Abstract
There are several treatment alternatives, especially for the treatment of high-energy complex pilon fractures. None of these methods can be claimed as a gold standard. Infection is commonly observed after internal fixation. The external circular Ilizarov fixator allows the patient being operated on early after the trauma and being mobilized. Fifty-three patients were treated at our clinic between 2010 and 2014 using the Ilizarov method due to tibia pilon fractures. The patients included 40 males and 13 females. Mean age was 45.3 years (range = 23–62 years). High-energy trauma such as traffic accidents and falls from a height was involved in more than 80% of the patients. Mean union duration was 14.6 months (12–22 months). According to the Mazur criteria, 39 patients (74%) sustained very good or good results. In 10 patients (19%) sufficient results were obtained, while in four patients (7%) the results were poor. Sufficient and good results were recorded for all type A (1, 2, 3) and type B (1, 2) fractures. Poor results were observed for type C2 and type C3 fractures.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The term pilon fracture was first used in 1911 by French radiologist Destot and comes from the French for pestle. Tibia pilon fracture is a fracture including the metaphysis section at the distal part of the tibia (plafond roof). The tibia plafond forms a roof over the talus bone and has a smooth surface ensuring contact between the distal tibia and the talus. The ankle is formed by the plafond above and by the talus below and by the lateral, medial, and posterior malleoli. In the sagittal plane the plafond is concave, while in the coronal plane it is convex. The anterior section of the plafond is wider to tolerate axial loads.
There is a broad range in terms of surgical treatment for tibia pilon fractures. There are several treatment alternatives, especially for the treatment of high-energy complex pilon fractures. None of these methods can be claimed as gold standard. Infection is commonly observed after internal fixation. McFerran et al. (1992) reported a 54% complication rate in treatment of these types of fractures, while Helfet et al. (1994) reported a complication rate of 70%. The final result is arthrodesis in 26% of patients, with amputation in 16% of patients. Teeny and Wiss (1993) reported complications like pseudoarthrosis, infection, and implant breakage in 50% of 60 patients operated on for tibia pilon fracture. When selecting the fixation method for a tibia pilon fracture, evaluation of the soft tissue condition and fracture fixation quality is important, to prevent complications (Casstevens et al. 2012; Newman et al. 2011). These complications are more common with high-energy trauma (Mauffrey et al. 2011). In addition to treatment planning in high-energy trauma, careful monitoring of soft tissue condition, and waiting 7–14 days for reduction of soft tissue edema are necessary to reduce the risk of complications (Yalçın et al. 2007).
Treatment of open fractures is difficult. To decrease complication risk, several methods and combinations have been described like minimally invasive methods, two-stage procedures, unilateral fixator applications, hybrid jointed ankle fixators, and circular Ilizarov external fixator. No matter which method is used, major skin incisions should be avoided (Mauffrey et al. 2011).
A staged protocol is important in treatment of tibia pilon fractures (Boraiah et al. 2010; Wyrsch et al. 1996). To date there is no consensus on the treatment of complications after pilon fractures such as delayed or nonunion and pseudoarthrosis. According to some studies, the infection risk during pilon fracture treatment approaches 55% (Joveniaux et al. 2010; Zelle et al. 2006). Infection risk increases with longer duration of the surgical procedures and open fractures (Miller et al. 2012). Hyperglycemia associated with diabetes is an additional serious risk factor for infection (Theuma and Fonseca 2003). This is related to microvascular pathology that creates ischemia in the extremities. These complications have also increased the popularity of external fixation. Until skin creases are clearly seen, patients should rest with leg elevation. Temporary fixator use may enable joint mobilization and thereby assist with edema reduction (Yalçın et al. 2007). A temporary fixator application means that the patient must undergo two surgical procedures, and treatment costs will be higher. Therefore, the ultimate treatment should take place soon after the trauma. The external circular ilizarov fixator enables earlier surgery post-trauma and earlier joint mobilization. Another advantage of the Ilizarov external fixation method is that it allows early ambulation with load bearing (Leung et al. 2004; McDonald et al. 1996).
