Abstract
The role of magnetic resonance (MR) imaging for diagnosing and staging of breast cancer is ever increasing. It has been shown that MR imaging can detect breast cancer that is occult on mammography, ultrasound, and clinical examination. With the increasing use of breast MR imaging, there is an increasing number of women who require an MR-guided intervention for lesions that are visible with breast MR imaging alone, i.e., that are occult on mammography and on second-look ultrasound. Until recently, MR-guided needle localization with subsequent surgical biopsy has been the standard technique to deal with this situation. During the last years, MR-guided breast biopsy is available and is gaining more and more importance in the management of only MR visible lesions. But MR-guided breast biopsy is a challenging endeavor for many reasons, including the requirement for equipment that will work in the MR imaging environment, need to remove the patient from the magnet to perform biopsy in closed systems, limited access to the medial and posterior part of the breast, decreasing lesion conspicuity with time after contrast injection (vanishing phenomenon), and difficulties confirming lesion retrieval. Semiautomatic core biopsy under MR guidance has been successfully performed, but for a variety of reasons did not gain broad clinical acceptance. MR-guided vacuum biopsy, however, is a technique that allows a more accurate and successful tissue sampling of lesions seen only on MR imaging. This chapter gives an overview about procedures and results of MR-guided breast needle localization and MR-guided breast biopsy using semiautomatic core needles and vacuum-assisted biopsy probes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Breast Magnetic Resonance Imaging
- Atypical Ductal Hyperplasia
- Needle Guide
- Biopsy Device
- Needle Localization
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The role of magnetic resonance (MR) imaging for diagnosing and staging of breast cancer is ever increasing. It has been shown that MR imaging can detect breast cancer that is occult on mammography, ultrasound, and clinical examination. With the increasing use of breast MR imaging, there is an increasing number of women who require an MR-guided intervention for lesions that are visible with breast MR imaging alone, i.e., that are occult on mammography and on second-look ultrasound. Until recently, MR-guided needle localization with subsequent surgical biopsy has been the standard technique to deal with this situation. During the last years, MR-guided breast biopsy is available and is gaining more and more importance in the management of only MR visible lesions. But MR-guided breast biopsy is a challenging endeavor for many reasons, including the requirement for equipment that will work in the MR imaging environment, need to remove the patient from the magnet to perform biopsy in closed systems, limited access to the medial and posterior part of the breast, decreasing lesion conspicuity with time after contrast injection (vanishing phenomenon), and difficulties confirming lesion retrieval. Semiautomatic core biopsy under MR guidance has been successfully performed, but for a variety of reasons did not gain broad clinical acceptance. MR-guided vacuum biopsy, however, is a technique that allows a more accurate and successful tissue sampling of lesions seen only on MR imaging. This chapter gives an overview about procedures and results of MR-guided breast needle localization and MR-guided breast biopsy using semiautomatic core needles and vacuum-assisted biopsy probes.
2 Indication
Before a breast MR-guided intervention of a suspicious lesion is performed, all patients should undergo an extensive workup in order to find out whether the questionable MR imaging detected lesion is visible, in retrospect, by conventional imaging studies. The workup should consist of a targeted ultrasound of the area of the MR-identified abnormality (“second-look ultrasound”) and a review of the respective mammograms. The diagnostic mammogram should be amended by additional mammographic views and spot compression over the area of the MR-detected abnormality. Only in case this workup does not reveal a clear correlate for the MR imaging finding, patients should proceeded to an MR-guided intervention.
3 Patient Preparation
Prior to MR-guided interventions, the procedure and all risks involved as well as the benefits should be explained to the patient. Written informed consent needs to be obtained from the patient.
Although the intervention is quite fast and is well tolerated, the procedure can cause patient anxiety. At our institution, patients receive intravenous sedation with 5–10 mg diazepam i.v. just before starting the intervention. MR-guided vacuum biopsy is not performed under the medication with anticoagulants. Any medication with aspirin or anticoagulants should be paused for at least 5 days. Blood values should be checked for thrombocytes, INR (international normalized ratio), and partial thromboplastin time (PTT).
