Abstract
Radiologic measurements of the pelvis and hip are primarily dictated by prior events in the paediatric age group, developmental conditions that present in the young adult and acquired adult hip disorders. Clinically, measurements are helpful for initial diagnosis, follow-up and assessment of the results of treatment. Most of the measurements are performed on plain radiographs. CT and MRI can provide additional measurements due to their capability for detailed anatomic depiction in multiple planes. Regarding each measurement, it is important to know its reproducibility and clinical relevance.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
The requirement for objective measurements of the mature pelvis and hip is primarily dictated by three major aetiologies: prior events in the paediatric age group (acetabular dysplasia, Perthes disease, SUFE), developmental conditions that present in the young adult (acetabular over- or under-coverage, femoroacetabular impingement—FAI) and acquired adult hip disorders (post-traumatic, avascular necrosis, osteoarthritis).
Hip dysplasia is a collective term which refers to a developmental abnormality of the acetabulum, femoral head or both regardless of aetiology. In acetabular dysplasia, most of the measurements utilised in the paediatric age group become unreliable and inappropriate after fusion of the epiphysis, although some (acetabular angle, centre-edge angle) are still useful, reliable and helpful. An array of measurements exists in assessing the adult dysplastic hip, and the more useful and practical ones are presented in this chapter. Most are based on radiographic assessment from the AP view utilising important reproducible and reliable landmarks. The centre-edge angle is important in assessing the superior and lateral femoral head coverage by the acetabulum, while the HTE angle assesses the roof orientation and coverage as well. The percentage of femoral head coverage assesses the congruity of the head in the acetabulum, while the acetabular depth-to-width index declares the acetabular depth. Evidence of dysplasia using these angle measurements on the AP view then requires further assessment of the acetabulum by the faux profile view which allows assessment of the anterior acetabular coverage using the VCA angle or by axial CT assessment which provides sector angles of both the anterior and posterior acetabular coverage.
FAI is described as being of two types: morphological acetabular abnormalities (coxa profunda, protrusio acetabuli, acetabular retroversion) that predispose to a pincer impingement and femoral head asphericity (focal or generalised) leading to cam impingement. However, measurements of the entire hip joint are required as both types are known to coexist in up to 86% of cases. Although measurements for assessing the underlying morphological characteristics of FAI have been established, it is important at the outset that one appreciates the importance of validating that the correct radiographic technique has been used as an essential prerequisite.
Measurements of the hip are also required in assessing the degree of morphological change related to a variety of acquired conditions that involve the hip, namely, the joint space. Trauma to the acetabulum or femoral head, avascular necrosis and primary osteoarthritis are the main conditions that lead to joint changes.
As most of the radiographic techniques are obtained in the supine position, it is important to remember that measurement values based on these projections do not necessarily represent the same acetabular-femoral relationships on dynamic weight-bearing positions. Accuracy and reliability factors apply not just to measurements based on conventional radiographic appearances but also to those based on cross-sectional imaging, namely, CT and MRI. Pelvic symmetry is important to minimise radiographic error rates, but it is also important to realise that the pelvic tilt introduces errors in the measurements not only on conventional radiographs but also in the 2D axial images generated by CT and MRI. Software dedicated to incorporate the pelvic inclination has been developed to reduce this source of error, as well as resorting to carrying out the required measurement parameters from 3D reformatted images. Although CT and MRI are as a rule deemed superior to radiography in providing some measurements, there are still residual unresolved areas of disagreement in the literature. Controversy exists on a number of fronts, ranging from the best modality deemed to be most reliable, the degree of abnormality related to symptom production and the way the measurements are used in clinical/surgical management.
2 Lines and Landmarks in Adult Pelvic/Hip Measurements
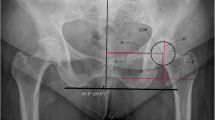
The majority of the tried and tested measurements are made with reference to the radiographic appearances on the AP and cross-lateral views. In the assessment of the adult dysplastic hip, the AP view of the pelvis is obtained with the patient supine, with 15–20° internal rotation of the lower limbs to correct the natural femoral anteversion, an FFD of 120 cm, with the central beam perpendicular to the table centred midway between the superior outline of the symphysis pubis and a line joining the ASIS’s. Criteria for acceptable standards for pelvic radiography are applied to cover correct exposure, symmetric appearance of the pelvis and a true AP appearance of the femoral necks. Radiographs must meet proper validation criteria before they are used for measurement estimation: coccygeal alignment with the mid-symphysis and a distance between the sacrococcygeal joint and the symphysis less than 32 mm in men and 47 mm in women. Anatomical pelvic and hip landmarks act as fixed points allowing reference lines to be made from which distances and subtended angles can be calculated. On the AP radiograph, the following radiographic lines and landmarks are utilised (Fig. 12.1).
(a, b) Acetabular and femoral head landmarks used in hip measurements. The anterior acetabular outline (A) normally lies superiorly and medial to the posterior (P) acetabular outline 1.5 cm apart at the level of the centre of the femoral head. Note that the ilioischial line normally lies medial to the medial wall of the acetabulum and teardrop
-
1.
Acetabular sourcil. Appearing as a curved eyebrow-shaped dense area of subchondral bone, the sourcil cotyloidien is readily identified on the superior weight-bearing articular surface of the acetabulum.
-
2.
Drifting laterally along the sourcil outline and starting from the lateral rim of the acetabulum edge (E point), two lines can be traced following the anterior and posterior acetabular rims. The anterior acetabular rim is less conspicuous and normally lies superior and medial to the easily defined posterior acetabular rim, which is more vertically orientated lying lateral and inferior to the anterior rim. As the acetabulum normally becomes more anteverted from a cranial to a caudal direction, the lines should diverge from their superolateral starting point as they course inferomedially. Along the femoral neck axis from the centre of the femoral head, the lines should be about 1.5 cm apart.
-
3.
The centre of the femoral head (C point) is easily defined due to the femoral head’s spherical shape. Normally the centre of the femoral head is along the same horizontal level as the superior tip of the ipsilateral greater trochanter. The posterior acetabular rim outline normally runs through the centre of the femoral head. A line joining the centre of both femoral heads, the C-C line, is the reference line as the horizontal to which other oblique lines intersect. A reference line parallel to the C-C line can be used instead drawn between the inferior points of the teardrops—horizontal teardrop line—when measuring some angles such as sharp’s angle.
-
4.
Drifting medially towards the medial limit of the weight-bearing sourcil (T point), one can identify the outline of the nonarticulating false acetabulum. The floor of the false acetabulum depicts the acetabular fossa and the most medial rim of the acetabulum.
-
5.
The lower end of the medial acetabular rim inferiorly becomes contiguous with Kohler’s teardrop. The teardrop’s lateral outline represents the wall of the acetabular fossa and is referred to as the acetabular line, while its medial outline is the anteroinferior margin of the quadrilateral surface. The inferiormost point of the acetabulum is the lower limit of the teardrop (I point). The teardrop is seen just above and lateral to the superolateral outline of the obturator foramen. On radiographs the teardrop is lateral to the ilioischial line. The wall of the acetabular fossa (which represents the medial acetabular floor inferiorly and is seen as the acetabular line) forms the lateral border of the teardrop which is continuous with the medial border of the tear drop which represents the cortex of the ischioilial pelvic wall. The acetabular fossa therefore normally lies lateral to the ilioischial line, and the medial acetabular rim denotes the limits of the medial joint space which should not be confused with the ilioischial line.
-
6.
The ilioischial line. The ilioischial line is actually formed by that portion of the quadrilateral plate which is tangential to the central beam projected as a line. It extends cranially towards the medial outline of the ilium of the pelvic brim, while caudally it merges with the medial outline of the ischium (Fig. 12.1). The acetabular line lies lateral to the ilioischial line in men by an average of 2 mm, while in women the acetabular line is an average of 1 mm medial to the ilioischial line. The acetabular line, which is the medial wall of the acetabulum, and the ilioischial line, which is a portion of the quadrilateral plate, are centrally located structures. Being centrally located, their interrelationship is not significantly affected by minimal degrees of rotation. It is this relationship that is measured in assessing their relative positions to establish the diagnosis of coxa profunda (deep acetabulum) and protrusio acetabuli. Estimating the medial acetabular wall thickness from AP radiographs for reaming capacity at hip arthroplasty is unreliable. For this purpose, CT is needed to measure the smallest quadrilateral plate acetabular distance (QPAD) which has a mean thickness normally of 1.1 mm, increasing directly proportionally with degree of severity up to 8 mm in dysplastic hips.
-
7.
Hip centre. The hip centre position is determined by the position of the medial aspect of the femoral head relative to the ilioischial line. The centre is lateralised if this distance is greater than 10 mm and not lateralised if its less than 10 mm. Lateralised femoral heads are considered to be a sign of structural instability or dysplasia.
-
8.
Skinner’s line. On an AP view of the pelvis, a line is drawn through and parallel to the femoral shaft axis. A second line (Skinner’s) is then drawn tangentially from the tip of the greater trochanter perpendicular to the shaft axis. The fovea capitis should normally lie at the level or above this line (Fig. 12.2). If the fovea lies below this line, then this indicates that the femur is displaced superiorly in relation to the head which is due to a fracture or other causes of coxa vara.
3 Joint Space Width (JSW): Teardrop Distance
3.1 Definition
The joint space width (JSW) is the distance from the most proximal surface of the femoral head to the opposing articular surface of the acetabulum.
The teardrop distance is defined as the distance from the lateral margin of the pelvic teardrop to the most medial aspect of the femoral head.
3.2 Indications
The hip joint space width is used for diagnosis and monitoring of osteoarthritis.
The teardrop distance is used for depicting joint fluid and early Perthes disease as discussed in the paediatric chapter.
3.3 Technique
AP radiography (Fig. 12.3).
3.4 Full Description of Technique
For follow-up measurement in the same individual, more than one joint space value is selected.
-
SJ: Super joint space is the distance from the femoral head subchondral outline to the acetabular sourcil line at 90° from the C-C horizontal line.
-
AJ: Axial joint space is the corresponding distance just lateral to the acetabular fossa (medial border of sourcil bony condensation).
-
MJ: Medial joint space is the distance along the C-C horizontal line through the centre of the femoral heads.
Normal JSW | ||
SJS | >40 years | 4 mm (2–7 mm) |
<40 years | 4 mm (3–6 mm) | |
AJS | <40 years | 4 mm (3–7 mm) |
>40 years | 4 mm (2–7 mm) | |
MJS | <40 years | 8 mm (4–12 mm) |
>40 years | 8 mm (4–14 mm) | |
Abnormal JSW | ||
Hip OA is defined according to minimum joint spaces of <2.5 mm (“probable” OA) and <1.5 mm (“definite” OA) | ||
The teardrop distance is defined as the distance from the lateral margin of the pelvic teardrop to the most medial aspect of the femoral head on an AP pelvic radiograph. Measurements of the teardrop distance are not influenced by age and positioning provided that there is no more than 30° internal or external rotation of the femur. A teardrop distance widening of 11 mm or more or the presence of a teardrop asymmetry of 2 mm or more, in the absence of degenerative joint disease, is consistent with joint fluid in adults. In the paediatric age group, a distance widening of 2 mm or more is an early indicator of Legg-Calve-Perthes disease.
3.5 Reproducibility/Variation
The SD for a joint space of 4 mm is less than 1 mm. There are no significant conflicting measurements in the literature within this range. The inter- and intraobserver variation is less than 4%.The supine position is employed routinely to obtain an AP pelvic radiograph. Comparative JSW studies in the same patients did not reveal any significant measurement differences in the supine and weight-bearing positions.
3.6 Clinical Relevance/Implications
Conventional radiographs have been used as the primary diagnostic method for hip OA for many decades. Asymmetric joint space narrowing is a highly reliable sign of OA.
It is a very important parameter in the assessment of hips with femoroacetabular impingement. The presence and degree of associated chondral damage carries a significant prognostic significance. A preoperative hip joint space equal or less than 2 mm was found to be predictive of a poor clinical outcome in arthroscopic treatment of FAI with patients subsequently requiring total hip arthroplasty.
