Abstract
Microdevices enable clinical diagnostics to be miniaturized for use at the point-of-care (POC). Microdevices can be composed of microfilters, microchannels, microarrays, micropumps, microvalves, and microelectronics, and these mechanical and electrical components can be integrated onto chips to analyze and control biological objects at the microscale. The miniaturization of diagnostic tests offers many advantages over centralized laboratory testing, such as small reagent volumes, rapid analysis, small size, low power consumption, parallel analysis, and functional integration of multiple devices. Here, we review work on the development of microdevices to diagnose disease at POC settings.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Microfluidic Device
- Microfluidic Chip
- Noncommunicable Disease
- Recombinase Polymerase Amplification
- Nucleic Acid Testing
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
An exciting application of microdevices is miniaturized clinical diagnostic methods for point-of-care testing. Microdevices are defined as systems which employ analytical components and techniques at microscopic scales (ranging from 1 to \(500\,\mu \mathrm{m}\)), including microfilters, microchannels, microarrays, micropumps, microvalves, and bioelectronic chips [1, 2]. Advantages over tests in centralized laboratories include small reagent volumes, rapid analysis, small size, low power consumption, parallel analysis, and functional integration of multiple devices [3–5]. Because of these advantages, microdevices are capable of being low cost and portable – two qualities critical for implementation of point-of-care (POC) diagnostics.
POC tests are important in settings where timing is critical (e.g., emergency triage), where laboratory facilities are nonexistent (e.g., military or extraterrestrial functions), and where resources are low (e.g., in developing countries). They help deliver appropriate and prompt treatments and improve clinical outcomes [5–7].
The development of microdevice-based diagnostics originated from driving forces in molecular analysis, biodefence, molecular biology, and microelectronics, the last of which provided tools for miniaturization and microfabrication [1, 8]. However, miniaturized silicon-based devices were not suited to biological applications with physiological fluids because of difficulty of optical detection, high material cost, low biocompatibility, and lack of available rapid prototyping. The extension of microfabrication techniques to first glass then polymers such as elastomers and hard plastics enabled the construction of a set of microfluidic mechanical devices grouped under the broad category of microelectromechanical systems (MEMS) or lab-on-a-chip (LOC) systems [9]. These technologies, in turn, have led to developments in sensors for medical, environmental, and life science applications [1].
2 Comparisons Between Point-of-Care Tests in Developed Versus Developing Worlds
Integration, portability, low power consumption, automation, and ruggedness are several important qualities common to point-of-care tests in both developed and developing countries. (Here we define the developed world as the group of high-income countries and the developing world as the groups of low- and middle-income countries, based on classifications by the World Bank). These general design constraints suggest some LOC components and procedures to be more appropriate than others in point-of-care settings (Fig. 1.1). In general, the differences in appropriate LOC procedures are more pronounced between tests performed at centralized settings versus point-of-care settings than between point-of-care tests performed at high-income versus low-income settings [10]. For instance, the presence of reliable ground electricity at centralized testing facilities allows for active mixing on-chip and bulky signal detection systems which draw significant power. At point-of-care, however, the lack of ground electricity requires passive or low-power approaches for mixing on-chip and portable signal detection systems which can be powered by battery (or read by eye) (Fig. 1.1). By virtue of the common design criteria in point-of-care tests, engineers interested in developing microdevices for point-of-care testing in resource-limited settings can leverage the large body of existing research on LOC designs for point-of-care testing for physicians and home use [11, 12], devices for military applications [13] and first responders, and extraterrestrial sensors [14–16].
Appropriateness of technologies for important LOC procedures according to setting (centralized versus point-of-care) and resource-level (high income versus low income) ([5] – reproduced by permission of the Royal Society of Chemistry)
There are, however, at least two important distinctions between LOC point-of-care tests intended for developed countries versus developing countries. The first is cost. Due to vastly smaller budgets via public financing, the budget available to spend on medical diagnostics devices in developing countries is limited compared to that of developed countries. Thus, the cost of the microfluidic device (which includes both the material and the manufacturing process) must be kept extremely low in POC testing in developing countries; the fixed instrument must be portable and cheap, and the disposable must be extremely cheap. All components of the device (including the instrument and disposable) must be robust and rugged under a variety of environmental conditions.
Clinical need is another feature distinguishing POC tests in the developed versus the developing worlds (Fig. 1.2). The burden of disease in the developed world skews heavily toward noncommunicable diseases: cardiovascular disease (stroke, heart disease), cancer, respiratory disease (COPD and asthma), and neuropsychiatric conditions are some of the more significant causes [17]. By contrast, in the developing world, while noncommunicable diseases are prevalent, a significant burden of disease is attributed to infectious diseases, many of which can be treated and prevented. Major infectious diseases according to the burden of disease include HIV/AIDS, tuberculosis, malaria, diarrheal diseases, and lower respiratory infections. Maternal and perinatal conditions and nutritional deficiencies are also significant causes of disease and disability in the developing world.
Distribution of disease burden (DALYs) in high-income, middle-income and low-income countries [17]
Point-of-care tests based on LOC technologies have the potential for rapid and portable diagnosis of a range of conditions. The rest of this chapter will describe the range of analytes detected by low-cost microdevices at point-of-care and their specific applications.
3 Classes of Analytes
Microdevices have been used in academic, government, nonprofit, and commercial settings to detect a range of analytes using many types of biological fluids. These studies have demonstrated assays with better performance than benchtop tests with regards to speed, portability, sensitivity, and multiplexing. The classes of analytes detected include proteins, nucleic acids, cells, and small molecules [5]. Each analyte class will be described in the section on applications.
3.1 Proteins
Proteins in clinical specimens in whole blood, serum/plasma, saliva, urine, and other sample matrices have been used for clinical diagnostics and monitoring disease states [18]. Microdevice-based technologies at point-of-care for detecting proteins have included both immunoassays and enzymatic assays. Currently available clinical tests for microdevices at point-of-care include viral infections (anti-HIV antibodies, antibodies against influenza A/B virus, rotavirus antigens), bacterial infections (antibodies against Streptococcus A and B, Chlamydia trachomatis, Treponema pallidum), parasitic infections (histidine-rich protein 2 for P. falciparum, trichomonas antigens), and noncommunicable diseases (PSA for prostate cancer, C-reactive protein for inflammation, HbA1c for plasma glucose concentration) [5, 19, 20]. For example, a saliva-based nano-biochip immunoassay has been constructed to detect a panel of C-reactive protein, myoglobin, and myeloperoxidase in acute myocardial infarction patients [21].