The patient is positioned prone with both breasts in a dedicated surface breast in the magnet. Then the skin is cleansed with alcohol or povidone-iodine (Fig. 10.1a). The breast undergoing the intervention is fixated with a breast immobilization system. Breast immobilization is important in MR-guided interventions for several reasons. Often the lesion becomes less evident during the procedure due to the transient nature of contrast enhancement; it is therefore essential to identify the lesion at the outset of the procedure and then to ensure that the lesion remains fixed in position. Furthermore, breast immobilization is necessary to help minimize lesion motion during needle placement. Immobilization of the breast can be achieved by immobilizing the breast between two compression plates. Compression plates are usually oriented in the mediolateral plane. Compression plates have been manufactured with perforated holes, four flexible horizontal bands, or fixed grid lines (Fig. 10.1b, c). Only gentle breast fixation should be used in order to avoid nonenhancement of the lesion, due to a too strong compression of vessels.
Compression device for MR-guided intervention. (a) For interventional MR imaging examinations as for diagnostic studies, the patient lies prone with the breast having biopsy in the dedicated breast coil. The breast is cleansed with alcohol. (b) Breast MR coil with compression grid (Biopsy Device Model MR-BI-160, MRI devices) in place. The patient is positioned that way that the expected lesion is located under the grid system. (c) Breast MR coil with compression post and pillar system (Biopsy Device Model MR-BI-160, MRI devices). The immobilization system housed a perforated compression plate and a striated hole structure consisting of four 2 cm wide and 10 cm long openings. The pillar needle holder consisted of detachable pillar on a rail. This pillar has housing for needle holder collars of different sizes from 9 to 18 gauges. The pillar can be repositioned and fixed to certain position both horizontally and vertically. The system enables an oblique approach. Therefore, the needle guide can be angulated up to 15° which allows to biopsy or the mark lesions which are very close to the chest wall
4 Imaging Protocol
To identify the target lesion, a diagnostic breast MR imaging study needs to be performed. For example, the following imaging protocol can be used: axial 2D T1-weighted gradient echo, contrast-enhanced, and dynamic series (290/4.6 (repetition time msec/echo time msec), 90° flip angle, slice thickness 3 mm (no gap), matrix 512 × 512) before and four times after bolus injection of gadolinium dimeglumine. In addition, a T2-weighted turbo spin echo images (3,000/120 (repetition time msec/echo time msec), slice thickness 3 mm, matrix 512 × 512) with the same anatomic parameters as the gradient echo sequence should be obtained. As in most cases only on breast will be biopsied, the field of view should be adjusted to the single breast setting (e.g. 220 mm).
5 Calculation of the Target’s Coordinates
The target’s coordinates and an appropriate needle trajectory can be calculated by using dedicated software tools (e.g., DynaCAD, MRI devices/Invivo, Orlando USA). The software automatically calculates based on the coil, the immobilization system and the biopsy device, the coordinates of the lesion location, and the desired depth of probe insertion. With these coordinates, the location of the lesion and the corresponding needle trajectory can be directly established on the breast compression device.
If such software is not available, prior to the diagnostic imaging, a marker (e.g., a vitamin E capsule) is placed on the skin overlying the expected lesion localization. For sagittal images (Fig. 10.2a), after reviewing the images at the console, a cursor is placed over the lesion on the monitor; the horizontal (x) and vertical (y) coordinates of the lesion are measured in cm on the basis of the spatial relationship between the lesion, vitamin E marker, and grid lines. The depth (z) coordinate of the lesion is determined on the basis of the relationship between the lesion and the skin surface. The skin surface is at the slice where the indentations from the grid are evident as low signal intensity lines. The depth of the lesion from the skin surface in millimeters (z) is calculated by determining the number of sagittal slices between the skin and the lesion and multiplying by the slice thickness (e.g., 3 mm).
For axial images (Fig. 10.2b), the horizontal (x) coordinate is determined on the basis of the difference in cm between the vitamin E marker and the lesion. The vertical (y) coordinate is calculated by determining the number of axial slices between the slice of which the marker is visible and the slice of which the lesion is visible and multiplying by the slice thickness (e.g., 3 mm). The depth (z) is determined by measuring the distance between the skin surface and the lesion.
After calculating the lesion coordinates and establishing these on the compression device, the breast is anesthetized in the area of the calculated lesion position with 10 ml or more of local anesthetics.
6 Procedure MR-Guided Needle Localization and MR-Guided Biopsy
6.1 MR-Guided Needle Localization
Magnetic resonance imaging-guided interventions can be performed free hand or by using guidance methods, such as a compression grid system (Fig. 10.1b). The freehand method has the advantage of allowing the needle to be angled, but the potential disadvantage of a long examination time because of repeated imaging to confirm needle placement. Because of these disadvantages, the standard method is needle localization by using compression systems that allow more accurate initial needle placement.
