Abstract
Bone bruises represent an important cause of pain and loss of joint function. They represent histopathological lesions that can be detected by magnetic resonance imaging that depict hemorrhage, edema, and microtrabecular subchondral bone fractures. They can be observed using low signal intensity in T1-weighted sequences in fat-suppressed sequences or using high signal intensity in T2-weighted sequences. They may represent from traumatic or non-traumatic lesions with wide spectrum of distinctive features.
Traditionally, bone bruises are treated by limiting activities that increase joint symptoms. Lesions formed by low-energy trauma usually last for a shorter time than high-energy lesions. Bone bruises after high-energy trauma may present with a subchondral or intra-articular fracture pattern. Recovery from high-energy bone bruise lesions may take several months or even years. Larger bone bruises that involve subchondral bone are more likely to be associated with other osteochondral sequelae, including long-term osteoarthritis. Although more commonly observed among athletically active patients, bone bruises may occur in a wide variety of patients. There is no report on the most effective surgical treatment method for these lesions. Several surgical approaches exist. There is a need for prospective studies to investigate the efficacy of differing surgical approaches that treat bone bruise lesions. High-quality patient outcome studies that include sequential magnetic resonance imaging (MRI) evaluation and return to sport and daily activity rates will help to better delineate surgical outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Bone bruises cannot be easily identified through plain radiographic imaging. Since the late 1980s, magnetic resonance imaging (MRI) use has increased the diagnosis of these lesions (Berger et al. 1989; Mandalia et al. 2005; Vellet et al. 1991; Yao and Lee 1988). A bone bruise is defined as focal signal changes in subchondral bone marrow without any cortex fracture, microtrabecular fractures, hemorrhage, or edema (Rangger et al. 1998; Ryu et al. 2000). Bone bruises were primarily detected around the knee joint, especially after MRI to investigate anterior cruciate ligament (ACL) ruptures and other knee ligament injuries (Ege et al. 2001; Engebretsen et al. 1993; Graf et al. 1993; Vellet et al. 1991; Yao and Lee 1988). In contrast, hip, ankle, shoulder, wrist, and other small joint bone bruise injuries have been visualized less frequently than in relation to knee injuries. Bone marrow edema (BME) is frequently encountered on MRI examinations with the complaint of unexplained joint pain. BME is also seen in various joint diseases. There are ischemic, mechanical, and reactive conditions in the etiology of BME (Mink and Deutsch 1989). Microfractures, stress fractures, and bone bruises are seen in the mechanical etiologies of BME. BME without trauma has been described primarily at the hip joint. Unfortunately, there are few reports on the prognosis as well as short-term and long-term effects of these painful lesions. The resolution of bone bruises, effects on short-term recovery and function, long-term sequelae, and the clinical implications of these results are not yet well established. Bone bruises cannot be directly identified using standard radiographs. However, they can be detected on radiographs following the presence of accompanying avulsion fractures or fissures. Bone bruises are histopathologically based on edema and hemorrhage. Due to the fatty nature of the subcortical bone marrow, MRI of edema is mainly based on fat-suppressed sequences. While bone bruise appears in low signal intensity in T1 sequences, it is encountered in high signal intensity in T2-weighted sequences. In particular, it gives insight into the acuity of the T2 imaging lesion (Mandalia et al. 2005; Nakamae et al. 2006). More information can be obtained about the increased density of bone edema by the short tau inversion recovery (STIR) imaging in which the signal in the normal medullar is suppressed. Bone bruise and BME are often indistinguishable on MRI. The trauma history and clinical presentation of the patient must be taken into account to make a better distinction between the two (Figs. 1.1 and 1.2).
2 Bone Bruise Classification
Mink and Deutsch (1989) were the first to classify bone bruise. Despite many classification attempts, the clear distinction between an existing cortical fracture and hidden fracture that reaches the osteochondral surface has not been fully established. Mink and Deutsch (1989) divided these lesions into four groups: bone bruises, stress fractures, femur and tibia fractures, and osteochondral fractures. On MRI, femur, tibia, and osteochondral fractures are more prominent than the other two lesion groups. Lynch et al. (1989) modified the classification of Mink and Deutsch (1989) to distinguish three types of bone bruises (Table 1.1).