3.7 Analysis/Validation of Reference Data
Various studies have challenged the application of absolute measurements since a wide JSW variation exists in the normal values described above, ranging from 3 to 8 mm and from 2 to 6 mm at the superolateral and superomedial sites, respectively, with an associated right/left asymmetry in about 6% of subjects.
In addition, a JSW variability exists because of changes induced by the way patients hold their legs when the joint is painful. Finally, the JSW appears to be related to acetabular anatomy, regardless of the presence of OA, and is larger in dysplasia (negative correlation with CE angle) and smaller in coxa profunda (positive correlation with HTE angle). Technically optimised acquisition of the X-rays is therefore important.
3.8 Conclusion
The limited ability of the plain radiograph to detect osteoarthritis at its early stage limits the usefulness of JSW as a diagnostic tool. However, joint space narrowing can be considered the most reliable marker in the evaluation of the progression of OA.
4 Pelvic Inclination Formula/Pelvic Symmetry
These important considerations need to be re-emphasised, and the readers are recommended to familiarise themselves with the coverage found in the preceding chapter. Some further expansion on the effect of pelvic tilt in the adult measurements will be included in the individual measurements presented in this section with coverage of both radiographic and axial imaging (CT/MRI).
Using the AP view of the pelvis, one can work out whether the degree of pelvic inclination is acceptable by measuring the distance from the superior border of the symphysis pubis to the tip of the coccyx which normally should be between 1 and 3 cm.
This method is preferred to that proposed by Siebenrock et al. who provided measurement values for acceptable pelvic inclination in men and women by measuring the distance from the superior border of the symphysis pubis to the junction of the sacrococcygeal joint. The latter landmark is not always easy to identify.
Normal symphysis pubis–sacrococcygeal junction distance | |
Men | 32.3 mm |
Women | 47.3 mm |
5 Acetabular Version
5.1 Definition
The acetabulum is anteverted when the orientation of its opening is medial to the sagittal plane and retroverted when lateral to the sagittal plane.
5.2 Indications
Patients with hip pain and/or early osteoarthritis. Preoperative planning for surgical correction of the dysplastic hip.
5.3 Techniques
Radiography.
CT.
MRI.
5.4 Full Description of Technique
The acetabulum is normally anteverted. Acetabular anteversion can be first evaluated on the AP radiograph. The AP radiograph for this purpose needs to be obtained in a standard manner. The patient is supine with the legs internally rotated by about 15–20° to adjust for the natural femoral anteversion. In this position, only the tip of the lesser trochanter is seen to project beyond the outline of the medial femoral cortex. The centring of the beam is crucial and is different from the one employed in obtaining an AP radiograph for preoperative planning for a total hip replacement which requires a lower centring point. The employment of the lines and landmarks previously introduced in the assessment of acetabular morphology for this purpose is based on this AP radiograph and not on focal AP views of the individual hip. The hip view is obtained with a different centring point which is not useful or reliable in assessing acetabular anatomical status. In addition the horizontal C-C line and teardrop line cannot be drawn from this hip view. Comparative studies have shown that the relationship of the acetabular rim line configuration alters on the hip view. The hip view produces an increase in the anteversion of the anterior wall of the acetabulum. This means that the anterior and posterior acetabular lines can appear normally related to each other on this view masking the presence of abnormal acetabular morphology. In addition it also falsely increases the apparent depth of the acetabulum. Lastly an altered FFD can also result in a false apparent relationship of the anterior and posterior rim outlines as well.
It is also essential to know the pelvic tilt for reliable interpretation of the hip and acetabular parameters. Pelvic tilt can have a profound effect on the measurements from this AP radiograph. In an acceptable AP radiograph, the tip of the coccyx should point to the middle of the symphysis pubis. Neutral pelvic tilt around the horizontal can be broadly defined if the distance between the superior borders of the symphysis pubis to the sacrococcygeal junction is 3.2 cm in men and 4.7 cm in women. Measurement accuracy however relies on factoring in of the pelvic tilt as previously described in the paediatric section. A shoot-through true lateral pelvic radiograph determines the pelvic tilt which normally should reveal a 60° pelvic inclination angle between the horizontal line and the oblique line joining the symphysis pubis superiorly to the sacral promontory. Increased pelvic tilt is seen on the AP view as an increased distance between the symphysis pubis and the sacrococcygeal joint. This leads to an apparent retroversion of the acetabular rim on both sides with crossover of the anterior and posterior acetabular lines.
On this AP view, the anterior and posterior acetabular rim margins are normally approximately 1.5 cm apart as measured from the centre of the head in a plane vertical to the anterior aspect of the acetabular rim (Fig. 12.4). The distance shown in the figure is lower than the normal range. The acetabulum is anteverted if the line of the anterior aspect of the rim does not cross the line of the posterior aspect of the rim before reaching the lateral aspect of the sourcil. Conversely it is deemed retroverted if the line of the anterior rim does cross the line of the posterior rim before reaching the lateral edge of the sourcil. If the posterior rim line runs lateral to the femoral head centre, there is posterior acetabular wall over-coverage. In acetabular retroversion, there is anterior acetabular wall over-coverage which results in an approximation of both the acetabular lines with eventual crossover producing a figure-of-eight configuration. True acetabular retroversion has a deficient posterior wall which is highlighted by the centre of the femoral head lying lateral to the posterior aspect of the hip. In anterior over-coverage, the hip also exhibits a crossover sign, but there is no associated posterior wall deficiency.
CT and MRI scans are suitable to draw the lines used to measure acetabular version. A line is drawn midway between the two halves of the pelvis to define the sagittal plane because the scan often cuts the hemipelves at different levels or the body is not perfectly horizontal. On each side, a parallel line is drawn in the sagittal plane, beginning at the posterior margin of the acetabulum. The angle of acetabular anteversion is measured between the line corresponding to the sagittal plane and a line drawn tangential to the anterior and posterior acetabular margins (Fig. 12.5). The normal values for acetabular anteversion are 15–20°.
Anda et al. suggested that the axial CT slice at the femoral head centre is sufficient for measuring acetabular version, but they did not refer this to a gold standard (Fig. 12.6). Using this method, they objectively calculated the acetabular version in males and females as follows:
Males | 18.5 ± 4.5° |
Females | 21.5 ± 5° |
Other authors suggest using the most cranial axial slice through the femoral head claiming that this is more clinically significant and accurate. The cranial slice however not uncommonly has the drawback of a poorly defined anterior edge of the acetabulum promoting inconsistency in measurements (Fig. 12.5).
5.5 Reproducibility/Variation
Although there has been controversy on the accuracy and reproducibility of the methods used in measuring acetabular version, most agree with favouring CT over radiography. CT is highly reproducible if the technique is standardised. CT allows objective assessment of the degree of acetabular retroversion as specific measurements can be made. Two critical issues need to be agreed to optimise CT—a standard axial level for the measurement and the effect of pelvic tilt. The accuracy of CT measurements to a large part relates to the points on the acetabulum from which these measurements are made. This is complicated by the anatomical fact that the acetabulum normally becomes more anteverted as one extends from a cranial to caudal plane, so that the level at which the measurements are made significantly affects the resultant values. There is still no universal agreement on the axial level at which acetabular version is measured.
As explained above, pelvic tilt does alter the measurements. Radiographically the relationship of the acetabular walls to each other including the presence/absence of the crossover sign can be greatly affected by the degree of pelvic tilt. CT analysis is also affected by the degree of pelvic tilt which means that establishing a measurement in relation to a fixed anatomical landmark is beneficial. Anterior pelvic tilt reduces the acetabular anteversion, whereas posterior pelvic tilt (an upright pelvic position) increases it. A neutral position of the pelvis may be obtained by placing the patients in the prone position, with the anterior tips of the iliac crests and the symphysis pubis resting on the table. Care should be taken for scanning the pelvis at exactly the same height at both sides.
In a comparative study, 2D CT measurements were done at two different axial levels—cranially at the level of the top of the femoral head and caudally at the equator of the femoral head. The measurements were then repeated after pelvic tilt correction.
The mean version results were as follows:
Cranial slice | 9.3° (SD 6.5) | Before pelvic tilt correction |
15.7° (SD 8.0) | After pelvic tilt correction | |
Caudal slice | 16.4° (SD 4.2) | Before pelvic tilt correction |
19.0° (SD 5.0) | After pelvic tilt correction |
In a further comparative study between the above 2D CT measurements and a method using 3D CT measurements which automatically corrects for pelvic tilt, the cranial measurements after pelvic tilt correction had the best intraclass correlation coefficient.
5.6 Clinical Relevance/Implications
On cross-sectional imaging (CT or MR), retroversion can be identified if the anterior rim of the acetabulum is lateral to the posterior rim on the first axial image that includes the femoral head.
5.7 Analysis/Validation of Reference Data
A number of CT-based studies have shown that the acetabular version increases caudally in both normal and dysplastic hips. Traditionally, DDH was thought to be associated with anteversion of the acetabulum. Recently, an association between DDH and acetabular retroversion has been shown. Therefore, the quantification of the retroversion is important for treatment planning. In addition, various disorders have been associated with retroversion, and therefore quantification of retroversion is important in patients with non-specific hip pain.
5.8 Conclusion
Proper assessment of the standard AP radiograph may reliably suggest the presence of a normally anteverted acetabulum or the presence of acetabular retroversion, but CT is required to provide specific objective measurements. The 2D CT axial methods give variable results for acetabular version depending on whether pelvic tilt has been accounted for and the axial level chosen. Acetabular retroversion is a form of acetabular dysplasia and is commonly found in patients with osteoarthritis, DDH and Legg-Calve-Perthes disease. This condition may result from a traumatically induced premature closure of the triradiate cartilage in childhood or may be idiopathic. Clinically, it can be associated with hip and groin pain, clicking and clunking.
6 Acetabular or Sharp’s Angle
This angle is used before and after skeletal maturity and is covered in the previous chapter.
7 Centre-Edge or Wiberg’s Angle
7.1 Definition
The centre-edge (CE) angle is formed from the centre of the femoral head and two lines: a vertical one through the centre of the femoral head parallel to the long axis of the body and the other to the superolateral rim of the acetabulum.
7.2 Indications
This important angle is the starting point for assessing the dysplastic hip because an abnormal value is diagnostic. The CE angle, originally described by Wiberg, evaluates the degree of superior and lateral acetabular coverage of the femoral head in the frontal plane, in patients with suspected DDH, and assesses the outcome after reduction.
7.3 Technique
AP radiography (Fig. 12.7).
7.4 Full Description of Technique
The CE angle is formed by a vertical line through the centre of the femoral head and parallel to the longitudinal body axis and the line connecting the centre of the femoral head with the most lateral point (E) of the acetabular sourcil. The vertical line through the centre of the femoral head should be perpendicular to the C-C line joining the centres of the femoral heads.
Normal | >25° |
Dysplasia | <20° |
Borderline | 20–25° |
Coxa profunda | 39–44° |
Protrusio acetabuli | >44° |
It is important to carefully study the radiographic anatomy of the lateral acetabular margin before drawing the oblique line. If the sourcil and lateral acetabular rim are conjoined laterally (with or without a beak), then the E point is easily defined. If there is a gap between the lateral limit of the sourcil and lateral edge of the lateral acetabular rim, then the oblique line needs to pass through the lateral limit of the sourcil and not the E point. The CE angle is a more reliable measure of head cover when the lateral limit of the sourcil (E2) is chosen as the reference point rather than the lateral edge of the acetabulum (E1) when these two points do not overlap. This is referred to as the refined CE angle or Ogata’s angle. When there is an interval separating the lateral sourcil limit from the lateral edge of the acetabulum, the most lateral point of the acetabular roof on AP radiographs is actually anterior and lateral to the most superior part of the acetabulum. It is imperative to distinguish between these two lateral acetabular points of reference in these circumstances, as the most lateral classical reference point (E1) will overestimate the head coverage (Fig. 12.8).
7.5 Reproducibility/Variation
Highly reproducible if applied after the age of 6. In descriptive statistics comparing measurements in asymptomatic men and women, significant differences were observed. The mean CE angle for all patients was 36.3°, with a measurement of 37.7° (95% CI, 26.9–48.5°) in men and 34.9° (95% CI, 23.5–43°) in women.
