Abstract
This chapter is intended to give an overview of the influence of hormone replacement therapy in cardiovascular disease, broadly talking about the epidemiology of cardiovascular disease in women and the possible mechanisms by which hormone replacement therapy may be a cardioprotective factor. They also comment on recent controversies on this subject and present indications of HRT.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Postmenopausal Woman
- Hormone Replacement Therapy
- Coronary Heart Disease Risk
- Tissue Factor Pathway Inhibitor
- Medroxyprogesterone Acetate
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The predominant perception for many years has been that coronary artery disease is a rare occurrence in women, especially in young women, leading to the view that arteriosclerotic disease of the vascular tree is less important in women overall. Both perceptions are incorrect (Knopp 1998). Cardiovascular disease across the entire lifetime is slightly more common as a cause of mortality in women than in men. In the middle-age years, cardiovascular disease is associated with multiple risk factors, possibly with more in women than one sees with men of the same age having coronary artery disease (Knopp 1998). Postmenopausal hormone replacement is a very important therapy, but it is not entirely without side effects. Until less than a decade ago, it was thought that hormone replacement therapy might be beneficial for the prevention of cardiovascular disease in postmenopausal women but is now considered to be ineffective both as primary or as secondary preventions and even that it can increase venous thromboembolic events and stroke (The Cochrane Collaboration 2013).
Epidemiology
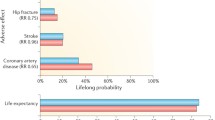
Overall, one in five women has some form of CVD, but this proportion varies depending on age: only one in seven women has CVD at ages 45–64 years, but almost one in three women has CVD at age older than 65.
Although the death rate from CVD in men has declined, the mortality rate has remained relatively constant for women.
Although women develop coronary artery disease (CAD) on average 10–20 years later than men, because they constitute a much larger proportion of the population older than 65, more women than men die annually of myocardial infarction.
Differences between men and women have been identified for the impact of diabetes and dyslipidemia on female health as well as the effect of combinations of risk factors on distribution of vascular disease in the arterial tree. It has long been recognized that women have greater increment in susceptibility to diabetes than men, resulting in diabetic women having a coronary disease rate equaling or approaching that of men (Table 1). Diabetes in women increases cardiovascular risk by three- to sevenfold compared with a two- to threefold increase for men.
Women tend to have a 10–15 year delay in the curve describing the rise in cardiovascular disease. The leading condition embodying multiple risk factors is the metabolic syndrome, also known as insulin-resistance syndrome or syndrome X (Knopp 1998). This syndrome is associated with obesity, a propensity to hypertension, overt diabetes, and combined hyperlipidemia consisting of elevated plasma triglyceride, very low-density lipoprotein cholesterol (VLDL-C), intermediate-density lipoprotein cholesterol (IDL-C), low-density lipoprotein cholesterol (LDL-C), small dense LDL, and low high-density lipoprotein cholesterol (HDL-C).
Oral Contraceptive Use in Cardiovascular Disease Risk
The putative benefits of the use of hormone replacement therapy for the prevention of clinical coronary artery disease among postmenopausal women have been documented by most, but not all, observational studies (Sidney et al. 1997; Mosca et al. 1998; Meilahn 1999). Barrett- Connor and Grady (1998) estimated that, comparing users versus nonusers, estrogen therapy alone was associated with about a 35–50 % reduction and estrogen-progesterone with about 33 % reduction in the risk of coronary disease. The Nurses’ Health Study research group (Grodstein et al. 1996, 1997) estimated that there was about a 20 % reduction in cardiovascular disease among hormone users and a 30 % reduction in risk. The results of these observational studies have led to widespread use of HRT among postmenopausal women for the prevention of cardiovascular disease (Meilahn 1999).