Using MRI, Vellet et al. (1991) prospectively investigated 120 patients with acute knee injury. The bone bruises observed were classified as reticular, geographic, linear, impaction, and osteochondral fractures. The most common occult lesions were the reticular type. These were wide lesions spreading to the periphery distant from the cortex or joint surface. The geographic types were lesions that displayed continuous signal changes representing coalescence with subchondral bone. Osteochondral fractures and impact fractures represented intra-articular fractures that reach the joint surface. Difficulties can be encountered with almost all classifications. Since this is a radiologic classification, its prognostic value is unclear; therefore, its use is limited for clinical assessment.
3 Bone Bruise Location and Mechanism
The majority of bone bruise and BME research has focused on the knee joint. The reason for this is that MRI screenings are common following potential knee ligament injuries. The mechanisms of injury may be direct, or the bones that form the joint may be in forceful contact with each other. For this reason, bone bruises are common around the knee joint.
A study of 434 patients with acute knee injuries reported a 20% incidence of bone bruises, most in association with ACL rupture (Lynch et al. 1989). With the increased use of MRI in knee ligament injury diagnosis, many bone bruising investigations on lesions are associated with injuries to the lateral collateral ligament, medial collateral ligament, posterior cruciate ligament, and, of course, the ACL (Graf et al. 1993; Kaplan et al. 1992; Murphy et al. 1992; Speer et al. 1995; Tung et al. 1993). Terzidis et al. (2004) examined the MRI of 255 patients with acute knee injuries, and 27.8% of the patients were found to have a bone bruise. Approximately 77% of these patients had sustained an ACL rupture. During the acute period, bone bruises were observed on MRI in more than 80% of ACL ruptures (Rosen et al. 1991; Speer et al. 1995; Spindler et al. 1993). In studies which included patients scanned over a longer period, a smaller incidence ranging from 40 to 56% was reported. In a study by Spindler et al. (1993), it was reported that among knees that displayed a bone bruise, 86% occurred at the lateral femoral condyle. Sixty-five percent of patients with a lateral femoral condyle bone bruise had a matching lateral tibial plateau bone bruise (Spindler et al. 1993). These matching lesions were associated with the valgus knee injury mechanism that injured the ACL. The existence of a “kissing lesion” was also supported by Kaplan et al. (1992) in a study they conducted by examining 100 MRI images of patients with acute ACL injuries. In association with sudden ACL rupture, the injury mechanism that led to bone bruising was blunt trauma from lateral tibial plateau and lateral femoral condyle impact. Chondral defects and intra-articular fractures related to this traumatic injury mechanism were likely precursor to bone bruise formation.
Contusion in the lateral knee compartment correlates with the ACL injury mechanism. After an ACL rupture, the tibia is subluxed in front of the femur, particularly on the lateral side. During this axial and valgus force “pivot shift” injury mechanism, the middle part of the lateral femoral condyle and the posterior aspect of the lateral tibial plateau come into direct impact creating these lesions.
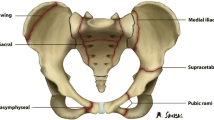
The posterior aspect of the lateral tibial plateau may be structurally weaker than the lateral femoral condyle, and thus lesions of the lateral tibial plateau are more common. Bone bruises may also develop in the knees of patients who experience ipsilateral traumatic hip dislocations. In patients who have sustained hip dislocation, bone bruises may occur at the femoral head or acetabulum with or without associated femoral head or acetabular fracture (Schmidt et al. 2005). Pinar et al. (1997) reported that bone bruises were more common in the medial ankle compartment after ankle ligamentous injuries. Ege et al. (2001) reviewed MRI of 49 patients who presented with knee trauma and reported bone bruises (n = 33) as the most common finding. Baker et al. (2016) examined the MRI of professional ice hockey players who experienced a total of 31 ankle injuries. Three different researchers reviewed each MRI for bone bruises and fractures that were not detectable on plain radiographs. The researchers reported that the number of serious bone bruises was eight, seven, and six, respectively, while the fractures were found to be ten, eight, and eight. This suggests greater disagreement among researchers in terms of bone bruise severity at the time of diagnosis (Baker et al. 2016).
