Abstract
Age-related losses in muscle mass, strength, and function (termed sarcopenia) coupled with a deterioration in brain structure and cognitive function have been associated with a greater risk for incident disability, falls, fractures, and frailty as well as incident dementia. As a result, there has been considerable interest in identifying strategies that can simultaneously improve muscle and cognitive health outcomes. Regular exercise and adequate nutrition are promoted as two key modifiable lifestyle factors that can optimize physical, functional, and cognitive health into old age. To date, the vast majority of research has focused on the independent effects of exercise and various nutritional factors on physical and/or cognitive function. However, combining exercise and nutritional approaches may provide additive or synergistic health benefits due to their similar cellular and molecular pathways, including the regulation of various growth and neurotrophic factors and the modulation of systemic inflammation. This chapter provides an overview of the independent and combined effects of exercise with various nutritional factors, specifically protein and dairy supplementation, vitamin D, fish oil and omega-3 fatty acids, creatine, antioxidant nutrients, and multi-nutrient supplements, on muscle mass, strength and functional performance, and cognitive function in older people.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Exercise
- Nutrition
- Supplementation
- Muscle mass
- Muscle strength
- Physical performance
- Cognitive function
- Older adults
Introduction
The 2015 World Health Organization (WHO) report on aging and health reported that “the health of older people is not keeping up with increasing longevity” and outlined a framework for action around the concept of functional ability to foster healthy aging [1]. By definition, functional ability is comprised of an individual’s intrinsic capacity, both physical and mental, as well as relevant environmental characteristics and their interactions [1]. It is well established that aging is associated with a loss in muscle mass, strength, power, and function, which has been linked to multiple chronic diseases as well as an increased risk for falls, frailty, disability, loss of independence, and reduced quality of life [2,3,4]. There is also evidence that dementia and related cognitive deficits that can occur with advancing age, particularly deficits in executive function including the ability to concentrate, attend selectively, multi-task, plan, and strategize, are key risk factors for falls [5]. Other cognitive abilities commonly shown to experience an age-related deterioration include working memory, episodic memory, processing speed, and attention, but the age of onset for the decline in these measures varies. Conversely, crystallized abilities and faculties acquired over a lifetime such as vocabulary, visuospatial ability, and procedural memory tend to display greater stability with aging [6]. With the exception of cognitive assessments designed to aid in the diagnosis of cognitive impairment related to dementia and other neurological conditions, there is currently no “gold standard” or standardized measures of cognitive function for use in research. Studies focused on exercise or dietary interventions tend to include a range of measures of individual cognitive domains (e.g., executive function, memory, attention), and it is recommended that a composite of individual measures be used to provide an index of global cognitive function [7].
Several overlapping mechanisms are currently proposed to contribute to both cognitive and functional impairments , which can lead to an increased risk for falls and frailty. For instance, chronic inflammation, insulin resistance, vascular risk factors, and hormonal changes are all relevant to both declines to brain health and physical function [8]. Recent data also indicate that low muscle mass and strength and accelerated losses in muscle mass are associated with cognitive impairment [9,10,11,12] and brain atrophy [13]. Similarly, poor gait performance and a decline in gait speed over time have been shown to be predictive of incident dementia [14, 15]. Collectively, these findings provide evidence to support a link between cognition and muscle mass and function, but questions still remain as to the direction of this relationship. It is possible that there is a bidirectional relationship: factors causing muscle or functional losses may contribute to impaired cognitive function, or factors leading to cognitive impairment may contribute to a decline in muscle health and function. Despite this, there is growing interest in identifying strategies that can simultaneously improve muscle and cognitive health to ensure that older people maintain their physical and cognitive functions in order to live an independent and relatively disease- and disability-free life.
Regular exercise and adequate nutrition are widely promoted as two key modifiable lifestyle factors that can optimize physical, functional, and cognitive health into old age. To date, the vast majority of research has focused on the independent effects of exercise and various nutritional factors on physical or cognitive function. Whether combining these two health-related behaviors can result in additive or synergistic health benefits to both muscle and cognitive functions remains uncertain. However, as illustrated in Fig. 8.1 and discussed throughout this chapter, there is a sound rationale to support the role of exercise and nutrition for improving both cognitive- and muscle-related outcomes. This chapter will provide a brief overview of the evidence related to the role of exercise and nutrition for optimizing muscle, mobility, and cognition in older adults, followed by a discussion on the latest research into whether various nutritional factors can enhance the effects of exercise on muscle health, functional ability, and cognitive function. The aim is not to provide a complete review of all the available literature and the underlying mechanisms but to provide an update on more recent randomized controlled trials (RCTs) in older adults which included both muscle and functional measures with cognition as outcomes.
Exercise to Optimize Muscle Health and Mobility in Older Adults
Regular exercise and physical activity have been consistently shown to have beneficial effects on a broad range of physical, functional, and cognitive measures in older people [16,17,18]. However, not all forms of exercise are equally effective, with the benefits being modality and intensity-dependent and reliant on adequate nutrition. For instance, progressive resistance training (PRT) has been shown to be effective for improving muscle mass, size, and strength in older adults and the frail elderly [19, 20], but there remains considerable uncertainty with regard to the effect of this mode of training on functional ability (e.g., balance, mobility, gait speed) and reducing falls in older people [17, 21]. This is likely related in part to the lack of training specificity, that is, most resistance training programs focus on slow and controlled movements to maximize muscle strength and not the ability to generate force quickly (termed muscle power) which is often needed for a rapid coordinated and dynamic response specific to many functional tasks (e.g., stepping quickly in response to a trip). Indeed, there is evidence that many common tasks of daily living are more strongly related to muscle power than muscle mass or maximal muscle strength [22]. Thus, targeted programs that are designed to optimize neuromuscular function and which are specific to tasks of daily living are likely to provide the greatest benefits.