2 Surgical Technique
Fifty-three patients with tibia pilon fractures were treated at our clinic between 2010 and 2014 using the Ilizarov method. The patients included 40 males and 13 females. The mean age was 45.3 years (range = 23–62 years). High-energy trauma such as traffic accidents and falls from a height was involved in more than 80% of the patients. According to AO classification, four fractures were type A1, four were type A2, four were type A3, eight were type B1, five were type B2, seven were type B3, six were type C1, seven were type C2, and eight were type C3. The surgical procedure followed these stages:
-
1.
External ring fixation, according to the fracture shape.
-
2.
Fracture continuity was ensured.
-
3.
Fixation and compression of fracture fragments with reduction and arrangement was ensured using Kirschner (K) wires.
The location of Ilizarov rings was completed according to the fracture type in the AO classification. A type fractures had the Ilizarov apparatus planned and set with three full rings used, B type fractures had two full rings and one half ring, and C type fractures had three full rings and one half ring. Patients were positioned in supine and transcalcaneal traction was applied. Reduction after ligamentotaxis was checked using fluoroscopy.
While applying the three-ring Ilizarov apparatus, K-wires linked to the proximal ring were passed through the proximal metaphysis of the tibia. Wires holding the central ring passed close to the distal part of the proximal fragment of the tibia. Changes in fragment location were noted when placing the wires. Depending on fragment location, they were inserted from inside to outside, or outside to inside, and wires with stops and abutment points were used. The distal ring was joined to the base rings without wires. A wire with an abutment point (stop) was passed from the calcaneus, and the half ring was fixed and tensioned. Diastasis was created at the ankle joint, and fragment displacement was roughly corrected. The remaining fragment displacement was reduced with an awl (Kirschner, hook) “joystick” with 3–4 mm pointed tip and reduced percutaneously under fluoroscopic control. Fragment fixation was completed using 1.8–2.0 mm olive wire. Using the distal tip of the tibia as a reference point, the fragments of the anterior and posterior edges of the ankle joint surface were reduced. It is important that reduction of the tibia plafond forming the ankle joint surface be carefully performed. However, in situations where this may not be possible especially in C type fractures, reduction was attempted after a small incision was made, and the reduced fragments were fixed with olive wires. To prevent supination and drop foot, the foot was fixated with the ankle in neutral alignment. The wire through the calcaneus was generally removed after 1 month (40–45 days for some type C2 and C3 fractures), and ankle movement was allowed.
Patients were not allowed to bear weight until the wire was removed. After the calcaneal wire was removed, ankle movement and partial weight-bearing were allowed. No bone grafts were used. While surgery was completely closed in 43 patients, in 10 patients a small incision was made to ensure reduction.
3 Results
Mean union duration was 14.6 months (12–22 months). According to the Mazur’s criteria, 39 patients (74%) sustained very good or good results. In ten patients (19%) sufficient results were obtained, while in four patients (7%) the results were poor. Sufficient and good results were recorded for all type A (1, 2, 3) and type B (1, 2) fractures. Poor results were observed for type C2 and type C3 fractures.
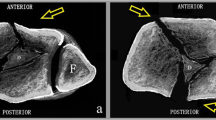
No patient developed an infection or deep vein thrombosis. In 11 patients superficial soft tissue infections occurred around the K-wires. This situation was treated with oral antibiotics and dressings. In four out of seven patients with open fracture, skin necrosis was observed after surgery (Fig. 38.1). In all patients wounds healed without complications except for one patient that required a skin graft. More than 80% of the patients had full return of ankle range of motion. Ankle arthrodesis was performed in two patients.
4 Discussion
The Ilizarov method is a minimally invasive method allowing fixation of the bone with the aid of K-wires, threaded rods, and a frame (Fig. 38.2). It was described by Gavriil Abramovich Ilizarov at the beginning of the 1950s. It gained global popularity after an Italian reporter was treated with this method. It provides satisfying results for open fractures, pseudoarthrosis, lengthening extremities, and deformities. Among the advantages of this method are that it is minimally invasive, the patient may ambulate with early weight-bearing and may return quickly to normal daily activities, and the apparatus can be adjusted during recovery to maintain ligamentotaxis effects.
