Abstract
Sporotrichosis is a subacute or chronic disease that afflicts animals and humans, caused by the dimorphic fungus Sporothrix schenckii. Although it has a universal distribution, sporotrichosis is more frequent in regions with tropical and subtropical climates, being the most common subcutaneous mycosis in Latin America. Sporotrichosis affects both sexes and can occur at any age. Recently, it has been proposed, based on physiologic and molecular aspects, that S. schenckii is a complex of four distinct species: S. brasiliensis, S. mexicana, S. globosa, and S. schenckii sensu strictu.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Chronic Obstructive Pulmonary Disease
- Erythema Multiforme
- Hematogenous Dissemination
- Cutaneous Form
- Anterior Chamber Paracentesis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Core Messages-
Sporotrichosis is caused by the dimorphic fungus Sporothrix schenckii.
-
Disease can be transmitted by direct inoculation via trauma or close contact with infected animals, especially the domestic cat.
-
Disease has a subacute/chronic course with cutaneous or extracutaneous involvement.
-
The lymphocutaneous form is the most common mode of presentation of sporotrichosis.
-
Humoral and cellular immune responses as well as the mode of inoculation and the virulence of the fungus seem to affect the clinical form of the disease.
-
Ophthalmic manifestations include palpebral lesions, granulomatous conjunctivitis, anterior and/or posterior granulomatous uveitis and endophthalmitis.
1 Definition
Sporotrichosis is a subacute or chronic disease that afflicts animals and humans, caused by the dimorphic fungus Sporothrix schenckii. Although it has a universal distribution, sporotrichosis is more frequent in regions with tropical and subtropical climates, being the most common subcutaneous mycosis in Latin America [3, 11, 18]. Sporotrichosis affects both sexes and can occur at any age. Recently, it has been proposed, based on physiologic and molecular aspects, that S. schenckii is a complex of four distinct species: S. brasiliensis, S. mexicana, S. globosa, and S. schenckii sensu strictu [13].
2 Clinical Manifestations
2.1 General Disease
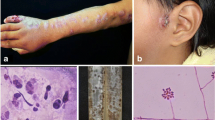
Systemic diseases may be divided into cutaneous and extracutaneous clinical forms. The cutaneous form can either be lymphocutaneous, localized, or disseminated. The lymphocutaneous form is the most common and is characterized by a primary lesion which may be a papule, nodule, or ulcer, generally occurring in the upper extremities. From this initial lesion, a chain of painless cutaneous nodes appears, which may soften and ulcerate along the route of lymphatic channels, in a “sporotrichoid pattern” (Fig. 126.1a). The second most common manifestation is the localized cutaneous form, in which the lesion remains restricted to the site of inoculation, as a verrucose plaque or an ulcero-vegetant lesion, indistinctive from chromomycosis, verrucous tuberculosis, and American tegumentary leishmaniasis. The disseminated cutaneous form affects especially immunosuppressed patients. The lesions are usually papules or nodules that can ulcerate and are diffusely located on various segments of the skin, unrelated to the site of inoculation [11, 18, 21].
(a) Typical lymphocutaneous sporotrichosis. (b) Positive culture for Sporothrix schenckii. (c) Parinaud’s oculoglandular syndrome secondary to Sporothrix schenckii infection. (d) Fundus photography showing retinal granuloma and fluffy opacities in a subject with sporotrichosis ((b, d) Reproduced with permission from Curi et al. [6])
The extracutaneous forms are very rare and difficult to diagnose, accounting for less than 5 % of cases. The osteoarticular tissue beyond the skin is the most frequently involved. However, any organ or tissue can be affected by sporotrichosis, and symptoms are related to the compromised organ. The disease may also involve the lungs, the nervous system, the testicles, and the ocular, oral, nasal, pharyngeal, and laryngeal mucosae. Diabetes mellitus, alcoholism, leukemia, chronic obstructive pulmonary disease, and AIDS, as well as drug immunosuppression for organ transplantation or for autoimmune diseases, may predispose to this form of sporotrichosis [11, 18, 21].
In a recent sporotrichosis epidemic transmitted by cats in the state of Rio de Janeiro, Brazil, unusual clinical forms with disseminated cutaneous lesions associated with involvement of conjunctival and/or nasal mucosae have been described in immunocompetent individuals. Likewise, there were also manifestations of hypersensitivity such as erythema nodosum, erythema multiforme, and inflammatory arthritis, the latter described for the first time in association with sporotrichosis [2, 7, 9, 10, 16, 17].
2.2 Ocular Disease
Manifestations of ocular sporotrichosis include palpebral lesions, granulomatous conjunctivitis, anterior and/or posterior granulomatous uveitis, and endophthalmitis [5].
Ocular trauma and close contact with infected animals are usually reported. Schubach et al. described two cases of primary Sporothrix schenckii conjunctivitis without cutaneous or pulmonary involvement, which were presumably related to close contact between the patient and an infected cat [16]. Various cases of Parinaud’s oculoglandular syndrome due to Sporothrix schenckii diagnosed by conjunctival biopsy and/or smear have been also recently observed in Rio de Janeiro (unpublished data – Fig. 126.1c).