High-velocity PRT or functional power training, which is characterized by rapid concentric movements or muscle contractions, is an alternative approach that has been shown to improve movement speed, muscle power, and functional performance in older adults [23]. In fact, there is evidence this mode of training is more effective than traditional PRT for improving physical performance [18], as well as “real-life” functional ability (e.g., car braking speed) in the elderly [24]. While the long-term effects of high-velocity training on falls remain unknown, the findings from a meta-analysis of seven RCTs indicated that volitional and reactive step training interventions involving quick, multidirectional stepping movements and weight transfers, which incorporate elements of functional muscle power, improved functional ability and reduced the rate of falls by 52% [rate ratio 0.48 (95% CI, 0.36–0.65)] in older people [17, 25]. It is noteworthy that the magnitude of the reduction in falls following step training interventions is greater than that reported in previous meta-analyses and a Cochrane collaboration for general exercise interventions (21–32% reduction in the rate of falls following general exercise training, multicomponent group and/or home-based exercise training) and more specific exercise combinations (39% falls reduction with challenging balance training and 3 or more hours of exercise training per week) [17, 26]. Collectively, these findings highlight that targeted multicomponent exercise programs incorporating high-velocity PRT, functional activities relevant to everyday tasks, and challenging balance activities are likely to provide the greatest benefits in terms of optimizing muscle mass, strength, power, and functional capacity and reducing falls risk in older people.
Exercise to Optimize Cognitive Function in Older Adults
There is mounting evidence from animal and human studies indicating that regular exercise can induce a cascade of neural and vascular adaptations which can improve brain structure, function, and/or neural connectivity through the promotion of neurogenesis, angiogenesis, and synaptic plasticity, the release of various growth and neurotrophic factors [e.g., insulin-like growth factor-1 (IGF-1) and brain-derived neurotrophic factor (BDNF)], and the modulation of systemic inflammation and oxidative stress (Fig. 8.1). While more detailed information is provided in several reviews [27, 28], additional mechanisms include exercise-related benefits to cardiovascular health and insulin sensitivity, which can have long-term effects on brain health and dementia risk later in life [29]. For instance, a study of over 3000 individuals above the age of 60 from the Framingham Study found that those within the lowest category of physical activity had a 1.5-fold increased 10-year risk of dementia incidence compared to those with higher levels of physical activity [30]. While these findings suggest that exercise might exert a neuroprotective effect on the aging brain, questions still remain as to whether there is an optimal type and dose of exercise that is needed to elicit cognitive benefits and/or prevent the progression to dementia. To date, a larger body of research has focused on aerobic training benefits to cognition than PRT or multicomponent programs. However, a systematic review and meta-analysis of 36 RCTs in community-dwelling adults aged 50 years and older reported that aerobic training, PRT, and the combination all had significant and similar effects on cognitive function (effect size, 0.24, 0.29, and 0.33, respectively), regardless of cognitive status [16]. However, moderator analysis revealed that moderate- to high-intensity (but not low intensity) training and a duration of at least 45 minutes were most effective [16].
There is also emerging data that functional training programs designed to prevent falls, including step training interventions [25] and dual-task cognitive-motor programs [31], whereby cognitive or motor tasks are performed sequentially or simultaneously with exercise training, can improve measures of cognitive function, including executive function, attention, and short-term memory. Moreover, the performance of functional tasks (e.g., stepping) and/or exercise in combination with a secondary task may be innately cognitively demanding as they require the engagement of executive processes (e.g., inhibition, planning, and execution of a rapid motor response in response to an external cue) and attentional aspects (e.g., distribution of attention between movement components). At present, the neurophysiological mechanisms underlying any cognitive improvements following combined cognitive and exercise training remain uncertain, but cognitive and exercise training may stimulate similar neurobiological processes which could produce a synergistic response (refer to Tait et al. [31] for a more detailed review). In this regard , a combination of physical exercise, sensorimotor stimulation, and cognitive engagement may also facilitate neurophysiological changes that contribute to wider cognitive benefits which may translate into physical or functional benefits. In part support of this notion, a 2017 review that included 19 studies found that interventions that adopted physical-cognitive training or multimodal programs were most effective for improving a range of physical, motor, and cognitive outcomes in older adults than single intervention programs [32]. Collectively, these findings suggests that exercise programs designed to optimize muscle mass and function and prevent falls in the elderly may also simultaneously improve cognitive health , but further study is needed to define whether there is an optimal type (or combination) and dose.
Nutritional Approaches to Optimize Muscle Health and Mobility in Older Adults
In a comprehensive review of the role of nutrition for the prevention and management of sarcopenia, Robinson et al. [33] highlighted that many epidemiologic and prospective cohort studies have shown that various nutritional factors (protein, vitamin D, antioxidant nutrients, omega-3 fatty acids), whole foods (dairy products), and dietary patterns (Mediterranean diet) can play a role in attenuating age-related losses in muscle mass and to a lesser extent muscle strength and/or function. However, the findings from several systematic reviews and meta-analyses of RCTs have shown that the effects of specific nutrients or supplements alone (without exercise) on muscle and functional outcomes in older adults are equivocal [34,35,36,37], with the exception of perhaps vitamin D that appears to have a small positive effect on muscle strength and function in older adults, particularly in those with low basal levels [38, 39]. While it has been suggested that the lack of any marked effects of various nutritional factors on muscle or mobility-related outcomes may be related to the low number of studies, short-term follow-up periods, and heterogeneous study designs [33], it is also likely that some of these trials were biologically flawed. For instance, many recruited healthy older people who were not functionally impaired, already had adequate intakes, and/or failed to provide a sufficient dose of a given nutrient to markedly increase levels above baseline or relative to controls. As a result of these limitations, many trials lacked the ability to detect any marked effects and were essentially designed to fail. In part support of this notion, a recent meta-analysis of RCTs in adults aged ≥ 55 years found no overall effect of dairy-based protein supplementation and vitamin D on muscle or functional measures, but there was a trend for a positive effect on lean body mass when supplemental doses of protein were ≥ 20 g per day or when given to (pre)frail or inactive older adults [40].