7.6 Clinical Relevance/Implications
The CE angle quantifies the subluxation of the femoral head which leads to reduced weight-bearing area and focal concentration of compressive stress resulting to accelerated degeneration of the articular cartilage and osteoarthritis.
Normal values for CE angles are more than 20° for ages 3–17 years and more than 25° in adults. Values below 20° in adults and below 15° in children and adolescents are considered abnormal. Hips with CE angles between 20° and 25° in adults and between 15° and 20° in children and adolescents are “uncertain” for dysplasia hips. The CE angle is associated with the pelvic inclination; a decrease of the CE angle of 2–4° is expected if the pelvis tilts about 15° posteriorly.
Values between 39° and 44° correspond to a deep acetabulum (coxa profunda), whereas values over 44° correspond to protrusio acetabuli.
7.7 Analysis/Validation of Reference Data
Ogata et al. observed that a poor acetabular cover may develop in some hips which originally had a normal CE angle. In these hips, the lateral border of bony condensation (E2) did not reach the lateral rim of the acetabular roof (E1). The classic CE angle measurements thus may overestimate the femoral head coverage, particularly in children between 3 and 8 years of age.
7.8 Conclusion
The CE angle is one of the most easy and widely performed measurements on hip radiographs.
8 Horizontal Toit Externe (HTE) or Tonnis Angle
8.1 Definition
The horizontal toit externe (HTE) angle assesses acetabular inclination and is formed by the horizontal line and the weight-bearing surface of the acetabulum. It is also known as the Bombelli’s angle of weight-bearing zone.
8.2 Indications
The HTE angle is used to evaluate the slope and orientation of the acetabular roof in the coronal plane, providing information about the superolateral coverage of the femoral head by the bony acetabulum.
8.3 Techniques
AP radiography (Fig. 12.9).
8.4 Full Description of Technique
The HTE angle is measured between a line parallel to the horizontal C-C line joining the centres of the femoral heads and an oblique line extending from the most medial point of the weight-bearing acetabulum (T), to the lateral acetabular margin (E). The weight-bearing portion of the acetabulum (sourcil) is demonstrated as a sclerotic and arched appearance.
Normal | 0 to <10° |
Abnormal | |
Dysplasia | >10° |
Pincer type FAI | <0° |
Coxa profunda | −5° |
8.5 Reproducibility/Variation
Highly reproducible.
8.6 Clinical Relevance/Implications
The HTE angle supports further evidence on the possible underlying acetabular dysplasia. Its normal value should be under 10°.
Values over 12° correspond to dysplasia, whereas values less than −5° to a deep acetabulum.
9 ACM Angle (Idelberger-Frank Acetabular Angle)
9.1 Definition
The ACM angle measures the depth of the acetabulum.
9.2 Indication
Acetabular dysplasia.
Normal | 45° (±3°) |
Abnormal | >50° |
9.3 Technique
AP radiography (Fig. 12.10).
9.4 Full Description of Technique
The ACM angle is formed by the AC line and the MC line. The lettering designations of the radiographic landmarks are specific for this measurement and are as follows: A is the most lateral edge of the acetabulum, B is the lowest point of the acetabular margin, M represents the midpoint between A and B, and C is the point on the bony acetabulum intersected by a perpendicular from point M. In young children, the point C can be at the cartilaginous part. If the value of ACM is 45°, the acetabulum can be considered as a hemisphere. The sphericity of the acetabulum decreases with increasing ACM values. In the original description, the normal values range between 42° and 50°. Others showed that in the first 6 years of life, values above 45° can be considered normal. For newborns, this value can even be as high as 60°. Beyond 8 years of age though, the data of various age groups lies between 40° and 45°.
9.5 Reproducibility/Variation
Moderately reproducible because of the poor definition of the depth of the acetabulum and to a lesser degree of the inferior margin of the acetabulum. More reliable and consistent after puberty as landmarks are more readily definable.
9.6 Clinical Relevance/Implications
One of the advantages of this measurement method is that the value of this angle is less sensitive to the position of the pelvis.
9.7 Analysis/Validation of Reference Data
Limited data regarding validation in the value of this measurement in its application before and after puberty.
9.8 Conclusion
Useful particularly in the mature pelvis but not used widely.
10 Acetabular Depth and Acetabular Depth-to-Width Index
10.1 Definition
Acetabular depth is the measurement of the deepest diameter of the acetabulum coverage.
10.2 Indications
Acetabular dysplasia.
10.3 Technique
AP radiography (Fig. 12.11).
Normal | > 9mm |
Abnormal | < 9mm |
10.4 Full Description of Technique
Acetabular depth is defined as the greatest perpendicular distance from the acetabular roof to a line joining the lateral margin of the acetabular roof and the upper corner of the symphysis pubis on the same side. An acetabular depth of <9 mm suggests acetabular dysplasia.
The depth of the acetabulum can be also evaluated by the acetabular depth-to-width index which is estimated by dividing the width (measured from the lateral acetabular rim to the teardrop-apex) by the depth (measured at the most medial point of the weight-bearing acetabulum). The width line (W) of the acetabulum is measured between the E and the I points. Acetabular depth (d) is the length of the line from point T (the medial end of the sourcil) perpendicular to the constructed line depicting W (Fig. 12.12).
The depth-to-width index is calculated by the ratio of depth to width (d/W) multiplied by 100 (Fig. 12.13). Values of the ratio (d/W) × 100 in vivo have been found to be around 60 in adults. In Murphy et al.’s study comparing normal and dysplastic hips with secondary OA, all of the dysplastic hips had an index lower than 39.
Normal index | >39 (Average 60) |
Abnormal (dysplasia) index | <39 |
10.5 Reproducibility/Variation
Moderate reproducibility.
10.6 Clinical Relevance/Implications
Although clinically relevant when <9 mm, the acetabular depth measurement has no upper normal limits. Indeed, a high value may be found in abnormal cases, such as coxa profunda and protrusio acetabuli.
10.7 Analysis/Validation of Reference Data
In a comparative study between normal and dysplastic hips with osteoarthritis, all normal hips were shown to have acetabular index values over 38°.
10.8 Conclusion
Reliable discriminator.
11 Anterior Centre-Edge or VCA (Vertical-Centre-Anterior) Angle of Lequesne and De Seze
11.1 Definition
The VCA angle measured from the false-profile (FP) view is formed by the vertical line through the centre of the femoral head and the line connecting the centre of the femoral head to the most anterior aspect of the acetabulum.
11.2 Indications
When an abnormality of the acetabulum seen on the AP radiograph signals a deficiency of acetabular roof coverage (abnormal CE angle), a false-profile view of the pelvis which allows the measurement of the VCA angle will evaluate the anterior coverage of the acetabulum.
Normal | >25° | Abnormal | <20° |
11.3 Technique
Radiography—false-profile view (Fig. 12.14).
11.4 Full Description of Technique
The anterior centre-edge angle, or VCA angle, is measured on oblique radiographs of the pelvis (false-profile view). The view in essence represents a true lateral view of the abnormal hip. Patients are in the standing position with the pelvis rotated at an angle of 25° relative to the X-ray beam and 65° to the X-ray film cassette. The foot closest to the bucky stand is parallel to the X-ray film cassette plane (Fig. 12.14). The side to be examined is positioned next to the film cassette and the central beam centred on its femoral head. This radiograph is technically correct if the distance between the two femoral heads is approximately the size of one femoral head.
The VCA angle is formed by the vertical line (V) through the centre of the femoral head and the line connecting the centre of the femoral head (C) to the most anterior aspect of the acetabular sourcil margin (A). VCA angle values of 25° or more are normal, whereas 20–25° is borderline and less than 20° abnormal (Fig. 12.15).
11.5 Reproducibility/Variation
Highly reproducible if the radiographic view is technically correct.
11.6 Clinical Relevance/Implications
The false-profile view corresponds to a true lateral view of the hip and allows measurement of the anterior/superior coverage by the acetabulum. This view is able to demonstrate early degenerative changes which commonly tend to begin at the anterior aspect of the joint.
11.7 Analysis/Validation of Reference Data
As indicated previously, values less than 20° correspond to dysplasia. Values between 39° and 44° correspond to a coxa profunda and more than 44° suggest protrusio acetabuli.
11.8 Conclusion
Requires good technique to ensure consistently reliable measurements. The VCA angle measured on the FP view is not identical to the AASA as measured on CT which will be discussed in the next section. The VCA is measured in the sagittal plane demonstrating the anterior/superior coverage by the acetabulum, while the AASA is measured in the horizontal plane demonstrating anterior coverage only.
12 AASA-PASA-HASA
12.1 Definition
The anterior acetabular sector angle (AASA), the posterior acetabular sector angle (PASA) and the horizontal acetabular sector angle (HASA) describe the anterior, posterior and global coverage of the femoral head by the acetabulum.
12.2 Indications
Acetabular dysplasia. Hip dysplasia is usually associated with hypoplasia of the anterior acetabulum and reduced femoral head coverage. Once an acetabular morphological abnormality has been established (abnormal CE angle, etc.) on the AP radiograph, further information concerning acetabular coverage is required. The VCA angle as described above is a radiographic option to provide anterior coverage information using the false-profile view. CT lends itself as a helpful modality to assess the acetabular morphology.
Normal values | AASA | Males | 63 ± 6° |
Females | 64 ± 6° | ||
PASA | Males | 102 ± 8° | |
Females | 105 ± 8° | ||
HASA | Males | 167 ± 11° | |
Females | 169 ± 10° |
12.3 Technique
CT (Fig. 12.16).
12.4 Full Description of Technique
Anda et al. described a standardised CT technique for this purpose. First a scout view of the pelvis is obtained. Then axial scans are obtained through the centre of both femoral heads. An optimal axial section through the centre of the femoral heads should be used for measurements. The anterior coverage is evaluated by the AASA, the posterior coverage by the PASA and the global acetabular coverage by the HASA. The HASA value is the sum of AASA and PASA.
The angles are drawn from a horizontal C-C line through the centre of the femoral heads and two oblique lines from the centre of each of the heads to the most anterior and posterior point of the acetabulum, respectively, of each hip. The mean normal values are 63° in men and 64° in women for the AASA and around 105° for the PASA in both sexes (see normal value range above). These values are decreased in patients with hip dysplasia (Fig. 12.17).
12.5 Reproducibility/Variation
Highly reproducible.
12.6 Clinical Relevance/Implications
Developmental dysplasia results in a decreased acetabular support and this is better appreciated with CT.
12.7 Analysis/Validation of Reference Data
Accepted technique with a well-described standard using reliable fixed points and producing reproducible values.
12.8 Conclusion
A deficiency of the anterior coverage is commonly found in patients with hip dysplasia. Μeasurement of the PASA is important in neuromuscular dysplasia and in cerebral palsy, where a significant number of hips show a severely deficient posterior acetabulum. The PASA is also needed when a Salter osteotomy is planned.
13 M-Z Distance
13.1 Definition
It is the distance in mm between the centre of the acetabulum and the centre of the femoral head.
13.2 Indications
Developmental dysplasia.
13.3 Technique
AP radiography (Fig. 12.18).
13.4 Full Description of Technique
MZ is the distance (in mm) between points M (centre of acetabulum) and Z (centre of femoral head). The critical point for MZ between normal and dysplastic hip joints was found to be 6–8 mm.
13.5 Reproducibility/Variation
In children younger than 5 years of age, it is difficult to define point Z accurately.
Intraobserver and interobserver variations of MZ measurement were reported to be 3.3 and 3.1 mm, respectively, in children and adolescents and 3.8 and 5.7 mm, respectively, in adults.
Poor reproducibility is the result of the difficulty in defining both the inferior border of the acetabulum and the lateral end (lateral rim or lateral border of bony condensation).
13.6 Clinical Relevance/Implications
The MZ distance has been described to evaluate the lack of concentricity between the femoral head and acetabulum, but is not widely used.
13.7 Analysis/Validation of Reference Data
Limited data renders validation difficult
13.8 Conclusion
Easy to perform if landmarks are well delineated.