6.1.1 Material
A variety of needles are now commercially available for MR-guided needle localization. Conventional ferromagnetic needles cannot be used for MR-guided localization procedures due to the high magnetic field. Nonferromagnetic materials such as stainless steel produce severe artifacts. Materials with increased nickel content such as iconel and other high nickel and low susceptibility alloys generate fewer artifacts. Titanium wires and needles also have fewer artifacts and are used widely at present. Usually needles with a size of 18 or 20 G are usually used. Table 10.1a gives an overview over available MR compatible wires.
6.1.2 Performing Needle Localization
A needle guide that is provided with the grid compression system is inserted into the grid at the calculated position overlaying the target lesion (Fig. 10.3a). The needle guides are manufactured to have 18- or 20-gauge holes to accommodate various needle sizes. The needle guide is used to enable insertion of the needle in a straight approach, without angulation. The MR compatible needle/hook wire is then placed in the calculated hole of the needle guide. The needle is inserted to the desired depth. After needle insertion, a T1-weighted spin echo sequence is obtained to document the location of the needle. The needle is evident as a low signal intensity structure with adjacent susceptibility artifact (Fig. 10.3e). If the needle is too deep or too superficial, adjustments are made. When the needle tip is in good position, the wire is deployed by advancing the wire to the mark, indicating that the tip had emerged from the needle. The needle is then removed, leaving the wire in place, and a final series of T1-weighted spin echo sequence images are obtained to document the final wire position (Fig. 10.3f).
MR-guided needle localization. (a) Picture of needle guide and needle in place. (b–f) 56-year-old patient with biopsy proven breast cancer on the right breast. Preoperative breast MR imaging showed a suspicious focal (<5 mm) retromamillary lesion in the left breast. (b) T1-weighted gradient echo (TR/TE, 290/4.6; flip angle, 90°) before contrast and (b) first contrast enhanced, (d) subtraction. (e) T1-weighted spin echo sequence after placing the needle to control the correct position of the needle. The needle is evident as a low signal intensity structure with adjacent susceptibility artifact (arrow). Needle tip is in good position. (f) T1-weighted spin echo sequence after deploying the hook wire from the needle. Needle tip is in a good final position (arrow)
After localization, a two-view mammogram can be obtained so that the surgeon can see the location of the wire with respect to the nipple, the chest wall, and the remainder of the breast tissue.
6.2 MR-Guided Core Biopsy
MR-guided semiautomatic core biopsy can be performed with MR compatible, single-use, semiautomatic core guns with 14–20 gauge. After determining the lesion coordinates and local anesthetics, a skin nick is made with a scalpel, and the coaxial needle is placed until the calculated depth. Then the position of the needle is verified with a T1-weighted spin echo sequence. If necessary, the needle position is adjusted. Then 5–10 core biopsies should be obtained with rotating the biopsy notch in a clockwise direction. After the biopsy, a second contrast-enhanced series (T1-weighted turbo SE before and after contrast injection) can be obtained to control whether the biopsy was sufficient or not. Alternatively a contrast-enhanced T1-weighted turbo SE with spectral-selective fat suppression can be performed. If the lesion has not been sufficiently biopsied, another 5–10 core biopsies should be obtained.
6.3 MR-Guided Vacuum Biopsy
6.3.1 Material
Different vacuum biopsy devices are commercially available with 11–7G probes (Table 10.1b). With all available systems, a quick and accurate MR-guided vacuum biopsy is possible, and differences exist only regarding handling of the biopsy device.
6.3.2 Performing Vacuum Biopsy
The appropriate hole of the needle guide is selected. A stylet and an introducer sheath are then placed through the needle guide and advanced to the calculated depth (Fig. 10.4a). Then the stylet is removed, and an obturator is placed inside the introducer sheath to assist in MR imaging confirmation of location (Fig. 10.4b). A fast T1-weighted gradient echo sequence is performed to document the location of the obturator, with the ideal location of the tip being at the site of the lesion. A distance of 5 mm between the tip of the obturator and the lesion is still acceptable because the lesion will still be sampled due to the strong vacuum of the system. If positioning is appropriate, the biopsy device is inserted (Fig. 10.4c). The direction of tissue acquisition is chosen based on location of the introducer with respect to the lesion. The radiologist performing the biopsy controls the direction of tissue acquisition, by turning the biopsy probe in the desired direction. Most of the biopsy systems allow a continuous sampling of tissue without removing the biopsy needle. Each specimen is then automatically transported into a container. Only one system (VACORA System) does not allow continuous tissue sampling. With this system after each needle pass, the needle needs to be removed to retain the specimen from the biopsy notch. Then the biopsy device needs to be reinserted into the introducer sheath again to obtain the next specimen. In general, 15–30 specimens should be obtained.