Nutritional Approaches to Optimize Cognitive Function in Older Adults
Several review articles have concluded that, based on evidence from epidemiologic studies and a limited number of RCTs, that certain dietary patterns or nutrients, including but not limited to the Mediterranean diet, omega-3 fatty acids, vitamin D, antioxidants, creatine, and B-vitamins, may be protective against cognitive decline and even the risk of incident dementia [41,42,43]. Albeit limited, there is also evidence that dietary protein and its constituent amino acids, particularly tryptophan and tyrosine, may provide some cognitive benefits [44]. Despite these findings, a meta-analysis of 24 nutritional RCTs (six using omega-3 fatty acids, seven using B-vitamins, three using vitamin E, eight using other interventions) in non-demented middle-aged and older adults [45] and a systematic review of randomized, double-blinded controlled trials of nutraceuticals and dietary supplements of at least 1-year duration and with at least 100 participants aged ≥65 years [46] both reported no consistent evidence to support any beneficial effects of nutrition on cognition. This may be related to a number of factors, including the health status of participants and the lack of sensitivity of certain cognitive measures to detect subtle changes over time. While it is clear that further long-term and adequately powered RCTs in suitable populations are still needed, given that multiple lifestyle factors (as well as environment and genetic factors) have been implicated with cognitive related disorders, it is likely that the greatest benefits on cognition (and muscle health and functional ability) will occur with a targeted exercise program combined with a nutritional intervention.
Effect of Nutrition Combined with Exercise on Muscle, Mobility, and Cognition in Older Adults
As illustrated in Fig. 8.1, from a mechanistic perspective, there is a sound rationale to support an interactive effect of exercise and nutrition on both muscle and cognitive functions. For instance, animal and human studies have reported that both exercise and various nutritional factors can influence various growth and neurotrophic factors [e.g., IGF-1, BDNF, and vascular endothelial growth factors (VEGF)] as well as modulate various inflammatory markers, all of which have been implicated with muscle and cognitive/brain health [27, 28]. A more comprehensive review of the potential underlying mechanisms by which exercise and nutrition may enhance cognitive function is provided in several excellent reviews [28, 47, 48]. The focus of this chapter is to briefly review the latest evidence from RCTs addressing whether various nutritional factors, specifically protein and dairy-based supplementation, vitamin D, fish oil, and omega-3 fatty acids, creatine, antioxidant nutrients, and multi-nutrient supplements, can enhance the effects of exercise on muscle health and/or function and cognition in older adults.
Protein or Dairy Supplementation with Exercise
Over the past decade , there have been equivocal findings from many intervention trials and meta-analyses of RCTs investigating the combined effects of exercise with different types of protein, essential amino acids, β-hydroxy-β-methylbutyrate (HMB), or dairy food supplements, on muscle mass, strength, and function in older adults. This is highlighted in a 2017 systematic review of combined exercise and nutrition interventions in adults aged 60 years and over which reported that only 25% (3/12) of protein supplementation (including dairy, whey, meat, collagen peptide) trials and 0 (0/3) to 33% (1/3) of essential amino acids or HMB trials detected a significant additive effect on muscle mass or strength; none of the trials observed an added benefit on physical performance [49] (Table 8.1). The lack of a consistent effect may be due to a range of factors, including differences in the type and dose of protein/dairy prescribed; differences in the timing of consumption, compliance, spread, and/or pattern of intake; as well as heterogeneity in the cohorts studied (age, physical and nutritional status, current activity levels), study duration, and the type and dose of exercise prescribed [50]. Nevertheless, it is likely that the greatest benefits will be apparent in high-risk individuals (e.g., frail or sarcopenic) who have inadequate dietary intakes (e.g., protein intake below the recommended level of 0.8–1.0 g/kg/d).
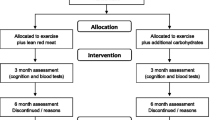
With regard to whether additional protein can enhance the effects of exercise on cognitive function in older adults, we are aware of only two published trials [51, 52]. In a 24-week RCT in 62 frail elderly people aged 65 years and over, neither twice weekly PRT alone nor with protein supplementation (2 × 15 g milk protein concentrate per day) improved cognitive function [assessed via the Mini-Mental State Examination (MMSE)], despite a greater gain in lean mass in the PRT plus protein group [51]. The same group then combined the findings from the above study with a parallel run protein (2 × 15 g/d milk protein concentrate) versus placebo supplementation trial in frail and pre-frail adults and reported that there were no exercise-protein interactions on a larger battery of cognitive tests [51, 52]. However, they did find that PRT plus protein improved information processing speed compared to protein supplementation alone, but surprisingly protein supplementation improved verbal fluency compared to exercise plus protein. Given that cognition was a secondary outcome in both these trials and neither was adequately powered to detect an interactive effect, these findings must be interpreted with caution and highlight the need for further well-designed , long-term trials.
Vitamin D Supplementation with Exercise
Exercise and vitamin D supplementation have been independently shown to improve muscle strength and function, and thus it has been hypothesized that there might be an additive effect when combining these two approaches. However, the findings from a meta-analysis of seven trials (792 participants aged ≥65 years) reported that there were no additive benefits of combined exercise (predominantly PRT) and vitamin D (this included studies using vitamin D and calcium supplementation or fortified milk) on muscle function in older adults, but there was a trend for a greater improvement in muscle strength [53]. The lack of a consistent additive effect is likely related to the marked heterogeneity with regard to the study durations (12 weeks to 24 months), dose of vitamin D prescribed (400–1920 IU/d), basal serum 25(OH)D concentrations, differences in the exercise regimens, and/or study methodology (e.g., functional measures) [53]. To our knowledge, there are no published intervention trials which have investigated whether exercise combined with vitamin D supplementation alone can improve cognitive function in older people. However, in a 2-year factorial design RCT in healthy older women aged 70–80 years which was designed to examine the independent and combined effects of exercise (functional balance and weight-bearing exercise and resistance training) and vitamin D (800 IU/d) supplementation on falls and muscle function, Uusi-Rasi et al. reported that there was no effect of the intervention on cognitive function [assessed by the Mini-Mental State Examination (MMSE) , a brief screening measure for cognitive impairment] (personal communication). This is likely due to the inclusion of healthy women with adequate basal vitamin D levels [mean 25(OH)D ~67 nmol/L] who were cognitively intact (mean baseline MMSE scores were at the upper range, 28/30) and the use of the MMSE tool which may not be sensitive to subtle changes that can occur across specific cognitive domains [54].