The majority of cases of intraocular sporotrichosis present as a granulomatous uveitis and eventually evolve to endophthalmitis. Hematogenous dissemination of the fungus may be implicated in these cases. Cartwright et al. [4] described a case of granulomatous uveitis which, despite specific therapy, progressed to endophthalmitis. Vieira-Dias et al. [22] reported a case of granulomatous uveitis in which the diagnosis of ocular sporotrichosis was achieved by anterior chamber paracentesis and isolation of the fungus in culture. Font and Jakobiec [8] described a case of ocular sporotrichosis affecting mainly the retina and the vitreous. Diagnosis was performed by means of histopathological examination since the condition progressed to endophthalmitis. Curi et al. [6] described a case of disseminated sporotrichosis with a retinal granuloma (Fig. 126.1d) and vitritis, which regressed after specific therapy.
3 Etiology and Pathogenesis
S. schenckii lives saprophytically in nature and may be isolated from the soil and organic matter. Transmission is caused through inoculation via skin trauma [11, 12, 18]. Some animals can transmit S. schenckii, but it is the cat that has the highest zoonotic potential. The fungus may be transmitted through scratches, bites, coughing, sneezing, and contact with cutaneous exudates [17]. People who are especially exposed to these conditions, such as foresters, gardeners, veterinarians, and animal care professionals, carry a higher risk of infection.
In humans, the lesions usually arise 3–12 weeks after infection. The disease may evolve subclinically with spontaneous cure. In the majority of cases, it is a benign infection restricted to the skin, subcutaneous, and adjacent lymphatic vessels. However, hematogenous dissemination to internal organs can also arise. More rarely, inhalation of the conidium with an initial pulmonary infection and further systemic dissemination may occur [11, 12, 18, 21]. Humoral and cellular immune responses as well as the mode of inoculation and the virulence of the fungus seem to affect the clinical form of the disease [19, 20]. When the microorganisms do not form colonies when incubated at 37 °C but rather at 35 °C, the infection is milder in experimental models [14]. The capacity of S. schenckii to synthesize melanin enhances virulence, as observed in various fungi [15].
4 Diagnosis
Diagnosis of sporotrichosis is based on the isolation of S. schenckii in clinical samples. S. schenckii elements are rarely observed through direct examination. Seeding of the fungus on Sabouraud agar results in the appearance of yellow, brown, or black colonies within 3–5 days (Fig. 126.1b) . To confirm the diagnosis, it is necessary to convert the filamentous form of the fungus into the yeast form which grows in BHI (Brain-Heart Infusion) broth at a temperature of 37 °C. Histopathological examination, which may only be suggestive, is characterized by pyogenic and or granulomatous inflammatory infiltration with the possible presence of cigar-shaped or boat-shaped microorganisms [11, 12, 18].
There are several serological techniques for the diagnosis of sporotrichosis. ELISA (enzyme-linked immunosorbent assay) shows a high sensitivity and specificity [1]. Nevertheless, a positive serological result merely suggests and does not confirm the mycosis. These investigations are especially useful in cases of extracutaneous involvement.
5 Differential Diagnosis
Differential diagnosis includes other systemic fungal diseases, tuberculosis, syphilis, leishmaniasis, atypical mycobacteriosis, and cat scratch disease.
6 Treatment
Itraconazole is the drug of choice, with a dose of 100–200 mg/day after meals for 90 days. Terbinafine may also be used in a dose of 250–500 mg/day, with good results. This medication is particularly useful for patients who use drugs which may interact with imidazoles. Saturated solution of potassium iodide may also be used with good results, although its mechanism of action is unknown. In case of systemic involvement, intravenous amphotericin B deoxycholate (0.25–1 mg/kg/day) or liposomal or colloidal dispersion formulations (1–5 mg/kg/day) are very effective, with a total dose of 2–4 g. The latter formulations are associated with less frequent and intense adverse reactions, allowing the use of larger daily doses and thus shortening the treatment period.
Children should receive itraconazole (5 mg/kg/day or 100 mg/day). If possible, treatment is avoided in pregnant women. Amphotericin B is the preferred drug to be used during gestation.
For cutaneous and lymphocutaneous sporotrichosis, daily heat applications may be used at the lesion site (42–43 °C, for about 15 min, three times a day for several weeks), by means of a hot water bottle, infrared source, or similar method. The application of iodine solutions on open lesions may also help. Additional management with cryotherapy and/or curettage of the lesions may also be beneficial on certain lesions which slowly respond to treatment.
7 Prognosis
The prognosis of the cutaneous and lymphocutaneous forms of sporotrichosis is usually good. Ocular disease will depend on rapid diagnosis and aggressive therapy.
Take-Home Pearls
-
Conjunctival sporotrichosis may occur in the absence of cutaneous disease.
-
Sporotrichosis may be considered in the differential diagnosis of Parinaud’s oculoglandular syndrome.
-
Intraocular sporotrichosis occurs secondarily to disseminated disease.
-
Antifungals are the mainstay of treatment.