When introduced in the 1960s, the oral contraceptive pills contained between 100 and 150 μg of ethinyl estradiol, which is about 10 times the postmenopausal replacement amount (Knopp 1998). The doses of oral contraceptive estrogens have declined over the ensuing decades to 20–35 μg daily of ethinyl estradiol which is about 1.3–2 times postmenopausal replacement levels. Even at these doses, venous thrombosis still occurs (Lewis et al. 1996). Several studies in the mid- and late 1980s have verified the earlier epidemiological surveys that show that even with lower estrogen dose oral contraceptives, the risk of coronary artery disease in cigarette smoking oral contraceptive user is about tenfold increased from baseline and about three- to fourfold above the risk of cigarette smoking alone for coronary artery disease (Rosenberg et al. 1985). The current oral contraceptives have much lower estrogen content and do not appear to increase the risk of myocardial infarction or stroke; however, there is still a twofold increased risk of deep venous thrombosis or pulmonary embolism. Women smokers who use oral contraceptives are more likely to develop hypertension, heart attack, and stroke than nonsmokers, a risk that increases with age. Therefore, oral contraceptives are contraindicated in female smokers older than 35 years.
Mechanism of Action
The mechanisms of the increased risk of coronary artery disease in postmenopausal women and its prevention by hormone replacement treatment have not been fully elucidated (Lip et al. 1997). Abnormalities in plasma coagulation factors, which are indicative of a prothrombotic state, may partly account for this risk in postmenopausal women compared with premenopausal state. Many such prothrombotic factors exist, which have been generally associated with cardiovascular risk. For example, elevated plasma fibrinogen levels which are associated with an increased risk of coronary heart disease and stroke may promote the disease by increasing fibrin formation and platelet aggregation or by rheologic effects on blood viscosity and red cell aggregation, which may promote disturbed blood flow (Edmunds and Lip 2000). Plasminogen activator inhibitor (PAI) is an index of fibrinolysis, and thus, high levels are a marker of increased thrombogenesis (Dawson and Henney 1992).
Plasma fibrin D-dimer levels are an index of fibrin turn over and thus of ongoing intravascular thrombogenesis. The levels of plasma fibrin D-dimer are elevated in venous thrombosis and peripheral arterial disease and in patients at risk of coronary heart disease (Lip and Love 1995). Lipoprotein A is a lipid fraction that is closely associated with thrombogenesis and atherogenesis (Lip and Jones 1995). In addition, endothelial function has been implicated in atherogenesis and cardiovascular disorders (Blann and Taberner 1996). Various markers of endothelial functions have been suggested. Plasma von Willebrand factor (vWF), for example, is a marker of endothelial disturbance that is associated with thromboembolic stroke, coronary heart disease, and peripheral arterial disease (Lip and Blann 1995). The soluble leukocyte adhesion molecule P-selectin is also increased in atherosclerosis (Blann et al. 1995) and is a possible marker of platelet activation (Chong et al. 1994). Other plasma factors that may be important in atherosclerosis and have been suggested as markers of endothelial function include soluble thrombomodulin (sTM) and tissue plasminogen activator antigen (TPA) (Blann and Taberner 1996).
Lip et al. (1997) studied the effect of estrogen-only HRT (oral conjugated estrogen as Premarin, 0.625 mg) on 27 premenopausal women undergoing hysterectomy and bilateral salpingo-oophorectomy. They found that there was a significant elevation in sTM and a trend toward higher median soluble P-selectin, PAI, and mean TPA levels. There was also a significant reduction in mean vWF levels compared with premenopausal levels. They felt that their study showed that HRT had some beneficial effects on endothelial function, probably as a result of a combination of both enhanced inotropism and vasodilation with direct effects on the arterial system by other endothelial products such as nitric oxide.
In the Framingham Offspring Study (Otavio et al. 1995), the investigators measured PAI-1 and TPA antigen levels in 1,431 participants. They found that women receiving hormone replacement therapy had 35 % lower levels of PAI-1 than postmenopausal women not receiving hormones. Premenopausal women had a lower mean level of PAI-1 levels than men of comparable age. PAI-1 levels in postmenopausal women not receiving hormone replacement therapy did not differ from those observed in older men. Premenopausal women had a 25 % lower level of PAI-1 antigen levels than postmenopausal women not receiving hormones. Postmenopausal women receiving hormones had lower levels of TPA than those not receiving hormones. Plasma triglycerides were significantly correlated with PAI-1 and TPA antigen levels. They concluded that the protective effect of estrogen against coronary heart disease may be due in part to the beneficial effects on fibrinolysis.