3.2 Cells
Cell-based POC testing is often needed for disease diagnosis and hematological analysis. Full blood cell counts provide information in diagnosing and monitoring conditions such as anemia and HIV/AIDS. For instance, CD4 + lymphocyte counting is used to monitor the progression of HIV/AIDS, and microdevices have been developed to substitute the conventional method (bulky and expensive instruments such as flow cytometry) for POC testing. Traditional methods also often require trained personnel and ground electricity. On-chip cell sorting techniques from heterogeneous cell suspensions (such as whole blood) can be classified into two main categories: size- and density-based techniques and affinity-based techniques (chemical, electrical, or magnetic) [22]. Several novel size-based separation methods force a stream of cells through a series of channels by hydrodynamic flow switching, electrokinetic flow switching, dielectrophoresis, electrowetting-assisted flow switching, or valves [5] which provide predictable and reproducible cell movement [22]. These methods do not employ the use of any proteins or biologies to achieve cell separation, hence, these size-based devices would have longer shelf lives. Affinity-based methods include the specific capture of cells using antibodies such as with magnetic beads coated with antibodies, which is a common laboratory protocol and can be miniaturized easily. Another affinity-based method makes use of dielectrophoresis. This method makes use of the differential response of cells to electric fields due to their density, physiological, and metabolic states. Other approaches involve lysing the undesired cells, leaving behind the desired cells in the reaction chamber [23]. This technique can reduce the processing time and therefore avoid cell damage from prolonged contact with lysis agents and centrifugation [22]. These approaches are easily implemented on microfluidic devices and usually followed by downstream analysis such as fluorescence microscopy or proteomics/genomics analysis following the lysing of the captured cells [24].
3.3 Nucleic Acids
Clinical diagnoses can be made based on the analysis of DNA or RNA sequences. Nucleic acid detection and analysis can identify the type of infection or pathogen and diseases. It can be used in prenatal diagnosis of inherited disorders, clinical disease diagnosis (genetic disease, infection, disease staging, drug resistance mutation, and pathogen presence/abundance), and forensic investigations. Nucleic acid testing (NAT) offers detection that is highly sensitive (due to amplification) and specific (due to specific base pairing of complementary nucleotides). NAT also reduces the window period between infection and detectability of disease. Currently available clinical tests mostly target infectious diseases, for instance, HIV (diagnosis and viral load monitoring), H1N1 influenza, tuberculosis, and group B streptococcal disease. These available systems are mainly used in hospitals and centralized laboratories with complex operation steps and high-cost instruments [25]. In order to achieve NAT for POC diagnosis, fully integrated system is preferable; for instance, to avoid contamination issues, reduce worker steps, and deliver rapid results.
3.4 Small Molecules
Analyzing electrolytes from body fluids is used to monitor health parameters in disease prevention. The ranges of electrolytes (\({\mathrm{Na}}^{+}\), \({\mathrm{K}}^{+}\), \({\mathrm{Cl}}^{-}\), \({\mathrm{Ca}}^{2+}\)), general chemistries (pH, urea, glucose), blood gases (pCO2, pO2), and hematology (hematocrit) are analyzed. Currently, methods are based on electrochemical detection such as potentiometry, amperometry, and conductance [5] (see applications for more details). Another microfluidic approach to ion analysis is optical sensing [26]. For example, a microfluidic device can be used for pH analysis based on the color change of pH-sensitive dyes immobilized in patterned hydrogels [27].
4 Applications
4.1 Immunoassays
One of the most common protein assays that are adapted for point-of-care microfluidic-based diagnostics is the immunoassay. This assay makes use of the binding interactions between antigens and antibodies to detect protein markers from either pathogen or host immune responses. Analytes for immunoassays span the entire range of pathogen types, from viruses (e.g., anti-HIV antibodies and p24 antigen for HIV) to bacteria (e.g., anti-treponemal antibodies for syphilis and early secretory antigenic target 6 for tuberculosis) and parasites (e.g., histidine-rich protein 2 for malaria). Immunoassays are also commonly used for detection of noncommunicable diseases, such as prostate cancer via measurement of levels of prostate specific antigen, as in a system by OPKO Diagnostics (formerly Claros Diagnostics) or heart disease via measurement of levels of B-type natriuretic peptide, as in the Triage BNP Test by Biosite [28].
Heterogeneous immunoassays are a popular immunoassay format where capture of analytes occurs at protein-modified surfaces. The reference standard of many heterogeneous immunoassays is the enzyme-linked immunosorbent assay (ELISA), which uses multiwell plates and can be automated for high-throughput processing at well-equipped central laboratories. Most ELISAs use colorimetric- or chemiluminescence-based detection and have detection limits typically in the pM range due to enzyme-mediated signal amplification and serial washing. Unfortunately, the traditional ELISA format, which requires expensive and bulky instrumentation (for liquid handling and signal detection) and trained workers, is ill-suited for point-of-care testing.
Microfluidics is an attractive technology for point-of-care immunoassays. Heterogeneous immunoassays, because they involve capture of analytes at surfaces, are well-suited to exploit the large surface-to-volume ratios encountered in microfluidics. Faster analysis times can be achieved because of the replenishment of analytes and detection reagents in the boundary layer above the surface in standard wellplate formats [29]. Below, we highlight recent advances in microfluidic immunoassays that are low cost, portable, and can be used at point-of-care settings.