14 Acetabular Head Index (AHI): Femoral Head Extrusion Index (FHEI)
14.1 Definition
The acetabular head index (AHI) refers to the proportion of the femoral head covered by the acetabulum.
Similarly, the femoral head extrusion index (FHEI) refers to the proportion of the uncovered femoral head.
14.2 Indications
Acetabular dysplasia.
Degree of containment in Perthes disease.
14.3 Technique
AP radiography (Fig. 12.19).
14.4 Full Description of Technique
The hip joint congruence is defined as the % of the femoral head that is covered by the acetabulum. Three vertical lines are required drawn perpendicular to the horizontal C-C line. Line 1 is through the most medial part of the joint space, line 2 passes through the lateral edge of the acetabulum the E point, while line 3 passes as a tangent through the lateral outline of the femoral head. Two horizontal measurements are made between these vertical lines. The horizontal distance A (between lines 1 and 2) is divided by B (the horizontal distance between lines 1 and 3). The ratio A/B is then multiplied by 100 producing the AHI. Normal values of femoral head coverage are above 75%. The smaller the index, the more dysplastic the hip is (Fig. 12.20).
Normal AHI | >75% | Normal FHEI | <25% |
Dysplasia | <75% | Dysplasia | >25% |
The FHEI quantifies similarly the degree of the femoral head uncovered by the acetabulum expressed in percentage. Values of more than 25% are frequent in acetabular dysplasia.
14.5 Reproducibility/Variation
The AHI and FHEI are highly reproducible and not significantly affected by pelvic rotation.
14.6 Clinical Relevance/Implications
This is a useful measurement in the follow-up assessment of the changes with growth in the femoroacetabular relationship. It is particularly suited in Perthes disease, acetabular dysplasia and outcome assessment following corrective surgery.
14.7 Analysis/Validation of Reference Data
CT evaluation to assess congruity can also be performed to study the acetabular coverage. There is no specific CT measurement to assess reliably the femoral head shape/position.
14.8 Conclusion
Both measurements are reliable in producing the required congruency assessment.
15 Acetabular Depth in Coxa Profunda
15.1 Definition
Acetabular morphological abnormality producing a deep-seated acetabulum with generalised over-coverage of the femoral head. It is highlighted on the AP view by the medial location of the floor of the acetabular fossa which touches or medially overlaps the ilioischial line.
15.2 Indications
Hip pain in the young adult could be due to an underlying impingement arising from a focal or generalised acetabular over-coverage. In coxa profunda, the generalised over-coverage is associated with abnormal measurements of previously described angles, namely:
CE angle | >39° |
Acetabular index | 0 or <0 (−value) |
15.3 Technique (Fig. 12.21)
An AP radiograph of the pelvis depicts the altered acetabular morphology.
15.4 Full Description of Technique
The standard radiographic technique described earlier in this chapter to assess acetabular version is required. A supine position with legs internally rotated by 15–20° is employed with the central beam focused midway between the ASIS distance at an FFD of 1.2 m. Pelvic symmetry is essential. It is stressed once again that a focal radiographic view of the hip is contraindicated as it is produces a false assessment of the lines and landmarks. This is a well-described pitfall as a beam centred on the hip instead of the pelvis produces pseudo-coxa profunda features and increases the anteversion of the anterior wall of the acetabulum.
On this pelvic view, normal acetabular relationships are highlighted with the ilioischial line lying medial to the outline of the acetabular fossa. The medial acetabular rim inferiorly is continuous with the teardrop forming its lateral wall.
Both the medial and lateral outlines of the teardrop normally lie lateral to the ilioischial line (Fig. 12.21). The distance between the ilioischial line and the medial acetabular rim is measured where the two lines cross the horizontal C-C line joining the centres of the femoral heads. The distance is designated positive when the ilioischial line is normally located medially and negative when it is abnormally located laterally which is what is seen in coxa profunda (and protrusio acetabuli—see later).
Coxa profunda diagnostic criteria for the distance (negative value) between the medial acetabular rim and the ilioischial line vary in adult men and women:
Men | <−3 mm |
Women | <−6 mm |
The radiographic outline of the femoral head despite its generalised acetabular over-coverage still lies lateral to the ilioischial line (Fig. 12.22).
15.5 Reproducibility/Variation
Accuracy and reproducibility are good but depend on proper radiographic technique and clear measurement landmark instructions. The measurement criteria in children are different with a cut-off of −0.8 mm for boys and −2.7 mm for girls (mean = 2 × SD).
15.6 Clinical Relevance/Implications
Coxa profunda is one of the underlying causes of the acetabular pincer type of femoroacetabular impingement from generalised over-coverage.
15.7 Analysis/Validation of Reference Data
Moderate data supporting validation
15.8 Conclusion
Useful and reliable if based on measurements applied on good radiographic technique.
16 Protrusio Acetabuli Distance
16.1 Definition
Protrusion distance is the measurement of the intrapelvic protrusion of the acetabulum. Protrusio acetabuli is present if on the AP view the medial aspect of the femoral head lies medial to the ilioischial line.
16.2 Indications
Measuring the progression of the protrusio acetabuli observed in association with various disorders. This is associated with underlying hormonal disorders, usually occurs in females, but is often idiopathic and bilateral. Although similar to coxa profunda in causing a generalised acetabular over-coverage and predisposing to the acetabular pincer type of FAI, it is different being progressive and associated with the femoral head outline extending medially to cross the ilioischial line.
16.3 Technique
AP radiography of the pelvis as described previously in the coxa profunda section (Fig. 12.23).
16.4 Full Description of Technique
The essential evaluation exercise and diagnostic criteria are similar to coxa profunda. The ilioischial Kohler line begins on the pelvic border of the ilium and ends on the medial border of the body of the ischium, abutting with the dome of the acetabulum on its way. If the outline of the acetabular dome passes medial to Kohler’s line, a protrusion exists and the magnitude is reflected by the distance between the medial acetabulum and the ilioischial line.
Protrusio is considered to be present if the medial wall of the acetabulum extends medial to the ilioischial line by 3 mm in males or 6 mm in females.
16.5 Reproducibility/Variation
This method is highly reproducible but is applicable to serial radiographs of individual patients and is not suitable for comparing patients.
16.6 Clinical Relevance/Implications
Protrusio acetabuli, also known as arthrokatadysis (Greek words arthro = joint and katadysis = diving), has been defined as a condition in which the head of the femur lies further in the pelvis than normal (Fig. 12.24).
16.7 Analysis/Validation of Reference Data
Reliable indicator of progression of protrusio acetabuli with time as long as the same radiographic technique is used in follow-up radiographs.
16.8 Conclusion
Measurement diagnostic and differentiates it from coxa profunda.
17 Acetabular Depth in Pincer-Type Femoroacetabular Impingement
17.1 Definition
Measurement of the deeply situated femoral head.
17.2 Indications
Patients who demonstrate on plain radiographs acetabular over-coverage (centre-edge angle of greater than 40° or abnormal VCA angle) and/or acetabular retroversion (crossover sign). This applies to coxa profunda and protrusio acetabuli as well.
17.3 Technique
CT.
MRI.
17.4 Full Description of Technique
The acetabular depth should be measured on the axial oblique image obtained from the coronal images, on the image through the centre of the femoral neck. The depth of the acetabulum is defined as the distance between the centre of the femoral head and the line connecting the anterior acetabular rim to the posterior acetabular rim. In pincer-type impingement, the value is negative since the centre of the femoral head lies medial to the line connecting the acetabular rim (Fig. 12.25).
17.5 Reproducibility/Variation
One study showed that in pincer impingement, the acetabular depth is about 5 mm.
17.6 Clinical Relevance/Implications
Femoroacetabular impingement results from an abnormal contact between the femur and the acetabular rim and has been recently recognised as a cause of hip pain in all age groups, possibly resulting in the development of early osteoarthritis. In pure pincer-type impingement, the predominant abnormality is with the morphology of the acetabulum resulting in over-coverage, with a relatively normal contour of the proximal femur. The acetabular over-coverage can be global, as in a patient with protrusio acetabuli, or localised, as in a patient with acetabular retroversion.
17.7 Analysis/Validation of Reference Data
Limited data does not allow satisfactory validation.
17.8 Conclusion
Good indicator of the presence of impingement.
18 Femoral Head Asphericity in Cam-Type Femoroacetabular Impingement: α-Angle/Anterior Offset/AO Ratio Measurements
18.1 Definition
Confirmation and quantification of femoral head asphericity has four possible measurable parameters: the alpha angle, femoral offset or offset ratio and triangular index.
The alpha (α) angle is a parameter used to quantify the degree of femoral deformity and reflects the insufficient anterolateral head-neck offset and femoral head asphericity. It is formed between the femoral neck axis and a line connecting the head centre with the point of commencement of the asphericity of the head/neck contour (Fig. 12.26). The method also evaluates the degree of femoral head-neck offset abnormality allowing the estimation of the offset ratio as well.
The anterior femoral head-neck offset is defined as the difference between the radius of the femoral head (R) and the widest part of the femoral neck anteriorly at its junction with the head (r) (Fig. 12.27). The offset ratio is defined as the ratio between the anterior offset and the diameter of the femoral head.
The triangular index will be dealt separately in the next section.
18.2 Indications
The term “pistol grip” or “tilt” deformity describes a flattened head/neck junction laterally by a bone bump seen on the standard AP radiographs of the hip. The degree of this deformity cannot be assessed optimally on the AP view which usually underestimates it as there is a sagittal component to the abnormality anterosuperiorly, which is not possible to detect/quantify on the AP view. Quantification of the degree of “pistol grip” deformity in the proximal femur suggestive of impingement, assessed previously on AP radiographs, is therefore needed. A lateral radiograph can be used to assess the anatomical relationship between the femoral head and neck anteriorly. MRI is increasingly being used for this purpose as it has a number of advantages.
Normal | <55° |
Abnormal | >55° (cam impingement) |
As discussed later on, the alpha angle threshold signalling, a head-neck deformity may in fact be even lower at about 42°.
18.3 Techniques
Radiography—If radiography is the chosen modality, it is imperative to assess femoral head asphericity on both the AP and lateral radiographs because the head can appear spherical on the AP view but be aspherical on the lateral view.
MRI
18.4 Full Description of Technique (Fig. 12.26)
Radiography. Mose’s concentric circular templates can be used as a quick initial assessment of the femoral head status whereby asphericity is present if the femoral epiphysis is seen to extend beyond the margins of the best-fit reference circle by more than 2 mm. If the femoral epiphysis extends beyond the margins of the reference circle by less than 2 mm, the head is likely to be spherical.
A radiograph can be employed to determine the alpha angle and offset ratio. There are however a number of possible radiographic techniques that can be used. In a comparative study on femoral specimens (11 aspherical heads and 10 spherical heads) using six radiographic projections to assess femoral head/neck asphericity, Meyer et al. found that the measured alpha angle varied with the projections. The Dunn view in 45° or 90° flexion of the hip, neutral rotation and 20° abduction or the crosstable projection in 15° internal rotation were found to be the best projections. These projections minimise the false-negative results. Crosstable lateral radiographs with external rotation in particular should not be used. The problem is that patients with cam impingement have diminished range of hip joint movement especially internal rotation (<20°) as one of the clinical features, which does introduce practical difficulties in obtaining optimally positioned radiographic projections.
The Dunn view can be obtained by flexing the symptomatic hip in 45° or 90° with the patient in the supine position. The hip is abducted by 20°, but there is neutral rotation. With an FFD of 120 cm, the beam is centred midway between the ASIS and symphysis pubis.
The crosstable lateral view requires the patient to lie supine with the contralateral hip and knee flexed beyond 80°. The symptomatic limb is internally rotated by 15°, and the X-ray beam is directed parallel to the tabletop orientated 45° to the symptomatic limb centred on the femoral head.
The frog lateral view is obtained with the patient supine and the affected limb flexed at the knee by 30–40° and the hip abducted by 45°. The heel of the affected limb rests against the medial aspect of the contralateral knee. Using an FFD of 102 cm, the X-ray beam is centred midway between the ASIS and symphysis pubis. Despite initial enthusiasm in some quarters, the frog lateral view is not regarded as a reliable predictor of the alpha angle in FAI.