Bonduki et al. (1998) investigated the effect of estrogen and progestin hormone replacement therapy on antithrombin III (AT III) levels in climacteric women, comparing oral to transdermal routes of estrogen administration. They found that there was a statistically significant reduction of plasma AT III levels in patients receiving oral conjugated estrogen, whereas patients who received transdermal 17-β-estradiol presented no change. Harris et al. (1999) studied the effect of the use of combined oral contraceptives on tissue factors pathway inhibitor (TFPI). They found that ethinyl estradiol in doses between 30 and 50 μg per day in combination with a variety of progestagens resulted in a 25 % reduction in TFPI antigen and 29 % decrease in activity. TFPI is the major physiological inhibitor of factor 7A activity indicating activation of the extrinsic coagulation pathway. Changes in the plasma TFPI levels may be an important factor in the procoagulant and thrombotic risks associated with oral contraceptive use.
In contrast, Scarabin et al. (1993) concluded that their study showed a potentially protective effect of HRT against an increased thrombotic tendency. They measured hemostatic variables in 293 consecutive healthy women aged 45–54 years who attended a health checkup center in Paris. Most women using HRT were given 17-β-estradiol in combination with progestin. Mean levels of plasma fibrinogen, factor 8 coagulant activity, and plasminogen activator inhibitor were significantly higher in postmenopausal women not taking HRT than premenopausal women within the same decade. HRT significantly reversed the menopause-related changes in factor 7.
In a review of estrogen and coronary heart disease in women (Barrett-Connor and Bush 1991), the authors found that with the exception of two studies all of the data on known contraceptive estrogen use and coronary heart disease risk in women are observational. Women using the estrogens had significantly less coronary artery stenosis than women not using estrogen. Eleven of the 24 published reports reviewed in their paper showed statistically significant reductions in coronary heart disease risk among women using estrogens. The authors therefore concluded that the weight of evidence pointed toward a substantial reduction in coronary heart disease risk among women using estrogens. They however added that these studies probably were inherently biased as women taking estrogen therapy were by definition compliant women.
Nabulsi et al. (1993) examined the association of hormone replacement therapy with concentrations of plasma lipids and hemostatic factors, fasting serum concentrations of glucose, and insulin and blood pressure on 4,958 postmenopausal women using estrogen alone (83 %) or using estrogen and progestin (17 %). They found that oral contraceptive users had a higher mean level of high-density lipoprotein cholesterol and apolipoprotein A1 than nonusers and lower mean levels of low-density lipoprotein cholesterol, apolipoprotein B, lipoprotein (a), fibrinogen, antithrombin III, and fasting serum glucose and insulin. They concluded that the use of estrogen combined with progestin appeared to be associated with a better profile than the use of estrogen alone.
Koh et al. (1997) studied the effect of hormone replacement therapy on PAI-1 levels. In a randomized crossover study, they investigated the effects of oral conjugated estrogen (0.625 mg per day) in 30 postmenopausal women and transdermal estradiol (0.1 mg per day) in 20 postmenopausal women either alone or in combination with medroxyprogesterone acetate (2.5 mg daily for one month) and plasma PAI-1 antigen levels. They measured the degradation products of cross-linked fibrin (D-dimer) as an index of fibrinolysis. PAI-1 levels were inversely associated with D-dimer levels at baseline. Conjugated estrogen alone or in combination with progestin therapy reduced PAI-1 levels by approximately 50 % and was associated with enhanced systemic fibrinolysis.
The postmenopausal estrogen/progestin intervention (PEPI) trial (1995) tried to assess pairwise differences between placebo, unopposed estrogen, and each of the three estrogen/progestin regimens on selected heart disease risk factors in healthy postmenopausal women. This was a three-year, multicenter, randomized, double-blind, placebo-controlled trial. The investigators found that the estrogen alone or in combination with a progestin improved lipoproteins and lowered fibrinogen levels without detectable effects on postchallenge insulin or blood pressure. Unopposed estrogen was found to be the optimal regime for elevation of HDL-C. In women with uterus, conjugated equine estrogen with cyclic medroxyprogesterone had the most favorable effect on HDL-C and no excess risk of endometrial hyperplasia.
