Abstract
Prior to 2015, intravenous administration of tissue plasminogen activator (tPA) was the only FDA-approved treatment modality for acute ischemic stroke, although many patients who did not meet the criteria for intravenous tPA were offered intra-arterial therapy. Rapid advances in devices and approaches have propelled the evolution of thrombectomy over the past decade from rudimentary mechanical disruption, followed by intra-arterial thrombolytic infusions to increasingly effective thrombectomy devices. We now have level IA evidence supporting mechanical thrombectomy for the treatment of acute ischemic stroke in patients with a large vessel occlusion. We review the critical advancements in thrombectomy technique that have evolved and the key anatomic and technical challenges they address, from first-generation Merci retrieval systems to second-generation Penumbra aspiration systems and third-generation stent retrievers, as well as nuances of their uses to maximize their effectiveness. We also highlight more recent advances that offer patients hope for more expedient vessel recanalization.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Thrombectomy
- Devices for acute stroke
- Acute stroke devices
- Intravenous plasminogen activator
- Intra-arterial thrombolysis
- Stent retrievers
Since its approval in 1995–2015, the administration of systemic intravenous tissue plasminogen activator (tPA) was the only FDA-approved treatment modality for acute ischemic stroke [1, 2], despite rapid advances in thrombectomy devices. However, the restrictive time window after symptom onset (up to 3–4.5 h) and educational, sociocultural, and geographical barriers to accessing rapid care resulted in only a small minority of patients with ischemic stroke receiving treatment with intravenous tPA [3, 4]. In addition, intravenous tPA was demonstrated to be less effective in large vessel occlusions [5]. Intra-arterial techniques were attempted to treat large vessel occlusions, initially using urokinase and prourokinase as described in the PROACT I and II trials [6, 7], which were followed by the development of devices designed for intra-arterial thrombectomy and thromboaspiration. Despite the initially futile thrombectomy trials [8,9,10,11], which failed to show a benefit over intravenous tPA of intra-arterial intervention using devices available at the time, patients outside the intravenous tPA window were still considered candidates for intra-arterial procedures. One of the critiques of these trials was that the lack of imaging identification of actual large vessel occlusions in both arms likely masked any treatment effect. Another was the long enrollment course, and they did not employ modern revascularization devices to achieve safe, efficacious, and expedient vessel revascularization. As such their results did not reflect modern practice at the time they were reported.
Fortunately, the “negative trials” did not temper the enthusiasm of interventionalists committed to improving stroke care but rather served as a rallying call to improve thrombectomy techniques further, streamline stroke triaging processes with an emphasis on LVO identification, and learn from the lessons of the past “futile” trials. Under mounting pressure to have evidence in support of thrombectomy over iv-tPA, five randomized controlled trials [12,13,14,15,16] were launched shortly after the release of the negative trials. An impressive collective effort and rapid enrollment culminated in the halting of the trials in 2015 due to overwhelming statistical efficacy of thrombectomy over medical management. That year marked the largest improvement in the therapeutic options for acute ischemic stroke care since the NINDs trial in 1995 and armed us for the first time with a mechanical thrombectomy device, the stent retriever, with level 1A evidence supporting its use. We now review the technological advances that led to these developments and review next-generation thrombectomy approaches.
Intra-arterial Thrombolysis
Historically, the mainstay of intra-arterial therapy for clot lysis in acute ischemic stroke was the administration of a thrombolytic agent into the vessel of interest [6, 17, 18]. The PROACT II study was a randomized trial of intra-arterial infusion of recombinant prourokinase (r-proUK) versus placebo (heparinized saline) in patients with angiographically documented proximal middle cerebral artery occlusion [7]. Thrombolytic infusion was associated with significantly higher recanalization rates and improved patient outcomes with acceptable complication rates [6, 7]. Despite this significant difference, the FDA did not approve prourokinase for this indication. Local thrombolytic infusions have been performed since the PROACT II study in “off-label” fashion to treat both anterior and posterior circulation occlusions [4, 17,18,19,20]. In addition, some operators employed intra-arterial infusions of tPA or abciximab to further promote clot lysis [21]. Despite the lack of evidence supporting its use, many operators adopted thrombolysis as an adjunct to mechanical thrombectomy. Anecdotally, it became commonplace to administer small doses of either tPA or abciximab intra-arterially to treat smaller, more distal vessel occlusions following a thrombectomy attempt [22,23,24,25].
Adjunctive Endovascular Thrombectomy Strategies
To overcome the limitations of intra-arterial thrombolytic infusions alone, neurointerventionalists initially began attempting clot disruption with microwire manipulation. Shaping the microwire into a “J” or “C” shape and repeatedly advancing it through th e thrombus were sometimes successful at recanalizing an occluded vessel. For more aggressive attempts, the microcatheter could be repeatedly advanced through the thrombus while leaving the microwire purchased in the distal vasculature to “plow” through the thrombus. The hope was that any mechanical disruption of the thrombus, however rudimentary, may promote its lysis especially in the setting of systemic or intra-arterial thrombolysis [26,27,28,29]. Early methods of thrombectomy included the use of the gooseneck snare for clot capture and removal [30, 31].
In 2005, flexible intracranial balloon catheters were introduced. They were initially designed for vessel angioplasty and later for balloon remodeling during aneurysm coil embolization. Shortly thereafter, these balloons were used to achieve mechanical clot disruption by repeated angioplasty of the thrombus itself [32]. The introduction of intracranial stents presented another potential tool to achieve thrombectomy [33]. The Enterprise vascular reconstructive device (Codman, Raynham, Massachusetts, USA) is a retrievable closed-cell design stent that could be partially deployed within the segment of the occluded vessel to achieve both mechanical disruption and partial flow restoration without committing to permanent stent deployment [34, 35]. Some operators reported deploying intracranial stents in the occluded vessel, even in cases not involving underlying intracranial stenosis [36, 37]. The SARIS trial [35, 38] was an FDA-approved pilot study of stent placement within occluded vessels in acute stroke that showed high recanalization rates and good functional outcomes; however, the technique was limited by the need for dual antiplatelet therapy and the concern for hemorrhagic complications including conversions of core infarcts.