4.1.1 Signal Detection
Our group has demonstrated signal amplification using reduction of silver ions on gold nanoparticles [30] in cassettes made of injection-molded plastic (from Claros Diagnostics) for the simultaneous detection of HIV and syphilis antibodies (Fig. 1.3). Gold-catalyzed silver reduction is an attractive method of signal amplification and detection because the signals can be developed under continuous flow and can be read using low-cost optics. In a preclinical evaluation at several clinical sites in Rwanda, the technology showed sensitivity and specificity rivaling those of reference benchtop assays on hundreds of patient samples, with a time-to-result of no more than 20 min [31]. We also demonstrated excellent performance of HIV diagnosis using only \(1\,\mu \mathrm{L}\) of unprocessed whole blood. The potential social impact of this test is high when used in remote settings (e.g., clinics providing antenatal care), since treatments for HIV and syphilis are affordable and effective for minimizing disease transmission from mother to child.
Microfluidic platform for miniaturized immunoassays at ELISA-level performance [31]. (a) Picture of injection-molded cassette. (b) Picture of reader
Surface plasmon resonance is another suitable detection method, given appropriate signal amplification schemes. Sensata Technologies has previously developed a low-cost, disposable device which can detect heterogeneous antigen/antibody binding with changes in refractive index measured at the gold surface.
4.1.2 Fluid Control
Valves are an essential component of fluid control on microdevices. Pneumatic deflection of elastomers, such as PDMS, in multilayer systems has been demonstrated to be robust, leak-free, and capable of facilitating highly multiplexed systems [32] and have been utilized in development of bead-based microfluidic ELISA systems [33]. However, these micromechanical valves require high pressure often supplied by gas tanks. Active microvalves which are based on elastomeric deflections and are better suited at point-of-care settings include hydraulic (liquid) deflection based on magnetic actuation with solenoids [34] and torque-actuated deflection using small machine screws [35].
Passive approaches, which leverage differences in fluid behavior from varying microchannel geometries in capillary systems, are attractive because they do not require external power and moving off-chip parts. Such control mechanisms include delay valves, which merge smaller channels into larger channels to allow for smooth collection of incoming fluid streams at different flowrates; stop valves, which reduce the width of a microfluidic path using a restriction and enlarge it abruptly to reduce capillary pressure of a liquid front to zero; and trigger valves, which are the assembly of multiple stop valves preventing further fluid flow into a common outlet until the arrival of all inlet streams [36]. Some of these microfluidic control elements have been integrated on a chip for detection of C-reactive protein [37]. In addition, check valves have been implemented on a microfluidic device for multistep ELISA, detecting botulinum neurotoxin [38].
We have developed valveless delivery of reagents in microfluidic systems which have been demonstrated for detecting anti-HIV antibodies [39] and anti-treponemal antibodies [30]. The plug-based reagent delivery is a robust and low-cost approach for delivering multiple reagents without the need for on-chip valves.
4.1.3 Fluid Actuation and Delivery
Movement of fluids by capillary forces is reliable and does not require external power or moving parts. Miniaturized immunoassays based on capillary forces have been used for detecting cardiac markers [40] and luteinizing hormone [41]. Paper-based microfluidic systems also leverage capillary flow and have been used to detect anti-HIV antibodies [42]. Despite the need for external power, electrophoretic immunoassays in capillaries can be utilized if the power requirement is low (allowing for battery operation) and external instrumentation integrated in a single, easy-to-use device; such has been demonstrated in a promising proof-of-concept device for integrated, rapid, point-of-care testing of biotoxins ricin, Shiga toxin I, and Staphylococcal enterotoxin B [28], as well as in a rapid bioassay for endogenous matrix metalloproteinase-8 in saliva [43]. Pneumatic-based actuation of fluids can be suited for point-of-care settings, for example, in the manual operation of on-card bellows in the commercially available ABO blood typing chip by Micronics. A hand pump can also be used for pneumatic fluid actuation in microfluidic immunoassays [30, 39]. Injection-molded centrifugal-based platforms (CDs) rely on spin frequency to drive fluid movement, and movements are gated by capillary or hydrophobic valves; these can be suited for point-of-care testing in resource-limited settings, where in one example a centrifugal bead-based immunoassay was developed for the detection of antigen and antibody to hepatitis B virus [44].
4.2 Cell-Based Assays
POC testing for cell-based diagnostics has been increasingly important in hematology laboratory practices. It involves the numeration of specific cell types, typically white blood cells, from whole blood for the diagnosis, monitoring, and staging of diseases such as HIV/AIDS. A common use of microfluidics for POC cellular analysis is to replace traditional, resource-intensive technologies such as those used for flow cytometry and cellular biosensors. Such microfluidic methods may involve cell (or microparticle) separation based on size [45] and are based on methods such as filtration [46], laminar flow [47], dielectrophoretic force [48], optical gradient force [49], magnetic force [50], and acoustic force [51]. Other methods are based on antibody-specific capture of cells [52].
POC testing has been increasingly important in hematology practices, especially in obtaining white cell counts. The HemoCue WBC system (HemoCue AB, Sweden) measures total white blood cells in just \(10\,\mu \mathrm{L}\) of sample [53] and consists of a photomicroscope, a microcuvette holder, and an LCD display (Fig. 1.4a). It is able to operate on batteries and has low power consumption, making it suitable for POCT. The Chempaq analyzer is a self-contained system that uses differential impedance to detect different types of cells to return full blood counts within 3 min [54].
HemoCue WBC System and Daktari CD4 cell counter. (a) Picture of the HemoCue WBC System for total white blood cell count (Taken from www.hemocue.com with permission from HemoCue Corporation). (b) Picture of the portable Daktari CD4 cell counting system that is currently undergoing performance evaluations (Image courtesy of Daktari Diagnostics, Inc)
Due to the pressing need for a point-of-care CD4 T-lymphocyte enumeration method for the management of HIV/AIDS epidemic, especially in underserved regions, much work has been done to develop a microfluidic approach. A lysate impedance measurement method has been developed where the specific cells of interest are captured and lysed, and the resulting change in impedance is measured using electrodes integrated on-chip [55]. This is the underlying technology behind the Daktari CD4 system, a POC microdevice developed by Daktari Diagnostics that is portable, handheld, and does not require complex sample processing [24] (Fig. 1.4b). Another method, being commercialized by LabNow, uses semiconductor quantum dots to label captured CD4 cells, and an automated software is then used to analyze the fluorescent images [56]. An interesting use of microfluidics to create POC microdevices for cell-based assays is the integration of commercially available fiber optics with the microdevices so as to miniaturize the whole system by reducing any required optical and mechanical hardware [57]. Finally, the Pima CD4 test is being tested in the developing world [58].