MR-guided vacuum biopsy (with Suros, ATEC system). (a) Equipment for MR-guided vacuum-assisted biopsy includes the needle guide; the white introducer sheath, which is scored with marks; the plastic obturator, which serves as a placeholder for MR imaging; the sharp stylet, which creates the tract. (b) Introducer sheath with the obturator positioned in the breast at the calculated lesion position. (c) Biopsy device inserted through the introducer sheath. The direction of tissue acquisition can be controlled by turning the arrow on the biopsy probe in the desired direction. The specimens are collected in a specimen collecting chamber at the end of the biopsy handpiece, which can be retrieved after tissue acquisition is complete. (d) Due to the strong vacuum, a high volume of tissue can be obtained with a high specimen quality
After tissue acquisition is complete, the biopsy device is removed. Then an axial T2-weighted turbo SE sequence is performed to show the biopsy cavity and to assess whether the biopsy site did include the target lesion. Due to the progressive enhancement in the surrounding fibroglandular tissue (“vanishing target”), it is impossible to directly image the target lesion in the late phase of an MR-guided intervention. Therefore, the location of the biopsy site must be carefully compared with the preinterventional images in order to find out whether the biopsy site should have included the target lesion. If any doubt persists, additional biopsy passes should be performed. Additional contrast-enhanced images can be obtained in case the lesion had a strong washout to help to decide whether the lesion has been removed or sampled or not (Figs. 10.5 and 10.6).
41-year-old patient with a history of a lobular carcinoma in situ of the left breast. Breast MR imaging showed a 6-mm mass-like lesion in the upper outer quadrant of the right breast (white arrow). Mammography and a second-look ultrasound did not reveal a correlate for the MR imaging finding. Vacuum biopsy with a 9-G system (ATEC, Suros) revealed an invasive ductal cancer, pT1b, pN0, G3. 5a-b: dynamic breast MR imaging of the right breast, axial orientation, T1-weighted 2D gradient echo TR/TE/FA 290/4.6/90°; (a) subtracted image, (b) first post-contrast image; (c): T2-weighted image (TR 3000/TE120) before vacuum biopsy, after placing an obturator, (d): T2-weighted image after vacuum biopsy and flushing the biopsy cavity with saline. The biopsy cavity can accurately be delineated on the T2-weighted TSE image (white arrows)
37-year-old woman. Prior history of an invasive breast cancer on the left. Breast MR imaging showed a 3-mm mass-like lesion in the upper outer quadrant of the right breast (white arrow). Mammography and a second-look ultrasound did not reveal a correlate for the MR imaging finding. Vacuum biopsy with a 9-G system (ATEC, Suros) revealed an invasive ductal cancer, pT1a, pN0, G3. (a) T1-weighted 2D gradient echo (TR/TE, 290/4.6; flip angle, 90°) before contrast and (b) first contrast enhanced, (c) subtraction, (d) T2-weighted (3,000/120) MR images obtained before vacuum biopsy, (e) T2-weighted image after vacuum biopsy and flushing the biopsy cavity (circle) with saline and (f) after placing a clip (arrow)
6.4 Clip Placing
A MR compatible clip should be placed immediately subsequent to the vacuum biopsy. This clip can serve as target for mammography-guided localization prior to definitive oncologic surgery. The clips are titanium clips. The clip is placed through the introducer sheath. Postclip MR imaging examination (T1-weighted gradient echo) is performed to assess clip deployment and to document clip position (Fig. 10.6f). Subsequently, a two-view mammogram can be obtained to determine the location of the clip with respect to the remainder of the breast parenchyma.
6.5 Postbiopsy Care
After biopsy, manual compression is held approximately 20 min to achieve hemostasis. The biopsy site is cleansed with alcohol and dried with sterile gauze. Sterile strips are placed over the biopsy site. A gauze bandage and a pressure dressing are placed over the sterile strips for 24 h. The patient should come back the next day for wound control and ultrasound at the biopsy site.