All of these devices were not primarily designed for stroke intervention and therefore were used in acute ischemic stroke in an “off-label” fashion. However, these devices and creative strategies set the stage for the design and development of dedicated thrombectomy devices. The following section outlines the various approaches, with a recognition that iterative improvements of each approach continue to be made.
Thrombectomy Techniques
Acute stroke thrombectomy approaches have evolved rapidly. Spurred primarily by advances in catheter technology as well as the thrombectomy device itself, we are now able to achieve higher recanalization rates than ever before. We review the key technological advances and design modifications that have allowed for navigation around the ophthalmic turn for more distal delivery of larger-bore catheters providing more aspiration force directly applied at the thrombus interface.
The First Device: The Merci Retriever
In 2004 the Merci retriever (Concentric Medical, Mountain View, California, USA) became the first mechanical thrombectomy device cleared for human use in the USA by the FDA [39]. The Merci device primarily works by engaging the thrombus with a “corkscrew” distal wire and suture tip deployed from within the clot and then removing the thrombus en bloc to achieve recanalization. The device itself is delivered within a microcatheter (18 L, Concentric Medical). The original iterations of the Merci X series included the 2.5, 3.0, and 3.5 mm diameters. Later, the L series was introduced in 2006 and the V series in 2008. All of these systems were employed using a balloon guide catheter that was positioned at the carotid bifurcation or internal carotid artery. Balloon inflation was intended to cause temporary flow reversal, allowing the Merci to be retrieved into the guide catheter while mitigating the possibility of emboli showering to distal territories. However, clot retrieval into the guide catheter still required a long distance to be traveled while maintaining purchase on the thrombus, most commonly from the M1 segment of the middle cerebral artery to the proximal cervical internal carotid artery. The vector force applied while pulling on the thrombus was suboptimal (downward along the long axis of the cervical carotid artery, not horizontally along the axis of the middle cerebral artery). This caused considerable torqueing, stretching, and distortion of the parent vessel and presented a biomechanical disadvantage to thrombus removal. Traction on the vasculature results in pain for the patient. To avoid the inevitable movement that is induced, many operators chose to perform thrombectomy under general anesthesia. In addition, the Merci technique required a long distance to be traveled while remaining engaged with the thrombus.
Revascularization rates in the Merci studies range from 43% to 55% [40,41,42] and as such represented a vast improvement to thrombolysis alone for LVO, with the caveat that distal embolization rates were incompletely captured by recanalization scales. However, thrombectomy with the Merci device as frontline therapy was not associated with a higher percentage of good functional outcomes (defined as modified Rankin Scale score≤ 2 at 90 days), reported in up to 36% of patients [42]. Recanalization rates with the Merci system are thought to have increased since the initial trial from design refinements as well as increased operator experience [43].
A landmark advancement came in 2010 with the approval of the outreach distal access catheter (DAC; Concentric Medical), which would have repercussions for the application of the Merci device and also for future iterations of thrombectomy approaches. The DAC was designed for the purpose of buttressing access for the Merci thrombectomy device, affording stable access to the target vessel. Use of the DAC optimized the vectors at play during pulling of the device. With further understanding of clot fragmentation and distal embolization, the DAC was used as an intermediate aspiration device which aided in preventing showering of distal emboli during clot retrieval, increased the aspiration power applied directly to the thrombus [44, 45]. The development of large-bore flexible catheters that could be delivered into the intracranial circulation represented a major advancement in thrombectomy technology and also in intermediate catheter technology [45, 46]. The DAC has a flexible distal shaft with increased proximal shaft strength and axial load-bearing characteristics as well as good hoop strength, allowing it to be delivered to the intracranial circulation around the ophthalmic bend when navigated over a coaxial catheter system. A major drawback to the Merci retrieval system was that it necessitated navigating past the ophthalmic bend with every pass, decreasing the efficiency of the system and adding to procedure times.
The EKOS MicroLysUS Catheter
The EKOS microcatheter system (Bothwell, Washington, USA) and family of devices were designed to provide ultrasonic vibration to facilitate thrombolysis. Earlier studies employed a 2.5 F infusion catheter with an ultrasound-generating 2 mm transducer ring [47]. The current EndoWave system (Bothwell) is a 5.2 F 106-cm-long device using ultrasonic waves delivered via core wire and designed to be used in conjunction with intra-arterial tPA [48]. Data regarding this device remain limited, but further development and experience may prove the approach beneficial. Indeed, transcranial ultrasonic disruption remains an approach undergoing research and development [49, 50].
Second Generation: Penumbra Aspiration System
The Penumbra aspiration system introduced in 2008 involves maceration of the thrombus with a separator which is repeatedly introduced and withdrawn from the thrombus under direct aspiration to prevent showering of fragments [51]. While the Merci system relied primarily on a delivery microcatheter (the 18 L; Stryker, Kalamazoo, Michigan, USA) to the site of occlusion, the Penumbra aspiration system relied on the delivery of a relatively large-bore catheter to the thrombus (up to effectively a 5 F device). The introduction of highly flexible lubricious polymers with good hoop strength allowed for safe placement of large intermediate-class catheters directly into the large intracranial vessels. While the later introduction of the DAC catheter resulted in similar catheter profiles in the distal vasculature, the development of large-bore flexible catheters was essential to the function of the Penumbra system.