Controversies in Hormone Replacement Therapy and Heart Disease Prevention
The heart and estrogen/progestin replacement study (HERS) (Shlipak et al. 2000) attempted to determine the relationships among treatment with estrogen and progestin, serum, and lipoprotein (a) levels and subsequent coronary artery disease events in postmenopausal women. This was a randomized, blinded, placebo-controlled secondary prevention trial with a mean follow-up of 4.1 years at 20 centers. A total of 2,763 postmenopausal women younger than 80 years with coronary artery disease and an intact uterus and a mean age of 66.7 years were randomly assigned to receive either conjugated equine estrogen 0.625 mg plus medroxyprogesterone acetate 2.5 mg in one tablet daily or identical placebo. The investigators found that increased baseline lipoprotein (a) levels were associated with subsequent coronary artery disease even among women in the placebo arm.
In a randomized subgroup comparison, women with low baseline lipoprotein (a) levels had less benefit from estrogen and progestin than women with high lipoprotein (a) levels. The relative hazards (RH) for women assigned with estrogen and progestin compared with placebo were 1.49 (95 % confidence interval, 0.97–2.26) in the lowest quartile and 1.05 (95 % CI, 0.67–1.65), 0.78 (0.52–1.18), and 0.8 (0.58–1.25) in the second, third, and fourth quartiles, respectively. They concluded that lipoprotein (a) is an independent risk factor for recurrent coronary artery disease in postmenopausal women and that treatment with estrogen and progestin lowered lipoprotein (a) levels.
They also found that treatment with oral conjugated equine estrogen plus medroxyprogesterone acetate did not reduce the overall rate of coronary artery disease events in postmenopausal women with established coronary disease (Hulley et al. 1998).
Observation studies of estrogen replacement therapy and coronary artery disease are numerous, and most of them show a lower risk of reinfarction, coronary heart disease-related death, and coronary artery stenosis in users of estrogen replacement therapy. Reasons to view cautiously the observational results have always existed. Women with healthy behavior, such as those who follow a low-fat diet and exercise regularly, may selectively use postmenopausal hormone replacement treatment.
Estimates of relative risk (RR) of coronary artery disease in hormone users will be biased toward finding a protective effective hormone use for coronary artery disease (prevention bias) (Petitt 1998). Compliance bias is large enough to explain entirely reductions in the relative risk of coronary artery disease between users and nonusers of hormone replacement therapy of the magnitude found in observation studies (Petitt 1998). The Coronary Primary Prevention Trial (Lipid Research Clinics program 1984), the West of Scotland Coronary Prevention Study (Shepherd et al. 1995), the Helsinki Heart Study (Frick et al. 1987), and the Scandinavian Simvastatin Survival Study (1994) have all shown that lipid lowering can predict reductions in the risk of coronary artery disease and that lipid lowering can be used as a surrogate end point for coronary artery disease. For female hormones, beneficial lipid effects do not directly translate the reductions in the disease end points, at least in persons with coronary disease.
The lipid hypothesis has dominated thinking about coronary artery disease for at least four decades (Petitt 1998). There is growing recognition that thrombotic phenomena play an important role in acute coronary syndromes (Petitt 1998). HRT increases the risk of venous thrombosis. Blumenthal et al. (2000) stated that the failure of HERS to achieve a positive result does not disprove the estrogen/heart disease hypothesis since the trial was significantly underpowered.
The new selective estrogen receptor modulators (SERMs), for example, raloxifene, have also been associated with increased risk of venous thromboembolism (Kuller 2000). The risk of venous thrombosis increases with age among women. There is little evidence at present that the risk of venous thrombosis is lessened among women taking SERMs as compared with estrogen or estrogen-progesterone (Kuller 2000).
A possible scenario to explain the divergent results of observational studies and the only randomized control trial of the use of HRT on coronary artery disease in postmenopausal women may be that estrogen or estrogen-progesterone therapy reduces the progression of atherosclerotic disease and therefore decreases the risk of coronary heart disease but has an adverse effect (at least in some women) and exerts a proinflammatory response on vulnerable plaques. Thus, for women who have had an acute myocardial infarction and perhaps women with extensive coronary atherosclerosis and many vulnerable plaques, estrogen or estrogen-progesterone therapy may be associated at least in the short term with an increased risk of cardiovascular disease (Kuller 2000).