Fish Oil and Omega-3 Supplementation with Exercise
Several short-term trials have reported that fish oil and omega-3 fatty acid supplementation may enhance the effects of PRT on muscle mass and strength in older adults [55, 56]. For instance, a study in 45 women (mean age 64 years) randomized to PRT alone for 90 days or PRT plus fish oil supplementation (2 g/d for 90 days or 2/d for 60 days before training followed by 2 g/d for 90 days) found that there were additive benefits on lower limb muscle strength (peak torque and chair rising time), but not muscle function; neither muscle mass nor cognition were assessed [56]. Several observational studies have indicated that a low omega-3 to omega-6 polyunsaturated fatty acid (PUFA) ratio may be protective against cognitive decline and dementia [57] and predict better cognitive function in healthy older people [58]. However, excess consumption of omega-6 PUFA, which is common among a Western dietary pattern, may adversely impact cognition by depleting docosahexaenoic acid (DHA), the omega-3 PUFA most prevalent in the brain [59]. Despite the rationale for increasing omega-3 intake, data from the 3-year randomized, placebo-controlled Multi-domain Alzheimer Prevention Trial (MAPT) in 1680 community-dwelling, non-demented adults aged 70+ years with either memory complaints, limitations with one instrumental activities of daily living, or slow gait speed reported that there were no significant effects of omega-3 fatty acid supplementation [800 mg/d (DHA) and 250 mg/d eicosapentaenoic acid (EPA)] and a multi-domain intervention (cognitive training, physical activity and nutrition advice, and three preventative consultations), alone or in combination, compared with placebo on cognitive (primary outcome) and physical (secondary outcome) function [short physical performance battery (SPPB)] [60] (Fig. 8.2). However, the combination of omega-3 fatty acids and the multi-domain intervention was found to enhance cognitive performance on a secondary measure of cognitive function. The lack of an effect, particularly on physical function, may be related in part to the fact that participants only received generic physical activity advice to be more active (e.g., walk 30 min per day) and not a targeted program designed to enhance functional capacity. Furthermore, exploratory subgroup analyses showed that the combined intervention arms or the multi-domain intervention alone may help to slow cognitive decline in those most at risk (e.g., those with an increased dementia risk score and those with evidence of brain amyloid pathology), but there was no evidence of any beneficial effects on functional capacity with the per protocol analysis (excluding non-compliers). Based on the above findings, it appears that omega-3 fatty acids do not enhance the effects of exercise on functional ability in healthy older people or those with impaired function, but there may be some added benefits to muscle mass and strength and cognitive function.
Mean changes (with 95% confidence intervals) after 3 years in global cognitive function and the short physical performance battery in participants (aged 70 years and older) enrolled in the Multi-domain Alzheimer Preventive Trial (MAPT) who were randomized to the multi-domain (MD) and polyunsaturated fatty acid supplementation (PUFA) group alone or in combination or placebo [60]. Error bar represents 95% confidence intervals
Creatine Supplementation with Exercise
As highlighted in Table 8.1, there are a number of RCTs which have shown that creatine supplementation is an effective approach to enhance the effects of exercise on muscle mass and strength (4/5 studies showed improvements) in older adults and to a lesser extent muscle function (only one of four studies reported an additive effect on physical performance) [49]. Further to its anabolic skeletal muscle effects, there is some evidence that creatine supplementation may improve cognitive function [61]. However, to our knowledge there is only one trial which has investigated whether creatine can enhance the effects of exercise on measures of cognition and muscle strength [62]. In a 24-week factorial design, double-blind, placebo-controlled RCT in 56 healthy older women aged 60–80 years, Alves et al. [62] reported that neither twice weekly PRT nor creatine supplementation (4 × 5 g/d for 5 days followed by 5 g/d) alone or in combination improved any measure of cognitive function, and there was no additive benefit of creatine on muscle strength. However, given the small sample size and the inclusion of healthy older women in this study, these findings must be interpreted with caution and highlight the need for further adequately powered trials in at-risk cohorts (e.g., those with cognitive and/or functional impairment).
Antioxidant Nutrients with Exercise
Aging is associated with a steady increase in oxidative stress (free radical production that can induce cell damage) that has been implicated in many chronic diseases, including sarcopenia and cognitive impairment. While regular exercise and various antioxidant nutrients (e.g., vitamins A, C, and E, selenium, and carotenoids) are reported to protect older people from oxidative stress, whether single antioxidant supplements or a combination can prevent muscle and cognitive decline remains uncertain [33]. At present, there are also conflicting findings from the limited trials available on the combined effects of antioxidant supplementation with exercise on muscle mass, strength, and/or function. For instance, a 6-month factorial design RCT in 57 healthy adults aged 59–73 years found that high-intensity PRT combined with vitamin C (1000 mg/d) and E (600 mg/d) supplementation significantly increased muscle mass (fat-free mass), but not muscle strength, in older adults [63]. In contrast, 6 months of vitamin E supplementation (900 IU/d) had no additive effects beyond aerobic training (walking) on physical function in 57 sedentary older adults [64]. Moreover, a 12-week trial in 34 elderly men aged 60–81 years found that vitamin C (1000 mg/d) and E (235 mg/d) supplementation attenuated PRT-induced gains in total lean mass and leg muscle thickness, but not muscle strength [65]. This suggests that antioxidants may blunt the anabolic skeletal muscle effects of PRT, but given the small sample size and short-term nature of this trial, further studies are needed to investigate this intriguing finding.
With regard to the effects of exercise and antioxidant supplementation on brain/cognitive health, we were unable to identify any long-term human RCTs that had been conducted in older adults. However, a narrative review on the effects of exercise with antioxidant supplementation (specifically vitamin C and E) on brain and/or cognitive function and related biomarkers highlighted that there are contrasting results from the limited number of animal and human studies that have been conducted [66]. For instance, some studies have reported an additive beneficial effect, while others reported no effects or a negative response in which antioxidants may block the beneficial effects of exercise [66]. Clearly this is an area that requires further study.