The original iteration of the Penumbra reperfusion catheter system included several different sized catheters (internal diameter 0.026″, 0.032″, and 0.041″) and accompanying separators to maximize clot interaction and force of aspiration in vessels of differing diameters (internal carotid artery terminus, M1, M2, M3) to address both proximal and distal thrombi [52]. The largest device had a lumen diameter of 0.041 inch, and it tracked suboptimally and required a median 45 min to achieve acceptable recanalization [53]. In 2009, the reperfusion catheter 054 became available which dramatically improved the aspiration efficiency to a median 20 min [53] due to its much larger tapered lumen. As the aspiration force is proportional to the square of the diameter of the catheter, the 054 catheter provided an estimated 4× aspiration force over the next smaller catheter, the 041 [53].
Despite the improved technology, the 054 still required a coaxial catheter for delivery to the middle cerebral artery. Although a larger catheter lumen provides higher suction and more rapid removal of material, it also results in a larger catheter profile and more difficult distal navigation. Owing to its size, the 054 catheter often required the use of a coaxial technique to facilitate navigation to the site of occlusion. When navigated over a 0.014 inch microwire alone, a significant ledge would get held up at the origin of the ophthalmic artery. To overcome this obstacle to the target lesion, access with the 054 catheter can be optimized with a coaxial technique (Fig. 32.1). The smaller 032 and 026 reperfusion catheters can be delivered simply over either a 0.014 or 0.016 inch wire and the larger 054 delivered over those. One of the major advantages of the Penumbra aspiration system was that once the catheter system was delivered to the target vessel, separator clot maceration could be performed without having to reaccess (additional “passes”), as was the case for the Merci device [54].
(a) While a larger catheter lumen provides higher suction and more rapid removal of thrombus, it results in a larger catheter profile and “ledge effect” which renders navigation past the ophthalmic artery origin challenging. (b) To overcome this obstacle, access with an intermediate catheter is optimized with a coaxial technique resulting in a more tapered construct that minimizes the “ledge effect”
Despite these advances in catheter technology, navigating past the carotid siphon was still a relative challenge during thrombectomy cases. In patients with very acute angulation in the ophthalmic segment, adjunctive techniques could be performed to obtain the necessary distal access. One approach used the Merci retriever system as an adjunct to improve the trackability of the 054 reperfusion catheter by altering the angle with which the catheter engages the ophthalmic segment and M1 origin. By deploying an appropriately sized Merci retriever (Concentric Medical), such as a V.2.0 or V.2.5 soft, in the mid-M1 segment through either the 032 catheter or an 18 L microcatheter and then applying gentle traction on the Merci retriever, the course of the wire straightens, approximating the inner curve of the vasculature, pulling the catheter complex away from the ledge of the vessel origins (“grappling hook” technique) [44, 55], an approach now used routinely using stent retrievers and intermediate catheters. The 054 catheter can then be more readily advanced into the target vessel. Once the 054 reperfusion catheter is in place, the retriever is resheathed into the 18 L microcatheter and then removed prior to separator placement and aspiration.
The next iteration of the Penumbra aspiration catheter family (Max series) was introduced in 2012 and included larger inner diameters at the distal end as well as the proximal end to increase the aspiration power. The larger proximal lumen reduces resistance to flow and therefore increases aspiration force at the catheter tip. Improvements in polymer and braid and ring reinforcement provide more catheter tip flexibility and an increased number of transition zones to improve trackability while maintaining hoop strength. The newly introduced intermediate catheters were named 5Max, 4Max, and 3Max. An increased number of transition zones in the catheter design and manufacturing allowed these catheters to be delivered primarily over either a 0.014 or 0.016 inch microwire, even past the ophthalmic origin.
Third Generation: Stent Retrievers
The next generation of mechanical thrombectomy devices includes the “stent retriever” family: Solitaire (ev3 Endovascular, Plymouth, Minnesota, USA), Trevo Pro (Stryker Neurovascular, Kalamazoo Michigan, USA), and arguably the Penumbra 3D separator (Penumbra, Alameda, California, USA). The formal stent retrievers are literally stents that are fully recapturable and fused to the delivery microwire. Differences in cell design and lubricity and end portion variations have also been introduced in pre-market stent retrievers and are beyond the scope of this article. The Penumbra 3D separator differs from formal stent retrievers in that there is no “stent.” A larger portion of the separator design by mass is designed to engage at the center of the vessel lumen rather than in an actual stent where the material is primarily at the outer margins of the vessel near the intima. These devices have the advantage of efficacious recanalization like a stent but are able to be removed, which obviates the need for clopidogrel and aspirin. While the Solitaire was the first to be released, all major device manufacturers produce similar devices [56]. The design differences in these devices have yet to show statistical differences in efficacy or safety.
Stent retrievers (SR) capitalize on the advantages observed with partial stent deployment and recapture during thrombectomy. The microcatheter is delivered across the thrombus, and the SR is unsheathed from within the thrombus itself. The outward radial force of the SR as it deploys promotes engaging the clot. While doing so, cerebral blood flow to the involved territory is temporarily restored, functioning as an “endovascular bypass.” Once the SR has engaged the thrombus, it is pulled back (“retrieved”) into a guide catheter. Application of suction with either a pump or manual syringe aspiration during retrieval may promote clot purchase and reduce the showering of emboli. Operators may also opt to employ a balloon guide catheter as an adjunct to decrease the likelihood of emboli to new territory. Recanalization rates with SR were found to be superior to the Merci device in several studies [49, 51], leading to rapid and widespread adoption.