Since the early 1980s several observational studies consistently showed that HRT users, many of whom started treatment shortly after menopause, had a significant reduction in total mortality and risk of CVD events of approximately 30–50 % relative to women who chose not to use HRT (Grady 1992; Grodstein 1999; Grodstein 2000; Mann 1994; Psaty 1994; Rosenberg 1993; Stampfer 1991).
The publication of the results from the Heart and Estrogen/Progestin Replacement Study (HERS I 1998) and the Women’s Health Initiative (WHI I 2002) trials appeared to strongly contradict conventional clinical practice based on the evidence from observational studies (Women’s Health Initiative Study Group 1998; The Cochrane Collaboration 2013).
The HERS I results showed that there was an excess risk of CVD events in the HRT group in the first year on treatment, for the overall 4.2 years of follow-up, and there were no differences in CVD events between the HRT and placebo groups, coupled with an increased risk of both venous thromboembolism and pulmonary embolism. A further 2.7 years of follow-up still showed no CVD benefit (Grady et al. 1998).
The WHI I 2002 was a primary prevention trial conducted in 16,609 postmenopausal women without hysterectomy. Participants were randomly assigned to combination therapy or placebo. There was an excess risk of CVD in the first year and a nearly 30 % increased risk of coronary events after 5.6 years. A subgroup analysis of the 400 women included in the trial who had a history of myocardial infarction or coronary revascularization and showed a similar risk (The Cochrane Collaboration 2013; Grady et al. 1998).
After the results obtained in these studies interest alighted upon the timing of initiation of HT in relation to the time of menopause. This “timing hypothesis” suggests that there is a window of opportunity where HRT may be beneficial for prevention of CVD in women 10 years postmenopause but that in older women, it does not appear to have the same benefits and may be associated with excess CVD risk (The Cochrane Collaboration 2013).
In support of the “timing hypothesis,” a stratified meta-analyses indicated differential treatment effects with HRT relative to placebo according to the participants’ baseline age (Salpeter 2004). This study analyses assessed 30 RCTs which compared HRT with placebo that included 26,798 participants and reported at least one death, to assess the effect of HRT on total mortality, due to CV disease, cancer, or other causes. Results indicated a significantly reduced risk of death in women with a mean age of under 60 years taking HRT compared to a placebo group, though no difference was found when older women were compared (The Cochrane Collaboration 2013).
Conclusion
The question of whether premenopausal women are protected from atherosclerotic disease by virtue of their hormonal status still remains unanswered (Edmunds and Lip 2000). The same risk factors for cardiovascular disease appear to operate in women as in men. Smoking, hyperlipidemia, hypertension, and diabetes are significant risk factors for the development of coronary artery disease in women and should be treated aggressively.
The guidelines agreed to by members of the roundtable discussion are summarized in Table 2. Estrogen has demonstrated cardiovascular benefits in healthy postmenopausal women, but the magnitude of these benefits may decrease with increasing age, time since menopause, and the presence of CVD or CVD risk factors. (Daniel and Mendelsohn 2002) (Table 2).
Use of HRT is recommended for the management of perimenopausal vasomotor symptoms and for the prevention of osteoporosis. The cardiovascular effects of HRT, including the effects of both estrogen and progestin, should be taken into consideration when prescribing HRT for healthy postmenopausal women (Daniel and Mendelsohn 2002).
Improvements in menopausal symptoms assessed in health-related quality of life with oral HRT compared with placebo are suggestive that short-term therapy could be considered for use by women seeking relief from menopausal symptoms. Short-term HRT treatment should be at the lowest effective dosage with special consideration of transdermal administration (The Cochrane Collaboration 2013).
There is an additional need for research on the efficacy and safety of alternative methods for the relief of menopausal symptoms for women who may wish to avoid its use.