MRI 1) Oblique angle assessment—The α-angle is measured on 2–3-mm-thick oblique axial gradient-echo, fat-suppressed PD or T1-W MR arthrographic images, planned on the coronal MR images. The oblique axial plane is acquired parallel to the axis of the femoral neck and passing through the centre of the femoral head. This plane, which is individual to the patient and chosen on the basis of the coronal scout view, corresponds to a lateral radiograph with the film cassette parallel to the femoral neck (Figs. 12.26 and 12.28).
MRI 2) Multiple radial assessment—The maximal α-angle value from multiple radial images can be used as an alternative MR method. The radial images are obtained using the centre of the femoral neck as the axis of rotation. Patients with clinically suspected FAI can have an underestimated or missed cam abnormality if only the oblique axial plane is the basis of assessment. In Rakhra et al.’s comparative study, 54% of subjects had an α-angle less than 55° on the conventional oblique axial plane image, but 55° or more on the radial plane images.
A 3D isotropic T1-wt spoiled gradient-echo (MPRAGE/Turbo-Flash) sequence with water excitation (1 mm slice thickness, 25 cm FOV, 256 × 256 matrix) is obtained, from which 2-mm-thick oblique sagittal MPR images are produced perpendicular to the long axis of the femoral neck. Using the latter plane, 2-mm-thick radial MPR images are generated at 15° interval using the centre of the femoral head as the centre of rotation. The generated images are all orthogonal to the head-neck junction. Then a clockface nomenclature is employed designating the anterior-most head-neck junction as the 3 o’clock position, with the 12 o’clock position representing the superior-most junction. Selected radial specific images, four in all, are chosen to evaluate the anterosuperior quadrant of the head-neck junction corresponding to the 12, 1, 2 and 3 o’clock positions (Fig. 12.29).
For the α-angle, a best-fit circle is drawn around the contour of the femoral head. A line is drawn from the centre of the circle outlining the femoral head to the point at which the femoral head or neck protrudes beyond the confines of the circle anteriorly. A second line is constructed along the long axis of the femoral neck starting from the centre of the femoral head extending laterally to the midpoint of the neck at its narrowest point. In the MR radial method, the α-angle value varies with the clockface position, and the maximal angle is recorded. It is worth noting that the radial value at the 3 o’clock position is equivalent to the value obtained from the image through the middle of the femoral neck using the oblique MR image method, and usually in a cam deformity, the radial values are higher at the 2 o’clock vector. An alpha angle greater than 50° is abnormal although using a threshold of 55° may be more specific to cam impingement (Fig. 12.29).
To determine the anterior femoral head-neck offset, the endpoints used in determining the alpha angle are used. Lines are drawn parallel to the longitudinal axis of the femoral neck from both anterior points on the femoral head and femoral neck, respectively (Fig. 12.30). The difference between the perpendicular distances between these lines and the femoral neck axis creates the anterior head-neck offset (Fig. 12.31).
Normal asymptomatic anterior offset | 11.6 ± 0.7 mm |
Cam impingement anterior offset | 7.2 ± 0.7 mm |
The anterior offset ratio can then be calculated between the anterior offset divided by the diameter of the femoral head.
Normal asymptomatic anterior offset | 0.21 ± 0.03 mm |
Cam impingement anterior offset | 0.13 ± 0.0 mm |
18.5 Reproducibility/Variation
The α-angle can be underestimated on the radiographic projection if rotation is not controlled.
Τhe α-angle measured on oblique MR images exhibits a high degree of intra- and interobserver agreement. However, values reporting average alpha angles in patients with FAI are higher in some studies (69.7° and 74.0°) compared with others that have found the abnormal threshold to be 55°. This could reflect the variability in location used to make the measurements.
The oblique axial plane optimally images the anterior contour of the femoral head-neck junction. More specifically however, it has been shown that the most pronounced femoral head offset is seen in the anterosuperior quadrant. For these reasons, there has been a move towards recommending MR radial images to evaluate the head-neck junction over its full circumference as opposed to just anteriorly using the oblique axial image method. Indeed rates of up to 54% false-negative values in FAI have been published when using the popular oblique axial plane protocol. As a result, the multiple radial plane protocol for its measurement was recently introduced as described above.
18.6 Clinical Relevance/Implications
Studies have shown that an elevated α-angle is associated with symptomatic impingement. Cam impingement refers to a “pistol grip” deformity in the contour of the anterior/superior femoral head-neck junction with the acetabulum being normal. Various methods have been described to measure the asphericity of the femoral head as well as the abnormal offset. These include measurement of the α-angle, the epiphyseal extension and the amount of femoral head-neck offset. The α-angle estimation is the easiest to measure and exhibits a high degree of intra- and interobserver agreement.
Impingement by the cam effect from femoral asphericity on the anterior acetabular rim induces cartilage injury predisposing to early osteoarthritis. Stulberg et al. proposed that the “pistol grip” deformity is seen in 40% of hip osteoarthritis.
18.7 Analysis/Validation of Reference Data
The α-angle was originally described as a measurement obtained from the oblique axial MR image through the centre of the femoral head. It is increasingly applied to conventional radiography, but it is not known if applying these definitions across imaging modalities is valid or not. In practice most patients with cam impingement have alpha angles in excess of 63°. Although the crosstable lateral radiograph in 15° internal rotation is the recommended view for assessing the alpha angle and AOR radiographically, there are no robust quantitative definitions of normal and abnormal anatomy based on this projection. Despite this, the measurements from this technique are employed in routine clinical use, and the user needs to be aware that a recent UK study with validation, good repeatability and measurement reproducibility has shown a wider reference interval in normal hips than previously thought. These reference intervals indicate that clinically and radiographically normal hips may have alpha angles and AORs that would be considered abnormal if the threshold value of 55° is employed. The values on normal asymptomatic hips from both genders were combined in Pollard et al.’s study, to derive 95% confidence intervals for the studied population as follows:
Normal values | ||
Alpha angle mean | 6–49° | (95% reference interval 32–62) |
Anterior offset ratio | 0.18–0.20 | (95% reference interval 0.14–0.24) |
Based on but extrapolating from this data of a sample from the general population, patients presenting with symptomatic FAI and an α-angle of 63° or more, or an AOR below 0.14, have proximal femoral anatomy beyond the reference interval.
As the proximal femur has greater offset anteromedially than anterolaterally, the α-angle increases and the AOR decreases with progressive internal rotation. The measurements from the crosstable lateral radiograph in 15° internal rotation have been validated (best reliability/reproducibility) for the purpose of quantifying the morphology and cam deformity of the proximal femur. In Notzli’s article, there was a high degree of intra- and interobserver agreement using the oblique axial MR method. Divergence of observational assessment occurred only in those hips with the largest alpha angles, but these were all clearly placed in the abnormal range. α-angle threshold values for cam deformities are still not fully agreed ranging between 50° and 55°.
Given the elliptical shape of the femoral neck, it is quite obvious that the oblique axial plane images will result in significantly lower α-angle measurements than the radial plane images. Rakhra et al.’s comparative study showed that the radial MR method is more sensitive to the presence, location and size of the anatomic deformity than the oblique axial method which had a false-negative rate of 56%.
For the mean AOR in normal asymptomatic hips, the values are quite consistent in the literature ranging between means of 0.15 and 0.19.
18.8 Conclusion
α-angle measurement is a reliable means of defining femoral head sphericity, is a good predictor for the risk of anterior FAI and is significantly correlated with the extent of cartilage hip defects. α-angle assessment using MRI is a fast and reliable measure to assess femoral asphericity.
19 Femoral Head Asphericity in Cam-Type Femoroacetabular Impingement: Triangular Index
19.1 Definition
The triangular index is a comparative measure between the natural radius of the femoral head (r) and the geometric resultant radius (R) calculated at the neck-head junction.
19.2 Indications
Hip pain in young adult to exclude underlying cam impingement.
19.3 Technique
AP radiograph (Fig. 12.32).
19.4 Full Description of Technique
This measurement technique requires a simple geometric calculation using Pythagoras theorem for right-angled triangles (a2 + b2 = C2). Firstly the centre of the femoral head is located using Mose’s circular templates. Then the longitudinal axis of the femoral neck is identified by connecting the femoral head centre to the midpoint of the narrowest dimensions of the femoral neck. The length of the natural radius of the femoral head (r) is then marked laterally along the constructed longitudinal axis of the femoral neck. Along this line, a point corresponding to the midpoint (i.e. halfway) of the natural radius is marked, and from this point, the perpendicular height (H) to the superior border of the head/neck junction is measured. Using this height (H), the corresponding radius (R) is calculated using Pythagoras theorem for right-angled triangles described above. If the resultant radius (R) at the point 0.5r along the axis of the femoral neck, at the head/neck junction, exceeds the natural radius (r) of the femoral head by 2 mm on a radiograph with 1.2 magnification, then a hump malformation is present indicating the presence of head asphericity.
-
R > r + 2 mm
19.5 Reproducibility/Variation
This method produces a reliable and accurate assessment of femoral head asphericity which can be applied to both AP and lateral radiographs.
19.6 Clinical Relevance/Implications
It provides a simple and accurate description of the bony hump deformity causing the femoral head asphericity. The greater R is at the femoral head/neck junction compared with the natural head radius r, the more severe the hump morphology.
19.7 Analysis/Validation of Reference Data
The triangular index is purely geometric in its calculation and is based on measurements from fixed reference points. It has been found to be more reliable than the radiographic estimation of the α-angle. Probably this is because the exact point at which the radius of the aspherical femoral head deviates from the natural radius and increases laterally on a curved surface is not easy to define accurately.
Importantly the triangular index is not affected by rotation. In a comparative study with α-angle measurements on femoral specimens radiographed at different degrees of rotations, the triangular index result did not change unlike the alpha angle measurement.
19.8 Conclusion
More reliable in assessing the presence and magnitude of femoral head asphericity from conventional radiographs.
20 3D MDCT Quantitative Assessment of Cam Deformity
The angular measurements that are available to detect the cam deformity in femoroacetabular impingement currently focus on defining a contour abnormality of the femoral head. These techniques do not provide a quantifiable estimate of the deformity (extent, height and spatial orientation/location) which is increasingly becoming relevant as a preoperative map for minimally invasive surgical techniques.
Harnessing 3D volumetric-based multidetector CT technology to acquire the 3D dataset holds great promise in quantifying the bony abnormality accurately. In a large study on 102 dry cadaveric femora, this technique identified 49 instances of a bony prominence at the head-neck junction anterolaterally. The capabilities of this method are reflected in the average measured values which were:
Average surface area | 326 mm2 (SD 172 mm2) |
Average height | 3.23 mm (SD 0.74 mm) |
Computed alpha angle of normal femora | 47.65° (38.67–59.81) |
Computed alpha angle of cam-type femora | 67.72° (53.04–88.02) |
In addition using this method, the 3D alpha angle can be calculated using the MR methods described previously. Limited studies have shown that when acquired accurately using 3D through automated computational analysis, the alpha angle correlates significantly with the 3D MDCT morphological detection method. Importantly there is also an acceptable correlation between the computed alpha angle and the multiple radial plane estimation but not the oblique axial plane estimation of the alpha angle. The technique has had to date only limited exploration in vivo and in vitro, but due to its potential, it is briefly included.
The rate of insufficient alpha angle corrections after corrective arthroscopic osteochondroplasty surgery in impingement patients is still in the order of 24%. This is despite using CT-based navigational systems which have an inherent accuracy of less than 1 mm. The CT-based protocol used in previous studies had major weaknesses which included the inability to display the amount of bone which needed to be resected. Without this information, it is not possible despite a very accurate navigational system to improve surgical accuracy and outcomes.
21 Femoroacetabular Impingement: Beta Angle
21.1 Definition
The (β) angle measures the angle between the head-neck junction and the acetabular rim with the hip in 90° flexion. It is useful in patients with FAI irrespective of the underlying FAI type.
21.2 Indication
FAI independent of aetiology. The increased α-angle (>55°) gives information about the severity of the femoral head-neck pathology, while the increased centre-edge angle (>40°) describes acetabular over-coverage, but neither are able to quantify the status during the impingement process.