To minimize the distance, the SR must travel while engaging the thrombus, especially into larger-caliber vasculature such as the internal carotid artery from the middle cerebral artery, and mitigating the possibility of losing purchase of the clot, variations to the SR technique have been employed with incorporation of Penumbra reperfusion catheters. For example, a 5Max catheter can be advanced over an 025 microcatheter and microwire up to the site of occlusion and left at the face of the thrombus. The SR is then deployed and the microcatheter is removed, leaving the SR in place. The SR is then pulled directly into the 5Max while maintaining aspiration (the so-called “Solumbra” technique since it combines a stent retriever (Solitaire) with a Penumbra aspiration catheter), and both are removed together (Fig. 32.2), much in the same way as the Merci retriever device was removed with a DAC. However, traction is minimized as compared with the Merci system since the force vectors are horizontal in orientation from the aperture of the aspiration catheter in parallel to the M1. This eliminated the painful stimulus that patients were formerly experiencing. Thus, in addition to representing a more effective technique, the now painless procedure had the added advantage of reintroducing the concept of the awake thrombectomy, with many operators now electing to perform the procedure with minimal conscious sedation. Advantages included the ability to examine the patient’s neurological status throughout the procedure, shorter CT to groin stick times, and avoiding the imminent risk of systemic hypotension from induction of general anesthesia. In refractory cases in which the thrombus cannot be extracted using a standard SR approach, two SR deployed in “Y” configuration (coined “Y-stent retriever”) have been described (Figs. 32.3 and 32.4).
“Solumbra” (Solitaire and Penumbra) technique. (a) Anteroposterior (AP) and (b) lateral digital subtraction angiography (DSA) demonstrates an M1 occlusion. (c) A Solitaire stent retriever (SR) is deployed across the M1 segment occlusion (large white arrow), with the aspiration catheter in the proximal M1 segment (small white arrow) and the guide catheter in the distal cervical internal carotid artery (black arrow). (d) The SR is then withdrawn back into the aspiration catheter under direct aspiration applied locally at the M1. Operator may choose to withdraw the SR entirely into the aspiration catheter or to partially withdraw and then pull both the SR and the aspiration catheter together back to the guide catheter. Aspiration can also be applied at the guide catheter. Some may choose to perform this technique with a balloon guide catheter to affect flow reversal for added protection against distal emboli in the event of thrombus fragmentation. (e) AP and lateral DSA demonstrates recanalization of the M1 occlusion (TICI 2B) with showering of distal fragments and small vessel occlusions
Illustration of the “Y-stent retriever” technique with schematic illustrations to depict the procedure. (a) A Headway 27 microcatheter (MicroVention Terumo) was navigated into the occluded vessel. (b) A 4 × 20 mm Solitaire SR (Covidien) was deployed from the right superior M2 branch to M1. (c) The microcatheter is removed to leave more space in the lumen of the guide catheter for another system and for more potent aspiration. Another system is navigated using a Headway 21 microcatheter is advanced to the right inferior M2 artery passing through the interstices of the stent previously deployed. (d) Once in this “Y” configuration, a 4 × 20 mm Catch stent retriever (Balt) is deployed from the right inferior M2 artery to M1, leaving the proximal tip of the Catch SR inside the Solitaire SR, thus forming the “Y-stent retriever.” (e) Both devices are slowly recovered by simultaneously pulling them together into guide catheter under continuous aspiration and fluoroscopic imaging control
(a) Anteroposterior projection of right internal carotid digital subtraction angiography. An occlusion at the level of the right proximal MCA-M1 is detected, TICI 0. (b) Angiographic imaging of the Y-SR technique procedure: front projection showing 4 × 20 mm Solitaire SR (Covidien) already deployed from the right superior M2 branch to M1 (white arrow). Another system is advanced to the right inferior M2 artery passing through the interstices of the stent previously deployed (black arrow). (c) Once in this “Y” configuration, a 4 × 20 mm Catch stent retriever (Balt) is deployed from the right inferior M2 artery to M1 (white arrow), leaving the proximal tip front projections of right internal carotid angiography. This resulted in complete recanalization of the branch with normal antegrade flow, Thrombolysis in Cerebral Infarction (TICI) scale 3, of the Catch SR inside the Solitaire SR. (d) AP view showing the stent retrievers in place. (e)
SR technology was employed exclusively in the ESCAPE, EXTEND-IA, SWIFT PRIME, and REVASCAT trials. While the MR CLEAN trial did not dictate which thrombectomy device was to be utilized, the majority of cases were also SR based. Given that SR were used in the overwhelming majority of patients enrolled in the positive trials, they have often been referred to as the “Stent Retriever trials,” which are reflected in the updated June 2015 American Heart Association/American Stroke Association guidelines recommending thrombectomy to be performed with a SR. However, thrombectomy techniques evolved even while those trials were enrolling, setting the stage for the next-generation strategy as detailed below. Although controversial, it is the belief of many stroke experts that it’s more important that the LVO is recanalized quickly and effectively (outcome specific), rather than how it is recanalized (device specific). This philosophy has allowed continued improvements in thrombectomy techniques which are now being tested in a randomized controlled trial setting (COMPASS), as detailed in the next section.
New Generation: Direct Aspiration
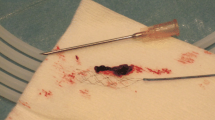
Direct aspiration [57,58,59,60] has become possible due to advances in catheter technology that allow large-caliber aspiration catheters to be advanced intracranially to the thrombus. In general, the largest size aspiration catheter that the vessel can accommodate should be utilized. In the first iteration, this was most commonly a Penumbra 5Max reperfusion catheter (Penumbra, Oakland, CA) for M1 or carotid terminus occlusions. The 5Max can be advanced to the level of the thrombus over any microcatheter and microwire the operator chooses but most commonly a Velocity microcatheter (Penumbra, Oakland, CA) over a 0.016 inch Fathom wire (Boston Scientific Corp., Naidich, MA). The microcatheter and wire are removed, and aspiration is applied by either a 20 or 60 cc syringe or the use of the Penumbra aspiration pump that is part of the Penumbra thrombectomy/aspiration system [38]. Inability to draw back blood on aspiration confirms optimal position of the 5Max catheter abutting the thrombus. The next iteration involved advancing the catheter slightly to ensure firm engagement with the thrombus. The 5Max catheter is then slowly withdrawn while maintaining aspiration. Aspiration is also applied to the side port of the guide catheter to prevent dislodging the thrombus from the 5Max aperture as it is withdrawn into the sheath. Clots are typically removed en bloc, minimizing the risk of downstream emboli (Fig. 32.5). When this technique is successful, it eliminates the need to introduce stent retriever or Penumbra separator devices, leading to an overall much lower procedure device cost. [57, 58] Thus, we have found the initial application of this technique to provide the highest cost-effective value in acute stroke treatment.
