, Thilmann AF (1984) The ankle stretch reflexes in normal and spastic subjects. The response to sinusoidal movement. Brain 107(P2):637–654
Singh P, Joshua AM, Ganeshan S, Suresh S (2011) Intra-rater reliability of the modified Tardieu scale to quantify spasticity in elbow flexors and ankle plantar flexors in adult stroke subjects. Ann Indian Acad Neurol 14(1):23–26
Sommerfeld DK, Eek EU, Svensson AK, Holmqvist LW, Von Arbin MH (2004) Spasticity after stroke: its occurrence and association with motor impairments and activity limitations. Stroke 35:134–139
Stefanovska A, Vodovnik L, Gros N, Rebersek S, Acimović-Janezic R (1989) FES and spasticity. IEEE Trans Biomed Eng 36:738–745
Tardieu G, Shentoub S, Delarue R (1954) Research on a technic for measurement of spasticity. Rev Neurol (Paris) 91:143–144
Vles GF, de Louw AJ, Speth LA, van Rhijn LW, Janssen-Potten YJM, Hendriksen JG, Vles JSH (2008) Visual analogue scale to score the effects of botulinum toxin A treatment in children with cerebral palsy in daily clinical practice. Eur J Paediatr Neurol 12(3):231–238
Voerman GE, Gregoric M, Hermens HJ (2005) Neurophysiological methods for the assessment of spasticity: the Hoffman reflex, the tendon reflex and the stretch reflex. Disabil Rehabil 27(1–2):33–68
Walker HK, Hall WD, Hurst JW (1990) Deep tendon reflexes. Clinical methods: the history, physical and laboratory examinations, 3rd edn. (Chapter 72). Butterworths, Boston
Walsh E (1992) Thixotropy: a time dependent stiffness. In: Muscles masses and motion: the physiology of normality, hypotonicity, spasticity and rigidity, vol 125. Cambridge University Press, Cambridge, pp 78–102
Wartenberg R (1951) Pendulousness of the legs as a diagnostic test. Neurology 1:18–24
Willis AW, Crowner B, Brunstrom JE, Kissel A, Racette BA (2007) High dose botulinum toxin A for the treatment of lower extremity hypertonicity in children with cerebral palsy. Dev Med Child Neurol 49(11):818–822
Wood DE, Burridge JH, Van Wijck FM, McFadden C, Hitchcock RA, Pandyan AD, Haugh A, Salazar-Torres JJ, Swain ID (2005) Biomechanical approaches applied to the lower and upper limb for the measurement of spasticity: a systematic review of the literature. Disabil Rehabil 27(1/2):19–32
Yates C, Garrison K, Reese NB, Charlesworth A, Garcia-Rill E (2011) Chapter 11: novel mechanism for hyperreflexia and spasticity. Prog Brain Res 188:167–180
Zhang LQ, Wang G, Nishida T, Xu D, Sliwa JA, Rymer WZ (2000) Hyperactive tendon reflexes in spastic multiple sclerosis: measures and mechanisms of action. Arch Phys Med 81(7):901–909
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Pajaro-Blázquez, M., Maciejasz, P., McCamley, J., Collantes-Vallar, I., Copaci, D., Rymer, W.Z. (2014). Challenges in Measurement of Spasticity in Neurological Disorders. In: Pons, J., Torricelli, D. (eds) Emerging Therapies in Neurorehabilitation. Biosystems & Biorobotics, vol 4. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-38556-8_7
Download citation
DOI: https://doi.org/10.1007/978-3-642-38556-8_7
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-38555-1
Online ISBN: 978-3-642-38556-8
eBook Packages: EngineeringEngineering (R0)