7 Results
7.1 Results: Needle Localization
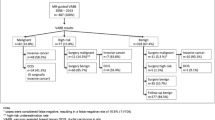
Magnetic resonance imaging-guided needle localization can be readily performed with commercially available equipment. In published series of MR-guided needle localization, the technical success rate was 98–100 %; histological analysis revealed cancer in 31–73 % [of which up to half were ductal carcinoma in situ (DCIS)] and high-risk lesions such as atypical ductal hyperplasia (ADH) or lobular carcinoma in situ (LCIS) in up to 29 %. Table 10.2 gives an overview over the results of MR-guided needle localizations.
7.2 Results: Core Biopsy
The use of magnetic resonance imaging-guided semiautomatic core biopsy is reported in different studies using 14–20-gauge needles (Table 10.3). In these studies, technical success rate ranged from 33 to 100 %. No major complications occurred in these studies. Although these studies indicate that MR-guided 14-gauge automated core biopsy can have high diagnostic yield, this method has potential limitations. A high proportion of lesions detected by breast MR imaging contain ductal carcinoma in situ (DCIS) or atypical ductal hyperplasia (ADH); a 14-gauge automated needle often underestimates the pathology of these complex lesions (Liberman 2002). In addition, MR-guided biopsy has the problem of the vanishing target—during the biopsy procedure, the lesion often becomes less conspicuous, due to washout of contrast material from the lesion and progressive enhancement of the surrounding breast parenchyma. For such lesions, it would be helpful to be able to acquire a larger volume of tissue than is possible with the 14-gauge automated needle. Finally, 14-gauge automated needles do not readily provide a mechanism for placement of an MR compatible localizing clip, which may be helpful for the small lesions that undergo MR-guided biopsy.
7.3 Results: MR-Guided Vacuum Biopsy
Vacuum-assisted biopsy has a higher technical success rate than semiautomatic biopsy, with fewer inadequate specimens. Compared with automated core biopsy, MR-guided vacuum biopsy enables retrieval of a larger volume of tissue, with each specimen weighing 200 mg (Fig. 10.4d) as compared with approximately 17 mg per specimen for 14-gauge automated needles (Schnall 2000). The larger volume of tissue can help compensate for decreasing lesion conspicuity during the MR-guided biopsy procedure and provides better characterization of complex lesions containing ADH and DCIS (Liberman et al. 2003). Table 10.4 gives an overview over the results of the use of MR-guided vacuum biopsy. In all studies, a very high success rate ranging from 96 to 100 % could be achieved. Another advantage of MR-guided vacuum biopsy is that significantly smaller lesions can be biopsied. In all published studies lesions also <5 mm could be sufficient biopsied. All studies confirm that MR-guided vacuum-assisted biopsy is a fast and safe method and an accurate alternative to surgical excision for MR-detected lesions that are suspicious or highly suggestive of malignancy.
8 Complications
In all published studies, major complications occurred neither for MR-guided needle localizations, MR-guided semiautomatic core biopsies, nor for MR-guided vacuum biopsies. Minor complications as larger hematoma or vasovagal reactions occurred in these studies in less than <1 %. Major complications such as hemodynamic relevant bleeding or hematoma, which needed surgical revision, occurred in under 0.01 % of all published cases. All published studies confirm that MR-guided semiautomatic and especially vacuum-assisted biopsy is a safe technique.
Appraisal
Magnetic resonance imaging-guided percutaneous biopsy can be accomplished with a variety of automated core needles and vacuum-assisted biopsy probes. MR-guided vacuum biopsy allows histological verification of “MR only” visible lesions with adequate reliability and reaches a diagnostic accuracy equivalent or even higher to that of MR-guided needle localization. Vacuum-assisted biopsy is advantageous over MR-guided automatic core biopsy for MR-guided percutaneous breast biopsy, because vacuum-assisted biopsy can be performed quickly, removes a large volume of tissue, provides more accurate characterization of lesions containing ADH and DCIS, and enables placement of a localizing clip.
Key Points
-
MR-guided needle localization using a needle guided followed by open surgery is a quick and accurate technique for histological verification of “MR-only” visible lesions. Freehand needle localizations should not be performed anymore.
-
As not all MR suspicious lesions are malignant, MR-guided biopsy should be performed to avoid unnecessary surgery of “MR only” visible lesions.
-
MR-guided vacuum biopsy has advantages over MR-guided core biopsy, e.g., higher technical success rate; higher tissue volume and smaller lesions can be biopsied. Therefore, if available, MR-guided vacuum biopsy should be used instead of MR-guided core biopsy.