ADAPT illustrations. Direct aspiration typically removed the thrombus en bloc, minimizing the risk of distal emboli. The largest-bore aspiration catheter that the occluded vessel will accommodate is advanced to the level of the thrombus. Aspiration is applied to engage the thrombus, which is then removed as demonstrated in the illustrations. (a,b,c) Carotid terminus occlusion recanalized in 15 min from groin puncture with direct aspiration thrombectomy in a single pass. (d, e, f) Basilar apex occlusion recanalized in 10 min with two passes of direct aspiration thrombectomy. (g, h, i) MCA bifurcation occlusion recanalized in 12 min with a single pass direct aspiration. (j, k, l) MCA bifurcation occlusion recanalized in 7 min with a single pass direct aspiration
This approach was facilitated by the development of the Penumbra Max aspiration catheter technology which significantly increased the ease and speed of navigation of a large-bore catheter into the intracranial circulation. The direct aspiration technique differs from prior thrombectomy methods, as it focuses on engaging and removing the clot in its entirety rather than the use of the separator that was designed to macerate the thrombus and clear the tip of the aspiration catheter [40]. Historically, due to the challenges with tracking an aspiration catheter into the intracranial circulation, catheters had to be telescoped with other catheters together or other tricks employed to advance through the siphon [32, 34, 41, 54, 55]. However, the superior trackability of the Penumbra Max catheters has given us the confidence to attempt direct aspiration alone without the fear that it will be a significant time and danger impediment to the patient if intracranial access is lost. The second iteration of the aspiration catheter, the 5Max ACE, has an increased inner diameter of 0060 at the distal 30 cm while housing a 0.068 proximal end for larger aspiration forces. Advances in catheter technology would soon follow, allowing for even larger-bore catheters to be safely delivered to the intracranial circulation. With the introduction of the ACE 064 and the ACE 068 (Penumbra, Oakland, CA), the direct aspiration technique was refined further. Owing to the larger aperture of these catheters, the aspiration catheter can now be advanced over the thrombus, to “ingest” the thrombus which is now typically aspirated directly into the catheter without having to remove it (Fig. 32.6).
Aspiration catheter technology has rapidly advanced. With the introduction of the ACE 064 and the ACE 068 (Penumbra, Oakland, CA), the direct aspiration technique has been refined further. Owing to the larger aperture of these catheters, the aspiration catheter can now be advanced directly over the thrombus to “ingest” the thrombus under aspiration. The thrombus is now typically aspirated directly into the catheter aspiration tubing without having to remove it
Perhaps most importantly, if aspiration alone is not successful at revascularizing the occluded vessel, the Penumbra 5Max catheter can also function as a distal conduit for other devices such as a smaller 3Max catheter for direct aspiration in more distal branches (e.g., M2, P2, or P3) or stent retrievers, balloons or stents. This forms the basis of the “ADAPT” technique (a direct aspiration first pass technique) which is gaining popularity. If direct aspiration attempts are unsuccessful, other attempts including SR thrombectomy can then be performed. At the time of this writing, enrollment is well on the way for the COMPASS trial, a randomized controlled trial of anterior circulation LVO treated within 6 h of symptom onset with thrombectomy technique randomized to either SR or direct aspiration first. If unsuccessful after three attempts, another technique is then allowed. Trial completion is expected in early 2017.
The newest iteration of direct aspiration involves its application in more distal vasculature. In smaller-caliber vessels, the technique can be employed with either a 4 Max or 3Max reperfusion catheter (Penumbra Inc., Oakland, CA). In principle, the largest-bore catheter that the occlude vessel can accommodate is selected for aspiration (Fig. 32.7), with effective (TICI ≥2B 97.1%) and fast recanalization (mean 35.7 min) achieved safely [59].
(a) Illustration demonstrating aspiration catheter size recommendations for anterior circulation thrombectomy. The guide catheter is positioned in the ICA, providing a platform for thrombectomy with aspiration catheters. (b) CT perfusion imaging demonstrating elevated mean transit time in the left frontal lobe consistent with a left M2 occlusion. (c) AP and (d) lateral projection cerebral angiogram during a left internal carotid injection demonstrating M2 occlusion with no flow past the site of thrombus (arrows). (e). AP and (f) lateral projection cerebral angiogram during a left internal carotid injection following thrombectomy demonstrating resolution of M2 occlusion and opacification of distal branches. (g) CT perfusion imaging demonstrating elevated mean transit time consistent with a left A2 occlusion. (h) Lateral projection cerebral angiogram demonstrating A2 occlusion (arrow), (i) post-thrombectomy lateral projection cerebral angiogram with resolution of A2 occlusion and complete opacification of distal branches. (j) CT perfusion imaging demonstrating elevated mean transit time in the right occipital lobe consistent with right P2 ischemia. (k) Cerebral angiogram with AP projection from a left vertebral artery injection demonstrating right P2 occlusion and no opacification distal to the thrombus (arrow). (l) Post-thrombectomy cerebral angiogram with AP projection from a left vertebral artery injection demonstrating resolution of the thrombus with opacification of the distal PCA branches
Future Devices
On-label intra-arterial devices for acute stroke intervention are developing rapidly with the introduction of both iterative changes and new classes of devices. With new generations of devices, increasingly high rates of recanalization are being reported. It is likely new techniques and devices will continue to evolve offering a more robust tool set and combination of devices for interventional management of acute stroke. However, futile recanalization remains a problem [43].