Multi-nutrient Supplements with Exercise
Since a number of different nutrients have been associated with exercise-induced gains in muscle health and/or cognitive function, there has been interest in whether multi-nutrient supplements (e.g., various combinations of protein, amino acids, vitamin D, calcium, creatine, omega-3 fatty acids, and/or other vitamins and/or minerals) can provide additive benefits to exercise on muscle and to a lesser extent cognitive function. Of the trials included in the systematic review by Beaudart et al. [49], there was little evidence of any additive benefits with multi-nutrient supplementation on muscle mass (0 of 4 trials), muscle strength (1 of 5 trials), or physical performance (0 of 4 trials) (Table 8.1). While the authors acknowledged that the majority of studies were poor quality (graded on the Jadad scale), a number of more recent well-designed trials have observed conflicting findings with regard to the combined effects of exercise with multi-nutrient supplements on muscle outcomes in older adults (mean age ≥65 years) [67,68,69,70]. For instance, 12 weeks of a daily nutritional supplement (whey protein, essential amino acids, vitamin D, and other minerals) with exercise (5/week of muscle strengthening and balance training) led to greater gains in fat-free mass, handgrip strength, and physical functioning compared to exercise alone in sarcopenic older men and women [70]. The positive findings in this study are likely due in part to the fact that participants were screened from hospitalized patients with evidence of malnutrition. In contrast to these findings, the provision of a daily multi-nutrient drink (whey protein, vitamin D, calcium, and an assortment of other vitamins and minerals) for 24 weeks did not enhance the effects of exercise (3/week of walking, lower limb strength, balance, and flexibility exercises) on physical function (400 m walk or SPPB), muscle strength, or power in 149 adults aged 70 years and over with mobility limitations (SPPB ≤9) and low vitamin D status (25OHD ≥9 and ≤24 ng/ml) [68, 71]. However, nutritional supplementation was associated with a greater reduction in thigh intermuscular fat, which is important given that increased muscle fat infiltration has been associated with both metabolic and muscular dysfunctions [72]. While many of the above trials did include a measure of cognition (e.g., MMSE) as part of the baseline assessment, changes in response to the intervention were not assessed (or reported), but given that most studies included cognitively intact older adults and were relatively short-term (12 weeks to 6 months), it is likely that any potential benefits on cognition would be modest.
There have been a number of recent multi-domain intervention trials incorporating exercise training, nutritional supplementation, cognitive training, medication review, and/or vascular risk monitoring, which have quantified changes in both cognitive and physical functions in older adults [73, 74]. In a 12-week multi-domain intervention involving twice weekly strength/balance training with a daily protein nutritional supplement for 6 weeks, twice weekly memory workshops for 6 weeks, and medication review in 352 pre-frail/frail elderly people (mean age 77 years), Romera-Liebana et al. [73] reported that there were significant improvements in both functional and cognitive performance measures relative to usual care controls, despite relatively poor adherence to both the exercise and memory training sessions (mean adherence 54%). Furthermore, many of the functional and cognitive benefits were maintained up to 18 months, despite the intervention ceasing after 3 months. While it is difficult to explain these findings given the short-term nature (6 weeks) and modest adherence to the intervention, it is possible that the positive findings are related to the inclusion of a high-risk cohort of elderly people (e.g., 75% were classified as frail).
To our knowledge, the 2-year Finnish Geriatric Intervention Study (FINGER) is the largest multi-domain intervention trial in older adults with cognition as the primary outcome and functional performance as a secondary outcome. In this study, 1260 community-dwelling older people aged 60–77 with risk factors for dementia were randomized to an intensive multi-domain intervention (described below) or regular health advice (oral and written information regarding strategies to maintain a healthy diet, physical and social activities, and management of vascular factors and disability prevention) [74]. The multi-domain intervention incorporated four components: (1) individual and group nutrition sessions in which participants were advised to consume a diet with 10–20% of daily energy from proteins, 25–35% from fat [<10% from saturated plus trans-fatty acids, 10–20% from monounsaturated fatty acids, 5–10% from polyunsaturated fatty acids (including 2.5–3.0 g/day omega-3 fatty acids)], 45–55% from carbohydrates (<10% refined sugar), 25–35 g/day dietary fiber, <5 g/day salt, and < 5% from alcohol, (2) individually tailored PRT (one to three times a week) in combination with aerobic training (two to five times a week) and postural exercises, (3) group and individual computer-based cognitive training, and (4) social interactions (group meetings). The main finding from this trial was that the multi-domain intervention was associated with significantly greater improvements to global cognitive function, executive function, and processing speed compared to regular health advice. Improvements to cognition were in the magnitude of 25–150% greater than the control group. In contrast, there was no effect of the intervention on physical performance (assessed via SPPB) [74]. It is difficult to explain this latter finding given that 76–83% of participants reported completing the resistance or aerobic exercise one or more times per week and the programs did include exercises to improve postural balance. One possible explanation for the lack of any functional benefits is that the participants included were not functionally impaired and were relatively active (e.g., >70% reported being active two or more times per week). Based on these findings, further trials are needed to explore the optimal multi-domain approach that can improve both cognitive and physical performance measures in older adults and whether this ultimately translates into a reduction in the incidence of dementia, sarcopenia, and falls.
Conclusion
In summary, there is strong evidence that targeted and progressive exercise programs, particularly multicomponent interventions incorporating resistance training, functional activities relevant to everyday tasks (e.g., rapid stepping), and challenging balance training, can improve muscle mass, strength, power, and function and reduce falls risk in older people. Whether this translates into a reduction in fracture risk remains unknown. While there is also emerging evidence that the above modes of training, along with aerobic exercise, can improve measures of cognitive function, questions still remain with regard to the optimal dose (intensity, duration, and frequency). In contrast, there is little evidence from RCTs to support the role of individual or a combination of nutrients as an effective approach to improve muscle health, functional performance, or cognition in healthy older adults. There is, however, some evidence showing that various nutritional factors can improve muscle mass and/or strength in the elderly at risk (e.g., those with functional impairment, frailty, sarcopenia, or malnutrition), but the greatest benefits are likely to be achieved with exercise. Currently, however, the vast majority of intervention trials which have investigated whether individual nutrients or multi-nutrient supplements can enhance the effects of exercise on measures of muscle mass, strength, and function and/or cognition have produced negative findings. While this is likely due to the fact that most studies included relatively healthy older adults who did not present with nutritional deficiency, many of these studies were also not designed nor powered to detect improvements in muscle, functional, and cognitive measures. Given the emerging link between muscle mass, strength, and function with brain health and cognitive function and subsequent disease risk (e.g., dementia and falls), there is a need for further long-term, well-designed, and appropriately powered intervention trials to evaluate the combined effects of exercise and nutrition, including dietary approaches (e.g., Mediterranean diet), on muscle, mind, and mobility outcomes in the elderly.