-
MR-guided vacuum-assisted biopsy is a fast, safe, and accurate alternative to surgical excision for the diagnosis of lesions detected on MR imaging.
References
Chen X, Lehman CD, Dee KE (2004) MRI-guided breast biopsy: clinical experience with 14 gauge stainless steel core biopsy needle. AJR Am J Roentgenol 182:1075–1080
Doler W, Fischer U, Metzger I et al (1996) Stereotaxic add-on device for MR-guided biopsy of breast lesions. Radiology 200:863–864
Fischer U, Kopka L, Grabbe E (1998) Magnetic resonance guided localization and biopsy of suspicious breast lesions. Top Magn Reson Imaging 9:44–59
Heywang-Kobrunner SH, Huynh AT, Viehweg P et al (1994) Prototype breast coil for MR-guided needle localization. J Comput Assist Tomogr 18:876–881
Heywang-Kobrunner SH, Heinig A, Schaumloeffel-Schulze U et al (1999) MR-guided percutaneous excisional and incisional biopsy of breast lesions. Eur Radiol 9:1656–1665
Kuhl CK, Elevelt A, Leutner CC et al (1997) Interventional breast MR imaging: clinical use of a stereotactic localization and biopsy device. Radiology 204:667–675
Kuhl CK, Morakkabati N, Leutner CC et al (2001) MR imaging-guided large-core (14-gauge) needle biopsy of small lesions visible at breast MR imaging alone. Radiology 220:31–39
Lehman CD, Deperi E, Peacock S, McDonough M, DeMartini W, Shook J (2005) Clinical experience with MRI-guided vacuum-assisted breast biopsy. AJR Am J Roentgenol 184:1782–1787
Liberman L (2002) Percutaneous image-guided core breast biopsy. Radiol Clin North Am 40:483–500
Liberman L, Morris EA, Dershaw DD et al (2003) Fast MRI-guided vacuum-assisted breast biopsy: initial experience. AJR Am J Roentgenol 181:1283–1293
Liberman L, Bracero N, Morris E, Thornton C, Dershaw D (2005) MRI-guided 9-gauge vacuum-assisted breast biopsy: initial clinical experiences. AJR 185:183–193
Morris EA, Liberman L, Dershaw DD et al (2002) Preoperative MR imaging-guided needle localization of breast lesions. AJR Am J Roentgenol 178:1211–1220
Orel SG, Schnall MD, Newman RW et al (1994) MR imaging-guided localization and biopsy of breast lesions: initial experience. Radiology 193:97–102
Orel SG, Schnall MD, Czerniecki B et al (1999) MRI-guided needle localization: indications and clinical efficacy. Radiology 213:454 [Abstract]
Orel SG, Rosen M, Mies C, Schnall MD (2006) MR imaging-guided 9-gauge vacuum-assisted core-needle breast biopsy: initial experience. Radiology 238:54–61
Perlet C, Heinig A, Prat X et al (2002) Multicenter study for the evaluation of a dedicated biopsy device for MR-guided vacuum biopsy of the breast. Eur Radiol 12:1463–1470
Schnall MD (2000) MR-guided breast biopsy. In: Lufkin RB (ed) Interventional MRI. Mosby, St. Louis, pp 315–319
Schneider JP, Schulz T, Horn LC et al (2002) MR-guided percutaneous core biopsy of small breast lesions: first experience with a vertically open 0.5 T scanner. J Magn Reson Imaging 15:374–385
Schrading S, Simon B, Braun M, Wardelmann E, Schild HH, Kuhl CK (2010) MRI-guided breast biopsy: influence of choice of vacuum biopsy system on the mode of biopsy of MRI-only suspicious breast lesions. AJR Am J Roentgenol 194:1650–1657
Taourel PH, Sittek H, Boetes C et al (2002) MR-guided localization and surgery: results of a European multicenter study. Radiology 225:556
Viehweg P, Heinig A, Amaya B, Alberich T, Laniado M, Heywang-Kobrunner SH (2002) MR-guided interventional breast procedures considering vacuum biopsy in particular. Eur J Radiol 42:32–39
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Schrading, S. (2013). MR-Guided Breast Intervention. In: Mahnken, A., Wilhelm, K., Ricke, J. (eds) CT- and MR-Guided Interventions in Radiology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-33581-5_10
Download citation
DOI: https://doi.org/10.1007/978-3-642-33581-5_10
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-33580-8
Online ISBN: 978-3-642-33581-5
eBook Packages: MedicineMedicine (R0)