Conclusion
There have been rapid advances in thrombectomy devices and approaches over the past decade, from rudimentary mechanical disruption, followed by intra-arterial thrombolytic infusions to increasingly effective thrombectomy devices (Fig. 32.8) [61]. While it remains unknown what combinations of techniques, devices, selection criteria, and medicines will yield the best outcomes, ongoing improvements in the devices and techniques are yielding improved angiographic and clinical outcomes. Device technology, selection strategies, and medical management will likely evolve in tandem, and we look forward to the continued evolution of thrombectomy approaches for acute stroke in the future. We remind our colleagues in the neurointerventional field that high enrollment in clinical trials will be required to secure the role of intra-arterial therapy in the management of stroke.
References
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–7.
Jauch EC, Saver JL, Adams HP, et al. American Heart Association Stroke C, Council on Cardiovascular N, Council on Peripheral Vascular D, Council on Clinical C: guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947.
Hirsch JA, Yoo AJ, Nogueira RG, Verduzco LA, Schwamm LH, Pryor JC, Rabinov JD, Gonzalez RG. Case volumes of intra-arterial and intravenous treatment of ischemic stroke in the USA. J Neurointerv Surg. 2009;1:27–31.
Fonarow GC, Smith EE, Saver JL, Reeves MJ, Bhatt DL, Grau-Sepulveda MV, Olson DM, Hernandez AF, Peterson ED, Schwamm LH. Timeliness of tissue-type plasminogen activator therapy in acute ischemic Stroke Clinical perspective patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123:750–8.
Wechsler LR, Roberts R, Furlan AJ, Higashida RT, Dillon W, Roberts H, Rowley HA, Pettigrew LC, Callahan AS, Bruno A. Factors influencing outcome and treatment effect in PROACT II. Stroke. 2003;34:1224–9.
del Zoppo GJ, Higashida RT, Furlan AJ, Pessin MS, Rowley HA, Gent M. PROACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. PROACT Investigators Prolyse in Acute Cerebral Thromboembolism. Stroke. 1998;29:4–11.
Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, Pessin M, Ahuja A, Callahan F, Clark WM. Intra-arterial prourokinase for acute ischemic stroke. JAMA. 1999;282:2003–11.
Kidwell CS, Jahan R, Gornbein J, Alger JR, Nenov V, Ajani Z, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368:914–23.
Ciccone A, Valvassori L, Nichelatti M, Sgoifo A, Ponzio M, Sterzi R, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013;368:904–13.
Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Endovascular therapy after intravenous t-pa versus t-pa alone for stroke. N Engl J Med. 2013;368:893–903.
Chimowitz MI. Endovascular treatment for acute ischemic stroke--still unproven. N Engl J Med. 2013;368:952–5.
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, van Walderveen MA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, Kappelle LJ, Lo RH, van Dijk EJ, de Vries J, de Kort PL, van Rooij WJ, van den Berg JS, van Hasselt BA, Aerden LA, Dallinga RJ, Visser MC, Bot JC, Vroomen PC, Eshghi O, Schreuder TH, Heijboer RJ, Keizer K, Tielbeek AV, den Hertog HM, Gerrits DG, van den Berg-Vos RM, Karas GB, Steyerberg EW, Flach HZ, Marquering HA, Sprengers ME, Jenniskens SF, Beenen LF, van den Berg R, Koudstaal PJ, van Zwam WH, Roos YB, van der Lugt A, van Oostenbrugge RJ, Majoie CB, Dippel DW, MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11–20. https://doi.org/10.1056/NEJMoa1411587. Erratum in: N Engl J Med. 2015 Jan 22;372(4):394
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD, ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–30.
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M, Ang T, Scroop R, Barber PA, McGuinness B, Wijeratne T, Phan TG, Chong W, Chandra RV, Bladin CF, Badve M, Rice H, de Villiers L, Ma H, Desmond PM, Donnan GA, Davis SM, EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009–18.
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W, Jansen O, Jovin TG, Mattle HP, Nogueira RG, Siddiqui AH, Yavagal DR, Baxter BW, Devlin TG, Lopes DK, Reddy VK, du Mesnil de Rochemont R, Singer OC, Jahan R, SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372(24):2285–95.
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, San Román L, Serena J, Abilleira S, Ribó M, Millán M, Urra X, Cardona P, López-Cancio E, Tomasello A, Castaño C, Blasco J, Aja L, Dorado L, Quesada H, Rubiera M, Hernandez-Pérez M, Goyal M, Demchuk AM, von Kummer R, Gallofré M, Dávalos A, REVASCAT Trial Investigators. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015 Jun 11;372(24):2296–306.
Suarez J, Sunshine J, Tarr R, Zaidat O, Selman W, Kernich C, Landis D. Predictors of clinical improvement, angiographic recanalization, and intracranial hemorrhage after intra-arterial thrombolysis for acute ischemic stroke. Stroke. 1999;30:2094–100.
Ernst R, Pancioli A, Tomsick T, Kissela B, Woo D, Kanter D, Jauch E, Carrozzella J, Spilker J, Broderick J. Combined intravenous and intra-arterial recombinant tissue plasminogen activator in acute ischemic stroke. Stroke. 2000;31:2552–7.
Hacke W, Zeumer H, Ferbert A, Bruckmann H, del Zoppo GJ. Intra-arterial thrombolytic therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke. 1988;19:1216–22.
Brandt T, von Kummer R, Muller-Kuppers M, Hacke W. Thrombolytic therapy of acute basilar artery occlusion. Variables affecting recanalization and outcome. Stroke. 1996;27:875–81.