For a more stable fixation with the Ilizarov method, three or four rings may be used. If the fracture is closer than 3–4 cm from the joint level, a fourth ring may be used as a foot ring for more stable fixation including the foot. To shorten the surgery duration, planning should be made before surgery, and the rings preassembled. The rings should be perpendicular to the mechanical axis and parallel to each other. Full rings created by joining two half rings should be placed at least 2 cm from the skin. The Ilizarov frame should be at least 2 cm from the skin to reduce pressure on the skin from the frame if edema develops in the extremity and to reduce the necrosis risk. In practice, a distance of two fingers between the frame and skin should be sufficient. However, leaving more space between the frame and the skin to reduce this risk may cause a biomechanically weaker fixation. Leaving four rods between the rings ensures better fixation. Carbon rings should be used to be able to evaluate joint congruency on postoperative radiographs.
If the fracture line is closer than 3–4 cm to the joint level, the foot should be included in the frame for more stable fixation. When including the foot within the Ilizarov system, care should be taken that it not be placed in a drop foot position (Dağlar 2016).
Another advantage of Ilizarov external fixator is ligamentotaxis (Bone et al. 1993; Lovisetti et al. 2009). Ligamentotaxis is an important factor in functional healing of fractures. However, the necessity of including the ankle may be considered a disadvantage (Mauffrey et al. 2011). Foot fixation does not always result in decreased ankle movement. Okcu and Aktuğlu (2004) stated that external fixator use ensured better ankle movement. Additionally, there are reports stating that external fixator application provides worse results in terms of post-traumatic arthrosis (White et al. 2010), while there are also reports stating that it makes no difference (Davidovitch et al. 2011). To prevent limited subtalar joint movement, it is recommended that wires passing through the ankle joint bypass the talus (Fırat et al. 2013). Another advantage of the Ilizarov system is that it allows stable fixation in osteoporotic bone.
While threaded rods may be used for fixation of the frame proximal to the fracture line, for distal ring fixation at the distal tibia, we may use K-wire and reduction (olive) wires. The threaded rods should be inserted 90 degrees perpendicular to each other. Kirschner (K) wires should be inserted into the distal tibia at a minimum of 60 degrees apart (Aktuğlu and Özkayın 2013). Fracture fragment reduction may be easier with olive wires (Yalçın et al. 2007). With ligamentotaxis, unreduced fragments may be reduced with a pointed awl or K-wire “joystick.” The surgical procedure should be performed on large bone fragments (Mauffrey et al. 2011). Tension on the wires reduces the infection risk.
While infection is a risk of every surgery, Ilizarov apparatus application especially for high-energy trauma reduces this risk (Yalçın et al. 2007). The risk of deep infection is lower compared with open surgery. The complication incidence rate in patients with internal osteosynthesis may approach 70% (Helfet et al. 1994). A comparative prospective randomized study of internal osteosynthesis and external osteosynthesis by Wyrsch et al. (1996) reported lower complication rates in the group with external osteosynthesis. Research by El-Mowafi et al. (2015) stated that Ilizarov apparatus external fixator use reduced the need for a large surgical incision and was a useful method for pilon fracture treatment.
In retrospective research, Okcu and Aktuğlu (2004) reported that patients treated with the Ilizarov method had better ankle joint mobility than after open fixation. Fırat et al. (2013) showed that hinged Ilizarov external fixator use was an effective treatment method for tibia pilon fractures.
Pilon fracture treatment complication rates are high (Helfet et al. 1994). While choosing the fixation method, it is important to take note of complication risks linked to the soft tissue condition (Casstevens et al. 2012; Newman et al. 2011).