21.3 Technique (Fig. 12.33)
The β-angle is an additional technique allowing measurement of the distance between the femoral head-neck junction and the acetabular rim with the hip in a position promoting impingement. This assessment can be measured on images produced by a special radiographic technique or positioning in an open MR scanner.
Radiography. Beta view radiographs are obtained with the patient sitting in a chair, with the hip in 90° flexion and the femur in 20° abduction and 0° rotation. The femur needs to be horizontal, and this is checked by ensuring that the plane between the greater trochanter and lateral condyle is parallel to the ground. The beam is angled 15° in the AP direction rendering it tangential to the acetabular plane. It is centred on the femoral shaft about 6 cm lateral to the ASIS using 84 kV. On the resulting radiograph, the head-neck junction lies superiorly, with the femoral neck perpendicular to the acetabular plane.
MRI. An open MRI system is required for a positional study to show the space between the anterior femoral neck and the acetabular rim with the hip in 90° flexion. When the hip is in 90° flexion, the anterior femoral neck faces cephalad. The MRI plane needs to be in the orientation that allows measurement of the minimum space between the neck and rim at the site of potential FAI. As this space can be measured as an angle in the plane of motion, it is comparable with the clinically measured internal rotation. The patient is placed supine, and with the help of a support, the hip is placed in 90° of flexion and in neutral rotation in the sagittal plane before a flexible radiofrequency coil is positioned around the hip.
A coronal scout view passing through the centre of the hip is used with the hip in 90° flexion to determine the plane of acetabular anteversion. Then anteroposterior sections through the acetabulum are obtained tilted 90° to the acetabular opening. On this basis, 4-mm-thick sections are obtained. Using this technique, Wyss et al. found that the available space between the rim and femoral neck was consistently smallest in the section 4 mm anterior to the hip centre. The neck-rim relationship is then measured from this scan.
Using the MR image, the anterior limit of head congruency can be defined as the point where the distance from the centre of the head first exceeds the true radius of the cartilage-covered head. The lateral bony margin of the acetabulum is then identified, and lines are drawn from the centre of the femoral head to the previously identified points. The angle formed by these lines is called the beta angle. It represents the arc of congruent internal rotation available with the hip in 90° flexion.
Normal asymptomatic individuals | 30 ± 9° |
FAI patients | 5 ± 9° |
21.4 Full Description of Technique
To measure the β-angle from the obtained radiograph, the method is similar to the one described above on the MR image. Briefly three points are defined: firstly the centre of the femoral head, secondly the point representing the anterior limit of head-neck congruency from where the distance from the bone to the head centre first exceeds the radius of the femoral head and thirdly the point which is at the superolateral rim of the acetabulum. The β-angle is subtended by the lines from the head centre to these points, respectively (Fig. 12.33).
Normal beta angle | 38.7° (95% confidence interval 36.5–41.0) |
FAI beta angle | 15.6° (95% confidence interval 13.3–17.7) |
21.5 Reproducibility/Variation
There are no significant differences in the measured β-angle values between men and women in either normal or FAI patients.
Excellent inter- and intraobserver correlation with a high reliability and reproducibility in both normal and FAI patients. This is seen using both radiographic and MRI techniques.
21.6 Clinical Relevance/Implication
A radiographically measured beta angle >30° is normal and in keeping with symptomatic FAI if <29°.
Using both radiographic and MRI-based measurements, the β-angle when compared with clinical examination showed significant correlation with range of internal rotation but not degree of flexion.
The β-angle can also be used postoperatively, and studies have shown improvement in the measurements following arthroscopic osteochondroplasty of the head-neck junction. This also correlated with clinical improvement of internal rotation.
21.7 Analysis/Validation of Reference Data
The mean β-angle in FAI measured radiographically is 15.6° compared with a mean β-angle measurement on MRI of 4°. This could be due to the inclusion of cartilaginous components of the bony bump visualised by MR not seen radiographically. However, it is also possible that it is not always possible to extrapolate measurements done using two different imaging techniques.
21.8 Conclusion
As the measurement is done with the hip at 90° flexion, any deformity impinging on joint motion is assessed whether it originates from the femoral, acetabular or both sides of the hip joint. It also shows that the physical examination with specific reference to internal rotation is reliable in indicating the presence of FAI. It provides additional objective dynamic dimension in FAI patients both preoperatively and postoperatively.
22 Femoral Anteversion and McKibbin Instability Index
22.1 Definition
Femoral anteversion is the angle between the transverse axis of the knee joint and the transverse axis of the femoral neck.
22.2 Indications
Diagnosis and selection of patients for derotational osteotomies.
22.3 Techniques
CT.
MRI.
The subject is covered further in the chapter on Long Bone Measurements.
22.4 Full Description of Technique
Femoral anteversion is the angle between the transverse axis of the knee joint, which is best indicated by a line drawn tangential to the maximum posterior convexity of both femoral condyles, and the transverse axis of the femoral neck. The latter line is drawn through the centre of the femoral head and along the central axis of the femoral neck.
Τhe transverse axis of the knee joint has been a topic for discussion. Instead of the posterior tangential line, some propose the transcondylar axis. The latter is determined by first drawing tangents to the anterior and posterior aspects of the femoral condyles, and then a line drawn bisecting the angle between the two lines represents the transcondylar axis.
The diacondylar plane proposed by others connects two points at the widest flare of the condyles.
Since the femoral neck cannot be visualised in the transverse plane because of its anterior and cephalad orientation, images made at different levels can be superimposed to create a summation image (Fig. 12.34).
Alternatively, the angles of the femoral neck and femoral condyles formed with respect to the transverse plane are subtracted. However, if the femoral condyles are internally rotated on the images, the angle of rotation must be added to the angle of anteversion.
Normal values | 15–20° |
Dysplasia | >20° |
22.5 Reproducibility/Variation
Highly reproducible in adults.
Clinical Relevance/Implications
Precise measurement of femoral anteversion is important in the selection of patients for preoperative planning of derotational osteotomy of the femur.
The McKibbin instability index is based on the assumption that the effects of femoral and acetabular anteversion may be additive or may offset each other. The McKibbin instability index is calculated as the sum of the angles of femoral and acetabular anteversion, with an index of 60 denoting severe instability. The normal range for the McKibbin instability index is 30–40°. Abnormal values are associated with hip pain and osteoarthritis.
Normal McKibbin index | 30–40° |
Abnormal McKibbin index | >40° |
22.6 Analysis/Validation of Reference Data
Decreased femoral anteversion is seen in association with slipped capital femoral epiphysis, coxa vara, deep acetabulum, dysplasia of the hip and pistol grip deformity, after derotational varus osteotomy in children (when the femoral anteversion, which has been reduced to 0°, does not remodel), and in patients with previous fractures of the femoral shaft. Increased femoral anteversion is seen in developmental dysplasia of the hip, Legg-Calve-Perthes disease, intoeing gait and cerebral palsy.
The measurement on a single image of the proximal neck has been reported to underestimate anteversion by about 10° in normal patients. This error is greater for images through the proximal part and less for images that were taken in the distal part of the femoral neck. This inaccuracy may be explained by the fact that a single section through the femoral neck often fails to indicate the direction of the axis of the femoral neck. The most proximal portion of the inferior neck with no head portion on the CT axial slice provides the most accurate estimate of the neck axis.
22.7 Conclusion
It is unclear whether isolated anteversion of the femur can be considered a form of hip dysplasia. Even though increased anteversion is commonly found in hip dysplasia, no relationship has been established with the acetabular development.
23 Femoral Neck Shaft Angle (NSA) or Centrum-Collum-Diaphyseal (CCD) Angle of Muller
23.1 Definition
The NSA is the angle formed by lines drawn along the long axis of the femoral shaft and along the axis of the femoral neck passing through the centre of the femoral head. It is also known as centrum-collum-diaphyseal (CCD) angle of Muller.
23.2 Indications
Along with the angle of femoral anteversion, the NSA is required prior to surgery for correcting the dysplastic hip. A coxa valga deformity is the usual abnormality in hip dysplasia patients. Further indications include detection and preoperative planning of femoral fractures and developmental coxa vara.
23.3 Technique (Fig. 12.35)
AP radiography. The appearance of the femoral neck radiographically is significantly affected by femoral anteversion. To counteract this, the NSA is most accurately measured with the legs in 20° internal rotation which is the standard in obtaining this radiograph.
23.4 Full Description of Technique
The patient is placed flat on the back with the feet pointing medially. The central ray passes through a point 1 in. below the centre of the inguinal ligament perpendicular to the plane of the film. An angle is formed by the long axes of the femoral shaft and neck (see below).
The most reliable method of constructing the respective femoral shaft and femoral neck axis needs to be employed (Fig. 12.35). Firstly the femoral shaft axis is determined by joining two points obtained by bisecting two transverse diameters of the proximal subtrochanteric femoral diaphysis. Secondly the centre of the femoral neck is determined. To do this, a circle is first drawn around the femoral head outline and the centre of the femoral head is located. This circular arc intersects the femoral neck at two points on the superior and inferior femoral neck outlines, respectively. A line is then drawn joining these two points, and a bisector is created to this line. The line joining this line’s midpoint to the centre of the femoral head is the femoral neck. (Please refer to the Paediatric section for diagram details.)
Normal values | 125–135° |
Abnormal values | Coxa vara, <125° |
Coxa valga, >140° |
23.5 Reproducibility/Variation
Highly reproducible if applied after the age of 6.
23.6 Clinical Relevance/Implications
Apart from surgical planning, the study of NSA is important to study osteoarthritis in an individual patient. In addition, the use of a combination of femoral BMD and NSA may improve hip fracture risk prediction as the latter is significantly higher in patients with hip fractures.
23.7 Analysis/Validation of Reference Data
Using this radiographic method, the NSA measurement is a close approximation of the true NSA. The measurement is significantly affected by femoral neck anteversion, and attention to the correct interpretation of the measurements is vital prior to surgical planning. If corrective surgery is being planned, an exact value must be obtained using charts (not included) taking into account the degree of femoral anteversion.
In congenital coxa vara, the medial contour of the femoral neck is often deficient. Alternatively the inferior point of femoral neck intersection with the circular arc is replaced by obtaining a point where a perpendicular to the femoral shaft axis intersects the highest point on the inferomedial outline of the femoral neck to define the centre of the femoral neck.
23.8 Conclusion
As femoral anteversion significantly affects the radiographic projection of the neck shaft angle, accurate positioning is a mandatory prerequisite. Both angles are required prior to carrying out any planning for corrective surgery.
24 Stem Anteversion
24.1 Definition
This is the angle between the transverse axis of the stem and the transverse axis of the knee joint.
24.2 Indications
To assess postoperatively the stem anteversion in patients with total hip replacements and hip pain.
24.3 Technique (Fig. 12.36)
CT
24.4 Full Description of Technique
The femoral stem axis is defined as the line along the anterior and posterior borders of the implant. The stem anteversion is evaluated as an angle between the posterior condylar axis and the axis of the femoral stem at the most proximal portion of the inferior neck with no head portion included in the image.
24.5 Reproducibility/Variation
Highly reproducible.
24.6 Clinical Relevance/Implications
An excess or deficit in the value of stem anteversion may influence the range of motion because of impingement effects and may be the cause of loosening.
24.7 Analysis/Validation of Reference Data
The surgeon’s intraoperative intention using visual assessment in placing the stem in an anteversion of 10–20° is imprecise especially in the cementless femoral stem.
24.8 Conclusion
This measurement often indicates that the stem is often not within the intended range of anteversion.
25 Femoral Head: Index of Necrotic Extent
25.1 Definition
The measurement of the extent of the avascular necrotic process in the femoral head.
25.2 Indications
Quantification of avascular necrosis of the femoral head.
25.3 Techniques
MRI.
25.4 Full Description of Technique
A is the necrotic arc angle in the coronal plane, and B is the necrotic arc angle in the sagittal plane. The index of necrotic extent ([A/180] × [B/180]) × 100 is derived from the size of subchondral involvement at the midcoronal and midsagittal planes, and the modified index of necrotic extent is derived from the maximum size of subchondral involvement in both planes (Fig. 12.37).