Abbreviations
- CAD:
-
Coronary artery disease
- CDV:
-
Cardiovascular disease
- HERS:
-
The heart and estrogen/progestin replacement study
- HRT:
-
Hormone replacement therapy
- SERMs:
-
Selective estrogen receptor modulators
- TPA:
-
Tissue plasminogen activator antigen
- WHI:
-
Women’s Health Initiative trial
References
Barrett- Connor E, Grady D (1998) Hormone replacement therapy, heart disease and other considerations. Annu Rev Public Health 19:55
Barrett-Connor E, Bush TL (1991) Estrogen and coronary artery disease in women. JAMA 265:1861–1867
Blann AD, Dobrotova M, Kubisz P, McCollum CN (1995) von Willebrand factor, soluble P-selectin, tissue plasminogen activator and plasminogen activator inhibitor in atherosclerosis. Thromb Haemost 74:626–630
Blann AD, Taberner DA (1996) A reliable marker of endothelial cell dysfunction: does it exist. Br J Haematol 90:244–248
Blumenthal RS, Zacur HA, Reis SE, Post WS (2000) Beyond the null hypothesis- Do the HERS results disprove the estrogen/coronary heart disease hypothesis? Am J Cardiol 85:1015–1017
Bonduki CE, Lourenco DM, Baracat E et al (1998) Effect of estrogen-progestin hormonal replacement therapy on plasma antithrombin-III of postmenopausal women. Acta Obstet Gynecol Scand 77:330–333
Castelli WP (1988) Cardiovascular disease in women. Am J Obstet Gynecol 158:1553–1560
Chong BH, Murray B, Berndt MC, Dunlop LC, Brighton T, Chesterman CN (1994) Plasma P-selectin is increased in thrombotic consumptive platelet disorders. Blood 83:1535–1541
Daniel RM Jr, Mendelsohn ME (2002) Introduction: the role of hormone replacement therapy in prevention and treatment of cardiovascular disease in postmenopausal women. Am J Cardiol 89(12A)
Dawson S, Henney A (1992) The status of PAI-1 as a risk factor for arterial and thrombotic disease: a review. Atherosclerosis 95:105–117
Edmunds E, Lip GYH (2000) Cardiovascular risk in woman: the cardiologists’ perspective. Q J Med 93:135–145
Frick MH, Elo O, Haapa K et al (1987) Helsinki Heart Study. Primary prevention trial with gemfibrozil in middle aged men with dyslipidaemia. Safety of treatment, changes in risk factors and incidence of coronary heart disease. N Engl J Med 317:1237–1245
Grady D, Applegate W, Bush T, Furberg C, Riggs B, Hulley S et al (1998) Heart and Estrogen/progestin Replacement Study (HERS): design, methods, and baseline characteristics. Control Clin Trials 19(4):314–335
Grodstein F, Manson JE, Stampfer MJ (1996) Postmenopausal hormone therapy. In: Manson JE, Ridker PM, Gaziano JM et al (eds) Prevention of myocardial infarction. Oxford University Press, New York, p 413
Grodstein F, Stampfer MJ, Colditz GA et al (1997) Postmenopausal hormone therapy and mortality. N Engl J Med 336:1769
Harris GM, Stendt CL, Vollenhoven BJ, Gan TE, Tipping PG (1999) Decreased plasma tissue factor pathway inhibitor in women taking combined oral contraceptives. Am J Hematol 60:175–180
Hulley SB, Grady D, Bush TL, Furberg C, Herrington D, Riggs B, Vittinghoff E (1998) Randomised trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal. JAMA 280:605–613
Knopp RH (1998) Estrogens, female gender and heart disease. In: Topol EJ (ed) Textbook of cardiovascular disease. Lippincott-Raven, Philadelphia, pp 195–218
Koh KK, Mincemoyer RRN, Bui MN, Csako G, Pucino F, Guetta V, Waclaviv M, Cannon RO III (1997) Effects of hormone replacement therapy on fibrinolysis in postmenopausal women. N Engl J Med 336:683–690
Kuller LH (2000) Hormone replacement therapy and coronary heart disease- A new debate. Med Clin North Am 84:181–195
Lewis MA, Spitzer W, Heinemann LAJ et al (1996) Third generation oral contraceptives and the risk of myocardial infarction: an international case–control study. BMJ 312:88–90
Lip GYH, Blann AD (1995) von Willebrand factor and its relevance to cardiovascular disease. Br Heart J 74:580–583