Complication rates tend to be lower with treatment methods involving external fixators (Wyrsch et al. 1996). However, results may be worse for multifragmented pilon fracture cases, especially with central collapse. As fragments with no link to soft tissue cannot be reduced with ligamentotaxis, they may require fixation with minimally invasive methods (Yalçın et al. 2007). In these types of cases, additional fixation with percutaneous cannula screws and grafting may provide better results (Ersan et al. 2005). Early ankle mobilization may prevent Sudeck’s atrophy and may improve cartilage healing (Ersan et al. 2005). Following external fixation, minimally invasive plates are useful to enable early ankle movement. However, it should not be forgotten that good results strictly with external fixator use have been reported (Aktuğlu and Özkayın 2013; Pavolini et al. 2000; Vidyadhara and Rao 2006).
Factors that limit the use of the Ilizarov apparatus method are the difficulty in using the device and complications related to its external presence. While reduction of fractures with ligamentotaxis is the aim of using external fixators, it is difficult to ensure full repositioning of multifragmented fractures of the distal joint surface of the tibia (Bone et al. 1993; Lovisetti et al. 2009). For better reduction of the fracture line, it may be helpful to use arthroscopically assisted minimally invasive methods (Fischer et al. 1991). Opinions differ in terms of two-stage surgery (Aktuğlu and Özkayın 2013; Pugh et al. 1999; Sirkin et al. 1999).
5 Conclusion
The Ilizarov apparatus should be applied according to the AO classification of fractures of the tibial distal epiphysis. For closed reduction with ligamentotaxis of fragments in distal tibial epiphysis fractures, fixation should be performed with wires. In the presence of multifragmented displaced fractures, a pointed awl allows percutaneous fragment reduction without the need to open the fracture. Percutaneous Ilizarov system use does not disrupt endosteal and periosteal nutrition, and fragments may be compressed with olive wires (Vidyadhara and Rao 2006). When closed reduction is not possible, reduction may be performed using a small incision and olive wire fixation.
Treatment of pilon fractures with a circular external fixator without internal fixation (in accordance with Ilizarov principles) appears to require less soft tissue dissection. The Ilizarov external fixator system is a reliable method for treatment of fragmented pilon fractures with low complication rates.
References
Aktuğlu K, Özkayın N (2013) Tibia pilon kırıklarında cerrahi yaklaşımlar. TOTBİD Dergisi 12:142–152
Bone L, Stegemann P, McNamara K, Seıbel R (1993) External fixation of severely comminuted and open tibial pilon fractures. Clin Orthop Relat Res 292:101–107
Boraiah S, Kemp TJ, Erwteman A, Lucas PA, Asprinio DE (2010) Outcome following open reduction and internal fixation of open pilon fractures. J Bone Joint Surg Am 92:346–352
Casstevens C, Le T, Archdeacon MT, Wyrick JD (2012) Management of extra-articular fractures of the distal tibia: intramedullary nailing versus plate fixation. J Am Acad Orthop Surg 20:675–683
Dağlar B (2016) Tibia pilon kırıklarının tedavisinde kullanılan cerrahi yaklaşımlar. TOTBİD Dergisi 15:231–239
Davidovitch RI, Elkhechen RJ, Romo S, Walsh M, Egol KA (2011) Open reduction with internal fixation versus limited internal fixation and external fixation for high grade pilon fractures (OTA type 43C). Foot Ankle Int 32:955–961
El-Mowafi H, El-Hawary A, Kandil Y (2015) The management of tibial pilon fractures with the Ilizarov fixator: the role of ankle arthroscopy. Foot (Edinb) 25:238–243
Ersan Ö, Çelik B, Kovalak E, Ateş Y (2005) Tibia Pilon Kırıkları. TOTBİD Dergisi 4:127–137
Fırat A, Tecimel O, Işık Ç, Özdemir M, Öçgüder A, Bozkurt M (2013) Tibia pilon kırıklarının tedavisinde İlizarov eksternal fiksatörü:Ayak bileği eklemli mi yoksa sabit mi? Eklem Hastalik Cerrahisi 24:133–138