25.5 Reproducibility/Variation
Highly reproducible.
25.6 Clinical Relevance/Implications
The size of the necrotic lesion is important in determining whether a subchondral fracture will occur.
25.7 Analysis/Validation of Reference Data
There are numerous methods for quantifying the extent of osteonecrosis of the femoral head, some quite complicated requiring advanced software analysis.
25.8 Conclusion
There is no consensus regarding which method is the most reliable.
26 Pelvic Instability: Symphysis Pubis Excursion on Flamingo Radiographs
26.1 Definition
Translation of the symphysis pubis is the total excursion measured at the symphysis pubis on alternating single-leg-stance radiographs.
26.2 Indications
Pelvic pain due to instability from anatomical, hormonal, biomechanical, metabolic and endocrine causes.
26.3 Technique
AP radiography of the pelvis to assess symphysis pubis (Fig. 12.38).
26.4 Full Description of Technique
Three AP radiographs are required at an FFD of 0.6 m with the patient standing: dual stance, single-leg-stance on the right and single-leg-stance on the left. The dual stance film acts as the control. In every case, the high pubic ramus changed from right to left coinciding with the change of stance leg.
A vertical reference line is drawn to pass through the spinous process of L4 and L5 and the tip of the coccyx. Two lines are then drawn perpendicular to this line to the most superior aspect of the pubic symphysis on the right and left. The distance between these lines is equal to the translation, and the degree of motion can be compared with the baseline dual-leg-stance film. The sum of the translation from baseline is then added to give a total translation in centimetre. Under normal conditions, there is a difference in the magnitude of the translation between men and women and nulliparous and multiparous women.
Normal Physiological Translation of Mean Translation at Symphysis Pubis in mm + SD
Men | 1.4 ± 1.0 mm | Women | |
Nulliparous | 1.6 ± 0.8 mm | ||
Multiparous | 3.1 ± 1.5 mm | ||
The increased normal translation in multiparous women is also directly proportional to the number of pregnancies.
Abnormal translation in keeping with pelvic instability is defined as >0.5 cm of change in alignment between the views.
26.5 Reproducibility/Variation
There is excellent interobserver correlation highlighting the repeatability of this method of measurement.
26.6 Clinical Relevance/Implications
During single-leg-stance, strong shearing forces act on the symphysis pubis in two opposite vertical directions simultaneously and create the shift seen in pelvic relaxation. The diagnosis of pelvic instability is made on the basis of the difference in the heights of the symphyseal bodies on the two AP single-leg-stance radiographs. The measurements are made from the top of the symphyseal bodies with respect to the perpendicular plumbline from the sacrum. The vertical difference in height between the two points is measured in centimetre, and the values from both radiographs are added together to provide a total translation value.
26.7 Analysis/Validation of Reference Data
Previously Chamberlain had concluded that the upper limit of normal physiological range is 2 mm.
26.8 Conclusion
Normally up to 0.5 cm of physiological motion can take place at the symphysis pubis in asymptomatic individuals as seen on alternating single-leg-stance AP radiographs.
27 MRI Pelvimetry
27.1 Definition
Pelvimetry is the evaluation of the relative sizes of the fetal head (Fig. 12.39) and the maternal pelvis.
A positive cephalopelvic disproportion index is present if the narrowest pelvic diameter (either the sagittal diameter of the inlet or the transverse diameter of the midpelvis) is less than 9 mm wider than the fetal biparietal diameter.
27.2 Indications
To select women with potential difficulties in vaginal delivery.
27.3 Technique
MRI.
27.4 Full Description of Technique
MRI pelvimetry has replaced radiographic and CT pelvimetry due to the ability for multiplanar imaging and the lack of ionising radiation. MRI pelvimetry is applied on midsagittal, transverse and oblique sections of the pelvis.
Axial Image
Interspinous (bispinous, midpelvic) diameter: This is the most important measurement as it is usually the narrowest point of the midpelvis, where obstructive labour most often occurs. The measurement is made at the level where the ischial spines are best visualised. This level is usually within 1–2 cm of the femoral head fovea (Fig. 12.40).
Intertuberous diameter: This is the widest distance between the ischial tuberosities (Fig. 12.41).
Midsagittal Image
Anterior-posterior inlet diameter (obstetric conjugate): This measurement is the distance from the posterior-superior aspect of the pubic symphysis to the most anterior aspect of the first sacral vertebral body (sacral promontory).
Sagittal outlet: This is the distance from the bottom of the inner cortex of the symphysis to the end of the sacrum (Fig. 12.42).
Oblique Coronal Image
The oblique section is performed in a plane through the superior pubic symphysis and the promontorium. The transverse inlet diameter is the largest transverse distance of the pelvis. A line is drawn through the widest area of the pelvis between the arcuate lines of the iliac bones (Fig. 12.43).
27.5 Reproducibility/Variation
The intertuberous diameter is the most difficult to define. Moderate difficulty in definition demonstrates the sagittal outlet. All other parameters are highly reproducible.
27.6 Clinical Relevance/Implications
A small maternal pelvis is a contraindication for vaginal delivery of a fetus in breech presentation because of the potential difficulty in delivering the fetal head.
A pelvis too small for safe vaginal delivery has been defined as one measuring less than 12 cm in the widest transverse inlet diameter, 11 cm in the anterior-posterior inlet diameter or 10 cm in the interspinous diameter.
27.7 Analysis/Validation of Reference Data
While most investigators agree that pelvimetry will not alter the conduct of labour in a vertex presentation, it may reveal small-sized pelvis in breech presentation which if associated with hyperextension of the fetal head may result in increased risk of cervical cord damage and is an indication for caesarean section. MRI implies no radiation but does not show a significant improvement over previously described pelvimetric techniques.
27.8 Conclusion
MRI is the modality of choice for assessing the maternal pelvis.
28 Ischiofemoral Space: Quadratus Femoris Space
28.1 Definition
The ischiofemoral space (IFs) lies between the ischial tuberosity and the lesser trochanter.
The quadratus femoris space (QFs) contains the quadratus femoris muscle (QFm), and it lies between the hamstring tendons and the lesser trochanter.
28.2 Indications
The abnormally narrowed IFs and QFs are related to the ischiofemoral impingement syndrome (IFIs) which is clinically demonstrated with hip pain. The QFm shows on MRI abnormal morphology and/or signal intensity.
28.3 Techniques
CT/MRI.
Axial images.
Axial T1-wt images.
28.4 Full Description of Technique
The following spaces should be assessed on thin section axial images whether with CT or MRI. MRI should be performed with high-field scanners (1.5–3.0 T) and a phased array coil.
Ischiofemoral space (IFs): The smallest distance between the lateral cortex of the ischial tuberosity and the medial cortex of the lesser trochanter.
Quadratus femoris space (QFs): The smallest space for passage of the quadratus femoris muscle (QFm) bordered by the superolateral surface of the hamstring tendons and the posteromedial surface of the iliopsoas tendon or lesser trochanter (Fig. 12.44). Axial T1-W MR images are the preferred ones for measurements (Fig. 12.45).
Reproducibility/Variation
No currently available data exist on the reproducibility of the above measurements.
In one cadaveric study, the mean IFs was 23.5 ± 4.7 mm and the mean QFs 20.4 ± 5.6 mm. In the same study, 52% of the hips showed abnormalities within the QF muscle.
In a MRI study, the IFs was found 23 ± 8 mm in controls vs 13 ± 5 mm in patients. The QFs was, respectively, found 12 ± 4 mm vs 7 ± 3 mm (lower leg in internal rotation).
In another MRI study of symptomatic patients examined with the lower leg in neutral position, IFs was found 12.9 mm and the QFs 6.7 mm on the average.
28.5 Clinical Relevance/Implications
Patients with IFIs present with chronic pain in the groin or buttock. The pain may radiate to the lower extremity due to the proximity of the QFm to the sciatic nerve. The symptomatic patients with narrowed IFs and QFs show on MRI oedema, partial tear and fatty infiltration of the QFm and oedema and partial tears of the hamstring tendons. CT scanning can show the narrowed space but is not capable of depicting the QFm abnormalities.
Normal IFs | >20 mm |
Abnormal IFs | <20 mm |
References
Abitbol MM, Taylor UB, Castillo I, Rochelson BL (1991) The cephalopelvic disproportion index: combined fetal sonography and x-ray pelvimetry for early detection of cephalopelvic disproportion. J Reprod Med 36:369–373
Anda S, Terjesen T, Kvistad KA, Svenningsen S (1991a) Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comput Assist Tomogr 15:115–120
Anda S, Terjesen T, Kvistad KA (1991b) Computed tomography measurements of th acetabulum in adult dysplastic hips: which level is appropriate? Skeletal Radiol 20(4):267–271
Armbuster RG, Guerra J, Resnick D, Goergen TG, Feingold ML, Niwayama G, Danzig L (1978) The adult hip: an anatomic study, part 1: the bony landmarks. Radiology 128:1–10
Audenaert E, Baelde N, Huysse W, Vigneron L, Pattyn C (2011) Development of a three-dimensional detection method of cam deformities in femoroacetabular impingement. Skeletal Radiol 40:921–927
Beaule PE, Zaragoza E, Motamedi K, Copelan N, Dorey FJ (2005) Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res 23(6):1286–1292
Boniforti FG, Fujii G, Anfliss RD, Benson MKD (1997) The reliability of measurements of pelvic radiographs in infants. J Bone Joint Surg Br 79-B:570–575
BruckI R, Hepp WR, Tonnis D (1974) Eine abgrenzung normaler und dysplastischerjugendlicher huftgelenke durch den huftwert. Arch Orthop Unfallchir 74:13–32
Brunner A, Hamers AT, Fitze M, Herzog RF (2010) The plain Beta-angle measured on radiographs in the assessment of femoroacetabular impingement. J Bone Joint Surg Br 92-B:1203–1208
Buckley SL, Sponseller PD, Magid D (1991) The acetabulum in congenital and neuromuscular hip instability. J Pediatr Orthop 11:498–501
Busse J, Gasteiger W, Tonnis D (1972) A new method for roentgenologic evaluation of the hip joint-the hip factor. Arch Orthop Unfallchir 72:1–9
Cherian SF, Laorr A, Saleh KJ, Kuskowski MA, Bailey RF, Cheng EY (2003) Quantifying the extent of femoral head involvement in osteonecrosis. J Bone Joint Surg Am 85:309–315
Cibere J (2006) Do we need radiographs to diagnose osteoarthritis? Best Pract Res Clin Rheumatol 20:27–38
Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB (2008) A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am 90(Suppl 4):47–66
Cooperman DR, Wallensten R, Stulberg SD (1983) Acetabular dysplasia in the adult. Clin Orthop 175:79–85
Dandachli W, Islam SU, Liu M, Richards R, Hall-Craggs M, Witt J (2009) J Bone Joint Surg Br 91(8):1031–1036
Dandachli W, Islam SU, Tippett R, Hall-Craggs M, Witt J (2011) Analysis of acetabular version in the native hip: comparison between 2D axial and 3D CT measurements. Skeletal Radiol 40:877–883
Delaunay S, Dussault RG, Kaplan PA, Alford BA (1997) Radiographic measurements of dysplastic adult hips. Skeletal Radiol 26:75–81
Dorr LD, Wan Z, Malik A, Zhu J, Dastane M, Deshmane P (2009) A comparison of surgeon estimation and computed tomographic measurement of femoral component anteversion in cementless total hip arthroplasty. J Bone Joint Surg 91:2598–2604