References
World Health Organisation. World report on ageing and health. Geneva; 2015.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. 2010;39(4):412–23.
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, Abellan van Kan G, Andrieu S, Bauer J, Breuille D, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–56.
Scott D, Daly RM, Sanders KM, Ebeling PR. Fall and fracture risk in sarcopenia and dynapenia with and without obesity: the role of lifestyle interventions. Curr Osteoporos Rep. 2015;13(4):235–44.
Hsu CL, Nagamatsu LS, Davis JC, Liu-Ambrose T. Examining the relationship between specific cognitive processes and falls risk in older adults: a systematic review. Osteoporos Int. 2012;23(10):2409–24.
Harada CN, Natelson Love MC, Triebel KL. Normal cognitive aging. Clin Geriatr Med. 2013;29(4):737–52.
Posner H, Curiel R, Edgar C, Hendrix S, Liu E, Loewenstein DA, Morrison G, Shinobu L, Wesnes K, Harvey PD. Outcomes assessment in clinical trials of Alzheimer’s disease and its precursors: readying for short-term and long-term clinical trial needs. Innov Clin Neurosci. 2017;14(1–2):22–9.
Halil M, Cemal Kizilarslanoglu M, Emin Kuyumcu M, Yesil Y, Cruz Jentoft AJ. Cognitive aspects of frailty: mechanisms behind the link between frailty and cognitive impairment. J Nutr Health Aging. 2015;19(3):276–83.
Boyle PA, Buchman AS, Wilson RS, Leurgans SE, Bennett DA. Association of muscle strength with the risk of Alzheimer disease and the rate of cognitive decline in community-dwelling older persons. Arch Neurol. 2009;66(11):1339–44.
Hsu YH, Liang CK, Chou MY, Liao MC, Lin YT, Chen LK, Lo YK. Association of cognitive impairment, depressive symptoms and sarcopenia among healthy older men in the veterans retirement community in southern Taiwan: a cross-sectional study. Geriatr Gerontol Int. 2014;14(Suppl 1):102–8.
Nourhashemi F, Andrieu S, Gillette-Guyonnet S, Reynish E, Albarede JL, Grandjean H, Vellas B. Is there a relationship between fat-free soft tissue mass and low cognitive function? Results from a study of 7,105 women. J Am Geriatr Soc. 2002;50(11):1796–801.
Tolea MI, Galvin JE. Sarcopenia and impairment in cognitive and physical performance. Clin Interv Aging. 2015;10:663–71.
Burns JM, Johnson DK, Watts A, Swerdlow RH, Brooks WM. Reduced lean mass in early Alzheimer disease and its association with brain atrophy. Arch Neurol. 2010;67(4):428–33.
Beauchet O, Annweiler C, Callisaya ML, De Cock AM, Helbostad JL, Kressig RW, Srikanth V, Steinmetz JP, Blumen HM, Verghese J, et al. Poor gait performance and prediction of dementia: results from a meta-analysis. J Am Med Dir Assoc. 2016;17(6):482–90.
Dumurgier J, Artaud F, Touraine C, Rouaud O, Tavernier B, Dufouil C, Singh-Manoux A, Tzourio C, Elbaz A. Gait speed and decline in gait speed as predictors of incident dementia. J Gerontol A Biol Sci Med Sci. 2017;72(5):655–61.
Northey JM, Cherbuin N, Pumpa KL, Smee DJ, Rattray B. Exercise interventions for cognitive function in adults older than 50: a systematic review with meta-analysis. Br J Sports Med. 2018;52(3):154–60.
Sherrington C, Michaleff ZA, Fairhall N, Paul SS, Tiedemann A, Whitney J, Cumming RG, Herbert RD, Close JCT, Lord SR. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51(24):1750–8.
Steib S, Schoene D, Pfeifer K. Dose-response relationship of resistance training in older adults: a meta-analysis. Med Sci Sports Exerc. 2010;42(5):902–14.
Borde R, Hortobagyi T, Granacher U. Dose-response relationships of resistance training in healthy old adults: a systematic review and meta-analysis. Sports Med. 2015;45(12):1693–720.
Stewart VH, Saunders DH, Greig CA. Responsiveness of muscle size and strength to physical training in very elderly people: a systematic review. Scand J Med Sci Sports. 2014;24(1):e1–10.
Latham NK, Bennett DA, Stretton CM, Anderson CS. Systematic review of progressive resistance strength training in older adults. J Gerontol A Biol Sci Med Sci. 2004;59(1):48–61.
Bean JF, Kiely DK, Herman S, Leveille SG, Mizer K, Frontera WR, Fielding RA. The relationship between leg power and physical performance in mobility-limited older people. J Am Geriatr Soc. 2002;50(3):461–7.
Reid KF, Fielding RA. Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev. 2012;40(1):4–12.
Sayers SP, Gibson K. Effects of high-speed power training on muscle performance and braking speed in older adults. J Aging Res. 2012;2012:426278.
Okubo Y, Schoene D, Lord SR. Step training improves reaction time, gait and balance and reduces falls in older people: a systematic review and meta-analysis. Br J Sports Med. 2017;51(7):586–93.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146.
Cotman CW, Berchtold NC, Christie LA. Exercise builds brain health: key roles of growth factor cascades and inflammation. Trends Neurosci. 2007;30(9):464–72.
Meeusen R. Exercise, nutrition and the brain. Sports Med. 2014;44(Suppl 1):S47–56.
Kennedy G, Hardman RJ, Macpherson H, Scholey AB, Pipingas A. How does exercise reduce the rate of age-associated cognitive decline? A review of potential mechanisms. J Alzheimers Dis. 2017;55(1):1–18.
Tan ZS, Spartano NL, Beiser AS, DeCarli C, Auerbach SH, Vasan RS, Seshadri S. Physical activity, brain volume, and dementia risk: the Framingham study. J Gerontol A Biol Sci Med Sci. 2017;72(6):789–95.
Tait JL, Duckham RL, Milte CM, Main LC, Daly RM. Influence of sequential vs. simultaneous dual-task exercise training on cognitive function in older adults. Front Aging Neurosci. 2017;9:368.