Lip GYH, Jones AF (1995) Lipoprotein(a) and vascular disease: thrombogenesis and atherogenesis. Q J Med 88:529–539
Lip GYH, Love GDO (1995) Fibrin D-dimer: a useful clinical marker of thrombogenesis. Clin Sci 89:205–214
Lip GYH, Blann AD, Jones AF, Beevers DG (1997) Effects of hormone replacement therapy on hemostatic factors, lipid factors and endothelial function in women undergoing surgical menopause: implications for prevention of atherosclerosis. Am Heart J 134:764–771
Meilahn E (1999) Sex steroid hormonal influences on coronary artery disease. In: Ness RB, Kuller LH (eds) Health and disease among women, biological and environmental influences. Oxford University Press, New York, pp 155–162
Nabulsi AA, Folsom AR, White A et al (1993) Association of hormone replacement therapy with various cardiovascular risk factors in postmenopausal women. N Engl J Med 328:1069–1075
Otavio CE, Gebara MD, Murray A et al (1995) Association between increased estrogen status and increased fibrinolytic potential in the Framingham offspring study. Circulation 91:1952–1958
Petitt DB (1998) Hormone replacement therapy and heart disease prevention: experimentation trumps observation. JAMA 280:650–651
Rosenberg L, Kaufman DW, Helmrich SP et al (1985) Myocardial infarction and cigarette smoking in women younger than 50 years of age. JAMA 253:2965
Scarabin P-Y, Plu-Bureau G, Bara L, Boniyhon-Kopp C, Guize L, Samama MM (1993) Haemostatic variables and menopausal status: influence of hormone replacement therapy. Thromb Haemost 70:584–587
Shepherd J, Cobb SM, Ford I et al (1995) Prevention of coronary heart disease with pravastatin in men with hypercholesterolaemia. The West of Scotland Coronary Prevention Study Group. N Engl J Med 333:1301–1307
Shlipak MG, Simon JA, Vittinghoff E, Lin F, Barrett-Connor E, Knopp RH, Levy RI, Hulley SB (2000) Estrogen and progestin, lipoprotein(a), and the risk of recurrent coronary heart disease events after menopause. JAMA 283:1845–1852
Sidney S, Petitti DB, Queensberry CP (1997) Myocardial infarction and the use of estrogen and estrogen-progesterone in postmenopausal women. Ann Intern Med 127:501
The Cochrane Collaboration (2013) Hormone therapy for preventing cardiovascular disease in post-menopausal women (Review). Wiley, New York
The Lipid Research Clinics program (1984) Lipid research clinics coronary primary prevention trial results; reduction in incidence of coronary heart disease. JAMA 251:351–364
The Scandinavian Simvastatin Survival Study (1994) Randomised study of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 344:1383–1389
The Writing Group for the PEPI trial (1995) Effects of estrogen or estrogen/progestin regimens on heart disease risk factors in postmenopausal women. JAMA 273:199–208
Women’s Health Initiative Study Group (1998) Design of the women’s health initiative trial and observational study. Control Clin Trials 19:61–109
Further Reading
Ernst E, Resch KL (1993) Fibrinogen as a cardiovascular risk: a meta-analysis and review of literature. Ann Intern Med 118:956–963
Mosca L, Manson JE, Sutherland SE et al (1997) Cardiovascular disease in women: a statement for healthcare professionals from the American Heart Association. Circulation 96:2468
Raymond JR, van den Berg EK, MJ K Jr (1988) Nontraumatic prehospital sudden death in young adults. Arch Intern Med 148:303–308
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this entry
Cite this entry
Fernández, M.G., Resmini, E. (2015). Hormone Replacement Therapy and Cardiovascular Disease in Women. In: Lanzer, P. (eds) PanVascular Medicine. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-37078-6_172
Download citation
DOI: https://doi.org/10.1007/978-3-642-37078-6_172
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-37077-9
Online ISBN: 978-3-642-37078-6
eBook Packages: MedicineReference Module Medicine