The presence of occult bone bruise without cortical bone injury has become a hot research topic. Miller et al. (1998) reported the incidence of bone bruises associated with medial collateral ligament injury to be approximately 45%. Most of the studies on ACL injury and pivot shift movement have focused on the lateral femur condyle. After patellar dislocation, an isolated bone bruise may also occur at the lateral femur condyle (81–100%) and the medial patella (30%) (Wright et al. 2000). Talus and medial malleolus bone bruises are found in 40% of lateral ligament ankle sprains (Dienst and Blauth 2000; Sijbrandij et al. 2000). Bilateral calcaneal bone bruises have also been reported after axial loading. These bone bruises may be accompanied with avulsion fractures associated with the comparatively stronger ligaments than growth plates in childhood (Figs. 1.3 and 1.4).
4 Clinical and Histological Findings
It is often difficult to distinguish clinical findings of bone bruises as the traumas leading to their appearance are accompanied with soft tissue lesions and intra-articular injuries. Greater focus on these associated lesions likely contributes to a bone bruise diagnosis not being made during the initial clinic visit. While these may occur due to ACL injury in the knee joint, they can also be associated with other ligament injuries, patellar dislocation, and strains without bone trauma. Bone bruises may also occur after traumatic hip lesions, intracapsular fractures, femoroacetabular impingement, and load distribution impairment from acetabular roof mismatches in congenital hip dysplasia cases. Additionally, ligament injuries at the ankle and in other joints may present as stress fractures, load distribution changes, and ischemic lesions. Due to the wide etiological spectrum of bone marrow lesions, it is often difficult to recognize clinical markers and symptoms. Vincken et al. (2006) observed that patients with bone crush injuries had worse function (in terms of pain-free walking, normal range of motion) and that their activity scores were lower when they were accompanied by intra-articular pathologies. Alanen et al. (1998) followed 95 patients with a 27% bone bruising incidence after inversion ankle injuries. They reported no significant differences in physical activity, limitation of walking, duration of return to work, and clinical scores between patients who had and who did not have a bone bruise.
Valuable histological findings may come from biopsies being taken at different times following joint injury (Fang et al. 2001; Johnson et al. 2000). Following acute knee lesions, Rangger et al. (1998) detected trabecular bone microfractures, edema, and hemorrhage. In a study of Johnson et al. (2000), all patients displayed evidence of articular cartilage and subchondral bone changes following ACL reconstruction. Chondrocytes in the superficial region of the articular cartilage revealed different stages of degeneration. Loss of matrix proteoglycan and osteocytosis were observed in the underlying subchondral bone (Johnson et al. 2000). Fang et al. (2001) reported approximately ten times more intra-articular matrix protein breakdown products in the ACL-injured knee of patients compared with the uninjured knee.
Using in vivo animal models, histological investigations of the effects of blunt trauma on articular cartilage have also been performed (Thompson Jr et al. 1991). It is suggested that bone bruises, which produce no obvious surface deterioration, may lead to chondrocyte loss by creating histological and biochemical articular cartilage surface damage (Donohue et al. 1983; Newberry et al. 1998; Terzidis et al. 2004). There are several mediators associated with bone edema presentation and inflammatory processes that may contribute to articular cartilage degeneration following trauma. Articular cartilage damage can occur from direct lesions or from intra-articular fractures. New tissue at the intra-articular fracture site will be weaker than normal tissue and more fragile to loading forces, particularly shear forces. As a result the risk of joint osteoarthrosis increases (Bretlau et al. 2002; Fang et al. 2001; Kim et al. 2000; Rangger et al. 1998).
5 The Natural Course
Bone bruises are lesions that can heal spontaneously. However, the healing time frame is quite variable. This variability is due to the fact that evaluations based on MRI findings often do not correlate with the patient’s clinical presentation. It has been reported that patients with bone bruises take longer for symptom resolution, have higher pain scores, take longer to recover normal joint range of motion, and take longer to return to pain-free walking (Johnson et al. 1998; Johnson et al. 2000; Vincken et al. 2006; Wright et al. 2000).