We have utilized ultrasensitive chemiluminescence for detection of \(\mathrm{CD}4+\) cells on a microfluidic platform [59]. Compared to other optical-based LOC approaches for CD4 counting, this method used an instrument that requires no external light source and no image processing to produce a digitally displayed result only seconds after running the test.
4.3 Nucleic Acid Amplification Testing
In order to perform nucleic acid testing on a microfluidic chip, the main functionalities that have to be integrated on-chip include sample preparation, nucleic acid amplification, and the detection of the amplified product. While these steps can be easily integrated together and performed in a general laboratory, miniaturization of such disparate processes onto a single microfluidic chip is still a topic of intense research [60–62]. A fully integrated system could avoid contamination, reduce worker steps, and deliver rapid results. However, most of the devices that have been reported are single-function and require separate modules for detection and analysis due to the challenges involved in combining and miniaturizing these functionalities into a cost-effective, simple, and robust platform which these processes require much effort and time [25, 60].
4.3.1 Sample Preparation
After biological samples are collected, cell isolation and lysis followed by nucleic acid extraction, purification, and preconcentration may be performed [63]. This “sample processing” or “sample preparation” step has been less developed than other assay steps because of its intrinsic complexity. Moreover, contamination and inhibitors for subsequent amplification steps, and nucleic acid degradation are also critical and influence diagnostic testing as these factors impede quantitative assessment of the analyte in question, leading to misinterpretation of results [62, 64]. Therefore, sample preparation tends to be performed off-chip (using laboratory equipment such as centrifuge), while amplification and detection can be accomplished in microfluidic systems [65]. Nonetheless, efforts have been made to integrate cell capture, cell lysis, and nucleic acid purification into a single microfluidic device [66]. Integration of sample pretreatment with analysis could lead to improvements in sensitivity (as less sample is lost in between steps) and convenience [5]. One of the first microfluidics-based DNA purification procedures has been demonstrated using silicon microdevices, taking advantage of high-aspect ratio features to increase the capture surface area and hence the loading capacity [67]. Other work has focused on single-cell mRNA extraction and analysis via cDNA synthesis on a microfluidic chip [66]. The Cepheid’s GeneXpert has employed a macrofluidic approach integrated with a miniaturized sonicator [68]; this system has shown success in detecting drug-resistant tuberculosis in the developing world [69]. In another approach, Claremont BioSolutions has developed a miniaturized bead blender for sample preparation.
4.3.2 Signal Amplification
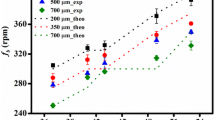
Since the amount of nucleic acid acquired from either the preparation step or from the raw sample is usually low for immediate identification and quantification [60], a method of amplification is needed to obtain a sufficiently nucleic acid detection signal. The most common technique is the polymerase chain reaction (PCR), for which miniaturization promotes the ability to reduce the reagent consumption, reduce the cycle time, and automate the process [5]. PCR requires thermal cycling for the reaction. Miniaturization of PCR provides many advantages, such as decreased cost of fabrication and operation, decreased reaction time for DNA amplification, reduced cross talk of the PCR reaction, and ability to perform large numbers of parallel amplification analyses on a single PCR microfluidic chip. Also, microfluidics allows for increased portability and integration of the PCR device. One of the first silicon-based stationary PCR chip was described several years after the introduction of PCR itself [70]. Since then, many research groups began to develop microdevice-based PCR devices. Most of these devices are based on silicon and glass, but more recently, polymer materials such as PDMS [71], PMMA, polycarbonate, SU-8, polyimide, poly(cyclic olefin), and epoxy are being used. HandyLab (HandyLab, Inc., is now part of Becton Dickinson) has also developed a disposable microfluidic chip that implements heat and pressure gradients to move microliter-sized plugs via valves and gates through different temperature zones within the chip [49, 72]. Flow-through designs also decrease the possibility of cross-contamination between samples as well as allow for the incorporation of many other functions, which is appealing as it leads toward the development of a micro total analysis system. As PCR is a temperature-controlled, enzyme catalyzed biochemical reaction system, the method in which the different temperature zones are generated and maintained is crucial to the design of PCR microfluidics. Various heating methods have been employed, and they can be broadly categorized into contact and noncontact heating methods. Contact heating has been implemented in PCR microfluidics using integrated thin-film platinum resistors as both the heating and sensing elements on these chips [73] and noncontact methods include hot-air cycling [74]. Both methods have low power consumption and are amenable for use at the point-of-care.
By contrast, isothermal techniques have been developed to perform nucleic acid amplification without thermal cycling. This feature removes the need of using different temperatures by making use of enzymes to perform reaction at a single temperature which translates into less complex and cheaper instrumentation that is amenable for point-of-care use [25, 69]. Current commercially available platforms [25], for example, helicase-dependent amplification (HDA; BioHelix), transcription-mediated amplification (TMA; Gen-Probe), nucleic acid sequence-based amplification (NASBA; BioMerieux), strand displacement amplification (SDA; Becton Dickinson), loop-mediated amplification (LAMP; Eiken), and recombinase polymerase amplification (RPA; TwistDx) are implemented in laboratory-based NAT and microdevices for point-of-care.
4.3.3 Product Detection
Amplified product can be examined at the end of reaction (end-point detection) or during the reaction (real-time detection). There are many techniques to detect nucleic acids, which one of the primary methods is quantifying nucleic acids by ultraviolet light (260 nm) absorption. Nonetheless, fluorescence-based techniques remain the most commonly employed due to its high level of sensitivity and low background noise [64]. Fluorescent dyes can either bind to nonspecific locations (general interactions) or specific locations of molecule, depending on the application. Cepheid Inc., for example, has developed a real-time fluorescent PCR detection (fluorescently labeled probes), requiring instruments that may be used in some but not all point-of-care settings. Cepheid’s GeneXpert test platform (Fig. 1.5a) has been tested for clinical trials in four developing countries and showed promising results for detecting tuberculosis [69]. However, this system requires uninterrupted and stable electrical power supply and annual validation of the system, and generates considerable more waste than microscopy technique [75] which may lead to problems of waste management in resource-limited settings.