Levin O, Netz Y, Ziv G. The beneficial effects of different types of exercise interventions on motor and cognitive functions in older age: a systematic review. Eur Rev Aging Phys Act. 2017;14:20.
Robinson SM, Reginster JY, Rizzoli R, Shaw SC, Kanis JA, Bautmans I, Bischoff-Ferrari H, Bruyere O, Cesari M, Dawson-Hughes B, et al. Does nutrition play a role in the prevention and management of sarcopenia? Clin Nutr. 2017;37(4):1121–32. pii: S0261-5614(17)30299-6.
Beaudart C, Rabenda V, Simmons M, Geerinck A, Araujo De Carvalho I, Reginster JY, Amuthavalli Thiyagarajan J, Bruyere O. Effects of protein, essential amino acids, B-Hydroxy B-Methylbutyrate, creatine, dehydroepiandrosterone and fatty acid supplementation on muscle mass, muscle strength and physical performance in older people aged 60 years and over. A systematic review on the literature. J Nutr Health Aging. 2018;22(1):117–30.
Cruz-Jentoft AJ, Landi F, Schneider SM, Zuniga C, Arai H, Boirie Y, Chen LK, Fielding RA, Martin FC, Michel JP, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the international sarcopenia initiative (EWGSOP and IWGS). Age Ageing. 2014;43(6):748–59.
Nowson CA, Service C, Appleton J, Grieger JA. The impact of dietary factors on indices of chronic disease in older people: a systematic review. J Nutr Health Aging. 2018;22(2):282–96.
Mithal A, Bonjour JP, Boonen S, Burckhardt P, Degens H, El Hajj Fuleihan G, Josse R, Lips P, Morales Torres J, Rizzoli R, et al. Impact of nutrition on muscle mass, strength, and performance in older adults. Osteoporos Int. 2013;24(5):1555–66.
Beaudart C, Buckinx F, Rabenda V, Gillain S, Cavalier E, Slomian J, Petermans J, Reginster JY, Bruyere O. The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: a systematic review and meta-analysis of randomized controlled trials. J Clin Endocrinol Metab. 2014;99(11):4336–45.
Muir SW, Montero-Odasso M. Effect of vitamin D supplementation on muscle strength, gait and balance in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2011;59(12):2291–300.
Dewansingh P, Melse-Boonstra A, Krijnen WP, van der Schans CP, Jager-Wittenaar H, van den Heuvel E. Supplemental protein from dairy products increases body weight and vitamin D improves physical performance in older adults: a systematic review and meta-analysis. Nutr Res. 2018;49:1–22.
Vauzour D, Camprubi-Robles M, Miquel-Kergoat S, Andres-Lacueva C, Banati D, Barberger-Gateau P, Bowman GL, Caberlotto L, Clarke R, Hogervorst E, et al. Nutrition for the ageing brain: towards evidence for an optimal diet. Ageing Res Rev. 2017;35:222–40.
Moore K, Hughes CF, Ward M, Hoey L, McNulty H. Diet, nutrition and the ageing brain: current evidence and new directions. Proc Nutr Soc. 2018;77(2):1–12.
Hardman RJ, Kennedy G, Macpherson H, Scholey AB, Pipingas A. Adherence to a Mediterranean-style diet and effects on cognition in adults: a qualitative evaluation and systematic review of longitudinal and prospective trials. Front Nutr. 2016;3:22.
van de Rest O, van der Zwaluw NL, de Groot LC. Literature review on the role of dietary protein and amino acids in cognitive functioning and cognitive decline. Amino Acids. 2013;45(5):1035–45.
Forbes SC, Holroyd-Leduc JM, Poulin MJ, Hogan DB. Effect of nutrients, dietary supplements and vitamins on cognition: a systematic review and meta-analysis of randomized controlled trials. Can Geriatr J. 2015;18(4):231–45.
D’Cunha NM, Georgousopoulou EN, Dadigamuwage L, Kellett J, Panagiotakos DB, Thomas J, McKune AJ, Mellor DD, Naumovski N. Effect of long-term nutraceutical and dietary supplement use on cognition in the elderly: a 10-year systematic review of randomised controlled trials. Br J Nutr. 2018;119(3):280–98.
Barha CK, Galea LA, Nagamatsu LS, Erickson KI, Liu-Ambrose T. Personalising exercise recommendations for brain health: considerations and future directions. Br J Sports Med. 2017;51(8):636–9.
Gomez-Pinilla F. Brain foods: the effects of nutrients on brain function. Nat Rev Neurosci. 2008;9(7):568–78.
Beaudart C, Dawson A, Shaw SC, Harvey NC, Kanis JA, Binkley N, Reginster JY, Chapurlat R, Chan DC, Bruyere O, et al. Nutrition and physical activity in the prevention and treatment of sarcopenia: systematic review. Osteoporos Int. 2017;28(6):1817–33.
Daly RM. Dietary protein, exercise and skeletal muscle: is there a synergistic effect in older adults and the elderly? In: Weaver CM, Daly RM, Bischoff Ferrari HA, editors. Nutritional influences on bone health: 9th international symposium. Basel: Springer; 2016. p. 63–78.
Tieland M, Dirks ML, van der Zwaluw N, Verdijk LB, van de Rest O, de Groot LC, van Loon LJ. Protein supplementation increases muscle mass gain during prolonged resistance-type exercise training in frail elderly people: a randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc. 2012;13(8):713–9.
van de Rest O, van der Zwaluw NL, Tieland M, Adam JJ, Hiddink GJ, van Loon LJ, de Groot LC. Effect of resistance-type exercise training with or without protein supplementation on cognitive functioning in frail and pre-frail elderly: secondary analysis of a randomized, double-blind, placebo-controlled trial. Mech Ageing Dev. 2014;136-137:85–93.
Antoniak AE, Greig CA. The effect of combined resistance exercise training and vitamin D3 supplementation on musculoskeletal health and function in older adults: a systematic review and meta-analysis. BMJ Open. 2017;7(7):e014619.
Uusi-Rasi K, Patil R, Karinkanta S, Kannus P, Tokola K, Lamberg-Allardt C, Sievanen H. Exercise and vitamin D in fall prevention among older women: a randomized clinical trial. JAMA Intern Med. 2015;175(5):703–11.