Miller et al. (1998) reported that recovery from bone bruise injuries took 6–12 weeks when bruises were associated with nonsurgically treated medial collateral ligament injuries, displaying a better natural history, than bruises associated with surgically treated ACL injuries. In an ankle injury study using MRI, Pinar et al. (1997) reported that most bone bruises healed by 6–8 weeks, with only one patient displaying persistent bone bruising for approximately 7 months. Sijbrandij et al. (2000) reported that bone bruises at the ankle took longer to recover than bone bruises at the knee. They reported that ankle joint re-injuries and trauma mechanisms might have contributed to the prolonged recovery time (Sijbrandij et al. 2000). Other studies have reported longer recovery time frames. Bretlau et al. (2002) reported that 12% of the patients with acute knee injuries still had MRI evidence of bone bruising after 12 months. Among 13 patients who experienced conservatively treated hip dislocations or fractures, Wikerøy et al. (2012) reported that bone bruises regressed within 2 years. In studying 176 patients following acute knee joint injuries, Roemer and Bohndorf (2002) likewise reported that regression of these injuries took at least 2 years.
In a prospective study that examined the course of post-traumatized knees, Boks et al. (2007) followed 157 bone bruises detected in the femur and tibia of 80 patients. Mean lesion recovery time based on MRI evaluations was found to be 42.1 weeks (Boks et al. 2007). Graf et al. (1993) reviewed patients after an ACL injury and reported that while 71% of those who underwent MRI in the first 6 weeks displayed evidence of bone crushing, they appeared to be resolved 6 months later (Graf et al. 1993).
Vellet et al. (1991) reported that while all reticular structure knee bone bruises regressed, osteochondral sequelae were observed in two-thirds of the geographic-type lesions. Davies et al. (2004) reported that lesion regression occurred in two forms, either from the periphery or toward the joint margin in cases of bone crushing. Slower healing was observed in cases where regression was toward the joint margin. Osteochondral lesions accompanied each of these lesions. In these cases, the rehabilitation progress may need to be slowed or delayed, as the injured joint may be more prone to develop early osteoarthritis. In a case report, Dienst and Blauth (2000) described bilateral calcaneal bone crushing. The patient displayed complete recovery on MRI 6 months after he was restricted from weight-bearing for 4 months.
Although bone fractures have generally been reported to heal within about 6–12 weeks, reported healing times for bone bruises are much more variable. Geographic bone bruises and those with an osteochondral intra-articular component may last for many years. The clinical importance of this is not yet well established. However, chondral defects or intra-articular fractures may prolong bone bruise healing time. The severity of the initial injury, accompanying ligament injuries, the trauma pattern, patient compliance throughout the treatment period, rehabilitation program effectiveness, and the presence of lesions that reach the joint surface are important variables in bone bruise recovery.
6 Treatment
The basic approach should be to refrain from heavy weight-bearing loads at the injured area. In the acute phase, cryotherapy, joint elevation, and nonsteroidal anti-inflammatory drugs (NSAID) can be used for symptom relief. Braces can help to support or protect the affected area. Instead of weight-bearing, closed kinetic chain exercises, non-weight-bearing, and open kinetic chain exercises using an isokinetic instrument with range of motion control are preferred. Patients with osteochondral injuries or intra-articular fractures with geographic lesions should have bed rest, refrain from lifting heavy objects, and obtain partial weight bearing through crutch use. The amount of lesion regression and healing time frame should be monitored using serial MRI.
The presence of associated soft tissue and connective tissue lesions in the treatment of bone bruise affects the prognosis and treatment duration. Bone bruises that are identified after low-energy trauma such as knee medial collateral ligament injuries regress more quickly than more central, intra-articular bone bruises located in a primary weight-bearing zone. For patients with internal ligament ruptures or isolated bone crush injuries, it may be sufficient to limit joint loading until clinical findings improve. The situation is different after the high-energy trauma associated with ACL injury (Mankin 1982; Wright et al. 2000). Possible osteochondral injuries associated with high-energy ACL injuries may benefit from delaying full weight-bearing loads until both MRI and clinical evidence of bone bruise regression are observed (Johnson et al. 2000). In patients with ankle injuries, it is appropriate to use a supportive semirigid brace when crutch ambulation is started.