(a) Cepheid’s GeneXpert test platform (right) integrates sample processing and PCR in a disposable plastic cartridge (left) containing reagents for cell lysis, nucleic acid extraction, amplification and amplicon detection. This system has been used to detect drug-resistant tuberculosis cases (Taken from www.cepheid.com with permission from Cepheid, Inc.) (b) Nanosphere Verigene system. Picture of a Nanosphere cartridge with loaded reagent wells (left). Picture of Verigene readers with touch-screen control panels (right) (Taken from www.nanosphere.us with permission from Nanosphere, Inc.)
At the point-of-care, electrochemical methods may also be suitable due to their compatibility with low-cost and portable analyzers [60]. For example, Nanosphere is building a scanner-based detector to detect DNA via nanoparticle probes [60]. Gold nanoparticles functionalized with oligonucleotides are used as probes for DNA sequences complementary to the sequences of those oligonucleotides (Fig. 1.5b). Visualization of the gold nanoparticle, and hence DNA content, is performed using a signal amplification method in which silver is reduced at the surface of the gold, and a scanner is used to measure amount of light scattered.
Lateral flow devices for end-point detection have been used for simple and low-cost method. A DNA strip using specific probes functionalized on membrane to capture target sequences from amplification reaction can be used for identification of target strains. GenoType (Hain Lifescience GmbH) and INNO-LiPA (Innogenetics NV) have developed assays to detect infectious diseases. BioHelix has developed a strip cassette for the isothermal amplification assay (Fig. 1.6).
BioHelix’ IsoAmp Molecular Analyzer is an instrument-free molecular diagnostic platform for IsoAmp assays (Taken from www.biohelix.com with permission from BioHelix Corp)
Other commercial effort toward a point-of-care nucleic acid device includes Spartan RX CYP2C19, by Spartan Bioscience, which is the first point-of-care genetic testing system to receive the CE marking from the European regulatory health authorities [53]. T2 Biosystems is based on magnetic resonance signal detection from nanoparticles coupled with target analytes which does not require sample purification; therefore, rapid turnaround time can be achieved.
4.4 Clinical Chemistry Assays
Clinical chemistry encompasses the measurement of a wide range of blood parameters, including gases, electrolytes, hemoglobin, pH, enzymes, metabolites, lipids, hormones, vitamins and trace factors, inflammatory markers and cytokines, coagulation proteins, therapeutic drugs, and drugs of abuse [12, 76]. Frequent sampling and fast diagnostic monitoring (in situations such as intensive care units and operating rooms) drive the need for clinical chemistry tests at the point-of-care [12]. In addition, POC testing for clinical chemistry markers can be more accurate by avoiding analyte changes during sample transport to laboratories. These analyte changes can be caused by the delayed release of analytes (e.g., release of \({\mathrm{K}}^{+}\) from red blood cells during refrigerated storage), by continued metabolism (e.g., decrease in glucose and pH and increase in lactate from active red blood cells under hypoxic conditions), and by protein/peptide degradation in whole blood [76].
Electrochemical detection methods are popular for quantitative analysis of blood parameters [77]. The iSTAT device from Abbott Laboratories (Abbott Park, IL, USA), which uses microfabricated thin-film electrodes to measure levels of electrolytes, general chemistries, blood gases, and hematocrit, has an electrochemical detection system which includes amperometry, voltammetry, and conductance, depending on the analyte [5]. The iSTAT device uses disposable cartridges for performing sample preconcentration and separation, and a portable instrument for electrochemical detection [12]. Conventional glucose meters are also based on electrochemical assays [77, 78]. However, devices that feature electrochemical detection have several disadvantages with regard to POC testing. Electrodes are required to be integrated onto the disposable, increasing per-test costs; detecting hundreds of simultaneous reactions at once is difficult to achieve with electrodes; and incompatibilities exist between capabilities of existing microelectronics fabrication facilities and specifications of sensors, with regard to dimensions, materials, passivation layer, and others [5, 77]. With the increasing availability of cheap, high-quality optoelectronic components such as CCDs and laser diodes, optical detection may be more suited for POC testing of blood chemistry parameters. For situations where semiquantitative analysis is sufficient, paper-based microfluidic devices may be attractive [78, 79].
4.5 Hematology
The most widely tested hematology parameters in point-of-care situations are hemoglobin and hematocrit (for anemia, red blood cell transfusion therapy, and acute hemodilution during surgery), and coagulation/clotting time (for cardiac surgical and catheterization procedures) [80]. Sphere Medical (Cambridge, United Kingdom) has developed a microanalyzer technology with silicon chips for signal processing and sensing based on three transducer technologies: potentiometry, amperometry, and conductimetry. Different membranes and receptor materials are used to cover the sensors to detect specific analytes. The technology can measure hematocrit and small molecule analytes.
Activated clotting time, activated partial thromboplastin time, and prothrombin time are monitored for high-dose heparin therapy (a blood clot inhibitor) and blood-thinning medications (such as warfarin). Companies with POC instruments for monitoring coagulation include Medtronic (Minneapolis, MN, USA), Abbott Diagnostics (Abbott Park, IL, USA), Roche Diagnostics (Indianapolis, IN, USA), and Hemosense (owned by Alere) (Waltham, MA, USA).
5 Outlook
Over the last decade, microdevices for point-of-care testing have generated great progress in both academic and industrial laboratories. Several challenges remain before these technologies can be translated to be effective POC tests, including the need to miniaturize all peripheral instrumentation. An important recent trend is the increased attention in developing POC tests for the developing world [4, 5]. Although targeted toward use in emerging and low-income countries, the design constraints are remarkably similar across the world (Fig. 1.1). Trends toward decentralized healthcare and personalized medicine ensure the importance in the future of microdevices for point-of-care testing.
References
P.N. Floriano, Microchip-based assay systems: methods and applications: (Humana Press, Totowa, 2007)
L.J. Kricka, Microchips, microarrays, biochips and nanochips: personal laboratories for the 21st century, Clin. Chim. Acta 307, 219–223 (2001).