Fischer MD, Gustilo RB, Varecka TF (1991) The timing of flap coverage, bone-grafting, and intramedullary nailing in patients who have a fracture of the tibial shaft with extensive soft-tissue injury. J Bone Joint Surg Am 73:1316–1322
Helfet DL, Koval K, Pappas J, Sanders RW, DiRasquale T (1994) Intraarticular “Pilon” fracture of the tibia. Clin Orthop Relat Res 298:221–228
Joveniaux P, Ohl X, Harisboure A, Berrichi A, Labatut L, Simon P, Mainard D, Vix N, Dehoux E (2010) Distal tibia fractures: management and complications of 101 cases. Int Orthop 34:583–588
Leung F, Kwok HY, Pun TS, Chow SP (2004) Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury 35:278–283
Lovisetti G, Agus MA, Pace F, Capitani D, Sala F (2009) Management of distal tibial intra-articular fractures with circular external fixation. Strategies Trauma Limb Reconstr 4:1–6
Mauffrey C, Vasario G, Battiston B, Lewis C, Beazley J, Seligson D (2011) Tibial pilon fractures: a review of incidence, diagnosis, treatment, and complications. Acta Orthop Belg 77:432–440
McDonald MG, Burgess RC, Bolano LE, Nicholls PJ (1996) Ilizarov treatment of pilon fractures. Clin Orthop Relat Res 325:232–238
McFerran MA, Smith SW, Boulas HJ, Schwartz HS (1992) Complications encountered in the treatment of pilon fractures. J Orthop Trauma 6:195–200
Miller AG, Margules A, Raikin SM (2012) Risk factors for wound complications after ankle fracture surgery. J Bone Joint Surg Am 94:2047–2052
Newman SD, Mauffrey CP, Krikler S (2011) Distal metadiaphyseal tibial fractures. Injury 42:975–984
Okcu G, Aktuğlu K (2004) Intra-articular fractures of the tibial plafond. A comparison of the results using articulated and ring external fixators. J Bone Joint Surg Br 86:868–875
Pavolini B, Maritato M, Turelli L, D’Arienzo M (2000) The Ilizarov fixator in trauma: a 10-year experience. J Orthop Sci 5:108–113
Pugh KJ, Wolinsky PR, McAndrew MP, Johnson KD (1999) Tibial pilon fractures: a comparison of treatment methods. J Trauma 47:937–941
Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr (1999) A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma 13:78–84
Teeny SM, Wiss DA (1993) Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res 292:108–117
Theuma P, Fonseca VA (2003) Novel cardiovascular risk factors and macrovascular and microvascular complications of diabetes. Curr Drug Targets 4:477–486
Vidyadhara S, Rao SK (2006) Ilizarov treatment of complex tibial pilon fractures. Int Orthop 30:113–117
White TO, Guy P, Cooke CJ, Kennedy SA, Droll KP, Blachut PA et al (2010) The results of early primary open reduction and internal fixation for treatment of OTA 43.C-type tibial pilon fractures: a cohort study. J Orthop Trauma 24:757–763
Wyrsch B, McFerran MA, McAndrew M (1996) Operative treatment of fracture of the tibial plafond: a randomized prospective study. J Bone Joint Surg Am 78:1646–1657
Yalçın N, Uğurlu M, Ezdeşir Ö, Doğan M, Tosun N (2007) Tibia pilon kırıklarında fonksiyonel bir tedavi yöntemi: ilizarov eksternal fiksatör. Turkish Med J 1:17–21
Zelle BA, Bhandari M, Espiritu M, Koval KJ, Zlowodzki M, Evidence-Based Orthopaedic Trauma Working Group (2006) Treatment of distal tibia fractures without articular involvement: a systematic review of 1125 fractures. J Orthop Trauma 20:76
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gahramanov, A., Aytekin, K., Esenyel, C.Z. (2019). Treatment of Tibia Pilon Fractures with the Ilizarov Method. In: Doral, M., Karlsson, J., Nyland, J., Benedetto, K. (eds) Intraarticular Fractures. Springer, Cham. https://doi.org/10.1007/978-3-319-97602-0_38
Download citation
DOI: https://doi.org/10.1007/978-3-319-97602-0_38
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-97600-6
Online ISBN: 978-3-319-97602-0
eBook Packages: MedicineMedicine (R0)