-
The prognosis of ocular disease depends on rapid diagnosis and aggressive therapy.
References
Almeida-Paes R, Pimenta MA, Pizzini CV et al (2007) Use of mycelial-phase Sporothrix schenckii exoantigens in an enzyme-linked immunosorbent assay for diagnosis of sporotrichosis by antibody detection. Clin Vaccine Immunol 14:244–249
Barros MB, Schubach Ade O, do Valle AC et al (2004) Cat-transmitted sporotrichosis epidemic in Rio de Janeiro, Brazil: description of a series of cases. Clin Infect Dis 38:529–535
Conti Diaz IA (1989) Epidemiology of sporotrichosis in Latin America. Mycopathologia 108:113–116
Cartwright MJ, Promersberger M, Stevens GA (1993) Sporothrix schenckii endophthalmitis presenting as granulomatous uveitis. Br J Ophthalmol 77:61–62
Curi ALL, Gonçalves RM, Hamdan J et al (2005) Uveítes Fungicas. In: Orefice F (ed) Uveíte Clinica e Cirúrgica. Cultura Médica, Rio de Janeiro, pp 651–675
Curi ALL, Feliz S, Azevedo KML et al (2003) Retinal granuloma due to Sporothrix schenkii. Am J Ophthalmol 136:205–207
de Lima Barros MB, de Oliveira SA, Galhardo MC et al (2003) Sporotrichosis with widespread cutaneous lesions: report of 24 cases related to transmission by domestic cats in Rio de Janeiro, Brazil. Int J Dermatol 42:677–681
Font RL, Jacobiek FA (1976) Granulomatous necrotizing retinochoroiditis caused by Sporotrichum schenckii. Arch Ophthalmol 94:1513–1519
Gutierrez–Galhardo MC, Schubach AO, Barros MBL et al (2002) Erythema nodosum associated with sporotrichosis. Int J Dermatol 41:114–116
Gutierrez-Galhardo MC, Barros MB, Schubach AO et al (2005) Erythema multiforme associated with sporotrichosis. J Eur Acad Dermatol Venereol 9:507–509
Kwon-Chung K, Bennet J (1992) Sporotrichosis. In: Kwon-Chung K, Bennet J (eds) Medical mycology. Lea & Febiger, Philadelphia, p 707
Lacaz CS (1991) Esporotricose e outras micoses gomosas. In: Lacaz CS, Porto C, Martins JEC (eds) Micologia Médica. Sarvier, São Paulo, pp 233–241
Marimon R, Cano J, Gene J, Sutton DA et al (2007) Sporothrix brasiliensis, S. globosa, and S. mexicana, three new Sporothrix species of clinical interest. J Clin Microbiol 45:3198–3206
Mesa-Arango AC, Del Rocio R-MM et al (2002) Phenotyping and genotyping of Sporothrix schenckii isolates according to geographic origin and clinical form of sporotrichosis. J Clin Microbiol 40:3004–3011
Morris-Jones R, Youngchim S, Gomez BL et al (2003) Synthesis of melanin-like pigments by Sporothrix schenckii in vitro and during mammalian infection. Infect Immun 71:4026–4033
Schubach A, de Lima Barros MB, Schubach TM et al (2005) Primary conjunctival sporotrichosis: two cases from a zoonotic epidemic in Rio de Janeiro, Brazil. Cornea 24:491–493
Schubach TM, Schubach AO, Okamoto T et al (2004) Evaluation of an epidemic of sporotrichosis in cats: 347 cases (1998–2001). J Am Vet Med Assoc 224:1623–1629
Rippon J (1988) Sporotrichosis. In: Rippon J (ed) Medical mycology – the pathogenic fungi and pathogenic actinomycetes. WB Saunders Company, Philadelphia, pp 325–352
Tachibana T, Matsuyama T, Mitsuyama M (1998) Characteristic infectivity of Sporothrix schenckii to mice depending on routes of infection and inherent fungal pathogenicity. Med Mycol 36:21–27
Tachibana T, Matsuyama T, Mitsuyama M (1999) Involvement of CD4+ T cells and macrophages in acquired protection against infection with Sporothrix schenckii in mice. Med Mycol 37:397–404
Valle ACF, Gutierrez-Galhardo MC (2012) Esporotricose. In: Tavares W, Marinho A (eds) Rotinas de diagnóstico e tratamento das doenças infecciosas e parasitárias. Atheney, São Paulo, pp 348–352
Vieira-Dias D, Sena CM, Orefice F et al (1997) Ocular and concomitant cutaneous sporotrichosis. Mycoses 40:197–201
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Curi, A.L.L., Galhardo, M.C.G., do Valle, A.C.F. (2016). Sporotrichosis. In: Zierhut, M., Pavesio, C., Ohno, S., Orefice, F., Rao, N. (eds) Intraocular Inflammation. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-75387-2_126
Download citation
DOI: https://doi.org/10.1007/978-3-540-75387-2_126
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-540-75385-8
Online ISBN: 978-3-540-75387-2
eBook Packages: MedicineMedicine (R0)