J. Lii, W. Hsu, W. Lee and S.K. Sia, Microfluidics, in Kirk-Othmer Encyclopedia of Chemical Technology (Wiley, New York, 2006)
P. Yager, T. Edwards, E. Fu, K. Helton, K. Nelson, M.R. Tam, and B.H. Weigl, Microfluidic diagnostic technologies for global public health. Nature 442, 412–418 (2006)
C.D. Chin, V. Linder, and S.K. Sia, Lab-on-a-chip devices for global health: Past studies and future opportunities. Lab on a Chip 7, 41–57 (2007)
P. Yager, G.J. Domingo, and J. Gerdes, Point-of-care diagnostics for global health. Annu. Rev. Biomed. Eng. 10, 107–144 (2008)
S.K. Sia and L.J. Kricka, Microfluidics and point-of-care testing. Lab Chip 8, 1982–1983 (2008)
G.M. Whitesides, The origins and the future of microfluidics. Nature 442, 368–373 (2006)
J.B. Angell, S.C. Terry, and P.W. Barth, Silicon Micromechanical Devices. Sci. Am. 248, 44-55 (1983)
D. Mabey, R.W. Peeling, A. Ustianowski, and M.D. Perkins, Diagnostics for the developing world. Nat. Rev. Microbiol. 2 231–40 (2004)
I.R. Lauks, Microfabricated biosensors and microanalytical systems for blood analysis. Acc. of Chem. Res. 31, 317–324 (1998)
A.J. Tudos, G.A.J. Besselink, and R.B.M. Schasfoort, Trends in miniaturized total analysis systems for point-of-care testing in clinical chemistry. Lab Chip 1, 83–95 (2001)
P. Belgrader, S. Young, B. Yuan, M. Primeau, L.A. Christel, F. Pourahmadi, and M.A. Northrup, A battery-powered notebook thermal cycler for rapid multiplex real-time PCR analysis. Anal. Chem. 73 286, 391 (2001)
C.T. Culbertson, Y. Tugnawat, A.R. Meyer, G.T. Roman, J.M. Ramsey, and S.R. Gonda, Microchip separations in reduced-gravity and hypergravity environments. Anal. Chem. 77, 7933–7940 (2005)
A.M. Skelley, J.R. Scherer, A.D. Aubrey, W.H. Grover, R.H.C. Ivester, P. Ehrenfreund, F.J. Grunthaner, J.L. Bada, and R.A. Mathies, Development and evaluation of a microdevice for amino acid biomarker detection and analysis on Mars, Proc. Natl. Acad. Sci. 102, 1041–1046 (2005)
T. Akiyama, S. Gautsch, N.F. de Rooij, U. Staufer, P. Niedermann, L. Howald, D. Muller, A. Tonin, H.R. Hidber, W.T. Pike, and M.H. Hecht, Atomic force microscope for planetary applications. Sensor. Actuat. A-Phys. 91, 321–325 (2001)
WHO, The global burden of disease: 2004 update (World Health Organization, Geneva, 2008)
D.A. Hall, J. Ptacek, and M. Snyder, Protein microarray technology. Mech. Ageing Dev. 128, 161–167 (2007)
P. Madhivanan, K. Krupp, J. Hardin, C. Karat, J.D. Klausner, and A.L. Reingold, Simple and inexpensive point-of-care tests improve diagnosis of vaginal infections in resource constrained settings. Trop. Med. Int. Health 14, 703–708 (2009)
P. von Lode, Point-of-care immunotesting: Approaching the analytical performance of central laboratory methods. Clin. Biochem. 38, 591–606 (2005)
P.N. Floriano, N. Christodoulides, C.S. Miller, J.L. Ebersole, J. Spertus, B.G. Rose, D.F. Kinane, M.J. Novak, S. Steinhubl, S. Acosta, S. Mohanty, P. Dharshan, C.K. Yeh, S. Redding, W. Furmaga, and J.T. McDevitt, Use of Saliva-Based Nano-Biochip Tests for Acute Myocardial Infarction at the Point of Care: A Feasibility Study. Clin. Chem. 55, 1530–1538 (2009)
M. Radisic, R.K. Iyer, and S.K. Murthy, Micro- and nanotechnology in cell separation. Int. J. Nanomedicine 1, 3–14 (2006)
P. Sethu, M. Anahtar, L.L. Moldawer, R.G. Tompkins, and M. Toner, Continuous row microfluidic device for rapid erythrocyte lysis. Anal. Chem. 76, 6247–6253 (2004)
X. Chen, D.F. Cui, C.C. Liu, H. Li, and J. Chen, Continuous flow microfluidic device for cell separation, cell lysis and DNA purification. Anal. Chim. Acta 584, 237–243 (2007)
A. Niemz, T.M. Ferguson, and D.S. Boyle, Point-of-care nucleic acid testing for infectious diseases. Trends Biotechnol. 29, 240–250 (2011)
R.D. Johnson, V.G. Gaualas, S. Daunert, and L.G. Bachas, Microfluidic ion-sensing devices. Anal. Chim. Acta 613, 20–30 (2008)
J. Moorthy and D.J. Beebe, A hydrogel readout for autonomous detection of ions in microchannels. Lab Chip 2, 76–80 (2002)
R.J. Meagher, A.V. Hatch, R.F. Renzi, and A.K. Singh, An integrated microfluidic platform for sensitive and rapid detection of biological toxins. Lab Chip 8 2046–53 (2008)
H. Parsa, C.D. Chin, P. Mongkolwisetwara, B.W. Lee, J.J. Wang, and S.K. Sia, Effect of volume- and time-based constraints on capture of analytes in microfluidic heterogeneous immunoassays. Lab Chip 8, 2062–2070 (2008)
S.K. Sia, V. Linder, B.A. Parviz, A. Siegel, and G.M. Whitesides, An integrated approach to a portable and low-cost immunoassay for resource-poor settings. Angew. Chem. Int. Ed. Engl. 43, 498–502 (2004)
C.D. Chin, T. Laksanasopin, Y.K. Cheung, D. Steinmiller, V. Linder, H. Parsa, J.J. Wang, H. Moore, R. Rouse, G. Umviligihozo, E. Karita, L. Mwamarangwe, S. Braunstein, J.V.D. Wijgert, R. Sahabo, J. Justman, W. El-Sadr, and S.K. Sia, Microfluidics-based diagnostics of infectious diseases in the developing world. Nat. Med. 17, 1015–1019 (2011)