Different BME treatment options have been defined in the literature. The cause of traumatic pain is soft tissue damage, in addition to cortical and intra-articular damage. Nonsurgical treatment including NSAID can be used during the acute phase. Vasodilator pharmacological agents and bisphosphonates can be used in the subacute phase. Surgical core decompression may help reduce the increased intramedullary pressure, which is often associated with long-term pain. Although this application yields good results, it may also increase the risk of fracture and collapse in weight-bearing joints (Hofmann et al. 1993; Leder and Knahr 1995). Nabil et al. (2015) applied three percutaneous cannulated screws in 12 patients with extensive bone bruises in the tibia plateau. Patients were followed up for 15 months, with confirmation that patients complied with rehabilitation exercises and activities including no joint load during the initial 4 weeks post-surgery. On the fifth postoperative week, patients reported that their knee pain was significantly reduced and that they were able to apply full weight-bearing without pain (Ebraheim et al. 2015). This surgical procedure remains controversial, however. Some surgeons perform drilling and decompression treatments for patients with persistent bone bruises. This is followed by rehabilitation exercises and activities without joint loading for the first 6 weeks, followed by partial weight-bearing.
7 Conclusion
Despite several studies that have covered this topic, the natural course of bone bruise healing remains controversial and largely unknown. Researchers have focused bone bruise studies on the natural progression, classification, treatment, lesion histology, and whether or not it leads to articular cartilage damage. Bone bruises, which cannot be visualized by conventional imaging methods, can be diagnosed by MRI. Therefore, most studies on this topic rely on MRI evidence of tissue healing status. The reported periods of bone bruise healing are variable and range from 3 weeks to 2 years after the initial injury. Factors affecting this period include the severity of trauma, the type of lesion, the affected bone, and the dimensions of the contusion area, associated soft tissue lesions, post-injury rehabilitation methods, and patient compliance.
Despite these inconsistencies, it appears reasonable to protect the joint from weight-bearing in the early stages after bone bruise, as this is the time associated with microfracture healing. Clinical and MRI evidence of bone bruise healing coincides with decreased inflammation and edema. Progressive rehabilitation and NSAID or other pharmaceutical agent use may also help decrease patient symptoms.
Studies have reported that bone bruise regression may be related to the patient’s age, sporting activity, and type of bone bruise. Treatment is generally focused on limited activity and symptom management. Small bone bruises caused by low-energy trauma usually last for a short time. However, in bone bruises that arise from high-energy trauma, the healing can take several months, or even years. Larger bone bruises associated with high-energy trauma that include a subchondral injury component carry a greater risk of developing osteochondral sequelae leading to osteoarthrosis. In the presence of intra-articular fractures and chondral lesions, recovery and improvement of the activity score take a long time. As a result, it is necessary to undertake longer-term prospective studies to clarify the pathophysiology, natural history of bone bruises, and their relation with osteoarthritis and to determine the correct clinical approach. Even though traumatic causes are frequently responsible for the etiology of bone bruises, other causes should not be overlooked.