Abou-Chebl A, Bajzer CT, Krieger DW, Furlan AJ, Yadav JS. Multimodal therapy for the treatment of severe ischemic stroke combining GPIIb/IIIa antagonists and angioplasty after failure of thrombolysis. Stroke. 2005;36:2286–8.
Gobin YP, Starkman S, Duckwiler GR, Grobelny T, Kidwell CS, Jahan R, Pile-Spellman J, Segal A, Vinuela F, Saver JL. MERCI 1: a phase 1 study of mechanical embolus removal in cerebral ischemia. Stroke. 2004;35:2848–54.
Smith WS, Sung G, Starkman S, Saver JL, Kidwell CS, Gobin YP, Lutsep HL, Nesbit GM, Grobelny T, Rymer MM. Safety and efficacy of mechanical embolectomy in acute ischemic stroke results of the MERCI trial. Stroke. 2005;36:1432–8.
Lewandowski CA, Frankel M, Tomsick TA, Broderick J, Frey J, Clark W, et al. Combined intravenous and intra-arterial r-TPA versus intra-arterial therapy of acute ischemic stroke emergency management of stroke (EMS) bridging trial. Stroke. 1999;30(12):2598–605.
Zeumer H, Freitag HJ, Zanella F, Thie A, Arning C. Local intra-arterial fibrinolytic therapy in patients with stroke: urokinase versus recombinant tissue plasminogen activator (r-TPA). Neuroradiology. 1993;35(2):159–62.
Smith W. Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi mechanical embolus removal in cerebral ischemia (MERCI) trial, part I. Am J Neuroradiol. 2006;27:1177–82.
Flint AC, Duckwiler GR, Budzik RF, Liebeskind DS, Smith WS. Merci, multi MWC: mechanical thrombectomy of intracranial internal carotid occlusion: pooled results of the MERCI and multi MERCI part I trials. Stroke. 2007;38:1274–80.
Qureshi AI, Siddiqui AM, Suri MFK, Kim SH, Ali Z, Yahia AM, et al. Aggressive mechanical clot disruption and low-dose intra-arterial third-generation thrombolytic agent for ischemic stroke: a prospective study. Neurosurgery. 2002;51(5):1319–29.
Barnwell SL, Clark WM, Nguyen TT, O’Neill OR, Wynn ML, Coull BM. Safety and efficacy of delayed intraarterial urokinase therapy with mechanical clot disruption for thromboembolic stroke. Am J Neuroradiol. 1994;15(10):1817–22.
Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, Lutsep HL, Rymer MM, Higashida RT, Starkman S. Mechanical thrombectomy for acute ischemic stroke final results of the multi MERCI trial. Stroke. 2008;39:1205–12.
Chopko BW, Kerber C, Wong W, Georgy B. Transcatheter snare removal of acute middle cerebral artery thromboembolism: technical case report. Neurosurgery. 2000;46(6):1529–31.
Spiotta AM, Hussain MS, Sivapatham T, Bain M, Gupta R, Moskowitz SI, Hui FK. The versatile distal access catheter: the Cleveland Clinic experience. Neurosurgery. 2011;68:1677.
Jankowitz B, Aghaebrahim A, Zirra A, Spataru O, Zaidi S, Jumaa M, Ruiz-Ares G, Horowitz M, Jovin TG. Manual aspiration thrombectomy adjunctive endovascular recanalization technique in acute stroke interventions. Stroke. 2012;43:1408–11.
Turk A, Manzoor MU, Nyberg EM, Turner RD, Chaudry I. Initial experience with distal guide catheter placement in the treatment of cerebrovascular disease: clinical safety and efficacy. J Neurointerv Surg. 2013;5(3):247–52.
Mahon BR, Nesbit GM, Barnwell SL, Clark W, Marotta TR, Weill A, Teal PA, Qureshi AI. North American clinical experience with the EKOS MicroLysUS infusion catheter for the treatment of embolic stroke. Am J Neuroradiol. 2003;24:534–8.
Kuliha M, Roubec M, Fadrná T, Šaňák D, Herzig R, Jonszta T, Czerný D, Krajča J, Procházka V, Školoudík D. Endovascular sono-lysis using EKOS system in acute stroke patients with a main cerebral artery occlusion–a pilot study. Pers Med. 2012;1:65–72.
Clark W, Lutsep H, Barnwell S, Nesbit G, Egan R, North E, Yanase L, Lowenkopf T, Petersen B, Grunwald I. The penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009;40:2761–8.
Yoo AJ, Frei D, Tateshima S, Turk AS, Hui FK, Brook AL, Heck DV, Hirsch JA. The penumbra stroke system: a technical review. J Neurointerv Surg. 2012;4:199–205.
Frei D, Gerber J, Turk A, McPherson M, Heck D, Hui F, Joseph G, Jahan R, Miskolczi L, Carpenter J, Grobelny T, Goddard J, Turner RD, Huddle D, Bellon R, Chaudry I. The SPEED study: initial clinical evaluation of the Penumbra novel 054 Reperfusion Catheter. J Neurointerv Surg. 2013;5(Suppl 1):i74–6.
Tarr R, Hsu D, Kulcsar Z, Bonvin C, Rufenacht D, Alfke K, Stingele R, Jansen O, Frei D, Bellon R. The POST trial: initial post-market experience of the penumbra system: revascularization of large vessel occlusion in acute ischemic stroke in the United States and Europe. J Neurointerv Surg. 2010;2:341–4.
Hui FK, Hussain MS, Spiotta A, Bhalla T, Toth G, Moskowitz SI, Elgabaly M, Sivapatham T, Rasmussen PA. Merci retrievers as access adjuncts for reperfusion catheters: the grappling hook technique. Neurosurgery. 2012;70:456–60.
Ringer AJ, Qureshi AI, Fessler RD, Guterman LR, Hopkins LN. Angioplasty of intracranial occlusion resistant to thrombolysis in acute ischemic stroke. Neurosurgery. 2001;48:1282–90.