T. Thorsen, S.J. Maerkl, and S.R. Quake, Microfluidic large-scale integration Science 298, 580–584 (2002)
M. Herrmann, E. Roy, T. Veres, and M. Tabrizian, Microfluidic ELISA on non-passivated PDMS chip using magnetic bead transfer inside dual networks of channels. Lab Chip 7, 1546–1552 (2007)
K.A. Addae-Mensah, Y.K. Cheung, V. Fekete, M.S. Rendely, and S.K. Sia, Actuation of elastomeric microvalves in point-of-care settings using handheld, battery-powered instrumentation. Lab Chip 10, 1618–1622 (2010)
D.B. Weibel, M. Kruithof, S. Potenta, S.K. Sia, A. Lee, and G.M. Whitesides, Torque-actuated valves for microfluidics Anal. Chem. 77 4726–4733 (2005)
J. Ziegler, M. Zimmermann, P. Hunziker, and E. Delamarche, High-performance immunoassays based on through-stencil patterned antibodies and capillary systems. Anal. Chem. 80, 1763–1769 (2008)
L. Gervais and E. Delamarche, Toward one-step point-of-care immunodiagnostics using capillary-driven microfluidics and PDMS substrates. Lab Chip 9, 3330–3337 (2009)
J. Moorthy, G.A. Mensing, D. Kim, S. Mohanty, D.T. Eddington, W.H. Tepp, E.A. Johnson, and D.J. Beebe, Microfluidic tectonics platform: A colorimetric, disposable botulinum toxin enzyme-linked immunosorbent assay system. Electrophoresis 25, 1705–1713 (2004)
V. Linder, S.K. Sia, and G.M. Whitesides, Reagent-loaded cartridges for valveless and automated fluid delivery in microfluidic devices. Anal. Chem. 77, 64–71 (2005)
D. Juncker, H. Schmid, U. Drechsler, H. Wolf, M. Wolf, B. Michel, N. de Rooij, and E. Delamarche, “Autonomous microfluidic capillary system, Anal. Chem. 74 6139–6144 (2002)
K.Y. Weng, N.J. Chou, and J.W. Cheng, Triggering vacuum capillaries for pneumatic pumping and metering liquids in point-of-care immunoassays. Lab Chip 8, 1216–1219 (2008)
C.M. Cheng, A. W. Martinez, J. Gong, C.R. Mace, S.T. Phillips, E. Carrilho, K.A. Mirica, and G.M. Whitesides, Paper-based ELISA. Angew. Chem. Int. Ed. Engl. 49, 4771–4774 (2010)
A.E. Herr, A.V. Hatch, D.J. Throckmorton, H.M. Tran, J.S. Brennan, W.V. Giannobile, and A.K. Singh, Microfluidic immunoassays as rapid saliva-based clinical diagnostics. Proc. Natl. Acad. Sci. U. S. A. 104, 5268–5273 (2007)
B.S. Lee, Y.U. Lee, H.S. Kim, T.H. Kim, J. Park, J.G. Lee, J. Kim, H. Kim, W.G. Lee, and Y.K. Cho, Fully integrated lab-on-a-disc for simultaneous analysis of biochemistry and immunoassay from whole blood. Lab Chip 11, 70–78 (2011)
H. Tsutsui and C.M. Ho, Cell separation by non-inertial force fields in microfluidic systems. Mech. Res. Commun. 36, 92–103 (2009)
V. VanDelinder and A. Groisman, Separation of plasma from whole human blood in a continuous cross-flow in a molded microfluidic device. Anal. Chem. 78, 3765–3771 (2006)
N.N. Ma, K.W. Koelling, and J.J. Chalmers, Fabrication and use of a transient contractional flow device to quantify the sensitivity of mammalian and insect cells to hydrodynamic forces. Biotechnol. Bioeng. 80, 428–437 (2002)
I. Doh and Y.H. Cho, A continuous cell separation chip using hydrodynamic dielectrophoresis (DEP) process. Sensor. Actuat. A-Phys. 121, 59–65 (2005)
M.M. Wang, E. Tu, D.E. Raymond, J.M. Yang, H.C. Zhang, N. Hagen, B. Dees, E.M. Mercer, A.H. Forster, I. Kariv, P.J. Marchand, and W.F. Butler, Microfluidic sorting of mammalian cells by optical force switching. Nat. Biotechnol. 23, 83–87 (2005)
Y. Sai, M. Yamada, M. Yasuda, and M. Seki, Continuous separation of particles using a microfluidic device equipped with flow rate control valves. J. Chromatogr. A 1127, 214–220 (2006)
F. Petersson, L. Aberg, A.M. Sward-Nilsson, and T. Laurell, Free flow acoustophoresis: Microfluidic-based mode of particle and cell separation. Anal. Chem. 79 5117–5123 (2007)
X.H. Cheng, D. Irimia, M. Dixon, K. Sekine, U. Demirci, L. Zamir, R.G. Tompkins, W. Rodriguez, and M. Toner, A microfluidic device for practical label-free CD4+T cell counting of HIV-infected subjects. Lab Chip 7, 170–178 (2007)
A. Osei-Bimpong, C. Jury, R. McLean, and S.M. Lewis, Point-of-care method for total white cell count: an evaluation of the HemoCue WBC device. Int. J. Lab. Hematol. 31, 657–664 (2009)
L.V. Rao, B.A. Ekberg, D. Connor, F. Jakubiak, G.M. Vallaro, and M. Snyder, “Evaluation of a new point of care automated complete blood count (CBC) analyzer in various clinical settings. Clin. Chim. Acta. 389, 120–125 (2008)
X. Cheng, Y.S. Liu, D. Irimia, U. Demirci, L. Yang, L. Zamir, W.R. Rodriguez, M. Toner, and R. Bashir, Cell detection and counting through cell lysate impedance spectroscopy in microfluidic devices. Lab Chip 7, 746–755 (2007)