References
Alanen V, Taimela S, Kinnunen J, Koskinen SK, Karaharju E (1998) Incidence and clinical significance of bone bruises after supination injury of the ankle. A double-blind prospective study. J Bone Joint Surg Br 80:513–515
Baker JC, Hoover EG, Hillen TJ, Smith MV, Wright RW, Rubin DA (2016) Subradiographic foot and ankle fractures and bone contusions detected by MRI in elite ice hockey players. Am J Sports Med 44:1317–1323
Berger PE, Ofstein RA, Jackson DW, Morrison DS, Silvino N, Amador R (1989) MRI demonstration of radiographically occult fractures: what have we been missing? Radiographics 9:407–436
Boks SS, Vroegindeweij D, Koes BW, Bernsen RM, Hunink MG, Bierma-Zeinstra SM (2007) MRI follow-up of posttraumatic bone bruises of the knee in general practice. AJR Am J Roentgenol 189:556–562
Bretlau T, Tuxoe J, Larsen L, Jørgensen U, Thomsen HS, Lausten GS (2002) Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc 10:96–101
Davies NH, Niall D, King LJ, Lavelle J, Healy JC (2004) Magnetic resonance imaging of bone bruising in the acutely injured knee-short-term outcome. Clin Radiol 59:439–445
Dienst M, Blauth M (2000) Bone bruise of the calcaneus. A case report. Clin Orthop Relat Res 378:202–205
Donohue JM, Buss D, Oegema TR Jr, Thompson RC Jr (1983) The effects of indirect blunt trauma on adult canine articular cartilage. J Bone Joint Surg Am 65:951–957
Ebraheim N, Zhang J, Liu J, Gregory O, Johnson J, Blevins AL (2015) Preliminary result of percutaneous screw fixation for bone bruise of the tibial plateau. Orthopedics 38:747–750
Ege G et al (2001) Travmatik diz: MR bulguları. Ulus Travma Derg 7:60–65
Engebretsen L, Arendt E, Fritts HM (1993) Osteochondral lesions and cruciate ligament injuries. MRI in 18 knees. Acta Orthop Scand 64:434–436
Fang C, Johnson D, Leslie MP, Carlson CS, Robbins M, Di Cesare PE (2001) Tissue distribution and measurement of cartilage oligomeric matrix protein in patients with magnetic resonance imaging-detected bone bruises after acute anterior cruciate ligament tears. J Orthop Res 19:634–641
Graf BK, Cook DA, De Smet AA, Keene JS (1993) “Bone bruises” on magnetic resonance imaging evaluation of anterior cruciate ligament injuries. Am J Sports Med 21:220–223
Hofmann S, Engel A, Neuhold A, Leder K, Kramer J, Plenk H Jr (1993) Bone-marrow oedema syndrome and transient osteoporosis of the hip: an MRI-controlled study of treatment by core decompression. J Bone Joint Surg Br 75:210–216
Johnson D, Urban WP, Caborn DNM, Vanarthos WJ, Carlson CS (1998) Articular cartilage changes seen with magnetic resonance imaging detected bone bruises associated with acute anterior cruciate ligament rupture. Am J Sports Med 26:409–414
Johnson DL, Bealle DP, Brand JC Jr, Nyland J, Caborn DN (2000) The effect of a geographic lateral bone bruise on knee inflammation after acute anterior cruciate ligament rupture. Am J Sports Med 28:152–155
Kaplan PA, Walker CW, Kilcoyne RF, Brown DE, Tusek D, Dussault RG (1992) Occult fracture patterns of the knee associated with anterior cruciate ligament tears: assessment with MR imaging. Radiol 183:835–838
Kim YM, Oh HC, Kim HJ (2000) The pattern of bone marrow edema on MRI in osteonecrosis of the femoral head. J Bone Joint Surg Br 82:837–841
Leder K, Knahr K (1995) Effect of core decompression in the early stages of necrosis of the femoral head. Orthop Int 3:411–422
Lynch TC, Crues JV 3rd, Morgan FW, Sheehan WE, Harter LP, Ryu R (1989) Bone abnormalities of the knee: prevalence and significance at MR imaging. Radiology 171:761–766
Mandalia V, Fogg AJB, Chari R, Murray J, Beale A, Henson JH (2005) Bone bruising of the knee. Clin Radiol 60:627–636
Mankin HJ (1982) The response of articular cartilage to mechanical injury. J Bone Joint Surg Am 64:460–466
Miller MD, Osborne JR, Gordon WT, Hinkin DT, Brinker MR (1998) The natural history of bone bruises. A prospective study of magnetic resonance imaging-detected trabecular microfractures in patients with isolated medial collateral ligament injuries. Am J Sports Med 26:15–19
Mink JH, Deutsch AL (1989) Occult cartilage and bone injuries of the knee: detection, classification and assessment with MR imaging. Radiology 170:823–829