Da Boit M, Sibson R, Sivasubramaniam S, Meakin JR, Greig CA, Aspden RM, Thies F, Jeromson S, Hamilton DL, Speakman JR, et al. Sex differences in the effect of fish-oil supplementation on the adaptive response to resistance exercise training in older people: a randomized controlled trial. Am J Clin Nutr. 2017;105(1):151–8.
Rodacki CL, Rodacki AL, Pereira G, Naliwaiko K, Coelho I, Pequito D, Fernandes LC. Fish-oil supplementation enhances the effects of strength training in elderly women. Am J Clin Nutr. 2012;95(2):428–36.
Loef M, Walach H. The omega-6/omega-3 ratio and dementia or cognitive decline: a systematic review on human studies and biological evidence. J Nutr Gerontol Geriatr. 2013;32(1):1–23.
Andruchow ND, Konishi K, Shatenstein B, Bohbot VD. A lower ratio of omega-6 to omega-3 fatty acids predicts better hippocampus-dependent spatial memory and cognitive status in older adults. Neuropsychology. 2017;31(7):724–34.
Sheppard KW, Cheatham CL. Omega-6 to omega-3 fatty acid ratio and higher-order cognitive functions in 7- to 9-y-olds: a cross-sectional study. Am J Clin Nutr. 2013;98(3):659–67.
Andrieu S, Guyonnet S, Coley N, Cantet C, Bonnefoy M, Bordes S, Bories L, Cufi MN, Dantoine T, Dartigues JF, et al. Effect of long-term omega 3 polyunsaturated fatty acid supplementation with or without multidomain intervention on cognitive function in elderly adults with memory complaints (MAPT): a randomised, placebo-controlled trial. Lancet Neurol. 2017;16(5):377–89.
Gualano B, Rawson ES, Candow DG, Chilibeck PD. Creatine supplementation in the aging population: effects on skeletal muscle, bone and brain. Amino Acids. 2016;48(8):1793–805.
Alves CR, Merege Filho CA, Benatti FB, Brucki S, Pereira RM, de Sa Pinto AL, Lima FR, Roschel H, Gualano B. Creatine supplementation associated or not with strength training upon emotional and cognitive measures in older women: a randomized double-blind study. PLoS One. 2013;8(10):e76301.
Bobeuf F, Labonte M, Dionne IJ, Khalil A. Combined effect of antioxidant supplementation and resistance training on oxidative stress markers, muscle and body composition in an elderly population. J Nutr Health Aging. 2011;15(10):883–9.
Nalbant O, Toktas N, Toraman NF, Ogus C, Aydin H, Kacar C, Ozkaya YG. Vitamin E and aerobic exercise: effects on physical performance in older adults. Aging Clin Exp Res. 2009;21(2):111–21.
Bjornsen T, Salvesen S, Berntsen S, Hetlelid KJ, Stea TH, Lohne-Seiler H, Rohde G, Haraldstad K, Raastad T, Kopp U, et al. Vitamin C and E supplementation blunts increases in total lean body mass in elderly men after strength training. Scand J Med Sci Sports. 2016;26(7):755–63.
Mock JT, Chaudhari K, Sidhu A, Sumien N. The influence of vitamins E and C and exercise on brain aging. Exp Gerontol. 2017;94:69–72.
Ng TP, Feng L, Nyunt MS, Feng L, Niti M, Tan BY, Chan G, Khoo SA, Chan SM, Yap P, et al. Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: a randomized controlled trial. Am J Med. 2015;128(11):1225–36. e1221
Fielding RA, Travison TG, Kirn DR, Koochek A, Reid KF, von Berens A, Zhu H, Folta SC, Sacheck JM, Nelson ME, et al. Effect of structured physical activity and nutritional supplementation on physical function in mobility-limited older adults: results from the VIVE2 randomized trial. J Nutr Health Aging. 2017;21(9):936–42.
Bell KE, Snijders T, Zulyniak M, Kumbhare D, Parise G, Chabowski A, Phillips SM. A whey protein-based multi-ingredient nutritional supplement stimulates gains in lean body mass and strength in healthy older men: a randomized controlled trial. PLoS One. 2017;12(7):e0181387.
Rondanelli M, Klersy C, Terracol G, Talluri J, Maugeri R, Guido D, Faliva MA, Solerte BS, Fioravanti M, Lukaski H, et al. Whey protein, amino acids, and vitamin D supplementation with physical activity increases fat-free mass and strength, functionality, and quality of life and decreases inflammation in sarcopenic elderly. Am J Clin Nutr. 2016;103(3):830–40.
Englund DA, Kirn DR, Koochek A, Zhu H, Travison TG, Reid KF, von Berens A, Melin M, Cederholm T, Gustafsson T, et al. Nutritional supplementation with physical activity improves muscle composition in mobility-limited older adults, the VIVE2 study: a randomized, double-blind, placebo-controlled trial. J Gerontol A Biol Sci Med Sci. 2017;73(1):95–101.
Addison O, Marcus RL, Lastayo PC, Ryan AS. Intermuscular fat: a review of the consequences and causes. Int J Endocrinol. 2014;2014:309570.
Romera-Liebana L, Orfila F, Segura JM, Real J, Fabra ML, Moller M, Lancho S, Ramirez A, Marti N, Cullell M et al. Effects of a primary-care based multifactorial intervention on physical and cognitive function in frail, elderly individuals: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2018. doi:https://doi.org/10.1093/gerona/glx259.
Ngandu T, Lehtisalo J, Solomon A, Levalahti E, Ahtiluoto S, Antikainen R, Backman L, Hanninen T, Jula A, Laatikainen T, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385(9984):2255–63.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Daly, R.M., Formica, M.B., Tait, J.L., Macpherson, H. (2019). Nutrition and Exercise Approaches to Enhance Muscle, Mobility, and Cognition During Aging. In: Weaver, C., Bischoff-Ferrari, H., Daly, R., Wong, MS. (eds) Nutritional Influences on Bone Health. Springer, Cham. https://doi.org/10.1007/978-3-319-98464-3_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-98464-3_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98463-6
Online ISBN: 978-3-319-98464-3
eBook Packages: MedicineMedicine (R0)