J.V. Jokerst, P.N. Floriano, N. Christodoulides, G.W. Simmons, and J.T. McDevitt, Integration of semiconductor quantum dots into nano-bio-chip systems for enumeration of CD4 + T cell counts at the point-of-need. Lab Chip 8, 2079–2090 (2008)
D. Schafer, E.A. Gibson, E.A. Salim, A.E. Palmer, R. Jimenez, and J. Squier, Microfluidic cell counter with embedded optical fibers fabricated by femtosecond laser ablation and anodic bonding. Opt. Express 17, 6068–6073 (2009)
S. Mtapuri-Zinyowera, M. Chideme, D. Mangwanya, O. Mugurungi, S. Gudukeya, K. Hatzold, A. Mangwiro, G. Bhattacharya, J. Lehe, and T. Peter, Evaluation of the PIMA point-of-care CD4 analyzer in VCT clinics in Zimbabwe. J. Acquir. Immune. Defic. Syndr. 55, 1–7 (2010)
Z. Wang, S.Y. Chin, C.D. Chin, J. Sarik, M. Harper, J. Justman, and S.K. Sia, Microfluidic CD4 + T-cell counting device using chemiluminescence-based detection. Anal. Chem. 82, 36–40 (2010)
T.M. Lee and I.M. Hsing, DNA-based bioanalytical microsystems for handheld device applications. Anal. Chim. Acta. 556, 26–37 (2006)
M.A. Dineva, L. MahiLum-Tapay, and H. Lee, Sample preparation: a challenge in the development of point-of-care nucleic acid-based assays for resource-limited settings. Analyst 132, 1193–1199 (2007)
L. Chen, A. Manz, and P.J. Day, Total nucleic acid analysis integrated on microfluidic devices. Lab Chip 7, 1413–1423 (2007)
F.M. Ausubel et al., Short Protocols in Molecular Biology: A Compendium of Methods from Current Protocols in Molecular Biology (Wiley, New York, 1992)
C. Lui, N.C. Cady, and C.A. Batt, Nucleic Acid-based Detection of Bacterial Pathogens Using Integrated Microfluidic Platform Systems. Sensors 9, 3713–3744 (2009)
A.G. Crevillen, M. Hervas, M.A. Lopez, M.C. Gonzalez, and A. Escarpa, Real sample analysis on microfluidic devices. Talanta 74, 342–357 (2007)
J.S. Marcus, W.F. Anderson, and S.R. Quake, Microfluidic single-cell mRNA isolation and analysis. Anal. Chem. 78, 3084–3089 (2006)
L.A. Christel, K. Petersen, W. McMillan, and M.A. Northrup, Rapid, automated nucleic acid probe assays using silicon microstructures for nucleic acid concentration. J. Biomech. Eng-Trans. ASME 121, 22–27 (1999)
WHO, Roadmap for rolling out Xpert MTB/RIF for rapid diagnosis of TB and MDR-TB (World Health Organization, Geneva, 2010). 6 Dec 2010
C.C. Boehme, P. Nabeta, D. Hillemann, M.P. Nicol, S. Shenai, F. Krapp, J. Allen, R. Tahirli, R. Blakemore, R. Rustomjee, A. Milovic, M. Jones, S.M. O’Brien, D.H. Persing, S. Ruesch-Gerdes, E. Gotuzzo, C. Rodrigues, D. Alland, and M.D. Perkins, Rapid molecular detection of tuberculosis and rifampin resistance. N. Engl. J. Med. 363, 1005–1015 (2010)
C.S. Zhang, J.L. Xu, W.L. Ma, and W.L. Zheng, PCR microfluidic devices for DNA amplification. Biotechnol. Adv. 24, 243–284 (2006)
N.C. Cady, S. Stelick, M.V. Kunnavakkam, and C.A. Batt, Real-time PCR detection of Listeria monocytogenes using an integrated microfluidics platform. Sensor. Actuat. B-Chem. 107, 332–341 (2005)
D. Braun, PCR by thermal convection. Mod. Phys. Lett. B 18, 775–784 (2004)
D.S. Lee, S.H. Park, H.S. Yang, K.H. Chung, T.H. Yoon, S.J. Kim, K. Kim, and Y.T. Kim, Bulk-micromachined submicroliter-volume PCR chip with very rapid thermal response and low power consumption. Lab Chip 4, 401–407 (2004)
J. Van Ness, L.K. Van Ness, and D.J. Galas, Isothermal reactions for the amplification of oligonucleotides. Proc. Natl. Acad. Sci. U. S. A. 100, 4504–4509 (2003)
T.A. Taton, C.A. Mirkin, and R.L. Letsinger, Scanometric DNA array detection with nanoparticle probes. Science 289, 1757–1760 (2000)
E. Schleicher, The clinical chemistry laboratory: current status, problems and diagnostic prospects. Anal. Bioanal. Chem. 384, 124–131 (2006)
F.B. Myers and L.P. Lee, Innovations in optical microfluidic technologies for point-of-care diagnostics. Lab Chip 8, 2015–2031 (2008)
A.W. Martinez, S.T. Phillips, M.J. Butte, G.M. Whitesides, Patterned paper as a platform for inexpensive, low-volume, portable bioassays. Angew. Chem. Int. Ed. 46, 1318–1320 (2007)
A.W. Martinez, S.T. Phillips, G.M. Whitesides, Three-dimensional microfluidic devices fabricated in layered paper and tape, Proc. Natl. Acad. Sci. 105, 19606–19611 (2008).
G.J. Kost, Principles and Practice of Point-of-Care Testing: (LWW, Philadelphia, 2002)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Chin, C.D., Chin, S.Y., Laksanasopin, T., Sia, S.K. (2013). Low-Cost Microdevices for Point-of-Care Testing. In: Issadore, D., Westervelt, R. (eds) Point-of-Care Diagnostics on a Chip. Biological and Medical Physics, Biomedical Engineering. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-29268-2_1
Download citation
DOI: https://doi.org/10.1007/978-3-642-29268-2_1
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-29267-5
Online ISBN: 978-3-642-29268-2
eBook Packages: Physics and AstronomyPhysics and Astronomy (R0)