Murphy BJ, Smith RL, Uribe JW, Janecki CJ, Hechtman KS, Mangasarian RA (1992) Bone signal abnormalities in the posterolateral tibia and lateral femoral condyle in complete tears of the anterior cruciate ligament: A specific sign? Radiology 182:221–224
Nakamae A, Engebretsen L, Bahr R, Krosshaug T, Ochi M (2006) Natural history of bone bruises after acute knee injury: clinical outcome and histopathological findings. Knee Surg Sports Traumatol Arthrosc 14:1252–1258
Newberry WN, Mackenzie CD, Haut RC (1998) Blunt impact causes changes in bone and cartilage in a regularly exercised animal model. J Orthop Res 16:348–354
Pinar H, Akseki D, Kovanlikaya I, Araç S, Bozkurt M (1997) Bone bruises detected by magnetic resonance imaging following lateral ankle sprains. Knee Surg Sports Traumatol Arthrosc 5:113–117
Rangger C, Kathrein A, Freund MC, Klestil T, Kreczy A (1998) Bone bruise of the knee, histology and cryosections in 5 cases. Acta Orthop Scand 69:291–294
Roemer FW, Bohndorf K (2002) Long-term osseous sequelae after acute trauma of the knee joint evaluated by MRI. Skelet Radiol 31:615–623
Rosen MA, Jackson DW, Berger PE (1991) Occult osseous lesions documented by magnetic resonance imaging associated with anterior cruciate ligament ruptures. Arthroscopy 7:45–51
Ryu KN, Jin W, Ko YT et al (2000) Bone bruises: MR characteristics and histological correlation in the young pig. Clin Imaging 24:371–380
Schmidt GL, Sciulli R, Altman GT (2005) Knee injury in patients experiencing a high-energy traumatic ipsilateral hip dislocation. J Bone Joint Surg Am 87:1200–1204
Sijbrandij ES, van Gils AP, Louwerens JW, de Lange EE (2000) Posttraumatic subchrondral bone contusions and fractures of the talotibial joint occurrence of “kissing” lesions. Am J Roentgenol 175:1707–1710
Speer KP, Warren RF, Wickiewicz TL, Horowitz L, Henderson L (1995) Observations on the injury mechanism of anterior cruciate ligament tears in skiers. Am J Sports Med 23:77–81
Spindler KP, Schils JP, Bergfeld JA et al (1993) Prospective study of osseous, articular and meniscal lesions in recent anterior cruciate ligament tears by magnetic resonance imaging and arthroscopy. Am J Sports Med 21:551–556
Terzidis IP, Christodoulou AG, Ploumis AL, Metsovitis SR, Koimtzis M, Givissis P (2004) The appearance of kissing contusion in the acutely injured knee in the athletes. Br J Sports Med 38:592–596
Thompson RC Jr, Oegema TR Jr, Lewis JL, Wallace L (1991) Osteoarthritic changes after acute transarticular load. J Bone Joint Surg Am 73:990–1001
Tung GA, Davis LM, Wiggins ME, Fadale PD (1993) Tears of the anterior cruciate ligament: Primary and secondary signs at MR imaging. Radiology 188:661–667
Vellet AD, Marks PH, Fowler PJ, Munro TG (1991) Occult posttraumatic osteochondral lesions of the knee: Prevalence, classification and short-term sequelae evaluated with MR imaging. Radiology 178:271–276
Vincken PW, Ter Braak BP, van Erkel AR, Coerkamp EG, Mallens WM, Bloem JL (2006) Clinical consequences of bone bruise around the knee. Eur Radiol 16:97–107
Wikerøy AK, Clarke-Jenssen J, Ovre SA et al (2012) The natural history of bone bruise and bone remodelling in the traumatised hip: a prospective 2-year follow-up study of bone bruise changes and DEXA measurements in 13 patients with conservatively treated traumatic hip dislocations and/or fractures. Injury 43:1672–1677
Wright RW, Phaneuf MA, Limbird TJ, Spindler KP (2000) Clinical outcome of isolated subcortical trabecular fractures (bone bruise) detected on magnetic resonance imaging in knees. Am J Sports Med 28:663–667
Yao L, Lee JK (1988) Occult intraosseous fracture. Detection with MR imaging. Radiology 167:749–751
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kemal Aktuğlu, S., Kayaokay, K. (2019). Natural History of Bone Bruise. In: Doral, M., Karlsson, J., Nyland, J., Benedetto, K. (eds) Intraarticular Fractures. Springer, Cham. https://doi.org/10.1007/978-3-319-97602-0_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-97602-0_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-97600-6
Online ISBN: 978-3-319-97602-0
eBook Packages: MedicineMedicine (R0)