Eijer H, Leunig M, Mahomed MN, Ganz R (2001) Crosstable lateral radiograph for screening of anterior femoral head-neck offset in patients with femoro-acetabular impingement. Hip Int 11:37–41
Eyring EJ, Bjornson DR, Peterson CA (1965) Early diagnostic and prognostic signs in Legg-Calve-Perthes disease. Am J Roentgenol 93:382–387
Ezoe M, Naito M, Inoue T (2006) The Prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am 88:372–379
Fowkes LA, Petridou E, Zagorski C, Karuppiah A, Toms AP (2011) Defining a reference range of acetabular inclination and centre-edge angle of the hip in asymptomatic individuals. Skeletal Radiol 40:1427–1434
Fredensborg N (1976) The CE angle of normal hips. Acta Orthop Scand 47:403–405
Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA (2003) Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop 417:112–120
Garras DN, Carothers JJ, Olson SA (2008) Single-leg-stance (Flamingo) radiographs to assess pelvic instability. How much motion is normal? J Bone Joint Surg Am 90:2114–2118
Gimovsky ML, Willard K, Neglio M, Howard T, Zeme S (1985) X-ray pelvimetry in a breech protocol: a comparison of digital radiography and conventional methods. Am J Obstet Gynecol 153:887–888
Giori NJ, Trousdale RT (2003) Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res 417:263–269
Gnudi S, Ripamonti C, Gualtieri G, Manavolta N (1999) Geometry of proximal fêmur in the prediction of hip fracture in osteoporotic women. Br J Radiol 72:729–733
Gosvig KK, Jacobsen S, Palm H, Sonne-Holm S, Magnusson E (2007) A new radiological index for assessing asphericity of the femoral head in Cam Impingement. J Bone Joint Surg 89-B:1309–1316
Gusis SE, Babini JC, Garay SM, García Morteo O, Maldonado Cocco JA (1990) Evaluation of the measurement methods for protrusio acetabuli in normal children. Skeletal Radiol 19(4):279–282
Herrlin K, Pettersson H, Selvik G, Lidgren L (1988) Femoral anteversion and restricted range of motion in total hip prostheses. Acta Radiol 29:551–553
Heyman CH, Herndon CH (1950) Legg-Perthes Disease: a method for the assessment of the roentgenographic result. J Bone Joint Surg Am 32A:767–778
Hoiseth A, Reikeras O, Fonstelien E (1989) Lack of correlation between femoral neck anteversion and acetabular orientation. Acta Orthop Scand 60:93–96
Hubbard MJS (1969) The measurement of progression in protrusion acetabuli. Am J Roentgenol 106:506–508
Idelberger K, Frank A (1952) Uber eine neue methode zur bestimmung des pfannendachwinkels bei jugendlichen und erwachsenen. Z Orthop 82:571578
Ito K, Minka MA 2nd, Leunig M, Werlen S, Ganz R (2001) Femoroacetabular impingement and the cam-effect: an MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br 83:171–176
Keller TM, Rake A, Michel SC, Seifert B, Efe G, Treiber K, Huch R, Marincek B, Kubik-Huch RA (2003) Obstetric MR pelvimetry: reference values and evaluation of inter- and intraobserver error and intraindividual variability. Radiology 227:37–43
Kim YM, Ahn JH, Kang HS, Kim HJ (1998) Estimation of the extent of osteonecrosis of the femoral head using MRI. J Bone Joint Surg Br 80:954–958
Kim SS, Frick SL, Wenger DR (1999) Anteversion of the acetabulum in developmental dysplasia of the hip: analysis with computed tomography. J Pediatr Orthop 19(4):438–442
Kleemann RU, Heller MO, Stoeckle U, Taylor WR, Duda GN (2003) THA loading arising from increased femoral anteversion and offset may lead to critical cement stresses. J Orthop Res 21:767–774
Konan S, Rayan F, Haddad FS (2010) Is the frog lateral plain radiograph a reliable predictor of the alpha angle on femoroacetabular impingement? J Bone Joint Surg Br 92-B:47–50
Koo K-H, Kim R (1995) Quantifying the extent of osteonecrosis of the femoral head. A new method using MRI. J Bone Joint Surg Br 77:875–880
Lequesne M (1963a) Mesure des angles fondamentaux de la hanche radiographique de l’adulte par un rapporteur combine. Rev Rheum 30:479–485
Lequesne M (1963b) Coxometrie. Mesure des angles fondamentaux de la hanche radiographique de l’adulte par un rapporteur combiné. Rev Rhum 30:479–485
Lequesne M, deSeze S (1961) Le faux profil du bassin: Nouvelle incidence radiographique pour l’edude de la hanche: Son utilite dans les dysplasies et les differentes coxpathies. Rev Rhum Mal Osteoartic 28:643–652
Lequesne M, Laredo JD (1998) The faux profil (oblique view) of the hip in the standing position. Contribution to the evaluation of osteoarthritis of the adult hip. Ann Rhum Dis 57:676–681
Lequesne M, Lemoine A, Massare C (1964) Le “complet” radiographique coxofemoral. Depistage et bilan préopératoire des vices architecturaux de la hanche. J Radiol Electrol 1(2):27–44
Lequesne M, Malghem J, Dion E (2004) The normal hip joint space: variations in width, shape, and architecture on 223 pelvic radiographs. Ann Rheum Dis 63:1145–1151
McBride MT, Muldoon MP, Santore RF, Trousdale RT, Wegner DR (2001) Protrusio acetabuli: diagnosis and treatment. J Am Acad Orthop Surg 9:79–88
Meyer DC, Beck M, Ellis T, Ganz R, Leunig M (2006) Comparison of six radiographic projections to assess head/neck asphericity. Clin Othop Rel Res 445:181–185
Moore RJ, Fazzalari NL, Manthey BA, Vernon-Roberts B (1994) The relationship between head-neck-shaft angle, calcar width, articular cartilage thickness and bone volume in arthrosis of the hip. Br J Rheumatol 33:432–436
Murphy SB, Kijewski PK, Wilkinson RH, Griscom NT (1987) Femoral anteversion. J Bone Joint Surg Am 69:1169–1176
Murphy S, Ganz R, Muller M (1995) The prognosis of untreated dysplasia of the hip. J Bone Joint Surg 77-A:986–989
Murray RO (1965) The aetiology of primary osteoarthritis of the hip. Br J Radiol 38:810–824
Nelitz M, Guenther KP, Gunkel S, Puhl W (1999) Reliability of radiological measurements in the assessment of hip dysplasia in adults. Br J Radiol 72:331–334
Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J (2002) The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 84:556–560
Ogata S, Moriya H, Tsuchiya K, Akita T, Kamegaya M, Someya M (1990) Acetabular cover in congenital dislocation of the hip. J Bone Joint Surg Br 72:190–196
Omeroglu H, Bicimoglu A, Agus H, Tumer Y (2002) Measurement of center-edge angle in developmental dysplasia of the hip: a comparison of two methods in patients under 20 years of age. Skeletal Radiol 31:25–29
Ozcelik A, Omeroglu H (2003) Two alternative methods for the measurement of MZ distance on a hip radiograph. Arc Orthop Trauma Surg 123:215–218
Pessis E, Chevrot A, Drape JL, Leveque C, Sarazin L, Minoui A, Le Blevec G, Chemla N, Dupont AM, Godefroy D (1999) Study of the joint space of the hip on supine and weight-bearing digital radiographs. Clin Rad 54:528–532
Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J (2006) Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology 240:778–785
Philippon MJ, Briggs KK, Yen YN, Kuppersmith DA (2009) Outcomes for hip arthroscopy for femoroacetabular impingement associated with chondrolabral dysfunction: minimum two year follow-up. J Bone Joint Surg Br 91:16–23
Pollard TCB, Villar RN, Norton MR, Fern ED, Williams MR, Simpson DJ, Murray DW, Carr AJ (2010) Femoroacetabular impingement and classification of the cam deformity: the reference interval in normal hips. Acta Orthop 81(1):134–141
Rakhra KS, Sheikh AM, Allen D, Beale PE (2009) Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Rel Res 467(3):660–665
Reynolds D, Lucas J, Klaue K (1999) Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br 81:281–288
Ruby L, Mital MA, O’Connor J, Patel U (1979) Anteversion of the femoral neck: comparison of methods of measurement in patients. J Bone Joint Surg Am 61:46–51
Ryder CT, Crane L (1953) Measuring femoral anteversion: the problem and a method. Bone Joint Surg Am 35:321–328
Siebenrock KA, Kalbermatten DF, Ganz R (2003) Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res 407:241–248
Siebenrock KA, Wahab KH, Werlen S, Kalhor M, Leunig M, Ganz R (2004) Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop 418:54–60
Siegel J, Templeman DC, Tornetta P III (2008) Single-leg-stance radiograph in the diagnosis of pelvic instability. J Bone Joint Surg Am 90:2119–2125
Stark DD, McCarthy SM, Filly RA, Parer JT, Hricak H, Callen PW (1985) Pelvimetry by magnetic resonance imaging. Am J Roentgenol 144:947–950
Steinberg ME, Bands RE, Parry S, Hoffman E, Chan T, Hartman KM (1999) Does lesion size affect the outcome in avascular necrosis? Clin Orthop 367:262–271
Stulberg SD, Cordell LD, Harris WH, Ramsey PL, MacEwen GD (1975) Unrecognised childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: The hip. Proc of the third meeting of the Hip Society. CV Mosby Co., St Louis, pp 212–228
Sugano N, Noble PC, Kamaric E (1998) A Comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr 22:610–614
Suh KT, Kang JH, Roh HL, Moon KP, Kim HJ (2006) True femoral anteversion during primary total hip arthroplasty: use of postoperative computed tomography-based sections. J Arthroplasty 21:599–605
Sussman WI, Han E, Schuenke MD (2013) Quantitative assessment of the ischiofemoral space and evidence of degenerative changes in the quadratus femoris muscle. Surg Radiol Anat 35:273–281
Sweeney JP, Helms CA, Minagi H, Louie KW (1987) The widened teardrop distance: a plain film indicator of hip joint effusion in adults. Am J Roentgenol 149:117–119
Taneja AK, Bredella MA, Torriani M (2013) Ischiofemoral impingement. Magn Reson Imaging Clin N Am 21:65–73
Tannast M, Siebenrock KA, Anderson SE (2007) Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. Am J Roentgenol 188:1540–1552
Terjesen T, Benum P, Anda S, Svenningsen S (1982) Increased femoral anteversion and osteoarthritis of the hip. Acta Orthop Scand 53:571–575
Than P, Sillinger T, Kranicz J, Bellyei A (2004) Radiographic parameters of the hip joint from birth to adolescence. Pediatr Radiol 34:237–244
Tönnis D (1976) Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop 119:39–47
Tonnis D, Heinicke A (1999) Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am 81:1747–1779
Torriani M, Souto SC, Thomas BJ et al (2009) Ischiofemoral impingement syndrome: an entity with hip pain and abnormalities of the quadratus femoris muscle. Am J Roentgenol 193:186–190
Tosun O, Algin O, Yalcin N et al (2012) Ischiofemoral impingement: evaluation with new MRI parameters and assessment of their reliability. Skeletal Radiol 41:575–587
Visser JD, Jonkers A, Hillen B (1982) Hip joint measurements with computerized tomography. J Pediatr Orthop 2:143–146
Werner CML, Copeland CE, Ruckstuhl T, Stromberg J, Turen CH, Bouaicha S (2011) Relationship between Wiberg’s lateral centre edge angle. Lequesne’s acetabular index, and medial acetabular bone stock. Skeletal Radiol 40:1435–1439
Wiberg G (1939) Studies on dysplastic acetabuli and congenital subluxation of the hip joint : with special reference to the complication of osteoarthritis. Acta Chir Can 58(S):7–38
Wiberg G (1953) Shelf operation in congenital dysplasia of the acetabulum and in subluxation and dislocation of the hip joint. J Bone Joint Surg Am 35:65–80
Wyss TF, Clark JM, Weishaupt D, Notzli HP (2007) Correlation between internal rotation and bony anatomy in the hip. Clin Orthop 460:152–158
Zaretsky MV, Alexander JM, McIntire DD et al (2005) Magnetic resonance imaging pelvimetry and the prediction of labor dystocia. Obstet Gynecol 106:919–926
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer-Verlag GmbH Germany, part of Springer Nature
About this chapter
Cite this chapter
Karantanas, A. (2020). Pelvis/Hip: Adult. In: Cassar-Pullicino, V., Davies, A. (eds) Measurements in Musculoskeletal Radiology. Medical Radiology(). Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-68897-6_12
Download citation
DOI: https://doi.org/10.1007/978-3-540-68897-6_12
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-540-43853-3
Online ISBN: 978-3-540-68897-6
eBook Packages: MedicineMedicine (R0)