Levy EI, Siddiqui AH, Crumlish A, Snyder KV, Hauck EF, Fiorella DJ, Hopkins LN, Mocco J. First Food and Drug Administration-approved prospective trial of primary intracranial stenting for acute stroke SARIS (stent-assisted recanalization in acute ischemic stroke). Stroke. 2009;40:3552–6.
Kelly ME, Furlan AJ, Fiorella D. Recanalization of an acute middle cerebral artery occlusion using a self-expanding, reconstrainable, intracranial microstent as a temporary endovascular bypass. Stroke. 2008;39:1770–3.
Levy EI, Ecker RD, Horowitz MB, Gupta R, Hanel RA, Sauvageau E, Jovin TG, Guterman LR, Hopkins LN. Stent-assisted intracranial recanalization for acute stroke: early results. Neurosurgery. 2006;58:458–63.; discussion 458–463.
Mocco J, Hanel RA, Sharma J, Hauck EF, Snyder KV, Natarajan SK, Linfante I, Siddiqui AH, Hopkins LN, Boulos AS. Use of a vascular reconstruction device to salvage acute ischemic occlusions refractory to traditional endovascular recanalization methods: clinical article. J Neurosurg. 2010;112:557–62.
Levy EI, Rahman M, Khalessi AA, Beyer PT, Natarajan SK, Hartney ML, Fiorella DJ, Hopkins LN, Siddiqui AH, Mocco J. Midterm clinical and angiographic follow-up for the first food and drug administration-approved prospective, single-arm trial of primary stenting for stroke: saris (stent-assisted recanalization for acute ischemic stroke). Neurosurgery. 2011;69:915–20.
Roth C, Papanagiotou P, Behnke S, Walter S, Haass A, Becker C, Fassbender K, Politi M, Körner H, Romann M-S. Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke. 2010;41:2559–67.
Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, Clark W, Budzik R, Zaidat OO. Solitaire flow restoration device versus the Merci retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012;380(9849):1241–9.
Schellinger PD, Alexandrov AV, Barreto AD, Demchuk AM, Tsivgoulis G, Kohrmann M, et al. Combined lysis of thrombus with ultrasound and systemic tissue plasminogen activator for emergent revascularization in acute ischemic stroke (CLOTBUST-ER): design and methodology of a multinational phase 3 trial. Int J Stroke. 2015;10(7):1141–8.
Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, Liebeskind DS, Smith WS, Trialists T. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012;380:1231–40.
Turk AS, Spiotta A, Frei D, Mocco J, Baxter B, Fiorella D, Siddiqui A, Mokin M, Dewan M, Woo H. Initial clinical experience with the ADAPT technique: a direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg. 2014;6(3):231–7.
Turk AS, Campbell JM, Spiotta A, Vargas J, Turner RD, Chaudry MI, Battenhouse H, Holmstedt CA, Jauch E. An investigation of the cost and benefit of mechanical thrombectomy for endovascular treatment of acute ischemic stroke. J Neurointerv Surg. 2014 Jan;6(1):77–80.
Park MS, Stiefel MF, Fiorella D, Kelly M, McDougall CG, Albuquerque FC. Intracranial placement of a new, compliant guide catheter: technical note. Neurosurgery. 2008;63:E616–7.
Chaudhary N, Pandey AS, Thompson BG, Gandhi D, Ansari SA, Gemmete JJ. Utilization of the neuron 6 French 0.053 inch inner luminal diameter guide catheter for treatment of cerebral vascular pathology: continued experience with ultra distal access into the cerebral vasculature. J Neurointerv Surg. 2012;4:301–6.
Molina CA. Futile recanalization in mechanical embolectomy trials a call to improve selection of patients for revascularization. Stroke. 2010;41:842–3.
Turk AS, Frei D, Fiorella D, Mocco J, Baxter B, Siddiqui A, Spiotta A, Mokin M, Dewan M, Quarfordt S, Battenhouse H, Turner R, Chaudry I. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2014;6(4):260–4. https://doi.org/10.1136/neurintsurg-2014-011125.
Turk AS, Turner R, Spiotta A, Vargas J, Holmstedt C, Ozark S, Chalela J, Turan T, Adams R, Jauch EC, Battenhouse H, Whitsitt B, Wain M, Chaudry MI. Comparison of endovascular treatment approaches for acute ischemic stroke: cost effectiveness, technical success, and clinical outcomes. J Neurointerv Surg. 2015 Sep;7(9):666–70. https://doi.org/10.1136/neurintsurg-2014-011282.
Vargas J, Spiotta A, Fargen K, Turner R, Chaudry I, Turk A. Long term experience using the ADAPT technique for the treatment of acute ischemic stroke. J Neurointerv Surg. 2016; pii: neurintsurg-2015-012211. doi: https://doi.org/10.1136/neurintsurg-2015-012211.
Vargas J, Spiotta AM, Fargen K, Turner RD, Chaudry I, Turk A. Experience with ADAPT for thrombectomy in distal cerebral artery occlusions causing acute ischemic stroke. World Neurosurg. 2017;99:31–6.
Spiotta AM, Chaudry MI, Hui FK, Turner RD, Kellogg RT, Turk AS. Evolution of thrombectomy approaches and devices for acute stroke: a technical review. J Neurointerv Surg. 2015;7(1):2–7. https://doi.org/10.1136/neurintsurg-2013-011022.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Spiotta, A.M., Hui, F.K. (2019). Evolution of Thrombectomy Approaches, Philosophy, and Devices for Acute Stroke. In: Spiotta, A., Turner, R., Chaudry, M., Turk, A. (eds) Management of Cerebrovascular Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-99016-3_32
Download citation
DOI: https://doi.org/10.1007/978-3-319-99016-3_32
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-99015-6
Online ISBN: 978-3-319-99016-3
eBook Packages: MedicineMedicine (R0)